Abstract
Purpose
Many centers perform catheter ablation for atrial fibrillation (AF) with periprocedural interruption of oral vitamin K antagonists. In this scenario, the optimal post-procedural anticoagulation strategy is still under debate. We sought to compare the incidence of major complications associated with post-procedural use of low molecular weight heparin (LMWH) versus unfractioned heparin (UFH) as a bridge to reinitiation of oral anticoagulation after an AF ablation procedure.
Methods
We retrospectively reviewed medical history data of all patients undergoing catheter ablation for AF at three Spanish referral centers between January 2009 and January 2014. A total of 702 patients were included in the analysis. We compared the incidence of major complications (a combination of major bleeding and thromboembolic events) between patients receiving UFH (291) and those receiving LMWH (411) after the procedure.
Results
The overall incidence of major complications was 4.1 %, including five thromboembolic events (0.7 %) and 24 major bleeding events (3.4 %), with no significant differences in patients treated with LMWH vs. UFH (2.9 vs. 4.1 %; P = NS). The presence of peripheral vascular disease emerged as the only independent predictor of major complications (adjusted odds ratio (OR) 9.1; confidence interval (CI) 95 % 1.7–49.3; P < 0.01).
Conclusions
Immediate post-procedural bridging with UFH or with LMWH are equally safe strategies in patients undergoing catheter ablation for AF in whom oral anticoagulation is interrupted for the procedure. Due to its greater simplicity of use, LMWH may be the preferred option. The presence of peripheral vascular disease is a potent predictor of major post-procedural complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Since its introduction to clinical practice in the late 1990s [1], radiofrequency ablation therapy (RFA) has become one of the cornerstones in the management of atrial fibrillation (AF). Despite its favorable safety profile, complications do occur [2, 3], and most clinically relevant complications fall under two categories: bleeding and thromboembolic events. Patients undergoing RFA for AF are under increased risk for thromboembolic events (TE) during and after the procedure. This increased risk justifies the widespread use of intra-procedural and post-procedural systemic anticoagulation in all patients as well as pre-procedural anticoagulation in most [3]. The need for anticoagulation in turn leads to increased bleeding risk, especially involving vascular access sites required for the procedure. An adequate balance between avoidance of TE and bleeding risk is thus needed. Increasingly, a strategy of uninterrupted oral anticoagulation with vitamin K antagonists is being pursued in patients undergoing RFA for AF [4–6]. Nonetheless, as many as 50 % of HRS/EHRA/ECAS Task Force members continue to use an interrupted oral anticoagulation approach [3], requiring bridging with heparin after the procedure until a target INR >2 has been achieved, and recent publications have cast doubts on the risks and benefits of the systematic use of an uninterrupted warfarin approach [7, 8]. Clear recommendations regarding the choice of unfractioned heparin (UFH) or low molecular weight heparin (LMWH) for this purpose are lacking in current guidelines [3, 9]. We sought to evaluate the relative merits of either type of anticoagulant in terms of risk of bleeding and thromboembolic complications in patients undergoing RFA for AF with an interrupted oral anticoagulation strategy. Additionally, we analyzed the impact of protamine administration for activated clotting time (ACT) normalization and prompt sheath extraction on the occurrence of both bleeding and thromboembolic complications in this patient population.
