Abstract
The feasibility and clinical utility of the endotracheal cardiac output monitor (ECOM) to optimize intraoperative hemodynamics and improve short-term outcome in off-pump coronary artery bypass grafting (OPCAB) is unknown. We aimed to compare ECOM with a standard of care in that specific surgical setting. Twenty consecutive adult ECOM-monitored patients undergoing OPCAB were prospectively included (ECOM group) and retrospectively compared to 42 patients scheduled for similar surgery without ECOM monitoring (Control group). The primary endpoint was the global rate of postoperative admission to the intensive care unit (ICU). Secondary endpoints were the time to extubation, the length of stay in ICU and in hospital, the postoperative levels of lactate and troponin and the feasibility of ECOM. The rate of postoperative admission to the ICU was 38/42 (90%) in the Control group versus 11/20 (55%) in the ECOM group, P = 0.008. None unexpected admission for hemodynamic instability was observed in the ECOM group. The time to extubation, the length of stay in ICU, and both troponin level at admission and lactate level at H6 were all significantly decreased in the ECOM group. On a scale ranging from 0 to 5, convenience and satisfaction regarding ECOM were 4.30 ± 1.17 and 3.45 ± 0.68, respectively. The systematic use of ECOM is associated with a significant reduction in the rate of admission to the ICU and an improvement in immediate outcome in OPCAB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Intraoperative advanced hemodynamic monitoring is useful for moderate to high-risk patients undergoing cardiac surgery [1]. Hemodynamic optimization with early goal-directed therapy (EGDT) has proven its ability to reduce morbidity [2–6], time to extubation [7], and length of stay in the intensive care unit (ICU) [3, 8, 9]. EGDT strategies for elective cardiac surgical procedures usually rely on stroke volume and/or cardiac output optimization [1, 2]. Off-pump coronary artery bypass grafting (OPCAB) is a simplified surgical procedure avoiding cardiopulmonary bypass that could shorten postoperative rehabilitation [10–12]. Patients undergoing OPCAB are most often admitted postoperatively first to the Post Anesthesia Care Unit and then assessed for secondary admission either to the ward or to the ICU, depending of their hemodynamic and clinical status during the first postoperative hours. To date, there is no standardization regarding the choice of advanced hemodynamic monitoring in OPCAB, and systematic intraoperative cardiac output and/or stroke volume assessment by means of transeosophageal echocardiography (TEE) is not yet a routine practice in France.
The endotracheal cardiac output monitor (ECOM Medical, Inc., San Juan Capistrano, CA) is a new Food and Drug Administration-approved plug and play device that provides continuous cardiac output measurement via a specifically designed endotracheal tube using three-dimensional bioimpedance in conjunction with an arterial catheter [13]. This new mini-invasive cardiac output monitor was previously evaluated with encouraging results in seven human studies including 196 cardiac surgical patients and compared either to bolus thermodilution or echocardiography [14–20]. Recently, we reported a randomized controlled study suggesting that ECOM could be of clinical utility in coronary surgery with cardiopulmonary bypass [7]. Whether ECOM could also be of some usefulness in OPCAB is unknown.
Therefore, we conducted a new study aiming to assess both the feasibility and clinical utility of ECOM to optimize intraoperative hemodynamics in OPCAB surgery compared to a standard of care. We hypothesized that ECOM would improve overall intraoperative hemodynamic management and subsequently immediate postoperative outcome in that specific surgical setting.
2 Methods
2.1 Patient population
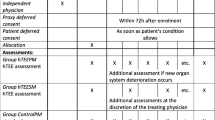
A case-control study was conducted over an 8-month period in a single University Teaching Hospital after approval from the local Research Ethics Committee (Chairperson Pr. J.F. Guérin, date of approval 26th of February 2015). Because data were collected during routine care that conformed to standard procedures currently used in the institution, authorization was granted to waive written informed consent. Verbal consent was however obtained from all participants. From March to April 2015, 20 consecutive ECOM-monitored adult patients (so-called the ECOM group) undergoing elective OPCAB were prospectively included in the study and compared to 42 consecutive controlled adult patients having undergone elective OPCAB by the same surgeon (FF) from September 2014 to February 2015 without ECOM monitoring (so-called the Control group). Inclusion criteria were elective OPCAB. Patients undergoing emergent surgery (less than 24 h) or redo surgery, and patients with severe aortic valvular disease were not included into the study.
