Abstract
Pediatric obsessive–compulsive disorder (OCD) is a chronic condition affecting millions of children. Though well intentioned, accommodation (i.e., a parent’s attempt to assuage their child’s distress and anxiety) is thought to increase OCD symptom severity and may cause greater OCD-related impairment. The present study sought to examine the relative contribution of parental accommodation in predicting OCD symptom severity. Children between the ages of 6 and 18 (and their parents) participated in a prospective, longitudinal study investigating the course of pediatric OCD utilizing a longitudinal design. Data was collected at intake (n = 30) and two-years (n = 22) post-intake controlling for age, anxiety and depression. Parental accommodation (measured at intake) significantly predicted OCD symptom severity and was the strongest predictor at both intake and two-year follow-up. These preliminary findings highlight the importance of further research seeking to delineate factors relevant to the development and maintenance of accommodation as well as parent-level variables that might mediate the relationship between accommodation and OCD symptom severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obsessive compulsive disorder (OCD) is a chronic and impairing psychiatric disorder that is relatively common in children and highly comorbid with other Axis I disorders, with 75–84 % of these children also meeting diagnostic criteria for at least one other psychiatric disorder (Geller 2006; Geller et al. 1996) Between 1.5 and 2.2 million children in the United States are affected (2–3 % prevalence rate; (Valleni-Basile et al. 1994; Zohar 1999) and the disorder leads to significant distress and impairment in several life domains, including social, academic, and family functioning (Association 2000; Lewin et al. 2006; Piacentini et al. 2007; Storch et al. 2007). Children’s OCD-related symptoms impact and are impacted by their family members (Flessner et al. 2011). Families may experience distress and disruptions in social (e.g., avoidance of people and experiences that might cause the child distress; (Storch et al. 2007) occupational (e.g., lateness for work as a result of time spent accommodating compulsions) and daily (e.g., serving as a key component in a bedtime ritual) functioning as a result of their participation in, and/or facilitation of the child’s OCD-related symptoms (Storch et al. 2007). The aforementioned disruption in a family’s day-to-day functioning (via participation in or facilitation of OCD symptoms) has been termed parental accommodation and has been shown to be highly prevalent amongst families of children with OCD (Peris et al. 2008). Though well-intentioned, substantial evidence links increased accommodation to increased impairment and greater OCD-related symptom severity in children (Albert et al. 2010; Maina et al. 2006; Merlo et al. 2009; Steketee and Van Noppen 2003; Stengler-Wenzke et al. 2006) by increasing the family’s involvement in rituals and reinforcing avoidance (Storch et al. 2007). Empirical evidence also points to a greater incidence of family dysfunction, depression, and anxiety in family members with greater levels of accommodation (Flessner et al. 2011, 2009; Merlo et al. 2009). These data clearly point to the importance of accommodation for developing a more comprehensive understanding of OCD during childhood and highlight the importance of research within this domain.
Significant gaps still remain in our understanding of the correlates and effects of accommodation on OCD symptoms in childhood. For example, increased parental accommodation is known to have a significant and positive association with OCD symptom severity in children. Because parental accommodation is such a ubiquitous phenomenon amongst these families, it is important to assess not only the immediate impact of accommodation on symptom severity (i.e., a “one-shot” assessment), but also its impact at later points in time. Such evidence, in combination with past research, may help to inform the development of new and more robust interventions. This line of inquiry, however, can only be undertaken through the use of longitudinal research which, to date, is largely non-existent within the child OCD literature. While a very small number of studies exist examining family accommodation in pediatric obsessive–compulsive disorder longitudinally (Merlo et al. 2009; Piacentini et al. 2011), these studies have examined accommodation within a treatment context rather than utilizing a prospective, longitudinal design, as in the current study. Additionally, recent advances in the development of parent-report measures of accommodation, the Family Accommodation Scale (FAS-PR), have aided researchers’ ability to characterize this facet of family functioning within OCD (Flessner et al. 2009). Parents, however, may under- or overestimate the frequency of their accommodating behaviors and the degree to which these behaviors contribute to family dysfunction. Therefore, an approach to characterizing parental accommodation that employs a more direct, semi-structured interview format provides the opportunity to obtain a more comprehensive and, potentially, less biased assessment of this parenting practice. The direct interview technique employed in the current study (FAS; Calvocoressi et al. 1999) allows the interviewer to probe for specific examples of the child’s compulsions using information obtained from the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) and is also more consistent with the approach undertaken in the development of the original, clinician-administered version of the FAS (Calvocoressi et al. 1995)—which represents the gold-standard for measuring family accommodation. The use of a prospective, longitudinal design and the utilization of the original, clinician-administered version of the FAS (Calvocoressi et al. 1995) modified for use with children and families will help to address these limitations.
