Abstract
Oppositional defiant disorder (ODD) frequently co-occurs with depression in youth, and it has been proposed that ODD Angry/Irritable Mood symptoms predict depression in these youth. Another explanation is that the ODD Angry/Irritable Mood dimension is a component of a broader emotion dysregulation syndrome. This study examined the relationship of ODD Angry/Irritable Mood symptoms with depression, and the Child Behavior Check List (CBCL) Dysregulation Profile with co-occurring ODD and depression in clinic-referred youth. Of 310 youth referred to an outpatient clinic, 86 were diagnosed with ODD without depression, and 78 were diagnosed with co-occurring ODD and depression. These groups did not differ in number of ODD Angry/Irritable Mood symptoms, and ODD affective symptoms showed a low correlation with youth-reported depression and parent- reported CBCL Anxious/Depressed symptoms. Logistic regression analysis with ODD Angry/Irritable Mood symptoms did not differentiate youth who were diagnosed with ODD without depressive disorder from youth who were diagnosed with co-occurring ODD and depression. The 55 youth who fit the CBCL – Dysregulation Profile were more likely to be diagnosed with depression than youth who did not fit the profile. Logistic regression analysis with this profile differentiated youth with co-occurring ODD and depression from youth diagnosed with ODD without co-occurring depression. Present results did not support the hypothesis that ODD Angry/Irritable Mood symptoms are differentially associated with depression in clinic-referred youth with ODD. However, the results did support the hypothesis that the parent-report CBCL dysregulation profile differentiates youth with co-occurring ODD and depression from ODD youth without depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The co-occurrence of mental disorders in children and adolescents has attracted considerable attention in recent years, and comorbidity is recognized as the rule rather than the exception (Angold et al. 1999). An influential meta-analysis of childhood and adolescent community samples showed high rates of co-occurring disorders for both internalizing and externalizing disorders (Angold et al. 1999). More recently, Merikangas et al. 2010 reported similar findings for the National Comorbidity Survey Replication – Adolescent Supplement study (NCS-A). Of those adolescents who met DSM-IV (American Psychiatric Association. 2000) diagnostic criteria for one category of disorder (e.g., anxiety, behavior disorder) in the NCS-A study, approximately 40% reported more than one lifetime disorder (Merikangas et al. 2010). Mood disorders were more likely to co-occur with other categories of disorders.
An extensive body of research documents high rates of co-occurring conduct problems and depression in children and adolescents (Wolff and Ollendick 2006). As noted by Wolff and Ollendick (2006) and Burke and Loeber (2010), the co-occurrence of depression and conduct problems like oppositional defiant disorder (ODD) is puzzling because the characteristics of these disorders are quite different. According to DSM-5 (American Psychiatric Association. 2013), features of ODD include a pattern of angry, irritable, defiant, or vindictive behavior that persists for at least six months. In contrast, key features of depression include sadness, along with a lack of pleasure, apathy, loss of energy, and sleep problems.
In addition to research documenting the high rates of co-occurring ODD and depression, there is a growing body of research showing that ODD usually develops before the onset of depression and anxiety (e.g., Costello et al. 2003; Maughan et al. 2004; Nock et al. 2007). Moreover, relative to all other mental disorders, ODD is the strongest predictor of future depression (Burke and Loeber 2010; Burke et al. 2005; Copeland et al. 2009). This body of research appears to indicate that ODD may play a role in the etiology and course of other externalizing (e.g., ADHD, conduct disorder) and internalizing disorders (e.g., Burke et al. 2010).
Although it is clear that many youth with ODD are likely to experience depression (Angold et al. 1999; Boylan et al. 2007; Burke and Loeber 2010), it is less clear why this comorbidity occurs. One possible explanation has been advanced by Stringaris and colleagues (Stringaris and Goodman 2009a, 2009b, 2009c; Stringaris et al. 2010). Their research indicates that the diagnostic criteria for ODD consist of three subsets of symptoms that may be differentially associated with other disorders. Youth who are diagnosed with ODD are defiant and noncompliant with adults’ directives, but they also annoy and blame others, have difficulty controlling their temper, are irritable and angry, and act out in spiteful or vindictive ways (American Psychiatric Association. 2013). Stringaris and colleagues found that an Irritable subset of ODD, reflected in three DSM-IV items (often loses temper, is angry and resentful, is often touchy or easily annoyed by others) was associated with depression in a sample of community children and adolescents. A Headstrong subset of ODD, comprised of four DSM-IV items (often argues with adults, often actively defies or refuses to comply with adults’ requests or rules, often deliberately annoys other people, often blame others for his or her mistakes or misbehavior) was associated with ADHD in this community sample. The third, Hurtful, subset was comprised of a single DSM-IV item (has been spiteful or vindictive at least twice in the past 6 months) that was associated with conduct disorder.
The findings of Stringaris and colleagues influenced the formulation of three subsets of ODD symptoms in DSM-5 (American Psychiatric Association. 2013): (1) Angry/Irritable Mood, (2) Argumentative/Defiant Behavior, and (3) Vindictiveness. The symptoms in these subsets correspond exactly to the Irritable, Headstrong, and Hurtful dimensions described by Stringaris and colleagues (Stringaris and Goodman 2009a, 2009b, 2009c; Stringaris et al. 2010). Although subsequent research has confirmed that ODD has specific symptom dimensions that correspond to the DSM-5 subsets of Angry/Irritable Mood and Argumentative/Defiant Behavior (Burke et al. 2014; Ollendick et al. 2018), only a small number of studies have attempted to replicate Stringaris’s finding that the ODD Angry/ Irritable Mood dimension is differentially associated with depression (Burke 2012; Hipwell et al. 2011; Evans et al. 2016a, b).
To date, only one study has examined the relationship of the ODD Angry/Irritable Mood dimension with depression in a clinic-referred sample. Using a sample of 177 boys between the ages of 7 and 12 years who were recruited from two psychiatric clinics, Burke (2012) reported that the ODD symptoms of being touchy, angry, and spiteful predicted increasing symptoms of depression and anxiety through age 18 years. It should be noted that the three ODD symptoms that predicted depressive symptoms in adolescence differ from the subset reported by Stringaris (and adopted in DSM-5). Specifically, Burke’s (2012) study included the vindictive/spiteful item instead of often loses temper in the Irritability cluster of items that predicted later depression and anxiety.
