Abstract
Purpose of review
Left ventricular assist device (LVAD) implantation is a well-known treatment option for patients with advanced heart failure refractory to medical therapy and is recognized both as bridge to transplant and a destination therapy. The risk of ventricular arrhythmias (VAs) is common after LVAD implantation. We review the pathophysiology and recent advances in the management of VA in LVAD patients.
Recent findings
VAs are most likely to occur in the early post-operative periods after LVAD implantation and a prior history of VA is the most important risk factor. Post-LVAD VAs are usually well tolerated with less morbidity and decreased risk of sudden cardiac death. However, risk of right heart failure in the setting of persistent VAs is being increasingly recognized. The mechanisms of post-LVAD VAs may vary depending on the time from LVAD implantation. Electrical remodeling may play an important role in the immediate post-implant phase. Preexisting myocardial scar and to a lesser extent mechanical irritation from the LVAD cannula are important in the later phases. Most LVAD patients have a previously placed implantable cardioverter-defibrillator (ICD). The benefit of implanting a new ICD in LVAD patients is unknown and should be individualized. For ICD programming, a conservative strategy with higher detection zones and prolonged time to detection is usually recommended aiming to minimize ICD shocks. More aggressive programming is appropriate if the VA results in hemodynamic instability. Antiarrhythmic drugs including amiodarone, mexiletine, and beta blockers are usually the first-line therapy for VAs. Catheter ablation has been shown to be safe and effective in LVAD recipients with recurrent VAs not responsive to antiarrhythmic drugs.
Summary
LVAD-related VA is most frequently reentrant secondary to myocardial scar and usually well tolerated. Management options include antiarrhythmic drugs and catheter ablation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its first introduction in 1969—when the world’s first artificial heart was placed [1]—a left ventricular assist device (LVAD) has emerged to become a well-established mode of treatment in patients with end stage or advanced heart failure (New York Heart Association class IIIB or IV symptoms) refractory to standard medical therapy [2]. It has shown survival benefit with decreased morbidity and overall improvement in quality of life [3, 4]. LVAD was first introduced as a bridge to transplant (BTT). However, only a minority of advanced heart failure patients were found eligible for heart transplant. Now, LVAD is also well recognized as destination therapy (DT) since its approval for this in January 2010, with approximately 50% of implants in the USA currently for this indication [1]. The first generation introduced was a pulsatile pump which evolved to become a continuous flow pump in the second- and third-generation LVADs.
Ventricular arrhythmias in LVAD patients
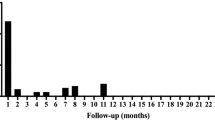
It is now widely known that LVAD implantation is associated with increased risk of arrhythmias particularly ventricular arrhythmias (VAs). VAs occur more frequently in the early post-operative period, principally in the first 30 days post-implantation [5•, 6, 7]. The reported incidence of VA in LVAD patients is between 22 and 59% [6, 8, 9]. This wide range in the reported incidence is likely due to variability in the patient population and implantable cardioverter-defibrillator (ICD) programming. VAs can occur de novo after LVAD implantation without a prior history of VAs. However, previous history of VA is reported as one of the main predictors among others like ischemic heart disease [6, 7, 9,10,11]. Also, the type of the implanted assist device plays a role with VAs being more recognized in continuous flow LVAD (CF-LVAD) [8].
The majority of LVAD patients have good tolerability to VAs with decreased morbidity, mild symptoms, and considerably decreased risk of sudden cardiac death compared with those without a LVAD [12, 13]. This is even more pronounced in CF-LVAD when the outflow is less affected by the native heart preload [14, 15]. The most common symptoms are palpitations, pre-syncope, and fatigue, but syncope is rare. This being said, LVAD inflow can be affected if there is underlying pulmonary hypertension or right ventricular (RV) dysfunction that impairs left ventricular (LV) filling. Some patients can experience significant symptoms, mainly of right heart failure, ICD shocks, and hemodynamic instability, affecting their quality of life. There is also potential for RV thrombosis due to lack of contraction. Cardiac arrest, however, is rarely seen [16]. Concerns about the association between post-LVAD VAs and mortality was raised and reported in few studies. In some studies, a significant increase in mortality was described in the first month after LVAD implantation [17, 18] with preexisting VAs as a major risk for mortality [19•]. However, this association was not confirmed in another study [20]. It is also unclear if the VA has a causal effect on mortality or if it is a marker of cardiac dysfunction. LVAD-associated VAs are also recognized to cause increased financial burden with increased use of resources from multiple hospital readmissions [21, 22].
