Abstract
Purpose
Assess if timing of removal of a percutaneous left ventricular assist device (pLVAD) after ventricular tachycardia (VT) ablation alters patient outcomes.
Methods
Sixty-nine patients underwent pLVAD support. Patients were divided into early (< 24 h, n = 43) and delayed (≥ 24 h, n = 26) removal groups after ablation. Factors for delayed pLVAD removal and predictors of 90-day mortality were analyzed.
Results
The delayed removal group had lower LVEF (27.1 ± 9.3% vs. 20.6 ± 5.4%, p = 0.002), greater percentage LVEF < 25% (58.1% vs. 84.6%, p = 0.02), and more VT storm (41.9% vs. 96.2%, p < 0.001). Ventricular fibrillation (VF) was induced in 9/69 (13%), with incidence higher in delayed removal group (27% vs. 5%, p = 0.002). VT storm (OR = 34.72, 95% CI, 4.30–280.33; p = 0.001), LVEF < 25% (OR = 3.95, 95% CI, 1.16–13.48; p = 0.03), and VF induced during ablation (OR = 9.25, 95% CI, 1.71–50.0; p = 0.01) were associated with delayed pLVAD removal in univariate analysis. Delayed pLVAD removal had a significantly higher 90-day mortality rate (2.3% vs 30.2%; p < 0.001). Univariate Cox proportional hazard regression analysis revealed delayed pLVAD removal was a significant predictor of 90-day mortality.
Conclusions
Prolonged pLVAD insertion (≥ 24 h) after VT ablation was associated with VT storm, LVEF < 25%, and VF induced during ablation. Delayed pLVAD removal was a significant predictor of 90-day mortality in patients undergoing VT ablation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Catheter ablation is an established therapy in the management of ventricular tachycardia (VT) in patients with structural heart disease [1, 2]. In selected high-risk patients, a percutaneous left ventricular assist device (pLVAD) may be useful to avoid acute hemodynamic deterioration and allow mapping and ablation of unstable VT [3, 4]. These high-risk features include severely depressed LVEF and VT storm [5,6,7]. Currently, pLVAD use is considered a class II recommendation by the updated expert consensus statement on catheter ablation of ventricular arrhythmias [8].
The significance, however, regarding the time of removal of pLVAD support after VT ablation remains unknown. Clinical practice is to remove the device immediately after the procedure, but a subset of patients may have a tenuous hemodynamic status at baseline or post procedure. Hemodynamic support could be continued after the procedure as an aid in ventricular unloading and diuresis. Which factors are related to the delayed removal of a pLVAD and whether this delayed removal has an impact on patient outcomes is uncertain. We aimed to compare mortality outcomes among patients with delayed (≥ 24 h) versus early (< 24 h) removal of a pLVAD after VT ablation, as well as determine factors associated with delayed removal of a pLVAD.
2 Methods
2.1 Patient selection
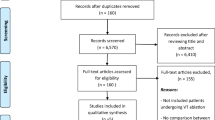
A total of 183 patients with structural heart disease (LVEF ≤ 40%) underwent VT ablation at Texas Heart Institute/Baylor St. Luke’s Medical Center between June 2010 and November 2017, of which 69 patients (38%) underwent pLVAD support at the time of ablation per operator discretion. Patients with existing pLVAD support prior to ablation were excluded. The study cohort consisted of these 69 patients who underwent catheter ablation of VT supported by a pLVAD. All patients were divided into two groups: one group had the pLVAD removed less than 24 h and the other group 24 h or more after VT ablation. The end point was 90-day mortality during follow-up. The study was approved by the local institutional review board.
2.2 Percutaneous left ventricular assist device implantation
The use and type of pLVAD was up to operator discretion. Insertion of an Impella™ 2.5 or CP device (Abiomed, Inc., Danvers, MA) was performed via a 13F/14F femoral arterial sheath respectively, and performance was set to a maximum level (2.5—2.0–2.5 L/min, CP 3.8–4.1 L/min) throughout the procedure. After removal, hemostasis was achieved via manual pressure or closure device (PerClose Proglide™, Abbott Medical, Abbott Park, IL) to the femoral artery. Surgical closure was performed if any concern for vascular compromise existed.
