Abstract
Purpose
This study aimed to present the clinical features and gene mutation characteristics of a child with 46,XY disorders of sex development (DSD) caused by a novel heterozygous mutation in the NR5A1 gene to determine the potential association between this heterozygous mutation and the pathogenesis of 46,XY DSD.
Methods
We present the case of a Chinese child with ambiguous genitalia at birth but a normal adrenal gland. Targeted next-generation sequencing, comprising 163 candidate genes involved in sexual differentiation and development, was performed, followed by the functional evaluation of the novel NR5A1 mutation.
Result
The patient had a novel heterozygous mutation in the NR5A1 gene, c.630delG (p.Y211Tfs*85). Results revealed that overexpression of p.Y211Tfs*85 impaired steroidogenic factor-1 (SF-1) protein synthesis. Immunofluorescence analysis revealed that both SF-1 wild-type and p.Y211Tfs*85 mutation proteins were localized in the cell nucleus. Furthermore, dual-luciferase reporter assay results revealed that the p.Y211Tfs*85 mutation could effectively downregulate the transcriptional activation of anti-Müllerian hormone and steroidogenic acute regulatory protein genes (P < 0.01). Additionally, the p.Y211Tfs*85 mutation changed three-dimensional conformation of SF-1, and three conformations could be constructed with the mutated amino acid sequences. Therefore, the novel frameshift mutation could result in decreased protein expression of SF-1.
Conclusion
We described a novel mutation in NR5A1 and showed that it might affect protein structure, thereby seriously compromising the role of SF-1 in regulating gonadal development. The novel p.Y211Tfs*85 mutation in the NR5A1 gene enriches the boy of information available regarding the mutation spectrum of this gene in the Chinese population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disorders of sex development (DSD) are congenital conditions characterized by atypical development of chromosomal, gonadal, or anatomical sex. On the basis of the sex chromosome content, DSD are divided into three categories: sex chromosome DSD; 46,XX DSD; and 46,XY DSD [1]. Heterozygous mutations of NR5A1 are the most prevalent genetic cause in 46,XY DSD individuals, with a frequency of approximately 15–20% [2]. Steroidogenic factor-1 (SF-1), encoded by NR5A1, plays a pivotal role in the adrenal and reproductive development and function as well as in the transcription of genes involved in steroidogenesis [3]. In early male development, SF-1 is expressed in the bipotential gonad, and it regulates the differentiation toward testes through modulation of the expression of genes such as SRY and SOX9. A previous study has showed that NR5A1 can regulate the expressions of Sry-box 9 (SOX9) and anti-Müllerian hormone (AMH) genes during mammalian testicular differentiation [4]. Additionally, steroidogenic acute regulatory protein (STAR), a pivotal factor that is involved in cholesterol mobilization and steroid hormone biosynthesis, can also be regulated by NR5A1 [5]. Furthermore, SF-1 is involved in the regression of the paramesonephric duct, which is initiated through the expression of AMH in Sertoli cells and virilization by regulation of testosterone biosynthesis in Leydig cells [6, 7]. The phenotypical spectrum encompasses not only hypospadias, ambiguous genitalia (e.g., a hypoplastic phallus), or a complete external female appearance but also male infertility [8]. At present, > 100 different mutations, mainly associated with 46,XY DSD, in the NR5A1 gene have been described, and the reported NR5A1 gene mutations related to the sex reversal phenotype mainly include NR5A1 p.R92W, p.Arg92Gln, p.T40P, p.18DKVSG22del[c.51_65del], p.Y211Tfs*83[c.630_636del], p.C33S, p.R84H,p.Y138X,c.1277dupT, [c.424_427dupCCCA]1[p.G146A],p.Gly35Asp,p.Arg84His,p.His310Asp,p.Asp364Tyr,p.47_54del, p.Arg89Glyfs17*, p.Leu209Cysfs87*, p.[Pro210Gln;Tyr211*][c.[C629A;C633A]], p.Arg39Cys, p.Ser32Asn, p.Lys396Argfs*34, and p.Cys247* [3, 9,10,11,12,13,14,15,16]. This extensive range of phenotypes hinders a direct phenotype–genotype correlation, thus highlighting the importance of molecular studies on the NR5A1 gene mutations and their impact on protein function. At present, the molecular basis of 70–80% of patients with 46,XY reversal remains unclear because of the normal sex-determining genes in these patients. Therefore, in addition to a sequencing analysis of candidate genes, various detection techniques are used to screen new related genes in sexual reversal.
