Abstract
This study examined whether providing additional support to individuals with poor initial weight loss improves 12-week outcomes. Participants were randomized to a 12-week internet-delivered behavioral weight loss program (IBWL; n = 50) or the identical internet program plus the possibility of extra support (IBWL + ES; n = 50). IBWL + ES participants losing <2.3 % at Week 4 (early non-responders; n = 12) received one individual meeting and two follow-up phone calls with an interventionist, and were compared to IBWL ‘early non-responders’ who did not receive extra support (n = 21), and to ‘early responders’ in both treatment arms (i.e., 4-week weight loss ≥2.3 %; n = 59). IBWL + ES early non-responders had greater program adherence (p’s < 0.055) and lost twice as much weight (p = 0.036) compared to IBWL early non-responders. Program adherence did not differ between early responders and IBWL + ES early non-responders. However, 12-week weight loss was greater in the early responders compared to both early non-responder groups (p’s > 0.05). Providing additional intervention to early non-responders in an Internet program improves treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous research suggests that weight losses achieved in the first few months of a behavioral intervention are predictive of post-treatment and long-term success in both in-person and Internet-based weight loss programs (Elfhag & Rossner, 2010; Nackers et al., 2010; Unick et al., 2014, 2015a, b). Further, individuals who fail to achieve significant weight losses early in a program are less adherent and often become disengaged (Colombo et al., 2014; Unick et al., 2015b). Thus, the first few months of a treatment program may be an opportune time to identify individuals with poor initial weight loss (i.e., suggestive of an increased likelihood of poor long-term success) and provide additional intervention support.
This approach of intervening on early non-responders is consistent with the “stepped care” intervention model which posits that treatment should begin with a low intensity intervention that is increased in intensity if specific weight loss goals are not met at specified time points (Carels et al., 2005, 2009). Given that Internet-based programs are by nature minimally intensive, the Internet may be an ideal treatment medium for implementing a stepped care intervention model. However to date, the majority of studies which have utilized a stepped care approach have been within the context of face-to-face treatment programs (Carels et al., 2008; Jakicic et al., 2012). For example, the provision of more intensive behavioral treatment to those with lower than expected weight loss at 3 months did not improve weight loss outcomes within an in-person program (Carels et al., 2008; Jakicic et al., 2012). However, treatment outcomes were improved when individuals who lost <2.5 % of initial body weight following a 6-week, in person self-help program were provided with a weekly group-based behavioral intervention (Carels et al., 2009). This suggests that the timing of the intervention may be important and earlier identification of non-responders may be beneficial. Further, increasing the intensity of the intervention for early non-responders may be most helpful when implemented within the context of minimally intensive programs (e.g., Web-based programs). Applying a ‘stepped care’ approach within an Internet-based program may be more advantageous than applying such an approach within a more intensive face-to-face program, given that it may be less cost-effective to provide an intensive intervention to everyone, when some individuals can be successfully treated with a low-intensity intervention. Thus a ‘stepped care’ approach allows for the examination of whether a particular ‘step’ (i.e., treatment component) can effectively ‘rescue’ individuals with poor initial success. However early intervention for non-responders has not yet been tested within the context of an Internet-delivered weight loss program.
The current study randomized participants to a 12-week Internet-delivered behavioral weight loss program (IBWL) or the same Internet program plus the possibility of receiving extra support (IBWL + ES). The primary aim was to examine whether the provision of a brief period of interventionist support improved 12-week weight loss and program adherence among early non-responders (i.e., 4-week weight loss <2.3 %) in IBWL + ES, compared to early non-responders in IBWL who did not receive extra support. The secondary aims were to determine whether weight and adherence outcomes differed between early non-responders and early responders (i.e., 4-week weight loss ≥2.3 %), and to examine whether weight loss and program adherence in the IBWL + ES group as a whole differed from those randomized to IBWL. It was hypothesized that the provision of additional support to those with poor initial weight losses would improve treatment outcomes.
