Abstract
With the passage of the Patient Protection and Affordable Care Act (ACA) of 2010, the health insurance literacy of Americans became a critical issue. In response, a consumer education program was created and tested by university researchers and educators associated with Cooperative Extension. This article draws extensively on the emerging literature on health insurance literacy and on data from participants in the Smart Choice Health Insurance™ program. The intent of the study was to understand socio-demographic and environmental variables that predict initial health insurance literacy and gains in health insurance literacy. A standardized instrument measuring health insurance literacy was used to collect the data. Multivariate analysis showed higher income consumers demonstrated greater initial health insurance literacy scores compared to middle income consumers, whereas younger, male and lower educated consumers reported lower initial health insurance literacy. After participating in the Smart Choice Health Insurance™ program, consumers who made greater gains in their health insurance literacy tended to be female, higher income, and consumers residing in states that showed supportiveness of the ACA. The findings highlight the importance of considering sociodemographic characteristics in program design and delivery, as well as how contextual issues, such as the political environment, might impact the delivery of educational efforts. Findings from the analyses help inform ways to adapt and tailor educational opportunities that focus on health insurance literacy for a range of consumers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The goal of the Patient Protection and Affordable Care Act (ACA) of 2010 was to increase access to health insurance and health care options through advanced premium tax credits, cost-sharing subsidies, and expansion of the Medicaid program (Roby et al. 2013; Tanner 2013). However, a critical barrier to expanding health insurance coverage is a lack of consumer knowledge about options and responsibilities (Kaiser Family Foundation [KFF] 2013). According to a recent poll, over half of the uninsured were unaware that the ACA provides financial help to low and moderate income Americans (KFF 2014). The Health Reform Monitoring Survey found that 61 % of consumers who were still uninsured after the first open enrollment period had heard “little” or “nothing” about tax credits or cost-sharing subsidies introduced by the ACA (Dorn 2011). In addition, success of health care reform is attributable, at least partially, to consumers’ health insurance literacy (Paez et al. 2014). Many consumers do not understand important terms, features, or how to shop and compare health insurance plans (American Public Health Association 2012; Consumers Union 2011; Kim et al. 2013; Loewenstein et al. 2013). Together, these findings present an opportunity to increase awareness and understanding of the ACA and to address health insurance literacy.
Health insurance literacy is defined as the “knowledge, ability, and confidence to find and evaluate information about health plans, select the best plan for his or her family for their own or their family’s financial and health circumstances, and use the plan once enrolled” (Consumers Union 2011, p. ii). Health insurance literacy is a relatively new phenomenon that can be conceptualized as the integration of health literacy and financial literacy, which are two types of consumer literacy (Fitzgerald et al. 2015; McCormack et al. 2009). In the context of the ACA, financial literacy is relevant to the selection and use of insurance whereas health literacy may be relevant to understanding new consumer protections under the ACA (e.g., essential health benefits including preventive care) (Fitzgerald et al. 2015). Health insurance literacy is distinct from health literacy in the financial understanding required to estimate costs as well as the ability to understand different benefit structures (Paez et al. 2014). The common ground between health insurance literacy and health literacy is the knowledge “about health services and one’s health status, and the ability to use this information to make decisions” (Paez et al. 2014, p. 226). McCormack et al. (2009) developed a conceptual model for health insurance literacy that describes the associations: “basic financial literacy influences a person’s choice of health insurance (or lack thereof) and use of the health care system, which feeds into their health-related numeracy and health insurance literacy levels” (p. 228). Similar to financial literacy research (Buckland 2010; Fernandes et al. 2014), McCormack et al.’s (2009) model recognizes the importance of individual variables (e.g., age, education, race, and culture) and system-level variables (e.g., use of health care services, health insurance). Researchers have been concerned with the impact of socio-demographic factors on health and financial literacy rates (Kutner et al. 2006; Logan et al. 2015). Consumers with low literacy levels may not understand the financial and health implications of health insurance plans and may distrust the information received from employers and insurance companies (Consumers Union 2011).
The purpose of this study was to investigate health insurance literacy in two ways: (1) by testing associations of sociodemographic and environmental characteristics and health insurance literacy in a community sample, and (2) by assessing whether particular sociodemographic and environmental characteristics (e.g., state’s supportiveness of ACA) are associated with having greater gains in health insurance literacy after participating in a community-based health insurance literacy curriculum called Smart Choice Health Insurance TM (Smart Choice™). A strength of the study is the use of a clearly defined, conceptualized, and psychometrically tested measure of health insurance literacy (Paez et al. 2014). By assessing program evaluation data from a health insurance literacy program, the study can help: (1) assess which groups are more or less health insurance literate, and (2) assess differential gains achieved in health insurance literacy by examining which groups respond to educational programming.
Background
Passage of the ACA is a politically contentious issue, with numerous attempts to repeal and defund the law. The ACA established minimum federal standards that states were required to meet when implementing the law, yet states were given flexibility in participation and implementation (Holahan et al. 2014; Roby et al. 2013). Consequently, a consumer’s experience and interface with insurance is influenced by a state’s commitment to the ACA. For example, consumers were impacted by whether a state created a health insurance marketplace or expanded Medicaid (Holahan et al. 2014; Roby et al. 2013). The ACA funded navigator and in-person assistor programs to assist consumers through outreach, education, and enrollment. According to an Urban Institute report, states with state-based marketplaces had $20.97 (US) per uninsured person to spend on outreach, education, and enrollment assistance, compared to $5.90 (US) per uninsured person in federally facilitated marketplaces (Holahan et al. 2014).
The ACA addressed several factors associated with consumers’ abilities to select a health insurance plan and make use of their health insurance benefits; however, during implementation, consumers’ health insurance literacy received less attention (Paez et al. 2014). For example, some states restricted the number of plans an insurer could offer on the health insurance marketplace to simplify the consumer’s health insurance shopping experience (Dash et al. 2013). The study reported here expects that a state’s environment that is supportive of the ACA would contribute positively to a consumers’ health insurance literacy because of the quality and level of support given to outreach and education efforts. Effective outreach and education may increase health insurance literacy.
American’s Lack of Health Insurance Literacy
Under the ACA, uninsured consumers were expected to make an enrollment decision—one that requires a relatively high level of prose, document, and numerical literacy. For these reasons, health insurance literacy is essential to the well-being of American families (Kim et al. 2013). Possessing a high level of both health and financial literacy is necessary, given the complexity of the marketplace, the abundance of choices in coverage, and the required understanding of individual family and health needs as well as financial considerations. Unfortunately, most Americans have been shown to be deficient in consumer literacy measures. Of the US population, 36 % of adults are at a low level of health literacy and only 12 % have proficient health literacy, described as the skills necessary to read long and complex health-related communication (Kutner et al. 2006). Almost 90 % of adults report difficulty using health information to make an informed health decision (America’s Health Insurance Plans 2013). With respect to financial literacy, Americans were only able to correctly answer an average of 2.88 questions on a five question financial literacy test (FINRA 2013). In another study, 40 % of US adults gave themselves a grade of C, D, or F on their knowledge of personal finance (National Foundation for Credit Counseling 2013), indicating a subjective rating of below average to failing scores on financial literacy.
Most Americans are not literate when it comes to health insurance; they lack understanding of: (1) basic health insurance terms like premium, deductible, copayment, and (2) how to use their health insurance (American Institutes for Research [AIR] 2014; American Institutes of CPAs [AICPA] 2013). One study found that more than half of those polled were unable to define at least one of common health insurance terms (AICPA 2013) and another found that only 20 % could correctly estimate the cost incurred during a routine doctor visit (AIR 2014). A study of older adults and the Medicare program found low to moderate health insurance literacy levels (McCormack et al. 2009).