Other methodological issues may be important to consider. For example, some studies have examined the association of the ODD Angry/Irritable Mood dimension in samples of young children (e.g., age 5–12 years; Evans et al. 2016a, b) whereas others have examined this association in youth through age 18 (Burke 2012). Age may be an important consideration because the prevalence of depression increases during adolescence (Hammen et al. 2014). Another issue is that investigators have relied on parent-report measures to assess their children’s depression (e.g., Diagnostic Interview Schedule for Children). Unlike disruptive behavior disorders, which primarily have features that can be observed by parents or teachers, depression has several features that may be known only to the youth (e.g., self-criticism). Therefore, it would be beneficial to include both parent-report and child-report measures of depression in research that examines the association of the ODD Angry/Irritable Mood dimension and depression in youth.
Irritability is not unique to ODD or depression, but instead it is a common presentation of many disorders in children and adolescents (Brotman et al. 2017; Leibenluft and Stoddard 2013; Safer 2009). In addition to its association with depression, one study found that the 3-item DSM-IV Angry/Irritable Mood dimension of ODD was associated with generalized anxiety disorder, major depressive disorder, social anxiety disorder, and manic symptoms, suggesting that Angry/Irritable Mood “may be one component of a broader emotion dysregulation syndrome” (Drabick and Gadow 2012, p. 388).
Alongside research that used the Angry/Irritable Mood dimension of ODD to examine the co-occurrence of ODD and depression is an emerging body of research that examined the Child Behavior Check List Dysregulation Profile (CBCL-DP) as an indicator of a number of externalizing and internalizing disorders in children and adolescents. The CBCL-DP (formerly called the Juvenile Bipolar Disorder Profile; Biederman et al. 1995; Doerfler et al. 2011b), which is based on a profile of T-scores greater than 70 on the CBCL Anxious/Depressed, Aggression, and Attention Problems subscales, identifies youth who present with serious difficulties in mood, behavior, and cognition (Althoff 2010; Bellani et al. 2012; Doerfler et al. 2011a). Youth with elevated scores on this profile exhibit elevated irritability and anger, depression and anxiety and high rates of disruptive behavior (e.g., Biederman et al. 1995; Doerfler et al. 2011a, 2011b; Volk and Todd 2007). This profile is also associated with suicidal ideation and suicidal behavior (Ayer et al. 2009; Volk and Todd 2007) and substance abuse (Holtmann et al. 2011).
If, as suggested by Drabick and Gadow (2012), the Angry/Irritable Mood dimension of ODD is a component of a broader emotion dysregulation syndrome, youth who present with co-occurring ODD and depression may exhibit other internalizing (e.g., anxiety disorders) and externalizing (e.g., ADHD, anger) disorders or problems. To date, investigators have not compared the ODD Angry/Irritable Mood dimension and the CBCL-DP in the same study. Moreover, only one study has examined the relationship of the ODD Angry/Irritable Mood dimension with depression in a clinic-referred sample of youth.
The present study examined the relationship of the Angry/Irritable Mood symptoms of ODD with depression, as well as the relationship of the CBCL-DP, with co-occurring ODD and depression in a sample of youth who had been referred to a pediatric psychopharmacology clinic for evaluation. As noted above, relatively little is known about these relationships because most studies recruited community samples. Because anger and aggressive behavior have been associated with ODD and the CBCL-DP, several measures of anger and aggression were examined in this study. Categorical DSM diagnoses and dimensional measures of psychological symptoms (e.g., Children’s Depression Inventory) and related problems (e.g., Proactive/Reactive Aggression) were examined in this study.
We hypothesized that in comparison to youth diagnosed with ODD – but not co-occurring depressive disorder, youth who were diagnosed with ODD and co-occurring depressive disorder would exhibit a higher number of ODD Angry/ Irritable Mood symptoms. With respect to the CBCL-DP, we hypothesized that youth who met this profile would be more likely to be diagnosed with co-occurring ODD and depressive disorder than youth who did not meet the CBCL-DP profile.
Method
Participants and Procedure
Participants in this study were referred to the outpatient Pediatric Psychopharmacology Clinic at the University of Massachusetts Medical School. Children and adolescents referred to this clinic presented with a wide range of psychiatric disorders and problems and all youth referred to this clinic were included in the sample. The youth were systematically evaluated for psychopathology as part of the routine clinical evaluation in this clinic. Clinical assessment included information from the child, parent, and teacher. Evaluations included child psychiatrist-administered clinical and structured diagnostic interviews. The Schedule for Affective Disorders and Schizophrenia for School Age Children—Epidemiologic Version (K-SADS; Orvaschel 1995) was used to obtain DSM-IV diagnoses for each child. Diagnoses were assigned based on parental report data from the K-SADS. Parental report was emphasized because children under the age of 10 years may be unreliable when reporting symptoms (Edelbrock et al. 1986; Grills and Ollendick 2002; Schniering et al. 2000). Because many youth referred to this clinic were below 10 years old, parental report was used to maintain consistency in diagnostic procedures. Psychiatrists also conducted a clinical interview with each child. Children completed several self-report rating scales and parents and teachers completed rating scales assessing the child’s behavior. Parents and legal guardians provided clinical consent for all evaluation procedures. The study was approved by the University of Massachusetts Medical Center’s Institutional Review Board. Children with autism, mental retardation (IQ < 70), or unstable medical or neurological illness were excluded from the study. For the purposes of this study, the DSM-IV hierarchical exclusion rule stating that in the presence of a diagnosis of depression ODD is not diagnosed was ignored.
The sample included 310 children and adolescents (217 male, 93 female). The mean age of these youth was 10.65 years (SD = 3.4). With regard to racial background, 92% of the youth were Caucasian, 4% were Hispanic, 2% were African-American, 1% were Asian, and 2% were another ethnic group. In terms of annual family income, 26% earned less than $40,000, 13% earned $40,000–$49,000, 23% earned $50,000–$75,000, and 37% earned more than $75,000.
Of the 310 children and adolescents evaluated in this clinic, 164 (108 male, 56 female) received a diagnosis of oppositional defiant disorder according to the DSM-IV criteria (American Psychiatric Association. 2000). The 164 youth diagnosed with ODD comprised 53% of youth evaluated in this clinic. Mean age for youth diagnosed with ODD was 10.65 years (SD = 3.20). Of the youth evaluated in this clinic, 138 (90 male, 48 female) received a diagnosis of depression (Major Depressive Disorder or Dysthymia) according to the DSM-IV criteria (American Psychiatric Association. 2000). Youth diagnosed with depressive disorder comprised 45% of youth evaluated in this clinic. Mean age for youth diagnosed with depressive disorder was 10.71 years (SD = 3.12).
