Abstract
Objective
External fixators are important for correcting length discrepancies and axis deformities in pediatric or trauma orthopedic surgery. Pin loosening is a common pitfall during therapy that can lead to pain, infection, and necessary revisions. This study aims to present clinical data using calcium titanate (CaTiO3) Schanz screws and to measure the fixation strength.
Patients and methods
22 titanate screws were used for external fixators in 4 pediatric patients. Therapy was initiated to lengthen or correct axial deformities after congenital abnormalities. The maximum tightening torque was measured during implantation, and the loosening torque was measured during explantation. In addition, screws of the same type were used in a cadaver study and compared with stainless steel and hydroxyapatite-coated screws. 12 screws of each type were inserted in four tibias, and the loosening and tightening torque was documented.
Results
The fixation index in the in vivo measurement showed a significant increase between screw insertion and extraction in three of the four patients. The pins were in situ for 91 to 150 days, and the torque increased significantly (P = 0.0004) from insertion to extraction. The cadaveric study showed lower extraction torques than insertion torques, as expected in this setting. The calculated fixation index was significantly higher in the CaTiO3 group than in the other groups (P = 0.0208 vs. HA and P < 0.0001 vs. steel) and in the HA group vs. plain steel group (P = 0.0448).
Conclusion
The calcium titanate screws showed favorable fixation strength compared to HA and stainless steel screws and should be considered in long-term therapy of external fixation.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
External fixation is a key tool in both traumatology and reconstructive orthopedic surgery. Advantages include fast and simple application, minimal soft tissue damage, and the possibility of individual adjustment after surgery [1]. The technique can be used to correct congenital or acquired deformities, non-unions, or soft tissue defects. However, external fixation is associated with serious complications, especially when prolonged therapy is necessary. Common complications include pin tract infections, pin loosening, and osteomyelitis. Pin loosening or infection occurs in approximately 10% of pins when implanted in a lower extremity [2]. Some authors associate improved fixation strength with a lower rate of pin tract infection [3]. Stainless steel screws are still the worldwide standard for external fixation, even though prospective and randomized studies have shown that hydroxyapatite (HA)-coated screws are clinically effective in improving the strength of fixation of the bone-pin interface [4, 5]. HA coatings can increase the attachment of bone to metal implants and bioactive surfaces and demonstrate osteoconductive properties [6, 7]. However, the coated layer is not stable in living bone for long periods and can debond from the metal surface [8]. HA debris may have adverse effects on integration and stability.
A new innovation is a surface modification with calcium titanate (CaTiO3). The idea is to induce apatite formations on the surface in living bone, leading to improved bonding [9]. The material is bioactive and osteoconductive like HA, but the calcium is incorporated into the titanium so that there is no risk of flaking.
The aim of this study is to evaluate the osseous integration and fixation strength of calcium titanate Schanz screws in long-term treatment and to compare the material with stainless steel and HA screws. The screws were used in vivo when a long-term therapy for external fixation was indicated. All screws were also tested in a cadaver study to evaluate the biomechanical effects on the fixation strength. The working hypothesis predicted a higher stability with lower complication and loosening rates due to the favorable integration of the calcium titanate design.
2 Patients and methods
2.1 In vivo study
To evaluate the fixation of the new calcium titanate material, EpicalTM Screws (Merete GmbH, Berlin, Germany) were used in a monolateral external fixator (ABS External Fixator, Orthofix, Lewisville, USA). The patients were treated for congenital and post-traumatic length discrepancies or deformities in the lower or upper extremities. A total of 22 screws were inserted, and the maximum insertion and extraction torque was measured using a torque wrench. To eliminate several variables that are relevant to the fixation strength, such as the diameter, cone, and thread, the contact area between the screw and bone in the Fixation Index was determined. The Fixation Index is the quotient of maximum extraction torque over maximum insertion torque and allows us to appreciate the specific fixation strength as published before by this group [10]. The study was approved by the local institutional review board (Ethics Committee No. AZ 67/16).