Several studies suggest that consumers want to better understand health insurance terminology, plan costs, and the details of their health insurance benefits (Consumers Union 2011; Kim et al. 2013; Sinaiko and Hirth 2011). Most American adults (75 %) were moderately or very confident they knew how to use health insurance, yet when presented with a cost-sharing scenario only 20 % could estimate the correct cost of a doctor’s visit (Paez et al. 2014). The study also found that less than half (42 %) of those surveyed were unlikely or somewhat likely to find out what their health plan covered before they went for health care services (Paez et al. 2014). To reduce the complexity and suboptimal decision-making, consumers prefer fewer options and information that is presented in a single or simplified format (Hibbard et al. 2002; Loewenstein et al. 2013).
Health Insurance Literacy and Sociodemographic Characteristics
Prior studies show that consumer literacy differs by sociodemographic characteristics. For example, individuals with low health literacy tend to be low income, lower educated, older, and members of minority groups (Kutner et al. 2006). Sociodemographic characteristics associated with below average financial literacy scores include low income and less educated individuals (Lusardi and Mitchell 2011), women (Fonseca et al. 2010), Hispanics (Hogarth et al. 2003), African Americans (Hogarth et al. 2003), younger adults (in their 20s) (Lusardi and Mitchell 2011) and older adults (retirees and near retirees) (Agarwal et al. 2009).
Similarly, consumers with low levels of health insurance literacy are typically younger, minority status, have lower levels of income and education, and use fewer health care services (Paez et al. 2014). A KFF survey, Assessing Americans’ Familiarity with Health Insurance Terms and Concepts, found health insurance literacy to be a concern for both insured and uninsured consumers, but uninsured consumers had lower scores than those with insurance (Norton et al. 2014). Another study found the health insurance literacy of older adults was lowest among those with lower education and income and older adults with poorer health (McCormack et al. 2009). Health insurance literacy also varies by type of insurance plan. Consumers with an employer-provided insurance plan tend to have higher levels of health insurance literacy compared to those on Medicare or Medicaid or without health insurance (Kutner et al. 2006; Loewenstein et al. 2013).
Newly Eligible Consumers Lack Experience with Health Insurance Coverage
As a result of the ACA, many consumers are purchasing insurance for the first time. Leading up to the enactment of the ACA, several consumer and health-policy organizations conducted small- and large-scale qualitative and quantitative studies to determine the effectiveness of outreach strategies and tactics to enroll the uninsured in health care coverage (Cox-Chapman and Lee 2013). Lessons from the field suggested that when it comes to enrolling in health care coverage, consumers know very little and those likely to benefit the most know even less (KFF 2013). A national study commissioned by Enroll America found that most consumers who were eligible for the marketplace had negative experiences that framed their expectations around the health insurance purchase (Perry and Undem 2013). Most marketplace eligible consumers have found it hard to locate a plan they could afford (77 %); understand the details and fine print of a plan (70 %); find a plan covering all of their health care needs (66 %); and know where to look for a plan (55 %) (Perry and Undem 2013). In their previous health insurance shopping experience, more than half of marketplace eligible consumers did not find and purchase a plan. To reduce barriers to purchasing health insurance, the findings suggest facts and information about costs and coverage of health insurance and the ACA be presented in a way that is credible, raises awareness, addresses skepticism, and motivates people to learn (Perry and Undem 2013).
Addressing Health Insurance Literacy: Smart Choice Health Insurance™
Although the ACA provides greater consumer protection, researchers and practitioners advocate for improved health insurance education (Frank and Lamiraud 2009; Hanoch and Rice 2011; Hibbard et al. 2002; Wroblewski 2007). Several federal agencies (e.g., Centers for Medicare and Medicaid [CMS]) and national organizations such as Families USA, Enroll America, Consumers Union, and Cooperative Extension are working to increase consumers’ health insurance literacy and bring momentum to this issue. With health insurance in the public spotlight, Smart Choice™ was developed to capitalize on a teachable moment and help Americans take control of their personal and family financial health coverage needs. The Smart Choice™ curriculum and workshop materials were developed by a national work group of state specialists and Extension educators, with leadership from the University of Maryland Extension and the University of Delaware Cooperative Extension.
Grounded in research and theory, Smart Choice™ is an entrepreneurial, comprehensive, unbiased curriculum designed to improve consumers’ health insurance literacy by equipping them with the tools needed to make the best possible decision when choosing health insurance plans for themselves and their families. The Smart Choice™ program design was informed by research that identified a consumer’s outlook and motivation, as discussed earlier (Perry and Undem 2013). In addition, segmentation research on the uninsured from the Centers for Medicare and Medicaid Services (CMS 2013) also informed the development of the Smart Choice™ curriculum. For example, consumers at 400 % federal poverty level (FPL) or less suggests that financial security and plan security were important motivators for all audiences. The most important driver for looking into new options for coverage for uninsured and low-income individuals is plan affordability—the idea of finding a plan that fits their budget (Perry and Undem 2013). These motivators and concepts are addressed in the Smart Choice™ curriculum through the facilitation of a case study, discussion, and construction of a monthly spending plan.
Health Insurance Literacy Program Design
The Smart Choice™ curriculum addresses multiple populations by incorporating respect for diversity with regard to ideas, principles, and language. Smart Choice™ materials, available in English and Spanish, written at the seventh grade level, address barriers of reaching audiences with low rates of literacy and English fluency. Outreach analysis by KFF (2013) concluded that “having outreach materials and application forms available in plain language and in multiple languages may reduce enrollment barriers for individuals with limited English proficiency and low literacy” (p. 6). Additionally, Smart Choice™ was grounded in adult learning theory and principles. The Smart Choice™ curriculum provides clear, measurable learning and behavioral objectives explicitly linked to learning theory, evaluation questions linked to learning objectives, and opportunities for active engagement of learners. Program materials (e.g., vocabulary puzzle, worksheets, and case studies) were developed to support adult learning principles and active engagement through learner-centered instruction. Interactive audience response was integrated through TurningPoint© clicker technology, a software and hardware tool that collects real-time responses from participants. The interactive nature of the clicker technology and program materials was designed to enhance participant learning and learning styles.
Smart Choice™ Pilot
Smart Choice™ was piloted in seven states (Delaware, Iowa, Maryland, Michigan, Minnesota, North Dakota, and Oregon) during the first open enrollment of the ACA between September 2013 and May 2014. The community-based educational program reached over 1000 consumers. Some of those consumers were: Extension educators and staff; university residential facilities staff, healthcare professionals, navigators, direct-care professionals, Medicaid and Medicare recipients, and Certified Application Counselors. Workshops were conducted at Extension offices, worksites, community centers, schools, libraries, and hospitals. The curriculum was piloted again in 2015.
Extension faculty teaching the workshops volunteered to become certified to teach the new curriculum. During the initial pilot phase, 39 Extension educators in 25 states were trained through an intensive two-day face-to-face training period between August and November 2013. During the train-the-trainer workshops, Extension educators participated in a consumer Smart Choice™ workshop and then focused on teaching the curriculum. They explored the Educator Toolkit, including PowerPoint® slides, evaluation protocol, and supplemental learning materials. The educators reviewed effective adult education and learner-centered teaching techniques and learned about health reform. Additional supports were available, including consultation, website and resource portal, and webinars.
The main objectives of the current study were to investigate the determinants of health insurance literacy and to assess which determinants were associated with gains achieved in health insurance literacy. We asked the following research questions:
-
(1)
Were any sociodemographic and environmental characteristics associated with health insurance literacy?