Here, we report the identification of a novel c.630delG (p.Y211Tfs*85) NR5A1 mutation, which has not been reported in the previous studies to the best of our knowledge, in a 46,XY DSD patient with ambiguous genitalia at birth and a normal adrenal gland. We demonstrated the functional properties of this mutation and better elucidated the genotype–phenotype relationship, thus extending the mutation atlas of the NR5A1 gene and improving the understanding of genotype–phenotype correlations. We also investigated the altered function of SF-1 derived from the p.Y211Tfs*85 mutation in the NR5A1 gene.
Material and methods
Clinical history
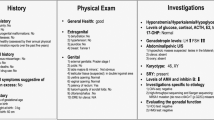
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University, China. Written informed consent was obtained from the patient’s parents. The proband was first child of non-consanguineous healthy parents. The family history was negative for DSD. The patient was born at term with a normal weight (2700 g) and length (48 cm). Ambiguous genitalia were noted at birth, micropenis, bifid scrotum, penoscrotal hypospadias, chordee, location of the urethral opening below the coronal sulcus, and labioscrotal folds without palpable gonads. A thorough evaluation was initiated at the age of 4 weeks. This included the measurement of hormone levels in the setting of a human chorionic gonadotropin (HCG) stimulation test and an ultrasound.
Mutation screening
Target-specific oligonucleotide probes were modified to capture 163 gonad-related target genes by MyGenostics Inc., and sequence libraries of the corresponding targeted genes were generated using 500 ng of DNA from a clinical sample, according to the manufacturer’s instructions. Sequencing was performed on a HiSeq 2000 System (Illumina, San Diego, CA, USA) using the Illumina Multiplexing Sample Preparation Oligonucleotide Kit and the HiSeq Paired-End Cluster Generation Kit according to the manufacturer’s instructions. After applying a quality control filter, the raw data was aligned to the human reference genome (hg19). Sequence variants were called using Sequence Alignment/Map format (SAM tools) and Picard tools (http://samtools.sourceforge.net/). Variants were filtered using the Ingenuity Variant Analysis website (http://ingenuity.com) or the gNOME project pipeline (http://gnome.tchlab.org/). The identified common variants were then reviewed for the presence or absence of the pre-selected candidate genes.
Sanger sequencing
Genomic DNA was extracted from whole blood samples taken from the patient and the parents with a Quick DNA Extraction Kit (CW3011; CWBIO). Subsequently, gDNA (2.5 ng/μl, 10 μl reactions) was amplified using 35 cycles of polymerase chain reaction (PCR) on a C1000 thermal cycler (Bio-Rad) with 2 × Flash Hot Start Master Mix (Dye) (CW3007; CWBIO) and 20 pmol of gene-specific primers. The primer sequences used to amplify NR5A1 (c.630delG (p.Y211Tfs*85)) were 5′-GAGAGCCAGAGCTGCAAGAT-3′ (forward) and 5′-CTTGTACATCGGCCCAAACT-3′ (reverse). The PCR products were purified with DNA Clean-up Kit (CW2301; CWBIO). Using a 3130xl Genetic Analyzer, the purified amplicons were directly cycle sequenced in both directions with BigDye Terminator 3.1 Ready Reaction Mix (Applied Biosystems, Grand Island, NY, USA) containing NR5A1 forward or reverse sequencing primers and then precipitated using ethanol and detected via capillary electrophoresis using Sequence Analysis 6.0 (Applied Biosystems) and Chromas 2.23 software (Technelysium, Tewantin, Queensland, Australia).