Mechanisms of VA in LVAD patients
The mechanism of VA may vary by the underlying heart disease, time interval from LVAD implantation, and patient characteristics. In the immediate post-implant phase, the left ventricle is unloaded, resulting in structural and electrophysiologic remodeling. This leads to a shortened QRS duration and prolonged QT interval, predisposing to VA [23]. The early remodeling also represents a stage of electrical instability and dispersion of repolarization. Increased QT after LVAD implantation was reported to be associated with 3-fold higher incidence of post-operative VA [24]. Electrolyte imbalance, inotropic drugs, changes in ion channel expression, and calcium handling post-operatively can also predispose to VAs [22]. Thereafter, weeks or months post-implantation, electrophysiological remodeling corresponds to the decreased risk of VAs [23].
In the later phases, preexisting myocardial scar plays the most important role in arrhythmogenesis. The most common underlying mechanism is re-entry, but enhanced and triggered automaticity can also be seen. Mechanical causes of VAs that are unique to the LVAD population have also been reported. These include reentrant ventricular tachycardia (VT) involving the apical scar created by insertion of the inflow cannula. Also, the inflow cannula can impinge on the myocardium resulting in VT that may sometimes be positional. Finally, mismatch between the VAD inflow and outflow can result in greater unloading of the LV compared with the venous return. This can cause a suction effect, small LV cavity size, and direct contact of the inflow cannula with the myocardium leading to VT [25, 26]. Echocardiography can help recognize LVAD “suck down” which can be addressed by reducing the rotational speed of the pump and increasing preload (fluid resuscitation). Although mechanical causes of VA are uncommon, their recognition is critical since they are usually not responsive to antiarrhythmic drugs. In a systematic review of VA mechanism in patients undergoing ablation, 90% were related to scar related re-entry, with cannula-related VT and focal VT accounting for the rest.
ICD programming in LVAD
Given advanced heart failure in LVAD patients, concomitant LVAD and ICD use is very common. In fact, the majority of patients with LVAD already have an ICD in place. Among those who do not, post-LVAD ICD placement remains of questionable benefit especially in the current generation of CF-LVAD [12]. The most recent American Heart Association (AHA) scientific statement concludes no sufficient data is available to declare a survival advantage from ICD in LVAD patients with the majority of the available data suggesting no survival benefit in patients with CF-LVAD [27••]. The 2017 AHA/American College of Cardiology (ACC)/Heart Rhythm Society (HRS) guidelines on VA give it a class IIa recommendation [28]. The decision to implant an ICD post-LVAD should be individualized, with greater consideration given to patients with hemodynamic instability during VA.
When it comes to tachyarrhythmia programming, given sustained VA’s associated with LVAD are usually well tolerated, conservative programming strategy is recommended aiming to minimize ICD shocks. ICD shocks that occur in conscious LVAD patients can have significant adverse psychological impact and should be avoided. The following general principles are applicable in patients with well-tolerated VAs:
- 1.
Programming a high VF zone (≥ 220 bpm) with prolonged intervals to detection.
- 2.
Multiple rounds of ATP can be programmed in the VF zone to increase the probability of painless termination of monomorphic VT or spontaneous termination of VA prior to triggering a shock. Current ICDs do not allow programming “off” shocks in the VF zone.
- 3.
A VT zone can be programmed, and the cut-off individualized to the patient’s prior VA characteristics. Prolonging the time to detection to the maximum allowed by the device will allow non-sustained VAs to terminate and prevent unnecessary therapies.
- 4.
Multiple rounds of ATP should also be programmed in the VT zone for reasons noted above. One caveat, however, is potential for acceleration of the VA following aggressive ATP resulting in rapid VAs leading to hemodynamic instability or shocks in a small proportion of patients. Aggressive ATP therapy should be avoided in patients who have previously demonstrated acceleration of VA.
- 5.
The VT zone can be programmed without shocks if the VA is hemodynamically stable. If ATP is not effective, an elective cardioversion can be considered under sedation.