Measures
K-SADS
A board-certified child psychiatrist administered the K-SADS (Orvaschel 1995) individually to the parent or guardian about the referred child. A total of five child and adolescent psychiatrists conducted the interviews. Interrater reliability for diagnosis was assessed using the Kappa statistic (Cohen 1960) in a subsample of 53 children by two psychiatrists. These psychiatrists listened to audiotapes of the parent interview (N = 23) or observed the interview directly (N = 30). Interrater reliability was high (K = 0.87) for all diagnoses (current and lifetime). Interrater reliability for individual diagnoses was as follows: ADHD (K = 0.85), bipolar disorder (K = 0.79), conduct disorder (K = 1.0), oppositional defiant disorder (K = 1.0), tic disorder (K = 1.0), separation anxiety disorder (K = 0.92), panic disorder (K = 0.89), social phobia (K = 0.85), generalized anxiety disorder (K = 0.88), obsessive compulsive disorder (K = 1.0), and major depression (K = 0.84). For the 164 youth who received an ODD diagnosis, the number of ODD symptoms and a severity rating for each symptom were recorded by the child psychiatrist. Severity of each symptom was rated on a four-point scale (0 = no symptom reported, 1 = mild, 2 = moderate, 3 = severe). Along with diagnosis, information about ODD symptoms was examined in the present study.
Impairment and Overall Severity of Psychopathology
In addition to the DSM-IV diagnosis, the child psychiatrist rated impairment using the Children’s Global Assessment Scale (CGAS), which is a reliable measure of daily functioning and impairment (Green et al. 1994; Shaffer et al. 1983). Agreement on this scale was measured with the intraclass correlation coefficient (ICC; Bartko 1966) between child psychiatrists for 50 children. Agreement on this measure was good (ICC = 0.74). Severity of illness was assessed using the psychiatrist-rated Clinical Global Impression (CGI) Severity Scale (Guy 1976). This scale was used to assess severity of psychopathology regardless of diagnosis. The CGI is a 7-point rating scale that ranges from (1) “no signs of illness” to (4) “moderately ill” to (7) “extremely ill.” The scale has been shown to have acceptable concurrent validity in children with severe emotional disturbance (Mattison et al. 1990).
Child Behavior Check List
Parents completed the CBCL (Achenbach 1991), a 118-item parent-report measure of children’s behavioral and emotional problems. The CBCL contains eight narrowband scales (Anxious/Depressed, Withdrawn, Somatic Complaints, Social Problems, Delinquent Behavior, Thought Problems, Attention Problems, and Aggressive Behavior) and two broad-band scales (Internalizing Problems, Externalizing Problems). A Total Score can also be calculated. For this study, T scores are reported.
Children’s Depression Inventory
The CDI (Kovacs 1992) is a 27-item child self-report measure of depressive symptoms. The CDI has sound psychometric properties, including high internal consistency, test–retest reliability, and discriminant validity.
Aggression and hostility
Proactive and reactive aggression was assessed using the Proactive/Reactive Aggression Rating Scale (Dodge et al. 1997). This scale consists of three questions assessing reactive aggression and three questions assessing proactive aggression. Parents completed the Reactive/Proactive Aggression Rating Scale. The Buss Durkee Hostility Inventory (Buss, et al. 1956; Treiber et al. 1989) was used to assess the child’s self-report of hostility. This scale yields an Expressed Hostility subscale, an Experienced Hostility subscale, and a Total Hostility score. The Modified Overt Aggression Scale (MOAS; Sorgi et al. 1991; Yudofsky et al. 1986) is a 20-item scale that assessed the frequency and severity of overt aggression during the previous month. Parents completed this scale. The MOAS assessed four categories of aggression: Verbal Aggression (threats to harm others), Object Aggression, (impulsive property destruction), Self-Aggression (self-injurious behavior), and Other Aggression (physical assault).
Data Analysis Plan
This study had two major hypotheses. Hypothesis 1 stated that youth who were diagnosed with ODD and co-occurring depressive disorder would exhibit a higher number of Angry/Irritable Mood symptoms than youth who were diagnosed with ODD but not co-occurring depressive disorder. The K-SADS (Orvaschel 1995) was used to assign ODD and depressive disorder diagnoses. Analyses for Hypothesis 1 used the subsample of 164 youth who were diagnosed with ODD. For these analyses, youth diagnosed with co-occurring ODD and depressive disorder were compared to youth who were diagnosed with ODD but not co-occurring depressive disorder for the number of ODD Angry/Irritable Mood symptoms, as well as other measures of psychopathology and functioning. Logistic regression analysis was then conducted to determine whether the number of ODD Angry/Irritable Mood symptoms differentiated youth with co-occurring ODD and depressive disorder from youth diagnosed with ODD without a co-occurring depressive disorder.
Hypothesis 2 stated that youth who met the CBCL-DP would be more likely to be diagnosed with co-occurring ODD and depressive disorder than youth who did not meet the CBCL-DP. Analyses for Hypothesis 2 used the entire sample of 310 youth who were referred to the clinic for evaluation. For these analyses, chi-square analyses were conducted to determine whether youth who fit the CBCL-DP were more likely than youth who did not fit the profile to be diagnosed with ODD or a depressive disorder. t-tests were then conducted to determine whether youth who fit the CBCL-DP exhibited higher levels of psychopathology and poorer functioning than youth who did not fit this profile. Finally, logistic regression analysis was conducted to determine whether the CBCL-DP would differentiate youth with co-occurring ODD and depressive disorder from youth diagnosed with ODD without co-occurring depressive disorder.
Results
Of the 310 youth in the overall sample, 86 (28%) were diagnosed with ODD without co-occurring depressive disorder, 60 (19%) were diagnosed with depressive disorder without co-occurring ODD, and 78 (25%) were diagnosed with co-occurring ODD and depressive disorder. Diagnosis of depressive disorder was not associated with the ODD diagnosis in this sample, X2 (1) = 1.31. The groups differed significantly for age, but not gender or ethnicity. A 2 (ODD diagnosis) X 2 (depressive disorder diagnosis) ANOVA showed a significant difference in age among the groups, F (31, 306) = 9.60, p < 0.001. There was a significant age difference for depression diagnosis, F (1, 306) = 27.18, p < 0.001, indicating that youth diagnosed with depression (M = 11.71 years, SD = 3.12) were older than youth who did not receive a depression diagnosis (M = 9.79 years, SD = 3.43). There were no significant differences for ODD diagnosis, F (1, 306) = 0.23. Mean age for youth diagnosed with ODD was 10.65 years (SD = 3.20); mean age for youth who did not receive an ODD diagnosis was 10.64 years (SD = 3.68).
