Abstract
Hypotension in patients under general anesthesia is prevalent and causes unfavorable outcomes. Carotid intima-media thickness (CIMT) is a surrogate marker for atherosclerosis and useful for evaluating the risk of cardiovascular diseases. We investigated the usefulness of preoperative CIMT measurement as a predictor of post-induction hypotension (PIH). The ultrasonographic measurement of CIMT was performed preoperatively on 82 patients scheduled for elective surgery under general anesthesia in a prospective, observational study. Mean blood pressure (MBP) was recorded before induction. Hypotension was defined as a 20% decrease in MBP from baseline. The ultrasonographic measurement of CIMT was unsuccessful in 2 (2.43%) patients, leaving 80 patients for analyses. Hypotension developed in 41 patients. CIMT was higher in the patient group with PIH than in the group without PIH (p < 0.001). There was statistically significant correlation between MBP decrease after induction and CIMT (r = 0.529, p < 0.0001). CIMT correlated positively with age (r = 0.739, p < 0.0001). The area under curve for CIMT was 0.753 [95% confidence interval (CI) 0.642–0.863]. The optimal cutoff value of CIMT was 0.65 mm with a sensitivity of 75.6% and a specificity of 74.4%. CIMT was an independent predictor of PIH after adjusting other factors with an odds ratio of 1.833 (95% CI 1.23–2.72; p = 0.003). The ultrasonographic imaging and measurement of CIMT can reliably predict hypotension with a 0.65-mm threshold level. We believe that the ultrasonographic measurements of CIMT may be included in point-of-care application in anesthesiology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Carotid intima-media thickness (CIMT) is an important marker that determines the amount of atherosclerotic burden in the common carotid artery [1]. CIMT is measured between the carotid artery of the intimal lumina and the medial–adventitial border with B-mode ultrasonography [2]. Ultrasonographic examination of changes in the arterial wall without atherosclerotic plaque has been shown to be a reasonable method for predicting atherosclerosis-related events, such as stroke, myocardial infarction, and peripheral artery disease. It is a cheap, reliable, and reproducible method [3, 4]. The American Heart Association guidelines recommend the ultrasonographic measurements of CIMT for intermediate-risk cerebrovascular diseases (CVD) in asymptomatic adults as class IIa level [5].
Intraoperative hemodynamic instability is one of the most important concerns for anesthesiologists during general anesthesia. Hemodynamic fluctuations in patients during anesthesia are important issues that cause adverse outcomes. In different clinical trials, unfavorable effects on organs due to intraoperative hypotension (IOH), including stroke and myocardial infarction, have been reported to be associated with mortality, morbidity, and prolonged hospital stay after general anesthesia and neurosurgical or cardiovascular surgeries [6,7,8,9]. There is no generally accepted definition of IOH. Different definitions, such as systolic arterial pressure (SAP) and mean arterial pressure (MAP) values below an absolute threshold, a decrease in blood pressure below patients’ baseline values, a combination of these parameters, and the duration of hypotension, and even therapeutic applications, such as infused fluid or vasopressor, are used [5]. Thus, the rates of hypotension were shown to be 5–99% during anesthesia in a large retrospective cohort study [10].
Factors that may cause hypotension after induction during general anesthesia include low preoperative SAP, advanced age (> 65 years), emergency surgery, male sex, and (ASA) IV patients in a large cohort study [11]. Although there are studies that predict post-induction hypotension (PIH), such as determining the severity of arteriosclerosis by measuring the brachial-ankle pulse wave velocity (baPWV) and central blood pressure and ultrasonography of inferior vena cava (IVC), [12, 13] there is no study showing the relationship between PIH and CIMT in literature review.
In this prospective, observational study, we investigated to predict PIH by the bedside ultrasonographic measurement of CIMT.
2 Methods
2.1 Study design
This clinical trial research was carried out at Diyarbakır State Hospital, Diyarbakır, Turkey. The approval of the study was granted by the Institutional Ethics Committee (Diyarbakir Gazi Yasargil Training and Education Hospital, decision no: 46/2018). A written approval was obtained from each participant.
