Abstract
Purpose
To evaluate the role of serum progesterone (P4) on the day of embryo transfer (ET) when dydrogesterone (DYD) and micronized vaginal progesterone (MVP) are combined as luteal phase support (LPS) in a hormone replacement therapy (HRT) frozen ET (FET) cycles.
Methods
Retrospective study, including single euploid HRT FET cycles with DYD and MVP as LPS and P4 measurement on ET day. Initially, patients with P4 levels < 10 ng/ml increased MVP to 400 mg/day; this “rescue” was abandoned later.
Results
560 cycles of 507 couples were included. In 275 women, serum P4 level was < 10 ng/ml on the ET day. Among those with low P4 levels, MVP dose remained unchanged in 65 women (11.6%) and was increased in 210 women (37.5%). Women with P4 levels ≥ 10 ng/ml continued LPS without modification. Overall pregnancy rates in these groups were 61.5% (40/65), 54.8% (115/210), and 48.4% (138/285), respectively (p = n.s.). Association of serum P4 levels with ongoing pregnancy rates was analyzed in women without any additional MVP regardless of serum P4 levels (n = 350); multivariable analysis (adjusted for age, BMI, embryo quality (EQ)) did not show a significant association of serum P4 levels with OPR (OR 0.96, 95% CI 0.90–1.02; p = 0.185). Using inverse probability treatment weights, regression analysis in the weighted sample showed no significant association between P4 treatment groups and OP. Compared to fair EQ, the transfer of good EQ increased (OR 1.61, 95% CI 1.22–2.15; p = 0.001) and the transfer of a poor EQ decreased the odds of OP (OR 0.73, 95% CI 0.55–0.97; p = 0.029).
Conclusion
In HRT FET cycle, using LPS with 300 mg/day MVP and 30 mg/day DYD, it appears that serum P4 measurement and increase of MVP in patients with P4 < 10 ng/ml are not necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent years have seen a distinct shift in the embryo transfer (ET) strategies in assisted reproductive technology (ART) treatments from fresh to frozen ET (FET) [1, 2]. Despite the increase in FET cycles, there is no consensus on the “optimal” endometrial preparation for achieving and maintaining a pregnancy.
Endometrial preparation approaches for FET cycles comprise different types of the natural (NC) or modified cycles (MNC) and the hormonal replacement cycle (HRT), in which administration routes for the exogenously administered hormones might differ [3]. The NC strategy is not appropriate for all individuals and clinical scenarios, despite findings suggesting benefits of an NC endometrial approach [4,5,6,7,8]. As a result, the HRT FET method continues to be widely used.
Regardless of the method of ET, a receptive endometrium and synchronicity between the endometrium and embryo developmental stage are necessary for successful embryo implantation. After sufficient estrogenization of the endometrium, endometrial receptivity in HRT FET cycles is achieved after about 120 h of progesterone (P4) exposure. The window of implantation has previously been identified through endometrial gene expression profile investigations [9, 10]. The appearance of P4 in serum and its magnitude depends on the way P4 is administered, how well it is absorbed, and patient-specific factors [11, 12].
In HRT FET cycles, measurements of serum P4 on or before the day of ET are frequently carried out as to evaluate P4 absorption, as research utilizing micronized vaginal progesterone (MVP) as luteal phase support (LPS) had revealed a negative impact of serum P4 levels below a particular threshold, often around 8–10 ng/ml, on FET outcomes [13, 14]. This notion led to the suggestion of “rescue” strategies to modify LPS by increasing the dosage of the same P4 and/or adding another one in a different form of either injectable P4 (i.m. or s.c.) or oral P4 (dydrogesterone (DYD)) [15,16,17,18,19]. However, the role of P4 level measurement in the assessment of a sufficient P4 supplementation may be questioned as serum P4 levels do not correspond to endometrial P4 levels [20] and the intake of DYD is not reflected in the measurement by routinely used P4 assays.
This retrospective study aims to shed further light into the role of P4 measurement in single euploid HRT FET cycles, when MVP and DYD are combined as LPS and whether increasing the dosage of MVP in patients with a P4 level < 10 ng/ml on the day of ET improves outcomes.
