Abstract
Purpose
To investigate the pregnancy and neonatal outcomes of letrozole-stimulated frozen embryo transfer (LTZ-FET) cycles compared with natural FET cycles (NC-FET).
Methods
Our retrospective cohort included all LTZ-FET (n = 161) and NC-FET (n = 575) cycles that transferred a single euploid autologous blastocyst from 2016 to 2020 at Stanford Fertility Center. The LTZ-FET protocol entailed 5 mg of daily letrozole for 5 days starting on cycle day 2 or 3. Outcomes were compared using absolute standardized differences (ASD), in which a larger ASD signifies a larger difference. Multivariable regression models adjusted for confounders: maternal age, BMI, nulliparity, embryo grade, race, infertility diagnosis, and endometrial thickness.
Results
The demographic and clinical characteristics were overall similar. A greater proportion of the letrozole cohort was multiparous, transferred high-graded embryos, and had ovulatory dysfunction. The cohorts had similar pregnancy rates (67.1% LTZ vs 62.1% NC; aOR 1.31, P = 0.21) and live birth rates (60.9% LTZ vs 58.6% NC; aOR 1.17, P = 0.46). LTZ-FET neonates on average were born 5.7 days earlier (P < 0.001) and had higher prevalence of prematurity (18.6% vs. 8.0%NC, ASD = 0.32) and low birth weight (10.4% vs. 5.0%, ASD = 0.20). Both cohorts’ median gestational ages (38 weeks and 1 day for LTZ; 39 weeks and 0 day for NC) were full term.
Conclusion
There were similar rates of pregnancy and live birth between LTZ-FET and NC-FET cycles. However, there was a higher prevalence of prematurity and low birth weight among LTZ-FET neonates. Reassuringly, the median gestational age in both cohorts was full term, and while the difference in gestational length of almost 6 days does not appear to be clinically significant, this warrants larger studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Clinical and laboratory advances have ushered in the widespread standard practice of single frozen embryo transfer and have lent increased importance to cycle optimization prior to embryo transfer, a crucial component of which is endometrial preparation. There are multiple protocols that may be utilized prior to embryo transfer—which include artificial (programmed, controlled, medicated), stimulated, and natural—and none has been definitively proven to be the superior preparation [1,2,3]. Recent evidence, however, suggests an increased risk of hypertensive disorders of pregnancy with artificial FET cycles, which has largely been attributed to the absence of corpus luteum formation [4,5,6,7]. This may well lead to a shift towards a higher utilization of natural-based FET cycles that use the body’s intrinsic physiology when possible. There has also been growing evidence in support of letrozole use during endometrial preparation [8,9,10,11,12]. As an aromatase inhibitor, letrozole reduces androgen conversion into estrogen in the ovarian granulosa cells. This initial decrease in estradiol (E2) upregulates estrogen receptors and increases endometrial sensitivity to rising estrogen levels, thereby enhancing endometrial proliferation prior to FET [8, 13,14,15,16,17]. There is also evidence to demonstrate letrozole’s role in improved endometrial receptivity in patients with endometriosis; increased endometrial integrin expression in response to letrozole has been shown to result in improved implantation and pregnancy rates [16, 18].
Despite this growing use, our understanding of the impact of letrozole on pregnancy outcomes in FET cycles is still in the early stages. In their large 2017 study from Japan, Tatsumi et al. found letrozole use in single blastocyst FET to be associated with increased rates of clinical pregnancy and live birth as well as a decreased rate of miscarriage [11]. More recently, Li et al.’s 2021 study from China and Takeshima et al.’s 2022 study from Japan found no significant differences in pregnancy outcomes with letrozole use [19, 20]. However, both studies included only transfer of cleavage stage embryos, and Takeshima et al. studied letrozole use for ovarian stimulation prior to natural IVF with only fresh embryo transfers, thereby limiting the generalizability to the USA as well as other countries where IVF has largely moved towards frozen embryo transfer of blastocyst stage embryos. Thus, our original study aims to evaluate whether there are differences in pregnancy outcomes between letrozole-stimulated and natural cycle frozen embryo transfer of euploid blastocysts.