The patients who were selected for elective surgery under general anesthesia were included in the study. The patients with CVD, coronary heart disease, coronary revascularization therapy, peripheral vascular disease, and allergies to general anesthetic agents were excluded from the study.
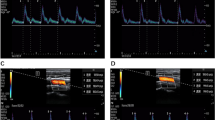
2.2 Assessment of CIMT
Assessment of CIMT was performed using B-mode ultrasonography including a 7.5-MHz superficial probe (Sonosite® M-Turbo, Sonosite, Bothell, WA, USA) by trained and approved sonographers. Carotid artery imaging was performed at an angle of about 20° to the opposite side of the neck when the patient was lying in a supine position. CIMT measurements were made only from the posterior (remote) wall of the main carotid artery. B-mode ultrasonographic measurements of CIMT were performed to determine the distance between the vessel lumen echogenicity and the media–adventitia echogenicity. Measurements were made from three different points of the right and left main carotid arteries: anterior oblique, lateral, and posterior oblique. Averages of the data from these three different angles were obtained. A predefined window of the right carotid artery bifurcation area, distal common carotid artery, bulb was scanned for plaques identified as focal thickening of the arterial wall (> 1.2 mm). Atherosclerotic plaque segments were not used for the measurement. The same operator manually calculated the measurements.
2.3 Anesthesia management
Intravenous catheters (18 G or 20 G) were inserted to all patients in the operating room. Standard electrocardiogram, non-invasive blood pressure, peripheral oxygen (O2) saturation, and end-tidal carbon dioxide monitoring were performed. The anesthetist caring for the patients were not aware of the study to overcome the bias. No acid premedication for stress ulcer was administered to the patients. Routine doses of midazolam [0.05–0.2 mg/kg of ideal body weight (IBW)], fentanyl (1–2 mcg/kg of IBW), propofol (2–2.5 mg of IBW), and rocuronium (0.6 mg/kg of IBW) were administered for general anesthesia. To interpret the incidence and degree of hypotension equally for the patients, the induction drugs were administered within a period 30 s.
Anesthesia was maintained by 40–50% O2 (air) and sevoflurane (1–2%). After orotracheal intubation, the mechanical ventilation was adjusted to maintain a tidal volume of 6–8 mL/kg, a partial carbon dioxide pressure of 35–40 mmHg, inspiratory:expiratory ratio of one-half with volume-controlled ventilation or pressure-controlled ventilation where appropriate (Datex Ohmeda, S/5 Avance, GE Healthcare, Helsinki, Finland). Anesthetic agents were adjusted to have a MAP of 20% and a heart rate of < 90 bpm, after we collected the data of our study, during the rest of the operation.
2.4 Data collection
Patients’ data were recorded prospectively during the study period. Patients’ age, gender, height, weight, body mass index (BMI) (calculated according to BMI = weight/height2 formula), and operation types were recorded. Comorbidities and medications were identified. Blood pressure values were measured from the left upper arm with an automated sphygmomanometer using oscillometric methods at intervals of 3 min. Heart rates and blood pressure values were recorded before the induction of anesthesia (baseline) and within 20 min after tracheal intubation [11]. If hypotension (MAP value below the 20% basal value) was observed, it was initially treated with fluid therapy. If the blood pressure did not improve, then 5–15 mg of ephedrine was applied. A bradycardic heart rate of below 45 bpm was accepted, and atropine (0.015 mg/kg) was administered if necessary.
Hypotension developed after the induction of anesthesia was defined as 20% lower than the MAP value.
2.5 Statistical analysis
The primary outcome measurement compared was defined as CIMT measurement predicting 20% MBP decrease after induction of general anesthesia between patients developed PIH and not developed PIH. We made a post hoc analysis according to the CIMT values between groups (0.782 ± 0.22 for patients developed PIH and 0.587 ± 0.189 for patients not developed PIH); our study power was 98.9% with α error of 0.05. G Power version 3.1.7 was used for sample size analysis.