The current exploratory study utilized data from an ongoing, prospective study, the Brown Longitudinal Obsessive Compulsive Disorder Study (BLOCS), examining the course of OCD across the lifespan. This was the first comprehensive, prospective study investigating the long-term course of pediatric OCD in a large clinical sample (Pinto et al. 2006). Our primary aim was to examine the relative contribution of parental accommodation (as assessed at intake) in predicting OCD symptom severity at intake and two-years post-intake after controlling for other relevant factors (e.g., child age, anxiety, and depression). Prior research has shown that children and adolescents with OCD and a comorbid anxiety disorder demonstrate greater OCD-related symptom severity compared to those failing to meet diagnostic criteria for another anxiety disorder or those with a comorbid externalizing disorder (Langley et al. 2010). Relatedly, children exhibiting a comorbid anxiety disorder and reporting greater depressive symptoms demonstrate even greater severity of OCD-related symptoms. This evidence suggests that comorbid depressive and anxiety symptoms are strongly predictive of increased OCD symptoms severity, and should be included as covariates in the current investigation. This may be particularly true of depressive symptoms and is consistent with findings from other research (Peris et al. 2010). Though this study is a preliminary investigation, relevant findings from prior literature examining parental accommodation has informed this study’s hypothesis that greater levels of parental accommodation (assessed at intake) would predict increases in OCD symptom severity at both intake and year two.
Method
Participants
Participants were children and adolescents between the ages of 6 and 18 and their parents participating in an ongoing, prospective follow-up study of OCD, recruited between June 2001 and December 2005. Inclusion criteria were (1) a primary DSM-IV diagnosis of OCD defined as the disorder that participants and parents considered their biggest problem overall across their lifetime, (2) minimum age of 6 years, (3) treatment-seeking within the last 5 years, and (4) participants and parents were willing and able to sign written assent and consent. Exclusion criteria included a diagnosis of either an organic mental disorder (e.g., stroke, trauma, infections such as meningitis, cancer, degenerative disorders, brain injury, etc.) or mental retardation at intake. Participants were recruited from clinical settings in Rhode Island and Massachusetts, including an outpatient OCD clinic, a private psychiatric hospital, and several large outpatient primary treatment sites for anxiety disorders. A detailed description of full sample characteristics and methods can be found in a previous paper (Mancebo et al. 2008).
The present report is based on the prospective data collected on 30 participants who met full criteria for OCD at intake and had complete data on the primary measures of interest to this investigation. This number of participants represents 54.4 % of the “in episode” (i.e., participants enrolled in the study who, at the time of intake, met full diagnostic criteria for OCD) sample (N = 70) at intake. Analysis revealed no statistically significant differences between participants classified as “in-episodes” compared to “out-of-episode” on key demographic variables including gender, age, race, age at onset of minor OCD symptoms, or age at onset of major OCD symptoms. Participants were assessed at intake and one- and two-years post-intake. Due to high rates of missingness, resulting in a small sample size (n = 18) at one-year follow-up, analyses were not conducted for this time point. Consequently, only participants with complete data at two-year follow-up were included in analyses (n = 22). Participants were 67 % male with a mean age of 14.1. Ninety-three percent of the sample was White. Full demographic characteristics and sample sizes are provided in Table 1.