Materials and methods
Patients
Our retrospective cohort study included all completed letrozole-stimulated FET (LTZ-FET) and natural FET (NC-FET) cycles with a single, autologous, and euploid blastocyst transferred at Stanford Fertility and Reproductive Health Center from June 2016 to June 2020. The LTZ-FET cohort included 134 individuals who underwent a total 161 cycles; the NC-FET cohort included 420 individuals who underwent 575 cycles. Patients with uterine anomalies and cycles that utilized donor oocytes, that were canceled, or that resulted in multiple gestations were not included. Information regarding demographic and clinical characteristics, fertility treatments, and pregnancy/neonatal outcomes were collected from medical records. Demographics and clinical characteristics included maternal age at FET, gravidity and parity, BMI, smoking status, race/ethnicity, and infertility diagnosis; cycle characteristics included serum estradiol, luteinizing hormone (LH), progesterone, and endometrial thickness at the time of ovulation trigger. The Stanford University Institutional Review Board approved the study protocol.
Natural cycle and letrozole FET treatment
The decision regarding which protocol to undergo (natural cycle or letrozole) was mainly at the discretion of the provider, utilizing shared decision-making with the patients. The standard protocol for LTZ-FET entailed the daily administration of 5 mg of letrozole for 5 days starting on cycle day 2 or 3 [8, 12]. Otherwise, patients in both cohorts underwent regular ultrasound monitoring until the dominant follicle was ≥ 18 mm, or a positive LH surge was noted (defined as LH ≥ 20 mIU/mL), at which point serum E2, progesterone, and LH levels were collected. Recombinant hCG (250 mcg Ovidrel, EMD Serono) was then used to trigger or supplement ovulation, and patients proceeded with FET only if endometrial thickness was ≥ 7 mm or if the current cycle was a personal best among a history of endometrial thicknesses below threshold (n = 4 for LTZ-FET and n = 7 for NC-FET). Two days after ovulation, patients started twice daily vaginal micronized progesterone (100 mg; Endometrin). Six days after natural LH surge or 7 days after ovulation trigger [21], FET was performed. Nine days after the transfer, serum βhCG was obtained, followed by a series of transvaginal ultrasounds 6–8 weeks after FET to assess for clinical pregnancy. Serum E2, LH, progesterone, and βhCG levels were assayed with the Roche Cobas E411 analyzer (Roche Diagnostics). The majority of patients received low-dose aspirin (81 mg) starting on cycle day 2 until 36 weeks of gestation unless they had a medical contraindication.
All embryos transferred were blastocysts derived from autologous oocytes. Blastocysts were graded from AA to DD based on the inner cell mass and trophectoderm morphology. Our clinic practice is to biopsy embryos with grade CC or higher for preimplantation genetic testing (PGT). Biopsy was performed by pipette removal of 5–8 trophectoderm cells from day 5 to day 6 fully expanded blastocysts. The survival rate of blastocyst thawing within our laboratory is 95–97%.
Study outcomes
The primary outcomes studied were rates of clinical pregnancy (presence of fetal cardiac activity), clinical miscarriage (pregnancy loss prior to 20 weeks of gestation), and live birth rate (live infant born after 24 weeks of gestation) per transfer. Additional outcomes examined were biochemical miscarriage (rise and fall in βhCG without evidence of a clinical pregnancy), ectopic pregnancy, intrauterine fetal demise/pregnancy loss after 20 weeks of gestation, caesarean delivery, gestational age at delivery, birth weight, low birth weight (< 2500 g, as defined by the World Health Organization), very low birth weight (< 1500 g), and sex assigned at birth.
Statistical analysis
Study data were managed in Stanford’s REDCap electronic data tool [22]. Patient and cycle characteristics for the LTZ-FET and NC-FET were compared using absolute standardized differences (ASD), which measure the difference in means or proportions between two groups in units of standard deviations [23]. ASD values of 0.2, 0.5, and 0.8 correspond to small, moderate, and large differences, respectively. Thus, the larger the ASD value, the larger the difference. Multivariable logistic and linear regression models determined differences in pregnancy and neonatal outcomes between the two groups while adjusting for maternal age at FET, BMI, nulliparity, embryo grade (categorized into AA, AB/BA, BB, and any C), endometrial thickness on day of trigger, race/ethnicity, ovulatory dysfunction diagnosis, polycystic ovary syndrome (PCOS) diagnosis, and recurrent pregnancy loss (RPL) diagnosis. We utilized generalized estimating equations (GEE) to account for correlation between cycles per patient. We calculated adjusted odds ratios (aOR) and 95% confidence intervals (CIs) to evaluate the association between FET type (LTZ or NC) and our outcomes of clinical pregnancies, clinical miscarriages, and live births; the LTZ-FET cohort was the reference group for all odds ratios. We calculated adjusted mean differences and 95% CI for gestational age at delivery and neonatal birth weight. Additional pregnancy and neonatal outcomes were compared between the two groups using ASD only.