2.2 Patients and operative technique
Four pediatric patients between 2 and 14 years old were included. Three patients had deformities of the lower extremity, and one had a deformity of the upper extremity.
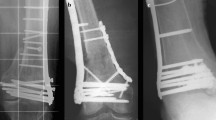
Patient 1 showed a proximal femoral focal deficiency (PFFD) of the left leg with a leg length difference of 5 cm. The therapy of choice was a callus distraction after osteotomy of the femoral shaft (Fig. 1). The external fixator was left for 112 days, and the age during index surgery was three years. No complications could be detected during therapy.
Patient 2 was a 10-year-old female with a complex deformity of the lower leg due to damage of the lamina epiphysialis after Waterhouse-Friedrichsen syndrome. The leg showed a combined varus and rotational deformity that was addressed by a focal-dome osteotomy (FDO) and external fixation for 150 days. Two screws showed clinical signs of infection (Checketts-Otterburn Grade 3) [11] and were exchanged during a revision surgery.
Patient 3 showed a congenital patella agnesis with further agenesis of the anterior crucial ligament and loss of 90° of extension in the knee joint. To restore full extension, a so-called parallelogram fixator was used with consequent daily external distraction until 0° extension in the joint was seen after 95 days of therapy.
Patient 4 was the oldest patient at 15 years of age and the only one who showed an axial malalignment of the upper extremity due to a fibrous dysplasia of the right humerus. Therapy included a multidimensional corrective osteotomy and application of an external fixator.
The basic operative technique was similar in all cases. Two or three screws were inserted proximally and distally of the osteotomy area. A small skin incision was made after radiological orientation of the bone structure. The underlying fascia was dissected to prevent interference with the pins. A drill guide was used to protect the soft tissue, and both cortexes were penetrated. The selected screw was then inserted using a T-handle. After penetrating the second cortex, the insertion torque was measured by a torque meter (Fig. 2). After therapy, the fixators were removed under anesthesia, and the first rotation was measured using a torque meter to quantify the extraction torque.
The number of pin tract infections was documented and classified using the Checketts-Otterburn grading system [1, 11]. Table 1 shows the grading system and the recommended treatment option for each grade.
2.3 Cadaver study
For the cadaver study, four human tibias were provided by the Institute of Anatomy at our institution. The same type Epical Screws as in the clinical trial were used. 6.5-mm HA and common steel screws were used in comparison (Orthofix, Lewisville, USA). Three screws of each type (Epical, HA, steel) were inserted in random order on every tibia. Figure 3 shows an example of the three products. As recommended by the manufacturer, the cavity was pre-drilled bicortically with a 4.1-mm drill. The screws were introduced manually using a T-handle. After piercing through the second corticalis, a torque meter was used to measure the maximum tightening torsion moment (Fig. 2). The screws were left for 24 h and then removed using the same torque meter to determine the maximum loosening torque. As in the clinical trial, the quotient of both values was computed to subtract possible inaccuracies due to various insertion points and bone diameters. Figure 4 shows the setup for the cadaver study.
2.4 Statistical analysis
Data from cadaveric torque measurements were gathered in Microsoft Excel 365 (Microsoft Corporation, Richmond, VA, USA), and the fixation index was calculated as described by this group [10]. The data were then transferred to GraphPad Prism v8.0.1 (GraphPad, LaJolla, CA, USA) for statistical analysis. The Gaussian distribution and equal standard deviation of insertion, extraction, and index results between the three screw types were confirmed using the D’Agostino & Pearson test and the Brown-Forsythe test, respectively. The data were then analyzed for significant differences between the screw types using an ordinary one-way ANOVA followed by a post-hoc analysis with Tukey’s multiple comparisons test. An adjusted P-value of P < 0.05 was considered significant.
In vivo data of insertion and extraction were also recorded in MS Excel and analyzed in Prism, and the fixation index was calculated. To assess for statistical significance between insertion and extraction torque, multiple Wilcoxon matched-pairs signed rank tests with a Sidak-Bonferroni correction for multiple testing were calculated for each patient separately and for pooled data. Again, a P-value of P < 0.05 was considered significant.
