Abstract
Purpose
This study aims to evaluate whether the clinical outcomes of cycles with frozen embryo transfer (FET) in hormonal replacement treatment supplemented with dydrogesterone (DYD) following detection of low circulating levels of progesterone (P4) were comparable to the results of cycles with otherwise normal serum P4 values.
Methods
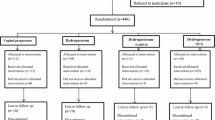
Extended analyses of a retrospective cohort that included FET cycles performed between July 2019 and March 2022 after a cycle of artificial endometrial preparation using valerate-estradiol and micronized vaginal P4 (400 mg twice daily). Whenever the serum P4 value was considered low on the morning of the planned transfer, 10 mg of DYD three times a day was added as a supplement. Only single-embryo transfers of a blastocyst were considered. The primary endpoint was live birth rate.
Results
Five-hundred thirty-five FET cycles were analyzed, of which 136 (25.4%) underwent treatment with DYD. There were 337 pregnancies (63%), 207 live births (38.6%), and 130 miscarriages (38.5%). The P4 values could be modeled by a gamma distribution, with a mean of 14.5 ng/ml and a standard deviation of 1.95 ng/ml. The variables female age on the day of FET, ethnicity, and weight were associated with a variation in the serum P4 values.
There were no differences in the results between cycles with or without the indication for DYD supplementation.
Conclusions
Live birth rate did not vary significantly in females with low and normal serum P4 levels on the day of FET when DYD was used as rescue therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Both the number of IVF/ICSI cycles and frozen embryo transfers (FET) have increased in the last few years. In 2017, more than 270,000 cycles were reported in Europe [1], with pregnancy rates ranging between 30.2% (autologous oocytes) and 41.1% (following oocyte donation). For this reason, there has been increasing attention regarding endometrial preparation for FET.
Endometrial preparation for FET can be achieved in either a natural (true or modified) or artificial cycle, with no significant differences in clinical pregnancy and live birth rates being reported thus far [2, 3]. In the case of artificial cycles, exogenous supplementation of estradiol usually is commenced following menses with progesterone (P4) being added after adequate endometrial proliferation. If a pregnancy is achieved, this artificial supplementation will need to be maintained until at least the 7th–9th week of gestation. In this type of treatment, the degree of hormonal fluctuation is considered small, since stable hormonal values are reached quickly following the start of the medication [4, 5].
Although recent publications suggest that there are favorable benefits of natural over artificial cycles, with a decrease in hypertensive disorders of pregnancy [6, 7], hormone-substituted cycles are often used owing to several perceived advantages including greater ease of programming and greater control of exposure to exogenous P4 [8]. Endometrial receptivity in this case seems to be related to the time and dose of exposure to P4 after adequate estrogen priming [9]. Exogenous P4 can be administered orally, vaginally, subcutaneously (SC), or intramuscularly (IM), without any one method demonstrating superiority over the others [10].
Recent publications demonstrate a negative association between low serum P4 levels on the day of embryo transfer and the final outcome, be it clinical pregnancy or childbirth [11,12,13,14,15,16], making it noteworthy to stress how the absorption and metabolism of vaginal P4 may eventually vary between different patients [4, 11, 13]. Considering this, several rescue attempts have been suggested, in most cases resorting to either subcutaneous or intramuscular P4.
Dydrogesterone (DYD) is an orally administered progestin [17] with a high specificity for the P4 receptor [18]. It has a very selective progestagenic activity, with no androgenic, glucocorticoid, or estrogenic activity [18]. Thus, it can be used in smaller doses and with fewer side effects [19]. The active metabolite is 20-alpha-dihydrodidrogesterone, which has a half-life of about 17 h. In the context of fresh IVF cycles, this drug has proved to be a good alternative when used in cycles with fresh embryo transfer [20, 21], with a good safety profile [22, 23].