Analyses were performed using the R statistical software version 3.6.2, and GEE analyses were performed using library geepack [24,25,26,27]. All statistical tests were two-sided and performed at the 0.05 significance level.
Results
Participant and cycle characteristics
From June 2016 to June 2020, a total of 134 individuals underwent 161 cycles of LTZ-FET, and a total of 420 individuals underwent 575 cycles of NC-FET. The demographic characteristics were overall similar between the two cohorts, including maternal age, BMI, smoking status, and race/ethnicity. A greater proportion of the LTZ-FET cohort was multiparous, transferred higher-grade embryos, and had an infertility diagnosis of PCOS or other ovulatory dysfunction, though these differences were not substantial with all the ASDs < 0.5 (Table 1). The cycle characteristics including peak estradiol, progesterone, and endometrial thickness at trigger were also overall similar, other than a small difference in median LH levels at trigger (Table 2).
Pregnancy outcomes
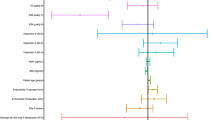
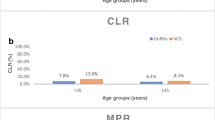
The study’s overall clinical pregnancy rate was 63.2%, miscarriage rate was 5.8%, and live birth rate was 59.1%. The LTZ-FET cohort’s clinical pregnancy rate was 67.1%, which was similar to NC-FET cohort’s 62.1% (ASD = 0.11). The two cohorts also had similar clinical miscarriage rates (8.3% for LTZ vs. 5.0% for NC; ASD = 0.13) and live birth rates (60.9% for LTZ vs. 58.6% for NC; ASD = 0.05). Furthermore, the cohorts had similar rates of biochemical miscarriage, ectopic pregnancy, intrauterine fetal demise, and caesarean delivery (Table 2). After adjusting for multiple confounders, the difference in clinical pregnancy between the two cohorts was not significant (aOR 1.31, 95% CI 0.86, 1.99; P = 0.21). Multivariable regression yielded similar results for clinical miscarriage (aOR 1.56, 95% CI 0.61, 3.99; P = 0.36) and live birth (aOR 1.17, 95% CI 0.77, 1.8; P = 0.46) (Table 3).
Neonatal outcomes
The LTZ-FET neonates had a mean gestational age of 38 weeks and 1 day at delivery (267 days; range 224–284 days), which was earlier than the NC-FET neonates’ mean gestational age of 39 weeks and 0 day (273 days; range 178–293 days) (ASD = 0.57). There was also a greater proportion of prematurity within the LTZ-FET cohort with 18.6% (n = 18) of neonates born before 37 weeks of gestation, compared to 8% (n = 27) of NC-FET neonates (ASD = 0.32) (Table 2). Notably, both cohorts of preterm neonates had similar rates of mothers with prior history of preterm birth (1.0% LTZ-FET vs 1.1% NC-FET). Among the premature neonates, the mean gestational age was 35 weeks and 3 days for LTZ-FET and 35 weeks and 5 days for NC-FET (ASD = 0.17). There were similar rates of medically indicated preterm delivery (6.1% LTZ-FET vs 4.5% NC-FET, ASD = 0.08). The medical indications for preterm delivery for LTZ-FET cohort were preeclampsia with severe features (n = 4), placenta previa (n = 1), and non-reassuring fetal status (n = 1). The indications for the NC-FET cohort were placenta previa (n = 6), preeclampsia with severe features (n = 4, one with concurrent intrahepatic cholestasis of pregnancy), history of abdominal myomectomy (n = 2), other maternal co-morbidity (n = 2), and non-reassuring fetal status (n = 1).