2.3 Electrophysiology study and catheter ablation
Antiarrhythmic drugs were discontinued for ≥ 4 half-lives before the procedure, if possible. General anesthesia was used in all the patients. Mapping was performed using activation and entrainment techniques during VT if tolerated, or by substrate mapping performed in sinus or paced rhythm. Heparin infusion was initiated after access to the left ventricle to maintain activated clotting time of 300–350 s. An impedance (EnSite, Abbott Medical) or hybrid magnetic/impedance (CARTO, Biosense Webster) electroanatomic mapping system was used in all cases to identify regions of scar where tissue voltage was ≤ 1.5 mV. The strategy of a substrate-based approach for ablation included ablation of late potentials within scar, sites with pace maps of induced or clinical VTs within scar, multi-exit sites, LAVA sites, and border zones of scar that were presumed exits of VT.
All procedures were performed via a trans-septal approach using either an Agilis sheath (Abbott Medical) or Mullins sheath (Medtronic, Minneapolis, MN). Ablation was performed using a 3.5-mm irrigated tip ablation catheter (Thermocool, Biosense Webster). Programmed electrical stimulation was performed using standard ventricular extrastimuli protocol to assess for initial inducibility and identification of a targeted VT for ablation. After ablation, repeat-programmed stimulation with ≤ 3 ventricular extrastimuli delivered from 2 different sites was performed to determine the procedural success, which was defined as lack of inducibility of the clinical VT and of all the mappable and unmappable non-clinical induced VT with cycle length > 200 ms.
2.4 Statistical analysis
Continuous data are reported as mean (+SD) or median (inter-quartile range [IQR]), and comparisons between groups were performed with the use of Student’s t test or Wilcoxon–Mann–Whitney test where appropriate. Categorical data were reported as proportions or percentages, and comparisons between groups were performed using x2 test or Fisher’s exact test where appropriate. Univariate logistic regression analysis was applied to assess the association of baseline clinical and procedural variables with the delayed removal of pLVAD ≥ 24 h. Mortality within 90 days after the ablation procedure was reported, and survival curves were created by using the Kaplan-Meier method with differences between groups compared with the log-rank test. Univariate Cox proportional hazard regression was used to identify baseline clinical variables predictive of mortality over 90-day follow-up. Relative risk estimates for mortality from univariate Cox regression analyses were reported as hazard ratio (HR) and 95% confidence interval (CI). A level of p < 0.05 was considered to indicate statistical significance. Statistical analyses were done by STATA 12.1 statistical package (Stata Corporation, College Station, TX).
3 Results
3.1 Clinical characteristics of patients with early or delayed removal of pLVAD
A total of 69 patients [mean age 65.2 ± 11.1 years; male = 66 (95.7%)] who underwent VT ablation with pre-emptive pLVAD implantation between June 2010 to November 2017 were included. A total of 51 patients (73.9%) had underlying ischemic cardiomyopathy, 63 (91.3%) had NYHA functional class III/IV, 47 (68.1%) had LVEF lower than 25%, and 63 (91.3%) had an implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy-defibrillator (CRT-D) before the ablation procedure.
All patients had either an Impella™ 2.5 or CP device implanted. The cohort was divided based on timing of pLVAD removal post ablation. Forty-three patients had pLVAD removed < 24 h (early), and the other 26 patients had it removed ≥ 24 h (delayed) after the VT ablation. A cutoff time of 24 h was used as some patients had a planned surgical removal of pLVAD later in the day of the procedure without any evidence of hemodynamic compromise. In the early removal group, 39 out of 43 (90.7%) patients had the pLVAD removed immediately at the end of the procedure, while 4 patients had it continued for less than 24 h (median 5.2 h) due to the planned surgical removal. Median time of delayed pLVAD support (≥ 24 h) was 60.5 h (25–168 h) support post procedure. In the delayed removal group (n = 26), 14 patients maintained Impella™ support, 9 patients changed from Impella™ to IABP, 2 patients from Impella™ to TandemHeart™, and 1 patient from Impella™ to ECMO. All changes in support device were due to persistently low mean arterial pressure, and based on clinical decision-making, these patients were felt to need continued forms of hemodynamic support due to tenuous hemodynamic status. There were no procedural related complications in patients with device changes. Fifteen patients had pLVAD removal between 24 and 72 h (10 of them between 24 and 48 h and 5 of them between 48 and 72 h), while 11 patients had greater than 6 days (the longest one is 9 days) of pLVAD support post procedure.