-
(2)
Did the gains achieved in health insurance literacy benefit differentially among Smart Choice™ participants’ sociodemographic and environmental factors?
Data and Methodology
Data
Data used in the current analyses were collected as part of the program evaluation. Outcome evaluation data are built into the Smart Choice™ program using TurningPoint© audience-response system technology, a data collection and assessment tool that is often referred to as clicker technology. In cases where the technology was not available, paper–pencil tests were administered. The purpose of the data collection was to determine program effectiveness on health insurance literacy and confidence about the health insurance decision. Workshop participants were informed of the purpose of the research at the beginning of the workshop. The informed consent and confirmation that all responses are anonymous and confidential were read aloud and displayed via PowerPoint® to ensure comprehension regardless of literacy level.
To assess the health insurance literacy levels, a health insurance literacy instrument measured the ability to make informed health insurance decisions and level of confidence in the decision. Additionally, an overall confidence measure and six demographic items were included. Testing was spread throughout the workshop to reduce testing fatigue. The first pre-test was given before the start of the program and the second portion of the pre-test was given in the middle of the program prior to the health insurance plan comparison section. The post-test collected additional item responses and participant demographics at the conclusion of the workshop to determine if participants experienced a change in confidence and capability to make a health insurance decision. Educator information was also collected through open-ended questions submitted to the research team post-program delivery. The data for this project came from 134 workshops conducted in seven states between September 2013 and March 2014. Participants were recruited through a variety of efforts including fliers, newspaper advertisements and articles, radio announcements and interviews, and electronic newsletters. Due to missing data and a few who refused to consent to participation, the current analyses were restricted to 623 cases with complete socio-demographic and health insurance literacy data.
Measures
Health Insurance Literacy
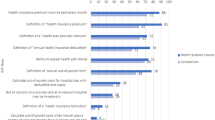
The dependent variable for the study included 11 items from AIR’s validated 21-item Health Insurance Literacy Measure that assesses self-confidence and behavior with choosing and using health insurance (Paez et al. 2014). Smart Choice™ program developers identified 11 items that matched the curriculum learning objectives of building self-confidence and behaviors associated with choosing health insurance. Participants rated the first four questions on a 4-point Likert scale, from not at all confident to very confident, that they could: (1) choose the best health plan, (2) understand health insurance terms, (3) know how to estimate health care needs, and (4) know what questions to ask to choose the best health plan. On a 4-point Likert scale, participants rated the next seven items from not at all likely to very likely that they would: (1) see which doctors and hospitals are covered in health insurance plans, (2) understand what they have to pay for prescription drugs, (3) understand what they would have to pay for emergency visits, (4) understand what they would have to pay for specialist visits, (5) find out if they had to meet a deductible for health care services, (6) find out if their plans covered unexpected costs such as hospital stays, and (7) understand how health insurance plans differ. Health insurance literacy was measured at the start of the program as a pre-test; the identical 11 items were also asked at the conclusion of the programming as a post-test. The 11-item measures were averaged. Initial health insurance literacy (pre-test mean) was 2.64 (standard deviation [SD] 0.75) and health insurance literacy at the conclusion (post-test) of the program was 3.24 (SD 0.66). The health insurance literacy scale showed acceptable reliability with Cronbach’s alphas of 0.914 (pre-test) and 0.939 (post-test).
To identify characteristics associated with gains in health insurance literacy, a dichotomous variable Gains in Health Insurance Literacy was constructed. The dependent variable can be thought of as achieving a desirable level of improvement in health insurance literacy/not achieving a desirable level of improvement in health insurance literacy. Subjects who had large gains in health insurance literacy at the end of the program were categorized based on a split in the distribution of the change score (post-health insurance literacy minus pre-health insurance literacy). Large gains in health insurance literacy were defined as a cut off of .90 or greater in the health insurance literacy change score. Participants with a large gain were coded with a 1 and the lower gains group was coded as 0. The split was based on a combination of the statistical properties of the sample and the nature of the distribution of the score. How people cluster on health insurance literacy has yet to be examined or established (Paez et al. 2014), even with established parameters the sample in this study is likely distinct from the general population. Benchmarks of the measure have not been established; our sample will contribute to establishing a baseline or groupings of high and low health insurance literacy (Paez et al. 2014).
Socio-Demographic Characteristics
Participants were asked about their individual characteristics, including age, gender, race/ethnicity, education, income, and insured status. For age, participants chose from one of five categories: 18–29, 30–49, 50–64, 65–75, and over 75. Response categories were dummy coded, with participants 65 years and older collapsed into one category, and the 50–64 year old group served as a reference. Gender was coded as male = 1, female = 0. Participants chose from six race/ethnicity categories and were re-categorized and dummy coded as White/Non-Hispanic (reference group), Black/African American, and Other (Asian/Pacific Islander, Hispanic or Latino, Native American or American Indian, and Other). Participants identified their total annual income (US) from all sources—less than $25,000, $25,000 to $49,999, $50,000 to $74,999, and $75,000 and over. These were dummy coded, with middle income ($25,000 to $49,999) serving as a reference group. Participants indicated the highest level of education completed. Four categories were used including high school graduates or less, some college or associate’s degree (reference group), bachelor’s degree, and graduate degree. Participants confirmed whether they currently had health insurance (uninsured = 1, insured = 0). Information on the type of insurance plan (e.g., public, private, employer-sponsored) was not collected and is a limitation of this measure.
Environmental Characteristics
Two environmental variables were constructed based on the state where the program was delivered (Delaware, Iowa, Maryland, Michigan, Minnesota, North Dakota, or Oregon). State supportiveness for the ACA was determined by the governor’s official position on the Supreme Court challenge of Medicaid expansion (KFF 2012). If the state had a supporting position the participant received a 1. If the state challenged the position, the participant received 0. Minnesota took no position in the litigation and was scored a 0. A variable was constructed for a state’s uninsured rate in 2013 (Majerol et al. 2014). Participants received a 1 if the state had an uninsured rate less than 10 % and a 0 if the uninsured rate was more than 10 %.
Methodology
To identify determinants of health insurance literacy, a multivariate regression model was run to examine the association between socio-demographic and environmental factors and health insurance literacy (pre-test measure). After identifying individual and environmental characteristics that predict initial health insurance literacy, hierarchical logistic regression was used to estimate the association of sociodemographic and environmental characteristics with the likelihood of achieving gains in health insurance literacy. Variables were entered in three blocks. Initial health insurance literacy was entered as a control in the first block; sociodemographic characteristics were added in the second block; and finally, a block of environmental variables was included. The dependent variable was a dichotomous variable (e.g., achieving a desirable level of improvement in health insurance literacy/not achieving a desirable level of improvement in health insurance literacy); therefore, logistic regression was used as an appropriate method of analysis.
Results
Sample Description
Descriptive statistics are presented in Table 1 including percentages and means for each variable. These summary statistics are presented for the entire sample and by gains to health insurance literacy. The health insurance literacy pre- and post-test scores demonstrated some negative skewness, but they were acceptable levels. The mean pre-test health insurance literacy score was 2.64 (SD 0.75); the mean post-test score was 3.24 (SD 0.65). Over half of the participants came into the workshop with low health insurance literacy—61.6 % scored a 1 or 2 on the 4-point measure, with only one percent measuring a four, indicating high health insurance literacy. Post-intervention health insurance literacy measure showed improvement among participants, with 11.6 % scoring a four and only 4.8 % scoring a one, compared to 20.7 % on the pre-test measure. There were positive and significant changes in all of the health insurance literacy items from pre- to post-test in analyses not shown here. Health insurance literacy from pre-test to post-test improved in almost nine of ten (86.8 %) participants; 3.9 % experienced no change; and, 9.3 % experienced a decline in their health insurance literacy from pre-test to post-test.