Methods
Participants
One-hundred individuals participated in this study. Participants were English speaking, 18–70 years of age, and had a BMI ≥25 kg/m2. Individuals were excluded from the study if they were pregnant, nursing, or had plans to become pregnant or relocate outside the area within the next 6 months. Further, individuals with serious medical conditions and those without Internet access were excluded. If an individual reported a medical condition that could interfere with safe participation in the program (e.g., diabetes controlled by insulin) physician consent was required. All study procedures were approved by The Miriam Hospital’s Institutional Review Board and informed consent was obtained from all participants included in this study.
Design
Participants were randomly assigned to IBWL (n = 50) or IBWL + ES (n = 50). Early non-responder was defined as losing <2.3 % at Week 4. This 2.3 % threshold was chosen because it is in line with previous reports which identified early non-responders as those achieving <2.0 % at Week 4 (Unick et al., 2014, 2015b) or <2.5 % at Week 6 (Carels et al., 2009). Further we wanted to optimize the percentage of individuals falling into the ‘early non-responder’ category, while protecting against high rates of false positives (i.e., providing extra support to individuals who didn’t really need it), particularly given that one of the purposes of a ‘stepped care’ intervention approach is to increase effectiveness while lowering cost. Given that for every 1 % increase in the weight loss threshold utilized, rates of false positives have been shown to double (Unick et al., 2014), this study focused on the subset of individuals least likely to be successfully treated and utilized a 2.3 % threshold. The primary outcome was 12 week weight loss and program adherence among early non-responders in IBWL + ES versus early non-responders in IBWL (i.e., early non-responders who were not offered extra support). Secondary outcomes compared early non-responders to early responders and examined overall weight loss and program adherence by intervention assignment.
Interventions
Internet-delivered behavioral weight loss program (IBWL)
Prior to the start of the 12-week online behavioral weight loss program, participants attended a 1.5 h in-person group session during which they received their randomization assignment, were given a weight loss goal of 1–2 pounds/week, were prescribed a daily calorie and fat gram goal based upon their starting weight (<200 lbs: 1200 kcal/day and 40 g of fat; 200–250 lbs: 1500 kcal/day and 50 g of fat; ≥250 lbs (1800 kcals/day and 60 g of fat), and were given a physical activity goal (gradually increase to 200 min/week of moderate-intensity exercise). During this session the importance of daily self-monitoring was emphasized and participants were provided with a Calorie King book and taught how to count calories. Further, participants were familiarized with all aspects of the study website.
The IBWL program website included a self-monitoring platform in which participants were instructed to track and record their daily weight, calorie, fat grams, and physical activity information. Based upon these self-report data, participants received weekly automated feedback related to their progress. In addition, participants were instructed to view a weekly, 10–15 min multimedia lesson modeled after the Look AHEAD Trial (Pi-Sunyer et al., 2007). Example lesson topics include: eating out at restaurants, increasing physical activity, dealing with environmental cues, problem solving, and healthy eating. The website also provided weekly recipes as well as useful tip sheets related to meal plans, prepackaged foods, negative thoughts, safe exercise, etc. This web-based program has been used in several studies which have been published previously (Leahey et al., 2014, 2015; Unick et al., 2015a).
Internet-delivered behavioral weight loss program plus extra support (IBWL + ES)
Participants randomized to IBWL + ES were provided with the identical IBWL program described above and were also told that there was a possibility that they would receive “extra support” in the form of 1 individual session and two, 10-min follow-up telephone calls. However, participants were not informed of the criteria that would be used to determine who would receive “extra support.” Only those individuals with a weight loss <2.3 % of their initial body weight at the end of Week 4 (i.e., early non-responders), were contacted via phone and given the opportunity to receive this additional support.