There was no significant difference in age (65.6 ± 9.3 vs. 64.6 ± 13.8 years old, p = 0.72), diabetes (32.6% vs. 46.2%, p = 0.26), hypertension (65.1% vs. 69.2%, p = 0.73), ischemic cardiomyopathy (79.1% vs. 65.4%, p = 0.21), COPD (14% vs. 23.1%, p = 0.33), chronic kidney disease (34.9% vs. 53.9%, p = 0.12), and the NYHA class III/IV (88.4% vs. 96.2%, p = 0.27) between the early and delayed removal groups. There was no difference in medications between the early and delayed removal groups, including β-blocker (76.7% vs. 73.1%, p = 0.73), ACEI/ARB (51.2% vs. 61.5%, p = 0.40), and diuretics (86.0% vs. 84.6%, p = 0.87). Finally, there was no significant difference in LVEDD between groups (median, early—6.25 cm vs delayed—6.1 cm). Often, pLVAD support may be more stable with less ventricular ectopy in patients with larger LV cavity as suggested by LVEDD (Table 1).
A total of 43 (62.3%) patients presented with VT storm, which was defined as ≥ 3 separate sustained episodes of VT in the 24 h before ablation, and the presence of VT storm was higher (25/26, 96.2% vs. 18/43, 41.9%, p < 0.001) in delayed removal group patients than that in the early removal group. Compared with the early removal group, the creatinine clearance was higher (1.32 ± 0.48 vs. 1.73 ± 1.05 mg/dL, p = 0.030), the LVEF was lower (27.1 ± 9.3% vs. 20.6 ± 5.4%, p = 0.002), and the number of patients with LVEF < 25% was higher (25/43, 58.1% vs. 22/26, 84.6%, p = 0.02) in the delayed removal group.
The PAINESD score was published in 2015 as a potential predictor of acute hemodynamic collapse during VT ablation [9]. In our cohort, the PAINESD risk score ranged from 9 to 31 points with 12 (17.4%) patients having a low-moderate risk score of 9 to 14 points, and the other 57 patients (82.6%) had a high risk score ≥ 15 points. Compared with patients in the early removal group, the PAINESD risk score was higher in the delayed removal group (17.9 ± 4.9 vs. 21.7 ± 5.3, p = 0.004), and the percentage of patients with risk score ≥ 15 points was also significantly higher (76.7% vs. 92.3%, p = 0.04) (Table 1). However, regression analysis revealed that the PAINESD risk score ≥ 15 had no association with the delayed removal of pLVAD (OR = 0.28, 95% CI, 0.06–1.37, p = 0.12) or with the 90-day mortality (HR = 1.50, 95% CI, 0.34–6.70, p = 0.60) (Tables 3 and 5).
Although left to operator discretion, there was a higher number of patients with an Impella CP device implanted in the delayed removal group (17/26, 65.4% vs 7/43, 16.3%, p < 0.01). This variable was also not associated with delayed pLVAD removal (HR = 0.75, 95% CI, 0.27–2.12, p = 0.59) or 90-day mortality (HR = 1.97, 95% CI 0.69–5.63, p = 0.20) (Tables 3 and 5).
