Abstract
This meta-analysis synthesizes studies of brief interventions (BIs) that targeted alcohol consumption and reported both alcohol and tobacco outcomes. It examines whether BIs reduce alcohol and tobacco use for adolescents and young adults among interventions that (1) directly targeted tobacco and alcohol use, or (2) did not target tobacco use but measured it as a secondary outcome. Multiple databases and grey literature sources were searched (1980–2012) resulting in the identification of 18 randomized or controlled quasi-experimental studies (5949 participants). Analyses were conducted using random effects inverse-variance weighted three-level models. BIs were associated with a significant reduction in alcohol consumption relative to control groups [\({{\bar{\text{g}}}}\) = 0.11, 95 % CI (0.04, 0.17)] but not with a significant decrease in tobacco use [\({{\bar{\text{g}}}}\) = 0.07, 95 % CI (−0.01, 0.16)]. Directly addressing tobacco was not a significant moderator affecting tobacco use outcomes. Post-hoc exploratory analysis revealed potential questions to address with future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are currently a range of tobacco use prevention efforts worldwide, including international treaties (World Health Organization, 2014), international and national campaigns (American Cancer Society, 2014), laws regulating the marketing and sales of tobacco products, and interventions delivered in healthcare, workplace, and school settings (U.S. Department of Health and Human Services, 2012). Despite these efforts, youth worldwide initiate smoking and use tobacco at alarming rates (Ng et al., 2012; Richardson et al., 2014), which is troubling given that earlier initiation of smoking often leads to later tobacco dependence (Nelson et al., 2008; Van De Ven et al., 2010; Riggs et al., 2007). For example, research has demonstrated that between 17 and 51 % of adolescent tobacco users progress to nicotine dependence by young adulthood (Riggs et al., 2007; Van de Ven et al., 2010). As nicotine dependence is difficult to treat and often requires sustained intervention (Steinberg et al., 2008), prevention of initiation or continued tobacco use among adolescents and young adults remains a pressing public health issue.
Research has also demonstrated the high prevalence of comorbid use of alcohol and tobacco over time (Jackson et al., 2002, 2005). In the 2012 National Survey of Drug Use and Health, approximately 53 % of adolescent heavy drinkers also reported using cigarettes [Substance Abuse and Mental Health Services Administration (SAMHSA) 2013]. Given the common comorbidity of alcohol and tobacco use, it has been hypothesized that their use may be the result of similar motivations, such as emotion regulation (Lippke et al., 2012), or due to similar psychosocial influences such as family or peer modeling and interactions (Chuang et al., 2009; Kobus, 2003). Thus, it may be advantageous for interventions to target both substances simultaneously.
Brief interventions (BIs), defined broadly as those delivered in a relatively circumscribed time, may be one important tool to prevent multiple risk behaviors. BIs have been used in diverse prevention and treatment settings (Baer et al., 2001; Eaton et al., 2012; Glasgow et al., 2000; Gmel et al., 2012) and accumulating evidence suggests they effectively reduce substance use among adolescents, young adults, and adults (Bien et al., 1993; Kaner et al., 2007; Moyer et al., 2002; Schubiner et al., 1998; Tait & Hulse, 2003; Tanner-Smith et al., 2015; Vasilaki et al., 2006). Interventions targeting two or more health behaviors simultaneously have also gained support in recent years as practitioners, funders, and policy-makers have sought to maximize existing resources (Prochaska et al., 2008). Indeed, recent research has explored whether some risk (or health) behaviors cluster together (Lippke et al., 2012), and if so, whether comparable behaviors within the clusters and/or the clusters themselves can successfully be addressed simultaneously. Proponents of multiple health behavior change interventions have drawn on the theory of triadic influence (Flay & Petraitis, 1994) and transfer (Barnett & Ceci, 2002). They posit that if factors leading to the behaviors are similar, and if the knowledge and skills needed to change the behavior are similar, then multiple behaviors could be successfully addressed through targeted programming (Lippke et al., 2012). Thus, given the association and similarities between alcohol and tobacco use, a generalization of intervention effects may occur when an intervention targets only one of these behaviors (SAMHSA, 2013).
A substantial amount of resources have been dedicated to address tobacco use among adolescents and young adults. It is therefore worthwhile to explore the potential effectiveness of BIs in directly addressing tobacco use in conjunction with related risk behaviors such as alcohol use; or if BIs primarily focused on alcohol consumption can have generalized (secondary) effects on tobacco use. Although prior literature syntheses have explored the effectiveness of interventions that directly address tobacco use among youth (Bryant et al., 2011; Hale et al., 2014; Hwang et al., 2004; Jensen et al., 2011; Suls et al., 2012; Sussman et al., 2006); to date it seems that only one meta-analysis has examined whether brief alcohol interventions have secondary effects on tobacco outcomes (McCambridge & Jenkins, 2008). In that meta-analysis, the authors found no significant beneficial effects of brief alcohol interventions on secondary tobacco outcomes; however, that study did not include adolescents (McCambridge & Jenkins, 2008) and thus it is unclear whether those findings can be generalized to youth populations.
Therefore, the primary objective of the present meta-analysis was to examine whether BIs that target alcohol consumption also have beneficial effects on tobacco use for adolescents and young adults among studies that (1) directly targeted tobacco use along with alcohol use, or (2) did not directly target tobacco use but measured post-intervention tobacco use as a secondary outcome. Given the potential for generalized intervention effects, it was hypothesized that although all BIs might be successful in reducing tobacco use, studies involving interventions that directly targeted tobacco use would have a greater effect on tobacco outcomes relative to studies that did not target tobacco use but nonetheless measured it as a secondary outcome.
