Abstract
Purpose
Inherited deficiencies of CD40 and CD40 ligand (CD40L) reflect the crucial immunological functions of CD40–CD40L interaction/signaling. Although numerous studies have provided a detailed description of CD40L deficiency, reports of CD40 deficiency are scarce. Herein, we describe the characteristics of all reported patients with CD40 deficiency.
Methods
The PubMed, Embase and Web of Science databases were searched for relevant literature published till 7th August 2023. Study deduplication and identification of relevant reports was performed using the online PICO Portal. The data were extracted using a pre-designed data extraction form and the SPSS software was used for analysis.
Results
Systematic literature review revealed 40 unique patients with CD40 deficiency. Respiratory tract and gastrointestinal infections were the predominant clinical manifestations (observed in 93% and 57% patients, respectively). Sclerosing cholangitis has been reported in nearly one-third of patients. Cryptosporidium sp. (29%) and Pneumocystis jirovecii (21%) were the most common microbes identified. Very low to undetectable IgG levels and severely reduced/absent switch memory B cells were observed in all patients tested/reported. Elevated IgM levels were observed in 69% patients. Overall, splice-site and missense variants were the most common (36% and 32%, respectively) molecular defects identified. All patients were managed with immunoglobulin replacement therapy and antimicrobial prophylaxis was utilized in a subset. Hematopoietic stem cell transplantation (HSCT) has been performed in 45% patients (curative outcome observed in 73% of these patients). Overall, a fatal outcome was reported in 21% patients.
Conclusions
We provide a comprehensive description of all important aspects of CD40 deficiency. HSCT is a promising curative treatment option for CD40 deficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CD40, a member of the tumor necrosis factor receptor superfamily, is expressed on various cells including B cells, endothelial cells, monocytes/macrophages, epithelial cells, platelets, keratinocytes, and dendritic cells [1]. CD40 interacts with CD40L which exists as a transmembrane protein on activated T-cells and platelets as well as in the soluble form [2]. Interaction of CD40 and CD40L plays a pivotal role in the development of the germinal center, antibody class switching, somatic hypermutation, and generation of memory B-cells [3]. In addition, CD40-CD40L signaling is also crucial for the maturation of dendritic cells and optimal T-cell function [4]. Inherited deficiency of CD40L is known to cause combined immunodeficiency (CID) and is commonly referred to as X-linked hyper IgM (HIGM) syndrome [5, 6]. Deficiency of CD40 also results in CID with HIGM phenotype and is inherited in an autosomal recessive manner (often referred to as HIGM type 3) [6, 7]. Although numerous studies have provided the clinical and immunological features of CD40L deficiency [8, 9], reports of CD40 deficiency are sparse [10]. Herein, we analyze the clinical features, immunological aberrations, molecular defects, and outcomes of all reported patients with CD40 deficiency. To the best of our knowledge, a comprehensive description of all patients with CD40 deficiency reported over the last two decades has not been published previously.
Methods
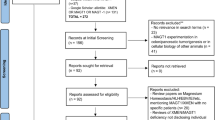
We performed this study according to the PRISMA 2020 guidelines (Fig. 1) [11]. The protocol of our systematic review is registered at PROSPERO (CRD42022360700, available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022360700). No changes were made in the protocol after registration in PROSPERO.
Types of Studies
All relevant study types including observational studies, case reports/series, letters, images, editorials, or posters/abstracts providing data regarding patients with CD40 deficiency were included.
Participants
All patients with CD40 deficiency reported in the literature.
Controls
None.
Intervention
Not applicable.
Outcome Measures
We analysed the clinical and immunohematological features, microbial profile, genetic variants, management strategies (including HSCT), and outcomes of patients with CD40 deficiency.
Search Methodology
We searched the PubMed, Embase and Web of Science databases for relevant data published till 7th August 2023. The keywords employed included the following MeSH (marked with asterisks ‘*’) and free-text terms combined using appropriate Boolean operators: CD40 deficiency, HIGM3, *hyper-IgM immunodeficiency syndrome, *CD40 antigens, TNFRSF5, *genes (recessive), type 3, *primary immunodeficiency diseases, variant, defect, deficiency, *mutation. No language restrictions were applied during the systematic search (Supplementary Data).
Data Extraction
We used PICO Portal for deduplication of reports and identification of relevant studies [12]. The data were extracted using a pre-designed data extraction form (Microsoft Excel 2010, Microsoft Corporation) [13]. Two authors independently extracted the following data from each report: authors, year of publication, location (country) of report, basic epidemiological data (patient origin/ethnicity, age at onset of symptoms, sex, presence/absence of parental consanguinity), clinical features (organ(s)-system(s) affected due to infections and/or autoimmune manifestations, presence of failure to thrive), pathogenic microbes identified (including site of isolation), hematological parameters (neutrophil, eosinophil, lymphocyte counts; bone marrow findings), immunological findings (levels of IgG, IgA, IgM; peripheral blood lymphocyte immunophenotyping; CD40 expression; lymphocyte responses to mitogens/antigens), variant details, treatment details (including HSCT protocols), and outcomes.
Data Synthesis/Analysis
Data were analysed using the Statistical Package for Social Sciences software (IBM Corporation, version 23). The notation ‘[a/b]’ has been utilized to represent number of patients ‘a’ with a particular characteristic (numerator) out of the total cohort of patients ‘b’ wherein the said data were available (denominator).
Assessment of Study Quality (Including Risk of Bias)
As all reports retrieved pertained to the clinical description of one or more cases of CD40 deficiency, study quality (including risk of bias) assessment was not performed.
Results
Systematic literature review revealed 40 unique patients with CD40 deficiency (excluding siblings of known patients who had features reminiscent of an inborn error of immunity (IEI) but died prior to any evaluation) (Table 1) [7, 14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. However, detailed data pertaining to disease characteristics were unavailable for 11 patients (Supplementary Table 1 [Table S1]) [26,27,28,29,30,31,32,33]. Notably, complete data (including follow-up) of many patients were retrieved from multiple different reports [10, 34,35,36,37,38,39,40].