2 Material and methods
2.1 Patient population and AF ablation protocol
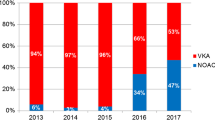
We retrospectively reviewed medical history data of all patients undergoing RFA for AF at three large referral centers (January 2009 to September 2014 for “center 1,” October 2011 to September 2014 for “center 2,” and November 2011 to September 2014 for “center 3”). As shown in Fig. 1, a total of 744 procedures were performed in the 3 participating institutions: 568 at center 1, 68 at center 2, and 108 at center 3. After excluding patients who received novel oral anticoagulant agents (N = 32) and 10 patients who for other reasons did not receive either UFH or LMWH, 702 patients were included in the analysis. Overall, the AF ablation protocol was similar in the 3 centers. Oral anticoagulation was withheld 3–5 days prior to the procedure and patients were bridged with full-dose subcutaneous low molecular weight heparin (enoxaparin 1 mg/kg bid) in the days leading up to the procedure, following interruption of oral vitamin K antagonists, with transesophageal echocardiography performed in all patients the day before the ablation. Patients taking antiplatelet agents prior to the procedure were given the last dose of the agent the night before the ablation. Procedures were performed under general anesthesia. Three femoral venous accesses were obtained in each patient, only the right groin was accessed, and either one or two long sheaths were used according to operator preference. Single transseptal puncture was achieved under fluoroscopic guidance. Transseptal sheaths were flushed with a bolus of heparinized saline and thereafter continuously flushed with an IV heparinized saline infusion. A duodecapolar circular mapping catheter (Optima®, St Jude Medical, or Lasso, Biosense-Webster) and a 3.5-mm open irrigated-tip RF ablation catheter (Navistar® Thermocool® or EZ Steer® Thermocool®, Biosense-Webster, Baldwin Park, CA) were advanced into the left atrium. Following 3D electroanatomical mapping of the left atrium, antral pulmonary vein isolation (PVI) was performed. Additional ablation lesions (roof line, mitral isthmus line, ablation of complex fractionated atrial electrograms) were delivered at the operator’s discretion.
2.2 Anticoagulation protocol
In all cases, oral vitamin K antagonists were interrupted before the procedure (INR < 1.5 on the day of the intervention). A heparin bolus (70–100 units/kg) was administered immediately before transseptal puncture, followed by continuous intravenous infusion, and an ACT target range of 300–350 ms was sought throughout the procedure. Two different immediate post-procedure anticoagulation strategies were used (Fig. 1):
-
UFH group: intravenous UFH was reinitiated 4–6 h after the procedure, with a target prothrombin time (PTT, monitored at 4-h intervals) of 50–70 ms, and discontinued the morning after the procedure. Oral anticoagulation was resumed 24 h after the procedure, with full-dose subcutaneous LMWH (1 mg/kg/12 h enoxaparin also initiated 24 h post-procedure) maintained until the INR was >2. This protocol was used in most cases in center 2 (N = 64) and prior to 2011 in center 1 (N = 227), adding up to a total of 291 patients.
-
LMWH group (center 1 from 2011 and all cases in center 3): patients were bridged exclusively with full-dose subcutaneous LMWH, with the first dose administered the evening of the procedure (4–6 h after the procedure), and oral anticoagulation resumed 24 h later, maintaining full-dose LMWH until the INR was >2. This protocol was used in all included cases in center 3 (N = 83), all procedures performed after 2011 in center 1 (N = 324), and a small number from center 2 (N = 4), totaling 411 patients.
In both groups, the INR was first assessed 2 days after initiation of oral vitamin K antagonists, and subsequently monitored weekly for a month, after which INR determinations were gradually spaced to every 2 weeks and eventually every 3 to 4 weeks in long-term follow-up so long as relatively stable INRs were achieved. At the end of the procedure, protamine was used at the operator’s discretion to reverse the effect of heparin, allowing for prompt sheath extraction. The dose of protamine was adjusted according to a predefined protocol (provided as supplementary material). The mean protamine dose (±SD) in patients receiving protamine was 43.5 (±18.3) mg.
2.3 Study variables
Baseline clinical and demographic variables were recorded including age, gender, presence or absence of coronary artery disease (CAD), peripheral vascular disease, prior cerebrovascular accident, diabetes or hypertension, left ventricular ejection fraction, left atrial size, and baseline creatinine clearance and hemoglobin. Left atrial size was defined as normal or mildly, moderately, or severely enlarged according to the left atrial area on four-chamber apical images (<20 mm2 normal, 20–30 mm2 mildly dilated, 30–40 mm2 moderately dilated, and >40 mm2 severely dilated). Creatinine clearance was calculated using the MDRD 4 variable formula [10]. CAD was defined as prior evidence of myocardial ischemia in non-invasive tests or proven coronary artery disease upon angiography. We reviewed procedure times, delivery of additional ablation lesions, and post-procedural use, and dosage of protamine.