IBWL + ES participants eligible to receive extra support attended a 30–45 min in-person meeting with an interventionist during which their progress to date was reviewed, goals for the upcoming week were set, and an individualized meal plan was formulated for the upcoming week. These meal plans were developed to ensure that participants were not exceeding their daily calorie intake goal and relied heavily on pre-packaged food products (e.g., meal replacement products, frozen entrees, snacks in single portion bags, etc) and fruits and vegetables. Moreover, participants were provided with samples of meal replacement bars and shakes in order to help promote the adoption of prepackaged foods to assist with weight loss. Approximately 1 week following the in-person visit, the interventionist called the participant to review whether they met their goals and followed the meal plan. Barriers to following the meal plan were discussed, the meal plan was modified if necessary, and new goals were set for the upcoming week. The same procedure was implemented for the 2nd follow-up telephone call, which was completed one week later.
Outcome measures
Participants completed assessment visits at baseline and following the completion of the 12-week Internet program. At the baseline visit, basic demographic information was obtained, height was measured to the nearest millimeter using a stadiometer, and weight was measured to the nearest 0.1 kg using a digital scale. At the 12-week visit, weight was objectively measured and participants completed a Program Satisfaction Questionnaire, which queried participants on the usefulness of various aspects of the IBWL program. Further, those participants who received extra support completed an additional questionnaire assessing their satisfaction with the “extra support” component of the study. All participants were compensated $25 at the completion of their 12-week visit.
Percent weight loss
Percent weight loss at Week 12 was calculated using the baseline and 12-week assessment weights. Given that participants did not come to our center throughout the intervention period and the desire to keep the method of measurement similar across observations time points, percent weight loss at Week 4 was calculated using the participant’s self-reported baseline weight (logged on the study website on the first day of the program using their home scale) as well as their self-reported weight at the end of Week 4 (logged on the study website; n = 89). Individuals who did not enter a weight at the end of Week 4 (n = 11) were contacted by a member of the research staff in order to obtain this weight (n = 6 weights were obtained via phone and the remaining 5 participants were unable to be reached and were excluded from the analyses).
Adherence
Participant adherence was objectively assessed using data obtained from the study website and was quantified over the 12-week period by the percentage of video lessons viewed (out of a possible 12 videos) and by the number of days that calorie intake was reported on the study website (out of a possible 84 days). In order to examine the effect of the extra support on adherence outcomes, the percentage of video lessons viewed and percentage of days that calorie intake was monitored was also calculated for the time period before the extra support was offered (e.g., 3 out of 4 video lessons viewed during Weeks 1–4 = 75 %) and for after the extra support was offered (e.g., 5 out of 8 video lessons viewed during Weeks 5–12 = 63 %).
Statistical analyses
Baseline differences between treatment arms were examined using independent samples t-tests for continuous variables and Chi square tests for categorical variables. Participants in both treatment arms were further stratified into 1 of 2 categories based upon their 4-week weight change: (1) “early non-responders”—4-week weight loss <2.3 %, and (2) “early responders”—4-week weight loss ≥2.3 %. The primary hypothesis, comparing 12-week weight outcomes in IBWL early non-responders to early non-responders in IBWL + ES, was analyzed by an independent samples t-test. Further, a 2 × 2 (condition: IBWL early non-responders vs. IBWL + ES early non-responders x time: Week 4 and Week 12) repeated measures ANOVA was used to determine whether the pattern of weight change across the 12-week intervention differed between IBWL and IBWL + ES early non-responders. One-way ANCOVAs were used to examine whether IBWL and IBWL + ES early non-responders differed in adherence between Weeks 5–12, after controlling for adherence during Weeks 1–4. To address the first secondary aim, the two early responder groups (IBWL: n = 27, IBWL + ES: n = 32) were collapsed and compared to early non-responders in IBWL and early non-responders in IBWL + ES. A one-way ANOVA was used to determine whether the 3 groups differed in weight loss at Week 12 and several one-way ANCOVAs (adjusting for adherence during Weeks 1–4) with Bonferonni adjustments for multiple comparisons were used to examine whether the 3 groups differed in adherence between Weeks 5–12. To address the other secondary aim, independent samples t-tests were used to determine whether the IBWL + ES group as a whole differed from IBWL on 12-week weight loss, program adherence, and program satisfaction. All analyses were conducted using SPSS for Windows (Version 18, Chicago, IL) and statistical significance was set at p < 0.05.