Epidemiology
More than one-third of patients reported were from Saudi Arabia (35%, [14/40]) and one-fifth from Turkey (20%, [8/40]). Other countries have reported only a few patients with CD40 deficiency – 3 from Germany; 2 each from Italy, Algeria, Egypt, India (including 1 patient from Bangladesh), Canada (1 patient of Iranian and French-Canadian descent), and United States (1 patient of Moroccan origin); and 1 each from Iran, Tunisia, and Venezuela. Most of the patients (94%, [29/31]) were born to consanguineous parents and no sex predilection was noted (17 females, 16 males, sex unreported: 7). Diagnosis of CD40 deficiency was established after onset of symptoms in nearly all patients (97%, [30/31]). In one patient with family history of CD40 deficiency, molecular diagnosis was established at 1 month of life (prior to onset of symptoms). None of the reported patients were identified as a result of newborn screening.
Clinical Features
CD40 deficiency manifested on or before the first birthday in 76% [22/29] patients. In 38% [11/29] patients, onset of symptoms was noted within the first 4 months of life (Fig. 2). Respiratory tract infections (including severe and recurrent pneumonias leading to bronchiectasis) was the predominant clinical manifestation observed in 93% [26/28] patients (interstitial pneumonia in 25% [7/28] patients). Recurrent/protracted/chronic diarrhea was the second most common clinical manifestation seen in 57% [16/28] patients. Failure to thrive (or growth faltering) was reported in 14 patients (~ 50%). Otorhinological involvement (encompassing sinusitis, otitis media, mastoiditis, and nasal infections) was noted in 39% [11/28] patients. Sclerosing cholangitis and dilatation of biliary radicles/duct has been observed in 29% [8/28] and 7% [2/28] patients, respectively. Purulent skin/soft-tissue infections (including 1 patient with otitis externa) were seen in 14% patients [4/28]. Arthritis was noted in 11% [3/28] (including one patient with septic arthritis) (Fig. 3). One patient each was diagnosed with inflammatory bowel disease (granulomas) and follicular lymphoma.
Microbiological Profile
Cryptosporidium (C. parvum) was the most frequently identified pathogen seen in nearly one-third of patients (29% [8/28]) with CD40 deficiency. Cryptosporidial infections were commonly associated with sclerosing cholangitis and diarrhea (isolated from bile and stools, respectively); however, disseminated C. parvum infection has also been observed in one patient (diarrhea and severe laryngotracheobronchitis). Pneumocystis jirovecii was identified in 21% [6/28] patients and resulted in pneumonia/interstitial pneumonia. Pseudomonas aeruginosa was identified in 18% [5/28] patients and resulted in destructive nasal infections [2/5], necrotizing pneumonia, otitis media, and perianal ulcer [each 1/5]. Oral and esophageal candidiasis (including necrotizing esophagitis resulting in fistulization in one patient) was noted in 11% [3/28] patients. Furthermore, Candida sp. were identified in one patient each with destructive nasal infection and chronic diarrhea. Klebsiella sp. were identified in 3 patients (K. oxytoca in one patient with urinary tract infection and K. pneumoniae in 2 patients) (Fig. 3). Mycobacterium tuberculosis complex and cytomegalovirus were identified in 2 patients each (resulting in pulmonary infections). Infections due to Staphylococcus aureus (skin abscess), Giardia sp. (chronic diarrhea), respiratory syncytial virus (severe pneumonia), Streptococcus pneumoniae, C. difficile, and Epstein-Barr virus were reported in 1 patient each.
Immunohematological Parameters
Very low to undetectable IgG levels is the most prominent immunological abnormality of CD40 deficiency which was observed in all patients tested/reported (n = 26). Very low to undetectable IgA levels were noted in 81% [17/21] patients tested/reported. Near-normal levels of IgA were noted in 10% [2/21] while normal-high levels of IgA were noted in the remaining [2/21] patients (on serial testing). Elevated IgM levels were observed in 69% [18/26] patients while normal IgM levels were noted in the rest. IgM levels of > 10 g/L (upto 20 g/L) were reported in 4 patients. Significant reductions in B-cell counts or proportions have not been recorded in patients with CD40 deficiency. On the other hand, profoundly reduced/absent switch memory B cells (< 1% of peripheral blood B cells) have been observed in all patients reported/tested [10/10]. Similarly, severe reduction or absence of switched B cells has been noted in all patients tested/reported [4/4] (Fig. 3). However, variable proportions of unswitched memory B cells (1.6–10% of peripheral B cells) have been reported (reduced or normal). Somatic hypermutation was also observed to be defective in a patient with CD40 deficiency.
Besides B-cell abnormalities, significantly reduced T-cells have been observed in 2 patients (resulting in lymphopenia). Furthermore, reversal of CD4:CD8 ratio (CD4/CD8 < 0.9) has been reported in 3 additional patients. In-vitro lymphocyte/T-cell proliferation on stimulation with phytohemagglutinin was normal in majority of patients tested (82%, [9/11]). These included one patient each with T-cell lymphopenia or reduced CD4:CD8 ratio. Lymphocyte proliferation on stimulation with anti-CD3 and concanavalin-A was normal in the few patients tested.
Neutropenia was observed in 61% [17/28] patients. Majority of these patients had severe neutropenia (absolute count of < 0.5 × 109/L). Maturation block at promyelocyte level has been reported in one of the two patients tested. However, detailed data regarding bone marrow myeloid differentiation are unavailable for rest of the patients with neutropenia. Eosinophilia (including counts of > 5.0 × 109/L) has been reported in 21% [6/28] patients. Dyserythropoiesis (on bone marrow examination) was observed in one patient with CD40 deficiency. None of the reports have reported thrombocytopenia in these patients.
