Abstract
Autoimmune lymphoproliferative syndrome (ALPS) is a disease of lymphocyte homeostasis caused by FAS-mediated apoptotic pathway dysfunction and is characterized by non-malignant lymphoproliferation with an increased number of TCRαβ+CD4−CD8− double-negative T cells (αβDNTs). Conversely, RAS-associated leukoproliferative disease (RALD), which is caused by gain-of-functional somatic variants in KRAS or NRAS, is considered a group of diseases with a similar course. Herein, we present a 7-year-old Japanese female of RALD harboring NRAS variant that aggressively progressed to juvenile myelomonocytic leukemia (JMML) with increased αβDNTs. She eventually underwent hematopoietic cell transplantation due to acute respiratory distress which was caused by pulmonary infiltration of JMML blasts. In general, αβDNTs have been remarkably increased in ALPS; however, FAS pathway gene abnormalities were not observed in this case. This case with RALD had repeated shock/pre-shock episodes as the condition progressed. This shock was thought to be caused by the presence of a high number of αβDNTs. The αβDNTs observed in this case revealed high CCR4, CCR6, and CD45RO expressions, which were similar to Th17. These increased Th17-like αβDNTs have triggered the inflammation, resulting in the pathogenesis of shock, because Th17 secretes pro-inflammatory cytokines such as interleukin (IL)-17A and granulocyte-macrophage colony-stimulating factor. The presence of IL-17A-secreting αβDNTs has been reported in systemic lupus erythematosus (SLE) and Sjögren’s syndrome. The present case is complicated with SLE, suggesting the involvement of Th17-like αβDNTs in the disease pathogenesis. Examining the characteristics of αβDNTs in RALD, JMML, and ALPS may reveal the pathologies in these cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We report an atypical RAS-associated leuko-proliferative disease (RALD) case which aggressively progressed to juvenile myelomonocytic leukemia (JMML) with various complications, including increased TCRαβ+CD4−CD8− double-negative T cells, chronic lymphadenopathy, hepatosplenomegaly, hemophagocytic lymphohistiocytosis (HLH), and systemic lupus erythematosus (SLE).
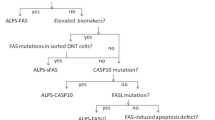
Autoimmune lymphoproliferative syndrome (ALPS) is a disease of lymphocyte homeostasis caused by FAS-mediated apoptotic pathway dysfunction and is characterized by lymphoproliferation with an increased number of TCRαβ+CD4−CD8− double-negative T cells (αβDNTs) [1]. Conversely, RALD is caused by gain-of-function somatic variants in KRAS or NRAS, clinically resembling ALPS [2, 3]. RALD shows autoimmunity, lymphadenopathy, and/or splenomegaly, but with no defect in FAS-dependent apoptosis and with normal or marginally increased αβDNTs in peripheral blood [1, 3]. Some cases with RALD show partial overlap with JMML, suggesting a continuous disease concept [4].
Herein, we report a 7-year-old Japanese female with RALD and SLE followed by JMML, who was finally successfully treated by allogenic hematopoietic cell transplantation (HCT). The clinical characteristics of this case were reported as patient 1 in a previous article [5]. We additionally report a detailed investigation of the difference between ALPS and RALD using flow cytometry.
At 4-month-old, she was admitted to our hospital with a developed fever and hepatosplenomegaly. Laboratory testing revealed pancytopenia, liver dysfunction, elevated serum lactate dehydrogenase (2909 U/L) and ferritin (12,122 U/ml), and severe coagulopathy (Table S1). She was diagnosed with HLH and was treated with dexamethasone, cyclosporine A, and prednisolone, which improve her condition. However, γ-globulin was gradually increased, and thrombocytopenia proceeded along with the dose de-escalation. She was suspected of ALPS at 2 years because of increased αβDNTs in her peripheral blood. However, we did not detect any coding variants in genes involved in the FAS pathway and known to underlie ALPS. A whole-exome sequencing was performed at the age of 2 years and 3 months, which detected a somatic mosaic variant of NRAS G13D, leading to RALD diagnosis. Functional analysis of the gain-of-function NRAS G13D variant has been reported previously [2]. In further analysis, NRAS G13D variant was observed as mosaicism in the nails (0–22%) and blood cells (67%), including T cells, natural killer cells, and αβDNTs [5]. Almost simultaneously, facial erythema and proteinuria appeared, and anti-dsDNA antibody turned positive. A renal biopsy revealed lupus type V, and she was diagnosed with SLE and lupus nephritis. These symptoms were improved with tacrolimus and remained in remission. However, monocytes markedly increased at around 4 years of age, and bone marrow examination revealed mild dysplasia and high granulocyte-macrophage colony-stimulating factor (GM-CSF) sensitivity, indicating the JMML diagnosis. Around this time, she began to have repeated hospitalizations for shock state (Fig. 1A).