Material and methods
This retrospective study included women, who underwent single euploid HRT FET cycles between September 2019 and July 2023, when the results of the serum P4 level on the day of the ET and the cycle outcome were known. Cycles in which the embryos had been biopsied and cryopreserved on day 7, as well as PGT-M cycles and cycles with previous downregulation, were excluded from the analysis. Outcomes were defined as ongoing pregnancy (OP) (with heartbeat > 12 weeks) or as no-OP (not pregnant, biochemical pregnancy, early miscarriage).
Endometrial preparation for HRT FET cycle
Patients were assessed on day 2/3 of their menses by vaginal ultrasound and measurement of serum estradiol (E2) and P4. Patients commenced oral E2 valerate 4 mg (2 × 2 mg) for 2 days and E2 dosage was increased to 6 mg on day 3 of treatment. Monitoring included ultrasonographic measurement of the lining and serial measurements of serum LH, E2, and P4 to exclude spontaneous ovulation. When a triple lining appearance without a minimal thickness of the endometrium was achieved, an initial MVP dose of 100 mg was commenced at 13 h and repeated at 21 h, and this day was considered to be day 0. The day after initiation of P4 (= day 1), MVP administration was increased to 100 mg vaginally three times daily. On day 3 of MVP exposure, DYD (Duphaston®) was started additionally at a dosage of 30 mg/day, according to our clinical standard to counterbalance a possible lack in the absorption of MVP and to avoid a too rapid increase in P4 after the start of the LPS. ET procedure was performed approximately 120 h after the start of MVP. While we used to “rescue” low P4 levels (< 10 ng/ml) on the day of FET by increasing the dose of MVP to 400 mg/day, later on we quit this “rescue” attempts. Medication was continued until the pregnancy test and in case of a positive outcome, until 12 weeks of pregnancy. Blood drawing for P4 measurement was performed before the ET procedure.
ET procedure
The ETs were performed under abdominal ultrasound guidance with a full bladder in lithotomy position by one of three physicians. Clinic key performance indicators demonstrated that there is no difference in the pregnancy rates after ET procedure between the physicians.
Embryo categorization
Embryos had been classified according to Gardner criteria and for embryo categories “good, fair and poor” as follows:
-
Good: day 5 only: expansion: BL 3/4/5/7; quality: AA/AB/BA
-
Fair: day 5: expansion: BL 3/4/5/7; quality: BB/BC/CB and day 6: expansion: BL 3/4/5/7; quality: AA/AB/BA/BB
-
Poor: day 5: expansion: BL 3/4/5; quality: CC; day 6: expansion: BL 3/4/5/6; quality: BC/CB/CC; 1 embryo with BL2, no quality
Ethical approval
The study was approved by the ethics committee of ART Fertility Clinics, Abu Dhabi, UAE (REFA084).
Statistical analysis
Variables are presented as median and interquartile ranges (Q1–Q3) for continuous variables and count with percentages of total for categorical variables. The association between transfer day serum P4 levels and OP rates was first assessed visually with conditional density plots using patients who did not increase MVP dosage after ET based on P4 levels. The regression analyses were performed with mixed-effects logistic models while adjusting for age, body mass index (BMI), and embryo quality effects. Restricted cubic splines were employed to account for possible non-linear effects where suspected (i.e., BMI).
We aimed to obtain an unbiased average treatment effect of protocols (low P4 with increase in MVP dosage, low P4 without increase in MVP dosage, and P4 levels ≥ 10 ng/ml without additional support) on OP rates by using inverse probability treatment weighting [21]. Variable selection was performed by observing baseline imbalances in the sample and including known prognostic factors of OP even if they may seem balanced between treatment groups initially. Age, BMI, and embryo quality were considered important prognostic factors and were balanced across treatment groups using generalized boosted models. Balances were checked with love plots comparing standardized mean differences (SMD) before and after weighting. Non-overlapping regions, if encountered, were trimmed to support positivity assumption [22]. The associations in the weighted sample were again tested with mixed-effects logistic models. Embryo quality was included in the regression analysis of weighted samples to obtain doubly robust estimates [23]. All analyses were conducted using R Studio Software (Posit Software, PBC, version 2023.006.2 running on R 4.2.2).