We calculated 34 patients in each group for a type 1 error of 0.05 and a power of 0.9. To account for potential dropouts, the sample size was increased 80 patients.
The lowest MAP values after anesthesia induction of the patients were calculated and recorded as percent decreases relative to baseline values. The data were summarized using the mean and standard deviations (SD) and as percentages for discrete variables. The Kolmogorov–Smirnov one-sample test was used for the assumption of normal distribution of continuous variables. The demographic data were calculated by descriptive statistics. If the variables were normally distributed, then the central tendency was expressed as the mean (SD). The continuous variables were compared using Student’s t-test and Chi square test. Spearman correlation analysis was used to find out a correlation between the percentage of CIMT and MAP decline. Fisher’s exact test was used for categorical data and expressed in counts and percentages. The receiver operating characteristic (ROC) analysis and area under curve (AUC) were used to examine the whole patient’s CIMT to predict PIH. The 95% sensitivity and specificity values were calculated. Optimal cutoff values were defined.
Multivariate regression analysis was used to define the relationship between CIMT and PIH. Confounders, such as age, ASA physical status, and basal MAP values, were used. Differences were considered significant if p was < 0.05. Statistical analysis was performed using SPSS 22 (Chicago, Illinois, USA).
3 Results
3.1 Patient data
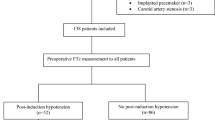
In total, 82 patients were recruited in the study. However, 2 (2.43%) patients were excluded because of poor CIMT visualizations at the right and left carotid arteries (Fig. 1). The mean age of the patients was 41.57 ± 15.97 years. The surgical procedures included in the study were as follows: general surgery, 39 (48.8%); orthopedic, 26 (32.5%); urology, 2 (2.5%); otolaryngology, 9 (11.3%). The demographic data of the patients are shown in Table 1.
3.2 Hemodynamic data
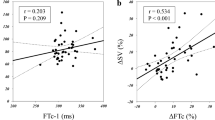
After induction of anesthesia, hypotension developed in 41 (51.25%) patients according to the study protocol. A 5–10 mcg dose of ephedrine was administered intravenously to 5 patients despite adequate fluid administration after PIH. Atropine was administered to 1 patient because of bradycardia accompanying hypotension. There was no difference between age, gender, and baseline heart rate variability between the group with PIH and the group without PIH (p > 0.05). Statistically significant values were found between the groups according to the baseline MAP and ASA values of the patients (p = 0.00; p = 0.037). CIMT was higher in the patient group with PIH than in the group without PIH (p < 0.001; Table 2). There was a statistically significant correlation between the mean blood pressure (MBP) decrease after induction and CIMT (r = 0.529, p < 0.0001; Fig. 2). CIMT correlated positively with age (r = 0.739, p < 0.0001; Fig. 3).
3.3 ROC analysis
ROC analysis for predicting PIH after general anesthesia induction demonstrated that AUC for CIMT was 0.753 [95% confidence interval (CI) 0.642–0.863; p < 0.0001; Fig. 4]. The optimal cutoff value of CIMT was 0.65 mm with a sensitivity of 75.6% and a specificity of 74.4%.
3.4 Regression analysis
Age, basal MBP, and CIMT values were found to be independent predictors of PIH in the logistic regression analysis (p < 0.05). There was an association between CIMT and PIH with an odd ratio of 1.833 (95% CI 1.23–2.72; p = 0.003). The results are shown in Table 3.
Age, basal MBP, and CIMT values are found as predictors according to the multivariate linear regression model (adjusted R2 = 0.346, R = 0.609, R2 = 0.371, F = 14.933; p < 0.0001). CIMT and baseline MBP had a positive association with the percentage decrease in MBP after the induction of anesthesia (p = 0.001 and p = 0.002, respectively) (Table 4).