A Clinical course from diagnosis to hematopoietic cell transplantation (HCT). B The conditioning regimen of HCT. The conditioning regimen was consisted of total body irradiation (3 Gy on day -3), busulfan (0.8 mg/kg × 4/day on days -11 and -10), L-PAM (90 mg/m2 × 2 from days -5 and -4), and flu (30 mg/m2 from days -9 to -6). Tacrolimus and short-term methotrexate (15 mg on day 3, 10 mg on day 7, and 10 mg on day 15) were employed for the prophylaxis of graft-versus-host disease (GVHD). TBI, total body irradiation. C–F All immunophenotyping analyses were performed at 5–6 years of age, almost same time progression to JMML. C CCR4 is highly expressed on the surface of αβDNTs in this case with RALD. D Comparison of surface CD45RO, CCR6, and CXCR3 expressions in αβDNTs of these RALD and ALPS cases. E Comparison of intracellular expression of RORγt in αβDNTs of these RALD and ALPS cases. The αβDNTs of RALD intracellularly expressed RORγt. F Comparison of IL-17A and IL-10 production in αβDNTs between RALD and ALPS cases. Stimulation was performed with PMA and ionomycin for 4 h. The αβDNTs of RALD can produce IL-17A and little IL-10, while the αβDNTs of ALPS can produce IL-10 and little IL-10
Respiratory distress symptoms appeared at the age of 6 years, and a chest computed tomography scan revealed mottled shadows around the bronchioles. A thoracoscopic lung biopsy was performed at the age of 7 years, which revealed monocyte infiltration in the lung tissue (Figure S1). She was diagnosed with acute exacerbation of JMML, and we decided to perform allogeneic HCT. She underwent HCT from an HLA fully matched unrelated donor. The conditioning regimen is shown in Fig. 1B. 5 × 106 total nucleus cells/kg (3 × 105 CD34 cells /kg) was transfused. Tacrolimus and short-term methotrexate (15 mg on day 3, 10 mg on day 7, and 10 mg on day 15) were employed for the prophylaxis of graft-versus-host disease (GVHD). The case suffered several transplantation-related complications, including grade 1 acute GVHD (mucositis, skin rash, fever, and diarrhea), which were detected on day 21 and were controllable with prednisolone. Hematological reconstitution was normally observed. The case had a good clinical course after transplantation, and since then, the disease has stabilized. Granular or mottled shadows of pulmonary infiltrates were dramatically improved (Figure S1). The incidence of αβDNTs has been in the same range as that of healthy subjects (Fig. 1C), and both SLE and JMML have ameliorated without event for >4 years without any relapse without steroid or immunosuppressive drug administration.
The αβDNTs of this case expressed CD45RO and chemokine receptors CCR4 and CCR6 [6]. However, the αβDNT cells of the case with ALPS expressed few of these (Fig. 1C and D). In contrast, CXCR3 was not expressed on αβDNTs of RALD but expressed on these of ALPS (Fig. 1D). CD45RO is the surface marker of memory T cells, and CCR4, CCR6, and CXCR3 can help discriminate between helper T cell subtypes: Th1, CCR4−CCR6−CXCR3+; Th2, CCR4+CCR6−CXCR3−; and Th17, CCR4+CCR6+CXCR3− (Supplementary Figure S2) [6].
The αβDNTs of RALD were recognized as CD45RO+CCR4+CCR6+CXCR3− in general [6], thereby indicating similarity as Th17 other than CD4 expression. As RORγt is the master regulator transcription factor for Th17 and Th17 has intracellular RORγt expression [7, 8], we analyzed RORγt expression in the αβDNTs. The αβDNTs of RALD had intracellular RORγt expression but not with ALPS (Fig. 1E). Th17 produces IL-17A and αβDNTs of ALPS produce IL-10 [9]; we analyzed whether αβDNTs produce IL-17A and IL-10 or not. The αβDNTs of RALD produced IL-17A, and ALPS did not produce it. Conversely, the αβDNTs of RALD did not produce IL-10. Hence, this RALD case produced IL-17A and little IL-10, while the two ALPS cases produced IL-10 without IL-17A (Fig. 1F).
We report a case of RALD that aggressively progressed to JMML with increased αβDNTs. αβDNTs are a legitimate component of the normal immune system. αβDNTs accumulate in the peripheral blood in ALPS and some diseases due to FAS apoptotic pathway variants. The number of αβDNTs is generally normal or slightly increased in cases with RALD. αβDNTs are thought to originate from CD4 and CD8 T cells that have lost their co-receptors, but their origin remains controversial. The αβDNTs of our case expressed CD45RO, CCR4, and CCR6 on the surface and RORγt in the cytoplasm and were capable of producing IL-17A, similar to Th17 and different from those observed in cases with ALPS-FAS. CD45RO is a T cell memory marker, and CCR4/CCR6 double-positive T cells have a Th17 phenotype. Thus, we speculated that the αβDNTs in this case were derived from Th17 after antigen exposure and that the NRAS variant contributed to αβDNT development. Th17 secretes a variety of inflammatory cytokines, such as GM-CSF as well as IL-17A, and this αβDNT might have a similar function. αβDNTs that produce IL-17A have been reported to be associated with infection [10], SLE [11], Sjögren’s syndrome [12], and other autoimmune diseases, but analysis using extracellular and intracellular markers has never been performed. The present case was complicated with SLE, suggesting the involvement of Th17-like αβDNTs in its pathogenesis. Some of the shock/pre-shock episodes of the case were induced by infection, but some of the symptoms were considered autoinflammatory based on primary disease exacerbation because the cause of the infection could not be identified. In particular, monocytes that met the diagnostic criteria for JMML and Th17-like αβDNT-induced inflammation were probably implicated in the shock pathogenesis. In this analysis, the association between these cells and the pathogenesis were not clearly proven, and further analysis is needed in similar cases. In the future, the characteristics of αβDNTs appearing in RALD and JMML may be investigated and accumulated to predict which pathology they may cause. Secondary gene alterations should be investigated in RALD cases in more detail.