Results
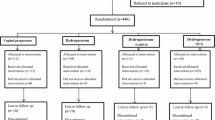
A total of 560 cycles of 507 couples were included in the analysis. There were 275 women whose serum P4 level was ≤ 10 ng/ml on the day of ET. Among those with low P4 levels, MVP dosage was increased in 210 women (37.5%) whereas in 65 women (11.6%), MVP dose remained unchanged. In 285 women (50.9%) with P4 levels 10 ng/ml or higher, LPS continued without modification. OP rates were 61.5% (40/65), 54.8% (115/210), and 48.4% (138/285) in low P4 without an increase in MVP dose, low P4 with MVP dose increase and P4 > 10 ng/ml without a change in the LPS, respectively, and without a significant difference between the groups (Figure 1). Miscarriage rates were 13.8% for P4 < 10 ng/ml, no increase in MVP group and 12.4% for P4 < 10 ng/ml, increase in MVP group, and 17.9% in the group with P4 ≥ 10 ng/ml (no change in LPS) (p = 0.199; Table 1).
Associations of serum P4 levels with OP rates were analyzed in women who did not receive any additional MVP regardless of P4 levels (n = 350). Visual inspection of conditional density plots did not show an increase in OP rates with increasing P4 levels (Figure 2). In multivariable analysis, serum P4 levels did not show a significant association with OP rates (OR 0.96, 95% CI 0.90–1.02, p = 0.185) and the estimate was adjusted for female age, BMI, and embryo quality.
Associations between P4 treatment groups and OP rates were investigated using inverse probability treatment weights. The baseline differences between treatment groups are shown in Table 2.
Initially, there were noteworthy differences (absolute SMD > 0.10 across treatment pairs) between groups in terms of female age and BMI. There was a slight imbalance (absolute SMD = 0.084) in terms of transferred poor quality embryos. After weighting, all covariates showed a maximum SMD across treatment pairs less than 0.10 (Figure S1) and the distributional balance of prognostic covariates was satisfactory (Figure S2). Regression analysis (Table 3) in the weighted sample showed no significant association between treatment groups and OP (low P4, no increase in MVP vs. P4 > 10 ng/ml, p = 0.954; low P4, no increase in MVP vs. low P4, with increase in MVP, p = 0.994). The interaction between P4 levels and treatment groups was not significant either. In the weighted sample, transfer of a good quality embryo was associated with increased odds of livebirth (vs. fair quality, OR 1.61, 95% CI 1.22–2.15, p = 0.001) and transfer of a poor quality embryo was associated with decreased odds of livebirth (vs. fair quality, OR 0.73, 95% CI 0.55–0.97, p = 0.029).
Discussion
The here presented data from single euploid HRT FET cycles using a combination of 300 mg/day MVP and 30 mg/day oral DYD for LPS suggest that measuring P4 levels on the ET day and increasing MVP in women with a P4 level < 10 ng/ml on the day of FET may not be necessary because they do not provide any therapeutic benefit and instead increase treatment inconvenience and costs.
P4 is crucial for secretory transformation of the endometrium, a prerequisite for an embryo to implant and remain implanted. Different P4 preparations are available and in routine use that can be applied orally, subcutaneously, intramuscularly, or vaginally [24]. The dosage and application method have a significant impact on the serum P4 level; the variations are briefly summarized here: MVP leads to high P4 concentrations in the myometrium and endometrium, but serum P4 levels are notably low as a result of MVP’s insufficient systemic absorption [25]; i.m. P4 injections result in an immediate rise in systemic P4 levels after 2 h and levels peak after 8 h [26]; subcutaneous administration will have peak levels after approximately 0.9 h [27]. A steady state of the oral P4 serum levels are reached after 3 days, but conventional P4 assays cannot measure circulating DYD or its active metabolite 20α-dihydrodydrogesterone; instead, only liquid chromatography-tandem mass spectrometry can detect DYD intake [28]. It must be remembered that the unique characteristics of each P4 supplementation strategy, as well as the use of various P4 measurement assays [29, 30], limit the comparability of the measured serum P4 levels and permit their interpretation only in the context of the corresponding application route.