Relationship of ODD Angry/Irritable Mood Symptoms with Depressive Disorder
ODD Symptoms
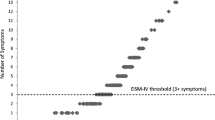
The mean number of symptoms for youth who were diagnosed with ODD was 6.20 (SD = 1.23). The mean number of Angry/Irritable Mood symptoms was 2.51 (SD = 0.74), and the mean number of Argumentative/Defiant Behavior symptoms was 3.43 (SD = 0.71). Parents reported that roughly a quarter of youth with ODD (N = 44) were spiteful or vindictive. Table 1 provides the frequencies for the Angry/Irritable Mood and Argumentative/Defiant Behavior symptom scores. Cronbach’s alpha for the number of Angry/Irritable Mood symptoms was 0.39 and Cronbach’s alpha for the number of Argumentative/Defiant Behavior symptoms was 0.14. Cronbach’s alpha for the Total number of ODD symptoms was 0.36.
The correlation of the number of Angry/Irritable Mood symptoms with Argumentative/ Defiant Behavior symptoms was 0.18. The correlation of the number of Angry/Irritable Mood symptoms with the Total Number of ODD symptoms was 0.67. The correlation of the number of Argumentative/Defiant Behavior symptoms with the Total Number of ODD symptoms was 0.67.
The mean severity rating for Angry/Irritable Mood symptoms was 2.51 (SD = 0.74). The mean severity rating for Argumentative/Defiant Behavior symptoms was 3.43 (SD = 0.72). The mean severity rating for with the Total ODD symptoms was 6.21 (SD = 1.25).
The correlation of the severity ratings of Angry/Irritable Mood symptoms with severity ratings of Argumentative/ Defiant Behavior symptoms was 0.02. The correlation of the severity ratings of Angry/Irritable Mood symptoms with the severity ratings of Total ODD symptoms was 0.67. The correlation of the severity ratings of Argumentative/Defiant Behavior symptoms with severity ratings of Total ODD symptoms was 0.68.
Table 2 presents the means and standard deviations for the number of Angry\Irritable Mood, Argumentative/Defiant Behavior, and Total ODD symptoms for youth diagnosed with ODD without co-occurring depressive disorder and youth diagnosed with both ODD and depressive disorder. The groups did not differ for the number of Angry\ Irritable Mood, t (162) = 0.96, Argumentative/Defiant Behavior, t (162) = 0.16, and Total ODD symptoms, t (162) = 1.18. Because the same results were obtained for ODD symptom severity ratings, those results are not reported in Table 2.
Association of ODD Symptoms with Psychopathology and Functioning
Table 3 presents correlations for number of Angry\Irritable Mood, Argumentative/ Defiant Behavior, and Total ODD symptoms with measures of internalizing problems, externalizing problems, and overall severity of psychopathology. The number of Angry\Irritable Mood symptoms showed a low correlation with scores on the CDI (r = .01), CBCL Anxious/ Depressed subscale (r = 0.07), and CBCL Internalizing Symptoms subscale (r = 0.00). In contrast, Reactive Aggression (r = 0.29), MOAS Verbal Aggression (r = 0.21), MOAS Self-Aggression (r = .24), and Total MOAS Score (r = 0.21) correlated significantly with the number of Angry\Irritable Mood symptoms.
There were significant correlations between the number of Argumentative/Defiant Behavior symptoms and the Buss-Durkee Hostility score (r = 0.18), Reactive Aggression (r = 0.28), Proactive Aggression (r = 0.31), and the CBCL Aggressive Behavior subscale (r = 0.18). The Total Number of ODD symptoms correlated significantly with measures of anger and aggressive behavior, but not depressive and anxious symptoms.
Logistic regression analysis
Logistic regression analysis was conducted to determine whether the number of ODD Angry/Irritable Mood symptoms would differentiate youth with co-occurring ODD and depressive disorder from youth diagnosed with ODD without a co-occurring depressive disorder. Predictors in this analysis included the child’s age, sex, ethnicity, and number of ODD Angry/Irritable Mood symptoms. Variables were entered into the regression equation in two steps. Demographic variables were entered in the first step, followed by the number of ODD Angry/Irritable Mood symptoms. When considered together, the demographic variables significantly predicted youth who were diagnosed with ODD and co-occurring depressive disorder, X2 (6) = 13.38, p < 0.05. Of the demographic variables, only age was a significant predictor of a depressive disorder diagnosis among youth who had been diagnosed with ODD, β = 0.14, S.E. = 0.05, Wald = 6.67, p < 0.01.
When age was included in the regression equation, 67.4% of youth were correctly identified as having ODD without co-occurring depressive disorder and 55.1% of youths were correctly identified as having ODD with co-occurring depressive disorder. Overall, the regression equation correctly identified 61.6% of youth, which was an improvement over the base rate of 52.4% of youth who were diagnosed with ODD without a co-occurring depressive disorder. The number of Angry/Irritable Mood symptoms did not improve the prediction equation when entered in the second step of the analysis, X2 (1) = 0.39.
A second logistic regression analysis was conducted, entering the number of Angry/ Irritable Mood symptoms, number of Argumentative/Defiant Behavior symptoms, and number of Vindictive/Spiteful symptoms in the second step of the analysis. When controlling for demographic variables, the full set of the number of ODD symptoms did not improve the prediction equation, X2 (3) = 1.89.
CBCL-DP Profile Analyses
Of the 310 youth evaluated in this clinic, 55 (42 males, 13 females; 18% of the overall sample) had a T-score >70 on the CBCL Anxious/Depressed, Aggression, and Attention subscales. The remaining 255 youth (175 male, 80 female) did not fit the CBCL-DP profile. The groups did not differ in age, t (308) = 0.76, gender, X2 (1) = 1.29, N = 310, or racial background, X2 (4) = 0.91, N = 310.
With respect to the diagnosis of ODD, youth with the CBCL-DP profile were more likely to be diagnosed with ODD than youth who did not fit the profile, X2 (1) = 5.54, p < 0.05, N = 310. Of the 55 youth who did fit the profile, 37 (67%) were diagnosed with ODD. In contrast, 127 youth (50%) who did not fit the profile were diagnosed with ODD.
