Abstract
The present study evaluated whether families receiving Parent–Child Interaction Therapy (PCIT) experienced significant improvements in both parent and child internalizing symptoms, and if so, whether the relationship between improvement in child externalizing symptoms and internalizing symptoms was mediated by reductions in parenting stress and parent depressive symptoms. Participants were an ethnically diverse sample of 72 families with 2–7-year-old children experiencing clinically significant externalizing symptoms who were assigned to receive a version of PCIT in one of two previously conducted clinical trials designed to evaluate culturally modified versions of PCIT. Analyses revealed that parent-reported child internalizing symptoms, parenting stress, and parent depressive symptoms improved significantly from pre to post treatment in PCIT. Additionally, the relation between child externalizing improvement and internalizing improvement was mediated through reduction in parenting stress, but not parent depressive symptoms. These findings suggest that ethnically diverse children are likely to experience significant improvement in co-occurring externalizing and internalizing symptoms following PCIT. Furthermore, decreases in parenting stress may play a role in the improvement of child internalizing symptoms.
Highlights
-
Both parent-reported child in- and externalizing symptoms decreased significantly after PCIT.
-
Parenting stress and parent depressive symptoms decreased significantly after PCIT.
-
Improvements in parenting stress mediated the relation between improvements in child externalizing and internalizing symptoms.
-
Improvement in parent depressive symptoms did not mediate the relation between improvements in child externalizing and internalizing symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Childhood mental health disorders are highly prevalent and costly to both individuals and society, with one in six U.S. children aged 2–8 years (17.4%) having a diagnosed mental, behavioral, or developmental disorder (Cree et al., 2018). Experts agree that intervening early in the development of mental health disorders has the potential to save both individual suffering and economic resources (World Health Organization, 2003). If left untreated, disorders that emerge in early childhood increase later risk for such outcomes as suicide (Cash & Bridge, 2009), school drop-out (Porche et al., 2011), substance use (Boyle et al., 1993; King et al., 2004) and violence (Borum, 2000). Childhood mental health disorders can be divided into two overarching categories: internalizing and externalizing (Achenbach, 1991). Internalizing disorders (e.g., major depressive disorder and separation anxiety disorder) are characterized by internal psychological distress, while externalizing disorders (e.g., oppositional defiant disorder, conduct disorder, and attention deficit hyperactivity disorder) are characterized by disruptive behaviors. Internalizing and externalizing disorders often co-occur; children ages 3–17 with externalizing disorders are also often diagnosed with anxiety (36.6%) or depression (20.3%; Ghandour et al., 2019).
Research shows that intervening early in childhood is crucial to reduce the negative impact of both externalizing and internalizing disorders on children’s lives and to provide them with the best chance to achieve optimal mental health (Chase & Eyberg, 2008). Behavioral Parent Training (BPT) interventions such as Parent–Child Interaction Therapy (PCIT; Eyberg & Funderburk, 2011) have been found to be highly efficacious in treating externalizing disorders in young children (Kaminski & Claussen, 2017). PCIT is conducted in two phases. In the first phase, Child Directed Interaction (CDI), therapists coach parents in skills that reinforce positive child behavior, extinguish negative attention-seeking behaviors, and help establish a warm parent–child relationship. In the second phase, Parent Directed Interaction (PDI), therapists introduce consistent discipline including a structured time-out procedure. Parent–child dyads typically complete PCIT in an average of 14 sessions, with progression determined by parents’ mastery of the skills taught (McNeil & Hembree-Kigin, 2010). A meta-analysis of 12 randomized controlled trials with children ages 2–5 concluded that children assigned to PCIT experience significantly greater reductions in externalizing symptoms than controls, with the average child experiencing a “large” reduction (Cohen’s d = 1.65, 95 % CI [1.41, 1.90], p < 0.001; Ward et al., 2016). Thus, PCIT is a highly efficacious treatment for young children with behavior problems.
To date, however, less is known about how to best treat young children who experience internalizing and externalizing symptoms simultaneously. For many children, it can be difficult to determine which symptoms to prioritize for treatment (Carpenter et al., 2014). Parents are more likely to seek treatment for externalizing symptoms because they are more disruptive to parents, teachers, and other family members (Mian et al., 2016), and BPT interventions have a strong evidence base for their treatment (Kaminski & Claussen, 2017). Conversely, although there is a large body of research supporting the efficacy of Cognitive Behavioral Therapy (CBT) for internalizing symptoms in school-aged children and adolescents (e.g., Higa-McMillan et al., 2015; Weisz et al., 2006), there are relatively few CBT studies which have focused specifically on preschool-aged children, perhaps because the cognitive demands of CBT require developmental adjustments (e.g., Luby, 2013; Reynolds et al., 2012). Most of these studies do not directly examine change in comorbid externalizing symptoms (e.g., Hirshfeld-Becker et al., 2010; Rapee et al., 2005) or report no significant improvement on externalizing symptoms (e.g., Monga et al., 2009; Scheeringa et al., 2010). On the other hand, there are a small number of lateral extensions that capitalize on PCIT’s strong developmental fit for young children that have shown promise in treating preschoolers’ internalizing symptoms (Carpenter et al., 2014). For example, PCIT-Emotion Development addresses childhood depression (Luby et al., 2018), PCIT + Bravery Directed Interaction (BDI) is adapted for children who suffer from Separation Anxiety Disorder (Pincus et al., 2008), and the Coaching Approach Behavior and Leading by Model (CALM) for children is adapted to treat a range of anxiety disorders (Comer et al., 2012). The PCIT platform may provide a developmentally appropriate model that does not rely on cognitive strategies, and instead emphasizes reinforcement through parental attention and praise (Carpenter et al., 2014; Comer et al., 2012). However, these adaptations of PCIT have not been tested with children who suffer from comorbid internalizing and externalizing symptoms, and may not be appropriate for treating such children. For example, while the CALM program shows promising results for young children with anxiety disorders, it does not incorporate the PDI module, an essential component for treating externalizing symptoms (Comer et al., 2012). Even if these adaptations of PCIT were found to benefit children with comorbid disorders, it may still be desirable to determine if standard PCIT is efficacious for such children because these adapted versions require additional training and expertise beyond what PCIT therapists may already have, and are therefore more difficult for families to access.
There is some evidence to suggest that standard PCIT, without any adaptations that directly address internalizing symptoms, may be a promising approach for treating children with co-occurring externalizing and internalizing symptoms. In a small study (n = 24) of standard PCIT that compared two different orders of delivering the intervention components, researchers found that children in the clinical range for behavior disorders (but not internalizing disorders) showed significant improvement in both types of symptoms from pre to post treatment (Eisenstadt et al., 1993). In a later study, Chase & Eyberg (2008) examined the outcomes of PCIT with 64 children diagnosed with oppositional defiant disorder, 26 of whom also had clinically elevated internalizing symptoms. Both children with clinically elevated internalizing symptoms and those whose symptoms were below the clinical cut point at pre-treatment experienced significant reductions in internalizing symptoms post-treatment. While these studies did not include control groups, they provide preliminary evidence that standard PCIT may be an effective treatment for the internalizing symptoms experienced by children with disruptive behavior disorders.