Overexpression in cell lines
A total of 293T and HeLa cell lines were purchased from American Type Culture Collection (VA, USA) and maintained in Dulbecco’s modified Eagle’s medium (DMEM) with 10% (v/v) fetal bovine serum (FBS) (Invitrogen, Carlsbad, CA) in a humidified chamber with 5% CO2 at 37 °C. The open reading frame plasmid of NR5A1 was obtained from GeneCopoeia (China). A eukaryotic gene expression pCMV6-entry vector (Forevergen Biosciences, China) was used to construct an NR5A1 overexpression system. Genes coding for NR5A1 (wild type, WT) and NR5A1 p.Y211Tfs*85 mutation were cloned into the pCMV6 vector to construct pCMV6-NR5A1 wild type (NR5A1-WT) and pCMV6-p.Y211Tfs*85 mutation plasmids (NR5A1-MUT), respectively.
Following transfection, the cells were seeded in 6-well plates (5 × 105 cell/well) containing DMEM (10% FBS without penicillin and streptomycin overnight). Quantitative reverse transcription (qRT)-PCR and western blot were performed to confirm the resultant constructs and verify the target mutation. Additionally, AMH and STAR luciferase reporter genes, which were the regulatory targets of NR5A1, NR5A1-WT, and NR5A1-MUT vectors, were co-transfected to HeLa cells. pRL-TK Renilla luciferase (Promega) was used as an internal fluorescent reference. The process of plasmid transfection was the same as mentioned above.
qRT-PCR
Reverse transcription of mRNA from differently treated 293T and HeLa cells was performed in a final volume of 100 μl from 400 ng of total RNA using the High-Capacity cDNA Archive Kit (Applied Biosystems) according to the manufacturer’s instructions. The primers utilized were the same as those used for Sanger sequencing. The qRT-PCR reactions were performed in a final volume of 50 μl containing SYBR Green PCR Master Mix (Perkin Elmer Applied Biosystems). Real-time PCR was performed using a GeneAmp PCR System 9600 (Perkin Elmer Applied Biosystems) in 96-well optical plates. The thermal cycling conditions were as follows: 2 min at 50 °C and 10 min at 95 °C followed by 40 cycles at 95 °C for 30 s, 60 °C for 30 s, and 72 °C for 2 min. Data were collected using the ABI analytical thermal cycle. RNA expression was calculated based on a relative standard curve with the ΔΔct method. The primer sequences were as follows: NR5A1, 5′-GAGAGCCAGAGCTGCAAGAT-3′ (sense) and 5′-CTTGTACATCGGCCCAAACT-3′ (antisense); GAPDH, 5′-GAGTCAACGGATTTGGTCGT-3′ (sense) and 5′-GAGTCAACGGATTTGGTCGT-3′ (antisense).
Western blot analysis
Total cellular protein in differently treated 293T and HeLa cells was isolated with the addition of 1% phenylmethylsulfonyl fluoride and radioimmunoprecipitation assay lysis buffer (50 mM Tris-HCl [pH 7.4], 150 mM NaCl, 1% NP-40, and 0.1% sodium dodecyl sulfate [SDS]). After boiling with SDS-polyacrylamide gel electrophoresis sample buffer for 5 min, the samples were electrophoresed. Then, the proteins were transferred onto a polyvinylidene difluoride membrane (Millipore, USA) and blocked for 1 h at room temperature before incubation with a 1:1000 dilution of rabbit polyclonal GAPDH and rabbit polyclonal SF-1/NR5A1/SF-1 antibody (NBP1-52823; Novus Biologicals) overnight. The primary antibody was used at a concentration of 0.5 μg/ml, and the detected molecular weight was 52 KDa. Before detection with an ECL chemiluminescence detection kit (Adventists), proteins were incubated with the corresponding secondary antibody at a concentration of Rb 1:3000. The bands were detected using an obtained by GeneGnome 5 chemiluminescence imaging system (Synoptics Ltd., UK).