3 Results
The torque measurements and fixation indices of the cadaveric study are summarized in Table 2. The extraction torques were generally lower than the insertion torques, as expected in a cadaveric setting with no chance of biological integration. This effect was more distinct with the steel screws and the HA-coated screws than in the CaTiO3 screws, but the differences between insertion and extraction did not achieve statistical significance in any group (P = 0.361 for CaTiO3, P = 0.063 for HA, P = 0.059 for steel).
We also found no significant differences in the insertion and extraction torques between the three screw types; however, the CaTiO3 screws showed a tendency toward higher extraction torques (see Fig. 5a, b). The calculated fixation index was significantly higher in the CaTiO3 group than in the two other groups (P = 0.0208 vs. HA and P < 0.0001 vs. steel) and in the HA group vs. plain steel group (P = 0.0448) (Fig. 5c).
The in vivo measurements (see Figs 6 and 7) showed a significant increase in torque measurements between screw insertion and extraction in three of the four patients and a positive fixation index. The pins were in situ for 91 to 150 days. Patient 2—150d, with no significant increase in torque, had severe pin infections in two out of six pins, which were loose and therefore could not be included in the analysis. There was no relevant correlation between the time in situ and increases in the fixation index in this small collective.
In vivo torque measurements of the four patients. Torque measurements (white and light gray) are plotted on the left y-axis, and the fixation index (dark gray) is plotted on the right. The x-axis shows the patient number and number of days the pins were in situ. ****p < 0.0001, ns: not significant. Two specimens of Patient 2 were excluded due to pin infection and loosening
4 Discussion
This paper focuses on testing calcium titanate screws for long-term therapy using external fixation for deformity correction. Common complications during therapy are pin tract infections and osteomyelitis. Pin loosening can also occur, leading to a secondary loss of reduction or axial correction. To prevent these complications, an enduring fixation strength with stable osseous integration might be beneficial [12, 13]. The fixation index was therefore measured in vivo and in an additional cadaver study. Our results showed a significantly higher fixation strength in three out of four patients treated for 91 to 150 days with the goal of limb lengthening or correction. The pooled measurements of all four patients showed significantly increased torque (P = 0.0004) from insertion to extraction.
The cadaver study supported the results, showing that the fixation index was significantly higher in the CaTiO3 group than in the two other groups (P = 0.0208 vs. HA and P < 0.0001 vs. steel) and in the HA group vs. plain steel group (P = 0.0448).
Antibacterial and bioactive properties have been reported in calcium titanate-enriched metal surfaces [14]. Furthermore, CaTiO3 can act as an apatite growth promoter [15]. A research group compared cylindrical calcium titanate implants with standard implants (Ti6AI4V surface) that were brought into the femurs of white rabbits. After 4, 12, and 36 weeks, the pull-off forces were measured. Compared to untreated implants (median = 16.68 Nm), the treated implants (median = 25.36 Nm) showed significantly higher pull-off forces (p = 0.043). The authors saw calcium titanate surfaces as a promising alternative for usage in total joint replacements to accelerate osseointegration, especially in patients with poor bone quality [16]. The applied HA and CaTiO3 pins in this study had a macroporous surface to allow bone ingrowth, leading to long-term stable fixation of the implants. The bone trabeculae interweaved with the pore struts established a large contact area, improving the load transfer and strengthening the implant/bone interface [17]. The surface modification might explain the favorable results for HA and CaTiO3 implants even in cadaver bone compared to polished stainless steel screws.