After accounting for multiple potential confounders, there was a statistically significant adjusted mean difference in gestational age between the two cohorts with LTZ-FET neonates born on average 5.7 days earlier than NC-FET neonates (95% CI − 8.3, − 3.0; P < 0.001) (Table 3). Furthermore, the LTZ-FET neonates overall weighed less and had more than double the rate of low birth weight (< 2500 g): 10.4% (n = 10) for LTZ-FET compared to 5.0% (n = 17) for NC-FET (ASD = 0.20; Table 2). Rates of very low birth weight neonates (< 1500 g) were similar and rare, for both cohorts. The difference in birth weight was not statistically significant after multivariable adjustment (Table 3).
Discussion
In light of the rising use of letrozole for endometrial preparation, more information is needed on the association of pregnancy and neonatal outcomes with use of letrozole. This study is the first in the USA to examine the pregnancy and neonatal outcomes of LTZ-FET cycles compared to NC-FET cycles. After controlling for multiple possible confounders, we found that LTZ-FET cycles had similar clinical pregnancy, miscarriage, and live birth rates as NC-FET cycles. While there was a higher prevalence of prematurity and low birth weight among LTZ-FET neonates, after adjusting for confounders, there was no difference in birth weight between cohorts. Furthermore, while LTZ-FET neonates arrived on average 6 days earlier, it is unclear if this difference is clinically meaningful since the overall mean and median gestational age in both cohorts were full term.
Thus far, only few studies have examined the use of letrozole for endometrial preparation, and only a small proportion of these use NC-FET cycles as the comparison; even fewer capture neonatal data. An updated 2020 Cochrane review comparing various endometrial preparations for FET noted “low-quality” evidence that suggests LTZ-FET cycles have improved clinical pregnancy rate compared to artificial cycles and “uncertain” evidence regarding miscarriage or live birth rates [1]. Zeng et al.’s 2021 metanalysis comparing stimulated to artificial FET cycles in PCOS patients found similar rates of implantation, clinical pregnancy, and live birth, but their subgroup analysis of LTZ-FET cycles noted lower miscarriage rates [28]. Another 2021 meta-analysis by Wu et al. that was not limited to one infertility diagnosis found LTZ-FET to have a significantly higher live birth rate than artificial cycles [3].
In examining outcomes compared to NC-FET, Tatsumi et al.’s large 2017 study from Japan demonstrated letrozole use in single blastocyst FET to be associated with increased rates of clinical pregnancy and live birth as well as a decreased rate of miscarriage [11]. Li et al.’s 2021 study from China found no significant differences in pregnancy rates [19], and a more recent 2022 study from Japan by Takeshima et al. found no significant differences in pregnancy or neonatal outcomes with letrozole use [20]. Both latter studies included only transfer of cleavage-stage embryos, and Takeshima et al.’s study solely examined letrozole for ovarian stimulation prior to natural cycle fresh embryo transfers.
The applicability of prior letrozole studies to current clinical settings in the USA and other countries with similar clinical practice is considerably limited by the fact that they were (1) all international with limited diversity of the population, (2) mostly included (some exclusively) cleavage-stage embryos, and (3) did not account for the use of preimplantation genetic testing (PGT) and thus embryo ploidy. Nonetheless, studies overall seem to favor the use of letrozole for endometrial preparation, suggesting that it may prime the endometrium for implantation and create a more physiologic hormonal profile to that of normal spontaneous ovulation [8,9,10,11,12]. This is thought to be achieved by letrozole’s initial reduction of serum estradiol during its use in the early follicular phase, leading to the upregulation of endometrial estrogen receptors, increased endometrial sensitivity to rising estrogen levels, increased integrin expression, and prevention of premature progesterone action; all of which could potentially enhance endometrial proliferation and receptivity prior to FET [13,14,15,16, 29]. However, given that our knowledge regarding letrozole’s effect on the endometrium is still limited, the initial reduction in estrogen biosynthesis and the postulated endometrial changes could negatively impact outcomes as well. It is our clinical experience that patients have quite variable responses to letrozole. This results in serum E2 levels that fall well outside what is thought to be physiologic in the follicular phase [30, 31], and there is some evidence that lower estradiol levels during LTZ-FET may be associated with both a higher miscarriage rate and a lower live birth rate [32].