Procedure
This study was approved by the institutional review boards at Brown University and Butler Hospital, and all participants and their parents provided consent and assent prior to enrollment. With the exception of the K-SADS-PL, all assessments were administered by interviewers with at least a bachelor’s degree who were closely supervised by a psychologist. The K-SADS-PL was administered at baseline by a Ph.D.-level interviewer trained in the proper administration of this interview. All raters completed a rigorous training protocol that included didactics, viewing and rating sample tapes, rating several live mock participants, and observing and coding interviews conducted by a senior rater or trainer. New raters were required to demonstrate interrater reliability with both senior raters and trainers (intraclass correlation coefficients >0.85 for SCID diagnoses and OCD severity). To minimize rater drift, assessment of interrater reliability was conducted periodically on random samples of taped interviews. Any reliability below 0.80 for two consecutive months triggered remediation procedures (e.g., retraining). More detailed information on training and inter-rater reliability procedures can be found elsewhere (Pinto et al. 2006).
Assessments occurred at intake and two-year follow-up and consisted of semi-structured interviews, rater-administered measures, and self-report questionnaires. A semi-structured interview was administered to obtain detailed information on demographic and clinical features of OCD, as well as past treatment history (Rasmussen and Eisen 1992). For child participants, parents were interviewed prior to the child. For adolescent participants, adolescents were interviewed first. Following the interview, raters met with parents and children/adolescents to clarify any discrepancies between parent and child/adolescent responses to interview questions. All interviews were staffed at weekly research meetings with psychologists and psychiatrists with expertise in OCD.
Measures
Family Accommodation Scale (FAS) (Calvocoressi et al. 1999)
At the initial intake assessment, family accommodation was measured using the Family Accommodation Scale (Calvocoressi et al. 1999). The FAS is a 12-item, clinician-administered measure assessing the degree to which parents accommodate their child’s OCD-related behaviors during the past week. Following review of the child’s current symptoms, parents are asked the degree to which they accommodate their child’s symptoms on a scale from 0 (never/none) to 4 (extreme), including the frequency and severity of these accommodations. This clinician-administered version of the FAS has demonstrated good reliability and validity in prior research (Calvocoressi et al. 1999). Total scores on the FAS range from 0 to 48, with higher scores indicating more accommodation.
Children’s Yale-Brown Obsessive–Compulsive Scale (CY-BOCS) (Scahill et al. 1997)
The CY-BOCS is a semi-structured, clinician-administered interview assessing the severity of OCD-related obsessions and compulsions in children. The scale also consists of two subscales assessing obsession (items 1–5) and compulsion (items 6–10) severity as well as providing a total severity score (summation of items 1–10) and demonstrates good psychometric properties (Scahill et al. 1997). For the purposes of this study, the Obsessions, Compulsion, and Total Severity scales were each utilized to provide a more fine-grained examination of the impact of parental accommodation on OCD symptom severity. Total scores range from 0 to 40, with scores from 0 to 7 indicating subclinical symptoms, 8–15 representing mild symptoms, 16–23 indicating moderate symptoms, 24–31 implying severe symptoms, and scores within the 32–40 range representing extreme symptoms.
Yale-Brown Obsessive–Compulsive Scale (Y-BOCS) (Goodman et al. 1989)
Only participants ages 18 years of age and older were administered the Y-BOCS. The Y-BOCS is an age-downward extension of the CY-BOCS designed for use with adults and is identical to the CY-BOCS except for the symptom checklist. It has been shown to demonstrate good psychometric properties (Goodman et al. 1989; Goodman et al. 1989). Scoring is identical to that of the CY-BOCS.
The Schedule for Affective Disorders and Schizophrenia for School-Age (K-SADS-PL) (Kaufman et al. 1997)
The K-SADS-PL is a semi-structured diagnostic interview that assesses current and lifetime history of child psychopathology according to DSM-IV criteria and has demonstrated adequate psychometric properties (Kaufman et al. 1997). All children between the ages of 6 and 12 were administered the K-SADS-PL.
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-P) (First et al. 1996)
The SCID-P is a semi-structured interview designed to assess Axis I psychiatric disorders. All adolescents (ages 13 and older) were administered the SCID-P.
Children’s Depression Inventory (CDI) (Kovacs 1992)
The CDI is a 27-item self-report measure of depression in children yielding both a total depression score and 5 subscale scores and demonstrates strong internal consistency and moderate test–retest reliability and convergent validity (Saylor et al. 1984). For the purposes of this study, only the CDI Total score was used. Total scores range from 0 to 54, with higher scores indicating higher depression symptoms. All children between the ages of 6 and 12 were administered the CDI.