Variant Profile
Overall, splice-site variants were the most common (36% [10/28]) molecular defects identified (Fig. 4). Of these, c.256 + 2T > C was the commonest variant seen in 7 patients. Other splice-site variants included c.257-2 A > T (2 patients) and c.408 A > T (1 patient). Missense variants were identified in 32% [9/28] patients. The most common missense variant identified was c.170 C > T, p.T57M (5 patients). Other missense variants identified were c.247T > C, p.C83R (2 patients), c.109T > G, p.C37G (1 patient), and c.430G > A, p.E144K (1 patient). Stop-loss variants were observed in 4 patients (c.832_*1delTGAG [p.X278Aext*33, 3 patients], c.823delG [p.E275RfsX38, 2 patients]). In-frame trinucleotide deletions (single amino acid deletions) were noted in another 2 patients (c.95_97delTAA, p.I33del and c.320_322delAAG, p.E107del). Variants in the upstream untranslated region have also been reported in 2 patients (c.-1T > C and c.-3G > A in 1 patient each). Stop-gain variant was identified in 1 patient (c.309 C > A, p.C103X). All variants were present in a homozygous state in affected individuals (no compound heterozygotes were reported). CD40 expression on B cells was severely reduced to absent in all patients except in patients with stop-loss variants (Table 1).
Except for variants in upstream untranslated region and stop-loss variants, all of the reported variants affect the cysteine-rich tumor necrosis factor receptor domains of CD40 (Fig. 4). The conformational structure of these conserved domains is stabilized by intrachain disulfide bonds. Missense variants (e.g. p.C37G, p.C83R) and small in-frame deletions (e.g. p.I33del) disrupt the formation of disulfide bonds (by directly affecting the conserved cysteine residues or by steric hindrance) resulting in abnormal protein folding and retention in the endoplasmic reticulum [35]. A similar mechanism is noted for c.257-2 A > T splice-site variant which results in p.NL86_87del + G88R abnormality in the protein sequence. Other splice-site and stop-gain variants abrogate normal translation of CD40 protein [35]. Stop-loss variants affecting the cytoplasmic domain (c.823delG, p.E275RfsX38) result in aberrant downstream signaling despite normal CD40 expression on the cell surface [19].
Treatment
All patients were managed with immunoglobulin replacement therapy (IgRT). Patients with neutropenia typically received granulocyte-colony-stimulating factor (G-CSF) therapy during the cytopenic episodes (except one patient with mild neutropenia) which usually responded well to treatment. Prophylactic antimicrobial therapy (mostly oral trimethoprim-sulfamethoxazole) has been reported to be utilized in 62% [18/29] patients. Antifungal prophylaxis has also been employed in a few patients. Hematopoietic stem cell transplantation (HSCT) has been performed in 45% patients [13/29].
Outcomes
Overall, a fatal outcome has been reported in 21% [6/29] patients with CD40 deficiency (Table S2). Survival frequency at 5-, 10-, and 20-years of age was 85.0% (95% CI: 71.3–98.7), 78.4% (95% CI: 60.8–96.0), and 67.2% (95% CI: 41.9–92.5), respectively (Fig. 5). In patients who did not undergo HSCT, 25% [4/16] mortality was observed. Reasons for death (age at death) in these four patients included chronic liver disease secondary to sclerosing cholangitis (16 years), severe gastroenteritis and respiratory infections (1.5 years and 4 years [two patients, 4-year old patient also had chronic liver disease secondary to sclerosing cholangitis]), and Pseudomonas sepsis (2 years [poor compliance with IgRT and G-CSF treatment]). Long-term morbidity (chronic diarrhea, stroke, failure to thrive) has also been reported in a few patients.
HSCT in CD40 Deficiency
HSCT has been performed in 13 patients with CD40 deficiency. Of these, 6 patients have been transplanted in Saudi Arabia, 4 in Turkey, 2 in Italy (one patient from Turkey), and 1 patient has received HSCT in the US (patient of Moroccan origin). To date, HSCT has mostly been performed in the first decade in patients with CD40 deficiency (median age at HSCT: 21.0 (11.2, 38.0) months, n = 10). In 75% [9/12] patients, a matched family donor (mostly sibling) served as source of the graft. One patient each received HSCT from a matched unrelated donor, 9/10 matched unrelated donor, and 9/10 matched sibling donor. Majority of patients (73% [8/11]) received busulfan (mostly 4 mg/kg/day for 4 days) and cyclophosphamide (mostly 50 mg/kg/day for 4 days) based conditioning regimens. Patients receiving transplant from a 9/10 matched unrelated/sibling donor also received antithymocyte globulin (ATG). Three patients received fludarabine based conditioning regimens with additional utilization of busulfan, melphalan + ATG, and treosulfan + methotrexate in one patient each. Patients received 5.45 (3.80, 8.62) ×108 cells/kg of mononuclear cells and 8.82 (6.12, 11.80) ×106 cells/kg of donor CD34+ stem cells (data from 8 patients respectively). Cyclosporine A was used for graft-versus-host disease (GVHD) prophylaxis in all patients with available data [10/10]. Seven patients also received methotrexate and 1 patient also received mycophenolate mofetil (in addition to cyclosporine A) for GVHD prophylaxis.
Curative outcome (within + 1 year) post-HSCT was noted in 73% [8/11] patients. Stable engraftment (including consistent expression of CD40 on lymphocytes/monocytes), resolution of neutropenia (if present), and successful discontinuation of IgRT (with improved IgA or total/specific IgG levels or without breakthrough infections) reflected cure in these patients. Notably, one of these 8 patients received transplant from a carrier (heterozygous CD40 variant) sibling with excellent outcomes. Total follow-up duration in these patients (who had curative HSCT) was 440 patient-months (individual follow-up duration range of 12 to 116 months).