The neonatal impact of letrozole stimulation remains largely unknown. The pharmaceutical maker of letrozole (Novartis Pharmaceuticals) warns in their report for healthcare providers the potential for letrozole to cause embryo and fetus toxicity based on animal studies findings that were corroborated by Tiboni et al.’s 2008 study [33]. Importantly, however, these studies were examining direct fetal exposure to letrozole during pregnancy. When used for endometrial preparation, letrozole’s short half-life of around 2 days implies that it should be largely cleared from the body by the time of FET [34, 35]. Thus, it theoretically should not affect the embryo and subsequent fetus [36]. A small single center study presented at the 2005 American Society for Reproductive Medicine conference suggested a higher rate of fetal malformation with the use of letrozole for ovulation induction [37], but the use of normal, spontaneously conceived deliveries as controls was non-ideal, and the study was never published. Subsequent larger, well-designed studies from multiple countries did not find increased rates of congenital anomalies with letrozole use [11, 38, 39]. In fact, data from studies such as Tatsumi et al.’s 2017 study on letrozole use in ART (n = 694 neonates) and Takeshima’s 2022 study (n = 510 neonates) reassuringly found no increased risk of major congenital anomalies following letrozole use prior to conception. Additionally, a recent 2021 meta-analysis found no evidence of increased risk of congenital fetal anomaly with letrozole use [40].
Only a few studies have looked at neonatal outcomes of letrozole for endometrial preparation, and they had similar findings to that of ours. Tatsumi et al. found slightly higher rates of prematurity and low birth weight among the letrozole cohort, while Li et al. found lower birth weights after matching for confounders, but this was not statistically significant [11, 19]. Of note, the latter study’s criteria for live birth were a gestational age of > 28 weeks, which may impact their neonatal data as extremely preterm births were not captured. Overall, these findings along with ours suggest that though there is no direct embryo or fetal exposure to letrozole, and its impact on the peri-implantation hormonal milieu and endometrium may influence the resulting conception. In fact, prior baboon studies found alterations in some indices of placental function and structure with letrozole treatment [41,42,43]. Given the lifelong consequences of prematurity, our findings highlight the need for larger and more longitudinal studies to adequately examine whether letrozole stimulation during the follicular phase impacts neonates and if there is any clinical significance to these findings.
Our cohort study has several unique characteristics. It is the first study in the USA to compare the pregnancy and neonatal outcomes of letrozole-stimulated to natural FET cycles. By including all completed cycles in our study’s 4-year period, this study minimized selection bias; by gathering all fertility, pregnancy, and neonatal data from medical records, this study minimized recall bias; and by accounting for multiple potential confounders, this study achieved a robust comparison. Lastly and importantly, all the embryos in our study were euploid blastocysts, which more accurately reflects current practice models in many countries as well as minimizes potential outcome confounders. With PGT utilization rapidly on the rise and now included in almost half of all cycles in the USA [44], it is increasingly important to account for PGT use when investigating pregnancy and neonatal outcomes [45,46,47,48].
The main limitations of our study were the sample size, the observational (non-randomized) nature, and the fact that our participant pool was from a single academic center. The lack of a unified medical record system in the USA continues to pose a significant challenge to accessing detailed pregnancy and neonatal medical records for a larger cohort of women who have undergone LTZ-FET and NC-FET cycles [49]. Furthermore, a portion of our patients delivered outside of the Stanford Health Care system, which limited our ability to ascertain the specific details of every pregnancy, including complications or detailed neonatal outcomes. The majority of our center’s patients were of Asian or Caucasian race, which could potentially limit the generalizability of our findings to other populations. Thus, further studies with broader populations are warranted.
It is important to note that, similar to all prior letrozole studies, the selection of which protocol to undergo for endometrial preparation was mainly based upon clinician judgment with no clear algorithm to guide selection. Though this study did account for multiple potential confounders in its analysis, there still remains the potential for systematic biases such as selection bias when such choices are at the discretion of the physician as they incorporate patient preferences and history, among other numerous factors. There are understandably limited means of accounting for this outside of a randomized control trial.