Pin tract infections and loosening are the most common complications when using external fixation. While some authors view infection as an almost inevitable complication that leads to loosening, other surgeons view the infection as a consequence of progressive pin loosening [1, 3, 18]. A recent review article investigating possible care protocols to reduce the incidence of pin site infections found no general or valid strategy to prevent infection but recommended the implementation of a standardized algorithm [19]. The rate of pin site infection ranged from 10 to 100%, whereas the reported incidence of chronic osteomyelitis ranged from 0.4 to 4% [20,21,22]. Of course, further parameters such as age, comorbidities, poor nutritional status, or bone quality also influence the rate of complication. The pin sites are essentially wounds, and wound healing cannot be achieved as long as the therapy via external fixation continues [23]. There is no gold standard yet, but almost all treatment protocols include frequent pin inspection and the use of antiseptic materials such as saline, iodine solutions, or impregnated gauzes [24,25,26]. In addition to pin care, the technique can be an influencing factor. A higher incidence of pin site infections has been observed with monolateral and hybrid fixators compared to ring fixators [22].
Biomechanical evaluations of different external fixator configurations showed a significantly higher stability in biplanar fixation compared to uniplanar fixation. However, a uniplanar fixation is easy to apply and showed favorable conditions at the site of bone fracture healing. Good stability in the transversal plane and compensation of rotational forces could be seen when using multiplanar fixators [27,28,29,30].
While most studies discuss pin care and the operation technique, few focus on the characteristics of the implants used. One possible approach is the antibacterial coatings of the pins. The use of iodine-supported titanium pins shows low infection rates of 3.6% compared to the reported rates in the literature [31]. However, similar to HA-coated screws, debonding may occur, leading to a remaining percentage of 42% iodine after 0–4 months of therapy. Another coating option to reduce potential bacterial colonization is silver. A reduction of pin tract infection of 22% is reported when using silver-coated pins compared to uncoated pins [32]. Moroni et al. tested 76 screws in 19 patients using either HA-coated, titanium, or steel pins. The authors found an elevated extraction torque in both cancellous and cortical bone using HA-coated pins. Further investigation of the pin-bone interface showed no deterioration, leading to optimal pin-bone contact [33]. There are numerous other reported coatings such as ultrahigh molecular weight polyethylene or tobramycin-impregnated polymethylmethacrylate with promising results regarding fixation strength and infection rate, but none have become a standard method [34, 35]. Like other authors [22], we believe that there is a close relationship between the motion of loose pins and infection. Accordingly, a high fixation strength is of utter importance. Lawes et al. tested the relation of the maximum insertion torque of external fixation pins with osseo-mechanical integration in an animal experiment [36]. The authors stated that a higher insertion torque optimized the mechanical stability in vivo. A torque higher than 7 Nm showed a measurable extraction torque in all screws and a torque higher than 5 Nm in 98% of tested screws. Another group tried to find a boundary value for the insertion torque and found a 69% loosening rate when the initial torque resistance was less than 0.68 Nm compared to only 9% of pins with an initial torque greater than 0.68 Nm [37]. As the link between the bone and the implanted material, the pin-bone interface is both the anchoring point and the weakest site of mechanical stability. Aro et al. investigated the cortical bone reaction at the interface of half-pins under loading conditions in a canine model. Remodeling of new bone structure was seen in 43% of the intercortical space along the pin tract but showed a massive porosity of cortical bone compared to intact bone value. Subsequently, micromotion and time-related decrease of pin removal torque was seen [38]. The results underline the importance of avoiding postoperative dynamic stress on the external fixation construct. Further histological examinations of the pin-bone interface found that, in general, tight pin tracts are characterized by a lack of bone resorption and sparse development of new bone, whereas the cortex around grossly loose pins showed a mostly resorbed bone structure (75% compared to 14%) [37].
One limitation of this study is the small sample in the in vivo group due to the rarity of long-term therapy using external fixation. Another limitation is the missing control group using screws of a different material in vivo. There is also no standardized method for measuring the fixation strength of pins for external fixation.
Considering factors like infection rate and fixation strength, the new calcium titanate pins promise favorable properties and are a promising alternative for use in external fixation. Our results showed a good practicability of calcium titanate screws for long-term therapy of external fixation. Use in short-term therapy does not seem practical due to the higher cost of materials and lack of time for osseointegration. Further randomized and prospective studies are necessary to evaluate the attributes of different screw types and to develop generally accepted therapy algorithms.