2.4 Definition of endpoints
We retrospectively reviewed electronic patient records for any thromboembolic complication or major bleeding occurring in the first 4 weeks after the procedure. Major bleeding was defined as bleeding requiring surgical or percutaneous intervention or blood transfusions or resulting in a >2-g/dL drop in hemoglobin levels or vascular access site complications such as AV fistula or femoral artery pseudoaneurysm, regardless of how they were managed. Pericardial bleeding occurring during the procedure was recorded but not considered as major bleeding in our analysis as it was not influenced by the immediate post-procedure anticoagulation strategy. All patients included in the analysis were followed for at least 3 months after the procedure.
2.5 Statistical analysis
Continuous variables are presented as means (±standard deviation) and were compared with the Student t test. Categorical variables are presented as proportions and were compared with the chi-square test (or Fisher exact test if any cell had a value <5). Univariate binomial logistic regression analysis was performed to calculate unadjusted odds ratios for the incidence of major complications in patients in the UFH group vs. those in the LMWH group and in patients taking protamine vs. those not taking protamine. We performed a propensity score to control potential differences or confounders in the risk profile of patients treated with one of the two anticoagulation protocols (although they were consecutive patients). With this aim, logistic regression was performed with intravenous UFH treatment as the dependent variable. Variables with P < 0.20 in univariate analysis were entered as independent variables. The resulting variable PRE_1 represented the probability that the patient would receive UFH. The area under the receiver operating characteristic curve was subsequently calculated with the variable PRE_1 to verify the ability of the propensity score to predict HNF or LMWH treatment. The AUC was >0.8, indicating excellent discriminatory ability. To evaluate the presence of independent predictors of complications, a logistic regression analysis was performed that included all variables with P < 0.20 in the univariate analysis or a plausible relationship with the presence of complications, as well as the PRE_1 variable from the propensity score (and thus the model was adjusted for the probability of a patient being assigned to one of the two anticoagulation protocols). The Holm method was used for correction for multiple testing. A bilateral P value <0.05 was considered significant. All statistical analyses were performed with SPSS software version 20.0 (SPSS Inc, Chicago, IL, USA).
3 Results
3.1 Baseline patient characteristics
Table 1 depicts the baseline characteristics of patients in both anticoagulation protocols. Patients in the LMWH group were older and had a higher prevalence of significant left ventricular systolic dysfunction, compared to those in the UFH group. Of all patients, 47 % presented with atrial fibrillation on the day of the procedure. Additional RF lesions were more often delivered in patients in the LMWH group and mean procedure time was also shorter in this group. Prior use of antiplatelet agents (which were given until the day before the procedure in those patients who were taking them) was more frequent in the UFH group (24.4 vs. 14.4 %, P = 0.001). Length of hospital stay was similar in both groups (1.14 vs. 1.27 days, P = 0.094).
3.2 Post-procedure complications
A total of 29 patients (4.1 %) experienced major post-procedural complications. Major bleeding occurred in 24 patients (3.4 %), comprising 20 cases (2.8 %) of vascular access site hematoma, including 4 cases of arterio-venous fistula (0.6 %), 3 of whom required surgery, and 3 cases of femoral artery pseudoaneurysm (0.4 %) of which 1 required vascular surgical repair and 2 were managed percutaneously. Additional bleeding complications comprised 1 case of retroperitoneal bleeding, which was successfully managed conservatively, 1 case of upper airway bleeding, and 2 cases of severe hematuria. Additionally, 9.1 % of patients (N = 64) experienced minor bleeding events, mostly consisting of uncomplicated minor femoral hematoma. There were no statistically significant differences in the incidence of minor bleeding in patients receiving LMWH compared to those receiving UFH (10.2 vs. 7.6 %, P = 0.228). The total incidence of acute intra-procedural cardiac tamponade in the larger cohort of patients undergoing RF ablation for AF during the study period (N = 744) at the three participating centers was 0.9 % (7 patients); in 4 of these cases, post-procedural anticoagulation was withheld; these patients were then excluded from our analysis. Thromboembolic events occurred in 5 patients (0.7 %), consisting of 3 transient ischemic attacks (TIA), 1 case of post-procedure ST elevation myocardial infarction, and 1 case of bilateral pulmonary embolism. All 5 thromboembolic complications occurred in the first 24 h after the procedure. No cases of persistent neurological deficit occurred. There were no patient deaths during the first 4 weeks post-ablation.