Fatal outcomes have been noted in 15% [2/13] patients who underwent HSCT (Fig. 6). Reasons for death (age at death [duration post-HSCT]) were severe pulmonary infection leading to respiratory failure (~ 1.9 years [+ 16 days]) and sepsis (~ 7.7 years [+ 5 months]). Neutrophil engraftment occurred at day + 10 in the first patient; however, engraftment of donor lymphocytes was not observed at demise (+ 16 days). This patient had had a severe pretransplant disease course with recurrent pulmonary infections including necrotizing pneumonia due to P. aeruginosa (followed by Pseudomonal respiratory tract colonization) and disseminated C. parvum infection (including severe respiratory tract infection) The second patient (demise at + 5.5 months) also suffered from infection (Aspergillus sp.) and GVHD (acute, affecting skin and liver) in the post-transplant period. Both these patients received a non-myeloablative HSCT from a matched related donor (Supplementary Fig. 1 [Fig. S1]).
Patient-wise post-transplant morbidity/complications included (i) CMV viremia (donor was CMV positive), (ii) RSV/CMV pneumonitis and renal tubular dysfunction, (iii) chronic GVHD and persistent severe B-cell lymphopenia (meriting utilization of IgRT), (iv) renal dysfunction (drug-induced), (v) acute GVHD (grade II skin involvement), veno-occlusive disease, and hemorrhagic cystitis (cyclophosphamide induced) [this patient was diagnosed on screening {age: 1 month} and transplanted pre-emptively {age: 6 months} before the onset of clinical manifestations].
Discussion
Summary of Findings
CD40 deficiency is a rare inborn error of immunity. Expectedly, data regarding the clinical features, immunohematological aberrations, treatment, and outcomes are based only on case reports/series or small-sized cohort studies (largest study comprised of 11 patients). Herein, we have provided a comprehensive overview of CD40 deficiency by performing a systematic review of all reported patients. CD40 deficiency presents in the first few years of life with infections from a wide variety of pathogens including parasites, fungi, bacteria, and uncommonly viruses. Sinopulmonary, gastrointestinal, and biliary systems are primarily afflicted. Severe reduction in serum IgG levels, normal/elevated IgM levels, and defective class-switching of B-cells/memory B-cells are the characteristic immunological aberrations. Neutropenia is a crucial accompaniment in nearly two-thirds of the patients. Although detection of defective CD40 expression on B-cells and/or monocytes serves as a rapid diagnostic tool in majority of the patients, molecular testing is required to confirm the diagnosis (notably, stop-loss variants are associated with normal CD40 expression). IgRT and antimicrobial prophylaxis are the standard treatment modalities while HSCT is a curative therapeutic modality with promising long-term outcomes.
Immunopathogenetic Mechanisms in CD40 Deficiency – a Brief Overview
CD40 deficiency is classified as a combined immunodeficiency according to the recent International Union of Immunological societies (IUIS) classification [6]. Impaired CD40-CD40L signaling results in profound functional defects in B-cells (including impaired antibody production and class switching, impaired generation of memory B-cells) which forms the etiopathogenetic basis of humoral immunodeficiency observed in these patients [1, 3, 5, 7]. Predisposition to develop opportunistic infections, particularly C. parvum and P. jirovecii, reflects clinically the underlying cellular immunodeficiency. Aberrant CD40 expression on dendritic cells results in impaired upregulation of MHC class II and other costimulatory molecules on these cells. Besides, dendritic cells in CD40 deficiency have defective production of various cytokines including IFN-α (crucial for antiviral responses) and IL-12 (vital for T-cell activation and production of IFN-γ) [4, 34, 41].
We noted neutropenia to occur in nearly two-thirds of children with CD40 deficiency. A similar frequency of neutropenia has also been observed in CD40L deficiency [8]. These clinical data reflect the importance of CD40-CD40L signaling in regulating granulopoiesis. Myelopoiesis is known to be a complex process dependent on numerous cytokines and transcription factors. Granulocyte- and granulocyte/monocyte- colony stimulating factors (G-CSF and GM-CSF, respectively) are two important regulators of granulopoiesis produced by fibroblasts, monocytes, macrophages, and endothelial cells [42]. The stromal cells of bone marrow also express CD40 and, on binding with CD40L, upregulates G-CSF and GM-CSF expression [43]. Other mechanisms (e.g. CD40L-mediated augmentation of myelopoiesis) may also play a role in evolution of neutropenia in CD40 and CD40L defects [44].
Sclerosing cholangitis (including biliary radicle dilatation) have been observed in more than one-third of patients in CD40 deficiency which has resulted in chronic liver disease and fatal outcomes in a subset. Impaired clearance of biliary tract C. parvum due to defective cell-mediated immunity appears to be the primary pathogenetic mechanism of sclerosing cholangitis in CD40 deficiency [45]. In various knockout mouse models of sclerosing cholangitis (corresponding to deficiencies of CD40, CD40L and IFNG [encoding IFN-γ]), persistent C. parvum has been shown to result in features reminiscent of sclerosing cholangitis (mediated through direct toxic effects of C. parvum and inflammatory cytokines like TNF-α) [46,47,48]. Increased gut permeability due to chronic diarrhea (microbial components and/or toxins entering portal circulation) and autoimmunity may be other potential mechanisms resulting in sclerosing cholangitis in patients with CD40 deficiency [49].