2.2 Perioperative management
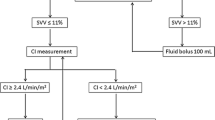
General anesthesia and postoperative management followed institutional standards and were similar in all patients. Briefly, intraoperative monitoring techniques included continuous five-lead electrocardiogram with computerized analysis of repolarization, pulse oximetry, invasive arterial blood pressure by means of a radial artery catheter and central venous pressure by means of a jugular central venous catheter. In addition, monitoring of the depth of anesthesia by means of the BiSpectral Index™ (Covidien, Mansfield, MA, USA), a cell salvage machine, and forced-air warming were used in all patients. Standardized total intravenous anesthesia (i.e., target-control propofol and remifentanil or sufentanil infusion, and cisatracurium) or inhaled sevoflurane in order to maintain a BIS value between 40 and 60 were used at the discretion of the attending practitioners. All patients were intubated with a 7.5 mm endotracheal tube after induction of general anesthesia. In the ECOM group, we used a specially designed endotracheal tube (ECOM-ETT 7.5G, ECOM Medical, Inc., San Juan Capistrano, CA) which contains seven silver electrodes on the cuff and tube that continuously measured the bioimpedance signal from the ascending aorta, in close proximity to the trachea (Fig. 1) [13]. The ECOM pressure monitor was connected to the radial arterial line and then to the ECOM endotracheal tube impedance wires. All pressure monitors were zeroed at the mid-axillary line. After processing, it provides real-time continuous stroke volume and cardiac index together with respiratory stroke volume variations as a dynamic test aiming to predict fluid responsiveness, and systemic vascular resistance calculation as an afterload valuable parameter. No previous adverse event was reported with the use of ECOM over a 24-h period [21] and it did not add any new invasive procedure when compared with the Control group. In the ECOM group, the device was available within the whole intraoperative period in order to help practitioners, familiar with the concept, in conducting their own EGDT strategy on a case-by-case basis. Mechanical ventilation was in accordance with the actual standards of care (tidal volume 6–8 ml/kg of predicted body weight and a positive end-expiratory pressure of 5 cmH2O). The same surgical technique including similar successive steps by a single surgeon (FF) was used in all patients: incision, sternotomy, harvesting of the grafts, stabilization of the heart (ACROBAT-i Stabilizer System, MAQUET Holding B.V. & Co. KG, Germany), coronary artery bypass, hemostasis and sternal fixation.
All patients were admitted postoperatively to the Post Anesthesia Care Unit for at least 2 h and then carefully assessed for admission either to the ward or to the ICU, at the discretion of attending physicians not involved in the study protocol and blinded to all study endpoints. Indeed, if they were aware of the availability of ECOM in the operative room and its possible use by the anesthesiologists to conduct EGDT, they did not know both primary and secondary study endpoints, so that the decision to admit or not a patient to the ICU could not be influenced by the study itself. The decision to admit a patient to the ICU was either preoperatively anticipated (in accordance with patients’ comorbidities and risk stratification) or postoperatively based on unexpected hemodynamic instability, bleeding, respiratory failure or early reoperation.
Patients’ demographic and clinical characteristics were collected preoperatively, as well as intraoperative hemodynamic parameters and postoperative outcomes. Acute renal failure was defined as an increase in peak postoperative creatinine of at least 30%. To assess the feasibility of ECOM monitoring in that specific surgical setting, we asked attending anesthesiologists at the end of surgery for convenience, satisfaction, and quality of ECOM signal by means of three different scales ranging from 0 to 5 (Appendix 1).
2.3 Study endpoints
The primary endpoint of the study was the all-cause rate of postoperative admission to the ICU (both preoperatively anticipated and postoperatively unexpected). Secondary endpoints were the unexpected rate of postoperative admission to the ICU for hemodynamic instability, the time to extubation, the length of stay in ICU and in hospital, the postoperative levels of lactate and troponin at the admission in ICU and 6 h later (H6), and the feasibility of ECOM in that specific surgical setting.
2.4 Statistical analysis
We performed a post hoc power calculation on the basis of a decrease in at least 40% of the rate of postoperative admission to the ICU in the ECOM group when compared with the Control group at a 5% type I error rate and a 20% type II error rate. Thus, the sample size revealed 62 patients divided into 21 patients in the ECOM group and 41 patients in the Control group, corresponding to a ratio case/control group of 1/2.