Modified Hamilton Rating Scale for Depression (MHRSD) (Miller et al. 1985)
The MHRSD is a 25-item rater-administered interview assessing depression severity in adolescents and adults demonstrating adequate reliability and validity (Miller et al. 1985). All adolescents (ages 13 and older) were administered the MHRSD. Total scores ranging from 0 to 7 are considered normal, while scores over 20 are suggestive of clinical depression
Multidimensional Anxiety Scale for Children (MASC) (March et al. 1997)
The MASC is a 39-item self-report measure of anxiety yielding an overall score and 4 subscale scores and demonstrates good psychometric properties (March et al. 1997; Wood et al. 2002). All participants were administered the MASC. Total scores range from 0 to 117, with higher scores indicating greater anxiety.
Screen for Childhood Anxiety-Related Emotional Disorders (SCARED) (Birmaher et al. 1997)
The SCARED is a 38-item self-report measure of child anxiety and yields a total score as well as five subscale scores including somatic/panic, general anxiety, separation anxiety, social phobia, and school phobia. The SCARED demonstrates good reliability and validity (Birmaher et al. 1997). The SCARED was not administered at intake but rather was first administered at one-year follow-up to participants age 8 and older. Scores range from 0 to 82, with higher scores indicating high anxiety. Total scores greater than or equal to 25 indicate the presence of an anxiety disorder.
Data Analyses
The present study used an empirically derived outcome measure of OCD—OCD Total Severity—at intake and two-year follow-up. The OCD Total Severity outcome measure consisted of the total score on either the Y-BOCS or the CY-BOCS. To account for those participants transitioning from adolescence (i.e., 18 years of age) to adulthood (i.e., 19 years of age) between intake and Year 2 assessments and to maximize sample size, Y-BOCS scores were used as a proxy for CY-BOCS scores for participants 19 years of age and older at two-year follow-up. Seven participants transitioned into adulthood throughout the course of the study and were administered the Y-BOCS.
Based on prior research and theoretical significance (Flessner et al. 2011), four variables were chosen as potential candidate predictors of OCD symptom severity from the intake battery. These variables included child age, child anxiety, child depression, and parental accommodation. Child age, anxiety, and depression were assessed at intake as well as two-year follow-up, while parental accommodation was assessed only at intake. Anxiety and depression symptoms as measured at intake were included in analyses rather than symptoms assessed at 2-year follow-up to account for their potential influence on changes in OCD symptoms over time and to better mirror those comparisons being conducted with respect to the accommodation practices. Other potential predictors of pediatric OCD symptom severity—including psychosocial stress (Lin et al. 2007) and the presence of other psychiatric diagnoses including anxiety disorders and body dysmorphic disorder (Hanna 1995)—have been examined in previous research. However, due to the small sample size, the power of our analyses was limited. Therefore, these variables were not included in our analyses.
MASC standardized scores were utilized to create Child Anxiety scores at intake. At Year 2, participants were administered both the MASC and the SCARED. To account for possible missing data and to maximize sample size, standardized scores were created for both the MASC and SCARED. In instances in which only one of these measures were available, the standardized score for that measure was used as the participants Child Anxiety score at Year 2. In instances in which both MASC and SCARED standardized scores were available, the mean of these two scores was used for the participant’s Child Anxiety score at Year 2. Participants who were not administered either the MASC or the SCARED were excluded from analyses. Child Depression scores consisted of the mean of CDI standardized scores and MHRSD standardized scores at each respective time point. Parental Accommodation scores consisted of the sum of item scores on the FAS.
Before developing final regression models, the distribution of the study’s outcome variables was examined. Analyses suggested that all outcome variables were normally distributed. Continuous independent variables were determined to be normally distributed using absolute cut-offs of skewness and kurtosis. Next, the relations between the predictor variables were examined using Pearson correlation and revealed that multicollinearity was not a concern. Durbin-Watson tests were used to test for the correlations among error terms and revealed that errors of prediction were non-correlated. Normal probability plots were used to test for linear relationships among the IVs and DVs and constancy in the variance in residual scores. The assumptions of linearity and homoscedasticity were both met.