Because PCIT was designed for children with externalizing symptoms, it is not obvious why children’s internalizing symptoms also improve significantly following PCIT. There are a number of possible explanations, including improvements in both child emotion regulation (Dunsmore et al., 2013; Rothenberg et al., 2019) and in the parent–child relationship that may have wide-reaching impacts across both types of symptoms (Lenze et al., 2011). However, it is also possible that improvements in children’s externalizing behaviors, the main target of PCIT, may have a strong influence on parenting stress and parent depressive symptoms, and that improvements in parents’ internalizing symptoms may then improve child internalizing symptoms. This explanation is plausible because children’s externalizing symptoms have been shown to increase parenting stress and parent depressive symptoms (Dollberg et al., 2020; Luby et al., 2012; Timmer et al., 2011). Furthermore, as children’s externalizing symptoms decrease in PCIT, parents’ levels of depressive symptoms and parenting stress decrease significantly (McNeil et al., 1999; Thomas et al., 2017; Timmer et al., 2011). Research has also established a strong cross-sectional relationship between child internalizing symptoms and both parenting stress (Anthony et al., 2005; Costa et al., 2006) and parent depressive symptoms (Marchand et al., 2002). In addition, at least one longitudinal cross-lagged study found that parenting stress predicts child internalizing problems over a one-year period, but that child internalizing problems do not predict parenting stress over the same time period (Stone et al., 2016), suggesting that parenting stress contributes to the development of child internalizing problems. These relations may be partially explained by the fact that parents’ mental health concerns may lead them to model inappropriate coping, to be more disengaged and critical, and less encouraging of child autonomy (Chase & Eyberg, 2008; Whaley et al., 1999; Woodruff-Borden et al., 2002). Parents experiencing internalizing symptoms have been found to express more parental disapproval and to use more harsh and inconsistent discipline than parents who are not experiencing such symptoms, which in turn have been shown to raise children’s risk for developing internalizing symptoms (Whaley et al., 1999). Therefore, engaging in treatment that reduces child behavior problems is likely to also reduce parent depressive symptoms and stress, which in turn may result in improvements in children’s own internalizing symptoms. Consistent with this notion, Shaw et al. (2009) examined the effects of The Family Checkup, a parent training intervention, and found that reductions in maternal depression between ages 2 and 3 mediated improvement in both child internalizing and externalizing behaviors between ages 2 and 4, even after accounting for the potential mediating effects of improvements in positive parenting. This suggests that reductions in maternal depressive symptoms may lead to improved internalizing outcomes for children in other behavioral parent interventions. However, to date this mediational model has not been tested with PCIT. Understanding how PCIT has its impact on internalizing symptoms is important to help clinicians decide whether standard PCIT is likely to require specific adaptations to assist children suffering from comorbid disorders.
In addition, there is currently little information available about the impact of PCIT on internalizing symptoms among ethnic minority families. While there has been increasing participation of ethnic minority families in BPT intervention studies, samples are still not representative of the U.S. population, with Asian American (Miranda et al., 2005) and Latinx families (Bernal & Domenech Rodríguez, 2009) particularly scarce. Findings that ethnic minority families experience higher attrition rates (Miller et al., 2008; Reyno & McGrath, 2006), longer treatment duration (Fernandez et al., 2011; Matos et al., 2009; McCabe and Yeh 2009; Ramos et al., 2018) and lower treatment engagement (Baker et al., 2011; Reid et al., 2001) suggests that cultural modifications may be needed to achieve benefits comparable to what has been found in large scale clinical trials of BPT conducted with largely Non-Hispanic White samples. Culturally adapted versions of BPT in general (van Mourik et al., 2016; Parra Cardona et al., 2012) and PCIT specifically (Matos et al., 2009; McCabe & Yeh, 2009), have demonstrated promise in improving outcomes for ethnic minority families. However, to our knowledge, studies have not examined the internalizing outcomes of these culturally modified versions of PCIT, nor have studies examining the internalizing outcomes of standard PCIT included ethnically diverse samples that would allow generalization to the wider population. Thus, studies examining internalizing outcomes of culturally modified PCIT among culturally diverse samples are greatly needed.
In the current study, we will examine changes in internalizing symptoms from pre to post treatment among culturally diverse families who participated in two previously conducted clinical trials of PCIT, one of which included a culturally modified version of PCIT called Guiando a Niños Activos (GANA) as well as a Standard PCIT condition, and the other which offered all participants a personalized version called MY PCIT. In addition, we will examine the role of improvements in parent mental health in improvements in children’s internalizing symptoms in PCIT. For the purposes of the current study, we have combined the standard PCIT and culturally modified conditions into a single group for two reasons. First, GANA and MY PCIT differed from standard PCIT primarily in the tailoring of treatment rationales and/or inclusion of engagement techniques to better fit with Mexican American culture (in the case of GANA) or culturally diverse families (in the case of MY PCIT), but did not alter the parenting skills that were taught; all three groups received a program with high fidelity to the PCIT manual. Second, the implementation of PCIT was identical across groups as it relates to the factors theorized to influence internalizing symptoms (externalizing symptom improvement, parental mental health; McCabe et al., 2005, 2020). Hence, future references to the PCIT condition will include both the culturally modified and standard PCIT conditions.
Previous analyses have established a significant decrease in externalizing symptoms in both PCIT samples (McCabe et al., 2005, 2019). In the current study, we hypothesized that families with young children suffering from clinically significant externalizing symptoms would also experience a significant reduction in internalizing symptoms from pre to post treatment. Second, we hypothesized that parenting stress and depressive symptoms would also significantly decrease from pre to post treatment. Finally, we predicted that reductions in parenting stress and depressive symptoms would mediate the relationship between child externalizing improvement and child internalizing improvement. If these hypotheses are supported, it will provide further evidence for the notion that PCIT is an appropriate treatment for children experiencing co-occurring externalizing and internalizing symptoms, extend those findings to an ethnically diverse sample of children, and help to elucidate the complex interrelationship between child externalizing symptoms, parenting stress, parent depressive symptoms, and child internalizing symptoms.