Regarding procedure-related parameters, all patients had endocardial ablation, and 6 had additional epicardial ablation. Regions of scar and/or VT location targeted for ablation were septal (n = 16), LV inferior wall (n = 26), LV lateral wall (n = 9), LV anterior wall (n = 8), LV apex (n = 6), RV (n = 1), or no endocardial scar (n = 3). There was no difference of procedure duration (331.1 ± 104.1 vs. 380.7 ± 116.8 min, p = 0.0717), time in sustained VT (26.9 ± 33.6 vs. 36.2 ± 35.0 min, p = 0.40), number of VT induced [(2.0 ± 1.5) vs. (2.9 ± 1.6), p = 0.07], and patients with a VT termination via ablation (14/43, 35.9% vs. 7/26, 31.8%, p = 0.75) between the early and delayed removal groups. VT was induced during the ablation procedure in 45/69 (65.2%) patients without difference between the early and delayed removal groups (26/43, 60.4% vs. 19/26, 73.1%, p = 0.14). Ventricular fibrillation was induced in 9/69 (13%) patients, with a higher incidence in the delayed removal group than in the early removal group (7/26, 26.9% vs. 2/43, 4.7%, p = 0.007) (Table 2).
3.2 Factors associated with the delayed removal of pLVAD
Delayed removal of pLVAD occurred in 26 (37.7%) patients. Univariate analysis revealed that delayed removal of pLVAD was associated with the presence of VT storm (OR = 34.72, 95% CI, 4.30–280.33; p = 0.001), LVEF < 25% (OR = 3.95, 95% CI, 1.16–13.48; p = 0.03), and VF induced during the procedure (OR = 9.25, 95% CI, 1.71–50.0; p = 0.01) (Table 3). Despite a higher percentage of patients in the delayed removal group with a PAINESD risk score ≥ 15, univariate analysis did not show a significant association with the delayed removal of pLVAD (OR = 0.28, 95% CI, 0.06–1.37, p = 0.12) (Table 3).
Multivariate analysis including LVEF <25%, creatinine ≥ 1.5 mg/dL, VT storm, procedure duration, and VF induced during ablation procedure revealed that the presence of VT storm before the procedure was associated with delayed removal of pLVAD (OR = 67.02, 95% CI, 4.79–938.68; p = 0.002) (Table 4).
3.3 The impact of delayed removal of pLVAD on mortality
At 90-day follow-up after VT ablation, 14/69 (20.3%) patients died within 90 days. The death events mostly happened in the first 2 weeks after the ablation procedure (78.6%, 11/14). Compared with patients in the early removal group, the 90-day mortality rate was significantly higher in the delayed removal group (13/26, 50% vs. 1/43, 2.3%; log-rank p < 0.001; Fig. 1). The cause of death in the vast majority of patients was progressive cardiogenic shock/refractory heart failure (n = 11 delayed removal, n = 1 early removal). Two patients developed refractory ventricular tachycardia/fibrillation which led to multi-system organ failure. Within the delayed removal group, there was no difference in the death rate between patients who had Impella™ removal less than 72 h and those over 6 days [(6/15, 40%) vs. (7/11, 63%), p = 0.43]. The mortality in patients without change of device was 6/14 = 42.8% compared with those with change of device of 7/12 = 58.3%. There was no association of change of devices and 90-day mortality (p = 0.695). Univariate Cox proportional hazard regression revealed the delayed removal of pLVAD was the only predictor of 90-day mortality (HR = 25.56, 95% CI, 3.33–196.23; p = 0.002) (Table 5).
Kaplan-Meier survival curve of the patients with structural heart disease undergoing catheter ablation of ventricular tachycardia under the support of percutaneous left ventricular assist device (pLVAD). Patients with pLVAD removed < 24 h had a significant higher probability of survival than those removed ≥ 24 h (p < 0.001) in 90 days after the ablation procedure
4 Discussion
The major findings of this study were (1) prolonged (≥ 24 h) pLVAD use for patients undergoing VT ablation associated with an increased 90-day mortality, (2) the main predictors of prolonged pLVAD use included VT storm and low LVEF (< 25%), and (3) intra-procedural induction of ventricular fibrillation was associated with prolonged pLVAD use post ablation on univariate analysis.