In conclusion, our study found similar rates of clinical pregnancy, miscarriage, and live birth between LTZ-FET and NC-FET cycles, which adds to a growing body of evidence suggesting letrozole as a prudent option for endometrial preparation. However, there was a higher prevalence of prematurity and low birth weight among the LTZ-FET neonates, who were on average born 6 days earlier. We hope that this study proves valuable in guiding patient-counseling, helps clinical decision-making prior to FET, and highlights the importance of further investigation into the neonatal consequences of letrozole use.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Glujovsky D, Pesce R, Sueldo C, Quinteiro RAM, Hart RJ, Ciapponi A. Endometrial preparation for women undergoing embryo transfer with frozen embryos or embryos derived from donor oocytes. Cochrane Database Syst Rev. 2020; 10:CD006359. https://doi.org/10.1002/14651858.CD006359.
Mumusoglu S, Polat M, Ozbek IY, Bozdag G, Papanikolaou EG, Esteves SC, et al. Preparation of the endometrium for frozen embryo transfer: a systematic review. Front Endocrinol (Lausanne). 2021;12:688237. https://doi.org/10.3389/fendo.2021.688237.
Wu H, Zhou P, Lin X, Wang S, Zhang S. Endometrial preparation for frozen-thawed embryo transfer cycles: a systematic review and network meta-analysis. J Assist Reprod Genet. 2021;38(8):1913–26. https://doi.org/10.1007/s10815-021-02125-0.
Conrad KP, von Versen-Höynck F, Baker VL. Potential role of the corpus luteum in maternal cardiovascular adaptation to pregnancy and preeclampsia risk. Am J Obstet Gynecol. 2022;226(5):683–99. https://doi.org/10.1016/j.ajog.2021.08.018.
von Versen-Höynck F, Narasimhan P, Selamet Tierney ES, Martinez N, Conrad KP, Baker VL, Winn VD. Absent or excessive corpus luteum number is associated with altered maternal vascular health in early pregnancy. Hypertension. 2019;73(3):680–90. https://doi.org/10.1161/HYPERTENSIONAHA.118.12046.
von Versen-Höynck F, Schaub AM, Chi YY, Chiu KH, Liu J, Lingis M, et al. Increased preeclampsia risk and reduced aortic compliance with in vitro fertilization cycles in the absence of a corpus luteum. Hypertension. 2019;73(3):640–9. https://doi.org/10.1161/hypertensionaha.119.13015.
Zhang J, Wei MJ, Bian XJ, Wu L, Zhang S, Mao XY, et al. Letrozole-induced frozen embryo transfer cycles are associated with a lower risk of hypertensive disorders of pregnancy among women with polycystic ovary syndrome. Am J Obstet Gynecol. 2021;225(1):59.e1-59.e9. https://doi.org/10.1016/j.ajog.2021.01.024.
Hu YJ, Chen YZ, Zhu YM, Huang HF. Letrozole stimulation in endometrial preparation for cryopreserved–thawed embryo transfer in women with polycystic ovarian syndrome: a pilot study. Clin Endocrinol. 2014;80(2):283–9.
Huang P, Wei L, Li X. Modified hMG stimulated: an effective option in endometrial preparation for frozen-thawed embryo transfer in patients with normal menstrual cycles. Gynecol Endocrinol. 2018;34:772–4.
Li SJ, Zhang YJ, Chai XS, Nie MF, Zhou YY, Chen JL, et al. Letrozole ovulation induction: an effective option in endometrial preparation for frozen-thawed embryo transfer. Arch of Gynecol Obstet. 2014;289(3):687–93.
Tatsumi T, Jwa SC, Kuwahara A, Irahara M, Kubota T, Saito H. Pregnancy and neonatal outcomes following letrozole use in frozen–thawed single embryo transfer cycles. Hum Reprod. 2017;32(6):1244–8.
Zhang J, Liu H, Wang Y, Mao X, Chen Q, Fan Y, et al. Letrozole use during frozen embryo transfer cycles in women with polycystic ovary syndrome. Fertil Steril. 2019;112(2):371–7.
Cortínez A, De Carvalho I, Vantman D, Gabler F, Iñiguez G, Vega M. Hormonal profile and endometrial morphology in letrozole-controlled ovarian hyperstimulation in ovulatory infertile patients. Fertil Steril. 2005;83(1):110–5.
Ganesh A, Chauhan N, Das S, Chakravarty B, Chaudhury K. Endometrial receptivity markers in infertile women stimulated with letrozole compared with clomiphene citrate and natural cycles. Syst Biol Reprod Med. 2014;60:105–11.