References
Ceroni D, Grumetz C, Desvachez O, Pusateri S, Dunand P, Samara E. From prevention of pin-tract infection to treatment of osteomyelitis during paediatric external fixation. J Child Orthop 2016;10:605–12.
Moroni A, Pegreffi F, Cadossi M, Hoang-Kim A, Lio V, Giannini S. Hydroxyapatite-coated external fixation pins. Expert Rev Med Devices. 2005;2:465–71.
Moroni A, Aspenberg P, Toksvig-Larsen S, Falzarano G, Giannini S. Enhanced fixation with hydroxyapatite coated pins. Clin Orthop 1998;346:171–7.
Moroni A, Heikkila J, Magyar G, Toksvig-Larsen S, Giannini S. Fixation strength and pin tract infection of hydroxyapatite-coated tapered pins. Clin Orthop 2001;388:209–17.
Saithna A. The influence of hydroxyapatite coating of external fixator pins on pin loosening and pin track infection: a systematic review. Injury. 2010;41:128–32.
Coathup MJ, Blunn GW, Flynn N, Williams C, Thomas NP. A comparison of bone remodelling around hydroxyapatite-coated, porous-coated and grit-blasted hip replacements retrieved at post-mortem. J Bone Joint Surg Br 2001;83:118–23.
Reikerås O. Femoral revision surgery using a fully hydroxyapatite-coated stem: a cohort study of twenty two to twenty seven years. Int Orthop 2017;41:271–5.
Collier JP, Surprenant VA, Mayor MB, Wrona M, Jensen RE, Surprenant HP. Loss of hydroxyapatite coating on retrieved, total hip components. J Arthroplast 1993;8:389–93.
Kokubo T, Yamaguchi S. Novel bioactive titanate layers formed on Ti metal and its alloys by chemical treatments. Materials. 2009;3:48–63.
Placzek R, Ruffer M, Deuretzbacher G, Heijens E, Meiss AL. The fixation strength of hydroxyapatite-coated Schanz screws and standard stainless steel Schanz screws in lower extremity lengthening: a comparison based on a new torque value index: the fixation index. Arch Orthop Trauma Surg 2006;126:369–73.
Checketts RG, MacEachem AG, Otterbum M. Pin track infection and the principles of pin site care. In: De Bastiani G, Apley AG, Goldberg A, (eds) Orthofix external fixation in trauma and orthopaedics. London: Springer London; 2000. http://springerlink.bibliotecabuap.elogim.com/10.1007/978-1-4471-0691-3_11.
Hedin H, Larsson S. Technique and considerations when using external fixation as a standard treatment of femoral fractures in children. Injury. 2004;35:1255–63.
Kazmers NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixation: a review of the literature. Strateg Trauma Limb Reconstr Online. 2016;11:75–85.
Kizuki T, Matsushita T, Kokubo T. Antibacterial and bioactive calcium titanate layers formed on Ti metal and its alloys. J Mater Sci Mater Med 2014;25:1737–46.
Coreño J, Coreño O. Evaluation of calcium titanate as apatite growth promoter. J Biomed Mater Res A 2005;75:478–84.
Haenle M, Lindner T, Ellenrieder M, Willfahrt M, Schell H, Mittelmeier W, et al. Bony integration of titanium implants with a novel bioactive calcium titanate (Ca4Ti3O10) surface treatment in a rabbit model. J Biomed Mater Res A. 2012;100:2710–6.
Braem A, Chaudhari A, Vivan Cardoso M, Schrooten J, Duyck J, Vleugels J. Peri- and intra-implant bone response to microporous Ti coatings with surface modification. Acta Biomater 2014;10:986–95.
Placzek R, Hempfing A, Meiss AL. Evaluation of hydroxyapatite-coated Schanz screws in the Heidelberg external fixation system (HEFS). Biomed Tech. 2001;46:172–5.
Ktistakis I, Guerado E, Giannoudis PV. Pin-site care: can we reduce the incidence of infections? Injury. 2015;46:S35–9.