Data Availability
All the data and material included in this work have been collected after signed informed consent by all the patients/patients’ relatives.
References
Oliveira JB, Bleesing JJ, Dianzani U, Fleisher TA, Jaffe ES, Lenardo MJ, et al. Revised diagnostic criteria and classification for the autoimmune lymphoproliferative syndrome (ALPS): report from the 2009 NIH International Workshop. Blood. 2010;116(14):e35–40.
Oliveira JB, Bidère N, Niemela JE, Zheng L, Sakai K, Nix CP, et al. NRAS mutation causes a human autoimmune lymphoproliferative syndrome. Proc Natl Acad Sci U S A. 2007;104(21):8953–8.
Takagi M, Shinoda K, Piao J, Mitsuiki N, Takagi M, Matsuda K, et al. Autoimmune lymphoproliferative syndrome-like disease with somatic KRAS mutation. Blood. 2011;117(10):2887–90.
Takagi M, Piao J, Lin L, Kawaguchi H, Imai C, Ogawa A, et al. Autoimmunity and persistent RAS-mutated clones long after the spontaneous regression of JMML. Leukemia. 2013;27(9):1926–8.
Shiota M, Yang X, Kubokawa M, Morishima T, Tanaka K, Mikami M, et al. Somatic mosaicism for a NRAS mutation associates with disparate clinical features in RAS-associated leukoproliferative disease: a report of two cases. J Clin Immunol. 2015;35(5):454–8.
Lubberts E. The IL-23-IL-17 axis in inflammatory arthritis. Nat Rev Rheumatol. 2015;11(7):415–29.
Ivanov II, McKenzie BS, Zhou L, Tadokoro CE, Lepelley A, Lafaille JJ, et al. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell. 2006;126(6):1121–33.
Evans CM, Jenner RG. Transcription factor interplay in T helper cell differentiation. Brief Funct Genomics. 2013;12(6):499–511.
Ohga S, Nomura A, Takahata Y, Ihara K, Takada H, Wakiguchi H. Dominant expression of interleukin 10 but not interferon gamma in CD4(-)CD8(-)alphabetaT cells of autoimmune lymphoproliferative syndrome. Br J Haematol. 2002;119(2):535–8.
Cowley SC, Meierovics AI, Frelinger JA, Iwakura Y, Elkins KL. Lung CD4-CD8- double-negative T cells are prominent producers of IL-17A and IFN-gamma during primary respiratory murine infection with Francisella tularensis live vaccine strain. J Immunol. 2010;184(10):5791–801.
Crispín JC, Oukka M, Bayliss G, Cohen RA, Van Beek CA, Stillman IE, et al. Expanded double negative T cells in cases with systemic lupus erythematosus produce IL-17 and infiltrate the kidneys. J Immunol. 2008;181(12):8761–6.
Alunno A, Bistoni O, Bartoloni Bocci E, Caterbi S, Bigerna B, Pucciarini A. IL-17-producing double- negative T cells are expanded in the peripheral blood, infiltrate the salivary gland and are partially resistant to corticosteroid therapy in cases with Sjögren’s syndrome. Reumatismo. 2013;65(4):192–8.
Acknowledgements
We thank Mayuko Miyake for her excellent assistance for the analysis of surface markers.
Funding
This work has been supported by basic research funds distributed annually by the university.
Author information
Authors and Affiliations
Contributions
T.O., H.K., and S.I. designed the research. D.K., T.O., N.S., and H.K. analyzed and interpreted data and wrote the manuscript. T.O., A.M., N.S., and H.K. performed flow cytometry analysis. D.K. and N.S. prepared the figures. M.T., Y.S., K.S., M.T., S.H., K.N., N.S., N.K., and S.I. treated the case; all authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Ethics Committee of the Yokohama City University Graduate School of Medicine (number: B160804004).
Consent to Participate
All the patients and relatives.
Consent for Publication
All the patients and relatives.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kurita, D., Shiba, N., Ohya, T. et al. Severe RAS-Associated Lymphoproliferative Disease Case with Increasing αβ Double-Negative T Cells with Atypical Features. J Clin Immunol 43, 1992–1996 (2023). https://doi.org/10.1007/s10875-023-01566-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-023-01566-9