Percutaneous LVAD support has been described to manage patients undergoing high-risk coronary interventions and to support patients in cardiogenic shock [10, 11]. Initial studies described the role of Impella™ support during VT ablation allowing for a greater time in VT for patients which allowed for a greater number of VT to be terminated during ablation [4]. Subsequent studies comparing pLVAD with IABP as well as conventional substrate-based mapping revealed similar findings of more time of hemodynamically tolerated VT and more VT termination via ablation [3, 6]. Based on these and other studies, pLVAD use has become a class II (A or B) indication for hemodynamic support during mapping of VT and/or prevention of acute hemodynamic collapse based on the 2019 Expert Consensus Statement on Ablation of Ventricular Arrhythmias [8].
When considering timing of removal of pLVAD post ablation, general clinical practice is to remove the support device either immediately post procedure or soon thereafter. To date, no studies have specifically assessed outcomes based on pLVAD removal. Given that most patients undergoing pLVAD insertion tend to have lower LVEF and multiple comorbidities, occasionally, it may be felt that prolonged pLVAD use post ablation may allow for recovery of acute heart failure post ablation, aid in diuresis, and potentially reduce hospitalization days [12]. Our study suggests that prolonged pLVAD use (≥ 24 h) post ablation is associated with increased 90-day mortality. Muser et al. assessed the role of pLVAD insertion for high-risk patients undergoing VT ablation [7]. In this propensity-matched analysis, 75 patients who underwent pLVAD insertion were compared with a matched 75 patients without pLVAD insertion. Within this study, 3 patients had prolonged pLVAD post ablation of > 24 h. One patient warranted this for a vascular complication while the other two patients died due to prolonged hemodynamic instability. Although a limited number of patients, the prolonged pLVAD was associated with poor outcomes. Reddy et al. described a series of patients undergoing VT ablation and compared outcomes with those receiving IABP versus Impella™ support. In this study, patients had pLVAD support post procedure on average of 4 ± 12 h [3]. Aryana et al. described a retrospective experience comparing 68 patients undergoing VT ablation with and without pLVAD. The composite endpoint of 30-day rehospitalization rates, 90-day mortality, recurrent ICD therapies, and repeat ablation was lower in those with pLVAD insertion compared with non-pLVAD patients (12% vs 35% (p = 0.043) [13]. In this study, all patients had pLVAD removed immediately post procedure. These experiences of limited time of pLVAD support post ablation may further highlight that timing of pLVAD removal could be a marker for patient outcomes.
Unlike prior studies, our study had a higher percentage of patients with prolonged pLVAD support (37.7%). Factors associated with prolonged pLVAD were pre-procedure VT storm, LVEF < 25%, and VF induction during ablation. Multivariate regression analysis revealed VT storm associated with prolonged pLVAD insertion. The reason for prolonged pLVAD support was typically for a gradual weaning of the device post ablation for hemodynamic optimization. Given that the factors associated with prolonged support were VT storm, severely depressed LVEF and VF during the procedure, it may identify patients with a poor prognosis with less hemodynamic reserve even despite hemodynamic support. Our findings are consistent with prior studies noting severely depressed LVEF and VT storm to be associated with acute hemodynamic collapse and/or increased mortality [3, 6, 9]. Further, although no differences within the pLVAD removal groups, the average procedure time in the prolonged pLVAD group was noted to be 380 min. Yu et al. described an institutional experience of 148 patients revealing prolonged VT ablation procedure duration correlated to increased in-hospital mortality [14]. This retrospective study showed an increased level of mortality risk with each hour to the procedure over3 h. Additionally, VT storm prior to the procedure was associated with in-hospital mortality on multivariate analysis, which was similar to the findings presented in our cohort.
In clinical practice, pLVAD is often used for hemodynamic support without intention of mapping during VT. With pLVAD support, however, if VT is induced (through programmed stimulation or inadvertently), operators may consider mapping while in VT given the hemodynamic support. In our cohort, the average time in VT was 36 min. Muser et al. described a 7% incidence of hemodynamic decompensation despite pre-emptive pLVAD use for VT ablation in a propensity-matched cohort [7]. It may be that certain patients may do poorly after the procedure given the prolonged time in VT despite hemodynamic support. Therefore, despite pLVAD support, mapping of a VT in patients with a planned substrate-based ablation should be carefully considered and perhaps not prolonged in high-risk patients.