4 Discussion
We found that ultrasonographic measurement of CIMT was a predictive value in patients with PIH in our study (p < 0.0001). The cutoff value that we can predict hypotension is 0.65 mm. We found that age and baseline MBP levels of patients were independent predictors of hypotension in logistic regression analysis.
IOH is a common side effect of anesthesia. IOH and hypertension were reported to be associated with postoperative complications and mortality [10, 14]. Monk et al. found that IOH was associated with 30-day mortality [15]. Walsh et al. showed an increase in acute renal damage and myocardial damage in patients with IOH (MBP < 55 mmHg) [7]. No clear description of IOH was identified. Bijker et al. identified over 140 definitions [10]. We used a 20% decrease in MBP from the baseline MBP in our study.
In the early period of atherosclerosis, there is an increase in the thickness of the intima-media of the arterial wall. This is observed in both the coronary arteries bed and the peripheral arteries [16]. Thus, CIMT, which is detected by non-invasive methods, predicts the presence or absence of coronary artery disease (CAD). In addition, CIMT can identify high-risk individuals for CAD and is associated with cardiovascular risk factors, including age, diabetes mellitus, and total cholesterol [3]. As of today, there is no CIMT threshold value and definition that poses a risk for CAD in association with CIMT and CAD. The general approach is that CIMT measurements above 0.9 mm or 1 mm are risk factors [17]. The mean CIMT measurements performed by Tossetto et al. was 0.88 mm for men and 0.89 mm for women [18]. Moreover, Stein et al. observed a 0.665–0.010 mm increase in CIMT per year [19]. Similar results have been achieved in our study (men, 0.595 mm; women, 0.789 mm). The reason why CIMT values are higher for women is probably that the mean age of the female patients in our study is higher than that of the males (male patients, 35.5 years; female patients, 48.1 years).
This is the first study to examine the relationship between CIMT and PIH in literature. We found a mean cutoff value of 0.65 mm (sensitivity: 75.6% and specificity: 74.4%). This value is equivalent to the CIMT of healthy individuals between 50 and 70 years of age [20, 21]. The presence of this relationship between PIH and this value is consistent with the knowledge that patients aged over 50 years were a risk factor for PIH according to the study by Reich et al. They retrospectively analyzed 4096 patients who underwent general anesthesia [22].
Bedside or point-of-care (POC) ultrasonography has emerged as a tool for diagnostic assessment in anesthesiology and perioperative period over the past two decades. It has been used for many applications such as transesophageal echocardiography, lung ultrasonography, confirmation of endotracheal tube positioning (airway ultrasonography), evaluation of gastric contents for aspiration risk (gastric ultrasonography), and estimation of intracranial pressure via the optic nerve sheath diameter [23, 24]. There are several studies to predict PIH by ultrasonography. Zhang et al. reported that preoperative POC IVC ultrasonography measurements can predict PIH in 75% of patients and the threshold was > 43% for Collapsibility Index [13]. However, this study has a number of limitations [25]. Firstly, previous studies had demonstrated moderate inter-rater reliability for IVC measurement. Secondly, IVC collapsibility may not be a reliable measurement because patients’ ventilation changed from spontaneous ventilation to positive ventilation, which can affect the results. In our study, sonographic CIMT has some superiority to sonographic IVC measurements with more convenient results, better images, and it is not affected by patients’ ventilation characteristics. In another study, Morimoto et al. identified the relationship between the level of arteriosclerosis and blood pressure changes during anesthesia induction by measuring the baPWV and central blood pressure. They concluded that baPWV was a predictor of PIH [26]. Compared with simpler measures, like the ankle-brachial index, CIMT has the psychological advantages of an imaging tool as patients and physicians tend to believe in visible structures rather than abstract concepts. Moreover, it is important to note that PIH can be predicted on certain threshold values of CIMT in our work. Therefore, we proposed that CIMT be used as a screening tool to identify subjects at risk for PIH.