More aggressive programming is appropriate if the VA results in hemodynamic instability.
Additional considerations include measures to increase battery longevity to minimize need for generator change with its attendant risk for infection. Given the uncertain utility of cardiac resynchronization therapy in LVAD patients, consideration can be given to turning off LV pacing to conserve battery. However, clinical data with regard to best practice are sparse.
Some LVAD patients might prefer programming their ICD off to minimize painful ICD shocks. This is based on the reduced risk of cardiac death from VAs post-LVAD. Such decision will need to be made in a shared fashion with the patient and the family on a case-by-case basis.
Management of VAs in LVAD
Medical management
As discussed previously, VAs are usually well tolerated by LVAD patients. Although antiarrhythmics can help prevent hemodynamic instability in LVAD patients with VAs, their use remains of questionable benefit with limited data guiding the medical therapy in this population [7, 20, 22].
Most LVAD patients, unless contraindicated, are usually already on the maximum tolerated dose of beta blockers. There are conflicting data about the benefit of initiating beta blockers after LVAD implantation. While one retrospective study showed significant association between increased risks of VAs and nonuse of beta blockers after LVAD placement [22], this was contradicted by a prospective study that revealed no association [7]. It is however reasonable to maximize beta blocker therapy in patients with VAs.
In the acute setting, intravenous amiodarone, lidocaine, or procainamide is usually advised. Chronically, oral amiodarone is frequently used to prevent recurrence of VA. In one randomized controlled study, amiodarone in combination with beta blocker reduced the risk of both appropriate and inappropriate ICD shock [29]. Although one small study showed significant arrhythmia-free survival with amiodarone used for secondary prevention [20], another multi-center study revealed amiodarone is independently associated with increased mortality [30]. There are also concerns regarding its use in cardiac transplant recipients. Amiodarone use in patients awaiting cardiac transplant is associated with increased one-year mortality after transplant. In conclusion, amiodarone use should always be balanced between benefits and side effects or drug interaction. Sotalol in one study of non-LVAD patients with VA significantly reduced the risk of any shock or death by 48% and is a potential option for patients with LVAD also [31]. Mexiletine can be added for breakthrough VA despite chronic use of amiodarone or as an alternative if amiodarone is not tolerated. It can also be used for adequate acute control in patients with successful use of lidocaine [1].
Ablation therapy
Catheter ablation for VAs in LVAD recipients is usually considered in recurrent VAs leading to either hemodynamic instability or recurrent ICD shocks despite antiarrhythmic drugs. VT storm is a common indication for ablation. Patients with slow hemodynamically tolerated VT should also be considered for ablation if there is concern for VA-induced RV failure or thrombosis.
Several small retrospective cohort studies [25, 32,33,34,35,36,37,38] have described techniques and outcomes of VT ablation in LVAD patients, but the collective experience remains limited. In a systematic review of the published literature, Anderson et al. [39•] reported VT ablation outcomes in 110 patients. One-third of ablations were performed for VT storm. Acute procedural success defined as non-inducible clinical VT was achieved in 78%. Two-thirds of patients were non-inducible for any VT at the end of the procedure. Major complications occurred in 5.5% including cerebrovascular accident, vascular access–related complications, and cardiogenic shock. There were no reports of pump thrombosis or catheter entrapment [36]. The rate of major complications is comparable with that of VT ablation in non-LVAD patients with structural heart disease.
During long-term follow-up, VT recurrence occurred in approximately 40% and repeat ablation was performed in 10%. However, a significant decrease in ICD shocks was observed. While there is insufficient data to assess survival benefit, catheter ablation can be useful to reduce morbidity associated with VT and to stabilize patients as a bridge to transplant [27••].
Technical considerations
The preferred access to the LV in LVAD patients is via the trans-septal approach. The retrograde aortic approach that was used in one-third of the reported cases may be more challenging due to low flow and poor opening of the aortic valve. [39•] Retrograde aortic access is not feasible if the aortic valve was oversewn during LVAD placement. Careful review of the operative report and echocardiogram is essential to recognize this. Percutaneous epicardial access is challenging if not impossible in these patients. In patients with hemodynamically significant epicardial VTs, surgical epicardial access with limited thoracotomy can be considered.