Youth who fit the CBCL-DP profile also were more likely to be diagnosed with depressive disorder than youth who did not fit the profile, X2 (1) = 6.49, p < 0.05, N < 0.05. Of the 55 youth who fit the CBCL-DP profile, 33 (60%) were diagnosed with a depressive disorder. There were 105 youth (41%) who did not fit the profile but were diagnosed with a depressive disorder.
Psychopathology and functioning of the CBCL-DP Group
t-tests were conducted to compare youth who fit the CBCL-DP profile with youth who did not fit the profile. Table 4 presents the means and standard deviations for measures of depression, daily functioning and impairment, hostility, and aggressive behavior. Results of the t tests also are presented in Table 4. With respect to self-reported depression on the CDI, youth who fit the CBCL-DP profile did not differ from youth who did not fit the profile, t (256) = 1.86.
However, youth who fit the CBCL-DP profile were rated by the child psychiatrist on the CGAS as exhibiting poorer daily functioning. In addition, in comparison to youth who did not fit the CBCL-DP profile, youth who did fit the profile were rated as exhibiting significantly higher levels of aggression on the following measures: Reactive Aggression, Proactive Aggression, MOAS Verbal Aggression, MOAS Object Aggression, MOAS Self-Aggression, MOAS Other Aggression, and Total MOAS Score.
CBCL-DP Logistic Regression Analysis
Logistic regression analysis was conducted to determine whether the CBCL-DP profile would differentiate youth with co-occurring ODD and depressive disorder from youth diagnosed with ODD without a co-occurring depressive disorder. Predictors in this analysis included the child’s age, sex, ethnicity, and number of ODD Angry/Irritable Mood symptoms. Variables were entered into the regression equation in two steps. Demographic variables were entered in the first step, followed by the CBCL-DP profile variable. When considered together, the demographic variables significantly predicted youth who were diagnosed with ODD and co-occurring depressive disorder, X2 (6) = 13.38, p < 0.05. Of the demographic variables, only age was a significant predictor of a depressive disorder diagnosis among youth who had been diagnosed with ODD, β = 0.14, S.E. = 0.05, Wald = 6.67, p < 0.01.
When age was included in the regression equation, 65.1% of youth were correctly identified as having ODD without co-occurring depressive disorder and 53.8% of youth were correctly identified as having ODD with co-occurring depressive disorder. Overall, the regression equation correctly identified 59.8% of youth, which was an improvement over the base rate of 52.4% of youth who were diagnosed with ODD without a co-occurring depressive disorder.
After demographic variables were accounted for, the CBCL-DP profile differentiated youth with co-occurring ODD and depressive disorder from youth diagnosed with ODD without a co-occurring depressive disorder, X2 (1) = 4.39, p < 0.05, β = 0.82, S.E. = 0.40, Wald = 4.24, p < 0.05. When the CBCL-DP profile was included in the regression equation, 67.4% of youth were correctly identified as having ODD without co-occurring depressive disorder and 59.0% of youth were correctly identified as having ODD with co-occurring depressive disorder. Overall, the final regression equation correctly identified 63.4% of youth.
Discussion
Results of the present study did not support the hypothesis that ODD Angry/Irritable Mood symptoms are differentially associated with depression in a clinic-referred sample of ODD youth evaluated using a cross-sectional methodology and assessed at the time of evaluation. Controlling for demographic variables, our results did support the hypothesis that the parent-report CBCL dysregulation profile differentiates youth with co-occurring ODD and depressive disorder from ODD youth without depression in our sample. This is consistent with previous research showing that youth identified by this profile may exhibit broad dysfunction across both internalizing and externalizing symptom domains (Drabick and Gadow 2012), and specifically extends this finding to include ODD youth with and without depression. One possible reason that the CBCL-DP differentiated youth with co-occurring ODD and depressive disorder from ODD youth without depression is that the profile is based in part on T scores on the CBCL Anxious/Depressed subscale. Hence, the overlap in the content of the CBCL-DP and K-SADS diagnostic criteria may have influenced this result. Our results also supported previous research finding that the CBCL dysregulation profile does not identify any specific psychiatric disorder but instead identifies a broad range of disorders associated with emotional and behavioral dysregulation (Drabick and Gadow 2012).
In contrast to the findings for the depression measures, parent ratings of aggression on the Modified Overt Aggression Scale (Sorgi et al. 1991; Yudofsky et al. 1986) and Reactive Aggression on the Proactive/Reactive Aggression Scale (Dodge et al. 1997) correlated significantly with the number of Angry/Irritable Mood symptoms. The number of ODD Argumentative/Defiant Behavior symptoms showed a different pattern, and instead correlated significantly with both Proactive and Reactive Aggression, as well as parent ratings on the CBCL Aggressive Behavior scale. This pattern of results suggests that the aggressive behavior assessed by the Modified Overt Aggression Scale (e.g., verbal aggression) in our sample involves negative emotion regulation and reactivity, which may be associated with the irritability dimension of ODD. It should be noted that reactive aggression, which is considered to be an emotion-driven form of aggression, but not proactive aggression, correlated significantly with Angry/Irritable Mood symptoms.
The present findings suggested that in clinic-referred youth, the presence of Angry/Irritable Mood symptoms may reflect a broad range of difficulties related to emotion regulation. That is, ODD Angry/Irritable Mood symptoms may be related to anxiety or anger, as well as depression. This hypothesis is consistent with emerging research showing that irritability is not associated with a specific disorder, but instead is linked with a variety of internalizing and externalizing disorders and problems (Brotman et al. 2017; Evans et al. 2016a, b; Leibenluft and Stoddard 2013). One possible explanation for the inconsistency between the present findings and the results reported by Stringaris and colleagues (Stringaris and Goodman 2009a, 2009b, 2009c; Stringaris et al. 2010) is that in contrast to community samples, clinic-referred youth have higher rates of co-occurring disorder (Angold et al. 1999) and more severe symptomatology.
Presently, it is unclear how community samples relate to clinical samples. In particular, were the youth in Stringaris and Goodman’s community sample, who were diagnosed with ODD based on a structured interview administered by lay interviewers, the same youth who were referred to an outpatient mental health clinic and diagnosed with ODD? Additional research is required to determine how well findings from community samples can be generalized to clinical samples.