CD40 Deficiency vs. CD40-Ligand Deficiency – Comparison of Clinical Phenotypes
Similar to CD40 deficiency, most of the patients with CD40L deficiency have sinopulmonary infections (Fig. S2). More than half of patients with CD40 deficiency experience chronic/recurrent diarrhea in comparison to nearly two-fifth of patients with CD40L deficiency [26, 50,51,52]. A comparable proportion of patients suffer from skin/soft tissue infections in CD40 and CD40L deficiency [26, 51,52,53]. Sclerosing cholangitis appears to be more prevalent in patients with CD40 deficiency (~ 30%) in comparison to CD40L defects (< 10%) [26, 50,51,52]. Cryptosporidal infections are reported in less than one-fifth of patients with CD40L deficiency [26, 49, 50]. On the other hand, infections with C. parvum are the most frequent in CD40 deficiency (seen in nearly one-third of patients). The differences in frequency of cryptosporidal infections (and hence sclerosing cholangitis) may be indicative of variability in the ethnic distribution of reported patients with CD40L/CD40 deficiency. Largest cohorts of patients with CD40L deficiency have been reported from US and (Western) Europe while majority of reported patients with CD40 deficiency belong to the Middle East and North Africa (MENA). Incidence of cryptosporidal infections in children has been noted to be higher in the MENA compared to US and Western Europe which may be related to disparities in social, economic, and demographic variables (including the amount of Cryptosporidium sp. present in ‘potable’ water) [54, 55]. P. jirovecii is, by far, the most frequently identified pathogen in patients with CD40L deficiency (seen in ≥ 30% patients in large cohorts) [8, 26, 49, 51]. Our systematic review revealed a lower frequency of pneumocystis infections in patients with CD40 deficiency (nearly one-fifth) as compared to CD40L deficiency (Fig. S2). Besides, the gamut of infectious organisms affecting patients with CD40 deficiency appears narrower. In contrast to X-HIGM, infections from herpes simplex virus, human papilloma virus, enteroviruses (including meningoencephalitis), molluscum contagiosum virus, parvovirus B19, JC virus, Cryptococcus sp., Histoplasma sp., Isospora sp., Microsporidium sp., Entamoeba histolytica, Salmonella sp., Campylobacter sp., and Bartonella sp. are not reported in CD40 deficiency [8, 50]. The precise reasons for the differences in clinical and microbial profile remain unknown. However, CD40L also binds to various integrins (including αMβ2 [CD11b/CD18] expressed on neutrophils, monocytes/macrophages, and NK cells) besides CD40 which may result in more pleotropic immune defects in CD40L deficiency as compared to CD40 deficiency [56]. The rarity of CD40 deficiency is an important confounding factor that needs to be considered while assessing these differences (especially restricted microbial profile in CD40 deficiency).
CD40 Deficiency vs. CD40-Ligand Deficiency – Comparison of HSCT Outcomes
Reports on outcomes of HSCT in CD40 deficiency have provided encouraging results. However, detailed data of only a dozen patients with CD40 deficiency who underwent a transplant have been published so far. Nonetheless, curative outcomes post-HSCT have been noted in nearly three-fourths of these patients who have fared well over the long-term (range ~ 1–10 years). Fatal outcomes have been reported in 2 (15%) patients while GVHD has been reported in 3 patients (~ 25% of patients with available data). Notably, post-transplant course has been reported to be uneventful in nearly 40% patients. Outcomes of HSCT have been reported for > 100 patients with CD40L deficiency with greater durations of follow-up (up to fourth decade) [53, 57]. Long-term (~ 10 years post-HSCT) overall survival of ~ 90% have been reported in these patients which appears to be better than CD40 deficiency [8, 53, 57]. Conversely, frequency of GVHD in CD40L deficiency (> 40%) appears to be higher than in CD40 deficiency [8]. Besides differences in disease pathobiology and variability of transplant protocols, number of patients transplanted, age at transplant, and duration of follow-up are important factors that need to be considered while interpreting these findings. We were unable to discern any significant differences in overall survival between transplanted and untransplanted patients with CD40 deficiency (Fig. 6). Similarly, the final edict regarding whether HSCT should be performed soon after diagnosis of CD40L deficiency is lacking (especially in absence of matched related donors). However, a significant probability of uneventful curative post-transplant outcomes and a better quality of life make HSCT a crucial therapeutic modality in these diseases.
Strengths and Limitations
An inclusive analysis of all reported patients with CD40 deficiency is the strength of our systematic review. Besides, we provide a comprehensive description of all important aspects of this inborn error of immunity ranging from basic clinical/immunohematological features, molecular defects, treatment modalities, and outcomes. Lack of complete clinical data of 11–13 patients (mostly published as part of large IEI registry data) limits the robustness of our study. Retrieval of pertinent data of these patients was beyond the scope of our study. Besides, a detailed genotype phenotype correlation could not be performed as meaningful grouping of molecular variants (with sufficient numbers in each group for statistical analysis) was not possible (Fig. S3, Table S3). Except patients with stop-loss variants, CD40 expression was severely reduced to absent across all other molecular subtypes (e.g. missense, splice-site, etc.).
Future Research Implications
The Jeffrey Modell Foundation global report on IEIs identifies dozens of patients with CD40 deficiency especially from the United States [58]. The clinicoimmunological profile, treatment strategies (including HSCT), and outcomes of these patients have not been published so far. Multicentric studies are needed to evaluate these data which would provide additional insights regarding this rare IEI. This would also facilitate optimal management of these patients the world over.
Data Availability
Relevant data/methods utilized in the preparation of this manuscript are provided in the manuscript and electronic supplementary material. Additional data underlying this article will be shared on reasonable request to the corresponding author.
References
van Kooten C, Banchereau J. Functions of CD40 on B cells, dendritic cells and other cells. Curr Opin Immunol. 1997;9(3):330–7. https://doi.org/10.1016/s0952-7915(97)80078-7.
Hollenbaugh D, Grosmaire LS, Kullas CD, Chalupny NJ, Braesch-Andersen S, Noelle RJ, et al. The human T cell antigen gp39, a member of the TNF gene family, is a ligand for the CD40 receptor: expression of a soluble form of gp39 with B cell co-stimulatory activity. EMBO J. 1992;11(12):4313–21. https://doi.org/10.1002/j.1460-2075.1992.tb05530.x.
Laman JD, Claassen E, Noelle RJ. Functions of CD40 and its ligand, gp39 (CD40L). Crit Rev Immunol. 2017;37(2–6):371–420. https://doi.org/10.1615/CritRevImmunol.v37.i2-6.100.