Method
Participants
Participants were 72 families of 2- to 7-year-old children who were assigned to receive a version of PCIT in one of two previously conducted clinical trials evaluating culturally modified versions of PCIT: GANA (n = 40) and MY PCIT (n = 32; see Table 1 for demographics). Children were eligible for each study if they met the following criteria: (1) were between the ages of 2 and 7, (2) had clinically significant behavior problems as measured by a caregiver on the Eyberg Child Behavior Inventory (ECBI) Intensity Scale, (3) did not have a diagnosis of autism, intellectual disability or psychosis, and (4) were not participating simultaneously in any other psychosocial treatment for behavior problems. The GANA study only included families who identified their child as Mexican American, while the MY PCIT study included families that identified their child as Latinx, African American, Asian American and/or Non-Hispanic White (NHW). Families in the GANA study (n = 58) were randomly assigned to receive GANA, standard PCIT, or treatment as usual (TAU). GANA retained the core features of PCIT and added culturally relevant elements designed to better engage families of Mexican American ethnicity (See McCabe et al., 2005; McCabe & Yeh, 2009 for a full description). The current study focuses only on subjects who received either GANA or standard PCIT (n = 40); TAU subjects (n = 18) were excluded. In the MY PCIT study, all families (n = 32) received a personalized version of PCIT (see McCabe et al., 2020 for a full description). All MY PCIT families completed pre-treatment assessments on culturally-influenced factors that may predict attrition, engagement, or family’s response to treatment; prior to beginning treatment, therapists were given assessment results as well as corresponding materials that would allow them to then tailor the intervention specifically to each family. For families with two primary caregivers participating in treatment (which was a female and a male in all instances), we used the female caregiver in our analyses.
Measures
Eyberg Child Behavior Inventory (ECBI)
The ECBI is a 36-item parent-report measure that is used to assess externalizing symptoms in young children (Eyberg & Pincus, 1999). The ECBI Intensity Scale evaluates the frequency of child behavior problems on a 7-point scale (Never [1] to Always [7]) and has established reliability and validity for both Spanish and English versions (Eyberg & Pincus, 1999; Garcia-Tornel et al., 1998). Participants were required to have a clinically elevated score on the ECBI Intensity Scale at pre-treatment in order to be eligible. Alpha reliability was 0.86 for the GANA study and 0.88 for the MY PCIT study.
Parenting Stress Index-Short Form (PSI-SF)
The PSI-SF is a 36-item parent-report measure that assesses parenting stress on a 5-point scale: Strongly Agree (1) to Strongly Disagree (5). The PSI-SF contains three subscales: Parental Distress (PD), Parent–Child Dysfunctional Interaction (PCDI), and Difficult Child (DC) that combine into a Total Stress Scale. The English version of the PSI has established content validity, convergent validity and reliability (Abidin, 1995), and the Spanish version of the PSI has shown adequate reliability and validity with Latinx populations (Solis & Abidin, 1991). Alpha reliability was 0.91 for the GANA study and 0.90 for the MY PCIT study.
Beck Depression Inventory (BDI-IA)
The BDI-IA is a 21-item self-report measure completed by the parents to reflect their own depressive symptomatology on a 4-point scale (0–3; Beck & Steer, 1993). The BDI-IA has well established reliability and validity for both English and Spanish versions (Beck & Steer, 1993; Bonicatto et al., 1998). Alpha reliability was 0.86 for the GANA study and 0.87 for the MY PCIT study.
Child Behavior Checklist (CBCL)
The CBCL is a standardized parent-report measure used to assess behavioral and emotional disorders in children (Achenbach & Rescorla, 2000, 2001). Parents are asked to rate child symptoms on a 3-point scale: Not true (0), Somewhat or Sometimes True (1), Very True or Often True (2). There are age-stratified norms provided for boys and girls, as well as different versions for younger (1.5–5 years old) and older (6–18 years old) children. The CBCL yields scores for Total Problems, Externalizing Problems, and Internalizing Problems, and has established reliability and validity for both Spanish and English versions (Achenbach & Rescorla 2000, 2001; Rubio-Stipec et al., 1990). In the current study, we used the CBCL Internalizing Problems score. At pre-treatment, 33 (46%) children were in the clinical range for internalizing symptoms, 14 (19%) were in the borderline range, and 25 (35%) were in the normative range. Alpha reliability for the Internalizing Problems scale of the CBCL was 0.86 for both the GANA and MY PCIT studies for the younger child version, and 0.87 for the GANA study and 0.69 for the MY PCIT study for the older child version.
Procedure
For both the GANA and MY PCIT studies, families were referred by community clinics, Head Start programs, and outreach to the community. Families were screened for eligibility by a study staff member on the phone. Eligible families were invited to complete a 3-4 hour pre-treatment assessment in person, at which time they gave informed consent. Families received $100 for completing the assessment, after which they were enrolled in the treatment program. In the GANA study, families were then randomly assigned to receive either GANA, standard PCIT, or TAU, while in the MY PCIT study, all families were assigned to receive the personalized version of PCIT. In the GANA study, assessors and families were blind to assignment. For both studies, therapy largely took place at community clinics affiliated with a children’s hospital, with a small number (n = 6) taking place at a university research lab. When families graduated from treatment or dropped out, they were re-contacted to complete a second our post-treatment assessment, for which they also received $100. All procedures were approved by the appropriate Institutional Review Boards and conducted in accordance with their guidelines.
Results
Preliminary Analyses
First, no significant differences were found between the GANA and MY PCIT samples on pre- or post-treatment study variables (see Table 2). Second, preliminary analyses looked at clinical and sociodemographic differences in post-treatment assessment completion. Most families (93%) completed their post-treatment assessment. Families (n = 5) who did not attend their post-treatment assessment were not significantly different on child age, annual income, or pre-treatment levels of child externalizing symptoms, child internalizing symptoms, parenting stress or parent depressive symptoms (all ps < 0.05). Post-treatment assessment completion rates were also similar across GANA (95%) and MY PCIT (91%) participants, girls (90%) and boys (94%), and child ethnic groups (91–100%). Third, a paired samples t-test found that there was significant pre- to post-treatment improvement on child externalizing symptoms as assessed by the ECBI Intensity Scale (t[66] = 14.67, p < 0.001, d = 1.77). At post-treatment, 76% (n = 55) of youth reached normative levels of externalizing symptoms on the ECBI.
Primary Analyses
A paired samples t-test provided support for our first hypothesis that there would be significant pre- to post-treatment improvement in child internalizing symptoms on the CBCL (t[62] = 9.11, p < 0.001; d = 1.15). Moreover, pre to post-treatment internalizing improvements were statistically significant for youth with normative (t[22] = 5.10, p < 0.001), borderline (t[11] = 3.96, p < 0.01), and clinical (t[27] = 6.48, p < 0.001) levels of internalizing symptoms at pre-treatment. Findings also demonstrated clinical changes on child internalizing symptoms for those who began treatment with internalizing problem scores in the clinical range and had post-treatment data available (n = 28): 64% (n = 18) moved to the normative range, 14% (n = 4) moved to the borderline range, and 21% (n = 6) stayed in the clinical range. Our second hypothesis was that parent’s levels of parenting stress and depressive symptoms would decrease from pre- to post-treatment in PCIT. From pre- to post-treatment, levels of parenting stress (t[64] = 7.16, p < 0.001; d = 0.89) and depressive symptoms(t[65] = 3.58, p = 0.001, d = 0.44) both decreased significantly.