The hemodynamic stability afforded by the LVAD allows arrhythmia induction and mapping in most cases. Anderson et al. [39•] reported the use of activation or entrainment mapping in 60% of cases, substrate only mapping in 20%, and a combination of these in the other 20%. This contrasts with non-LVAD patients in whom ablation is guided predominantly by the substrate due to hemodynamic instability during VT.
Careful monitoring of catheter position using intracardiac echocardiography and fluoroscopy is essential to avoid catheter entrapment inside LVAD. The risk of this complication is low but can occur if the catheter is placed deep in the rotating impeller. In the immediate post-implant period, caution should be exercised while mapping or ablating around fresh suture lines and is best avoided. Electromagnetic interference to magnetic guided mapping systems has been reported but is rarely significant enough to affect the outcome of the procedure. In our experience, magnetic interference that prevents acquisition of points and spatial localization of the catheter may occur during mapping at the apex in close proximity to the inflow cannula. The newer generation HeartMate 3 device has been reported to cause high-frequency noise on surface ECG which can pose challenges to pace mapping [39•]. Temporary reduction of pump speed can be tried in cases with electromagnetic interference but is not uniformly successful in eliminating this problem. However, use of purely impedance based mapping systems will eliminate electromagnetic interference.
Monitoring of hemodynamics is critical during the ablation. Commonly used targets for blood pressure are not applicable to this patient population. Hence, in addition to close monitoring of mean arterial pressure, pump-related parameters including rotations per minute and flow should be continuously monitored in collaboration with a heart failure LVAD specialist. Additional monitoring of markers of end-organ perfusion such as urine output, serum lactate, and pH is useful. Central venous pressure monitoring can also help identify and treat RV dysfunction and fluid overload.
Ablation during LVAD implantation
In order to limit post-operative VA in LVAD recipients and given the challenges of post-LVAD VA ablation, surgical ablation during the time of LVAD implantation is sometimes considered. Intraoperative epicardial and endocardial cryoablation in one study was found to be safe, leading to significantly reduced post-operative arrhythmia burden especially in patients with history of recurrent preoperative VA [40]. Another study with 2 patients found an increased risk of thrombosis with endocardial ablation and recommended surgical VT cryoablation to be limited only to epicardial ablation during LVAD placement [41]. In conclusion, the safety and efficacy of this preemptive approach remains uncertain warranting further evaluation.
Conclusion
Ventricular arrhythmias are common after LVAD implantation, with peak incidence in the immediate post-operative period. Most VAs are well tolerated in the context of an LVAD, and ICD programming must be revisited after LVAD implantation to minimize unnecessary shocks. Catheter ablation is feasible with good acute success rate for treatment of VT non-responsive to antiarrhythmic drugs, though recurrence is common.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nakahara S, Chien C, Gelow J, Dalouk K, Henrikson CA, Mudd J, et al. Ventricular arrhythmias after left ventricular assist device. Circ Arrhythm Electrophysiol. 2013;6(3):648–54.
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to update the 2001 guidelines for the evaluation and management of heart failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112(12):e154–235.
Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361(23):2241–51.
Mehra MR, Naka Y, Uriel N, Goldstein DJ, Cleveland JC Jr, Colombo PC, et al. A fully magnetically levitated circulatory pump for advanced heart failure. N Engl J Med. 2017;376(5):440–50.
• Ziv O, et al. Effects of left ventricular assist device therapy on ventricular arrhythmias. J Am Coll Cardiol. 2005;45(9):1428–34 Landmark manuscript that defined the natural history and risk factors for VA after LVAD implantation.
Miller LW, Pagani FD, Russell SD, John R, Boyle AJ, Aaronson KD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357(9):885–96.
Andersen M, Videbæk R, Boesgaard S, Sander K, Hansen PB, Gustafsson F. Incidence of ventricular arrhythmias in patients on long-term support with a continuous-flow assist device (HeartMate II). J Heart Lung Transplant. 2009;28(7):733–5.
Cao X, Haft J, Dyke DB, Wright S, Pagani FD, Aaronson KD. Increased incidence of ventricular tachycardia following left ventricular assist device implantation with continuous flow rotary pumps. J Card Fail. 2006;12(6):S45.