Aside from sample differences, a methodological issue could be responsible for the inconsistency between the present findings and the results reported by Stringaris and colleagues. In the present study, Cronbach’s alpha for the ODD Angry/Irritable Mood measure was .39. Low internal consistency indicated that in the present sample, Angry/Irritable Mood was not a unitary construct. However, Stringaris and colleagues (Stringaris and Goodman 2009a, 2009b, 2009c; Stringaris et al. 2010) did not report internal consistency for the Angry/Irritable Mood measure in their sample, precluding direct examination of this issue. Future investigators are encouraged to report the internal consistency of the ODD Angry/Irritable Mood and Argumentative/Defiant Behavior measures.
An alternative explanation is that youth who exhibit oppositional and defiant behavior along with chronic anger or irritability may experience a more severe type of ODD (Drabick and Gadow 2012; Evans et al. 2016a, b). Reflecting a referral bias, clinic samples are more likely to include youth who present with a more severe type of ODD. Future investigators are encouraged to explore whether clinic-referred youth with co-occurring ODD and depression are more likely to be diagnosed with anxiety disorders (generalized anxiety disorder, panic disorder), other disruptive behavior disorders, or impairment in social or academic functioning.
Transdiagnostic conceptualizations of psychopathology have gained prominence in the past decade, and irritability has emerged as a transdiagnostic feature because it has been linked to several internalizing and externalizing disorders in children (Brotman et al. 2017; Leibenluft and Stoddard 2013). Irritability’s severity can vary from transient and mild to chronic and severe, and as noted by Stringaris et al. (2018), severity of irritability is indicated by the frequency and intensity of angry responses, as well as duration of irritable mood. Despite the increasing evidence that irritability is associated with significant adverse psychosocial outcomes (Stringaris et al. 2018; Brotman et al. 2017), there is a lack of clarity in the definition and measurement of this construct (Toohey and DiGiuseppe 2017). This issue could account for the present findings. In this study, ODD Angry/Irritable Mood symptoms correlated significantly with measures of anger and aggression, but failed to differentiate youth who experienced co-occurring ODD and depression from youth who were diagnosed with ODD without co-occurring depression. In contrast, youth identified by the CBCL-DP, which included parental report that youth exhibit significant elevation of depressed and anxious symptomatology, differentiated depressed and non-depressed ODD youth. As reflected in the present study, most definitions of and measures of irritability fail to clarify the relationship between anger and sadness, and the link with irritability may depend on the specific measure used by investigators.
The different pattern of findings for the ODD Angry/Irritable Mood symptoms and CBCL-DP may be explained by the overlap in the measures of Angry/Irritable Mood symptoms (and CPCL-DP) with measures of anger/aggression (or emotional disorders). As recommended by Toohey and DiGiuseppe (2017), future investigators should adopt a more specific definition of irritability (and emotion dysregulation) that clearly differentiates it from related constructs.
In the present study, youth who were diagnosed with co-occurring ODD and depression were older than youth who were diagnosed with ODD without depression. Nonetheless, for many youth in this sample, onset of depression occurred prior to adolescence. Because childhood onset of depression predicts a range of psychological disorders, children who present with co-occurring ODD and depression “may not have a depressive disorder as such, but rather suffer from marked emotional and behavioral dysfunction that eventually coalesces into nondepressive psychopathology” (Hammen et al. 2014, p 229). Future investigations should examine the association between ODD and depression in youth with adolescent-onset depressive disorder.
The present study has several strengths. In contrast to some other studies (e.g., Stringaris and Goodman 2009a, 2009b, 2009c; Stringaris et al. 2010), structured diagnostic interviews conducted by child and adolescent psychiatrists were used to assign ODD and depressive disorder diagnoses. In addition, parent- and child-report measures were used to assess youth internalizing symptoms (depression, anger). Both categorical (DSM-IV diagnoses) and dimensional (e.g., CBCL and CDI scores) of youth psychopathology were examined in this study.
Several limitations to our study should be considered. Our methodology was cross-sectional and data accrued from a single time point. Results examining longitudinal ODD outcomes may be different. Next, our results are based on a clinical sample, which may not be representative of ODD youth who are not referred for treatment. However, few extant studies have examined correlations between ODD and depression symptoms in a clinical sample, so this is also a strength of our methodology. Internal consistency of the Angry/Irritable Mood symptom measure was low, which could be the reason that the measure did not differentiate depressed and non-depressed ODD youth in this study. The present study did not control for co-occurring anxiety disorders or ADHD, which are closely related to depression and ODD. Finally, many youth in the sample had not yet reached puberty. As a result, some youth in the ODD without depression group may have developed a depressive disorder during adolescence.
In conclusion, our results support the importance of emotional and behavioral dysregulation in identifying differences between ODD youth with/without depression. Our results also support previous research identifying the importance of the parent-report CBCL Dysregulation Profile in identifying emotionally dysregulated at-risk youth.
References
Achenbach, T. M. (1991). Manual for the child behavior check list/4-18 and 1991 profile. Burlington: University of Vermont, Department of Psychiatry.
Althoff, R. R. (2010). Dysregulated children reconsidered. Journal of the American Academy of Child & Adolescent Psychiatry, 49(4), 302–305. https://doi.org/10.1097/00004583-201004000-00004.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: Author. Text Revision.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. 5th ed. Washington, D.C.: Author.
Angold, A., Costello, E. J., & Erkanli, A. (1999). Comorbidity. Journal of Child Psychology and Psychiatry, 40(1), 57–87. https://doi.org/10.1111/1469-7610.00424.
Ayer, L., Althoff, R., Ivanova, M., Rettew, D., Waxler, E., Sulman, J., & Hudziak, J. (2009). Child behavior checklist juvenile bipolar disorder (CBCL-JBD) and CBCL posttraumatic stress problems (CBCL-PTSP) scales are measures of a single dysregulatory syndrome. Journal of Child Psychology and Psychiatry, 50(10), 1291–1300. https://doi.org/10.1111/j.1469-7610.2009.02089.x.
Bartko, J. J. (1966). The intraclass correlation coefficient as a measure of reliability. Psychological Reports, 19(1), 3–11. https://doi.org/10.2466/pr0.1966.19.1.3.
Bellani, M., Negri, G. A. L., & Brambilla, P. (2012). The dysregulation profile in children and adolescents: A potential index for major psychopathology? Epidemiology and Psychiatric Sciences, 21(2), 155–159. https://doi.org/10.1017/S2045796011000849.