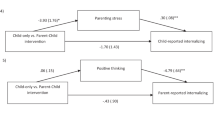
Finally, we examined the indirect effect of changes in the parent’s mental health on the relationship between a child’s externalizing and internalizing symptoms through two mediation models: one specific to parenting stress and the other to parent depressive symptoms. Each mediation model was tested using a series of regression analyses examining the relation between child externalizing improvement and child internalizing improvement, as mediated through improvements in parent’s mental health (see Fig. 1). Change scores were calculated by subtracting the post-treatment score from the pre-treatment score for each of the four main variables of interest (child externalizing symptoms, child internalizing symptoms, parent depressive symptoms and parenting stress). The indirect effect was calculated using the product of the coefficients method (MacKinnon et al., 2004), and significance testing utilized confidence interval and the Sobel test methods (MacKinnon et al., 1995, 2004; Mackinnon & Dwyer, 1993; Sobel, 1982).
To examine the hypothesis that the relationship between externalizing improvement and internalizing improvement would be mediated through improvement in parenting stress, we first determined that improvement in ECBI externalizing symptoms were significantly related to improvement in CBCL internalizing symptoms (Step 1: B = −0.14, SE = 0.03, p < 0.001). Second, we found that improvement in child’s ECBI externalizing symptoms were significantly associated with improvements in parenting stress levels (Step 2: B = 0.19, SE = 0.07, p < 0.01). Third, improvement in parenting stress levels were found to be significantly related to improvement in child’s internalizing symptoms, even after controlling for improvements in their ECBI externalizing symptoms (Step 3: B = −0.23, SE = 0.04, p < 0.001). Finally, adding change in parenting stress to the model reduced the relation between externalizing improvements and internalizing improvements (Step 4: B = −0.10, SE = 0.02, p < 0.001). The total indirect effect of parenting stress improvement is estimated to be –0.04 (95% CI [–0.08, –0.01]), indicating that the relationship between child’s externalizing improvement and internalizing improvement is mediated through improvement in parent’s stress levels (Sobel test p = 0.01).
Next, we examined the hypothesis that the relationship between externalizing improvement and internalizing improvement would be mediated through improvement in parent’s depressive symptoms. As previously stated, improvement in child’s ECBI externalizing symptoms were significantly related to improvement in their CBCL internalizing symptoms (Step 1: B = −0.14, SE = 0.03, p < 0.001). In the second step of these analyses, improvement in child’s ECBI externalizing symptoms did not significantly relate to improvement in parent’s depressive symptoms (Step 2: B = 0.02, SE = 0.02, p = 0.36). In the third step of the analyses, improvement in parent’s depressive symptoms were found to significantly relate to improvement in child’s internalizing symptoms, even after controlling for improvements in their ECBI externalizing symptoms (Step 3: B = −0.60, SE = 0.15, p < 0.001). Adding change in parent depressive symptoms to the model only slightly reduced the relation between externalizing improvements and internalizing improvements (Step 4: B = −0.12, SE = 0.02, p < 0.001). The total indirect effect of parent depressive symptom improvement is estimated to be –0.01 (95% CI [–0.03, 0.01]), indicating that the relationship between child’s externalizing improvement and internalizing improvement is not mediated through improvement in parent’s depressive symptoms (Sobel test p = 0.38).
Adding child gender and child age to the mediation models did not change the pattern of findings, therefore these variables were not included in the final mediation models. Further, sensitivity analyses were conducted to examine the potential of reverse causation. When each mediation model was re-examined with the proposed mediators and dependent variable switched, results showed that change in child internalizing symptoms mediates the relation between change in child externalizing symptoms and change in parent depressive symptoms or parenting stress levels, indicating that we cannot rule out the possibility that the relationships are bidirectional or work in reverse order of the model described here.
Discussion
The current study utilized data from two previously conducted clinical trials of PCIT with ethnically diverse samples to determine whether children with co-occurring externalizing and internalizing symptoms experience significant reductions in both types of symptoms after receiving PCIT. In support of this hypothesis, analyses revealed that young children with clinically elevated externalizing symptoms experienced a significant reduction in internalizing symptoms from pre to post treatment in PCIT, including those children whose internalizing symptoms were in the clinical range at pre-treatment. Additionally, analyses revealed that parents reported experiencing significant improvements in their own parenting stress and depressive symptoms from pre- to post-treatment. Finally, we examined the hypothesis that reductions in child externalizing symptoms in PCIT may be related to improvements in parent mental health, which may in turn be related to improvements in child internalizing symptoms. This hypothesis was partially supported, with results indicating that parenting stress, but not depressive symptoms, mediated the relationship between improvement in child externalizing and internalizing symptoms from pre- to post-treatment. Taken together, these findings suggest that in addition to significant reductions in child externalizing symptoms, families receiving PCIT may also experience significant improvements in child internalizing symptoms, as well as reductions in parenting stress and parent depressive symptoms, and that these findings are generalizable to an ethnically diverse sample. In addition, reductions in parenting stress appear to be related to reductions in child internalizing symptomatology, suggesting that improvements in parenting stress brought about by improving child behavior problems in PCIT may have the added benefit of positively impacting the child’s internalizing symptoms.
Our first hypothesis examined whether children receiving PCIT would experience reduction in child internalizing symptoms. We found that internalizing symptoms showed significant reductions from pre- to post-treatment in PCIT when examined as the total sample, as well as when analyses were limited to children with internalizing symptoms in the clinical range. At post-treatment, 79% of children who began in the clinical range moved into either the normative or borderline range. These results are consistent with past studies indicating that children referred to PCIT for externalizing behavior problems experience reductions in both internalizing and externalizing symptoms (Eisenstadt et al., 1993; Chase & Eyberg, 2008), and extend those previous findings to an ethnically diverse sample. Although the lack of a control group limits our ability to attribute the improvement in internalizing symptoms to PCIT, our findings suggest that young children suffering from co-occurring externalizing and internalizing symptoms do see improvement in both types of symptoms, indicating that PCIT may be a viable option for such children, even if it has not been adapted to address internalizing problems specifically. This method has the advantage of being more accessible to families, as few therapists have training in the versions of PCIT adapted for internalizing disorders, as well as saving families the time and resources they would have to spend to obtain multiple treatments.