Variables are expressed as mean ± SD or median (extremes) for non-normally distributed variables (D’Agostini Pearson test) or number, as appropriate. Comparisons between both groups were made by independent samples t test or Mann–Whitney test according to the distribution for continuous variables and Fischer’s exact test for categorical variables. We performed a multiple regression to look for potential statistical correlations between the primary endpoint and independent confusing variables.
A P value of <0.05 was considered as statistically significant and all P values were two-tailed. Statistical analyses were performed using MedCalc Statistical Software version 14.10.2 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2014).
3 Results
One patient was excluded because of the unavailability of the ECOM endotracheal tube at the time of intubation. Sixty-two patients were included within the 8-month period and divided into 20 patients in the ECOM group and 42 patients in the Control group.
Demographic and clinical characteristics are indicated in Table 1. No statistical difference was observed between both groups, except for the rate of preoperative diuretics use, the duration of surgery, and the number of grafts. Intraoperative variables and hemodynamic parameters are summed up in Table 2. Minimal heart rate and vasoactive support were significantly lower in the Control group when compared with the ECOM group. Postoperative data and outcomes are reported in Table 3. As a primary endpoint, the all-cause rate of postoperative admission to the ICU was reduced by 61% in the ECOM group: 11/20 (55%) versus 38/42 (90%), P = 0.008. While the preoperative anticipated rate of admission was similar in both groups [24/42 (57%) versus 10/20 (50%), P = 0.785, respectively], the unexpected rate of admission related to hemodynamic instability markedly differed between Control: 12/42 (29%) versus ECOM: 0/20 (0%), P = 0.006 (Table 3). As other secondary endpoints, the extubation time, the length of stay in ICU, and both troponin level at admission and lactate level at H6 were all significantly decreased in the ECOM group when compared with the Control group. Mediastinal bleeding was also significantly decreased in the ECOM group when compared with the Control group (Table 3).
The multiple regression showing the correlation between significant clinical variables and the primary endpoint is reported in Table 4. None independent variable was correlated with the all-cause rate of admission to the ICU. The coefficient of determination R2 was 0.122 and the analysis of variance accepted the absence of significant relationship (P = 0.289).
The feasibility of ECOM monitoring in OPCAB is depicted in Table 5. Both quality of signal and satisfaction were acceptable whereas the convenience was good.
4 Discussion
The main findings of the present case-control study are that the systematic availability of continuous intraoperative advanced hemodynamic monitoring by means of ECOM in an anesthesiologist staff familiar with the EGDT concept, is associated with both a marked decrease in the all-cause rate of postoperative admission to the ICU and an improvement in immediate postoperative outcome following OPCAB when compared with a standard of care.
Although the preoperative anticipated admission rate to the ICU was similar in both groups, no more admission related to unexpected hemodynamic instability was observed in the ECOM group, fully explaining the main result of the study. The ECOM device provides real-time cardiac output, preload dependency, and left ventricular afterload information that probably helped anesthesiologists to improve and/or stabilize patient’s hemodynamic status. Thus, the continuous knowledge of cardiac output/stroke volume values at any moment of the surgical procedure could have facilitated the decision to administrate more vasopressors, as suggested by the current results. As well, we observed a trend toward more fluid volume (+350 ml) in the ECOM group. Taken together, these changes in individual hemodynamic strategies could have contributed to immediate postoperative stability and the decision by attending physicians not to admit patients in the ICU. As no institutional EGDT protocol was suggested to practitioners, it may be that other non-measured hemodynamic variables differed between both groups, explaining the improvement in immediate postoperative outcome. It is noteworthy that almost all secondary endpoints were significantly improved in the ECOM group: extubation time and the length of stay in ICU were reduced, whereas troponin measurement at the admission in ICU and lactate at H6 were decreased when compared with the Control group, further suggesting that overall hemodynamic management was improved by the systematic availability of continuous intraoperative ECOM monitoring. These results are in accordance with a previous published study from our group suggesting a potential role for ECOM in coronary surgery patients [7]. As far as we acknowledge, no other data are available in the literature regarding the clinical utility of ECOM.
No standardization regarding the choice of advanced hemodynamic monitoring in OPCAB exists at the present time, and systematic intraoperative continuous cardiac output monitoring is far to be easy in that specific setting. It usually relies on TEE [22] and/or transpulmonary thermodilution [23, 24]. TEE images are however either partially unavailable or somewhat difficult to interpret during some crucial phases of the surgical procedure (as during luxation of the heart), and do not permit a true continuous hemodynamic monitoring. It is noteworthy that the use of TEE was uncommon in the present study, even in the Control group. Conversely, hemodynamic parameters given by ECOM were continuously available all along surgery. Thus, ECOM could meet many important theoretic characteristics of the ideal hemodynamic monitoring device, as operator independency, mini-invasiveness, and convenience [13]. The current results about convenience, quality of signal and satisfaction outline that practitioners trust the device and use it easily when available at the bedside.