At the Center for Infertility and Medically Assisted Procreation of Almada (CIRMA), a prospective study was conducted between May 2018 and June 2019, in which there was a strong trend towards worse outcomes in the group of patients with lower circulating P4 values [24]. Since then, oral P4 has been added at a dose of 10 mg of DYD thrice-daily in cycles with low P4. A preliminary analysis of 304 cycles showed favorable results regarding the rate of ongoing pregnancy, suggesting an improvement in outcomes [25]. This cohort was increased and further studied to evaluate if there are any differences in the rate of live birth deliveries between patients with low P4 values supplemented with DYD compared to cycles above the cutoff levels. Additionally we soght to identify which variables may influence the value of serum P4 on the FET day.
Materials and methods
This was an extended analysis of a retrospective cohort study of FETs carried out at CIRMA between 1 July 2019 and 31 March 2022. All embryos were transferred in a hormone-substituted cycle (1 blastocyst, with a degree of expansion equal to or greater than 2 and grade 1 or 2 in the internal cell mass and trophoectoderm) [26]. Women included in the study were aged between 21 and 39 years on the day of oocyte retrieval. Patients with an endometrial layer thinner than 7 mm prior to commencing P4, endocavitary pathology, uncorrected Mullerian anomalies, or serum P4 values incompatible with a luteal phase on the day of transfer (below 3 ng/ml, n = 2) were excluded from the analysis.
Variables
The main outcome was live birth > 24 weeks, with other pregnancy variables of interest including biochemical pregnancy (β-HCG > 5 IU/l — 9 to 12 days after transfer) and miscarriage (i.e., all the biochemical pregnancies that did not end in a live birth were considered miscarriages). Additionally, serum P4 value on the day of FET was also included as a secondary outcome of interest in order to evaluate potential predictors.
The explanatory variables evaluated were relevant female characteristics (female age at the oocyte retrieval and at FET day, body mass index (BMI), height, weight, ethnicity, and smoking habits), infertility factor (endometriosis, male factor, both female and male factor, unexplained, multiple female factors, disovulation, tubal, other), IVF/ICSI cycle characteristics (total gonadotropins dose, number of oocytes retrieved, number of 2PN embryos, type of fertilization), and relevant FET cycle parameters (whether the FET occurred after a freeze all strategy, endometrial thickness prior to starting exogenous P4, serum P4 value on the day of FET, number of days in culture before the blastocyst was frozen, rank of the embryo transfer, and use of DYD as rescue therapy).
Endometrial preparation protocol
On the 2nd or 3rd day of a spontaneous, post-progestin, or post-pill menses, the patient started the application of estradiol (Zumenon®, Bayer Portugal, SA, Portugal) at a dose of 2 mg of 12/12 h vaginally. Ultrasound control was performed 10 to 20 days later. If the endometrial thickness was 7 mm or above and ovaries were without a dominant follicle (> 14 mm) or corpus luteum, the patients started the administration of vaginal P4 (Progeffik, Laboratoires Effik®, Portugal) at a dose of 400 mg every 12 h. Embryo transfer was performed following the 11th dose of progesterone. On the morning of the transfer, a P4 assay was performed.
Embryos were vitrified in a Cryotop® support (Kitazato, Japan). Thawing was performed according to the following protocol: the Cryotop® was removed from the liquid nitrogen and immediately submerged in 300 μl of Thawing solution (TS) (Kitazato, Japan), previously heated to 37 °C. After 1 min, the embryo was transferred to a 60-μl drop of Diluent solution (DS) (Kitazato, Japan) for 3 min at room temperature. Finally, it was placed in a 60-μl drop of Washing solution (WS) (Kitazato, Japan) for 5 min at room temperature, and then washed for 1 min in another drop of 60 μl of WS at room temperature. The embryo was transferred to 30-μl drops of Sequential Blast® medium (ORIGIO, Denmark) covered with Liquid Paraffin (ORIGIO, Denmark) where they remained for at least 2 h prior to the transfer.