Due to the general importance of P4 supplementation and the seeming significance of serum P4 levels as a surrogate for inaccessible endometrial P4 tissue levels in continuing HRT FET cycles, the scientific community has focused on this topic. Different serum P4 cut-off levels have been identified as outcome predictors, decreasing the likelihood of implantation, continuation of pregnancy, and live birth in women with serum P4 levels below the threshold [13, 14, 31,32,33,34,35]. Despite the fact that serum P4 levels do not accurately reflect endometrial tissue P4 levels [20], the increase of P4 supplementation, either by raising the dosage of MVP, by adding injectable (subcutaneous or i.m.) P4 preparations, or the addition of DYD, has been suggested as rescue strategy [17, 18, 36, 37]. These studies came to the unequivocal conclusion that increasing the dosage of LPS enhances the results of ART. However, a (historic) control group with lower P4 levels in which no rescue technique was included only in the study by Labarta et al. [18].
DYD is an oral drug and patients may find it more convenient than injectable or vaginal P4 therapy. LPS using DYD seems to be non-inferior when compared to MVP in fresh IVF cycles [38, 39]. However, since DYD is a synthetic P4, questions regarding its safety for the developing embryo(s) are understandably raised. Large phase III trials [38, 39] and the systematic review and individual participant data meta-analysis, which included studies with administration of DYD in dosages of 20 to 40 mg/day [40], showed similar safety profile in women receiving DYD or MVP as LPS, hence recently published data from a global pharmacovigilance study [41], published as an abstract at the annual 2023 meeting of the European Society of Human Reproduction, reported an increase of birth defects. However, the abstract does not include any information on the daily DYD dosage, given to patients included in the analysis. Further research into the safe use of DYD as LPS throughout the early stages of pregnancy is warranted due to the significance of this topic and the discrepancy in the data.
Recent studies on the use of DYD alone in FET cycles described similar outcomes when compared to MVP or i.m. P4 supplementation; however, both studies had small sample sizes [42,43,44]. Furthermore, in HRT FET cycles with the exclusive use of DYD as LPS medication, patients with DYD levels in the lower quarter had a significantly lower OP rate, suggesting that a dosage of DYD three times daily might be a suboptimal dosage for some patients [45].
Vuong et al. [42] compared MVP (400 mg twice daily) alone to MVP plus DYD (400 mg MVP and 10 mg DYD, each twice daily) in a prospective cohort trial with approximately 1400 participants. The day before the ET, blood samples were taken for serum P4 measurements; hence, they were not intended for clinical use, and LPS was maintained unaltered until the pregnancy test. The LPS regimen with MVP and DYD was associated with a lower rate of miscarriage and a higher livebirth rate. However, the subgroup analysis did not reveal a significant difference in the miscarriage rates between the two LPS regimen groups in any serum P4 level quartile, pointing towards the limited significance of serum P4 measurements when MVP and DYD are used for LPS. They concluded that combining DYD and MVP adequately supplies the endometrium with P4 and might help resolve vaginal P4 absorption problems. Consistent with the findings from Vuong et al. [42], our study found no difference in the rate of OP between the groups with serum P4 levels below and above 10 ng/ml, allowing the conclusion that the combined MVP and DYD LPS approach provides adequate P4 exposure to the endometrium, even if the contribution of MVP, as estimated by serum P4 levels, is limited. Although the adequate progestogenic effect of this combination on the endometrium cannot be inferred directly from serum P4 levels, it can be inferred indirectly from the observation that increasing the dosage of MVP in women with serum P4 levels below 10 ng/ml does not increase the OP rate.