3.3 Predictors of major complications
Table 2 outlines the clinical profile of patients with and without major post-procedure complications. Peripheral vascular disease was the only variable that was significantly more common in cases with major complications. Immediate post-ablation anticoagulation strategy (LMWH vs. UFH) was not associated with the occurrence of major complications, nor with the rate of major bleeding and embolic events when analyzed separately (Table 3, Fig. 2). Prior therapy with antiplatelet agents was not associated with an increased risk of complications in univariate analysis. In multivariate analysis, peripheral vascular disease was the only predictor of major post-procedure complications (adjusted odds ratio (OR) 9.2, confidence interval (CI) 95 % 1.7–49.5, P < 0.01).
3.4 Protamine administration and major complications
A total of 262 patients (37 %) received protamine at the end of the procedure for ACT normalization. Patients who received protamine had modest but statistically significant reductions in procedure times, higher rates of paroxysmal AF, and lower creatinine clearance (Table 4). The relationship between protamine administration and the occurrence of major complications was also explored. There were no significant differences in univariate analysis in thromboembolic complications, major bleeding, or major complications in patients who received protamine compared to those who did not (Table 5).
4 Discussion
The main finding of our study is that, in patients undergoing catheter ablation for AF in whom oral anticoagulation is interrupted for the procedure, immediate post-procedural bridging with UFH and that with LMWH are equally safe strategies.
AF patients are at increased risk of TE during, immediately following, and for several months after an ablation procedure [11, 12]. Even patients deemed before ablation to be at low risk for thrombotic events are transiently exposed to a higher incidence of TE after an ablation procedure. A worldwide survey including over 16,000 patients reported an incidence of post-procedure ischemic stroke or TIA of 0.94 % [13], and a recent study including 2595 patients undergoing ablation between 2005 and 2009 reported a 0.61 % stroke/TIA risk at 30 days post-ablation [14]. Furthermore, a German registry including 3360 patients described a stroke/TIA rate of 0.5 % within 1 month of the procedure [15]. In our study, the incidence of thromboembolic complications (which also included extra-cranial thromboembolic events) was 0.7 %, thus similar to previously reported rates. Increased thromboembolic risk has been attributed to a number of causes. RF energy delivery leaves areas of damaged LA endothelium that can favor thrombus formation. Placement of transseptal sheaths and catheters within the left atrium can also lead to thrombus formation on the catheter surface [16–18] as well as to mobilization of preexisting thrombus. Additionally, even when sinus rhythm is restored during or immediately following the ablation, normal atrial contractile function may be impaired as a consequence of left atrial “stunning” [19]. Of note, in our series, 4 (80 %) of the patients experiencing TE events had a CHADSVASc score of 0, and the fifth had a score of 1, underlining the importance of careful attention to periprocedural anticoagulation in all patients, even those deemed to be at low thromboembolic risk before the procedure. Previous studies have shown that a CHADS score equal to or greater than 2 [11], a CHA2DS2VASc score greater than 6 [13], prior cerebrovascular accident [11, 13, 14], and peripheral vascular disease (PVD) [14] are independent predictors of increased periprocedural stroke risk. Specifically, Kosiuk et al. reported that the existence of peripheral vascular disease carries an adjusted OR of 9.4 for stroke or transient ischemic attack. In a large worldwide survey published by Cappato et al., the incidence of all major thrombotic and bleeding complications amounted to 3.7 % [13], similar to that observed in our study. Multivariate analysis of our data identified peripheral vascular disease as a potent independent predictor of any major vascular complications. Although it stands to reason that preexisting atherosclerotic vascular disease increases the risk of thromboembolic events, its association with vascular access site complications after femoral venous puncture deserves specific comment. Firstly, palpation of the arterial femoral pulse is the main reference for localization of the femoral vein; its absence in the presence of severe arterial vascular disease may significantly complicate venous access. Secondly, inadvertent arterial puncture while attempting to access the femoral vein may carry an increased risk of complication when occurring in patients with significant atherosclerotic femoral artery disease.