5 Limitations
This study has several limitations. Firstly, the sample size is small and it limits the power of subgroup analysis. Secondly, observer dependency in our manual measurements is higher than semiautomated CIMT measurements. It has been shown that the ultrasound settings and the observer’s interpretation of the CIMT may affect the measurement [27]. Because of the inability of the standard measurement of CIMT and imaging, researchers have used dissimilar ultrasound protocols, resulting in variability in CIMT measurements [28]. However, highly reproducible measurements can be obtained with an experienced CIMT reader through manual tracing [29]. We have used higher frequency ultrasound probes to obtain CIMT imaging. However, manual CIMT measurements are time consuming. In order to overcome the inter-reader and intra-reader variability of the CIMT measurements, semiautomated measurements have been introduced [29]. Moreover, while most of the measurement variability in the CIMT is due to differences between observers, the intra-observer variability over time appears to be very small. So, the measurements were performed by the same sonographer to overcome this variability.
6 Conclusion
Ultrasonographic imaging and measurement of CIMT can reliably predict hypotension, which we define as a 20% decrease in baseline MBP value after induction of anesthesia in the majority of patients. We found 0.65 mm of CIMT as the threshold level. For this reason, an experienced reader can provide clinically useful information about PIH to determine possible complications for high-risk patients. We think that sonographic CIMT measurement may be a part of POC application in anesthesiology with subsequent researches on this issue.
Authors’ contributions
AK contributed to conception and design, data acquisition, interpretation of data, and drafting and revision of article, data analysis. EG, DDG contributed to interpretation of data, drafting, and revision of article. All authors have provided final approval of the version submitted. All authors read and approved the final manuscript.
Abbreviations
- CIMT:
-
Carotid intima media thickness
- PIH:
-
Post-induction hypotension
- POC:
-
Point of care
- MBP:
-
Mean blood pressure
- IVC:
-
Inferior vena cava diameter
- baPW:
-
Brachial-ankle pulse wave velocity
- USG:
-
Ultrasonography
- IOH:
-
Intraoperative hypotension
- CAD:
-
Coronary artery disease
- SAP:
-
Systolic arterial pressure
- CCA:
-
Common carotid artery
References
van den Oord SCH, Sijbrands EJG, ten Kate GL, et al. Carotid intima-media thickness for cardiovascular risk assessment: systematic review and meta-analysis. Atherosclerosis. 2013;228:1.
Naya T, Hosomi N, Ohyama H, et al. Smoking, fasting serum insulin, and obesity are the predictors of carotid atherosclerosis in relatively young subjects. Angiology. 2008;58:677–84.
O’Leary DH, Bots ML. Imaging of atherosclerosis: carotid intima-media thickness. Eur Heart J. 2010;31:1682–9.
Naqvi TZ, Lee M-S. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC. 2014;7:1025–38.
Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary. J Am Coll Cardiol. 2010. https://doi.org/10.1016/j.jacc.2010.09.002
Bijker JB, Persoon S, Peelen LM, et al. Intraoperative hypotension and perioperative ischemic stroke after general surgery, a nested case-control study. Anesthesiology. 2012;116:658–64.
Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119:507–15.
Chang HS, Hongo K, Nakagawa H. Adverse effects of limited hypotensive anesthesia on the outcome of patients with subarachnoid hemorrhage. J Neurosurg. 2000;92:971–5.
Mascha EJ, Yang D, Weiss S, Sessler DI. Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology. 2015;123:79–91.
Bijker JB, Van Klei WA, Kappen TH, Van Wolfswinkel L, Moons KGM, Kalkman CJ. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107:213–20.
Südfeld S, Brechnitz S, Wagner JY, et al. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth. 2017;119:57–64.
Hanss R, Renner J, Ilies C, et al. Does heart rate variability predict hypotension and bradycardia after induction of general anaesthesia in high risk cardiovascular patients? Anaesthesia. 2008;63:129–35.