Next, we found support for the hypotheses that parenting stress and parent depressive symptoms would be significantly reduced from pre- to post-treatment in PCIT. These findings are consistent with past literature that has documented the positive effect of PCIT on parent mental health (McNeil et al., 1999; Thomas et al., 2017; Timmer et al., 2011). Previous studies have found that children’s externalizing symptoms are strongly related to parent’s depressive symptoms and stress (Dollberg et al., 2020; Luby et al., 2012; Timmer et al., 2011), likely because the strain of caring for a child with clinically significant behavior problems is considerable. Thus, it is not surprising that a treatment like PCIT that significantly reduces child externalizing symptoms, also reduces parenting stress and depressive symptoms. The current study extends these findings to a diverse sample of families receiving PCIT, and highlights the potential of interventions that improve child externalizing symptoms to positively impact parent mental health.
We also found support for the hypothesis that parenting stress would mediate the relationship between improvements in child externalizing and internalizing symptoms. This finding is consistent with the notion that interventions targeting child externalizing symptoms may be related to improvement in parent mental health, which in turn may also be related to improvements in child internalizing symptoms, even when the intervention does not directly address those symptoms. This is not surprising as increased child behavior problems have been associated with parenting stress (Ross et al., 1998), which in turn has been related to increased child internalizing symptoms (Stone et al., 2016). Conversely, as externalizing symptoms improve in PCIT, parenting stress is reduced (McNeil et al., 1999; Thomas et al., 2017; Timmer et al., 2011), which may in turn bring about improvements in child’s internalizing symptoms. This relationship suggests that therapists should be mindful of the importance of parenting stress as an intervention target. The multiple benefits to parent and child mental health indicate that PCIT may be an efficient way to address other issues that may be separate from, but related to, the primary presenting problem.
Lastly, the hypothesis that parent depressive symptoms would mediate the relationship between improvements in child externalizing and internalizing symptoms was not supported. This finding was somewhat surprising as both the current study and the previous literature have found an association between maternal depressive symptoms and both child internalizing and externalizing symptoms (Gunlicks & Weissman, 2008; Luby et al., 2012; Shaw et al., 2009; Wickramaratne et al., 2011). In the current study, although child externalizing symptoms and parental depressive symptoms both improved from pre- to post-treatment, improvement in child behavior problems were correlated with improvements in parenting stress, but not parent depressive symptoms. It is possible that children’s externalizing symptoms are more related to parenting stress than parental depressive symptoms, and thus improvement in behavior problems has a more significant and positive relationship with parenting stress than it does with parent depressive symptoms. Future research is needed before we can fully understand the complex relationships between child externalizing symptoms, parent depressive symptoms, and child internalizing symptoms.
Strengths and Limitations
One of the major strengths of the current study is the participation of an ethnically diverse sample, especially as ethnic minority families are underrepresented in BPT studies (Bernal & Domenech Rodríguez, 2009; Miranda et al., 2005). Studies have found that ethnic minority families are at greater risk for attrition (Miller et al., 2008; Reyno & McGrath, 2006), need more time to complete treatment (Fernandez et al., 2011; Matos et al., 2009; McCabe & Yeh, 2009; Ramos et al 2018), and when in treatment are less engaged (Baker et al., 2011; Reid et al., 2001). Thus, having a more representative sample allows us to generalize our findings to this understudied population that may be at higher risk of not completing treatment. Second, our study replicates the two previous studies that have investigated reductions in child internalizing symptoms after PCIT in children with co-occurring internalizing and externalizing symptoms (Chase & Eyberg, 2008; Eisenstadt et al., 1993), and extends those findings by examining the relation between parent and child mental health.
While the current study expands the limited knowledge of the outcomes of children experiencing co-occurring internalizing and externalizing symptoms in PCIT, the study also suffers from several limitations. First, the current study combined data sets from two previously conducted clinical trials, neither of which had elevated child internalizing symptoms as a criterion for study eligibility, nor were they designed to examine parent mental health as a mediating variable. Second, the TAU control group from the GANA study was too small to make any meaningful comparisons to the PCIT group, and therefore we could not conclusively say our findings show that PCIT leads to greater improvement in child internalizing symptoms than TAU. Third, the study relied mostly on the participation and responses of mothers, so the findings are not generalizable to fathers. Lastly, since the data lacked a time point in the middle of treatment for parenting stress and depressive symptoms, there is no temporal order for the mediation. Therefore, we cannot conclusively say that the statistically significant mediation represents the true order of events. However, the past literature supports the notion that improvements in child externalizing symptoms lead to reductions in parenting stress (McNeil et al., 1999, Thomas et al., 2017; Timmer et al., 2011), and that lower parenting stress leads to lower child internalizing symptoms (Stone et al., 2016). Furthermore, this sequence of events is consistent with the theoretical model underpinning PCIT (McNeil & Hembree-Kigin, 2010). It is suggested that future research should include a mid-point assessment in order to test this mediation model, as well as a control group for comparison.
While further research is needed to determine if the observed improvements in internalizing symptoms are due to PCIT versus spontaneous remission, these results do have several implications for clinical practice. First, they provide support for the use of PCIT as an intervention for children who are experiencing co-occurring externalizing and internalizing symptoms. Even if these data cannot demonstrate the causal role of PCIT in the improvement of internalizing symptoms, it does appear that the overwhelming majority of children with internalizing symptoms at the outset of PCIT have experienced significant reductions in those symptoms by post-treatment, and that a majority are in fact in the normal range, indicating that improvement in those symptoms can also be expected. This is an important insight, as children are more likely to be referred for treatment of externalizing than internalizing problems (Mian et al., 2016); thus, they may be more likely to enter mental health treatment with interventions targeting their externalizing symptoms. Our findings also suggest that treating child behavior problems may pay dividends in improved parent mental health for ethnically diverse families, and that monitoring parenting stress during the course of treatment may be worthwhile. Additional studies are needed to determine when standard PCIT versus a modified version of PCIT or other intervention directly targeting internalizing symptoms should be the preferred treatment for children with co-occurring internalizing and externalizing problems. Future research should focus on understanding the complex relation between child externalizing symptoms, parent mental health, and child internalizing symptoms for very young children.
References
Abidin, R. R. (1995). Parenting Stress Index, third edition: professional manual. Psychological Assessment Resources, Inc.
Achenbach, T. M. (1991). Manual for the Child Behavior Checklist/4-18 and 1991 profile. University of Vermont Department of Psychiatry.
Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA Preschool Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families.
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families.
Anthony, L. G., Anthony, B. J., Glanville, D. N., Naiman, D. Q., Waanders, C., & Shaffer, S. (2005). The relationships between parenting stress, parenting behaviour and preschoolers’ social competence and behaviour problems in the classroom. Infant and Child Development, 14(2), 133–154. https://doi.org/10.1002/icd.385.