In conclusion, P4 exposure to the endometrium seems to be sufficiently provided by the combination of 300 mg/day MVP and 30 mg/day DYD in HRT FET cycles. This might render serum P4 measurement and an increase in P4 medication in the event of “lower” serum P4 results unnecessary as demonstrated in this retrospective analysis. This study has various strengths despite its retrospective study methodology and the small sample size of women with a P4 level < 10 ng/ml and no increase in MVP, which might be considered as a limitation: aneuploidy as a contributing factor to implantation failure and miscarriage was eliminated by the analysis of just single euploid FET cycles. No other study has investigated whether any “rescue” strategy is helpful in HRT FET cycles using MVP and DYD in combination. The existence of a control group of patients with a P4 level 10 ng/ml, in which no rescue strategy was applied, points to a possible lack of a benefit of increasing MVP. Further studies are required to identify the most effective medication combination for a HRT approach, considering patient convenience and treatment costs as well as the safe use of DYD as LPS.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
References
Shapiro BS, Garner FC, Aguirre M. The freeze-all cycle: a new paradigm shift in ART. In: Nagy ZP, Varghese AC, Agarwal A, editors. In vitro fertilization [Internet]. Cham: Springer International Publishing; 2019. p. 765–78. https://doi.org/10.1007/978-3-319-43011-9_63.
European IVF Monitoring Consortium (EIM), for the European Society of Human Reproduction and Embryology (ESHRE), Wyns C, De Geyter C, Calhaz-Jorge C, Kupka MS, Motrenko T, et al. ART in Europe, 2018: results generated from European registries by ESHRE. Hum Reprod Open. 2022;2022:hoac022.
Mumusoglu S, Polat M, Ozbek IY, Bozdag G, Papanikolaou EG, Esteves SC, et al. Preparation of the endometrium for frozen embryo transfer: a systematic review. Front Endocrinol. 2021;12:688237.
Mackens S, Santos-Ribeiro S, Van De Vijver A, Racca A, Van Landuyt L, Tournaye H, et al. Frozen embryo transfer: a review on the optimal endometrial preparation and timing. Hum Reprod. 2017;32:2234–42.
von Versen-Höynck F, Schaub AM, Chi Y-Y, Chiu K-H, Liu J, Lingis M, et al. Increased preeclampsia risk and reduced aortic compliance with in vitro fertilization cycles in the absence of a corpus luteum. Hypertension. 2019;73:640–9.
Pape J, Levy J, von Wolff M. Early pregnancy complications after frozen-thawed embryo transfer in different cycle regimens: a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2022;279:102–6.
Roelens C, Blockeel C. Impact of different endometrial preparation protocols before frozen embryo transfer on pregnancy outcomes: a review. Fertil Steril. 2022;118:820–7.
Melado Vidales L, Lawrenz B, Vitorino RL, Patel R, Ruiz FJ, Marques LM, et al. Clinical and laboratory parameters associated with cycle outcomes in patients undergoing euploid frozen blastocyst transfer. Reprod BioMed Online. 2023;46:917–25.
Ruiz-Alonso M, Valbuena D, Gomez C, Cuzzi J, Simon C. Endometrial receptivity analysis (ERA): data versus opinions. Hum Reprod Open. 2021;2021:hoab011.
Díaz-Gimeno P, Ruiz-Alonso M, Blesa D, Bosch N, Martínez-Conejero JA, Alamá P, et al. The accuracy and reproducibility of the endometrial receptivity array is superior to histology as a diagnostic method for endometrial receptivity. Fertil Steril. 2013;99:508–17.
González-Foruria I, Gaggiotti-Marre S, Álvarez M, Martínez F, García S, Rodríguez I, et al. Factors associated with serum progesterone concentrations the day before cryopreserved embryo transfer in artificial cycles. Reprod BioMed Online. 2020;40:797–804.
Lawrenz B, Fatemi HM. Are serum progesterone measurements truly representative for the identification of an adequate luteal phase in hormonal replacement therapy frozen embryo transfers? Hum Reprod. 2022;37:639–43.
Labarta E, Mariani G, Holtmann N, Celada P, Remohí J, Bosch E. Low serum progesterone on the day of embryo transfer is associated with a diminished ongoing pregnancy rate in oocyte donation cycles after artificial endometrial preparation: a prospective study. Hum Reprod. 2017;32:2437–42.
Alsbjerg B, Thomsen L, Elbaek HO, Laursen R, Povlsen BB, Haahr T, et al. Progesterone levels on pregnancy test day after hormone replacement therapy-cryopreserved embryo transfer cycles and related reproductive outcomes. Reprod BioMed Online. 2018;37:641–7.