Some comments are necessary concerning the limitations of the present study. First, we only investigated a small cohort of patients in a monocenter case-control study. As there is at the present time no literature available on this specific topic, and as we were uncertain if such an advanced hemodynamic monitoring tool could be of some clinical interest in that subtype of high-risk surgical cardiac patients, we believe however our study design was adapted to provide preliminary results in that setting. Subsequently, the level of evidence suggesting there is a role for ECOM at the bedside remains low, and further randomized outcome studies are mandatory before recommending a wider use in routine practice. Second, the physicians assessing patients for postoperative admission either to the ICU or to the ward were not blinded to the use of ECOM in our study. They were however blinded to all study endpoints. As well, some significant clinical differences exist between the two groups of patients which could have partially explained our results, especially the decrease in postoperative mediastinal bleeding in the ECOM group. Subsequently, we performed a multiple regression to look for potential statistical correlations between the primary endpoint and independent confusing variables. We found that none independent variable was correlated with the all-cause rate of admission to the ICU, reinforcing the internal validity of our results. However, the decrease in postoperative mediastinal bleeding in the ECOM group could have influenced some secondary endpoints, as extubation time and length of stay in ICU. Again, future studies including more patients monitored with ECOM during major surgeries are warranted to confirm the potential improvement in outcome when using ECOM. Finally, we did not provide an institutional EGDT strategy based on ECOM in the present study but only gave the opportunity to systematically use (or not) hemodynamic parameters given by the ECOM device in order to guide the clinical decision making process. We actually do not know if practitioners did it or not and if they did, how do they did. A next step would be to evaluate the clinical interest of ECOM-induced EGDT strategies in the specific setting of OPCAB and other surgical subtypes of high-risk patients.
In conclusion, this case-control study suggests that intraoperative advanced mini-invasive hemodynamic monitoring by means of ECOM could reduce the admission rate in ICU and improve immediate postoperative outcome in OPCAB when compared to a standard of care. Considering the modern pattern of rapid postoperative rehabilitation following cardiac surgery, such results are encouraging while necessitating being further confirmed in well-designed randomized outcome studies before a wider use in clinical practice. Further studies are also mandatory to better assess both the economic and clinical impact of such a mini-invasive advanced monitoring tool in various clinical settings.
References
Kapoor PM, Kakani M, Chowdhury U, Choudhury M, Lakshmy R, Kiran U. Early goal-directed therapy in moderate to high-risk cardiac surgery patients. Ann Card Anaesth. 2008;11:27–34.
Aya HD, Cecconi M, Hamilton M, Rhodes A. Goal-directed therapy in cardiac surgery: a systematic review and meta-analysis. Br J Anaesth. 2013;110:510–7.
Donati A, Loggi S, Preiser J-C, Orsetti G, Munch C, Gabbannelli V, et al. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Chest. 2007;132(6):1817–24.
Grocott MPW, Mythen MG, Gan TJ. Perioperative fluid management and clinical outcomes in adults. Anesth Analg. 2005;100:1093–106.
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg. 2011;112:1392–402.
Jhanji S, Vivian-Smith A, Lucena-Amaro S, Watson D, Hinds CJ, Pearse RM. Haemodynamic optimisation improves tissue microvascular flow and oxygenation after major surgery: a randomised controlled trial. Crit Care Lond Engl. 2010;14:R151.
Fellahi J-L, Brossier D, Dechanet F, Fischer M-O, Saplacan V, Gerard J-L, et al. Early goal-directed therapy based on endotracheal bioimpedance cardiography: a prospective, randomized controlled study in coronary surgery. J Clin Monit Comput. 2015;29(3):351–8.
Goepfert MS, Richter HP, Zu Eulenburg C, Gruetmacher J, Rafflenbeul E, Roeher K, et al. Individually optimized hemodynamic therapy reduces complications and length of stay in the intensive care unit: a prospective, randomized controlled trial. Anesthesiology. 2013;119(4):824–36.
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial. Crit Care Lond Engl. 2005;9(6):R687–R93.