Dual-luciferase reporter assay
HeLa cells were seeded into 96-well plates at a density of 3 × 105 cells/well and transfected with 30 ng of WT or MUT NR5A1 construct or empty vector together with 200 ng of the respective AMH or STAR reporter plasmid (pGL3-AMH or pGL3-STAR, respectively) and 10 ng of pRL-TK Renilla luciferase (Promega) to normalize for transfection efficiency. The pRL-TK plasmid (Promega) was co-transfected with the pGL3-Basialong and pCMV6-entry vector to normalize the luciferase activity. Following transient transfection, the cells were then incubated for 24 h. The relative luciferase activity in the different treatment groups was examined using a Dual-Glo Luciferase Assay System (Promega). The relevant experiments were performed in triplicate.
Determination of subcellular localization by immunofluorescence assay
First, cells were seeded onto 20-mm glass-bottom cell culture dishes (NEST Scientific) at a density of 0.6 × 105 cells/ml and then transfected with WT NR5A1-pcDNA3.1 or Mut NR5A1-pcDNA3.1 expression plasmids using Lipofectamine® 3000 (Invitrogen; Thermo Fisher Scientific Inc.). Cells transfected with pCMV6-entry vector using Lipofectamine® 3000 served as the control group. The cells were then fixed in 3.7% formaldehyde/phosphate-buffered saline (PBS) for 20 min at room temperature and permeabilized with 0.1% Triton X-100/PBS for 1 h at room temperature after 48 h of transient transfection. Thereafter, they were incubated overnight at 4 °C with a primary antibody against NR5A1 (1:800; Abcam) and examined by applying anti-rabbit fluorescein isothiocyanate-conjugated secondary antibody (1:500; Abcam) at room temperature for 2 h. Finally, nuclear staining was performed using a 1:1000 dilution of 4′,6-diamidino-2-phenylindole (DAPI) at room temperature for 20 min. The results were observed under a Leica TCS SP8 laser scanning confocal microscope (Leica Microsystems GmbH).
Bioinformatics analysis
Using the resolved structure of NR5A1 as a template (Protein Data Bank Accession No. 4QJR), the structure of homologous WT and the mutation NR5A1 were modeled using the SWISS-MODEL server [17] and presented using the PyMOL molecular visualization system (Delano Scientific). GraphPad Prism 7 software was utilized for statistical analysis (Table 1).
Results
Patient examination data
The patient’s hormone levels were measured in the setting of a HCG stimulation test (Tables 1, 2 and 3). The baseline and stimulated levels of testosterone, dihydrotestosterone (DHT), and 17-hydroxyprogesterone (17-OHP) levels were 27 and 91 ng/dl, 55.89 and 189.36 pg/mL, and 6.52 ng/ml and 4.20 ng/ml, respectively (Table 2). Collectively, these results indicated that the function of testicular endocrine testosterone was preserved. The patient’s serum cortisol and adrenocorticotropin hormone values were normal, and there was no evidence of adrenal insufficiency. An ultrasound confirmed the presence of bilateral inguinal testes and revealed the absence of Müllerian structures (Table 1). G-banded chromosome analysis was performed, and an SRY-positive 46,XY karyotype was revealed. The parents raised their baby as a male. He was treated with an intramuscular injection of 250 μg HCG twice a week for 5 weeks (Table 3). The testes did not descend bilaterally, and he underwent orchidopexy at the age of 6 months and a urologic surgery to repair his hypospadias at 30 months of age.
Mutation screening
Targeted next generation sequencing did not reveal any related mutations in the patient’s parents (Fig. 1a). However, the novel NR5A1 gene mutation c.630delG (p.Y211Tfs*85) was detected in the patient. Further characterization was performed with Sanger sequencing (Fig. 1b), and the results were consistent with those obtained by the targeted next generation sequencing (Table 4). Therefore, we carried out further functional verification of the NR5A1 c.630delG (p.Y211Tfs*85) mutation.