Additionally, this analysis explores potential differences in intervention effects for adolescents and young adults. Initial use of tobacco often occurs in adolescence and studies have found that by the age of 18, approximately 82 % of those sampled have at least tried a cigarette (National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health, 2012). Studies have also demonstrated an uptake in tobacco use when youth enter college (Meier et al., 2015; Rigotti et al., 2000); therefore, young adults may have more opportunities than adolescents to initiate tobacco use in multiple settings. Given the established developmental trajectory from tobacco experimentation to frequent use (Nelson et al., 2008; Riggs et al., 2007; Van De Ven et al., 2010), young adults are also more likely than adolescents to be dependent users and smoking behaviors might be more difficult to change among this age group. Thus, a secondary aim of the current meta-analysis was to explore whether there were differences between adolescents and young adults in overall intervention effects.
Methods
Eligibility criteria
This meta-analysis includes a subset of studies that were collected for a parent meta-analysis summarizing the effectiveness of brief alcohol interventions (BAIs) for non-treatment-seeking adolescents and young adults (see Tanner-Smith & Lipsey, 2015 for full description). The larger meta-analysis focused on diverse types of BAIs; whereas the meta-analysis reported here focuses on a subset of outcomes identified through the original search, i.e., brief interventions (BIs) that reported both alcohol and tobacco use outcomes.
Studies were included in the larger review if they met the following inclusion criteria: (1) evaluated brief alcohol interventions, i.e. interventions that were primarily designed to reduce alcohol consumption and were delivered in <5 h of total contact time and <4 weeks between the first and last session; (2) used a randomized or controlled quasi-experimental research design that included a comparison condition of no treatment, wait-list control, or some form of treatment as usual; (3) provided enough information to calculate pretest and post-intervention effect sizes indexing differences between groups on relevant outcomes; (4) focused on youth age 11–25, or on samples of undergraduate college students no older than age 30; (5) assessed the effects on at least one alcohol use or alcohol related problem outcome, such as frequency of drinking, frequency of binge drinking, or driving under the influence of alcohol; (6) were conducted in 1980 or later. The year 1980 was chosen to include programs relevant to current intervention practices. There were no restrictions based on the baseline risk level of the sample; that is, participants could be described as current or non-users of alcohol or tobacco. There were no geographic or language limitations on eligibility.
The meta-analysis reported here included only those studies that (1) met all above eligibility criteria and reported effects on at least one tobacco use outcome; or (2) met all above eligibility criteria, were designed to reduce tobacco use in addition to alcohol consumption, and reported at least one alcohol and one tobacco use outcome. Tobacco use outcomes included behaviors such as the number of days cigarettes were smoked or the number of cigarettes smoked for a selected time period.
Information sources and search strategy
Using a comprehensive search strategy, published and unpublished studies that met the above criteria were identified for inclusion in the parent analysis. After confirming eligibility for review in the parent analysis, full-text articles were then re-reviewed for inclusion in this sub-analysis. Thus, for this sub-analysis, a new search was not conducted; only articles eligible for the parent analysis were reviewed for inclusion in this analysis. In the search for articles for the parent analysis, the following electronic bibliographic databases were searched, current through December 31, 2012: ERIC, International Bibliography of the Social Sciences, PsycARTICLES, PsycINFO, Social Services Abstracts, Sociological Abstracts, PubMed, CINAHL, Dissertation Abstracts International, Clinical Trials Register, NIH RePORTER, and WorldWideScience.org. Search terms were adapted to be appropriate for each database, but generally used three blocks of terms that described (1) the intervention, (2) alcohol outcomes, and (3) research design (for a search strategy example that includes key search terms, see Online Resource 1). In addition, websites for unpublished literature were searched, bibliographies of all screened and eligible studies and of prior narrative reviews and meta-analysis were reviewed, and hand searches of journals were conducted (list available from authors).
Study selection and data collection process
The project’s Principle Investigator (second author of this article) supervised the multi-step eligibility screening and coding process. A team of six research assistants first screened all identified abstracts and titles to eliminate clearly irrelevant study reports based on our inclusion and exclusion criteria. All six researchers initially screened 500 randomly selected abstracts/titles and discussed disagreements until consensus was reached. One team member screened the remaining abstracts/titles, with the second author reviewing all screening decisions. Any disagreements were discussed until consensus was reached. The same team then used the same procedure to screen full text reports and make final eligibility decisions. After all eligible reports were collected coders participated in several weeks of coding training led by the project’s Principle Investigator. The same research team then coded information from the eligible study reports using a standardized coding protocol. The items collected for this report are described below. Weekly meetings were held throughout coding, and the project’s Principle Investigator checked all coding and resolved coding discrepancies via consensus. If primary studies did not include the information needed to estimate effect sizes, primary study authors were contacted. Missing effect sizes were not imputed when these data could not be obtained.
Data items
Data were extracted from primary study reports on the following variables: participant age (years), percent male, percent White; average attrition; delivery format (one-on-one with practitioner/individual, self-administered); focal modality [motivational enhancement therapy (MET), psycho educational therapy (PET), personalized feedback only]; intervention duration (minutes); time between intervention end and posttest (weeks); intervention location (site; country); and study design [RCT or quasi-experimental; intent-to-treat (ITT) analysis (yes/no); program monitoring (yes/no)].
Summary measures
To properly synthesize effect sizes across all studies and permit comparison across outcomes, all effect sizes were transformed to the same metric (Lipsey & Wilson, 2001): the standardized mean difference (SMD). The SMD effect size metric was chosen because most primary studies reported outcomes via differences in group means on some continuous scale, and authors used a variety of measurement scales. Because some outcomes were binary (e.g., any use versus abstinence), the Cox transformation was used to convert log odds ratio effect sizes into SMD effect sizes (Sánchez-Meca et al., 2003). All effect sizes were coded so that positive values represent beneficial intervention effects (e.g., reduced tobacco use, higher abstinence). After SMD effect sizes were calculated for each study they were adjusted to correct for potential bias introduced by small samples resulting in Hedges’ g effect sizes (Hedges, 1981). Additionally, if authors did not properly account for cluster design in their analyses, standard errors of effect sizes in cluster-randomized trials were inflated to avoid potential bias in estimation of the study specific and overall mean effect sizes. This was done by multiplying the standard error of the effect size by the square root of the design effect (Higgins et al., 2008). When the intraclass correlation coefficient (ICC) required for the formula was missing, the estimated average ICC (0.13) for all alcohol consumption outcomes across all studies, was used (see Tanner-Smith & Lipsey, 2015).