Avoidance of thromboembolic complications relies on adequate periprocedural anticoagulation. Various studies have suggested lower complication rates with an uninterrupted oral anticoagulation strategy [4–6]. Specifically, Di Biase et al. observed that interruption of oral vitamin K antagonists and bridging with low molecular weight heparin were associated with an incidence of silent cerebral emboli (identified on post-procedure MRI) of 14 %, compared to 2 % of patients undergoing AF ablation procedures on uninterrupted anticoagulation [20]. We did not address this issue, as we do not systemically perform post-procedure cerebral MRI in our patients. Nonetheless, the clinical relevance of silent cerebral embolic events remains under debate [21]. Although uninterrupted oral anticoagulation is increasingly used, many centers still withhold oral anticoagulants prior to the procedure. Additionally, concerns have been raised recently over whether performing AF ablation without interruption of oral anticoagulation is indeed the best strategy in all patients [7, 8]. In patients in whom vitamin K antagonists are interrupted prior to the procedure, current guidelines consider both UFH and LMWH as valid options for anticoagulation in the first 12–24 h following the procedure [3] whereas earlier consensus documents recommended the use of intravenous UFH due to its shorter half-life, possibility of monitoring its effects with bedside activated clotting time (ACT) or prothrombin time (PTT), and potential for reversal with protamine. Our results show that there are no statistically significant differences in the incidence of major vascular complications, TE events, or major bleeding with either immediate post-procedure anticoagulation strategy, supporting that both strategies are valid.
Although antithrombotic therapy effectively reduces TE risk, this implies increased bleeding risk. In our study, major bleeding occurred in 3.4 % of patients, within the range of previously reported major bleeding rates after catheter ablation of AF (0 to 13 %[3]) and slightly lower (3.4 vs. 6.0 %) than those observed in the interrupted warfarin arm with LMWH bridging in the study by Page et al. [22]. Strikingly, major vascular complication rates in the overall population in our study are similar to those described in the uninterrupted warfarin arm of some of the studies comparing an interrupted vs. uninterrupted oral anticoagulation approach [5, 7, 22].
The role of heparin reversal with protamine to allow for prompt sheath extraction is also unclear, due to safety concerns owing to the possibility of allergic “protamine reactions” as well as to a potential increase in thromboembolic events. In a series of 158 undergoing RFA for AF, protamine administration was not associated with differences in the incidence of thromboembolic events [23]. With regard to heparin reversal in patients undergoing cryoballoon-based pulmonary vein isolation for AF, in a series of 380 patients, Gurses et al. observed that those who received protamine at the end of the procedure experienced lower vascular complication rates than those who did not (1.1 % incidence of hematoma/pseudoaneurysm/arterio-venous fistula vs. 6.3 %) with equal rates of thromboembolic events and shorter hospital stay in protamine-treated patients [24]. Furthermore, in a smaller series including 107 patients undergoing cryoballoon-based AF ablation, Conte et al. also found significantly lower rates of vascular complications in patients treated with protamine (0 vs. 11 %) [25]. Also of note, in published studies, the rate of adverse “protamine reactions” is low (0–1 %) and no fatal cases are described [24–26]. In our study, there were no differences in the incidence of major vascular complications, major bleeding, or thromboembolic events in patients who received protamine compared to those who did not; nonetheless, in light of our sample size and of the low incidence of post-ablation thromboembolism, one cannot establish definitive conclusions regarding protamine use and risk of thromboembolic events. Additionally, the aforementioned studies included patients undergoing cryoballoon ablation, which requires significantly larger vascular access than conventional RF ablation, a fact that could also influence the effect of protamine on vascular complication rates.
An additional conclusion derived from our data deserves mention. As the immediate post-procedure anticoagulation strategy in center 1 (which contributed a large fraction of patients) was switched sequentially from UFH to LMWH after 2011, one can infer from an analysis of the baseline characteristics of LMWH versus UFH subjects that patients undergoing RFA for AF over the past few years have become progressively more complex, with a higher mean age, more left ventricular dysfunction, and a non-significant trend towards a higher prevalence of previous myocardial infarction and peripheral vascular disease. This trend suggests increasing experience with radiofrequency ablation of AF, which is thus offered to sicker patients.