Overexpression of c.630delG (p.Y211Tfs*85) in 293T and HeLa cells
We constructed the NR5A1-MUT (c.630delG (p.Y211Tfs*85)) and NR5A1-WT plasmids for overexpression in 293T and HeLa cells (Fig. 2). The qRT-PCR results suggested that transfection by NR5A1-WT and NR5A1-MUT could promote the relative expression of NR5A1 in both 293T cells and HeLa cells (P < 0.001 vs. control cells). The relative expression of NR5A1 in the NR5A1-MUT group was also significantly higher than that in the NR5A1-WT group in both cell lines (P < 0.001 vs control cells). It was notable that the relative expression of NR5A1 in the mutation group did not exceed 100,000 times, which was more suitable for further study than that in the WT group (Fig. 2a). Meanwhile, western blot analysis did not detect NR5A1-MUT protein in the treated 293T cells and HeLa cells (Fig. 2b). This result revealed that p.Y211Tfs*85 mutation could cause destructive damage to affect SF-1 synthesis. Moreover, the NR5A1 expression determined by q-PCR and western blot analysis revealed that the HeLa cells was more appropriate for the latter research. Collectively, based on the evidence mentioned above, we selected HeLa cells to perform the further functional verification.
Cellular location analysis
To avoid or minimize the effects on the structure and function of SF-1, we used the pCMV6 vector to generate the SF-1 fusion protein. Both SF-1 WT and NR5A1-MUT proteins were expressed in HeLa cells. The expression levels of the transfected NR5A1-WT were more less than NR5A1-MUT. The corresponding immunofluorescence analysis showed that both SF-1 WT and NR5A1-MUT recombinant proteins were localized in the cell nucleus. Thus, the NR5A1-MUT did not affect the subcellular distributions (Fig. 3).
Regulation changes for downstream genes
To further validate the regulation changes of p.Y211Tfs*85 mutation to the downstream genes, we selected the known target genes of SF-1 (AMH and STAR) for further study [18]. The dual-luciferase assay system results revealed that overexpression of the NR5A1-WT plasmid could promote the transcriptional activity of AMH and STAR (P < 0.01). In contrast, overexpression of the NR5A1-MUT plasmid did not promote the transcriptional activity of AMH and STAR, which indicated that the NR5A1 c.630delG p.Y211Tfs*85 mutation could effectively downregulate the transcriptional activation of the AMH and STAR genes (Fig. 4 a and b). In summary, the NR5A1 c.630delG p.Y211Tfs*85 mutation caused destructive damage to the functional integrity of the NR5A1 protein.
The changes in transcriptional regulation of downstream target genes with mutation and WT NR5A1. The WT or mutation NR5A1 plasmid and its target gene AMH and STAR reporter gene were co-transfected into HeLa cells to detect luciferase activity. pRL-TK Renilla luciferase was used as the internal fluorescent reference. a Luciferase activity of WT and mutation NR5A1 plasmid and its target gene AMH. b Luciferase activity of WT and mutation NR5A1 plasmid with its target gene STAR. **P < 0.01
Conformational change
We constructed the conformations of WT and NR5A1-MUT type SF-1 based on the amino acid sequence (Fig. 5). The c.630delG (p.Y211Tfs*85) mutation caused a change in the three-dimensional conformation of the SF-1, with only 110 amino acids able to participate in the conformational prediction. Three different conformations could be constructed from the NR5A1-MUT type SF-1 in this study (https://swissmodel.expasy.org/interactive/XkeWFs/models/). The subsequent amino acid sequences were not involved in the formation of their spatial structure. Therefore, this frameshift mutation could result in decreased SF-1 expression.
Discussion
NR5A1 is a key transcriptional regulator in the hypothalamic–pituitary–gonadal axis. This gene was first identified on mouse chromosome 2 and named FtzF1. The frequency of NR5A1 loss-of-function mutations was found to occur in approximately 20% of 46,XY gonadal dysgenesis patients with abnormal androgenization but normal adrenal function. SF-1 was also identified as crucial for gonadal and adrenal differentiation in mammals. However, it was also revealed that heterozygous SF-1 mutations might trigger ambiguous genitalia and gonadal dysgenesis but not adrenal insufficiency in seven 46,XY patients [19]. In the present study, the novel NR5A1 heterozygous mutation c.630delG (p.Y211Tfs*85) was found in a Chinese boy without adrenal insufficiency. Hence, SF-1 mutations may occur in patients with 46,XY DSD at a much higher frequency. Furthermore, the above distinct gonadal and adrenal symptoms might result from their different susceptibilities to the partial loss of SF-1 function. Meanwhile, such causes are also responsible for 15% of patients with severe penoscrotal hypospadias and cryptorchidism [13, 20].