Results
Participants
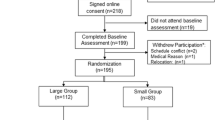
The flow of participants through the study is shown in Fig. 1. At baseline, participants weighed 90.0 ± 19.9 kg, had a mean BMI of 33.4 ± 6.6 kg/m2, and were 51.7 ± 10.3 years of age. Participants were predominately female (92 %), Caucasian (90 %) and college-educated (67 % with college degree or higher). There were no differences in any demographic variables between treatment arms (p’s > 0.40). Retention was high and similar between groups (p = 0.14), with 92 % of all participants having body weight measurements at Weeks 4 and 12.
Categorization of early responders and early non-responders
Participants were categorized based upon their 4-week weight loss; thus those missing 4-week weight data (n = 5) were excluded from the analyses (Fig. 1). Across both intervention arms, 64 % (n = 61) of participants were classified as “early responders” and the remaining 36 % (n = 34) were “early non-responders.” Early responders and early non-responders did not differ on any demographic variables examined (p’s > 0.18). The percentage of early non-responders in IBWL (n = 21; 44 %) was not statistically different from those in IBWL + ES (n = 13; 29 %; p = 0.14). Twelve out of the 13 (92 %) early non-responders in IBWL + ES received the extra support offered. Of note, the one participant who was eligible for extra support but did not come in for the intervention visit (stated she had family issues and time constraints), also did not report her 4-week weight on the study website (her weight was obtained via phone). Further, she did not use the website beyond Week 3 and was lost to follow-up. Therefore the following analyses which report on early non-responders in IBWL + ES include only those 12 participants who received the early intervention. All data presented below are from completer’s analyses, only including those 92 participants with weight data at Weeks 4 and 12.
Primary aim: comparison of IBWL and IBWL + ES early non-responders
Figure 2 shows the trajectory of weight change over the 12-week intervention for early non-responders in both treatment arms. At Week 4, weight losses did not differ between IBWL and IBWL + ES early non-responders (IBWL: −0.97 ± 0.90 %; IBWL + ES: −1.39 ± 1.1 %; p = 0.66); however there was a trend towards a significant time x condition interaction effect (p = 0.08), suggesting that the provision of extra support altered the trajectory of weight change from Weeks 4–12. At Week 12, weight losses in IBWL + ES early non-responders were twice as large as IBWL early non-responders who did not receive any additional intervention (−3.94 ± 2.02 % vs. −1.84 ± 2.92 %; p = 0.036; Cohen’s d = 0.84).
In terms of adherence, IBWL and IBWL + ES early non-responders did not differ in the percentage of video lessons viewed (IBWL: 75.0 ± 0.3 % vs. IBWL + ES: 81.3 ± 0.3 %; p = 0.57) or the percentage of days that calorie intake was logged on the study website (IBWL: 83.7 ± 0.3 % vs. IBWL + ES: 91.4 ± 0.2 %; p = 0.39) during Weeks 1–4. However in the time frame during and after the extra support was provided (i.e., Weeks 5–12), IBWL + ES participants who received the extra support viewed a greater percentage of video lessons (p = 0.017; Cohen’s d = 0.91) and logged calorie intake on a greater percentage of days (p = 0.055; Cohen’s d = 0.87), compared to IBWL early non-responders (Fig. 3).
Given that this was a preliminary investigation into whether the provision of extra support to early non-responders improves treatment outcomes, we also assessed the acceptability of the program. First, all 12 individuals who accepted the offer for extra support attended the in-person session and completed the two telephone calls with the interventionist. Further, on a 7-point Likert scale (1 = very dissatisfied, 7 = very satisfied), IBWL + ES early non-responders reported that they were significantly more satisfied with the program compared to IBWL early non-responders (5.4 ± 1.6 vs. 4.1 ± 1.7; p = 0.03). In addition, IBWL + ES early non-responders completed a separate questionnaire regarding the extra support received. Participants in IBWL + ES reported being highly satisfied (mean = 6.17 ± 1.1 on a scale ranging from 1 = ‘very dissatisfied’ to 7 = ‘very satisfied) with the individual visit and follow-up telephone calls and very glad (mean = 6.00 ± 1.5 on a scale ranging from 1 = ‘not at all glad’ to 7 = ‘very glad’) that we reached out to them and offered an individual visit. Participants also rated the usefulness of the one-on-one visit with the weight loss coach (5.75 ± 1.7) significantly higher than they rated the usefulness of the meal replacement products (4.58 ± 2.3) or following the meal replacement plan (4.33 ± 2.2; p’s < 0.05).