Ma DY, Clark EA. The role of CD40 and CD154/CD40L in dendritic cells. Semin Immunol. 2009;21(5):265–72. https://doi.org/10.1016/j.smim.2009.05.010.
Aruffo A, Farrington M, Hollenbaugh D, Li X, Milatovich A, Nonoyama S, et al. The CD40 ligand, gp39, is defective in activated T cells from patients with X-linked hyper-IgM syndrome. Cell. 1993;72(2):291–300. https://doi.org/10.1016/0092-8674(93)90668-g.
Tangye SG, Al-Herz W, Bousfiha A, Cunningham-Rundles C, Franco JL, Holland SM, et al. Human inborn errors of immunity: 2022 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol. 2022;42(7):1473–507. https://doi.org/10.1007/s10875-022-01289-3.
Ferrari S, Giliani S, Insalaco A, Al-Ghonaium A, Soresina AR, Loubser M, et al. Mutations of CD40 gene cause an autosomal recessive form of immunodeficiency with hyper IgM. Proc Natl Acad Sci U S A. 2001;98(22):12614–9. https://doi.org/10.1073/pnas.221456898.
França TT, Barreiros LA, Al-Ramadi BK, Ochs HD, Cabral-Marques O, Condino-Neto A. CD40 ligand deficiency: treatment strategies and novel therapeutic perspectives. Expert Rev Clin Immunol. 2019;15(5):529–40. https://doi.org/10.1080/1744666X.2019.1573674.
Hirbod-Mobarakeh A, Aghamohammadi A, Rezaei N. Immunoglobulin class switch recombination deficiency type 1 or CD40 ligand deficiency: from bedside to bench and back again. Expert Rev Clin Immunol. 2014;10(1):91–105. https://doi.org/10.1586/1744666X.2014.864554.
Lougaris V, Badolato R, Ferrari S, Plebani A. Hyper immunoglobulin M syndrome due to CD40 deficiency: clinical, molecular, and immunological features. Immunol Rev. 2005;203:48–66. https://doi.org/10.1111/j.0105-2896.2005.00229.x.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
PICO Portal. Identifying duplicates with PICO Portal. 2022. Available from: https://picoportal.org/2022/02/01/identifying-duplicates-with-pico-portal/. Accessed 7 Aug 2023.
Banday AZ, Jindal AK, Kaur A, Kumar Y, Nameirakpam J, Patra PK, Rawat A. A young girl with hypogammaglobulinemia and granulomatous hepatitis caused by a novel mutation in ZBTB24 gene: a case based analysis. Immunobiology. 2020;225(3):151912. https://doi.org/10.1016/j.imbio.2020.151912.
Kutukculer N, Moratto D, Aydinok Y, Lougaris V, Aksoylar S, Plebani A, et al. Disseminated cryptosporidium infection in an infant with hyper-IgM syndrome caused by CD40 deficiency. J Pediatr. 2003;142(2):194–6. https://doi.org/10.1067/mpd.2003.41.
Mazzolari E, Lanzi G, Forino C, Lanfranchi A, Aksu G, Ozturk C, et al. First report of successful stem cell transplantation in a child with CD40 deficiency. Bone Marrow Transplant. 2007;40(3):279–81. https://doi.org/10.1038/sj.bmt.1705713.
Karaca NE, Forveille M, Aksu G, Durandy A, Kutukculer N. Hyper-immunoglobulin M syndrome type 3 with normal CD40 cell surface expression. Scand J Immunol. 2012;76(1):21–5. https://doi.org/10.1111/j.1365-3083.2012.02697.x.
Al-Saud BK, Al-Sum Z, Alassiri H, Al-Ghonaium A, Al-Muhsen S, Al-Dhekri H, et al. Clinical, immunological, and molecular characterization of hyper-IgM syndrome due to CD40 deficiency in eleven patients. J Clin Immunol. 2013;33(8):1325–35. https://doi.org/10.1007/s10875-013-9951-9.
Mishra A, Italia K, Gupta M, Desai M, Madkaikar M. Hyperimmunoglobulin syndrome due to CD40 deficiency: possibly the first case from India. J Postgrad Med. 2015;61(1):46–8. https://doi.org/10.4103/0022-3859.147053.
Murguia-Favela L, Sharfe N, Karanxha A, Bates A, Dadi H, Cimpean L, Roifman CM. CD40 deficiency: a unique adult patient with hyper immunoglobulin M syndrome and normal expression of CD40. LymphoSign J. 2017;4(2):70–6. https://doi.org/10.14785/lymphosign-2017-0004.
Bahrami A, Soltani Z, Fazlollahi MR, Rahmani F, Houshmand M, Mazinani M, Rezaei N. Adenoid hyperplasia in a patient with a rare type of hyper immunoglobulin M syndrome due to CD40 deficiency. Acta Med Iran. 2018:811–4. Available from: https://acta.tums.ac.ir/index.php/acta/article/download/7252/5201/. Accessed 30 Nov 2022.
Al-Saud B, Al-Jomaie M, Al-Ghonaium A, Al-Ahmari A, Al-Mousa H, Al-Muhsen S, et al. Haematopoietic stem cell transplant for hyper-IgM syndrome due to CD40 defects: a single-centre experience. Bone Marrow Transplant. 2019;54(1):63–7. https://doi.org/10.1038/s41409-018-0219-0.
Renner ED, Krätz CE, Orange JS, Hagl B, Rylaarsdam S, Notheis G, et al. Class switch recombination defects: impact on B cell maturation and antibody responses. Clin Immunol. 2021;222:108638. https://doi.org/10.1016/j.clim.2020.108638.
Akarsu A, Halaçlı S, Tan Ç, Kuşkonmaz B, Küpesiz A, Çetinkaya D, et al. A single-center study points to diverse features and outcome in patients with hyperimmunoglobulin M syndrome and class‐switch recombination defects. Scand J Immunol. 2022;96(5):e13213. https://doi.org/10.1111/sji.13213.