Synthesis of results
Whereas a fixed effect meta-analysis model only accounts for sampling variability within studies, a random effects model assumes that there is both sampling variability within studies and study-specific differences between population effect sizes besides sampling error (Lipsey & Wilson, 2001). Given the diversity of interventions included in the current meta-analysis, we expected some degree of heterogeneity across studies and therefore conducted all analyses using a random effects statistical model. All analyses were weighted using inverse variance weights, such that each study was weighted by an estimate of its precision (Lipsey & Wilson, 2001).
Because the majority of studies reported multiple measures of alcohol and tobacco use outcomes at multiple follow-up waves, to handle the statistically dependent effect sizes three-level models were used (Cheung, 2013, 2014) in the R statistical environment (i386, 2.15.3). Three-level models can be used in meta-analyses to handle statistically dependent effect sizes originating from the same primary study. This method is used in place of, for example, averaging effect sizes into one mean effect size per study or selecting one effect size per study, both of which result in loss of information or assume homogeneity within studies. In the current meta-analysis, the first level of the three-level model represented participants in the primary studies, the second level represented the multiple effect sizes per study, and the third level represented each study. Using this multi-level approach, heterogeneity is partitioned at level two (indicating within-study variability) and level three (indicating between study variability). Following this analysis, the primary moderator, whether or not the intervention directly targeted tobacco, was tested in a multilevel meta-regression model. Further exploratory analysis was then conducted through graphical inspection of included studies.
Addressing study quality and risk of bias across studies
Sensitivity analysis to assess study quality was also conducted using multilevel meta-regression models that explored the impact of attrition, presence of intervention implementation monitoring, and whether intent-to-treat analysis was conducted. These specific variables were chosen given their significance in the parent analysis (see Tanner-Smith & Lipsey, 2015) and their correlation with the outcomes of interest in this analysis. The potential of publication bias, where studies with null or negative findings are systematically left out of the published literature (Rothstein et al., 2005), was examined through visual inspection of separate funnel plots of alcohol and tobacco use effect sizes and through three-level meta-regression analysis where tobacco use effect sizes were regressed on their standard errors.
Results
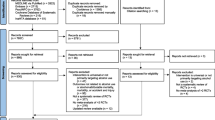
A total of 7593 reports were identified in the literature search: 2467 were duplicates and removed, 2641 were screened as ineligible at the abstract phase, and 1 report could not be located (Fig. 1). Of the 2484 full-text articles retrieved, 2444 were deemed ineligible for the analysis reported in the current meta-analysis. Thus, this meta-analysis included results from 18 unique study samples (5949 participants) reported in 40 documents (Table 1). The majority of studies were published in peer-reviewed journals, with the exception of two dissertations.
On average, the majority of intervention participants were male (61 %, SD = 0.23) and just under half were white (43 %, SD = 0.24; k = 14). Eleven studies (13 intervention groups) enrolled adolescents and 7 studies (9 intervention groups) enrolled young adults. All but 1 study used an RCT design, and 11 studies (61 %) explicitly reported conducting intent-to-treat analysis. Ten studies (56 %) were conducted in the United States, and the rest were located in England (22 %), Switzerland (17 %), and Brazil (6 %). The majority of interventions were implemented in an educational setting (High school, k = 10; University, k = 4) with the rest conducted in a health clinic (k = 1) or at a military recruitment center (k = 3). Almost all interventions were delivered one-on-one with a practitioner (k = 16) and the rest utilized a mixed-delivery format with self-administration and one-on-one delivery or self-administration via computer. Studies reported follow-up outcomes from 1 to 12 months post-intervention: within this range, only 5 studies (28 %) reported outcomes after 6 months. Average attrition across the interventions was 10.7 % (SD = 0.10, range 0–0.40 %).
In four studies two intervention groups were utilized: thus the analysis included 22 unique intervention groups. Tobacco use was directly targeted in at least one intervention group in 12 (67 %) of the 18 included studies, i.e., in 14 of the 22 intervention groups. In the remaining intervention groups tobacco use was not directly targeted but was nonetheless measured and reported as a secondary outcome. Finally, the majority (82 %; n = 18) of intervention groups utilized motivational enhancement therapy or motivational interviewing techniques, three used psycho educational therapy (PET), and one delivered personalized feedback via computer.
Effectiveness of brief interventions
In the three-level random-effects meta-analysis synthesizing results across all 18 included studies, brief interventions were effective in reducing alcohol consumption among youth [\({{\bar{g}}}\) = 0.11, 95 % CI (0.04, 0.17); τ 2(2) = 0.00; τ 2(3) = 0.01; Q = 121.3, p = 0.002; I 2(2) = 0 %; I 2(3) = 43 %]. There was no evidence, however, that the brief interventions were associated with tobacco use in these same studies [\({{\bar{g}}}\) = 0.07, 95 % CI (−0.01, 0.16); τ 2(2) = 0.0; τ 2(3) = 0.02; Q = 72.46, p = 0.013; I 2(2) = 0 %; I 2(3) = 57 %]. Thus, although brief interventions did significantly reduce the level of alcohol consumption among adolescents and young adults, they did not simultaneously reduce the level of tobacco use. Additionally, tobacco use effect sizes were statistically homogenous within studies; that is, if a study reported multiple tobacco outcomes, the effects were relatively statistically similar to each other. However, there was a small, significant degree of heterogeneity between studies on tobacco outcomes (τ 2(3) = 0.02), with the I 2(3) indicating that 57 % of that heterogeneity is due to true heterogeneity and not chance. Thus, differences in tobacco outcomes could be due to factors that vary across studies.