Secondary aim 1: comparison of early non-responders to early responders
A secondary aim was to examine whether the provision of extra support to early non-responders was sufficient enough to make them similar to early responders. Given that the two early responder groups received an identical intervention, had similar 4-week weight losses (IBWL: −3.84 ± 0.98 %; IBWL + ES: −3.82 ± 0.98 %; p > 0.05), and had similar adherence at Week 4, the two early responder groups were collapsed and compared to IBWL and IBWL + ES early non-responders. During Weeks 1–4, early responders viewed 96.2 ± 11.2 % of video lessons which was significantly greater than IBWL early non-responders (p < 0.001) and greater than IBWL + ES early non-responders (p = 0.058). Further, early responders logged their calorie intake on 95.0 ± 16.9 % of days during Weeks 1–4, which was not significantly different from IBWL + ES (p = 0.89) or IBWL (p = 0.082) early non-responders. During Weeks 5–12, early responders viewed 68.6 ± 33.2 % of all video lessons and logged calorie intake on 82.6 ± 28.3 % of possible days, which was significantly greater than IBWL early non-responders, after controlling for adherence during Weeks 1–4 (p’s < 0.02). Conversely, the provision of extra support to IBWL + ES early non-responders improved adherence such that it did not differ from that of early responders during Weeks 5–12 (p’s > 0.99). However at Week 12, early responders lost 6.4 ± 3.4 % of initial body weight which was significantly greater than IBWL early non-responders (p < 0.001) and IBWL + ES early non-responders (p = 0.048).
Secondary aim 2: comparison of all participants in IBWL versus IBWL + ES
An additional aim was to examine whether the provision of the extra support to early non-responders in the IBWL + ES improved weight loss and adherence in the treatment group as a whole, compared to the IBWL treatment condition. At Week 12, weight losses were similar between participants randomized to IBWL (−4.9 ± 4.2 %; p = 0.96) and IBWL + ES (−5.0 ± 3.4 %). The correlation between Week 4 and Week 12 weight loss was strong in IBWL (r = 0.71; p < 0.001), but not in IBWL + ES (r = 0.26; p = 0.09), suggesting that the provision of extra support broke the association between initial and post-treatment weight loss. Across the 12-week intervention period the treatment arms did not differ in the percentage of video lessons viewed (IBWL: 66.7 ± 32.9 % vs. IBWL + ES: 70.4 ± 25.0 %; p = 0.54) or the percentage of days that calorie intake was logged (IBWL: 75.6 ± 31.5 % vs. IBWL + ES: 82.9 ± 22.6 %; p = 0.20). Finally, IBWL + ES participants had slightly higher program satisfaction scores (5.60 ± 1.3) compared to IBWL (5.17 ± 1.6); however this was not statistically significant (p = 0.17).
Discussion
Previous trials have demonstrated that weight losses within the first 4 weeks of a weight loss intervention are associated with post-treatment and long-term weight loss outcomes in both face-to-face (Nackers et al., 2010; Unick et al., 2014, 2015b) and Internet programs (Unick et al., 2015a). However, this is the first study to utilize a stepped care intervention model to determine whether early non-responders in an Internet-based treatment program can be ‘rescued’ through the provision of extra support, thereby improving treatment outcomes. These preliminary findings indicate that early non-responders who received extra support adhered to the Internet program better, were more satisfied with the program they received, and lost twice as much weight at Week 12 compared to early non-responders in IBWL. On measures of adherence, the provision of extra support improved adherence to the point that it was no longer significantly different from early responders, although weight losses were still lower than that observed among early responders. Despite this study being only 12 weeks in duration, these findings provide preliminary evidence that early non-responders to an Internet-based weight loss intervention may be able to be ‘rescued’ when additional support is provided early within the intervention, thereby altering the weight change trajectory from pre- to post-treatment. This was supported by the strong correlation observed between 4- and 12-week weight loss in IBWL, but not in IBWL + ES.