Haouzi D, Assou S, Mahmoud K, Tondeur S, Rème T, Hedon B, et al. Gene expression profile of human endometrial receptivity: comparison between natural and stimulated cycles for the same patients. Human Reprod. 2009;24(6):1436–45.
Miller PB, Parnell BA, Bushnell G, Tallman N, Forstein DA, Higdon HL 3rd, et al. Endometrial receptivity defects during IVF cycles with and without letrozole. Hum Reprod. 2012;27(3):881–8.
Velasco G, Juan A. The use of aromatase inhibitors in in vitro fertilization. Fertil Steril. 2012;98:1356–8.
Lessey BA, Castelbaum AJ, Buck CA, Lei Y, Yowell CW, Sun J. Further characterization of endometrial integrins during the menstrual cycle and in pregnancy. Fertil Steril. 1994;62:497–506.
Li D, Khor S, Huang J, Chen QJ, Lyu QF, Cai RF, et al. Frozen embryo transfer in mildly stimulated cycle with letrozole compared to natural cycle in ovulatory women: a large retrospective study. Front Endocrinol. 2021;12: 677689.
Takeshima K, Ezoe K, Kawasaki N, Hayashi H, Kuroda T, Kato K. Perinatal outcomes and congenital anomalies associated with letrozole and natural cycles in single fresh cleaved embryo transfers: a single-center, 10-year cohort study. F S Rep. 2022;3(2):138–44. https://doi.org/10.1016/j.xfre.2022.03.001.
Johal JK, Bavan B, Zhang W, Gardner RM, Lathi RB, Milki AA. The impact of timing modified natural cycle frozen embryo transfer based on spontaneous luteinizing hormone surge. J Assist Reprod Genet. 2021;38(1):219–25.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Austin P. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38:1228–34.
Højsgaard S, Halekoh U, Yan J. The R Package geepack for generalized estimating equations. J Stat Softw. 2006;15:1–11.
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. Accessed March 2022
Yan J, Fine J. Estimating equations for association structures. Stat Med. 2004;23:859–80.
Yan J. Geepack: yet another package for generalized estimating equations. R News. 2002;2:12–4.
Zeng MF, Zhou X, Duan JL. Stimulated cycle versus artificial cycle for frozen embryo transfer in patients with polycystic ovary syndrome: a meta-analysis. Gynecol Endocrinol. 2021;37(4):294–9.
Simon C, Cano F, Valbuena D, Remohi J, Pellicer A. Clinical evidence for a detrimental effect on uterine receptivity of high serum oestradiol concentrations in high and normal responder patients. Hum Reprod. 1995;10(9):2432–7.
Becker KL (2001) Principles and practice of endocrinology and metabolism. Lippincott Williams & Wilkins. pp 889, 1059–1060, 2153
Hodgen GD. The dominant ovarian follicle. Fertil Steril. 1982;38(3):281–300.
Zhang WY, Gardner RM, Kapphahn KI, Ramachandran MK, Murugappan G, Aghajanova L, et al. The impact of estradiol on pregnancy outcomes in letrozole-stimulated frozen embryo transfer cycles. F S Rep. 2021;2(3):320–6. https://doi.org/10.1016/j.xfre.2021.05.007.
Tiboni GM, Marotta F, Rossi C, Giampietro F: effects of the aromatase inhibitor letrozole on in utero development in rats. Hum Reprod. 2008; 23(8):1719–23.
Femara® (letrozole) patient prescribing information. East Hanover, NJ: Novartis Pharmaceuticals Corp. U.S. Food and Drug Administration. Available at:www.pharma.us.novartis.com/product/pi/pdf/Femara.pdf. Revised 1/2014
U.S. Food and Drug Administration (FDA). Highlights of prescribing information: Femara (letrozole). Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/020726s027lbl.pdf. Revised 1/2014
Requena A, Herrero J, Landeras J, Navarro E, Neyro JL, Salvador C, et al. Use of letrozole in assisted reproduction: a systematic review and meta-analysis. Hum Reprod Update. 2008;14(6):571–82. https://doi.org/10.1093/humupd/dmn033.