The majority of participants were White (85.2 %) and female, less than one-third were male (28.4 %). More than half of participants were middle-aged; 55.4 % were between 50 and 64 years old. Almost one-third of participants had income in the $25,000 to $49,999 (US) category, with equal proportions in the $25,000 or less and $50,000 to $74,999 (25 %). In terms of education, less than a quarter (20.7 %) had a high school diploma or less, 36.8 % had some college, 26.3 % % were college educated, and 16.2 % had a graduate degree. About 19.3 % of participants reported being currently uninsured, a rate slightly higher than the national rate of 13 % in 2013, the period when workshops were conducted (KFF 2015a).
Results of Ordinary Least Square Regression
The first research question involved differential effects of sociodemographic and environmental factors on health insurance literacy. Using an Ordinary Least Square (OLS) regression analysis, health insurance literacy (pre-test measure) was regressed on socio-demographic and environmental characteristics. The estimated regression coefficients and t test statistics are displayed in Table 2. Results of the OLS regression show that age was associated with health insurance literacy. Relative to middle-aged participants, participants ages 18 to 29 (β = −1.92, p < .000) reported lower health insurance literacy. Gender was a predictor of health insurance literacy, male participants had a lower health insurance literacy score (β = −.211, p < .000) compared to female participants. The coefficients for race were not statistically significant (β Black = .052, ns; β Other = .022, ns). Income was associated with health insurance literacy. Compared to middle-income participants ($25,000 to $49,999), individuals in the higher income categories had higher health insurance literacy (β $50,000-$74,999 = .086, p < .049, β $75,000+ = .194, p < .000). Relative to participants who had some college education, individuals with a high school degree reported lower health insurance literacy (β = .018, p < .021). The effect of having no insurance coverage was not statistically significant (β = -.006, ns). Environmental characteristics were not associated with health insurance literacy. Residing in a state supportive of the ACA (β = .038, ns) and with a low uninsured population (β = −.030, ns) was not associated with the health insurance literacy.
Results of Logistic Regression
The second research question addressed differential effects of achieving a desirable gain or improvement in health insurance literacy. The overall model for each logistic regression was statistically significant. Logistic regression analyses showed that after controlling initial health insurance literacy (pre-test), the entry of the sociodemographic characteristics added to the model’s explanatory power (the block χ2 = 51.43, p < .000). The entry of the environmental characteristics in Model 3 also enhance explanatory value in the model (the block χ2 = 22.21, p < .000).
After controlling for initial health insurance literacy and entering the sociodemographic characteristics, gender predicted the odds of a participant’s gain in health insurance literacy. Logistic regression results are shown in odds ratio (OR), a change of less than one results in the decrease in the odds. Compared to females, males had a 58.4 % lower likelihood to achieve a significant improvement in their health insurance literacy (OR of 0.416 means a 58.4 % decrease in the odds, e.g., 1—0.462). The odds of a participant achieving gains in health insurance literacy were higher among African American participants compared to White participants. A change in the OR of 2.66 means African Americans are 2.66 times more likely to achieve gains in health insurance literacy compared to White participants.
Compared to middle income participants ($25,000 to $49,999), being in the highest income category ($75,000 or greater) was associated with a greater likelihood of achieving a gain in health insurance literacy: High-income participants had a 1.98 times greater odds of achieving a gain in health insurance literacy. At a marginally significant level, participants in the lowest income ($25,000 or less, OR = 0.59, p = .068) and education categories (high school or less, OR = 0.60, p = .085) had a lower likelihood of gains in health insurance literacy relative to middle income participants. The other age and education categories as well as insurance status were not significantly associated with gains in health insurance literacy in the second model. Participants with a high school degree or less moved from being marginally significant in the socio-demographic model to significant in the environmental model.
When environmental variables were added in Model 3, the significance of gender persisted, with males being 53.8 % less likely to make gains in health insurance literacy relative to females. The significant association of high income also persisted. Higher income participants were 2.1 times more likely to make gains in health insurance literacy compared to middle income participants. Being African-American no longer predicted the odds of gains in health insurance literacy (p = .538). Participants with a high school degree or less (OR = 0.52, p = .030) had reduced odds of making gains in health insurance literacy compared to college educated participants. Examining the addition of environmental factors, participants in a state not supportive of the ACA were 2.96 times more likely to achieve greater gains in a consumer’s health insurance literacy score. The state’s percent of uninsured was not associated with gains in health insurance literacy (Table 3).
Discussion
The purpose of this study was to identify factors that contribute to health insurance literacy and gains in health insurance literacy at the end of the Smart Choice™ program. Given the benefits of health insurance coverage, an increased understanding of people’s health insurance literacy is important for designing and delivering effective education programs that focus on improving health insurance literacy. Identifying socio-demographic and environmental factors help inform us about who can benefit from an educational program, and ways to adapt and tailor educational opportunities. The results of the study provide support for different associations between individual socio-demographic characteristics and health insurance literacy, as well as some evidence about the importance of where one lives and one’s environment at the time of the education.
Age was not associated with gains in health insurance literacy, but in the OLS model health insurance literacy model, the youngest program participants had significantly lower health insurance literacy relative to middle-aged participants. With certain tasks and decisions, like health insurance, there is evidence that individuals who are less experienced think they are worse than average (Rutter et al.1998), which might explain the lower post-health insurance literacy measure among young adults in our sample. Among the uninsured, CMS (2013) segmentation research describes the “Healthy and Young” (47.8 % of nonelderly uninsured US adults) as consumers who are less likely to value health insurance, who take their health for granted and are not highly motivated to enroll in insurance (pp. 9–10). Given this segmentation research, another explanation of this finding is the notion of relevance and readiness. Younger adult consumers may not be ready for health related information and perhaps health insurance literacy does not feel particularly relevant, given their higher perceived health status (CMS 2013). However, young adults have the greatest uninsured rate of any age group (RWJF 2013; Tanner 2013) and the lowest rate of access to employer-based insurance (Young Adults and the ACA 2010). Almost half report problems paying medical bills (Young Adults and the ACA 2010). Approximately 30 % of young adults (age 19–29) do not have insurance, which is more than one in five of the entire uninsured population in America (RWJF 2013; Tanner 2013; Young Adults and the ACA 2010). Yet, one in six young adults has a chronic illness, such as cancer, diabetes, or asthma (CMS 2015). The ACA provides an opportunity to improve access to health care for young adults. It also represents an unprecedented investment in the prevention, diagnosis, and management of chronic health conditions in younger generations.
These factors indicate that young adults could benefit from improved health insurance literacy to help them understand health insurance and the important considerations when selecting a plan. The question remains whether literacy from an educational program or some other outreach tactic can be effective. Most young adults report being unaware of how the ACA will affect them, however, once they receive basic coverage information, they indicate interest in coverage (Begley 2013). It is important for future consumer education to target young adults with a relevant message, through a channel or in a format of delivery that is appealing. Less than 10 % of the individuals who came to the program were 29 years old or younger, a possible indication that workshops are not a draw for this group.