Several findings from the current study confirm what has been reported previously. First, 37 % of participants lost <2.3 % at Week 4 and thus were classified as early non-responders. These results are in line with previous Internet and in-person interventions in which 27 % (Unick et al., 2015a) and 33 % (Unick et al., 2014) of participants respectively lost <2.0 % at Week 4. Second, this study confirmed that early weight loss is predictive of post-treatment weight loss within a standard Internet program (Unick et al., 2015a). This is evidenced by the high correlation observed between Week 4 and Week 12 weight loss within IBWL participants and the fact that IBWL early non-responders only lost 1.8 % at Week 12, compared to the 6.4 % weight loss achieved by early responders.
In addition to these confirmatory findings, this study adds to the existing literature by providing preliminary evidence that early rescue efforts can improve treatment outcomes within Internet programs. Given that Internet-based programs are by nature minimally intensive, the Internet may be an ideal treatment medium for employing a stepped-care intervention model. Stepped-care approaches start with a low intensity intervention (e.g., an Internet program) and only increase the intensity of the intervention for those individuals not meeting specific study goals (Brownell, 1986; Carels et al., 2009), as was the case in the IBWL + ES treatment arm. Findings from the current study suggest that providing a single 30–45 min face-to-face session and two, 10-min follow-up telephone calls to IBWL + ES participants with a 4-week weight loss <2.3 % altered the weight change and adherence trajectories from Weeks 5 to 12, compared to those not receiving this extra support. However, future studies should examine whether altered trajectories observed in the current study continue beyond 12 weeks and whether weight losses of early non-responders receiving extra support eventually coincide with that of early responders.
Given the small number of early non-responders (n = 12) who received additional support, findings from this study should be interpreted with caution and replicated using larger sample sizes. Future studies should also begin to investigate the optimal timing, intensity, and type of intervention which maximizes weight loss for early non-responders within the context of these stepped-care intervention models. Further, additional research is needed to determine what threshold is most cost-effective for identifying and intervening upon early non-responders. Based upon the current findings, specifically the improved weight loss and adherence observed among IBWL + ES early non-responders, it is hypothesized that this type of tailored treatment approach could lead to improved long-term obesity treatment outcomes in Web-based interventions.
While the preliminary findings from the current study are promising, it should be noted that the provision of a brief period of interventionist support for early non-responders did not result in significant differences in weight or adherence metrics at Week 12 between IBWL + ES as a whole and IBWL. There are several possibilities for this finding. First, this brief 3-week ‘rescue’ intervention began at Week 5 or 6 (depending upon the participant’s schedule); thus only allowing participants 6 weeks to ‘catch up’ and alter their weight change trajectory within this short, 12-week intervention. Thus, the additional 2 % weight loss which resulted from the extra support was quite significant given this shortened time frame. Second, only about one quarter of IBWL + ES study participants fell within the early non-responder category. Thus, the intervention only targeted a small proportion of participants, making it difficult to alter overall treatment outcomes by randomization arm in a study with a relatively small sample size and short study duration. Future studies will require significantly larger sample sizes in order to better understand the effect of early rescue on post-treatment and longer-term outcomes, as this preliminary investigation did not include an observational follow-up period post-treatment. Finally, our study sample was predominately Caucasian and female and thus future studies should investigate whether these findings generalize to more diverse populations.
In conclusion, this study provides preliminary evidence that the provision of extra support to individuals with poor initial weight loss improves program satisfaction, program adherence and 12-week weight loss within an Internet-based program, compared to early non-responders not receiving extra support. This suggests that individuals at risk of achieving little weight loss following an Internet program may be able to be ‘rescued’ if intervened upon early. Future studies with longer-term follow-up periods are needed to examine whether these improvements are sustained post-treatment.