4.1 Study limitations
We devised a retrospective study, and as is the case with this design, the lack of randomization can lead to selection bias and limits the ability to draw definitive conclusions. Multivariate regression and propensity score analysis partially overcome this limitation by controlling for potential confounders; nevertheless, the possibility that significant confounders may not have been recorded cannot be definitively ruled out.
An additional limitation imposed by a retrospective design is the unavailability of certain variables, such as, in this case, patient weight and height, average time to termination of LMWH bridging, and ACT levels for most patients (nonetheless, the study protocol in all three centers dictated strict adherence to an ACT range of 300–350 ms). Additionally, small thromboembolic event rates preclude from establishing definitive conclusions on the relative merit of either type of post-procedure anticoagulation strategy with regard to this specific endpoint. Notwithstanding, a combined assessment of all major vascular complications, as performed in our study, represents a clinically significant and relevant endpoint.
5 Conclusions
Three main conclusions can be derived from our findings. First, in patients undergoing radiofrequency ablation for atrial fibrillation with interrupted oral anticoagulation with vitamin K antagonists, immediate post-procedure bridging with low molecular weight heparin and that with unfractioned heparin are equally safe strategies with regard to the occurrence of major vascular complications; given its greater simplicity of use, low molecular weight heparin may be regarded as the first-choice agent. Interestingly, bleeding rates with either strategy in our series are similar to those described in the uninterrupted warfarin arm of some of the clinical trials comparing an uninterrupted oral anticoagulation approach with an interrupted strategy with post-procedural bridging. Secondly, peripheral vascular disease emerged as a potent independent predictor of major vascular complications, suggesting special care should be paid in these patients when considering the periprocedural anticoagulation strategy and when obtaining vascular venous access. Interestingly, our data would support the use of ultrasound guidance when obtaining femoral venous access for an AF ablation procedure in patients with peripheral vascular disease. Third, thrombotic events are rare in large-volume centers performing catheter ablation for AF, and lasting neurological sequelae are uncommon in those patients that do experience thromboembolic complications.
Abbreviations
- RFA:
-
Radiofrequency ablation
- AF:
-
Atrial fibrillation
- TE:
-
Thromboembolic events
References
Jaïs, P., Haïssaguerre, M., Shah, D. C., Chouairi, S., Gencel, L., Hocini, M., et al. (1997). A focal source of atrial fibrillation treated by discrete radiofrequency ablation. Circulation, 95(3), 572–576.
Calkins, H. (2012). Catheter ablation to maintain sinus rhythm. Circulation, 125(11), 1439–1445.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S., et al. (2012). HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace, 14(4), 528–606.
Hussein, A. A., Martin, D. O., Saliba, W., Patel, D., Karim, S., Batal, O., et al. (2009). Radiofrequency ablation of atrial fibrillation under therapeutic international normalized ratio: a safe and efficacious periprocedural anticoagulation strategy. Heart Rhythm, 6, 1425–1429.
Kwak, J. J., Pak, H. N., Jang, J. K., Kim, S. K., Park, J. H., Choi, J. I., Hwang, C., & Kim, Y. H. (2010). Safety and convenience of continuous warfarin strategy during the periprocedural period in patients who underwent catheter ablation of atrial fibrillation. Journal of Cardiovascular Electrophysiology, 21(6), 620–625.
Di Biase, L., Burkhardt, J. D., Santangeli, P., Mohanty, P., Sanchez, J. E., Horton, R., Gallinghouse, G. J., Themistoclakis, S., Rossillo, A., Lakkireddy, D., Reddy, M., Hao, S., Hongo, R., Beheiry, S., Zagrodzky, J., Rong, B., Mohanty, S., Elayi, C. S., Forleo, G., Pelargonio, G., Narducci, M. L., Dello Russo, A., Casella, M., Fassini, G., Tondo, C., Schweikert, R. A., & Natale, A. (2014). Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the Role of Coumadin in Preventing Thromboembolism in Atrial Fibrillation (AF) Patients Undergoing Catheter Ablation (COMPARE) randomized trial. Circulation, 129(25), 2638–2644.