Although small numbers, there was no difference in mortality rates among patients with pLVAD < 72 h or > 6 days. This suggests that even a shorter duration (24–72 h) pLVAD time in order to improve hemodynamics/filling pressures, etc. could be just as high risk for short-term mortality. It may be that aggressive heart failure management guided by pLVAD invasive parameters may not be warranted and potentially harmful. This could be viewed as an extension of prior studies which have shown increased adverse events, including mortality, with the use of pulmonary artery catheters in heart failure management [15, 16].
Delayed removal of pLVAD post VT ablation was an independent predictor of 90-day mortality in our cohort. Recent retrospective studies have assessed for predictors of mortality post VT ablation. Vergara and colleagues published a scoring system to predict mortality risk based on a large, multicenter retrospective review of 1251 patients undergoing VT ablation. Severely depressed LVEF and VT storm and prior ablation were the best predictors of mortality [17]. Our findings of severely depressed LVEF (< 25%) and VT storm being associated with prolonged pLVAD support, which was a predictor of mortality, are consistent with this published scoring system. Santangeli et al. in 2015 published predictors of early mortality (< 31 days) post VT ablation based on a retrospective, multicenter review of 2061 patients. The study revealed depressed LVEF, CKD, electrical storm, and unmappable VT to be associated with early mortality in this patient population [18]. Our study suggests that even with hemodynamic support, certain high-risk groups warrant collaboration with heart failure specialists and potential ablation be performed in centers with advanced heart failure therapies.
Beyond VT ablation, prolonged pLVAD support in the setting of complex coronary interventions has recently been studied. Davila et al. reviewed the cVAD (catheter-based ventricular assist device) registry of 507 patients undergoing prophylactic Impella™ insertion for coronary interventions. Of the cohort, 43 patients had prolonged support post procedure (11.4 ± 16.8 h). Compared with the only procedural support cases, patients with prolonged support post procedure had an increased in-hospital mortality (11.6% vs 1.9%, p = 0.004) [19]. Further, patients with prolonged pLVAD had increased bleeding complications, transfusions, and vascular access site complications. This large registry experience further highlights the potential limitations and complications associated with prolonged pLVAD use post procedure.
5 Limitations
This retrospective study is from a single institutional experience and may have reflected local practice patterns. Patients selected for pLVAD support were based on clinical discretion, although the patient demographics are consistent with a high-risk patient population. Although no differences related to outcomes were noted between groups based on type of pLVAD, a larger sample size could have altered the results. Third, timing of removal of pLVAD was also based on clinical judgment and may have varied among operators. Outside of mean arterial pressure monitoring, cerebral oximetry was not used consistently. All patients underwent a trans-septal approach only which could have limited mapping in a subset of patients. This added variable may have altered procedural approaches. Due to limited numbers, further predictive risk stratification of mortality based on timing of removal within in the delayed removal group was precluded.
6 Conclusions
The delayed removal (≥ 24 h) of pLVAD after VT ablation was a predictor of 90-day mortality in patients undergoing VT ablation. Factors associated with prolonged pLVAD use were the presence of VT storm, LVEF < 25%, and VF induced during VT ablation. Further studies are warranted to refine the role of hemodynamic support during and after VT ablation.
Abbreviations
- ACEI/ARB:
-
Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker
- ECMO:
-
Extracorporeal mechanical oxygenation
- pLVAD:
-
Percutaneous left ventricular assist device
- IABP:
-
Intra-aortic balloon pump
- LAVA:
-
Local abnormal ventricular activity
- LVEF:
-
Left ventricular ejection fraction
- NYHA:
-
New York Heart Association
- VT:
-
Ventricular tachycardia
- VF:
-
Ventricular fibrillation
References
Stevenson WG, Wilber DJ, Natale A, et al. Irrigated radiofrequency catheter ablation guided by electroanatomic mapping for recurrent ventricular tachycardia after myocardial infarction: the multicenter thermocool ventricular tachycardia ablation trial. Circulation. 2008;118:2773–82.