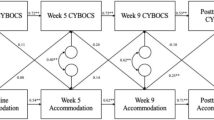
Two identical hierarchical linear regression analyses were employed to determine the final regression models (N = 2; OCD Total Severity at intake and year 2). For both regression analyses, child age, child anxiety and child depression were entered into step 1 and parental accommodation in step 2.
Results
Descriptive information for the FAS is available in Table 2. A correlational analysis was performed to examine the relationship between age and parental accommodation; results were not significant. Descriptive analyses revealed mean CY-BOCS scores of 22 at intake, indicating that the current sample demonstrates moderate OCD symptoms. A hierarchical multiple linear regression was conducted to investigate whether family accommodation predicted CY-BOCS Total Severity Score at intake after controlling for age, anxiety scores at intake, and depression scores at intake. Results showed that a final regression model explained 47.3 % of the variability in OCD Total Severity at intake (Adjusted R2 = 38.9 %; see Table 3). Anxiety, depression and age were not found to be statistically significant predictors. The addition of parental accommodation (β = .64, p < .001) significantly improved model fit, FΔ(1, 25) = 16.62, p < .001 and explained an additional 35.0 % of variance in OCD Total Severity.
Results showed that a final regression model explained 38.9 % of the variability in OCD Total Severity at two-year follow-up (Adjusted R2 = 24.5 %; see Table 4). Anxiety, depression, and age were not positively associated with OCD Symptom Severity. The addition of parental accommodation (β = .44, p < .05) significantly improved model fit, FΔ (1, 17) = 4.54, p < 0.05 and explained an additional 16.3 % of variance in OCD Total Severity.
Discussion
This is the first study to examine the longitudinal effects of parental accommodation on OCD symptom severity in children with OCD. Preliminary findings are consistent with prior research that has shown a positive association between parental accommodation and OCD symptom severity in children (Merlo et al. 2009; Storch et al. 2007). This preliminary study represents a significant addition to the available literature by demonstrating that parental accommodation (at intake) also represents a significant predictor of OCD symptom severity 2 years later thus highlighting the importance of further inquiry into those factors most influential in predicting the degree to which parents accommodate their child’s OCD-related symptoms.
Parental accommodation accounted for a significant, additional proportion of the variance in predicting OCD symptom severity at intake and two-year follow-up. These results suggest several possible implications. First, parental accommodation at a single point-in-time (i.e., intake), at least preliminarily, appears to exert a strong influence on the ability to predict OCD-related symptom severity in the future (i.e., 2 years post-intake). Although parental accommodation was only assessed at intake in the present study, this “snap-shot” of accommodation may be descriptive of the general approach to parenting that the families of children with OCD engage in over the course of the child’s illness. That is, parental accommodation—as measured at intake—may continue to exert such a strong predictive influence on OCD symptom severity in the future due to the pervasive and impulsive (i.e., immediate removal of parental accommodation is likely to result in a substantial and marked increase in a child’s distress) nature of this approach to responding to a child’s OCD symptoms. If so, it further corroborates past research suggesting the importance of reductions in parental accommodation for improving treatment outcome (Merlo et al. 2009) and highlights the importance of recent, family-based approaches to the treatment of pediatric OCD (Barrett et al. 2008; Freeman et al. 2008; Piacentini et al. 2011). Because parental accommodation directly contradicts the goals of cognitive-behavioral therapy (Merlo et al. 2009), future treatments may seek to include several parent-only sessions strategically spaced throughout treatment (i.e., prior to substantial “leaps” in a child’s symptom hierarchy) directly targeting strategies for aiding the parent(s) in reducing the degree to which they accommodate their child’s symptoms (i.e., managing the child’s distress, managing parent’s response to stress, reassessing short- and long-term goals of treatment, etc.).