Gao H, Ye J, Ye H, Hong Q, Sun L, Chen Q. Strengthened luteal phase support for patients with low serum progesterone on the day of frozen embryo transfer in artificial endometrial preparation cycles: a large-sample retrospective trial. Reprod Biol Endocrinol. 2021;19:60.
Álvarez M, Gaggiotti-Marre S, Martínez F, Coll L, García S, González-Foruria I, et al. Individualised luteal phase support in artificially prepared frozen embryo transfer cycles based on serum progesterone levels: a prospective cohort study. Hum Reprod. 2021;36:1552–60.
du Boulet B, Ranisavljevic N, Mollevi C, Bringer-Deutsch S, Brouillet S, Anahory T. Individualized luteal phase support based on serum progesterone levels in frozen-thawed embryo transfer cycles maximizes reproductive outcomes in a cohort undergoing preimplantation genetic testing. Front Endocrinol. 2022;13:1051857.
Labarta E, Mariani G, Rodríguez-Varela C, Bosch E. Individualized luteal phase support normalizes live birth rate in women with low progesterone levels on the day of embryo transfer in artificial endometrial preparation cycles. Fertil Steril. 2022;117:96–103.
Ozcan P, Cetin C, Okten B, Tanoglu FB, Taha HS, Pasin O, et al. The importance of serum progesterone concentration at embryo transfer day and effect of rescue additional progesterone during programmed artificial frozen embryo transfer cycles. Reprod BioMed Online. 2022;45:785–92.
Labarta E, Sebastian-Leon P, Devesa-Peiro A, Celada P, Vidal C, Giles J, et al. Analysis of serum and endometrial progesterone in determining endometrial receptivity. Hum Reprod. 2021;36(11):2861–2870. https://doi.org/10.1093/humrep/deab184.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34:3661–79.
Stürmer T, Rothman KJ, Avorn J, Glynn RJ. Treatment effects in the presence of unmeasured confounding: dealing with observations in the tails of the propensity score distribution—a simulation study. Am J Epidemiol. 2010;172:843–54.
Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol. 2011;173:761–7.
IVF worldwide survery luteal phase support. Available from: https://ivf-worldwide.com/survey/progesterone-support-in-ivf/progesteron-support-in-ivf-results.html. Accessed 04 Nov 2023.
Bulletti C, de Ziegler D, Flamigni C, Giacomucci E, Polli V, Bolelli G, et al. Targeted drug delivery in gynaecology: the first uterine pass effect. Hum Reprod. 1997;12:1073–9.
Nillius SJ, Johansson ED. Plasma levels of progesterone after vaginal, rectal, or intramuscular administration of progesterone. Am J Obstet Gynecol. 1971;110:470–7.
Cometti B. Pharmaceutical and clinical development of a novel progesterone formulation. Acta Obstet Gynecol Scand. 2015;94(Suppl 161):28–37.
Neumann K, Depenbusch M, Schultze-Mosgau A, Griesinger G. Characterization of early pregnancy placental progesterone production by use of dydrogesterone in programmed frozen-thawed embryo transfer cycles. Reprod BioMed Online. 2020;40:743–51.
Patton PE, Lim JY, Hickok LR, Kettel LM, Larson JM, Pau KYF. Precision of progesterone measurements with the use of automated immunoassay analyzers and the impact on clinical decisions for in vitro fertilization. Fertil Steril. 2014;101:1629–36.
Lawrenz B, Sibal J, Garrido N, Abu E, Jean A, Melado L, et al. Inter-assay variation and reproducibility of progesterone measurements during ovarian stimulation for IVF. PLoS One. 2018;13:e0206098.
Labarta E, Mariani G, Paolelli S, Rodriguez-Varela C, Vidal C, Giles J, et al. Impact of low serum progesterone levels on the day of embryo transfer on pregnancy outcome: a prospective cohort study in artificial cycles with vaginal progesterone. Hum Reprod. 2021;36:683–92.
Alsbjerg B, Labarta E, Humaidan P. Serum progesterone levels on day of embryo transfer in frozen embryo transfer cycles—the truth lies in the detail. J Assist Reprod Genet. 2020;37:2045–6.