Arshad, A., Johnson, C. K., Mittal, S., Buch, E., Hamam, I., Tran, T., Shaw, R. E., Musat, D., Preminger, M., Sichrovsky, T., Herweg, B., Shivkumar, K., Hummel, J., & Steinberg, J. S. (2014). Comparative safety of periablation anticoagulation strategies for atrial fibrillation: data from a large multicenter study. Pacing and Clinical Electrophysiology, 37(6), 665–673.
Winkle, R. A. (2014). Uninterrupted warfarin anticoagulation for atrial fibrillation ablation: too good to be true? Pacing and Clinical Electrophysiology, 37(6), 661–664.
Blanc, J. J., Almendral, J., Brignole, M., Fatemi, M., Gjesdal, K., González-Torrecilla, E., et al. (2008). Scientific Initiatives Committee of the European Heart Rhythm Association. Consensus document on antithrombotic therapy in the setting of electrophysiological procedures. Europace, 10(5), 513–527.
Levey, A. S., Bosch, J. P., Lewis, J. B., Greene, T., Rogers, N., & Roth, D. (1999). A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Annals of Internal Medicine, 130(6), 461–470.
Scherr, D., Sharma, K., Dalal, D., et al. (2009). Incidence and predictors of periprocedural cerebrovascular accident in patients undergoing catheter ablation of atrial fibrillation. Journal of Cardiovascular Electrophysiology, 20(12), 1357–1363.
Vazquez, S. R., Johnson, S. A., & Rondina, M. T. (2010). Peri-procedural anticoagulation in patients undergoing ablation for atrial fibrillation. Thrombosis Research, 126(2), e69–e77.
Cappato, R., Calkins, H., Chen, S. A., Davies, W., Iesaka, Y., Kalman, J., Kim, Y. H., Klein, G., Natale, A., Packer, D., Skanes, A., Ambrogi, F., & Biganzoli, E. (2010). Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 3(1), 32–38.
Srivatsa, U. N., Danielsen, B., Anderson, I., Amsterdam, E., Pezeshkian, N., Yang, Y., & White, R. H. (2014). Risk predictors of stroke and mortality after ablation for atrial fibrillation: the California experience 2005-2009. Heart Rhythm, 11(11), 1898–1903.
Kosiuk, J., Kornej, J., Bollmann, A., Piorkowski, C., Myrda, K., Arya, A., Sommer, P., Richter, S., Rolf, S., Husser, D., Gaspar, T., Lip, G. Y., & Hindricks, G. (2014). Early cerebral thromboembolic complications after radiofrequency catheter ablation of atrial fibrillation: incidence, characteristics, and risk factors. Heart Rhythm, 11(11), 1934–1940.
Dorwarth, U., Fiek, M., Remp, T., Reithmann, C., Dugas, M., Steinbeck, G., & Hoffmann, E. (2003). Radiofrequency catheter ablation: different cooled and noncooled electrode systems induce specific lesion geometries and adverse effects profiles. Pacing and Clinical Electrophysiology, 26(7 Pt 1), 1438–1445.
Maleki, K., Mohammadi, R., Hart, D., Cotiga, D., Farhat, N., & Steinberg, J. S. (2005). Intracardiac ultrasound detection of thrombus on transseptal sheath: incidence, treatment, and prevention. Journal of Cardiovascular Electrophysiology, 16(6), 561–565.
Wazni, O. M., Rossillo, A., Marrouche, N. F., Saad, E. B., Martin, D. O., Bhargava, M., Bash, D., Beheiry, S., Wexman, M., Potenza, D., Pisano, E., Fanelli, R., Bonso, A., Themistoclakis, S., Erciyes, D., Saliba, W. I., Schweikert, R. A., Brachmann, J., Raviele, A., & Natale, A. (2005). Embolic events and char formation during pulmonary vein isolation in patients with atrial fibrillation: impact of different anticoagulation regimens and importance of intracardiac echo imaging. Journal of Cardiovascular Electrophysiology, 16(6), 576–581.