Embryo transfers were routinely performed under ultrasound guidance. After the placement of a speculum and removal of cervical mucus and excess P4 with a swab, the embryo transfer catheter (Cook® or Wallace®) was introduced until it passed through the middle of the endometrial cavity, to where the embryos were transferred. The β-HCG test was performed 9 to 12 days after the transfer. In case of pregnancy, estradiol and P4 were maintained until at least the 10th week of pregnancy.
From a temporal point of view, between July 2019 and December 2020 patients with P4 < 10.0 ng/ml were supplemented with DYD (10 mg of DYD (Duphaston®, BGP products, Portugal), thrice daily); however, after January 2021, supplementation widened to levels < 12.5 ng/ml. If pregnancy was confirmed, DYD was maintained at least until the 10th week of pregnancy.
Hormonal assays of P4 and β-HCG were performed in a serum sample via Electrochemiluminescence (ECLIA) using a Modular EVO (E170) Roche Diagnostics® equipment. The method of assay of β-HCG was based on a sandwich-type immunological reaction and that of P4 on a competitive immunological reaction.
Statistical analysis
Statistical analysis was performed using IBM® SPSS® statistics v22.0 and R 4.2.2 for Windows. An initial exploratory analysis was performed using absolute and relative frequencies, mean values, standard deviations, and medians of the variables studied. The continuous variables were compared between groups by their corresponding means using the T-test and the categorical variables with the Chi-square independence test. To assess the ability to predict live birth, a multivariable analysis model was used, using a logistic regression model, including the variables that in the univariate analysis presented p < 0.150, in addition to the use of DYD as rescue therapy and the P4 values, both forced into the models because that were the focus of this study. The level of significance used was \(\alpha\) = 5%.
Results
We included 535 FET cycles, 136 of which (25.4%) performed additional treatment with DYD due to low circulating P4 values on the day of FET. There were 337 cases of biochemical pregnancy (63%), of which 207 (38.6%) delivered a newborn and 130 miscarried (38.5%).
Factors that influenced the value of progesterone
The serum P4 varied from 4.2 to 32.3 ng/dl, with an average of 14.93 ng/dl (SD 4.52). Several regression models were considered for explaining serum P4, with the following variables included: female age at transfer, female smoking, endometrial thickness, infertility factor, female ethnicity, female weight, and height. The models were tested considering either a normal distribution or a gamma distribution for the response variable. The model that showed the best performance was the one that considered a gamma distribution for P4. Based on the values obtained, female age on the FET day, female ethnicity, and female weight seemed to explain the variation of P4 (Supplementary Table 1). Figure 1 shows how the predicted P4 values may vary considering weight and ethnicity. The quality of the fit within the same response family distribution was based on the deviance statistics, measuring the discrepancy of the fit, which follows approximately a qui-square distribution (p > 0.05), and was based on the Akaike information criterion (AIC) for choosing between different family distributions.
Factors that influence live birth
We evaluated which variables could be individually associated with live birth. The thickness of the endometrium, the transfer of a blastocysts vitrified on the 5th day and - the female at the time of oocyte pick up or FET were different for cycles with and withou a live birth (Supplementary tables 2 and 3). The multivariable model revealed that older females at pick up, a thinner endometrial measure, and transferring a day 6 blastocyst were negatively associated with live birth (Table 1). Despite these variables being statistically significant, the Chi-Square test was used to assess the discrepancy of the deviance measure of fit, resulting in a p < 0.001, rejecting the hypothesis of a good fit. To assess the predictive quality of the model, the Hosmer–Lemeshow test was employed, yielding a p-value of < 0.05. Therefore, despite the statistically significant variables included in the model, it did not prove to be a good predictor of a live birth.
Progesterone values, dydrogesterone, and outcome
Firstly, a sensitivity analysis on the P4 values was performed. The data were divided into 5 groups according to P4 levels (Fig. 2) and the rate of live birth per quintile was evaluated. There were no statistically significant differences between the groups (Figs. 2 and 3 and Supplementary table 4).