Rawat A, Sharma M, Vignesh P, Jindal AK, Suri D, Das J, et al. Utility of targeted next generation sequencing for inborn errors of immunity at a tertiary care centre in North India. Sci Rep. 2022;12(1):10416. https://doi.org/10.1038/s41598-022-14522-1.
Hsu J, Massaad M, Notarangelo LD. Successful hematopoietic stem cell transplant for CD40 deficiency manifesting as hyper-IgM syndrome with absent CD40 expression and marked lymphocytosis. J Allergy Clin Immunol. 2014;133(2):AB95. https://doi.org/10.1016/j.jaci.2013.12.354.
Leven EA, Maffucci P, Ochs HD, Scholl PR, Buckley RH, Fuleihan RL, et al. Hyper IgM syndrome: a report from the USIDNET Registry. J Clin Immunol. 2016;36(5):490–501. https://doi.org/10.1007/s10875-016-0291-4.
Galal N, Meshaal S, Elhawary R, ElAziz DA, Alkady R, Lotfy S, et al. Patterns of primary immunodeficiency disorders among a highly consanguineous population: Cairo University Pediatric Hospital’s 5-year experience. J Clin Immunol. 2016;36(7):649–55. https://doi.org/10.1007/s10875-016-0314-1.
Barbouche MR, Mekki N, Ben-Ali M, Ben-Mustapha I. Lessons from genetic studies of primary immunodeficiencies in a highly consanguineous population. Front Immunol. 2017;8:737. https://doi.org/10.3389/fimmu.2017.00737.
Fioredda F, Pierri F, Palmisani E, Finocchi A, Di Matteo G, Palumbo G, et al. Severe chronic neutropenia: primary immunodeficiency mutations are frequent causative agents. Blood. 2018;132(S1):2402. https://doi.org/10.1182/blood-2018-99-114462.
El-Helou SM, Biegner AK, Bode S, Ehl SR, Heeg M, Maccari ME, et al. The German National Registry of primary immunodeficiencies (2012–2017). Front Immunol. 2019;10:1272. https://doi.org/10.3389/fimmu.2019.01272.
Linares NA, Bouchard M, Gutiérrez NS, Colmenares M, Cantor-Garcia A, Gabaldon-Figueira JC, et al. Immunological features in pediatric patients with recurrent and severe infection: identification of primary immunodeficiency diseases in Merida, Venezuela. Allergol Immunopathol (Madr). 2019;47(5):437–48. https://doi.org/10.1016/j.aller.2019.02.002.
Belaid B, Lamara Mahammed L, Drali O, Oussaid AM, Touri NS, Melzi S, et al. Inborn errors of immunity in Algerian children and adults: a single-center experience over a period of 13 years (2008–2021). Front Immunol. 2022;13:900091. https://doi.org/10.3389/fimmu.2022.900091.
Vonniessen N, Ahmed E, Hazzazi K, Mourad W, Mazer B. Profiling B-cell response: Hyperimmunoglobulin M syndrome due to CD40 deficiency. J Allergy Clin Immunol. 2023;151(2):AB334. https://doi.org/10.1016/j.jaci.2022.12.774.
Fontana S, Moratto D, Mangal S, De Francesco M, Vermi W, Ferrari S, et al. Functional defects of dendritic cells in patients with CD40 deficiency. Blood. 2003;102(12):4099–106. https://doi.org/10.1182/blood-2003-04-1244.
Lanzi G, Ferrari S, Vihinen M, Caraffi S, Kutukculer N, Schiaffonati L, et al. Different molecular behavior of CD40 mutants causing hyper-IgM syndrome. Blood. 2010;116(26):5867–74. https://doi.org/10.1182/blood-2010-03-274241.
Cicalese MP, Gerosa J, Baronio M, Montin D, Licciardi F, Soresina A, et al. Circulating follicular helper and follicular regulatory T cells are severely compromised in human CD40 deficiency: a case report. Front Immunol. 2018;9:1761. https://doi.org/10.3389/fimmu.2018.01761.
Kutukculer N, Aksoylar S, Kansoy S, Cetingul N, Notarangelo LD. Outcome of hematopoietic stem cell transplantation in hyper-IgM syndrome caused by CD40 deficiency. J Pediatr. 2003;143(1):141–2. https://doi.org/10.1016/S0022-3476(03)00274-9.
Dirim D, Dagci H, Turgay N. Disseminated cryptosporidiosis in Turkey: case report. East Afr Med J. 2003;80(10):550–2. https://doi.org/10.4314/eamj.v80i10.8760.
Al-Dhekri H, Al-Sum Z, Al-Saud B, Al-Mousa H, Ayas M, Al-Muhsen S, et al. Successful outcome in two patients with CD40 deficiency treated with allogeneic HCST. Clin Immunol. 2012;143(1):96–8. https://doi.org/10.1016/j.clim.2012.01.012.
Wintergerst U, Durandy A, Belohradsky BH. Clinical course of a female patient with CD40-deficiency. Clin Exp Immunol. 2008;154(S1):186.
Cella M, Sallusto F, Lanzavecchia A. Origin, maturation and antigen presenting function of dendritic cells. Curr Opin Immunol. 1997;9(1):10–6. https://doi.org/10.1016/s0952-7915(97)80153-7.
Mehta HM, Corey SJ. G-CSF, the guardian of granulopoiesis. Semin Immunol. 2021;54:101515. https://doi.org/10.1016/j.smim.2021.101515.
Mavroudi I, Papadaki V, Pyrovolaki K, Katonis P, Eliopoulos AG, Papadaki HA. The CD40/CD40 ligand interactions exert pleiotropic effects on bone marrow granulopoiesis. J Leukoc Biol. 2011;89(5):771–83. https://doi.org/10.1189/jlb.0610330.