Zhang J, Critchley LAH. Inferior vena cava ultrasonography before general anesthesia can predict hypotension after induction. Anesthesiology. 2016;124:580–9.
Monk TG, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10.
Monk TG, Bronsert MR, Henderson WG, et al. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology. 2015;123:307–19.
Society of Atherosclerosis Imaging and Prevention Developed in collaboration with the International Atherosclerosis. Society TS of AI and appropriate use criteria for carotid intima media thickness testing. Atherosclerosis. 2011;214:43–6.
Simon A, Gariepy J, Chironi G, Megnien JL, Levenson J. Intima-media thickness: a new tool for diagnosis and treatment of cardiovascular risk. J Hypertens. 2002;20:159–69.
Rodeghiero F, Tosetto A, Prati P, Baracchini C, Manara R. Age-adjusted reference limits for carotid intima-media thickness as better indicator of vascular risk: population-based estimates from the VITA project. J Thromb Haemost. 2005;3:1224–30.
Stein JH, Douglas PS, Srinivasan SR, et al. Distribution and cross-sectional age-related increases of carotid artery intima-media thickness in young adults: the Bogalusa Heart Study. Stroke. 2004;35:2782–7.
Youn YJ, Lee NS, Kim JY, et al. Normative values and correlates of mean common carotid intima-media thickness in the Korean rural middle-aged population: the atherosclerosis risk of rural areas in Korea general population (ARIRANG) study. J Korean Med Sci. 2011;26:365–71.
Beşir FH, Yazgan S, Celbek G, et al. Normal values correlates’ of carotid intima- media thickness and affecting parameters in healthy adults. Anadolu Kardiyoloji Dergisi. 2012;12:427–33.
Reich DL, Hossain S, Krol M, et al. Predictors of hypotension after induction of general anesthesia. Anesth Analg. 2005;101:622–8.
Ramsingh D, Fox JC, Wilson WC. Perioperative point-of-care ultrasonography: an emerging technology to be embraced by anesthesiologists. Anesth Analg. 2015;120:990–2.
Mahmood F, Matyal R, Skubas N, et al. Perioperative ultrasound training in anesthesiology: a call to action. Anesth Analg. 2016;122:1794–804.
Via G, Tavazzi G, Price S. Ten situations where inferior vena cava ultrasound may fail to accurately predict fluid responsiveness: a physiologically based point of view. Intensive Care Med. 2016;42:1164–7.
Morimoto Y, Yamagata K, Hanamoto H, et al. Arteriosclerosis can predict hypotension during anesthesia induction in patients 40 years and older. J Clin Anesth. 2015;27:132–9.
Dogan S, Plantinga Y, Dijk JM, van der Graaf Y, Grobbee DE, Bots ML. Manual B-mode versus automated radio-frequency carotid intima-media thickness measurements. J Am Soc Echocardiogr. 2009;22:1137–44.
Dogan S, Duivenvoorden R, Grobbee DE, et al. Ultrasound protocols to measure carotid intima-media thickness in trials; Comparison of reproducibility, rate of progression, and effect of intervention in subjects with familial hypercholesterolemia and subjects with mixed dyslipidemia. Ann Med. 2010;42:447–64.
Stein JH, Korcarz CE, Mays ME, et al. A semiautomated ultrasound border detection program that facilitates clinical measurement of ultrasound carotid intima-media thickness. J Am Soc Echocardiogr. 2005;18:244–51.
Funding
The study was funded by departmental resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was reviewed and approved by the institutional review board at the Diyarbakir Gazi Yasargil Training and Education hospital, ID: 46, 2018. Written informed consent was obtained from all patients.
Rights and permissions
About this article
Cite this article
Kaydu, A., Güven, D.D. & Gökcek, E. Can ultrasonographic measurement of carotid intima-media thickness predict hypotension after induction of general anesthesia?. J Clin Monit Comput 33, 825–832 (2019). https://doi.org/10.1007/s10877-018-0228-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0228-y