Melo P, Chung Y, Pickering O, Price MJ, Fishel S, Khairy M, et al. Serum luteal phase progesterone in women undergoing frozen embryo transfer in assisted conception: a systematic review and meta-analysis. Fertil Steril. 2021;116(6):1534–56.
Melo P, Wood S, Petsas G, Chung Y, Easter C, Price MJ, et al. The effect of frozen embryo transfer regimen on the association between serum progesterone and live birth: a multicentre prospective cohort study (ProFET). Hum Reprod Open. 2022;2022:hoac054.
Shekhar B, Mittal S, Majumdar G, Tiwari N, Majumdar A. Low serum progesterone on day of transfer adversely impacts ongoing pregnancy rates in hormonally prepared single blastocyst frozen embryo transfer cycles. Eur J Obstet Gynecol Reprod Biol. 2023;289:55–9.
Mackens S, Pais F, Drakopoulos P, Amghizar S, Roelens C, Van Landuyt L, et al. Individualized luteal phase support using additional oral dydrogesterone in artificially prepared frozen embryo transfer cycles: is it beneficial? Reprod BioMed Online. 2023;46:939–45.
Yarali H, Mumusoglu S, Polat M, Erden M, Ozbek IY, Esteves SC, et al. Comparison of the efficacy of subcutaneous versus vaginal progesterone using a rescue protocol in vitrified blastocyst transfer cycles. Reprod BioMed Online. 2023;47:103233.
Tournaye H, Sukhikh GT, Kahler E, Griesinger G. A Phase III randomized controlled trial comparing the efficacy, safety and tolerability of oral dydrogesterone versus micronized vaginal progesterone for luteal support in in vitro fertilization. Hum Reprod. 2017;32:1019–27.
Griesinger G, Blockeel C, Sukhikh GT, Patki A, Dhorepatil B, Yang D-Z, et al. Oral dydrogesterone versus intravaginal micronized progesterone gel for luteal phase support in IVF: a randomized clinical trial. Hum Reprod. 2018; https://doi.org/10.1093/humrep/dey306/5125950.
Griesinger G, Blockeel C, Kahler E, Pexman-Fieth C, Olofsson JI, Driessen S, et al. Dydrogesterone as an oral alternative to vaginal progesterone for IVF luteal phase support: a systematic review and individual participant data meta-analysis. PLoS One. 2020;15:e0241044.
Henry A, Santulli P, Bourdon M, Treluyer JM, Chouchana L. O-150 Birth defects reporting and the use of oral dydrogesterone in assisted reproductive technology: a global pharmacovigilance study. Hum Reprod. 2023;38:dead093.177.
Vuong LN, Pham TD, Le KTQ, Ly TT, Le HL, Nguyen DTN, et al. Micronized progesterone plus dydrogesterone versus micronized progesterone alone for luteal phase support in frozen-thawed cycles (MIDRONE): a prospective cohort study. Hum Reprod. 2021;36:1821–31.
de Macedo LCGM, Cavagna Neto M, Dzik A, Rocha A, do R, Lima SMRR. Oral dydrogesterone in frozen-thawed embryo transfer cycles. Rev Assoc Med Bras. 1992;2022(68):100–5.
Pabuccu E, Kovanci E, Israfilova G, Tulek F, Demirel C, Pabuccu R. Oral, vaginal or intramuscular progesterone in programmed frozen embryo transfer cycles: a pilot randomized controlled trial. Reprod Biomed Online. 2022;45:1145–51.
Neumann K, Masuch A, Vonthein R, Depenbusch M, Schultze-Mosgau A, Eggersmann TK, et al. Dydrogesterone and 20α-dihydrodydrogesterone plasma levels on day of embryo transfer and clinical outcome in an anovulatory programmed frozen-thawed embryo transfer cycle: a prospective cohort study. Hum Reprod. 2022;37:1183–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lawrenz, B., Kalafat, E., Ata, B. et al. The combination of dydrogesterone and micronized vaginal progesterone can render serum progesterone level measurements on the day of embryo transfer and rescue attempts unnecessary in an HRT FET cycle. J Assist Reprod Genet 41, 885–892 (2024). https://doi.org/10.1007/s10815-024-03049-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03049-1