A scatter plot was generated to represent the distribution of tobacco and alcohol effect sizes of included studies (Fig. 2). In this figure, each horizontal line represents a unique study. A weighted mean effect size was calculated so that there was only one tobacco (black circle, n = 18) and one alcohol (gray circle, n = 18) effect size per study. Each effect size was weighted by its appropriate relative contribution to the overall mean effect: the size of each bubble in the scatter plot represents this weight. Bubbles to the right of the dotted line (x = 0) indicate interventions with a positive effect (reduced alcohol or tobacco use) and bubbles to the left indicate negative intervention effects (increased alcohol or tobacco use). This approach differs from the statistical approach used in the analysis by using a weighted average of effect sizes per study to aid in the visual interpretation of the results (see Appendix for a complete list of all effect sizes). It was not appropriate to use a traditional forest plot given the multilevel nature of these data. However, like the forest plot, the bubble plot in Fig. 2 permits comparison of the average mean effect per study by outcome (i.e., alcohol or tobacco), and shows each study’s relative contribution to the overall mean effect for that outcome. For example, as demonstrated by the tobacco effect sizes, the smallest studies contributed the least weight to the overall mean effect size, but were more likely to have positive effects on tobacco use than the larger studies. This plot also indicates that alcohol effect sizes were typically positive (i.e., right of the null line) and favoring the intervention group, compared to the tobacco effect sizes.
Moderators of intervention effectiveness
As highlighted above, there was no within-study variability for the alcohol or tobacco effect sizes. However, given the significant amount of variability between studies for the tobacco use effect sizes, the primary a priori moderator of interest was tested: whether an intervention program directly targeted tobacco versus interventions that did not directly target tobacco use (i.e., tobacco was measured as a secondary untargeted outcome). Whether or not the program directly targeted tobacco was not a significant predictor of tobacco outcomes [b = 0.02, 95 % CI (−0.14, 0.18)]. Thus, these results provided no evidence that programs that directly targeted tobacco produced different effects than those that measured it as a secondary untargeted outcome.
Due to the amount of variability between studies as evidenced by τ 2(3) (0.02), prior to any further moderator analyses the data were explored graphically to visualize the distribution of tobacco effects depending on the intervention focus and target population. The horizontal boxplots (Fig. 3) illustrate the distribution of all tobacco effect sizes (n = 49): in this figure the effect sizes were categorized by (1) whether or not the program directly targeted tobacco and (2) participant group [adolescent (high school student or maximum sample range younger than 18 years) and young adult (university student or minimum sample range older than 18 years)].
There was more variability in the tobacco effect sizes among interventions that enrolled adolescents than interventions that included young adults (Fig. 3). This finding is supported when three-level random effects models are run separately for adolescents [\({{\bar{g}}}\) = 0.12, 95 % CI (−0.00, 0.24); τ 2(2) = 0.00; τ 2(3) = 0.03; Q = 55.37, p = 0.004] and young adults [\({{\bar{g}}}\) = 0.01, 95 % CI (−0.09, 0.10); τ 2(2) = 0.00; τ 2(3) = 0.01; Q = 14.11, p = 0.591]. Although neither model yields a significant mean effect size, there is a greater degree of true heterogeneity between studies targeting adolescents (I 2(3) = 61 %) than young adults (I 2(3) = 31 %). Thus, programs targeting adolescents might vary more on some element, which affects their outcomes. For example, studies with adolescents could have more diverse samples with different risk levels compared to interventions that enrolled young adults. As a result, there may be some untapped opportunities for intervening with adolescents through BIs that target alcohol and/or tobacco use. Although the median values shown in Fig. 3 suggest a possible larger effect of tobacco-focused interventions for adolescents versus young adults, there was no evidence of a significant difference between groups when directly tested with a three-level meta-regression model [b = 0.18, 95 % CI (−0.05, 0.42)]. This finding could be due to low statistical power, however, as this test was a comparison between seven adolescent studies and four young adult studies.
Study quality assessment and risk of bias
A series of sensitivity analyses was conducted to examine the effect of primary study quality on the meta-analysis results (Table 2). These analyses specifically examined whether study quality indicators, such as implementation monitoring, average attrition, and whether or not the authors conducted intent-to-treat (ITT) analysis were associated with intervention effects. Results from multi-level bivariate meta-regression models indicated that the use of ITT analyses, which is a more rigorous analytical method than treatment-on-the-treated (TOT) analysis, was a significant predictor of tobacco use [b = −0.19, 95 % CI (−0.34, −0.03)]. Namely, interventions in studies where ITT analysis was utilized reported null outcomes in reducing tobacco use compared to positive intervention outcomes in studies where TOT analysis was conducted [\({{\bar{g}}}\) = −0.02, 95 % CI (−0.13, 0.09) and \({{\bar{g}}}\) = 0.17, 95 % CI (0.05, 0.28), respectively]. This suggests that studies using TOT analysis were potentially upwardly biased in their estimate of intervention effects. Average attrition was also a significant predictor of tobacco use outcomes [b = 1.03, 95 % CI (0.00, 2.07)] indicating that studies with greater attrition also reported an increased effect on tobacco use compared to studies with lower attrition. This indicates that interventions with higher attrition may have suffered from selection bias, where those motivated to change remained in the intervention and those not as interested dropped out. Finally, monitoring of the intervention was not a significant predictor of intervention effectiveness on tobacco use outcomes [b = 0.07, 95 % CI (−0.14, 0.27)]. In sum, sensitivity analyses indicate that studies that use TOT analysis and studies with higher attrition may overestimate the positive effects of their intervention on youth’s tobacco use outcomes.
To assess the possibility of publication bias, separate funnel plots for tobacco and alcohol outcomes were visually inspected (not shown, available upon request). For both outcomes, the funnel plots were slightly asymmetric, with a large number of studies clustered toward the top of the funnel and almost no studies towards the bottom portions of either side of the funnel. This suggests a general lack of small sample studies with either positive or negative effects and could indicate publication bias. A three-level meta-regression model was used to regress the tobacco effect sizes on their standard errors to further examine potential existence of publication bias. Results from this analysis did not provide evidence of an association between the effect sizes and their standard errors [b = 0.63, 95 % CI (−0.24, 1.51)], which offered some reassurance against small study bias. Nonetheless, despite the systematic search process used to identify eligible studies, only 2 non-peer reviewed studies were identified. Thus, while there is no clear indication of publication or small study bias in this sample of studies, it is possible there is bias in the publication process favoring large-scale studies.