Solanilla A, Déchanet J, El Andaloussi A, Dupouy M, Godard F, Chabrol J, et al. CD40-ligand stimulates myelopoiesis by regulating flt3-ligand and thrombopoietin production in bone marrow stromal cells. Blood. 2000;95(12):3758–64.
Pollheimer MJ, Halilbasic E, Fickert P, Trauner M. Pathogenesis of primary sclerosing cholangitis. Best Pract Res Clin Gastroenterol. 2011;25(6):727–39. https://doi.org/10.1016/j.bpg.2011.10.009.
Stephens J, Cosyns M, Jones M, Hayward A. Liver and bile duct pathology following Cryptosporidium parvum Infection of immunodeficient mice. Hepatology. 1999;30(1):27–35. https://doi.org/10.1002/hep.510300138.
Ungar BL, Burris JA, Quinn CA, Finkelman FD. New mouse models for chronic Cryptosporidium Infection in immunodeficient hosts. Infect Immun. 1990;58(4):961–9. https://doi.org/10.1128/iai.58.4.961-969.1990.
Ponnuraj EM, Hayward AR. Requirement for TNF-Tnfrsf1 signalling for sclerosing cholangitis in mice chronically infected by Cryptosporidium parvum. Clin Exp Immunol. 2002;128(3):416–20. https://doi.org/10.1046/j.1365-2249.2002.01861.x.
Pollheimer MJ, Fickert P. Animal models in primary biliary Cirrhosis and primary sclerosing cholangitis. Clin Rev Allergy Immunol. 2015;48(2–3):207–17. https://doi.org/10.1007/s12016-014-8442-y.
Levy J, Espanol-Boren T, Thomas C, Fischer A, Tovo P, Bordigoni P, et al. Clinical spectrum of X-linked hyper-IgM syndrome. J Pediatr. 1997;131(1 Pt 1):47–54. https://doi.org/10.1016/s0022-3476(97)70123-9.
Winkelstein JA, Marino MC, Ochs H, Fuleihan R, Scholl PR, Geha R, et al. The X-linked hyper-IgM syndrome: clinical and immunologic features of 79 patients. Medicine (Baltim). 2003;82(6):373–84. https://doi.org/10.1097/01.md.0000100046.06009.b0.
Du X, Tang W, Chen X, Zeng T, Wang Y, Chen Z, et al. Clinical, genetic and immunological characteristics of 40 Chinese patients with CD40 ligand deficiency. Scand J Immunol. 2019;90(4):e12798. https://doi.org/10.1111/sji.12798.
Mitsui-Sekinaka K, Imai K, Sato H, Tomizawa D, Kajiwara M, Nagasawa M, et al. Clinical features and hematopoietic stem cell transplantations for CD40 ligand deficiency in Japan. J Allergy Clin Immunol. 2015;136(4):1018–24. https://doi.org/10.1016/j.jaci.2015.02.020.
Khalil IA, Troeger C, Rao PC, Blacker BF, Brown A, Brewer TG, et al. Morbidity, mortality, and long-term consequences associated with Diarrhoea from Cryptosporidium Infection in children younger than 5 years: a meta-analyses study. Lancet Glob Health. 2018;6(7):e758-68. https://doi.org/10.1016/S2214-109X(18)30283-3.
Hijjawi N, Zahedi A, Al-Falah M, Ryan U. A review of the molecular epidemiology of Cryptosporidium spp. and Giardia Duodenalis in the Middle East and North Africa (MENA) region. Infect Genet Evol. 2022;98:105212. https://doi.org/10.1016/j.meegid.2022.105212.
Aloui C, Prigent A, Sut C, Tariket S, Hamzeh-Cognasse H, Pozzetto B, et al. The signaling role of CD40 ligand in platelet biology and in platelet component transfusion. Int J Mol Sci. 2014;15(12):22342–64. https://doi.org/10.3390/ijms151222342.
de la Morena MT, Leonard D, Torgerson TR, Cabral-Marques O, Slatter M, Aghamohammadi A, et al. Long-term outcomes of 176 patients with X-linked hyper-IgM syndrome treated with or without hematopoietic cell transplantation. J Allergy Clin Immunol. 2017;139(4):1282–92. https://doi.org/10.1016/j.jaci.2016.07.039.
Modell V, Knaus M, Modell F, Roifman C, Orange J, Notarangelo LD. Global overview of primary immunodeficiencies: a report from Jeffrey Modell Centers worldwide focused on diagnosis, treatment, and discovery. Immunol Res. 2014;60(1):132–44. https://doi.org/10.1007/s12026-014-8498-z.
Acknowledgements
LDN is supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, Bethesda, MD, USA.
Funding
None.
Author information
Authors and Affiliations
Contributions
AZB, RN: Conception of idea and design of the study; literature review; acquisition, analysis, and interpretation of data; and drafted, edited, and revised the manuscript.
PKP, AK, RS, CC, STAB, SZB: Editing and revision of the manuscript; acquisition, analysis, and interpretation of data; and literature review.
DB, LDN: Editing and critical revision of the manuscript; interpretation of data; literature review; and overall supervision of manuscript preparation.
All authors approve the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
As this study pertains to literature review and analysis of previously published data, ethics approval and consent is not mandated.
Consent to Participate and Consent for Publication
Not applicable.
Conflict of Interest or Competing Interests
None.
Note
All figures provided in this article are original and have not been published elsewhere. Multiple affiliations of the first author (AZB) are sequential affiliations that have changed during the course of the work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aaqib Zaffar Banday and Rahila Nisar contributed equally and qualify as joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
ESM 1
(PDF 270 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Banday, A.Z., Nisar, R., Patra, P.K. et al. Clinical and Immunological Features, Genetic Variants, and Outcomes of Patients with CD40 Deficiency. J Clin Immunol 44, 17 (2024). https://doi.org/10.1007/s10875-023-01633-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10875-023-01633-1