Biederman, J., Wozniak, J., Kiely, K., Ablon, S., Faraone, S., Mick, E., & Kraus, I. (1995). CBCL clinical scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry, 34(4), 464–471. https://doi.org/10.1097/00004583-199504000-00013.
Boylan, K., Vaillancourt, T., Boyle, M., & Szatmari, P. (2007). Comorbidity of internalizing disorders in children with oppositional defiant disorder. European Child & Adolescent Psychiatry, 16(8), 484–494. https://doi.org/10.1007/s00787-007-0624-1.
Brotman, M. A., Kircanski, K., & Leibenluft, E. (2017). Irritability in children and adolescents. Annual Review of Clinical Psychology, 13, 317–341. https://doi.org/10.1146/annurev-clinpsy-032816-044941.
Burke, J., & Loeber, R. (2010). Oppositional defiant disorder and the explanation of the comorbidity between behavioral disorders and depression. Clinical Psychology Science and Practice, 17(4), 319–326. https://doi.org/10.1111/j.1468-2850.2010.01223.x.
Burke, J. D. (2012). An affective dimension within oppositional defiant disorder symptoms among boys: Personality and psychopathology outcomes into early adulthood. Journal of Child Psychology and Psychiatry, 53(11), 1176–1183. https://doi.org/10.1111/j.1469-7610.2012.02598.x.
Burke, J. D., Boylan, K., Rowe, R., Duku, E., Stepp, S. D., Hipwell, A. E., & Waldman, I. D. (2014). Identifying the irritability dimension of ODD: application of a modified bifactor model across five large community samples of children. Journal of Abnormal Psychology, 123(4), 841–851. https://doi.org/10.1037/a0037898.
Burke, J. D., Hipwell, A. E., & Loeber, R. (2010). Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child & Adolescent Psychiatry, 49(5), 484–492. https://doi.org/10.1097/00004583-201005000-00009.
Burke, J. D., Loeber, R., Lahey, B. B., & Rathouz, P. J. (2005). Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry, 46(11), 1200–1210. https://doi.org/10.1111/j.1469-7610.2005.00422.x.
Buss, A. H., Durkee, A., & Baer, M. B. (1956). The measurement of hostility in clinical situations. The Journal of Abnormal and Social Psychology, 52(1), 84–86. https://doi.org/10.1037/h0048398.
Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20, 37–46. https://doi.org/10.1177/001316446002000104.
Copeland, W. E., Shanahan, L., Costello, J., & Angold, A. (2009). Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry, 66(7), 764–772. https://doi.org/10.1001/archgenpsychiatry.2009.85.
Costello, E. J., Mustillo, S., Erkanli, A., Keeler, G., & Angold, A. (2003). prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60(8), 837–844. https://doi.org/10.1001/archpsyc.60.8.837.
Dodge, K. A., Lochman, J. E., Harnish, J. D., Bates, J. E., & Pettit, G. S. (1997). Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. Journal of Abnormal Psychology, 106(1), 37–51. https://doi.org/10.1037/0021-843X.106.1.37.
Doerfler, L. A., Connor, D. F., & Toscano, Jr, P. F. (2011a). Aggression, ADHD symptoms, and dysphoria in children and adolescents diagnosed with bipolar disorder and ADHD. Journal of Affective Disorders, 131(1-3), 312–319. https://doi.org/10.1016/j.jad.2010.11.029.
Doerfler, L. A., Connor, D. F., & Toscano, Jr, P. F. (2011b). The CBCL bipolar profile and attention, mood, and behavior dysregulation. Journal of Child and Family Studies, 20(5), 545–553. https://doi.org/10.1007/s10826-010-9426-z.
Drabick, D. A. G., & Gadow, K. D. (2012). Deconstructing oppositional defiant disorder: Clinic-based evidence for an anger/irritability phenotype. Journal of the American Academy of Child & Adolescent Psychiatry, 51(4), 384–393. https://doi.org/10.1016/j.jaac.2012.01.010.
Edelbrock, C. S., Costello, A. J., Dulcan, M. K., Conover, N. C., & Kala, R. (1986). Parent–child agreement on child psychiatric symptoms assessed via structured interview. Child Psychology & Psychiatry & Allied Disciplines, 27(2), 181–190. https://doi.org/10.1111/j.1469-7610.1986.tb02282.x.
Evans, S. C., Pederson, C. A., Fite, P. J., Blossom, J. B., & Cooley, J. L. (2016a). Teacher-reported irritable and defiant dimensions of oppositional defiant disorder: social, behavioral, and academic correlates. School Mental Health, 8(2), 292–304. https://doi.org/10.1007/s12310-015-9163-y.
Evans, S. C., Pederson, C. A., Fite, P. J., Blossom, J. B., & Cooley, J. L. (2016b). Teacher-reported irritable and defiant dimensions of oppositional defiant disorder: social, behavioral, and academic correlates. School Mental Health, 8(2), 292–304. https://doi.org/10.1007/s12310-015-9163-y.
Green, B., Shirk, S., Hanze, D., & Wanstrath, J. (1994). The children’s global assessment scale in clinical practice: an empirical evaluation. Journal of the American Academy of Child & Adolescent Psychiatry, 33(8), 1158–1164. https://doi.org/10.1097/00004583-199410000-00011.
Grills, A. E., & Ollendick, T. H. (2002). Issues in parent-child agreement: the case of structured diagnostic interviews. Clinical Child and Family Psychology Review, 5(1), 57–83. https://doi.org/10.1023/A:1014573708569.
Guy, W. (1976). Assessment manual for psychopharmacology. Washington, DC: U S Department of Health, Education, and Welfare.
Hammen, C. L., Rudolph, K. D., & Abaied, J. L. (2014). Child and adolescent depression. In E.J. Mash & R.A. Barkley (Eds.), Child psychopathology., 3rd ed. (pp. 225-263). New York, NY: Guilford Press.
Hipwell, A. E., Stepp, S., Feng, X., Burke, J., Battista, D. R., Loeber, R., & Keenan, K. (2011). Impact of oppositional defiant disorder dimensions on the temporal ordering of conduct problems and depression across childhood and adolescence in girls. Journal of Child Psychology and Psychiatry, 52(10), 1099–1108. https://doi.org/10.1111/j.1469-7610.2011.02448.x.