Baker, C. N., Arnold, D. H., & Meagher, S. M. (2011). Enrollment and attendance in a parent training prevention program for conduct problems. Prevention Science, 12(2), 126–138. https://doi.org/10.1007/s11121-010-0187-0.
Beck, A. T. & Steer, R. A. (1993). Manual for the Beck Depression Inventory. Psychological Corporation.
Bernal, G., & Domenech Rodríguez, M. M. (2009). Advances in Latino family research: cultural adaptations of evidence-based interventions. Family Process, 48(2), 169–178. https://doi.org/10.1111/j.1545-5300.2009.01275.x.
Bonicatto, S., Dew, A. M., & Soria, J. J. (1998). Analysis of the psychometric properties of the Spanish version of the Beck Depression Inventory in Argentina. Psychiatry Research, 79(3), 277–285. https://doi.org/10.1016/S0165-1781(98)00047-X.
Borum, R. (2000). Assessing violence risk among youth. Journal of Clinical Psychology, 56(10), 1263–1288. https://doi.org/10.1002/1097-4679(200010)56:10<1263::aid-jclp3>3.0.co;2-d.
Boyle, M. H., Offord, D. R., Racine, Y. A., Fleming, J. E., Szatmari, P., & Links, P. S. (1993). Predicting substance use in early adolescence based on parent and teacher assessments of childhood psychiatric disorder: results from the Ontario Child Health Study follow-up. Journal of Child Psychology and Psychiatry, 34(4), 535–544. https://doi.org/10.1111/j.1469-7610.1993.tb01034.x.
Carpenter, A. L., Puliafico, A. C., Kurtz, S. M., Pincus, D. B., & Comer, J. S. (2014). Extending Parent–Child Interaction Therapy for early childhood internalizing problems: new advances for an overlooked population. Clinical Child and Family Psychology Review, 17(4), 340–356. https://doi.org/10.1007/s10567-014-0172-4.
Cash, S. J., & Bridge, J. A. (2009). Epidemiology of youth suicide and suicidal behavior. Current Opinion in Pediatrics, 21(5), 613–619. https://doi.org/10.1097/mop.0b013e32833063e1.
Chase, R. M., & Eyberg, S. M. (2008). Clinical presentation and treatment outcome for children with comorbid externalizing and internalizing symptoms. Journal of Anxiety Disorders, 22(2), 273–282. https://doi.org/10.1016/j.janxdis.2007.03.006.
Comer, J. S., Puliafico, A. C., Aschenbrand, S. G., McKnight, K., Robin, J. A., Goldfine, M. E., & Albano, A. M. (2012). A pilot feasibility evaluation of the CALM Program for anxiety disorders in early childhood. Journal of Anxiety Disorders, 26(1), 40–49. https://doi.org/10.1016/j.janxdis.2011.08.011.
Costa, N. M., Weems, C. F., Pellerin, K., & Dalton, R. (2006). Parenting stress and childhood psychopathology: an examination of specificity to internalizing and externalizing symptoms. Journal of Psychopathology and Behavioral Assessment, 28(2), 113–122. https://doi.org/10.1007/s10862-006-7489-3.
Cree, R. A., Bitsko, R. H., Robinson, L. R., Holbrook, J. R., Danielson, M. L., Smith, C., Kaminsky, J. W., Kenney, M. K., & Peacock, G. (2018). Health care, family, and community factors associated with mental, behavioral, and developmental disorders and poverty among children aged 2–8 years. MMWR. Morbidity and Mortality Weekly Report, 67(50), 1377–1383. https://doi.org/10.15585/mmwr.mm6750a1.
Dollberg, D. G., Hanetz Gamliel, K., & Levy, S. (2021). Mediating and moderating links between coparenting, parental mentalization, parents’ anxiety, and children’s behavior problems. Journal of Family Psychology, 35(3), 324–334. https://doi.org/10.1037/fam0000728.
Dunsmore, J. C., Booker, J. A., & Ollendick, T. H. (2013). Parental emotion coaching and child emotion regulation as protective factors for children with oppositional defiant disorder. Social Development, 22(3), 444–466. https://doi.org/10.1111/j.1467-9507.2011.00652.x.
Eisenstadt, T. H., Eyberg, S., McNeil, C. B., Newcomb, K., & Funderburk, B. (1993). Parent-Child Interaction Therapy with behavior problem children: relative effectiveness of two stages and overall treatment outcome. Journal of Clinical Child Psychology, 22(1), 42–51. https://doi.org/10.1207/s15374424jccp2201_4.
Eyberg, S. M., & Funderburk, B. (2011). Parent-Child Interaction Therapy Protocol. Gainesville, FL: PCIT International.
Eyberg, S. M., & Pincus, D. (1999) Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory: Professional manual. Psychological Assessment Resources.
Fernandez, M. A., Butler, A. M., & Eyberg, S. M. (2011). Treatment outcome for low socioeconomic status African American families in parent-child interaction therapy: a pilot study. Child & Family Behavior Therapy, 33(1), 32–48. https://doi.org/10.1080/07317107.2011.545011.
Garcia-Tornel, S., Calzada, E. J., Eyberg, S. M., Alguacil, J. M., Serra, C. V., Mendoza, C. B., & Domenech, A. T. (1998). Inventario Eyberg del Comportamiento en Niños: Normalización de la versión española y su utilidad para el pediatra extrahospitalario. Anales Españoles de Pediatria, 48, 475–482.
Ghandour, R. M., Sherman, L. J., Vladutiu, C. J., Ali, M. M., Lynch, S. E., Bitsko, R. H., & Blumberg, S. J. (2019). Prevalence and treatment of depression, anxiety, and conduct problems in U.S. children. The Journal of Pediatrics, 206, 256–267.e3. https://doi.org/10.1016/j.jpeds.2018.09.021.
Gunlicks, M. L., & Weissman, M. M. (2008). Change in child psychopathology with improvement in parental depression: a systematic review. Journal of the American Academy of Child & Adolescent Psychiatry, 47(4), 379–389. https://doi.org/10.1097/chi.0b013e3181640805.
Higa-McMillan, C. K., Francis, S. E., Rith-Najarian, L., & Chorpita, B. F. (2015). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child & Adolescent Psychology, 45(2), 91–113. https://doi.org/10.1080/15374416.2015.1046177.
Hirshfeld-Becker, D. R., Masek, B., Henin, A., Blakely, L. R., Pollock-Wurman, R. A., McQuade, J., DePetrillo, L., Briesch, J., Ollendick, T. H., Rosenbaum, J. F., & Biederman, J. (2010). Cognitive behavioral therapy for 4- to 7-year-old children with anxiety disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 78(4), 498–510. https://doi.org/10.1037/a0019055.