Discussion
Primary results
This meta-analysis of 18 studies illustrates that brief interventions targeting alcohol consumption do reduce alcohol use among adolescents and young adults but do not appear to have similar beneficial effects on tobacco use. This finding was consistent regardless of whether tobacco was directly targeted by the intervention, or was measured as a secondary (untargeted) outcome. Although a previous review found support for the effectiveness of interventions targeting multiple risk behaviors among adolescents, including interventions that simultaneously targeted alcohol consumption, aggression, illicit drug use, sexual risk behaviors, and/or tobacco use (Hale et al., 2014), findings from this review stand in contrast. Results from the current review provide no evidence of tobacco use reduction as either a primary outcome in brief multi-target interventions or as a secondary outcome in brief alcohol interventions among adolescents and young adults. There are two potential explanations for these different findings. First, Hale et al. (2014) included a range of interventions that lasted from 4 to 140 sessions, while we focused only on BIs shorter than 5 h. Second, the previous review primarily addressed multi health behavior change interventions whereas ours included interventions that focused solely on alcohol but reported secondary tobacco outcomes. Thus, longer interventions targeting multiple risk behaviors among adolescents may indeed be effective, but results from the current meta-analysis provide no evidence that brief alcohol interventions are effective in simultaneously reducing tobacco use among youth.
Exploratory analyses did suggest potential differences between BI outcomes by target population, such that there may be more variability in tobacco outcomes among adolescents when compared to young adults. However, some participants may have enrolled in these studies before using tobacco and others may already have engaged in tobacco use. Therefore, the interventions may have served to prevent smoking in some participants and to reduce smoking in other participants. In the United States, approximately 86 % of adults reported initiating smoking by age 18, compared to only 37 % initiating by age 14 (National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health, 2012). Therefore, in the studies in this analysis, it is likely that compared to young adults who might already be using or dependent on tobacco, enrolled adolescents were more likely to be abstainers or experimenters upon study entry. Unfortunately, we do not have sufficient baseline data from the studies included in the meta-analysis to explore how this might affect the observed intervention effects. Research also suggests that younger participants are more likely to successfully quit using tobacco than older participants (Abrantes et al., 2009); thus, as demonstrated by our exploratory analysis, there may be greater potential impact on tobacco use among younger adolescents, particularly for interventions that target both alcohol and tobacco. Given the exploratory nature of our post hoc analysis, differences by age should be directly tested in future primary research.
This study’s findings are similar to previous meta-analyses in which tobacco-focused programs had smaller effects than interventions targeting other substance use outcomes (Jensen et al., 2011) or where alcohol-focused interventions do not have any secondary effects on tobacco use (McCambridge & Jenkins, 2008). One possible explanation for these findings is that BIs are simply not intense enough to produce measurable effects on tobacco use when alcohol consumption is addressed simultaneously. In this study, interventions ranged from 2.5 min (administered through a leaflet) to 75 min (including a parent booster session). Perhaps the attempt to target multiple risk behaviors in one short intervention mitigates potential effects on the use of highly addictive substances, such as tobacco products. Prior research has suggested that only small proportions of youth seeking cessation are successful and that sustained interventions to address tobacco dependence are necessary (Abrantes et al., 2009). Research has also demonstrated that brief alcohol interventions are effective for simultaneously targeting other substance use, such as marijuana, yet only when these are directly targeted and not measured as secondary outcomes (Tanner-Smith et al., 2015). Thus, a lack of secondary effects in this analysis may be because tobacco behavior should be handled differently from other substances.
Limitations
Caution must be exercised in interpreting these findings. Although BIs were effective only in reducing alcohol consumption and not in reducing tobacco use outcomes, it is important to recognize that this synthesis was not from the entire body of tobacco-related brief interventions, but a subset of that literature, that is interventions that also and sometimes primarily addressed, alcohol consumption. Reporting biases may exist in the literature, especially between the studies that chose to report secondary outcomes of their intervention and those that did not. Further, despite the systematic and rigorous search approach, the few non-peer reviewed studies identified in the search may point to small study bias in this field as other authors have suggested (Tanner-Smith & Polanin, 2014).
Additionally, although the majority of studies used MET/MI intervention approaches, which focus on enhancing participants’ motivations to self-evaluate and self-regulate their behavior, we have limited information from primary study reports on how these approaches were modified to address the different developmental needs of adolescents and young adults. This analysis may have also missed beneficial delayed effects due to the short follow-up periods available in the included studies. Namely, any delayed long-term effects among adolescents that could appear as late as a few years post-intervention (Hale et al., 2014) might not be apparent in this review because the follow-up period ended at 6 months post-intervention in over 70 % of the included studies. Thus, future research should attempt to collect longitudinal data on tobacco use, especially to capture the transition from adolescence to young adulthood.
Given the significance of attrition and TOT analysis in our sensitivity analysis, it is also possible that some elements of individual study design may have biased the analysis, and that, for example, different effects would be found if all studies had employed a more rigorous design and analysis approach. Because the sensitivity analyses indicated that studies using less rigorous design and analysis methods yielded inflated effect size estimates, this at least provides confidence that the overall effects from the current meta-analysis are conservative. However, this indicates that consumers of primary studies should be aware of the potential inflation of effect sizes in studies with high attrition or those using TOT analysis methods. Finally, the graphical figures included in this meta-analysis were designed to be exploratory and to help advance future primary research in this area. Thus, any implications of potential variability in effects across age groups or intervention types are exploratory and must be interpreted cautiously.