Afterwards, two groups (with and without addition of DYD) were compared (Tables 2 and 3). The group with added DYD had lower average P4 values (9.4 versus 16.2 ng/ml) and females were heavier (69.0 versus 63.4 kg), with higher BMI (25.8 vs 24.0). None of these variables was related to outcome in the multivariable regression for live birth and most of them are related with having low P4. Patients with low P4 which had DYD added had no statistical differences regarding deliveries, 40% vs 36% (p = 0.354).
Sub-group evaluation
Progesterone subgroup evaluation (4.2–12.5 ng/dl)
The group of patients to whom DYD was added was divided according to the median value of P4 (9.6 ng/ml) (Table 4). No statistically significant differences were identified.
Progesterone subgroup evaluation (10.0–12.5 ng/dl)
From a temporal point of view, between July 2019 and December 2020 patients with P4 < 10.0 ng/ml were supplemented with DYD; however, after January 2021, supplementation widened to levels < 12.5 ng/ml. Thus, the outcome of cycles with P4 levels between 10.0 and 12.5 ng/ml was compared according to the addition or not of DYD. Out of the 100 cases, 53 had DYD added while 47 did not. There were no statistically significant differences between the groups (Table 5).
Discussion
Several studies are consistent in demonstrating that lower P4 values are associated with lower outcomes in hormonal replacement treatment, with up to 30% lower ongoing pregnancy [27, 28]. The present study uses data from a cohort of 535 FET with single-embryo transfer in hormone-substituted cycles, conducted between June 2019 and March 2022. All patients with levels below 10 ng/ml were supplemented with DYD and some patients with values between 10 and 12.5 ng/ml were also supplemented.
Progesterone variation
Firstly we sought to determine whether it is possible to accurately predict which patients will have low P4 levels, avoiding further analysis. According to the pharmacokinetics of P4 administered vaginally, P4 can be monitored from the 2nd day of administration, since it reaches its stable state 6 h after its application, remaining for 24 h [4] [5]. However, these studies are usually performed in patients with a BMI between 20 and 25 kg/m2. In our study, there was a large variability in the P4 value measures ranging from 4.2 to 32.3 ng/ml, with a mean of 14.4 ± 4.6 ng/ml, following a gamma distribution. These values are slightly higher than those obtained in the study of Labarta or Gaggiotti-Marre S, [27, 28] were the mean was 12.1 ± 7.0 ng/ml for the first and 11.3 ± 5.1 ng/ml for the second. The variation observed may be related to the patient’s own characteristics or possibly to the laboratory methods used. For this reason, whenever possible, we chose to evaluate the impact of the variation of P4 values in percentiles and not in absolute terms.
In our sample, it was found that a lower female weight, caucasian ethnicity, and older age were positively related to the circulating P4 value. Previous publications also suggest that a higher weight correlates with a lower value of circulating P4 [27]. The work of González-Foruria [29] showed that weight, previous cycle with low P4 value, and time of blood collection can help explain P4 values in artificial cycles. Variations may be related to different absorption or elimination capacity between patients; for example, a thinner mucosa in older women may help explain better absorption [30]. The different distribution of fat mass associated with weight may also be of importance [14, 21].
Comparing dydrogesterone to other rescue therapy strategies
The idea of supplementing cycles with low P4 values has already been published. Cédrin-Durnerin et al. [16] proposed a cut-off level of 10 ng/ml after vaginal P4 administration, while Brady et al. [14] included cycles using intramuscular P4 and a cut-off value of 20 ng/ml. In both cases, the dose of the exogenous P4 used was increased instead of adding a different route of administration, but this was insufficient to rescue pregnancy rates. Two more recent studies suggest a different strategy, in which they added another route of administration according to the P4 values observed prior to embryo transfer. Labarta et al. [31] published a retrospective study showing that when patients with P4 values below 9.2 ng/ml in their cohort were supplemented with subcutaneous P4 at a dose of 25 mg/day (550 cases, corresponding to 29.7% of the sample), had similar ongoing pregnancy rates to those with a higher value (44.9 versus 45.2%, respectively). Another prospective study [32], in which all patients with P4 levels below 10.6 ng/ml (about 37.8% of the sample) 1 day before transfer were supplemented with subcutaneous P4 25 mg/day, found a non-statistically significant difference in ongoing pregnancy rate between the intervention and control groups (49.6% versus 43.6%, respectively).