Tung R, Vaseghi M, Frankel DS, et al. Freedom from recurrent ventricular tachycardia after catheter ablation is associated with improved survival in patients with structural heart disease: an international VT ablation center collaborative group study. Heart Rhythm. 2015;12:1997–2007.
Reddy YM, Chinitz L, Mansour M, et al. Percutaneous left ventricular assist devices in ventricular tachycardia ablation: multicenter experience. Circ Arrhythm Electrophysiol. 2014;7:244–50.
Miller MA, Dukkipati SR, Mittnacht AJ, et al. Activation and entrainment mapping of hemodynamically unstable ventricular tachycardia using a percutaneous left ventricular assist device. J Am Coll Cardiol. 2011;58:1363–71.
Kusa S, Miller MA, Whang W, et al. Outcomes of ventricular tachycardia ablation using percutaneous left ventricular assist devices. Circ Arrhythm Electrophysiol. 2017;10.
Turagam MK, Vuddanda V, Atkins D, et al. Hemodynamic support in ventricular tachycardia ablation: an international VT ablation center collaborative group study. JACC Clin Electrophysiol. 2017;3:1534–43.
Muser D, Liang JJ, Castro SA, et al. Outcomes with prophylactic use of percutaneous left ventricular assist devices in high-risk patients undergoing catheter ablation of scar-related ventricular tachycardia: a propensity-score matched analysis. Heart Rhythm. 2018;15:1500–6.
Cronin EM, Bogun FM, Maury P, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. J Arrhythm. 2019;35:323–484.
Santangeli P, Muser D, Zado ES, et al. Acute hemodynamic decompensation during catheter ablation of scar-related ventricular tachycardia: incidence, predictors, and impact on mortality. Circ Arrhythm Electrophysiol. 2015;8:68–75.
O'Neill WW, Kleiman NS, Moses J, et al. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation. 2012;126:1717–27.
Kar B, Gregoric ID, Basra SS, Idelchik GM, Loyalka P. The percutaneous ventricular assist device in severe refractory cardiogenic shock. J Am Coll Cardiol. 2011;57:688–96.
Aryana A, d'Avila A, Cool CL, et al. Outcomes of catheter ablation of ventricular tachycardia with mechanical hemodynamic support: an analysis of the Medicare database. J Cardiovasc Electrophysiol. 2017;28:1295–302.
Aryana A, Gearoid O'Neill P, Gregory D, et al. Procedural and clinical outcomes after catheter ablation of unstable ventricular tachycardia supported by a percutaneous left ventricular assist device. Heart Rhythm. 2014;11:1122–30.
Yu R, Ma S, Tung R, et al. Catheter ablation of scar-based ventricular tachycardia: relationship of procedure duration to outcomes and hospital mortality. Heart Rhythm. 2015;12:86–94.
Connors AF Jr, Speroff T, Dawson NV, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators JAMA. 1996;276:889–97.
Binanay C, Califf RM, Hasselblad V, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294:1625–33.
Vergara P, Tzou WS, Tung R, et al. Predictive score for identifying survival and recurrence risk profiles in patients undergoing ventricular tachycardia ablation: the I-VT score. Circ Arrhythm Electrophysiol. 2018;11:e006730.
Santangeli P, Frankel DS, Tung R, et al. Early mortality after catheter ablation of ventricular tachycardia in patients with structural heart disease. J Am Coll Cardiol. 2017;69:2105–15.
Davila CD, Sharma S, Krishnamoorthy P et al. Prevalence and clinical correlates of extended mechanical support in patients undergoing high-risk percutaneous coronary intervention in current clinical practice: insights from the cVAD registry. Cardiovasc Revasc Med 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local institutional review board.
Conflict of interest
Nilesh Mathuria—Research grant Abiomed (funds from this grant used to maintain patient database); no other author conflicts of interest to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Q., Pollet, M., Mehta, A. et al. Delayed removal of a percutaneous left ventricular assist device for patients undergoing catheter ablation of ventricular tachycardia is associated with increased 90-day mortality. J Interv Card Electrophysiol 62, 49–56 (2021). https://doi.org/10.1007/s10840-020-00875-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00875-y