Huffmyer J, Raphael J. The current status of off-pump coronary bypass surgery. Curr Opin Anaesthesiol. 2011;24:64–9.
Deppe A-C, Arbash W, Kuhn EW, Slottosch I, Scherner M, Liakopoulos O, et al. Current evidence of coronary artery bypass grafting off-pump versus on-pump: a systematic review with meta-analysis of over 16 900 patients investigated in randomized controlled trials. Eur J Cardio-Thorac Surg. 2016;49(4):1031–41.
Chaudhry UAR, Harling L, Sepehripour AH, Stavridis G, Kokotsakis J, Ashrafian H, et al. Beating-heart versus conventional on-pump coronary artery bypass grafting: a meta-analysis of clinical outcomes. Ann Thorac Surg 2015;100:2251–60.
Fellahi J-L, Fischer M-O. Electrical bioimpedance cardiography: an old technology with new hopes for the future. J Cardiothorac Vasc Anesth. 2014;28:755–60.
Ball TR, Culp BC, Patel V, Gloyna DF, Ciceri DP, Culp WC. Comparison of the endotracheal cardiac output monitor to thermodilution in cardiac surgery patients. J Cardiothorac Vasc Anesth. 2010;24:762–6.
Maus TM, Reber B, Banks DA, Berry A, Guerrero E, Manecke GR. Cardiac output determination from endotracheally measured impedance cardiography: clinical evaluation of endotracheal cardiac output monitor. J Cardiothorac Vasc Anesth. 2011;25:770–5.
Fellahi J-L, Fischer M-O, Rebet O, Massetti M, Gérard J-L, Hanouz J-L. A comparison of endotracheal bioimpedance cardiography and transpulmonary thermodilution in cardiac surgery patients. J Cardiothorac Vasc Anesth. 2012;26:217–22.
Fellahi J-L, Fischer M-O, Dalbera A, Massetti M, Gérard J-L, Hanouz J-L. Can endotracheal bioimpedance cardiography assess hemodynamic response to passive leg raising following cardiac surgery? Ann Intensive Care. 2012;2:26.
Møller-Sørensen H, Hansen KL, Østergaard M, Andersen LW, Møller K. Lack of agreement and trending ability of the endotracheal cardiac output monitor compared with thermodilution. Acta Anaesthesiol Scand. 2012;56:433–40.
van der Kleij SCJ, Koolen BB, Newhall DA, Gerritse BM, Rosseel PMJ, Rijpstra TA, et al. Clinical evaluation of a new tracheal impedance cardiography method. Anaesthesia. 2012;67:729–33.
Thonnerieux M, Alexander B, Binet C, Obadia J-F, Bastien O, Desebbe O. The ability of esCCO and ECOM monitors to measure trends in cardiac output during alveolar recruitment maneuver after cardiac surgery: a comparison with the pulmonary thermodilution method. Anesth Analg. 2015;121:383–91.
Wallace AW, Salahieh A, Lawrence A, Spector K, Owens C, Alonso D. Endotracheal cardiac output monitor. Anesthesiology. 2000;92:178–89.
Kapoor PM, Chowdhury U, Mandal B, Kiran U, Karnatak R. Trans-esophageal echocardiography in off-pump coronary artery bypass grafting. Ann Card Anaesth. 2009;12:167.
Kirov MY, Lenkin AI, Kuzkov VV, Suborov EV, Slastilin VY, Borodin VV, et al. Single transpulmonary thermodilution in off-pump coronary artery bypass grafting: haemodynamic changes and effects of different anaesthetic techniques. Acta Anaesthesiol Scand. 2007;51:426–33.
Smetkin AA, Hussain A, Kuzkov VV, Bjertnæs LJ, Kirov MY. Validation of cardiac output monitoring based on uncalibrated pulse contour analysis vs transpulmonary thermodilution during off-pump coronary artery bypass grafting. Br J Anaesth. 2014;112:1024–31.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding
Departmental funding only.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Verbal consent was obtained from all individual participants included in the study.
Appendix 1: Scales for feasibility of ECOM in off-pump coronary surgery
Appendix 1: Scales for feasibility of ECOM in off-pump coronary surgery

Rights and permissions
About this article
Cite this article
Leclercq, T., Lilot, M., Schulz, T. et al. Endotracheal bioimpedance cardiography improves immediate postoperative outcome: a case-control study in off-pump coronary surgery. J Clin Monit Comput 32, 81–87 (2018). https://doi.org/10.1007/s10877-017-9996-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-017-9996-z