As for vaginal P4, the administration of DYD is also associated with a plasma variability of its metabolite 20α-dihydrodydrogesterone. Unfortunately, the assay of 20α-dihydrodydrogesterone requires special laboratory requirements that are not readily available, which makes it difficult to use in clinical practice. However, taking advantage of such an assay, Neuman et al. [33] resorted to luteal supplementation only with DYD 10 mg tid and concluded that the rate of ongoing pregnancy was significantly reduced in the cycles of the first quartile when compared to the remaining quartiles (8% versus 27%, respectively).
Lan N. Vuong [34] reported on a prospective non-randomized study with two groups of patients, one did luteal support only with micronized vaginal P4 400 mg bi-daily (732 patients) and another in addition to P4 added bi-daily oral DYD (632 patients). Overall, the researchers concluded that the live birth rate was higher in the vaginal P4 + DYD group (46.3% versus 41.3%, with p = 0.06), with lower miscarriage rates as well. In this study, there seemed to be a greater difference for lower P4 levels who seem to benefit more. On the other hand, there is no apparent decrease in results for patients with high P4 values supplemented with DYD.
In this study there were no differences in the live birth rate suggesting that, in patients with low-serum P4, the addition of DYD may potentially lead to clinical outcome comparable to those with higher P4 values. A second evaluation that compared the results of 105 cycles with serum P4 between 4.2 and 12.5 ng/dl also did not reveal any statistically significant differences between lower and higher values when DYD was added. This conclusion is similar to that of a recently published study [35] with a similar protocol to this one, where patients with serum P4 values < 8.8 ng/ml received additional oral DYD showed comparable live birth rates.
It is questionable if high levels of P4 might result in a poorer outcome. However, this was not the case of the cohort studied by González-Foruria I. [36] who used vaginal micronized progesterone either alone or in combination with a daily subcutaneous injection of 25 mg of progesterone.
Regarding safety concerns related to the use of DYD in early pregnancy, the available literature is limited. Queisser-Luft A. [37] and Mahmoud et al. [38] reported on potential connections between maternal DYD use during pregnancy and congenital birth defects. However the LOTUS I trial [39] reported comparable rates of adverse effects associated with treatment, including congenital, familial, and genetic effects, between the DYD and micronized vaginal P4 groups (1.0% DYD vs. 1.2% MVP). Moreover, a recent systematic review evaluating the evidence on the efficacy and safety of oral DYD versus micronized vaginal P4 for luteal phase support revealed an overall incidence of congenital, familial, and genetic disorders that was similar between both groups [20]. Nonetheless, a recent study was presented [40] using an international pharmacovigilance database suggesting that more congenital heart defects and hypospadias have been reported to the database for DYD exposure when compared to progesterone.
As future perspectives, it may be important to keep on studying the impact of higher progesterone levels and the ideal DYD dose. The design of a prospective study of this type would require a sizeable population.
Strengths and limitations
The strengths of this study are the fact that the data were obtained from a single center, over a continuous period of time lasting 33 months with a large sample set. The laboratory assessment was also performed at the same center.
However, this is a retrospective cohort study without the control of an untreated group and, for this reason, there is always some heterogeneity to be expected between the groups and sub-groups evaluated. In an attempt to account for such, different sensitivity analyses were performed, all showing similar outcomes.
On the other hand, the fact that there is a part of the sample that was submitted to a different protocol — patients with P4 levels between 10.0 and 12.4 ng/ml in which some were exposed to DYD — may also constitute a limitation ins assessment of the use of this drug in this specific subgroup.