A second and particularly interesting implication of the present study is the possibility of some mediating variable, such as parental psychopathology (e.g., anxiety), that may aide in explaining the mechanism by which parental accommodation exerts such a strong influence on OCD symptom severity in children. In a recent study, Flessner and colleagues (Flessner et al. 2011) found that parental anxiety significantly predicted accommodation practices in families of children with OCD with prior research demonstrating similar findings (Peris et al. 2008). For example, it is plausible that increasingly anxious parents might be more motivated to prevent their children from experiencing the persistence of anxiety—albeit likely time limited—that may result from refraining from engaging in a ritual or compulsion. A novel and innovative line of future research may seek to explore the possibility that various parental factors (e.g., parental psychopathology) and/or psychosocial stressors (e.g., financial burden, stressful life events, multiple children in the family, etc.) may influence the pathogenesis of anxiety-enhancing parenting practices such as parental accommodation amongst the families of anxious children. Similarly, research seeking to examine the “goodness of fit” in relation to parenting behaviors and child temperament among children with OCD would be an interesting extension of this line of research and may provide similar insights regarding the pathogenesis and treatment of this disorder.
Several limitations to the present study should be noted. First, due to the inherent difficulties with longitudinal research, there was a decrease in sample size from intake to two-year follow-up. While a noteworthy limitation to the study (i.e., inability to track relationships among the same participants across these time points due to high missingness), this approach was necessary to maximize sample size and is a common drawback to most longitudinal studies. The approach for data analysis utilized herein provided for separate regression analyses and consequently does not require the same participants to be present at each time point. Given that this is the first study of its kind in the pediatric OCD literature, we do not view this as a significant limitation but rather an important starting point for future research. A second limitation to the current study was the assessment of accommodation solely at intake. It is not possible, using this assessment approach, to determine whether changes in parental accommodation occurred over time. While it would be valuable to measure the degree of change over time in future research, the knowledge that parental accommodation as measured at baseline predicts OCD symptom severity 2 years later remains a significant and novel contribution to the current literature. A third limitation is the exclusion of treatment data in the current analyses. However, as the current study is prospective and longitudinal in nature and thus, treatment is uncontrolled, the lack of control presents difficulties in drawing conclusions from treatment data (Leon 2011). In addition, the lack of demographic variability in the sample poses a problem for the generalizability of findings. However, as this was an exploratory study with a small sample size, we anticipate and suggest that future research examining this relationship utilize a larger, more diverse sample than that of the current study. Finally, because variability existed in the degree to which participants completed each of the child anxiety and depression measures at each time point, mean composite scores were utilized. While a limitation in that both measures of child anxiety (n = 2) and depression (n = 2) were not available for all participants at both intake and two-year follow-up, this approach allowed us to increase sample size and provide a more comprehensive evaluation of anxiety and depressive symptoms. In addition, though hypotheses can be made about the directionality of the relationship between parental accommodation and OCD symptom severity, it is important to note that the analyses conducted in the current study preclude inferences about the directionality of this relationship. Previous researchers examining this relationship (Merlo et al. 2009; Storch et al. 2007) have referenced similar limitations in their analyses. Despite the limitations noted above, the current study’s findings provide clear implications for future research.
Because parental accommodation plays such a large role in predicting the severity of OCD symptoms and is so ubiquitous among families of children with OCD, future research should examine the etiology of parental accommodation and other anxiety-enhancing parenting practices. There are many possible reasons why parents accommodate their child’s OCD, and it is important that researchers ascertain these reasons. This study and its findings represents an important first step in helping researchers and clinicians to obtain a more comprehensive characterization of parental accommodation in children with OCD and set the stage for intriguing future studies in this domain. It is only through empirical investigations of this sort that clinical researchers may truly begin to better understand and help the families of children with OCD.
References
Albert, U., Bogetto, F., Maina, G., Saracco, P., Brunatto, C., & Mataix-Cols, D. (2010). Family accommodation in obsessive-compulsive disorder: Relation to symptom dimensions, clinical and family characteristics. Psychiatry Research, 179(2), 204–211.
American Psychological Association. (2000). Diagnostic and statistical manual of mental disorders (4th edn., text rev.) (Vol. 4). Washington, DC: Author.
Barrett, P. M., Farrell, L., Pina, A. A., Peris, T. S., & Piacentini, J. (2008). Evidence-based psychosocial treatments for child and adolescent obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology, 37(1), 131–155.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., & Neer, S. M. (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 545–553.