Biljan MM, Hemmings R, Brassard N (2005) The outcome of 150 babies following the treatment with letrozole or letrozole and gonadotropins [abstract]. Fertil Steril 84 (Supp 1):O-231. Abstract 1033
Sharma S, Ghosh S, Singh S, Chakravarty A, Ganesh A, Rajani S, et al. Congenital malformations among babies born following letrozole or clomiphene for infertility treatment. PLoS One. 2014;9(10):e108219. https://doi.org/10.1371/journal.pone.0108219.
Tulandi T, Martin J, Al-Fadhli R, Kabli N, Forman R, Hitkari J, et al. Congenital malformations among 911 newborns conceived after infertility treatment with letrozole or clomiphene citrate. Fertil Steril. 2006;85:1761–5. https://doi.org/10.1016/j.fertnstert.2006.03.014.
Pundir J, Achilli C, Bhide P, Sabatini L, Legro RS, Rombauts L, et al. Risk of foetal harm with letrozole use in fertility treatment: a systematic review and meta-analysis. Hum Reprod Update. 2021;27(3):474–85.
Albrecht ED, Robb VA, Pepe GJ. Regulation of placental vascular endothelial growth/permeability factor expression and angiogenesis by estrogen during early baboon pregnancy. J Clin Endocrinol Metab. 2004;89:5803–9.
Babischkin JS, Burleigh DW, Mayhew TM, Pepe GJ, Albrecht ED. Developmental regulation of morphological differentiation of placental villous trophoblast in the baboon. Placenta. 2001;22:276–83.
Rosenthal MD, Albrecht ED, Pepe GJ. Developmental maturation of primate placental trophoblast: placental cytosolic and secretory phospholipase A2 expression after estrogen suppression of baboons. Prostaglandins Other Lipid Mediat. 2001;66:155–63.
Society for reproductive assisted technology. National Summary Report for 2020. Available at: https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?#patientcumulative. Accessed April 11, 2022
Makhijani R, Bartels CB, Godiwala P, Bartolucci A, DiLuigi A, Nulsen J, et al. Impact of trophectoderm biopsy on obstetric and perinatal outcomes following frozen-thawed embryo transfer cycles. Hum Reprod. 2021;36(2):340–8.
Feldman B, Orvieto R, Weisel M, Aizer A, Meyer R, Haas J, et al. Obstetric and perinatal outcomes in pregnancies conceived after preimplantation genetic testing for monogenetic diseases. Obstet Gynecol. 2020;136(4):782–91.
Li M, Kort J, Baker VL. Embryo biopsy and perinatal outcomes of singleton pregnancies: an analysis of 16,246 frozen embryo transfer cycles reported in the Society for Assisted Reproductive Technology Clinical Outcomes Reporting System. Am J Obstet Gynecol. 2021;224(5):500. https://doi.org/10.1016/j.ajog.2020.10.043.
Zhang WY, von Versen-Höynck F, Kapphahn KI, Fleischmann RR, Zhao Q, Baker VL. Maternal and neonatal outcomes associated with trophectoderm biopsy. Fertil Steril. 2019;112(2):283–90. https://doi.org/10.1016/j.fertnstert.2019.03.033.
Floyd EG, von Versen-Hoynck F, Liu J, Chi YY, Fleischmann RR, Baker VL. Collection of pregnancy outcome records following infertility-challenges and possible solutions. J Assist Reprod Genet. 2016;33(8):993–9.
Acknowledgements
The authors would like to thank all participants and hospitals that supported the collection of these data. The use of REDCap was supported by Stanford CTSA award number UL1 TR001085 from the National Center for Research Resources (NCRR) within the National Institutes of Health (NIH). This research was supported in part by the T32 TADA-BSSR training grant from the NIH National Heart, Lung, and Blood Institute (NHLBI, grant number 1T32HL151323).
Author information
Authors and Affiliations
Contributions
W.Y.Z., B.B., A.A.M., R.B.L., and L.A. contributed substantially to study design, supervision of study protocol, and interpretation of data; W.Y.Z., J.K.J., and B.B. were responsible for data collection; W.Y.Z. and R.M.G. were responsible for data analysis. The first draft of the manuscript was written by W.Y.Z. All co-authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, W.Y., Gardner, R.M., Johal, J.K. et al. Pregnancy and neonatal outcomes of letrozole versus natural cycle frozen embryo transfer of autologous euploid blastocyst. J Assist Reprod Genet 40, 873–881 (2023). https://doi.org/10.1007/s10815-023-02759-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02759-2