Conclusions
The additional use of DYD as rescue therapy, may be a good option for patients under hormonal replacement treatment with low P4 values.
References
European IVF-Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE); Wyns C, De Geyter C, Calhaz-Jorge C, Kupka MS, Motrenko T, Smeenk J, Bergh C, Tandler-Schneider A, Rugescu IA, Vidakovic S, Goossens V. ART in Europe, 2017: results generated from European registries by ESHRE. Hum Reprod Open. 2021(3):hoab026. https://doi.org/10.1093/hropen/hoab026
Groenewoud ER, Cohlen BJ, Macklon NS. Programming the endometrium for deferred transfer of cryopreserved embryos: hormone replacement versus modified natural cycles. Fertil Steril. 2018;109:768–74.
Yarali H, Polat M, Mumusoglu S, Yarali I, Bozdag G. Preparation of endometrium for frozen embryo replacement cycles: a systematic review and meta-analysis. J Assist Reprod Genet. 2016;33:1287–304.
Nahoul K, Dehennin L, Jondet M, Roger M. Profiles of plasma estrogens, progesterone and their metabolites after oral or vaginal administration of estradiol or progesterone. Maturitas. 1993;16(3):185–202.
Paulson RJ, Collins MG, Yankov VI. Progesterone pharmacokinetics and pharmacodynamics with 3 dosages and 2 regimens of an effervescent micronized progesterone vaginal insert. J Clin Endocrinol Metab. 2014;99(11):4241–9.
Jing S, Li XF, Zhang S, Gong F, Lu G, Lin G. Increased pregnancy complications following frozen-thawed embryo transfer during an artificial cycle. J Assist Reprod Genet. 2019;36:925–33.
Ernstad EG, Wennerholm UB, Khatibi A, Petzold M, Bergh C. Neonatal and maternal outcome after frozen embryo transfer: increased risks in programmed cycles. Am J Obstet Gynecol. 2019;221(2):126.e1-126.e18.
Blesa D, Ruiz-Alonso M, Simón C. Clinical management of endometrial receptivity. Semin Reprod Med. 2014;32:410–3.
Gellersen B, Brosens JJ. Cyclic decidualization of the human endometrium in reproductive health and failure. Endocr Rev. 2014;35:851–905.
van der Linden M, Buckingham K, Farquhar C, Kremer JA, Metwally M. Luteal phase support for assisted reproduction cycles. Cochrane Database Syst Rev. 2015(7):CD009154. https://doi.org/10.1002/14651858.CD009154.pub3
Yovich JL, Conceicao JL, Stanger JD, Hinchliffe PM, Keane KN. Mid-luteal serum progesterone concentrations govern implantation rates for cryopreserved embryo transfers conducted under hormone replacement. Reprod Biomed Online. 2015;31(2):180–91.
Basnayake SK, Volovsky M, Rombauts L, Osianlis T, Vollenhoven B, Healey M. Progesterone concentrations and dosage with frozen embryo transfers — what’s best? Aust N Z J Obstet Gynaecol. 2018;58(5):533–8.
Labarta E, Mariani G, Holtmann N, Celada P, Remohí J, Bosch E. Low serum progesterone on the day of embryo transfer is associated with a diminished se pregnancy rate in oocyte donation cycles after artificial endometrial preparation: a prospFETive study. Human Reprod. 2017;32(12):2437–42.
Brady PC, Kaser DJ, Ginsburg ES, Ashby RK, Missmer SA, Correia KF, Racowsky C. Serum progesterone concentration on day of embryo transfer in donor oocyte cycles. J Assist Reprod Genet. 2014;31:569–75.
Alsbjerg B, Thomsen L, Elbaek HO, Laursen R, Povlsen BB, Haahr T, Humaidan P. Progesterone levels on pregnancy test day after hormone replacement therapy-cryopreserved embryo transfer cycles and related reproductive outcomes. Reprod BioMed Online. 2018;37(5):641–7.