Cantillon DJ, Tarakji KG, Kumbhani DJ, Smedira NG, Starling RC, Wilkoff BL. Improved survival among ventricular assist device recipients with a concomitant implantable cardioverter-defibrillator. Heart Rhythm. 2010;7(4):466–71.
Arai H, et al. Importance of ventricular arrhythmias in bridge patients with ventricular assist devices. ASAIO Trans. 1991;37(3):M427–8.
Oswald H, Schultz-Wildelau C, Gardiwal A, Lüsebrink U, König T, Meyer A, et al. Implantable defibrillator therapy for ventricular tachyarrhythmia in left ventricular assist device patients. Eur J Heart Fail. 2010;12(6):593–9.
Oz MC, Rose EA, Slater J, Kuiper JJ, Catanese KA, Levin HR. Malignant ventricular arrhythmias are well tolerated in patients receiving long-term left ventricular assist devices. J Am Coll Cardiol. 1994;24(7):1688–91.
Sims DB, et al. Twelve hours of sustained ventricular fibrillation supported by a continuous-flow left ventricular assist device. Pacing Clin Electrophysiol. 2012;35(5):e144–8.
Baldwin ACW, Gemmato CJ, Sandoval E, Cohn WE, Morgan JA, Frazier OH. Tolerance of sustained ventricular fibrillation during continuous-flow left ventricular assist device support. Tex Heart Inst J. 2017;44(5):357–60.
Kadado AJ, Akar JG, Hummel JP. Arrhythmias after left ventricular assist device implantation: incidence and management. Trends Cardiovasc Med. 2018;28(1):41–50.
Moroney DA, Swartz MT, Reedy JE, Lohmann DP, McBride L, Pennington DG. Importance of ventricular arrhythmias in recovery patients with ventricular assist devices. ASAIO Trans. 1991;37(3):M516–7.
Brenyo A, et al. Risk of mortality for ventricular arrhythmia in ambulatory LVAD patients. J Cardiovasc Electrophysiol. 2012;23(5):515–20.
Genovese EA, Dew MA, Teuteberg JJ, Simon MA, Kay J, Siegenthaler MP, et al. Incidence and patterns of adverse event onset during the first 60 days after ventricular assist device implantation. Ann Thorac Surg. 2009;88(4):1162–70.
• Makki N, et al. Meta-analysis of the relation of ventricular arrhythmias to all-cause mortality after implantation of a left ventricular assist device. Am J Cardiol. 2015;116(9):1385–90 In this metaanalysis, Makki et al. reported that VA is an independent risk factor for mortality in LVAD patients.
Raasch H, Jensen BC, Chang PP, Mounsey JP, Gehi AK, Chung EH, et al. Epidemiology, management, and outcomes of sustained ventricular arrhythmias after continuous-flow left ventricular assist device implantation. Am Heart J. 2012;164(3):373–8.
Ambardekar AV, Allen LA, Lindenfeld JA, Lowery CM, Cannon AP, Cleveland JC Jr, et al. Implantable cardioverter-defibrillator shocks in patients with a left ventricular assist device. J Heart Lung Transplant. 2010;29(7):771–6.
Refaat M, et al. Ventricular arrhythmias after left ventricular assist device implantation. Pacing Clin Electrophysiol. 2008;31(10):1246–52.
Harding JD, Piacentino V III, Gaughan JP, Houser SR, Margulies KB. Electrophysiological alterations after mechanical circulatory support in patients with advanced cardiac failure. Circulation. 2001;104(11):1241–7.
Harding JD, Piacentino V III, Rothman S, Chambers S, Jessup M, Margulies KB. Prolonged repolarization after ventricular assist device support is associated with arrhythmias in humans with congestive heart failure. J Card Fail. 2005;11(3):227–32.
Cantillon DJ, Bianco C, Wazni OM, Kanj M, Smedira NG, Wilkoff BL, et al. Electrophysiologic characteristics and catheter ablation of ventricular tachyarrhythmias among patients with heart failure on ventricular assist device support. Heart Rhythm. 2012;9(6):859–64.
Vollkron M, Voitl P, Ta J, Wieselthaler G, Schima H. Suction events during left ventricular support and ventricular arrhythmias. J Heart Lung Transplant. 2007;26(8):819–25.