Primary recommendations
In conclusion, although brief interventions are effective in a wide variety of prevention and treatment settings, it appears they may have limited ability to address tobacco use among adolescents and young adults if alcohol consumption is the primary or simultaneous focus of the intervention. Given that the baseline status of tobacco dependence is unknown in many of the included studies, future interventionists should attend to the baseline level of tobacco use in their population and adjust their intervention approach accordingly, especially if tobacco use is a targeted outcome. If tobacco use is targeted a priori as a secondary outcome to measure, including baseline dependence data in primary studies would be useful for future syntheses of this literature. Future research should also address whether achieving secondary outcomes is only possible among certain populations (e.g. younger adolescents), and whether BIs should address certain risk behaviors simultaneously (e.g., drinking and sexual activity) or simply focus on one primary risk behavior.
References
Abrantes, A. M., Lee, C. S., Macpherson, L., Strong, D. R., Borrelli, B., & Brown, R. A. (2009). Health risk behaviors in relation to making a smoking quit attempt among adolescents. Journal of Behavioral Medicine, 32, 142–149. doi:10.1007/s10865-008-9184-1
American Cancer Society. (2014). History of the Great American smokeout. Available from http://www.cancer.org/healthy/stayawayfromtobacco/greatamericansmokeout/history-of-the-great-american-smokeout
Baer, J. S., Kivlahan, D. R., Blume, A. W., McKnight, P., & Marlatt, G. A. (2001). Brief intervention for heavy-drinking college students: 4-Year follow-up and natural history. American Journal of Public Health, 91, 1310–1316.
Barnett, S. M., & Ceci, S. J. (2002). When and where do we apply what we learn? A taxonomy for far transfer. Psychological Bulletin, 128, 612–637.
Bien, T. H., Miller, W. R., & Tonigan, J. S. (1993). Brief interventions for alcohol problems: A review. Addiction, 88, 315–335.
Bradley, E. (2009). The effects of a school-based motivational intervention on adolescent substance abuse (Doctoral dissertation, University of Massachusetts Amherst). Dissertation Abstracts International, Ph.D., 96. (University Microfilms No. 3359129)
Bryant, J., Bonevsiki, B., Paul, C., McElduff, P., & Attia, J. (2011). A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction, 106, 1568–1585. doi:10.1111/j.1360-0443.2011.03467.x
Cheung, M. W. -L. (2013). metaSEM: An R package for meta-analysis using structural equation modeling. Available from http://courses.nus.edu.sg/course/psycwlm/internet/metaSEM/
Cheung, M. W.-L. (2014). Modeling dependent effect sizes with three-level meta-analysis: A structural equation modeling approach. Psychological Methods, 19, 211–229. doi:10.1037/a0032968
Chuang, Y. C., Ennett, S. T., Bauman, K. E., & Foshee, V. A. (2009). Relationships of adolescents’ pereceptions of parental and peer behaviors with cigarette and alcohol use in different neighborhood contexts. Journal of Youth and Adolescence, 38, 1388–1398. doi:10.1007/s10964-009-9424-x
Daeppen, J.-B., Bertholet, N., Gaume, J., Fortini, C., Faouzi, M., & Gmel, G. (2011). Efficacy of brief motivational intervention in reducing binge drinking in young men: A randomized controlled trial. Drug and Alcohol Dependence, 113, 69–75. doi:10.1016/j.drugalcdep.2010.07.009
De Micheli, D., Fisberg, M., & Formigoni, M. L. (2004). Estudo da efetividade da intervenção breve para o uso de álcool e outras drogas em adolescentes atendidos num serviço de assistência primária à saúde [Study on the effectiveness of brief intervention for alcohol and other drug use directed to adolescents in a primary health care unit]. Revista Da Associacao Medica Brasileira, 50, 305–313.
Eaton, L. A., Huedo-Medina, T. B., Kalichman, S. C., Pellowski, J. A., Sagherian, M. J., Warren, M., et al. (2012). Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: Implications for bundling prevention packages. American Journal of Public Health, 102, e34–e44. doi:10.2105/AJPH.2012.300968
Feldstein, S. (2007). Motivational interviewing with late-adolescent/college underage drinkers: An investigation of therapeutic alliance. Dissertation, University of New Mexico.
Flay, B. R., & Petraitis, J. (1994). The theory of triadic influence. Advances in Medical Sociology, 4, 19–44.
Gaume, J., Daeppen, J. B., & Gmel, G. (2008). Administering brief motivational interventions to young men: results from a pilot census study among 19 year-old francophone Swiss men. Lausanne, Suisse: Centre hospitalier universitaire vaudois. Available from http://www.chuv.ch/projets_termines_rapport_phase_pilote_fobic.pdf
Gaume, J., Gmel, G., Faouzi, M., Bertholet, N., & Daeppen, J.-B. (2011). Is brief motivational intervention effective in reducing alcohol use among young men voluntarily receiving it? A randomized controlled trial. Alcoholism, Clinical and Experimental Research, 35, 1822–1830. doi:10.1111/j.1530-0277.2011.01526.x
Glasgow, R. E., Whitlock, E. P., Eakin, E. G., & Lichtenstein, E. (2000). A brief smoking cessation intervention for women in low-income planned parenthood clinics. American Journal of Public Health, 90, 786–789.
Gmel, G., Gaume, J., Bertholet, N., Fluckiger, J., & Daeppen, J. (2013). Effectiveness of a brief integrative multiple substance use intervention among young men with and without booster sessions. Journal of Substance Abuse Treatment, 44, 231–240. doi:10.1016/j.jsat.2012.07.005
Gmel, G., Venzin, V., Marmet, K., Danko, G., & Labhart, F. (2012). A quasi-randomized group trial of a brief alcohol intervention on risky single occasion drinking among secondary school students. International Journal of Public Health, 57, 935–944. doi:10.1007/s00038-013-0535-5
Gray, E., McCambridge, J., & Strang, J. (2005). The effectiveness of motivational interviewing delivered by youth workers in reducing drinking, cigarette and cannabis smoking among young people: Quasi-experimental pilot study. Alcohol Alcoholism, 40, 535–539.
Grossbard, J. R., Mastroleo, N. R., Kilmer, J. R., Lee, C. M., Turrisi, R., Larimer, M. E., & Ray, A. (2010). Substance use patterns among first-year college students: Secondary effects of a combined alcohol intervention. Journal of Substance Abuse Treatment, 39, 384–390.