References
Brownell, K. D. (1986). Public health approaches to obesity and its management. Annual Review of Public Health, 7, 521–533.
Carels, R. A., Darby, L., Cacciapaglia, H. M., Douglass, O. M., Harper, J., & Kaplar, M. E. (2005). Applying a stepped-care approach to the treatment of obesity. Journal of Psychosomatic Research, 59, 375–383.
Carels, R. A., Wott, C. B., Young, K. M., Gumble, A., Darby, L. A., & Oehlhof, M. W. (2009). Successful weight loss with self-help: A stepped-care approach. Journal of Behavioral Medicine, 32, 503–509.
Carels, R. A., Young, K. M., Coit, C. B., Darby, L. A., Clayton, A. M., & Spencer, A. C. (2008). The failure of therapist assistance and stepped-care to improve weight loss outcomes. Obesity, 16, 1460–1462.
Colombo, O., Ferretti, V. V., Ferraris, C., Trentani, C., Vinai, P., & Villani, S. (2014). Is drop-out from obesity treatment a predictable and preventable event? Nutrition Journal, 13, 13.
Elfhag, K., & Rossner, S. (2010). Initial weight loss is the best predictor for success in obesity treatment and sociodemographic liabilities increase risk for drop-out. Patient Education and Counseling, 79, 361–366.
Jakicic, J. M., Tate, D. F., Lang, W., Davis, K. K., Polzien, K., & Rickman, A. D. (2012). Effect of a stepped-care intervention approach on weight loss in adults: A randomized clinical trial. JAMA, 307, 2617–2626.
Leahey, T. M., Subak, L. L., Fava, J., Schembri, M., Thomas, G., & Xu, X. (2015). Benefits of adding small financial incentives or optional group meetings to a web-based statewide obesity initiative. Obesity, 23, 70–76.
Leahey, T. M., Thomas, G., Fava, J. L., Subak, L. L., Schembri, M., & Krupel, K. (2014). Adding evidence-based behavioral weight loss strategies to a statewide wellness campaign: A randomized clinical trial. American Journal of Public Health, 104, 1300–1306.
Nackers, L. M., Ross, K. M., & Perri, M. G. (2010). The association between rate of initial weight loss and long-term success in obesity treatment: Does slow and steady win the race? International Journal of Behavioral Medicine, 17, 161–167.
Pi-Sunyer, X., Blackburn, G., Brancati, F. L., Bray, G. A., Bright, R., & Clark, J. M. (2007). Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: One-year results of the look AHEAD trial. Diabetes Care, 30, 1374–1383.
Unick, J. L., Hogan, P. E., Neiberg, R. H., Cheskin, L. J., Dutton, G. R., & Evans-Hudnall, G. (2014). Evaluation of early weight loss thresholds for identifying nonresponders to an intensive lifestyle intervention. Obesity, 22, 1608–1616.
Unick, J. L., Leahey, T., Kent, K., & Wing, R. R. (2015a). Examination of whether early weight loss predicts 1-year weight loss among those enrolled in an internet-based weight loss program. International Journal of Obesity, 39(10), 1558–1560.
Unick, J. L., Neiberg, R. H., Hogan, P. E., Cheskin, L. J., Dutton, G. R., & Jeffery, R. (2015b). Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity, 23, 1353–1356.
Acknowledgments
The authors would like to acknowledge Abby Moylan and Lucie Rice with all of their assistance on this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tricia M. Leahey is the chief scientist at WayBetter Inc., Jessica L. Unick, Leah Dorfman and Rena R. Wing have declared that they have no conflict of interest.
Human and animal rights and Informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Unick, J.L., Dorfman, L., Leahey, T.M. et al. A preliminary investigation into whether early intervention can improve weight loss among those initially non-responsive to an internet-based behavioral program. J Behav Med 39, 254–261 (2016). https://doi.org/10.1007/s10865-015-9691-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-015-9691-9