•• Gopinathannair R, et al. Device therapy and arrhythmia management in left ventricular assist device recipients: a scientific statement from the American Heart Association. Circulation. 2019;139(20):e967–89 This scientific statement from the American Heart Association summarizes the current state of knowledge in the management of arrhythmias in LVAD patients.
Al-Khatib SM, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018;72(14):e91–e220.
Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES, et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC study: a randomized trial. Jama. 2006;295(2):165–71.
Gopinathannair R, Roukoz H, Bhan A, Ravichandran A, Ahmed MM, Familtsev D, et al. Cardiac resynchronization therapy and clinical outcomes in continuous flow left ventricular assist device recipients. J Am Heart Assoc. 2018;7(12):e009091.
Pacifico A, Hohnloser SH, Williams JH, Tao B, Saksena S, Henry PD, et al. Prevention of implantable-defibrillator shocks by treatment with sotalol. d,l-Sotalol Implantable Cardioverter-Defibrillator Study Group. N Engl J Med. 1999;340(24):1855–62.
Dandamudi G, Ghumman WS, Das MK, Miller JM. Endocardial catheter ablation of ventricular tachycardia in patients with ventricular assist devices. Heart Rhythm. 2007;4(9):1165–9.
Garan AR, Iyer V, Whang W, Mody KP, Yuzefpolskaya M, Colombo PC, et al. Catheter ablation for ventricular tachyarrhythmias in patients supported by continuous-flow left ventricular assist devices. ASAIO J. 2014;60(3):311–6.
Herweg B, et al. Clinical observations and outcome of ventricular tachycardia ablation in patients with left ventricular assist devices. Pacing Clin Electrophysiol. 2012;35(11):1377–83.
Hottigoudar RU, et al. Ventricular tachycardia ablation in patients with HeartMate II left ventricular assist devices: rhythm still matters in the bionic age. J Innov Card Rhythm Manage. 2011;2:537–47.
Moss JD, Flatley EE, Beaser AD, Shin JH, Nayak HM, Upadhyay GA, et al. Characterization of ventricular tachycardia after left ventricular assist device implantation as destination therapy: A Single-Center Ablation Experience. JACC Clin Electrophysiol. 2017;3(12):1412–24.
Sacher F, Reichlin T, Zado ES, Field ME, Viles-Gonzalez JF, Peichl P, et al. Characteristics of ventricular tachycardia ablation in patients with continuous flow left ventricular assist devices. Circ Arrhythm Electrophysiol. 2015;8(3):592–7.
Snipelisky D, et al. Effect of ventricular arrhythmia ablation in patients with Heart Mate II left ventricular assist devices: an evaluation of ablation therapy. J Cardiovasc Electrophysiol. 2017;28(1):68–77.
• Anderson RD, et al. Catheter ablation of ventricular tachycardia in patients with a ventricular assist device: a systematic review of procedural characteristics and outcomes. JACC Clin Electrophysiol. 2019;5(1):39–51 Anderson et al. provide an excellent review of outcomes of catheter ablation in LVAD patients. This manuscripts summarizes our aggregate experience with catheter ablation in this subset of patients.
Mulloy DP, Bhamidipati CM, Stone ML, Ailawadi G, Bergin JD, Mahapatra S, et al. Cryoablation during left ventricular assist device implantation reduces postoperative ventricular tachyarrhythmias. J Thorac Cardiovasc Surg. 2013;145(5):1207–13.
Casida JM, Combs P, Pavol MK, Hickey KT. Ready, set, go: how patients and caregivers are prepared for self-management of an implantable ventricular assist device. ASAIO J. 2018;64(6):e151–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Azza Ahmed, Mustapha Amin, Barry A. Boilson, and Ammar M. Killu each declare no potential conflicts of interest.
Malini Madhavan receives research funding from Bristol-Myers Squibb and Pfizer.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Arrhythmia
Rights and permissions
About this article
Cite this article
Ahmed, A., Amin, M., Boilson, B.A. et al. Ventricular Arrhythmias in Patients With Left Ventricular Assist Device (LVAD). Curr Treat Options Cardio Med 21, 75 (2019). https://doi.org/10.1007/s11936-019-0783-7
Published:
DOI: https://doi.org/10.1007/s11936-019-0783-7