Sparks, P. B., Jayaprakash, S., Vohra, J. K., Mond, H. G., Yapanis, A. G., Grigg, L. E., & Kalman, J. M. (1998). Left atrial "stunning" following radiofrequency catheter ablation of chronic atrial flutter. Journal of the American College of Cardiology, 32(2), 468–475.
Di Biase, L., Gaita, F., Toso, E., Santangeli, P., Mohanty, P., Rutledge, N., Yan, X., Mohanty, S., Trivedi, C., Bai, R., Price, J., Horton, R., Gallinghouse, G. J., Beheiry, S., Zagrodzky, J., Canby, R., Leclercq, J. F., Halimi, F., Scaglione, M., Cesarani, F., Faletti, R., Sanchez, J., Burkhardt, J. D., & Natale, A. (2014). Does periprocedural anticoagulation management of atrial fibrillation affect the prevalence of silent thromboembolic lesion detected by diffusion cerebral magnetic resonance imaging in patients undergoing radiofrequency atrial fibrillation ablation with open irrigated catheters? Results from a prospective multicenter study. Heart Rhythm, 11(5), 791–798.
Deneke, T., Jais, P., Scaglione, M., Schmitt, R., DI Biase, L., Christopoulos, G., Schade, A., Mügge, A., Bansmann, M., Nentwich, K., Müller, P., Krug, J., Roos, M., Halbfass, P., Natale, A., Gaita, F., & Haines, D. (2015). Silent cerebral events/lesions related to atrial fibrillation ablation: a clinical review. Journal of Cardiovascular Electrophysiology, 26(4), 455–463.
Page, S., Herring, N., Hunter, R., Withycombe, E., Lovell, M., Wali, G., Betts, T., Bashir, Y., Dhinoja, M., Earley, M., Sporton, S., Rajappan, K., & Schilling, R. (2014). Periprocedural stroke risk in patients undergoing catheter ablation for atrial fibrillation on uninterrupted warfarin. Journal of Cardiovascular Electrophysiology, 25, 585–590.
Patel, A. A., Clyne, C. A., Henyan, N. N., White, C. M., Zembrowski, B. F., Migeed, M., Yarlagadda, R., Kluger, J., & Coleman, C. I. (2007). The use of protamine after radiofrequency catheter ablation: a pilot study. Journal of Interventional Cardiac Electrophysiology, 18(2), 155–158.
Gurses, K. M., Kocyigit, D., Yalcin, M. U., Evranos, B., Yorgun, H., Sahiner, M. L., Kaya, E. B., Oto, M. A., Ozer, N., & Aytemir, K. (2015). Safety and efficacy outcomes of protamine administration for heparin reversal following cryoballoon-based pulmonary vein isolation. Journal of Interventional Cardiac Electrophysiology, 43(2), 161–167.
Conte, G., de Asmundis, C., Baltogiannis, G., Di Giovanni, G., Ciconte, G., Sieira, J., Saitoh, Y., Wauters, K., Mugnai, G., Julià, J., Irfan, G., Levinstein, M., Cotino-Moreno, H. E., Chierchia, G. B., & Brugada, P. (2014). Periprocedural outcomes of prophylactic protamine administration for reversal of heparin after cryoballoon ablation of atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 41(2), 129–134.
Chilukuri, K., Henrikson, C. A., Dalal, D., Scherr, D., MacPherson, E. C., Cheng, A., Spragg, D., Nazarian, S., Sinha, S., Berger, R., Marine, J. E., & Calkins, H. (2009). Incidence and outcomes of protamine reactions in patients undergoing catheter ablation of atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 25(3), 175–181.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table S1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Loughlin, G., Romaniega, T.D., Garcia-Fernandez, J. et al. Immediate post-procedure bridging with unfractioned heparin versus low molecular weight heparin in patients undergoing radiofrequency ablation for atrial fibrillation with an interrupted oral anticoagulation strategy. J Interv Card Electrophysiol 45, 149–158 (2016). https://doi.org/10.1007/s10840-015-0098-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-0098-x