DeJong ES, DeBerardino TM, Brooks DE, Nelson BJ, Campbell AA, Bottoni CR, et al. Antimicrobial efficacy of external fixator pins coated with a lipid stabilized hydroxyapatite/chlorhexidine complex to prevent pin tract infection in a goat model. J Trauma. 2001;50:1008–14.
Hosny G, Fadel M. Ilizarov external fixator for open fractures of the tibial shaft. Int Orthop 2003;27:303–6.
Parameswaran AD, Roberts CS, Seligson D, Voor M. Pin tract infection with contemporary external fixation: how much of a problem? J Orthop Trauma. 2003;17:503–7.
Britten S, Ghoz A, Duffield B, Giannoudis PV. Ilizarov fixator pin site care: the role of crusts in the prevention of infection. Injury. 2013;44:1275–8.
Davies R, Holt N, Nayagam S. The care of pin sites with external fixation. J Bone Jt Surg Br 2005;87:716–9.
Sian PS, Britten S, Duffield B. The care of pin sites with external fixation. J Bone Jt Surg Br 2006;88:558.
Lethaby A, Temple J, Santy-Tomlinson J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev. 2013;12:CD004551.
Hohloch L, Konstantinidis L, Wagner FC, Strohm PC, Südkamp NP, Reising K. Biomechanical evaluation of a new technique for external fixation of unstable supracondylar humerus fractures in children. Technol Health Care J Eur Soc Eng Med 2015;23:453–61.
Hohloch L, Konstantinidis L, Wagner FC, Strohm PC, Südkamp NP, Reising K. Biomechanical comparison of different external fixator configurations for stabilization of supracondylar humerus fractures in children. Clin Biomech Bristol Avon. 2016;32:118–23.
Li W-C, Meng Q-X, Xu R-J, Cai G, Chen H, Li H-J. Biomechanical analysis between Orthofix® external fixator and different K-wire configurations for pediatric supracondylar humerus fractures. J Orthop Surg 2018;13:188.
Grubor P, Grubor M, Asotic M. Comparison of stability of different types of external fixation. Med Arh 2011;65:157–9.
Shirai T, Watanabe K, Matsubara H, Nomura I, Fujiwara H, Arai Y, et al. Prevention of pin tract infection with iodine-supported titanium pins, J. Orthop. Sci. J Jpn Orthop Assoc 2014;19:598–602.
Collinge CA, Goll G, Seligson D, Easley KJ. Pin tract infections: silver vs uncoated pins. Orthopedics. 1994;17:445–8.
Moroni A, Vannini F, Mosca M, Giannini S. State of the art review: techniques to avoid pin loosening and infection in external fixation. J Orthop Trauma. 2002;16:189–95.
Manley MT, Hurst L, Hindes R, Dee R, Chiang FP. Effects of low-modulus coatings on pin-bone contact stresses in external fixation. J Orthop Res Publ Orthop Res Soc 1984;2:385–92.
Voos K, Rosenberg B, Fagrhi M, Seligson D. Use of a tobramycin-impregnated polymethylmethacrylate pin sleeve for the prevention of pin-tract infection in goats. J Orthop Trauma. 1999;13:98–101.
Lawes TJ, Scott JCR, Goodship AE. Increased insertion torque delays pin-bone interface loosening in external fixation with tapered bone screws. J Orthop Trauma. 2004;18:617–22.
Pettine KA, Chao EY, Kelly PJ. Analfysis of the external fixator pin-bone interface. Clin Orthop 1993;293:18–27.
Aro HT, Markel MD, Chao EY. Cortical bone reactions at the interface of external fixation half-pins under different loading conditions. J Trauma. 1993;35:776–85.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gathen, M., Ploeger, M.M., Jaenisch, M. et al. Outcome evaluation of new calcium titanate schanz-screws for external fixators. First clinical results and cadaver studies. J Mater Sci: Mater Med 30, 124 (2019). https://doi.org/10.1007/s10856-019-6325-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-019-6325-8