Kaminski, J. W., & Claussen, A. H. (2017). Evidence base update for psychosocial treatments for disruptive behaviors in children. Journal of Clinical Child & Adolescent Psychology, 46(4), 477–499. https://doi.org/10.1080/15374416.2017.1310044.
King, S. M., Iacono, W. G., & McGue, M. (2004). Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction, 99(12), 1548–1559. https://doi.org/10.1111/j.1360-0443.2004.00893.x.
Lenze, S. N., Pautsch, J., & Luby, J. (2011). Parent-Child Interaction Therapy emotion development: a novel treatment for depression in preschool children. Depression and Anxiety, 28(2), 153–159. https://doi.org/10.1002/da.20770.
Luby, J. L. (2013). Treatment of anxiety and depression in the preschool period. Journal of the American Academy of Child & Adolescent Psychiatry, 52(4), 346–358. https://doi.org/10.1016/j.jaac.2013.01.011.
Luby, J. L., Barch, D. M., Whalen, D., Tillman, R., & Freedland, K. E. (2018). A randomized controlled trial of parent-child psychotherapy targeting emotion development for early childhood depression. The American Journal of Psychiatry, 175(11), 1102–1110. https://doi.org/10.1176/appi.ajp.2018.18030321.
Luby, J., Lenze, S., & Tillman, R. (2012). A novel early intervention for preschool depression: Findings from a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry, 53(3), 313–322. https://doi.org/10.1111/j.1469-7610.2011.02483.
MacKinnon, D. P., & Dwyer, J. H. (1993). Estimating mediated effects in prevention studies. Evaluation Review, 17(2), 144–158. https://doi.org/10.1177/0193841x9301700202.
MacKinnon, D. P., Lockwood, C. M., & Williams, J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. https://doi.org/10.1207/s15327906mbr3901_4.
MacKinnon, D. P., Warsi, G., & Dwyer, J. H. (1995). A simulation study of mediated effect measures. Multivariate Behavioral Research, 30(1), 41–62. https://doi.org/10.1207/s15327906mbr3001_3.
Marchand, J. F., Hock, E., & Widaman, K. (2002). Mutual relations between mothers’ depressive symptoms and hostile-controlling behavior and young children’s externalizing and internalizing behavior problems. Parenting: Science and Practice, 2(4), 335–353. https://doi.org/10.1207/S15327922PAR0204_01.
Matos, M., Bauermeister, J. J., & Bernal, G. (2009). Parent-Child Interaction Therapy for Puerto Rican preschool children with ADHD and behavior problems: a pilot efficacy study. Family Process, 48(2), 232–252. https://doi.org/10.1111/j.1545-5300.2009.01279.x.
McCabe, K., & Yeh, M. (2009). Parent-Child Interaction Therapy for Mexican Americans: a randomized clinical trial. Journal of Clinical Child Psychology, 38(5), 753–759. https://doi.org/10.1080/15374410903103544.
McCabe, K. M., Yeh, M., Garland, A. F., Lau, A. S., & Chavez, G. (2005). The GANA program: a tailoring approach to adapting Parent Child Interaction Therapy for Mexican Americans. Education and Treatment of Children, 28(2), 111–129.
McCabe, K. M., Yeh, M., & Zerr, A. (2019). MY PCIT: a personalized version of PCIT for culturally diverse families. Invited keynote address to the biennial PCIT conference, Chicago, IL.
McCabe, K., Yeh, M., & Zerr, A. (2020). The case for personalizing behavioral parent training interventions to improve treatment engagement and outcomes for culturally diverse families. Psychological Research and Behavior Management, 13, 41–53. https://doi.org/10.2147/PRBM.S230005.
McNeil, C. B., Capage, L. C., Bahl, A., & Blanc, H. (1999). Importance of early intervention for disruptive behavior problems: comparison of treatment and waitlist-control groups. Early Education and Development, 10(4), 445–454. https://doi.org/10.1207/s15566935eed1004_2.
McNeil, C. B., Hembree-Kigin, T. L. (2010). Parent–Child Interaction Therapy (2nd ed.) Springer Science + Business Media. https://doi.org/10.1007/978-0-387-88639-8.
Mian, N. D., Godoy, L., Eisenhower, A. S., Heberle, A. E., & Carter, A. S. (2016). Prevention services for externalizing and anxiety symptoms in low-income children: the role of parent preferences in early childhood. Prevention Science, 17(1), 83–92. https://doi.org/10.1007/s11121-015-0601-8.
Miller, L. M., Southam-Gerow, M. A., & Allin, Jr, R. B. (2008). Who stays in treatment? Child and family predictors of youth client retention in a public mental health agency. Child & Youth Care Forum, 37(4), 153–170. https://doi.org/10.1007/s10566-008-9058-2.
Miranda, J., Bernal, G., Lau, A., Kohn, L., Hwang, W.-C., & LaFromboise, T. (2005). State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology, 1(1), 113–142. https://doi.org/10.1146/annurev.clinpsy.1.102803.143822.
Monga, S., Young, A., & Owens, M. (2009). Evaluating a cognitive behavioral therapy group program for anxious five- to seven-year-old children: a pilot study. Depression and Anxiety, 26(3), 243–250. https://doi.org/10.1002/da.20551.
Parra Cardona, J. R., Domenech, R. M., Forgatch, M., Sullivan, C., Bybee, D., Holtrop, K., Escobar, C. A. R., Tams, L., Dates, B., & Bernal, G. (2012). Culturally adapting an evidence‐based parenting intervention for Latino immigrants: the need to integrate fidelity and cultural relevance. Family Process, 51(1), 56–72. https://doi.org/10.1111/j.1545-5300.2012.01386.x.
Pincus, D. B., Santucci, L. C., Ehrenreich, J. T., & Eyberg, S. M. (2008). The implementation of modified Parent-Child Interaction Therapy for youth with separation anxiety disorder. Cognitive and Behavioral Practice, 15(2), 118–125. https://doi.org/10.1016/j.cbpra.2007.08.002.
Porche, M. V., Fortuna, L. R., Lin, J., & Alegria, M. (2011). Childhood trauma and psychiatric disorders as correlates of school dropout in a national sample of young adults. Child Development, 82(3), 982–998. https://doi.org/10.1111/j.1467-8624.2010.01534.x.
Ramos, G., Blizzard, A. M., Barroso, N. E., & Bagner, D. M. (2018). Parent training and skill acquisition and utilization among Spanish and English-speaking Latino families. Journal of Child and Family Studies, 27(1), 268–279. https://doi.org/10.1007/s10826-017-0881-7.