Holtmann, M., Buchmann, A. F., Esser, G., Schmidt, M. H., Banaschewski, T., & Laucht, M. (2011). The child behavior checklist‐dysregulation profile predicts substance use, suicidality, and functional impairment: a longitudinal analysis. Journal of Child Psychology and Psychiatry, 52(2), 139–147. https://doi.org/10.1111/j.1469-7610.2010.02309.x.
Kovacs, M. (1992). Children’s depression inventory. North Tonawanda, NY: Western Psychological Services.
Leibenluft, E., & Stoddard, J. (2013). The developmental psychopathology of irritability. Development and Psychopathology, 25(4, Pt 2), 1473–1487. https://doi.org/10.1017/S0954579413000722.
Mattison, R. E., Bagnato, S. J., Mayes, S. D., & Felix, B. C. (1990). Reliability and validity of teacher diagnostic ratings for children with behavioral and emotional disorders. Journal of Psychoeducational Assessment, 8(4), 509–517. https://doi.org/10.1177/073428299000800406.
Maughan, B., Rowe, R., Messer, J., Goodman, R., & Meltzer, H. (2004). Conduct Disorder and Oppositional Defiant Disorder in a national sample: developmental epidemiology. Journal of Child Psychology and Psychiatry, 45(3), 609–621. https://doi.org/10.1111/j.1469-7610.2004.00250.x.
Merikangas, K. R., He, J.-p, Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., & Swendsen, J. (2010). Lifetime prevalence of mental disorders in US adolescents: results from the national comorbidity survey replication-adolescent supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. https://doi.org/10.1016/j.jaac.2010.05.017.
Nock, M. K., Kazdin, A. E., Hiripi, E., & Kessler, R. C. (2007). Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: results from the national comorbidity survey replication. Journal of Child Psychology and Psychiatry, 48(7), 703–713. https://doi.org/10.1111/j.1469-7610.2007.01733.x.
Ollendick, T. H., Booker, J. A., Ryan, S., & Greene, R. W. (2018). Testing multiple conceptualizations of oppositional defiant disorder in youth. Journal of Clinical Child and Adolescent Psychology, 47(4), 620–633. https://doi.org/10.1080/15374416.2017.1286594.
Orvaschel, H. (1995). Schedule for affective disorders and schizophrenia for school-aged children. Epidemiologic version - 5. Studies, Nova Southeastern University. Fort Lauderdale, FL: Center for Psychological.
Safer, D. J. (2009). Irritable mood and the diagnostic and statistical manual of mental disorders. Child and Adolescent Psychiatry and Mental Health, 3. https://doi.org/10.1186/1753-2000-3-35.
Schniering, C. A., Hudson, J. L., & Rapee, R. M. (2000). Issues in the diagnosis and assessment of anxiety disorders in children and adolescents. Clinical Psychology Review, 20(4), 453–478. https://doi.org/10.1016/S0272-7358(99)00037-9.
Shaffer, D., Gould, M. S., Brasic, J., Ambrosini, P., Fisher, P., Bird, H., & Aluwahlia, S. (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. https://doi.org/10.1001/archpsyc.1983.01790100074010.
Sorgi, P., Ratey, J. J., Knoedler, D. W., Markert, R. J., & Reichman, M. (1991). Rating aggression in the clinical setting: a retrospective adaptation of the overt aggression scale: preliminary results. The Journal of Neuropsychiatry and Clinical Neurosciences, 3(2), S52–S56.
Stringaris, A., & Goodman, R. (2009a). Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. Journal of the American Academy of Child & Adolescent Psychiatry, 48(4), 404–412. https://doi.org/10.1097/CHI.0b013e3181984f30.
Stringaris, A., & Goodman, R. (2009b). Mood lability and psychopathology in youth. Psychological Medicine, 39(8), 1237–1245. https://doi.org/10.1017/S0033291708004662.
Stringaris, A., & Goodman, R. (2009c). Three dimensions of oppositionality in youth. Journal of Child Psychology and Psychiatry, 50(3), 216–223. https://doi.org/10.1111/j.1469-7610.2008.01989.x.
Stringaris, A., Maughan, B., & Goodman, R. (2010). What is a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: findings from the avon longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry, 49(5), 474–483. https://doi.org/10.1097/00004583-201005000-00008.
Stringaris, A., Vidal‐Ribas, P., Brotman, M. A., & Leibenluft, E. (2018). Practitioner review: definition, recognition, and treatment challenges of irritability in young people. Journal of Child Psychology and Psychiatry, 59(7), 721–739. https://doi.org/10.1111/jcpp.12823.
Toohey, M. J., & DiGiuseppe, R. (2017). Defining and measuring irritability: construct clarification and differentiation. Clinical Psychology Review, 53, 93–108. https://doi.org/10.1016/j.cpr.2017.01.009.
Treiber, F. A., Musante, L., Riley, W. T., Mabe, P. A., Carr, T., Levy, M., & Strong, W. B. (1989). The relationship between hostility and blood pressure in children. Behavioral Medicine, 15(4), 173–178. https://doi.org/10.1080/08964289.1989.9934581.
Volk, H. E., & Todd, R. D. (2007). Does the child behavior checklist juvenile bipolar disorder phenotype identify bipolar disorder? Biological Psychiatry, 62(2), 115–120. https://doi.org/10.1016/j.biopsych.2006.05.036.
Wolff, J. C., & Ollendick, T. H. (2006). The comorbidity of conduct problems and depression in childhood and adolescence. Clinical Child and Family Psychology Review, 9(3-4), 201–220. https://doi.org/10.1007/s10567-006-0011-3.
Yudofsky, S. C., Silver, J. M., Jackson, W., Endicott, J., & Williams, D. (1986). The overt aggression scale for the objective rating of verbal and physical aggression. The American Journal of Psychiatry, 143(1), 35–39. https://doi.org/10.1176/ajp.143.1.35.
Author Contributions
L.A.D. designed the study, conducted the data analyses, and wrote the first draft of the paper. A.M.V. and D.F. C. collaborated with the design and writing of the paper, and D.F.C. conducted the clinical evaluations of the youth who participated in this study.
Funding
The first author received support from the Assumption College Faculty Grant Program to write this research report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the parents or guardians for all individual participants included in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Doerfler, L.A., Volungis, A.M. & Connor, D.F. Co-occurence and Differentiation of Oppositional Defiant and Mood Disorders among Children and Adolescents. J Child Fam Stud 29, 2568–2579 (2020). https://doi.org/10.1007/s10826-020-01756-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-020-01756-8