Gender was significantly related to health insurance literacy. The findings from the OLS analysis indicated males had significantly lower health insurance literacy, and further analysis showed that males did not achieve gains in health insurance literacy compared to women. This finding is consistent with a national study that measured literacy and health literacy across all age groups: “The average health literacy score for women was 6 points higher than the average health literacy score for men. A higher percentage of men (by a margin of 4 percentage points) than women had Below Basic health literacy” (Kutner et al. 2006, p. 10). Health insurance literacy is a component of financial literacy (Kim et al. 2013). Our findings are contrary to the gender-based differences that have emerged in the study of financial literacy, with females typically faring slightly worse with financial literacy compared to men (Bucher-Koenen et al. 2014; Lusardi and Mitchell, 2008). It also contradicts the literature that has found men to be more overconfident about financial issues than women (Barber and Odean 2001). However, studies have found gender differences in health care and health behavior (Bierman 2007; Peerson and Saunders 2011; Vart 2010).
Women typically play a lead role in managing family health care issues. The men in our sample may have had limited experience with health insurance because of the role of women. Insurance is a risk management product and men tend to be greater risk takers than women. Men who feel more vulnerable may have been overrepresented in the program audience. Additionally, how men access, interpret, and apply information has been found to differ from women (Johnson and Learned 2004). The finding that men did not achieve gains in health insurance literacy indicates that, moving forward, health insurance literacy educational programming and informational outreach should consider gender differences. The notion of targeted educational programming is also found in the financial literacy literature (Joo and Grable 2004).
Our findings support the existing literature related to consumer financial education that has more often found the effects of low income and low education to be negatively associated with outcomes compared to highly educated and high income individuals (Bernheim and Kotlikoff 2001; Lyons et al. 2007). The current analyses showed that program participants with the lowest level of education had lower health insurance literacy, relative to college educated participants. Although only marginally significant, participants with the lowest income had lower health insurance literacy. In terms of gains in health insurance literacy, the highest income groups achieved gains in health insurance literacy. These finding are congruent with studies on consumer literacy measures. For example, several financial literacy studies have shown below average financial literacy scores to be associated with low income and less educated individuals (Bernheim and Kotlikoff 2001; Lusardi and Mitchell 2011). In their study of consumer literacy related to credit reports and credit scores, Lyons et al. (2007) showed that less literate consumers tended to be less educated and have lower incomes. Consumer learning is often achieved by real-world interaction and/or the school of hard knocks. However, this segment of the population–low income and lower educated consumers–tend to have greater uninsured rates (Majerol et al. 2014), reducing the likelihood of interacting with health insurance and the issues surrounding the health insurance decision (Smith and Medalia 2014).
A notable finding of the study was the association between a state’s supportiveness of the ACA and gains achieved in health insurance literacy. Residing in a state that took an opposing stand to Medicaid expansion in the Supreme Court challenge was associated with lower gains in health insurance literacy among the consumers attending the program. This finding highlights the importance of the context and environment of educational programming, and is consistent with findings on the importance of context and consumer literacy (Buckland 2010). States who were supportive of implementing the ACA actively developed marketing and outreach campaigns and enrollment strategies, as well as websites and materials that targeted uninsured consumers (Holahan et al. 2014; Roby et al. 2013); these efforts may be reflected in these findings.
A state’s effort to provide outreach and education is influenced by the political nature of the ACA. The current study is based on information collected from a health insurance literacy program delivered during a time of major and historic legislative health reform (Dolan and Mokhtari 2013). The program in this study was delivered to consumers when information was particularly confusing due to misinformation and political messaging. Since its passage, Congress has tried to repeal the ACA over 50 times. Furthermore, another US Supreme Court ruling on whether to strike down tax credits in states not running their own marketplace was decided in the summer of 2015. As of this writing, 30 states and the District of Columbia have expanded or have Medicaid expansion plans, another signal of state support or lack of support (KFF 2015b). The intention of the health insurance literacy program was to provide non-political, non-biased education in a highly contentious environment. Interestingly, gains in health insurance literacy were greater in those states that were supportive of ACA implementation, perhaps reflecting the importance of a positive learning environment.
Some of the variables in the current analysis were not significantly associated with health insurance literacy or gains in health insurance literacy. For example, whether a participant had insurance was not significant, but it was thought to have served as a proxy for experience and literacy because research has found that older consumers and those use more health services are more literate, which implies learning by doing to be an aspect of health insurance literacy (Paez et al. 2014). Similarly, the percent of uninsured in a state’s population was not associated with health insurance literacy. Greater health insurance literacy might have been demonstrated among the insured and among those in states with lower insured rates but our analysis did not bear this out. It is also possible that consumers may have insurance but not understand it. The current analysis highlights socio-demographic variables that identify vulnerable segments of the population—younger, males, low income, lower educated consumers and consumers who reside in a state that does not support the ACA. Additionally, the study demonstrates the promising value of a health insurance literacy program.
There are several limitations to this study. The generalizability is reduced because: (1) a non-random sample was used, (2) the approach was quasi-experimental vs. experimental (there was no designed control group), and (3) potential bias was introduced by the self-selection of the participants. The study is not longitudinal. It does not follow consumers after they make an enrollment decision. The sample may be biased by the over-representation of women. Another limitation is that other measures, not represented in this study, may be associated with an individual’s health insurance literacy. For example, studies examining financial literacy education have identified factors with predictive power including personality traits, family characteristics, and societal factors (like capitalist economy, social structures, power relationships) (Fernandes et al. 2014; Forté 2014; Gudmunson and Danes 2011). The data were collected from seven states, each of which had their own unique implementation of the ACA, including outreach strategies. The study did not collect the level of consumer exposure to outreach and enrollment information which might also influence health insurance literacy outcomes. Future studies would benefit from additional explanatory variables and design changes to reduce limitations. Despite these limitations, this study demonstrates the importance of educators considering the socio-demographic and environmental characteristics of consumers when trying to increase health insurance literacy.
Implications and Conclusion
By increasing health insurance literacy, consumers can make more optimal decisions which could ultimately lead to improved health outcomes (Kim et al. 2013; Loewenstein et al. 2013). The findings from the current study can be used to identify specific populations who may have greater gains in health insurance literacy at the end of a program, or alternatively, identifying those at risk for not achieving gains in health insurance literacy at the end of an educational program. Once groups are identified they can then be provided with the appropriate education or outreach tactic that promotes health insurance literacy to achieve better educational outcomes. The findings show that gender and education are associated with a risk of lower gains in health insurance literacy at the end of the program. In this case, being male and having a high school degree or less was associated with lower gains in health insurance literacy. For males, the lower gains achieved in health insurance literacy could be the program design. The interactive, case study approach of the program might not have resonated with the men participating in the program, as there is some evidence that men want clear, straightforward explanations (Osborne 2004). This finding provides evidence that the Smart Choice™ program designers and other educators consider gender differences in future program modifications.
Participants with the lowest educational achievement were also at risk for not achieving the gains in health insurance literacy as anticipated. Smart Choice™ empowers consumers to tackle the often-intimidating task of selecting health insurance coverage by explaining the process in plain language, outlining differences in plans, and highlighting the factors that may influence their decisions. However, the findings suggest that this program, and other education and outreach, needs to more fully understand and be able to address the vulnerabilities of this population. Consumer misunderstanding and lack of knowledge further complicate a decision that involves choosing appropriate levels of coverage, evaluating coverage needs, and examining financial aspects of coverage (Consumer Reports 2012; Consumers Union 2011; Kim et al. 2013). The implications may be that the program materials and activities are not simple enough, an important strategy to improve health insurance literacy (America’s Health Insurance Plans 2013).