In humans, the NR5A1 gene is located on the long arm of chromosome 9 (9q33.3), which contains six functional exons. The protein encoded by this gene includes a DNA-binding domain (DBD), containing two C4 zinc finger structures Zn I and Zn II; an N-terminal variable domain (FTZ-F1), which is a flexible hinge region; a ligand-binding domain at the end; and a main activated domain (AF2) [21]. Additionally, a series of variants of NR5A1, including missense, nonsense, splicing mutations, and small deletions and insertions, have been discovered in various diseases. Luo et al. found that the FTZ-F1 gene was essential for sexual differentiation and primary steroid formation in NR5A1 gene-deficient mice [22]. In the past studies, scientists have found that SF-1 plays a crucial role in sex differentiation in humans. Achermann et al. found a heterozygous mutation G35E in the DBD in the SF-1 gene of a 46,XY female patient. The patient’s clinical manifestations were primary adrenal failure and relatively severe gonadal dysplasia, which indicated that this site mutation seriously affected the function of SF-1 [18, 23]. Swartz et al. identified the p.R92Q mutation of the SF-1 gene in 46,XX patients with sexual developmental disorders, which could affect the differentiation of testes and ovary [10, 24]. Moreover, Lin et al. found four mutation sites in the study of 46,XY gonadal dysplasia, including V15M, M78I, G91S, and L437Q. V15M, M78I, and G91S were activated by DNA-binding, resulting in abnormal transcription; V15M and M78I could alter the subnuclear localization of SF-1; and L437Q was speculated to disrupt SF-1 binding to the ligand [19]. Additionally, Fabbri et al. detected a p.Cys65Tyr mutation in the DBD domain of SF-1 in three 46,XY siblings. This mutation might affect the structure of SF-1 [25]. In summary, studies of the mutation sites of 46,XY patients with NR5A1 gene mutations have been focused on exons 2 and 3. Both exons are located in DBD of SF-1, which contains two important zinc finger structures. These mutation sites have a large impact on the SF-1 structure. Therefore, both exons play a crucial role in the regulation of sex differentiation. Zangen et al. have shown the association of NR5A1 with ovarian developmental and functional impairment, and it was suggested that NR5A1 mutation is related to the gradual loss of ovarian reproductive ability and has incomplete dominance [26].
In this study, we have provided the first report of the novel mutation c.630delG (p.Y211Tfs*85) in the NR5A1 gene and verified that it impacted SF-1 synthesis. XY female sexual reversal patients often show primary amenorrhea and infertility due to hypogonadal hypoplasia. Kalfa et al. have employed RNA-sequencing technology to perform transcriptome sequencing analysis of patient lymphocytes. The results showed that the expression level of MAMLD1 was significantly upregulated [27], and subsequent study revealed that MAMLD1 is a direct target gene of NR5A1 [14]. Therefore, we speculated that MAMLD1 mutations were closely related to 46,XY sexual development disorders in humans.
Conclusion
In summary, although only one polymorphic mutation was detected in this experiment, NR5A1 has been proved to act as a key transcriptional regulatory gene that is related to the steroid axis in the hypothalamus-pituitary body. The NR5A1 gene plays an important role in sexual differentiation and gonadal development. Therefore, the genetic analysis of more samples of NR5A1 gene mutations and expression levels would be extremely meaningful for understanding the mechanism of sex determination. Elucidation of the regulation mechanism of the NR5A1 signaling pathway opens a new door for the diagnosis and treatment of sexual differentiation disorders and infertile patients. However, more work is necessary to thoroughly reveal the molecular mechanism of sex reversal disease.