Rapee, R. M., Kennedy, S., Ingram, M., Edwards, S., & Sweeney, L. (2005). Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting and Clinical Psychology, 73(3), 488–497. https://doi.org/10.1037/0022-006x.73.3.488.
Reid, M. J., Webster-Stratton, C., & Beauchaine, T. P. (2001). Parent training in Head Start: a comparison of program response among African American, Asian American, Caucasian, and Hispanic mothers. Prevention Science, 2(4), 209–227. https://doi.org/10.1023/A:1013618309070.
Reyno, S. M., & McGrath, P. J. (2006). Predictors of parent training efficacy for child externalizing behavior problem–a meta-analytic review. Journal of Child Psychology and Psychiatry, 47(1), 99–111. https://doi.org/10.1111/j.1469-7610.2005.01544.x.
Reynolds, S., Wilson, C., Austin, J., & Hooper, L. (2012). Effects of psychotherapy for anxiety in children and adolescents: a meta-analytic review. Clinical Psychology Review, 32(4), 251–262. https://doi.org/10.1016/j.cpr.2012.01.005.
Ross, C. N., Blanc, H. M., McNeil, C. B., Eyberg, S. M., & Hembree-Kigin, T. L. (1998). Parenting stress in mothers of young children with oppositional defiant disorder and other severe behavior problems. Child Study Journal, 28(2), 93–110.
Rothenberg, W. A., Di Giunta, L., Lansford, J. E., Lunetti, C., Fiasconaro, I., Basili, E., Thartori, E., Favini, A., Pastorelli, C., Eisenberg, N., Amico, F. D., Rosa, M., & Cirimele, F. (2019). Daily associations between emotions and aggressive and depressive symptoms in adolescence: the mediating and moderating role of emotion dysregulation. Journal of Youth and Adolescence, 48(11), 2207–2221. https://doi.org/10.1007/s10964-019-01071-6.
Rubio-Stipec, M., Bird, H., Canino, G., & Gould, M. (1990). The internal consistency and concurrent validity of a Spanish translation of the Child Behavior Checklist. Journal of Abnormal Child Psychology, 18(4), 393–406. https://doi.org/10.1007/BF00917642.
Scheeringa, M. S., Weems, C. F., Cohen, J. A., Amaya-Jackson, L., & Guthrie, D. (2010). Trauma-focused cognitive-behavioral therapy for posttraumatic stress disorder in three-through six year-old children: a randomized clinical trial. Journal of Child Psychology and Psychiatry, 52(8), 853–860. https://doi.org/10.1111/j.1469-7610.2010.02354.x.
Shaw, D. S., Connell, A., Dishion, T. J., Wilson, M. N., & Gardner, F. (2009). Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology, 21(2), 417–439. https://doi.org/10.1017/S0954579409000236.
Sobel, M. (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290–312. https://doi.org/10.2307/270723.
Solis, M. L., & Abidin, R. R. (1991). The Spanish version Parenting Stress Index: a psychometric study. Journal of Clinical Child Psychology, 20(4), 372–378. https://doi.org/10.1207/s15374424jccp2004_5.
Stone, L. L., Mares, S. H. W., Otten, R., Engels, R. C. M. E., & Janssens, J. M. A. M. (2016). The co-development of parenting stress and childhood internalizing and externalizing problems. Journal of Psychopathology and Behavioral Assessment, 38(1), 76–86. https://doi.org/10.1007/s10862-015-9500-3.
Thomas, R., Abell, B., Webb, H. J., Avdagic, E., & Zimmer-Gembeck, M. J. (2017). Parent-Child Interaction Therapy: a meta-analysis. Pediatrics, 140(3), 1–2. https://doi.org/10.1542/peds.2017-0352.
Timmer, S. G., Ho, L. K. L., Urquiza, A. J., Zebell, N. M., Fernandez y Garcia, E., & Boys, D. (2011). The effectiveness of Parent–Child Interaction Therapy with depressive mothers: the changing relationship as the agent of individual change. Child Psychiatry and Human Development, 42(4), 406–423. https://doi.org/10.1007/s10578-011-0226-5.
van Mourik, K., Crone, M. R., de Wolff, M. S., & Reis, R. (2016). Parent training programs for ethnic minorities: a meta-analysis of adaptations and effect. Prevention Science, 18(1), 95–105. https://doi.org/10.1007/s11121-016-0733-5.
Ward, M. A., Theule, J., & Cheung, K. (2016). Parent–Child Interaction Therapy for child disruptive behaviour disorders: a meta-analysis. Child and Youth Care Forum, 45(5), 675–690. https://doi.org/10.1007/s10566-016-9350-5.
Weisz, J. R., McCarty, C. A., & Valeri, S. M. (2006). Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychological Bulletin, 132(1), 132–149. https://doi.org/10.1037/0033-2909.132.1.132.
Whaley, S. E., Pinto, A., & Sigman, M. (1999). Characterizing interactions between anxious mothers and their children. Journal of Consulting and Clinical Psychology, 67(6), 826–836. https://doi.org/10.1037/0022-006X.67.6.826.
Wickramaratne, P., Gameroff, M. J., Pilowsky, D. J., Hughes, C. W., Garber, J., Malloy, E., King, C., Cerda, G., Sood, A. B., Alpert, J. E., Trivedi, M. H., Fava, M., Rush, A. J., Wisniewski, S., & Weissman, M. M. (2011). Children of depressed mothers 1 year after remission of maternal depression: findings from the STARD-Child study. The American Journal of Psychiatry, 168(6), 593–602. https://doi.org/10.1176/appi.ajp.2010.10010032.
Woodruff-Borden, J., Morrow, C., Bourland, S., & Cambron, S. (2002). The behavior of anxious parents: examining mechanisms of transmission of anxiety from parent to child. Journal of Clinical Child and Adolescent Psychology, 31(3), 364–374. https://doi.org/10.1207/153744202760082621.
World Health Organization. (2003). Investing in mental health. World Health Organization. https://apps.who.int/iris/handle/10665/42823.
Acknowledgements
This work was supported by National Institute of Mental Health (NIMH) Grants K01MH01924 and R34MH109561 as well as the University of San Diego Cadden Summer Research Award. Some data used in the preparation of this manuscript are available from the NIMH Data Archive (NDA). NDA is a collaborative informatics system created by the NIH (National Institutes of Health) to provide a national resource to support the sharing of federally funded data for accelerating research. Dataset identifier: 10.15154/1524646. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or University of San Diego.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McCabe, K.M., Zerr, A., Cook, M. et al. The Relation between Parent Mental Health and Child Internalizing Symptoms in Parent–Child Interaction Therapy. J Child Fam Stud 31, 2065–2076 (2022). https://doi.org/10.1007/s10826-022-02254-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-022-02254-9