A practical implication that can be derived from the findings is that consumers need help navigating the health insurance decision (Frank and Lamiraud 2009; Hanoch and Rice 2011). As the first release of a series of Cooperative Extension consumer health insurance literacy programs, Smart Choice™ is designed to reduce confusion, increase capability, and increase confidence of consumers as they make health insurance plan decisions (Russell et al. 2014). These findings provide evidence that consumer education can affect health insurance literacy. Cooperative Extension is well positioned to offer such education with their 100 year history of youth and adult education and their network of universities and offices in all states and counties. Educators have an opportunity to teach consumers to make informed choices by offering information and education on the topic of health insurance and health care reform. Extension and other professional educators have the expertise to address the gap in health insurance literacy. Though the ACA provided for navigators, certified application counselors, and insurance agents and brokers to assist consumers through outreach, education, and enrollment, many do not have sufficient expertise or time to educate consumers in a way that enables them to make independent decisions. Furthermore, the geographical reach of navigators and counselors is limited, reflecting the difficulty that states with federally facilitated marketplaces are having in creating strong enrollment assistance programs (Hagan 2012). Thus, many consumers are without assistance or adequate assistance to make a Smart Choice™.
The ACA is a major force shaping contemporary family realities and will affect their access to and cost of care that could affect both financial and health outcomes of consumers. They need educators able to put health insurance purchases into a broader personal and family perspective (Kim et al. 2013) that meets the individual and family health needs with available financial resources. The ACA has created new opportunities to provide more affordable health care options for individuals and families, but the benefits of affordability will be realized only if consumers are informed of these new options. For the current insurance consumer, managing spending can be extremely difficult when navigating health insurance expenditures (Braun 2012). Health care costs have become unaffordable for many because family earnings are unable to meet budget requirements and fewer people have employer-sponsored health insurance (Smith and Medalia 2014). The Smart Choice™ program delivered information on the cost-savings available as a result of new mandates, but the current study did not measure knowledge gains related to information on the ACA. The findings provided insight into gains achieved in health insurance literacy but future studies should determine whether individuals learned about new options under the ACA and whether they were able to take advantage of the new benefits that help lower monthly health insurance premiums and out-of-pocket costs.
These findings also represent an opportunity to increase awareness and understanding of ways to reduce family health insurance costs, particularly among those vulnerable populations identified in the study. Health care costs continue to rise and increasingly play a pivotal role in a family’s budget. In fact, Americans spend more on health care than on housing, food, national defense, or transportation (Tanner, 2013). In 2013, a family of four, on average, spent between 21 and 25 % of their household budget on healthcare expenses (Gould et al. 2013). As a result, individuals and families suffer financial consequences of health care costs or medical debt. According to the 2012 National Health Interview Survey, just over 1 in 4 American families experienced some problem paying for their medical bills (Cohen and Kirzinger 2014). The burden of medical bills and debt among families has been on the rise, largely due to stagnant income and high out-of-pocket spending. Some families are at greater risk—uninsured families, low-to-moderate income families, and families with children report a greater incidence of problems associated with medical bills and medical debt (Cohen and Kirzinger 2014; Pollitz et al. 2015).
The US Census Bureau reported a drop in the uninsured rate between 2013 and 2014 from 13.3 to 10.4 % (Rovner 2015). Among the 8.8 million adults gaining coverage are younger and low to moderate income consumers, typically with limited health insurance literacy. These estimates, in hand with the findings from the current study support continued efforts to boost Americans’ self-confidence and competency with choosing and using health insurance. Policy and programs need to address the health insurance literacy of low income consumers eligible for obtaining health insurance through marketplace exchanges, their employers, Medicare, and Medicaid. The current study found young adult consumers and consumers in the lowest income category had lower health insurance literacy (p = .10). These same consumers did not make significant gains at the end of the health insurance literacy educational program, yet they would likely benefit the most. These findings imply that the program may need to find a more effective way to reach younger, low income individuals through program design and delivery.
The importance of context and environment is highlighted in the finding that consumers from states not supportive of the ACA tended to have a lower likelihood of achieving gains in health insurance literacy. The program was designed to provide a balanced, unbiased view of the ACA with sensitivity to its political considerations. Smart Choice™ does not advocate for any one specific plan or source of plan but instead teaches consumers how to make their own informed decisions. The finding about state supportiveness implies that a neutral, unbiased educational program was not enough to cut through the highly contentious political environment for participants in states not supportive of the ACA, despite the design of the program and the neutral stance of the educators. The finding concurs with financial literacy literature: learning is contextual (Buckland 2010). The successful implementation of the ACA depends on consumers who are aware and informed about their new rights and responsibilities related to health insurance. As the ACA gains more acceptance and becomes less politicized, it is possible that greater gains can be made by participants in an educational program addressing health insurance literacy.
Consumers who become educated about health insurance would have the health insurance literacy necessary to understand and act upon health plan information consistent with their health and financial needs and the confidence to do so. When families enroll in health insurance, they are able to access comprehensive coverage and cost savings that will improve health outcomes and overall quality of life. The skills consumers gain can be used for making other informed health decisions thus increasing the effect and impact educators have on their audience. Health insurance literacy is a way to help strengthen the financial and health well-being of American families. Although education will not pay the medical bills, understanding why health insurance is important and how to select and use an affordable plan as part of financial and health well-being will contribute to financial stability.
Very limited health insurance literacy research has been conducted. Given its emerging nature, the current study extends the literature on programming and policy issues related to health insurance literacy. Smart Choice™ was designed to help consumers understand changes brought about by the ACA as well as enable consumers to make more accurate cost estimates and determine which health insurance plans best fit their needs, wants, and financial situation. This current study identified several individual factors that affect health insurance literacy, including consumer’s age, gender, income, and education. Most markedly, the state’s supportiveness of the ACA was found to be associated with gains in health insurance literacy, highlighting the importance of context when learning.
In the best of times, individuals and families are challenged to make health insurance purchases. The difficulties faced by individuals and families when selecting health insurance, the complicated nature of the decision and the product, and the lack of consumer knowledge and skills to make an optimal health insurance choice were highlighted in a recent review (Kim et al. 2013). With implementation of the ACA, the health insurance literacy of Americans will continue to gain attention. Based on the current study, it is clear that there are differences across sociodemographic characteristics in health insurance literacy. The work related to health insurance literacy by both educators and policy makers must continue.
References
Agarwal, S., Driscoll, J. C., Gabaix, X., & Laibson, D. (2009). The age of reason: Financial decisions over the life-cycle with implications for regulation. Brookings Papers on Economic Activity, 40(2), 51–117.
America’s Health Insurance Plans. (2013). New report highlights health plans’ commitment to health literacy. Retrieved from http://www.ahipcoverage.com/2013/12/10/new-report-highlights-health-plans-commitment-to-health-literacy-2/#sthash.czp7pF02.dpuf.
American Institutes for Research. (2014). Development of the health insurance literacy measure (HILM): Conceptualizing and measuring consumer ability to choose and use private health insurance. Journal of Health Communication, 19(2), 225–239. doi:10.1080/10810730.2014.936568.
American Institutes of CPAs. (2013). Affordable Care Act implications you need to know now. Podcast retrieved from http://blog.aicpa.org/2013/08/affordable-care-act-implications-you-need-to-know-now-podcast.html#sthash.C89xZkKl.dpuf.
American Public Health Association (2012). The Affordable Care Act: The “individual mandate” and other coverage provisions. Retrieved from http://www.apha.org/NR/rdonlyres/C69859CF-F012-4D52-BF52-8F6DAA68C431/0/ACAfactsheetJune2012CoverageProvisions.pdf.
Barber, B. M., & Odean, T. (2001). Boys will be boys: Gender, overconfidence, and common stock investment. Quarterly Journal of Economics, 116(1), 261-292. Retrieved from http://www.jstor.org/stable/2696449.