References
Pasterski V, Prentice P, Hughes IA. Impact of the consensus statement and the new DSD classification system. Best Pract Res Clin Endocrinol Metab. 2010;24(2):187–95. https://doi.org/10.1016/j.beem.2009.11.004.
Nagy O, Karteszi J, Hartwig M, Bertalan R, Javorszky E, Erhardt E, et al. The importance of the multiplex ligation-dependent probe amplification in the identification of a novel two-exon deletion of the NR5A1 gene in a patient with 46,XY differences of sex development. Mol Biol Rep. 2019;46:5595–601. https://doi.org/10.1007/s11033-019-04980-8.
Werner R, Monig I, Lunstedt R, Wunsch L, Thorns C, Reiz B, et al. New NR5A1 mutations and phenotypic variations of gonadal dysgenesis. PLoS One. 2017;12(5):e0176720. https://doi.org/10.1371/journal.pone.0176720.
Anamthathmakula P, Miryala CSJ, Moreci RS, Kyathanahalli C, Hassan SS, Condon JC, et al. Steroidogenic factor 1 (Nr5a1) is required for Sertoli cell survival post sex determination. Sci Rep. 2019;9(1):4452. https://doi.org/10.1038/s41598-019-41051-1.
Lin L, Achermann JC. Steroidogenic factor-1 (SF-1, Ad4BP, NR5A1) and disorders of testis development. Sexual Development : genetics, molecular biology, evolution, endocrinology, embryology, and pathology of sex determination and differentiation. 2008;2(4–5):200–9. https://doi.org/10.1159/000152036.
Suntharalingham JP, Buonocore F, Duncan AJ, Achermann JC. DAX-1 (NR0B1) and steroidogenic factor-1 (SF-1, NR5A1) in human disease. Best Pract Res Clin Endocrinol Metab. 2015;29(4):607–19. https://doi.org/10.1016/j.beem.2015.07.004.
Sekido R, Lovell-Badge R. Sex determination involves synergistic action of SRY and SF1 on a specific Sox9 enhancer. Nature. 2008;453(7197):930–4. https://doi.org/10.1038/nature06944.
Bashamboo A, McElreavey K. Human sex-determination and disorders of sex-development (DSD). Semin Cell Dev Biol. 2015;45:77–83. https://doi.org/10.1016/j.semcdb.2015.10.030.
Fabbri HC, Soardi FC, Calais FLD, Petroli RJ, Maciel-Guerra AT, Guerra-Júnior G et al. The novel p.Cys65Tyr mutation in NR5A1 gene in three 46,XY siblings with normal testosterone levels and their mother with primary ovarian insufficiency. BMC Med Genet,15,1(2014-01-10). 2014;15(1):7.
Swartz JM, Ciarlo R, Guo MH, Abrha A, Weaver B, Diamond DA, et al. A 46,XX ovotesticular disorder of sex development likely caused by a steroidogenic factor-1 (NR5A1) variant. Horm Res Paediatr. 2017;87(3):191–5. https://doi.org/10.1159/000452888.
Granados A, Alaniz VI, Mohnach L, Barseghyan H, Vilain E, Ostrer H, et al. MAP3K1-related gonadal dysgenesis: six new cases and review of the literature. Am J Med Genet C: Semin Med Genet. 2017;175(2):253–9. https://doi.org/10.1002/ajmg.c.31559.
Bashamboo A, Donohoue PA, Vilain E, Rojo S, Calvel P, Seneviratne SN, et al. A recurrent p.Arg92Trp variant in steroidogenic factor-1 (NR5A1) can act as a molecular switch in human sex development. Hum Mol Genet. 2016;25(23):5286. https://doi.org/10.1093/hmg/ddw390.
Kohler B, Lin L, Ferraz-de-Souza B, Wieacker P, Heidemann P, Schroder V, et al. Five novel mutations in steroidogenic factor 1 (SF1, NR5A1) in 46,XY patients with severe underandrogenization but without adrenal insufficiency. Hum Mutat. 2008;29(1):59–64. https://doi.org/10.1002/humu.20588.