Hale, D. R., Fitzgerald-Yau, N., & Viner, R. M. (2014). A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. American Journal of Public Health, 104, e19–e41. doi:10.2105/AJPH.2014.301874
Hedges, L. V. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics, 6, 107–128.
Higgins, J. P. T., Deeks, J. J., & Altman, D. G. (2008). Special topics in statistics. In J. P. T. Higgins & S. Green (Eds.), Cochrane handbook for systematic reviews of interventions (pp. 481–529). Chichester: Wiley.
Hwang, M. S., Yeagley, K. L., & Petosa, R. (2004). A meta-analysis of adolescent psychosocial smoking prevention programs published between 1978 and 1997 in the United States. Health Education and Behavior, 31, 702–719.
Jackson, K. M., Sher, K. J., Cooper, M. L., & Wood, P. K. (2002). Adolescent alcohol and tobacco use: Onset, persistence and trajectories of use across two samples. Addiction, 97, 517–531.
Jackson, K. M., Sher, K. J., & Schulenberg, J. E. (2005). Cojoint developmental trajectories of young adult alcohol and tobacco use. Journal of Abnormal Psychology, 114, 612–626. doi:10.1037/0021-843X.114.4.612
Jensen, C. D., Cushing, C. C., Aylward, B. S., Craig, J. T., Sorell, D. M., & Steele, R. G. (2011). Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology, 79, 433–440. doi:10.1037/a0023992
Kaner, E. F., Dickinson, H. O., Beyer, F. R., Campbell, F., Schlesinger, C., Heather, N. et al. (2007). Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2. Art. No.: CD004148. doi: 10.1002/14651858.CD004148.pub3
Kobus, K. (2003). Peers and adolescent smoking. Addiction, 98, 37–55.
Lippke, S., Nigg, C. R., & Maddock, J. E. (2012). Health-promoting and health-risk behaviors: Theory-driven analyses of multiple health behavior change in three international samples. International Journal of Behavioral Medicine, 19, 1–13. doi:10.1007/s12529-010-9135-4
Lipsey, M. W., & Wilson, D. (2001). Practical meta-analysis (Applied Social Research Methods) (Vol. 49). Thousand Oaks, CA: SAGE Publications Inc.
McCambridge, J. (2002). The efficacy of a brief motivational intervention in reducing drug consumption and related risk among young people involved in illegal drug use (Doctoral dissertation, University of London, Imperial College of Science, Technology and Medicine). Dissertation Abstracts International, Ph.D. (B2c 53-466)
McCambridge, J., Hunt, C., Jenkins, R. J., & Strang, J. (2011). Cluster randomised trial of the effectiveness of motivational interviewing for universal prevention. Drug and Alcohol Dependence, 114, 177–184. doi:10.1016/j.drugalcdep.2010.07.028
McCambridge, J., & Jenkins, R. J. (2008). Do brief interventions which target alcohol consumption also reduce cigarette smoking? Systematic review and meta-analysis. Drug and Alcohol Dependence, 96, 263–270. doi:10.1016/j.drugalcdep.2008.03.011
McCambridge, J., Slym, R. L., & Strang, J. (2008). Randomized controlled trial of motivational interviewing compared with drug information and advice for early intervention among young cannabis users. Addiction, 103, 1809–1818. doi:10.1111/j.1360-0443.2008.02331.x
McCambridge, J., & Strang, J. (2005). Deterioration over time in effect of motivational interviewing in reducing drug consumption and related risk among young people. Addiction, 100, 470–478.
Meier, E. M., Tackett, A. P., Miller, M. B., Grant, D. M., & Wagener, T. L. (2015). Which nicotine products are gateways to regular use? First-tried tobacco and current use in college students. American Journal of Preventive Medicine, 48, S86–S93. doi:10.1016/j.amepre.2014.09.018
Moyer, A., Finney, J. W., Swearingen, C. E., & Vergun, P. (2002). Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction, 97, 279–292.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. (2012). Preventing tobacco use among youth and young adults: A report of the surgeon general. 3, The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide. Atlanta (GA): Centers for Disease Control and Prevention (US). Available from http://www.ncbi.nlm.nih.gov/books/NBK99243/
Nelson, D. E., Mowery, P., Asman, K., Pederson, L. L., O’Malley, P. M., Malarcher, A., et al. (2008). Long-term trends in adolescent and young adult smoking in the United States: Metapatterns and implications. American Journal of Public Health, 98, 905–915. doi:10.2105/AJPH.2007.115931
Ng, M., Freeman, M. K., Fleming, T. D., Robinson, M., Dwyer-Lindgren, L., Thomson, B., et al. (2012). Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. Journal of the American Medical Association, 311, 183–192. doi:10.1001/jama.2013.284692
Prochaska, J. J., Spring, B., & Nigg, C. R. (2008). Multiple health behavior change research: An introduction and overview. Preventive Medicine, 46, 181–188. doi:10.1016/j.ypmed.2008.02.001
Richardson, A., Williams, V., Rath, J., Villanti, A. C., & Vallone, D. (2014). The next generation of users: Prevalence and longitudinal patterns of tobacco use among US young adults. American Journal of Public Health, 104, 1429–1436. doi:10.2105/AJPH.2013.301802
Riggs, N. R., Chou, C.-P., Li, C., & Pentz, M. A. (2007). Adolescent to emerging adulthood smoking trajectories: When do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine & Tobacco Research, 9, 1147–1154.
Rigotti, N. A., Lee, J. E., & Weschler, H. (2000). US college students’ use of tobacco products. Results of a National Survey. Journal of the American Medical Association, 284, 699–705. doi:10.1001/jama.284.6.699
Rothstein, H. R., Sutton, A. J., & Borenstein, M. (2005). Publication bias in meta-analysis: Prevention, assessment and adjustments. West Sussex: Wiley.
Sánchez-Meca, J., Marín-Martínez, F., & Chacón-Moscoso, S. (2003). Effect-size indices for dichotomized outcomes in meta-analysis. Psychological Methods, 8, 448–467.