Cédrin-Durnerin I, Isnard T, Mahdjoub S, Sonigo C, Seroka A, Comtet M, Herbemont C, Sifer C, Grynberg M. Serum progesterone concentration and live birth rate in frozen–thawed embryo transfers with hormonally prepared endometrium. Reprod Biomed Online. 2019;38(3):472–80.
Stanczyk FZ, Hapgood JP, Winer S, Mishell DR Jr. Progestogens used in postmenopausal hormone therapy: differences in their pharmacological properties, intracellular actions, and clinical effFETs. Endocr Rev. 2013;34:171–208.
Rižner TL, Brožič P, Doucette C, Turek-Etienne T, Muller-Vieira U, Sonneveld E, van der Burg B, Bocker C, Husen B. SelFETivity and potency of the retroprogesterone dydrogesterone in vitro. Steroids. 2011;76:607–15.
Griesinger G, Tournaye H, Macklon N, Petraglia F, Arck P, Blockeel C, van Amsterdam P, Pexman-Fieth C, Fauser BC. Dydrogesterone: pharmacological profile and mechanism of action as luteal phase support in assisted reproduction. Reprod Biomed Online. 2019;38(2):249–59.
Griesinger G, Blockeel C, Tournaye H. Oral dydrogesterone for luteal phase support in fresh in vitro fertilization cycles: a new standard? Fertil Steril. 2018;109(5):756–62.
Rashidi BH, Ghazizadeh M, Nejad EST, et al. Oral dydrogesterone for luteal support in frozen-thawed embryo transfer artificial cycles: a pilot randomized controlled trial. Asian Pac J Reprod. 2016;5:490–4.
Griesinger G, Blockeel C, Kahler E, Pexman-Fieth C, Olofsson JI, Driessen S, Tournaye H. Dydrogesterone as an oral alternative to vaginal progesterone for IVF luteal phase support: a systematic review and individual participant data meta-analysis. PLoS One. 2020;15(11):e0241044.
Ott J, Egarter C, Aguilera A. Dydrogesterone after 60 years: a glance at the safety profile. Gynecol Endocrinol. 2021;20:1–9.
Metello J, Tomás C, Ferreira P, Bravo I, Branquinho M, Santos-Ribeiro S. Impact of plasmatic progesterone on the day of frozen embryo transfer in hormone-induced cycles. Rev Bras Ginecol Obstet. 2021;43(8):608–61.
Metello J, Tomas C, Ferreira P, Santos-Ribeiro S. The addition of dydrogesterone after frozen embryo transfer in hormonal substituted cycles with low progesterone levels. Rev Bras Ginecol Obstet. 2022Oct;44(10):930–7.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26(6):1270–83. https://doi.org/10.1093/humrep/der037.
Labarta E, Mariani G, Paolelli S, Rodriguez-Varela C, Vidal C, Giles J, Bellver J, Cruz F, Marzal A, Celada P, Olmo I, Alama P, Remohi J, Bosch E. Impact of low serum progesterone levels on the day of embryo transfer on pregnancy outcome: a prospFETive cohort study in artificial cycles with vaginal progesterone. Human Reprod. 2021;36(3):683–92.
Gaggiotti-Marre S, Martinez F, Coll L, Garcia S, Álvarez M, Parriego M, Barri PN, Polyzos N, Coroleu B. Low serum progesterone the day prior to frozen embryo transfer of euploid embryos is associated with significant reduction in live birth rates. Gynecol Endocrinol. 2019;35(5):439–42.
González-Foruria I, Gaggiotti-Marre S, Álvarez M, Martínez F, García S, Rodríguez I, Coroleu B, Polyzos N. Factors associated with serum progesterone concentrations the day before cryopreserved embryo transfer in artificial cycles. RBMO. 2020;40(6):797–804.