Calvocoressi, L., Lewis, B., Harris, M., Trufan, S. J., Goodman, W. K., McDougle, C. J., & Price, L. H. (1995). Family accommodation in obsessive-compulsive disorder. American Journal of Psychiatry, 152(3), 441–443.
Calvocoressi, L., Mazure, C. M., Kasl, S. V., Skolnick, J., Fisk, D., Vegso, S. J., et al. (1999). Family accommodation of obsessive-compulsive symptoms: Instrument development and assessment of family behavior. Journal of Nervous and Mental Diseases, 187(10), 636–642.
First, M., Spitzer, R., Gibbon, M., & et al. (1996). Structured clinical interview for DSM_IV Axis I disorder, Patient Edition (SCID-P).
Flessner, C. A., Freeman, J. B., Sapyta, J., Garcia, A., Franklin, M. E., March, J. S., & Foa, E. (2011). Predictors of parental accommodation in pediatric obsessive-compulsive disorder: Findings from the pediatric obsessive-compulsive disorder treatment study (POTS) trial. Journal of the American Academy of Child and Adolescent Psychiatry, 50(7), 716–725.
Flessner, C. A., Sapyta, J., Garcia, A., Freeman, J. B., Franklin, M. E., Foa, E., & March, J. (2009). Examining the psychometric properties of the family accommodation scale-parent-report (FAS-PR). Journal of Psychopathology and Behavioral Assessment, 31(1), 38–46.
Freeman, J. B., Garcia, A. M., Coyne, L., Ale, C., Przeworski, A., Himle, M., et al. (2008). Early childhood OCD: Preliminary findings from a family-based cognitive-behavioral approach. Journal of the American Academy of Child and Adolescent Psychiatry, 47(5), 593–602.
Geller, D. A. (2006). Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatric Clinics of North America, 29(2), 353–370.
Geller, D. A., Biederman, J., Griffin, S., Jones, J., & Lefkowitz, T. R. (1996). Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 35(12), 1637–1646.
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Delgado, P., Heninger, G. R., & Charney, D. S. (1989a). The Yale-Brown obsessive compulsive scale. II. Validity. Archives of General Psychiatry, 46(11), 1012–1016.
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., et al. (1989b). The Yale-Brown obsessive compulsive scale. I. Development, use, and reliability. Archives of General Psychiatry, 46(11), 1006–1011.
Hanna, G. L. (1995). Demographic and clinical-features of obsessive-compulsive disorder in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 34(1), 19–27.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988.
Kovacs, M. (1992). Children’s depression inventory. New York: Multi-Health Systems.
Langley, A. K., Lewin, A. B., Bergman, R. L., Lee, J. C., & Piacentini, J. (2010). Correlates of comorbid anxiety and externalizing disorders in childhood obsessive compulsive disorder. European Journal of Child and Adolescent Psychiatry, 19(8), 637–645.
Leon, A. C. (2011). Evaluation of psychiatric interventions in an observational study: Issues in design and analysis. Dialogues in Clinical Neuroscience, 13(2), 191–198.
Lewin, A. B., Storch, E. A., Geffken, G. R., Goodman, W. K., & Murphy, T. K. (2006). A neuropsychiatric review of pediatric obsessive-compulsive disorder: Etiology and efficacious treatments. Neuropsychiatric Disorders and Treatment, 2(1), 21–31.
Lin, H. Q., Katsovich, L., Ghebremichael, M., Findley, D. B., Grantz, H., Lombroso, P. J., et al. (2007). Psychosocial stress predicts future symptom severities in children and adolescents with Tourette syndrome and/or obsessive-compulsive disorder. Journal of Child Psychology and Psychiatry, 48(2), 157–166.
Maina, G., Saracco, P., Albert, U., & Bogetto, F. (2006). Family-focused treatments for obsessive-compulsive disorder. Clinical Neuropsychiatry, 3(6), 382–390.
Mancebo, M. C., Garcia, A. M., Pinto, A., Freeman, J. B., Przeworski, A., Stout, R., et al. (2008). Juvenile-onset OCD: Clinical features in children, adolescents and adults. Acta Psychiatrica Scandinavica, 118(2), 149–159.