Begley, S. (2013). Insight: Poll shows healthy young adults may keep Obamacare afloat. Reuters. Retrieved from http://www.reuters.com/article/2013/09/10/us-usa-healthcare-poll-insight-idUSBRE98905M20130910.
Bernheim, B. D., & Kotlikoff, L. J. (2001). Household financial planning and financial literacy. In L. Kotlikoff (Ed.), Essays on saving, bequests, altruism and life-cycle planning (pp. 427–478). Cambridge, MA: MIT Press.
Bierman, A. (2007). Sex matters: Gender disparities in quality and outcomes of care. Canadian Medical Association Journal, 177(12), 1520–1521. doi:10.1503/cmaj.071541.
Braun, B. (2012). Responding to health care reform: Mobilizing Extension. Journal of Extension, 50(5). Retrieved from http://www.joe.org/joe/2012october/comm1.php.
Bucher-Koenen, T., Lusardi, A., Alessie, R., & Van Rooij, M. (2014). How financially literate are women? An overview and new insights (Working Paper No. w20793). Retrieved from National Bureau of Economic Research website: http://www.nber.org/papers/w20793.pdf.
Buckland, J. (2010). Are low-income Canadians financially literate? Placing financial literacy in the context of personal and structural constraints. Adult Education Quarterly, 60(4), 357–376.
Centers for Medicare and Medicaid Services (2013). The center for consumer information & insurance oversight: New funding opportunity announcement for navigators in federally facilitated and state partnership marketplaces. Retrieved from http://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/navigator-foa.html.
Centers for Medicare & Medicaid Services (2015). Young adults and the Affordable Care Act: Protecting young adults and eliminating burdens on families and businesses. Retrieved from: http://www.cms.gov/CCIIO/Resources/Files/adult_child_fact_sheet.html.
Cohen, R.A. & Kirzinger, W.K. (2014). Financial burden of medical care: A family perspective (NCHS Data Brief No. 142). Retrieved from http://www.cdc.gov/nchs/data/databriefs/db142.pdf.
Consumer Reports (2012). Health reform: Seven things you need to know now. Retrieved from http://www.consumerreports.org/health/resources/pdf/ncqa/The_Affordable_Care_Act-You_and_Your_Family.pdf.
Consumers Union (2011). Measuring health insurance literacy: A call to action and a report from the health Insurance literacy expert roundtable. Washington, DC: Author. Retrieved from http://consumersunion.org/pub/Health_Insurance_Literacy_Roundtable_rpt.pdf.
Cox-Chapman, L., & Lee, J. (2013). Talking about health insurance: An overview of messaging research on consumers and enrolling in health insurance. Retrieved from http://www.communitycatalyst.org/doc-store/publications/Message_Research_Memo_Talking_about_Health_Insurance_July_2013.pdf.
Dash, S., Lucia, K. W., Keith, K., & Monahan, C. (2013). Implementing the Affordable Care Act: Key design decisions for state-based exchanges. The Commonwealth Fund. Retrieved from http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2013/Jul/1696_Dash_key_design_decisions_state_based_exchanges.pdf.
Dolan, E. M., & Mokhtari, M. M. (2013). The Patient Protection and Affordable Care Act (ACA): Pros and cons. Journal of Family and Economic Issues, 34(1), 1–2. doi:10.1007/s10834-013-9352-5.
Dorn, S. (2011). The basic health program option under federal health reform: Issues for consumers and states. Retrieved from https://folio.iupui.edu/bitstream/handle/10244/965/72024.pdf?sequence=1.
Fernandes, D., Lynch, J. G, Jr, & Netemeyer, R. G. (2014). Financial literacy, financial education, and downstream financial behaviors. Management Science, 60(8), 1861–1883. doi:10.1287/mnsc.2013.1849.
FINRA Investor Education Foundation. (2013). FINRA Foundation releases nation’s state-by-state financial capability survey. Retrieved from http://www.finra.org/Newsroom/NewsReleases/2013/P268095.
Fitzgerald, M. P., Bias, T. K., & Gurley-Calvez, T. (2015). The Affordable Care Act and consumer well-being: Knowns and unknowns. Journal of Consumer Affairs, 1-27. doi: 10.1111/joca.12059
Fonseca, R., Mullen, K. J., Zamarro, G., & Zissimopoulos, J. (2010). What explains the gender gap in financial literacy? The role of household decision-making (Working Paper WR-762). RAND Labor and Population Working Paper Series. Retrieved from http://www.rand.org/content/dam/rand/pubs/working_papers/2010/RAND_WR762.pdf.
Forté, K. S. (2014). Sociocultural issues in adult financial education. New Directions for Adult and Continuing Education, 2014(141), 5–13. doi:10.1002/ace.
Frank, R. G., & Lamiraud, K. (2009). Choice, price competition and complexity in markets for health insurance. Journal of Economic Behavior & Organization, 71(2), 550–562.
Gould, E., Wething, H., Sabadish, N., & Finio, N. (2013). What families need to get by: The 2013 update of EPI’s family budget calculator (Economic Policy Institute Issue Brief, 368). Retrieved from http://www.epi.org/publication/ib368-basic-family-budgets/.
Gudmunson, C. G., & Danes, S. M. (2011). Family financial socialization: Theory and critical review. Journal of Family and Economic Issues, 32(4), 644–667. doi:10.1007/s10834-011-9275-y.
Hagan, E. (2012). Coordinating assistance efforts: Lessons from Wisconsin. Retrieved from http://www.enrollamerica.org/coordinating-assistance-efforts-lessons-from-wisconsin/.
Hanoch, Y., & Rice, T. (2011). The economics of choice: Lessons from the US health-care market. Health Expectations, 14(1), 105–112. doi:10.1111/j.1369-7625.2010.00646.x.
Hibbard, J. H., Slovic, P., Peters, E., & Finucane, M. L. (2002). Strategies for reporting health plan performance information to consumers: Evidence from controlled studies. Health Services Research, 37(2), 291–313. doi:10.1111/1475-6773.024.
Hogarth, J. M., Beverly, S. G., & Hilgert, M. (2003). Patterns of financial behaviors: Implications for community educators and policy makers. Retrieved from http://www.federalreserve.gov/communityaffairs/national/CA_Conf_SusCommDev/pdf/hogarthjeanne.pdf.
Holahan, J., Blumberg, L. J., Coughlin, T., Courtot, B., Hill, I., Peters, R., et al. (2014). The launch of the Affordable Care Act in selected states: State flexibility is leading to very different outcomes. Retrieved from http://www.urban.org/research/publication/launch-health-reform-eight-states-state-flexibility-leading-very-different-outcomes/view/full_report.
Johnson, L., & Learned, A. (2004). Don’t think pink: What really makes women buy—and how to increase your share of this crucial market. New York: AMACOM.
Joo, S. H., & Grable, J. E. (2004). An exploratory framework of the determinants of financial satisfaction. Journal of Family and Economic Issues, 25(1), 25–50. doi:10.1023/B:JEEI.0000016722.37994.9f.
Kaiser Family Foundation. (2012). States’ positions in the Affordable Care Act Case at the Supreme Court. Retrieved from http://kff.org/health-reform/state-indicator/state-positions-on-aca-case/
Kaiser Family Foundation. (2015a). Status of state action on the Medicaid expansion decisions. Retrieved from http://kff.org/health-reform/slide/current-status-of-the-medicaid-expansion-decision/.
Kaiser Family Foundation. (2015b). Health insurance coverage of the total population. Retrieved from http://kff.org/other/state-indicator/total-population/
Kaiser Family Foundation. (June, 2013). Key lessons from Medicaid and HIP for outreach and enrollment under the Affordable Care Act. Retrieved from http://kff.org/medicaid/issue-brief/key-lessons-from-medicaid-and-chip-for-outreach-and-enrollment-under-the-affordable-care-act/.