Levy T, Yairi Y, Bar-Hava I, Shalev J, Orvieto R, Ben-Rafael Z. Pharmacokinetics of the progesterone-containing vaginal tablet and its use in assisted reproduction. Steroids Progestins Progesterone Recept Modulators Progesterone Antagonists. 2000;65:645–9.
Labarta E, Mariani G, Rodríguez-Varela C, Bosch E. Individualized luteal phase support normalizes live birth rate in female with low progesterone levels on the day of embryo transfer in artificial endometrial preparation cycles. Fertil Steril. 2022;117(1):96–103.
Álvarez M, Gaggiotti-Marre S, Martínez F, Coll L, García S, González-Foruria I, Rodríguez I, Parriego M, Polyzos N, Coroleu B. Individualised luteal phase support in artificially prepared frozen embryo transfer cycles based on serum progesterone levels: a prospFETive cohort study. Human Reprod. 2021;36(6):1552–60.
Neumann K, Masuch A, Vonthein R, Depenbusch M, Schultze-Mosgau A, Eggersmann T, Griesinger G. Dydrogesterone and 20α-dihydrodydrogesterone plasma levels on day of embryo transfer and clinical outcome in an anovulatory programmed frozen-thawed embryo transfer cycle: a prospFETive cohort study. Hum Reprod. 2022;37(6):1183–93.
Vuong L, Pham T, Le K, Ly T, Ho Le, Nguyen D, Ho V, Dang V, Phung T, Norman R, Mol B, Ho T. Micronized progesterone plus dydrogesterone versus micronized progesterone alone for luteal phase support in frozen-thawed cycles (MIDRONE): a prospFETive cohort study. Human Reprod. 2021;36(7):1821–31.
Mackens S, Pais F, Drakopoulos P, Amghizar S, Roelens C, Van Landuyt L, Tournaye H, De Vos M, Blockeel C. Individualized luteal phase support using additional oral dydrogesterone in artificially prepared frozen embryo transfer cycles: is it beneficial? Reprod Biomed Online. 2023Jun;46(6):939–45.
González-Foruria I, García S, Álvarez M, Racca A, Hernández M, Polyzos NP, Coroleu B. Elevated serum progesterone levels before frozen embryo transfer do not negatively impact reproductive outcomes: a large retrospective cohort study. Fertil Steril. 2023;120(3 Pt 2):597–604.
Queisser-Luft A. Dydrogesterone use during pregnancy: overview of birth defects reported since 1977. Early Hum Dev. 2009;85(6):375–7.
Zaqout M, Aslem E, Abuqamar M, Abughazza O, Panzer J, De Wolf D. The impact of oral intake of dydrogesterone on fetal heart development during early pregnancy. Pediatr Cardiol. 2015;36(7):1483–8. https://doi.org/10.1007/s00246-015-1190-9.
Tournaye H, Sukhikh GT, Kahler E, Griesinger G. A Phase III randomized controlled trial comparing the efficacy, safety and tolerability of oral dydrogesterone versus micronized vaginal progesterone for luteal support in in vitro fertilization. Hum Reprod. 2017;32(5):1019–27.
Henry A, Santulli P, Bourdon M, Treluyer JM, Chouchana L. O-150 Birth defects reporting and the use of oral dydrogesterone in assisted reproductive technology: a global pharmacovigilance study. Human Reprod. 2023;38(Supplement_1):dead093.177.
Funding
The work of Isabel Natário was partially supported by the Fundação para a Ciência e a Tecnologia, I.P. (Portuguese Foundation for Science and Technology) under the scope of the projects UIDB/00297/2020 (https://doi.org/10.54499/UIDB/00297/2020) and UIDP/00297/2020 (https://doi.org/10.54499/UIDP/00297/2020) (Center for Mathematics and Applications).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Metello, J., Tomás, C., Ferreira, P. et al. Impact of dydrogesterone use in cycles with low progesterone levels on the day of frozen embryo transfer. J Assist Reprod Genet 41, 1577–1584 (2024). https://doi.org/10.1007/s10815-024-03118-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03118-5