March, J. S., Parker, J. D., Sullivan, K., Stallings, P., & Conners, C. K. (1997). The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 554–565.
Merlo, L. J., Lehmkuhl, H. D., Geffken, G. R., & Storch, E. A. (2009). Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 77(2), 355–360.
Miller, I. W., Bishop, S., Norman, W. H., & Maddever, H. (1985). The modified Hamilton rating scale for depression: Reliability and validity. Psychiatry Research, 14(2), 131–142.
Peris, T. S., Bergman, R. L., Asarnow, J. R., Langley, A., McCracken, J. T., & Piacentini, J. (2010). Clinical and cognitive correlates of depressive symptoms among youth with obsessive compulsive disorder. Journal of Clinical Child and Adolescent Psychology, 39(5), 616–626.
Peris, T. S., Bergman, R. L., Langley, A., Chang, S., McCracken, J. T., & Piacentini, J. (2008). Correlates of accommodation of pediatric obsessive-compulsive disorder: Parent, child, and family characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 47(10), 1173–1181.
Piacentini, J., Bergman, R. L., Chang, S., Langley, A., Peris, T., Wood, J. J., & McCracken, J. (2011). Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 50(11), 1149–1161.
Piacentini, J., Peris, T. S., Bergman, R. L., Chang, S., & Jaffer, M. (2007). Functional impairment in childhood OCD: Development and psychometrics properties of the child obsessive-compulsive impact scale-revised (COIS-R). Journal of Clinical Child and Adolescent Psychology, 36(4), 645–653.
Pinto, A., Mancebo, M. C., Eisen, J. L., Pagano, M. E., & Rasmussen, S. A. (2006). The Brown Longitudinal Obsessive Compulsive Study: Clinical features and symptoms of the sample at intake. Journal of Clinical Psychiatry, 67(5), 703–711.
Rasmussen, S. A., & Eisen, J. L. (1992). The epidemiology and clinical features of obsessive compulsive disorder. Psychiatric Clinics of North America, 15(4), 743–758.
Saylor, C. F., Finch, A. J, Jr, Spirito, A., & Bennett, B. (1984). The children’s depression inventory: A systematic evaluation of psychometric properties. Journal of Consulting and Clinical Psychology, 52(6), 955–967.
Scahill, L., Riddle, M. A., McSwiggin-Hardin, M., Ort, S. I., King, R. A., Goodman, W. K., et al. (1997). Children’s Yale-Brown obsessive compulsive scale: Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 36(6), 844–852.
Steketee, G., & Van Noppen, B. (2003). Family approaches to treatment for obsessive compulsive disorder. Revista Brasileira Psiquiatria, 25(1), 43–50.
Stengler-Wenzke, K., Kroll, M., Matschinger, H., & Angermeyer, M. C. (2006). Quality of life of relatives of patients with obsessive-compulsive disorder. Comprehensive Psychiatry, 47(6), 523–527.
Storch, E. A., Geffken, G. R., Merlo, L. J., Jacob, M. L., Murphy, T. K., Goodman, W. K., et al. (2007). Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology, 36(2), 207–216.
Valleni-Basile, L. A., Garrison, C. Z., Jackson, K. L., Waller, J. L., McKeown, R. E., Addy, C. L., & Cuffe, S. P. (1994). Frequency of obsessive-compulsive disorder in a community sample of young adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 33(6), 782–791.
Wood, J. J., Piacentini, J. C., Bergman, R. L., McCracken, J., & Barrios, V. (2002). Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child and Adolecsent Psychology, 31(3), 335–342.
Zohar, A. H. (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America, 8(3), 445–460.
Acknowledgments
This study was funded by a Grant awarded to Dr. Rasmussen from the National Institutes of Health, Bethesda, MD (Grant Number: R01-MH-060218).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Francazio, S.K., Flessner, C.A., Boisseau, C.L. et al. Parental Accommodation Predicts Symptom Severity at Long-Term Follow-Up in Children with Obsessive–Compulsive Disorder: A Preliminary Investigation. J Child Fam Stud 25, 2562–2570 (2016). https://doi.org/10.1007/s10826-016-0408-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-016-0408-7