Kaiser Family Foundation. (October, 2014). Kaiser Health Tracking Poll. Retrieved from: http://kff.org/health-reform/poll-finding/kaiser-health-tracking-poll-october-2014/.
Kim, J., Braun, B., & Williams, A. D. (2013). Understanding health insurance literacy: A literature review. Family and Consumer Sciences Research Journal, 42(1), 3–13. doi:10.1111/fcsr.12034.
Kutner, M., Greenburg, E., Jin, Y., & Paulsen, C. (2006). The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy (Working Paper NCES 2006-483). National Center for Education Statistics.
Loewenstein, G., Friedman, J. Y., McGill, B., Ahmad, S., Linck, S., Sinkula, et al. (2013). Consumers’ misunderstanding of health insurance. Journal of Health Economics, 32(5), 850–862. doi:10.1016/j.jhealeco.2013.04.004.
Logan, R. A., Wong, W. F., Villaire, M., Daus, G., Parnell, T. A., Willis, E., & Paasche-Orlow, M. K. (2015). Health literacy: A necessary element for achieving health equity. Retrieved from http://nam.edu/wp-content/uploads/2015/07/NecessaryElement.pdf.
Lusardi, A., & Mitchell, O. S. (2008). Planning and financial literacy: How do women fare? (Working Paper No. w13750). Retrieved from National Bureau of Economic Research website: http://www.nber.org/papers/w13750.pdf.
Lusardi, A., & Mitchell, O. S. (2011). Financial literacy and planning: Implications for retirement well-being (Eds). Financial literacy: Implications for retirement security and the financial marketplace (pp. 17–39). Oxford: Oxford University Press.
Lyons, A. C., Rachlis, M., & Scherpf, E. (2007). What’s in a score? Differences in consumers’ credit knowledge using OLS and quantile regressions. Journal of Consumer Affairs, 41(2), 223–249. doi:10.1111/j.1745-6606.2007.00079.x.
Majerol, M., Newkirk, V., & Garfield, R. (2014). The uninsured: A primer - key facts about health insurance and the uninsured in America. Retrieved from http://kff.org/report-section/the-uninsured-a-primer-what-was-happening-to-insurance-coverage-leading-up-to-the-aca/.
McCormack, L., Bann, C., Uhrig, J., Berkman, N., & Rudd, R. (2009). Health insurance literacy of older adults. Journal of Consumer Affairs, 43(2), 223–248.
National Foundation for Credit Counseling, Inc. (2013). NFCC and NBPCA financial literacy survey reveals consumers’ top financial concerns. Retrieved from http://www.nfcc.org/newsroom/newsreleases/NFCC_NBPCA.cfm, http://www.nfcc.org/NewsRoom/FinancialLiteracy/files2013/NFCC_NBPCA_2013%20FinancialLiteracy_survey_datasheet_key%20findings_032913.pdf.
Norton, M., Hamel, L., & Brodie, M. (2014). Assessing Americans’ familiarity with health insurance terms and concepts. Retrieved from http://kff.org/health-reform/poll-finding/assessing-americans-familiarity-with-health-insurance-terms-and-concepts/.
Osborne, H. (2004). What’s the difference? Does gender matter when communicating about health? Retrieved from http://www.healthliteracy.com/article.asp?PageID=3787.
Paez, K. A., Mallery, C. J., Noel, H., Pugliese, C., McSorley, V. E., Lucado, J. L., et al. (2014). Development of the Health Insurance Literacy Measure (HILM): Conceptualizing and measuring consumer ability to choose and use private health insurance. Journal of Health Communication, 19(sup2), 225–239. doi:10.1080/10810730.2014.936568.
Peerson, A., & Saunders, M. (2011). Men’s health literacy in Australia: In search of a gender lens. International Journal of Men’s Health, 10(2), 111–135. doi:10.3149/jmh.1002.111.
Perry, M., & Undem, T. (2013). Informing enroll America’s campaign: Findings from a National Study. Retrieved from https://s3.amazonaws.com/assets.enrollamerica.org/wp-content/uploads/2013/11/Informing-Enroll-America-Campaign.pdf.
Politi, M. C., Kaphingst, K. A., Liu, J. E., Perkins, H., Furtado, K., Kreuter, M. W., et al. (2015). A randomized trial examining three strategies for supporting health insurance decisions among the uninsured. Medical Decision Making.
Robert Wood Johnson Foundation [RWJF]. (2013. December 16). Young adults and the Affordable Care Act. Message posted to http://healthaffairs.org/blog/2013/12/16/recent-health-policy-brief-young-adults-and-the-affordable-care-act/
Roby, D. H., Watson, G., Jacobs, K., Graham-Squire, D., Kinane, C. M., Gans, D., et al. (2013). Modeling the impact of the Affordable Care Act and the individual mandate on Californians. Journal of Family and Economic Issues, 34(1), 16–28. doi:10.1007/s10834-012-9349-5.
Rovner, J. (2015). Nearly 9 million people gained insurance in health marketplace’s first year. Retrieved from http://khn.org/news/nearly-9-million-people-gained-insurance-in-health-marketplaces-first-year/.
Russell, M., Little, L., & Pippidis, M. (2014). Effective case studies: Making a smart choice health insurance decision™. The Forum for Family and Consumer Issues. Retrieved from http://www.ncsu.edu/ffci/publications/2014/v19-n2-2014-summer-fall/russell-little-pippidis.php.
Rutter, D. R., Quine, L., & Albery, I. P. (1998). Perceptions of risk in motorcyclists: Unrealistic optimism, relative realism, and predictions of behavior. British Journal of Psychology, 89, 681–696. doi:10.1111/j.2044-8295.1998.tb02710.x.
Sinaiko, A. D., & Hirth, R. A. (2011). Consumers, health insurance and dominated choices. Journal of Health Economics, 30(2), 450–457. doi:10.1016/j.jhealeco.2010.12.008.
Smith, J. C., & Medalia, C. (2014). Health insurance coverage in the United States: 2013. Retrieved from https://www.census.gov/content/dam/Census/library/publications/2014/demo/p60-250.pdf.
Tanner, M. (2013). The Patient Protection and Affordable Care Act: A dissenting opinion. Journal of Family and Economic Issues, 34(1), 3–15. doi:10.1007/s10834-013-9350-7.
Vart, G. F. (2010). How men differ from women in their attitudes towards bowel cancer screening and intentions to be screened. Journal of Men’s Health, 7(3), 241–248. doi:10.1016/j.jomh.2010.07.002.
Wroblewski, M. (2007). Uniform health insurance information can help consumers make informed purchase decisions. Journal of Insurance Regulation, 26(2), 21-37. Retrieved from http://search.proquest.com/docview/204952674?accountid=10906.
Young adults and the Affordable Care Act: Protecting Young Adults and Eliminating Burdens on Families and Businesses (2010). Retrieved from https://www.whitehouse.gov/sites/default/files/rss_viewer/fact_sheet_young_adults_may10.pdf.
Acknowledgments
The authors would like to share their deep appreciation to the Extension Educators across the nation for their contributions to the project.
Funding
This study was funded by University of Maryland Extension, the College of Agriculture and Natural Resources and the University of Delaware Cooperative Extension.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Bartholomae, S., Russell, M.B., Braun, B. et al. Building Health Insurance Literacy: Evidence from the Smart Choice Health Insurance™ Program. J Fam Econ Iss 37, 140–155 (2016). https://doi.org/10.1007/s10834-016-9482-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10834-016-9482-7