Schubiner, H., Herrold, A., & Hurt, R. (1998). Tobacco cessation and youth: The feasibility of brief office interventions for adolescents. Preventive Medicine, 27, A47–A54.
Steinberg, M. B., Schmelzer, A. C., Richardson, D. L., & Foulds, J. (2008). The case for treating tobacco dependence as a chronic disease. Annals of Internal Medicine, 148, 554–556. doi:10.7326/0003-4819-148-7-200804010-00012
Substance Abuse and Mental Health Services Administration. (2013). Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Substance Abuse and Mental Health Services Administration, Rockville, MD. Available from http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/NationalFindings/NSDUHresults2012.pdf
Suls, J. M., Luger, T. M., Curry, S. J., Mermelstein, R. J., Sporer, A. K., & An, L. C. (2012). Efficacy of smoking-cessation interventions for young adults. American Journal of Preventive Medicine, 42, 655–662. doi:10.1016/j.amepre.2012.02.013
Sussman, S., Sun, P., & Dent, C. W. (2006). A meta-analysis of teen cigarette smoking cessation. Health Psychology, 25, 549–557.
Tait, R. J., & Hulse, G. K. (2003). A systematic review of the effectiveness of brief interventions with substance using adolescents by type of drug. Drug and Alcohol Review, 22, 337–346.
Tanner-Smith, E. E., & Lipsey, M. W. (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. doi:10.1016/j.jsat.2014.09.001
Tanner-Smith, E. E., & Polanin, J. R. (2014). A retrospective analysis of dissemination biases in the brief alcohol intervention literature. Psychology of Addictive Behaviors, 29, 49–62. doi:10.1037/adb0000014
Tanner-Smith, E. E., Steinka-Fry, K. T., Hennessy, E. A., Lipsey, M. W., & Winters, K. C. (2015). Can brief alcohol interventions for youth also address concurrent drug use? Results from a meta-analysis. Journal of Youth and Adolescence, 44, 1011–1023.
Turrisi, R., Larimer, M. E., Mallett, K. A., Kilmer, J. R., Ray, A. E., Mastroleo, N. R., et al. (2009). A randomized clinical trial evaluating a combined alcohol intervention for high-risk college students. Journal of Studies on Alcohol and Drugs, 70, 555–567.
U.S. Department of Health and Human Services. (2012). Preventing tobacco use among youth and young adults. A report of the Surgeon General (executive summary). Rockville, MD: U.S. Department of Health and Human Services. Available from http://www.surgeongeneral.gov/library/reports/preventing-youth-tobacco-use/exec-summary.pdf
Van De Ven, M. O. M., Greenwood, P. A., Engels, R. C. M. E., Olsson, C. A., & Patton, G. C. (2010). Patterns of adolescent smoking and later nicotine dependence in young adults: A 10-year prospective study. Public Health, 124, 65–70. doi:10.1016/j.puhe.2009.11.009
Vasilaki, E. I., Hosier, S. G., & Cox, W. M. (2006). The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol Alcoholism, 41, 328–335.
Werch, C. E., Anzalone, D. M., Brokiewicz, L. M., Felker, J., Carlson, J. M., & Castellon-Vogel, E. A. (1996). An intervention for preventing alcohol use among inner-city middle school students. Archives of Family Medicine, 5, 146–152.
Werch, C. E., Bian, H., Carlson, J. M., Moore, M. J., DiClemente, C. C., Huang, I. C., et al. (2011). Brief integrative multiple behavior intervention effects and mediators for adolescents. Journal of Behavioral Medicine, 34, 3–12.
Werch, C. E., Bian, H., DiClemente, C. C., Moore, M. J., Thombs, D., Ames, S. C., et al. (2010a). A brief image-based prevention intervention for adolescents. Psychology of Addictive Behaviors, 24, 170–175. doi:10.1037/a0017997
Werch, C. E., Moore, M. J., Bian, H., DiClemente, C. C., Ames, S. C., Weiler, R. M., & Huang, I. C. (2008). Efficacy of a brief image-based multiple-behavior intervention for college students. Annals of Behavioral Medicine, 36, 149–157. doi:10.1007/s12160-008-9055-6
Werch, C. E., Moore, M. J., Bian, H., DiClemente, C. C., Huang, I. C., Ames, S. C., et al. (2010b). Are effects from a brief multiple behavior intervention for college students sustained over time? Preventive Medicine, 50, 30–34. doi:10.1016/j.ypmed.2009.12.010
Werch, C., Moore, M. J., DiClemente, C. C., Bledsoe, R., & Jobli, E. (2005a). A multihealth behavior intervention integrating physical activity and substance use prevention for adolescents. Prevention Science, 6, 213–226. doi:10.1007/s11121-005-0012-3
Werch, C. E., Moore, M. M., Diclemente, C. C., Owen, D. M., Carlson, J. M., & Jobli, E. (2005b). Single vs. multiple drug prevention: Is more always better? A pilot study. Substance Use and Misuse, 40, 1085–1101. doi:10.1081/ja-200030814
White, H. R., Mun, E. Y., & Morgan, T. J. (2008). Do brief personalized feedback interventions work for mandated students or is it just getting caught that works? Psychology of Addictive Behaviors, 22, 107–116. doi:10.1037/0893-164x.22.1.107
World Health Organization. (2014). About the WHO framework convention on tobacco control. Available from http://www.who.int/fctc/about/en/
Acknowledgments
This work was supported by Award Number R01AA020286 from the National Institute on Alcohol Abuse and Alcoholism. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
Conflict of Interest
Emily A. Hennessy, Emily E. Tanner-Smith and Katarzyna T. Steinka-Fry declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hennessy, E.A., Tanner-Smith, E.E. & Steinka-Fry, K.T. Do brief alcohol interventions reduce tobacco use among adolescents and young adults? A systematic review and meta-analysis. J Behav Med 38, 899–911 (2015). https://doi.org/10.1007/s10865-015-9653-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-015-9653-2