Baetens D, Stoop H, Peelman F, Todeschini AL, Rosseel T, Coppieters F, et al. NR5A1 is a novel disease gene for 46,XX testicular and ovotesticular disorders of sex development. Genet Med. 2017;19(4):367–76. https://doi.org/10.1038/gim.2016.118.
Robevska G, van den Bergen JA, Ohnesorg T, Eggers S, Hanna C, Hersmus R, et al. Functional characterization of novel NR5A1 variants reveals multiple complex roles in disorders of sex development. Hum Mutat. 2018;39(1):124–39. https://doi.org/10.1002/humu.23354.
Fabbri-Scallet H, de Mello MP, Guerra-Junior G, Maciel-Guerra AT, de Andrade JGR, de Queiroz CMC, et al. Functional characterization of five NR5A1 gene mutations found in patients with 46,XY disorders of sex development. Hum Mutat. 2018;39(1):114–23. https://doi.org/10.1002/humu.23353.
Arnold K, Bordoli L, Kopp J, Schwede T. The SWISS-MODEL workspace: a web-based environment for protein structure homology modelling. Bioinformatics (Oxford, England). 2006;22(2):195–201. https://doi.org/10.1093/bioinformatics/bti770.
Achermann JC, Ito M, Ito M, Hindmarsh PC, Jameson JL. A mutation in the gene encoding steroidogenic factor-1 causes XY sex reversal and adrenal failure in humans. Nat Genet. 1999;22(2):125–6. https://doi.org/10.1038/9629.
Lin L, Philibert P, Ferraz-de-Souza B, Kelberman D, Homfray T, Albanese A, et al. Heterozygous missense mutations in steroidogenic factor 1 (SF1/Ad4BP, NR5A1) are associated with 46,XY disorders of sex development with normal adrenal function. J Clin Endocrinol Metab. 2007;92(3):991–9. https://doi.org/10.1210/jc.2006-1672.
Kohler B, Lin L, Mazen I, Cetindag C, Biebermann H, Akkurt I, et al. The spectrum of phenotypes associated with mutations in steroidogenic factor 1 (SF-1, NR5A1, Ad4BP) includes severe penoscrotal hypospadias in 46,XY males without adrenal insufficiency. Eur J Endocrinol. 2009;161(2):237–42. https://doi.org/10.1530/eje-09-0067.
Ferraz-de-Souza B, Lin L, Achermann JC. Steroidogenic factor-1 (SF-1, NR5A1) and human disease. Mol Cell Endocrinol. 2011;336(1–2):198–205. https://doi.org/10.1016/j.mce.2010.11.006.
Luo X, Ikeda Y, Parker KL. A cell-specific nuclear receptor is essential for adrenal and gonadal development and sexual differentiation. Cell. 1994;77(4):481–90. https://doi.org/10.1016/0092-8674(94)90211-9.
Tremblay JJ, Viger RS. A mutated form of steroidogenic factor 1 (SF-1 G35E) that causes sex reversal in humans fails to synergize with transcription factor GATA-4. J Biol Chem. 2003;278(43):42637–42. https://doi.org/10.1074/jbc.M305485200.
Harrison SM, Campbell IM, Keays M, Granberg CF, Villanueva C, Tannin G, et al. Screening and familial characterization of copy-number variations in NR5A1 in 46,XY disorders of sex development and premature ovarian failure. Am J Med Genet A. 2013;161a(10):2487–94. https://doi.org/10.1002/ajmg.a.36084.
Fabbri HC, de Andrade JG, Soardi FC, de Calais FL, Petroli RJ, Maciel-Guerra AT, et al. The novel p.Cys65Tyr mutation in NR5A1 gene in three 46,XY siblings with normal testosterone levels and their mother with primary ovarian insufficiency. BMC Med Genet. 2014;15:7. https://doi.org/10.1186/1471-2350-15-7.
Zangen D, Kaufman Y, Zeligson S, Perlberg S, Fridman H, Kanaan M, et al. XX ovarian dysgenesis is caused by a PSMC3IP/HOP2 mutation that abolishes coactivation of estrogen-driven transcription. Am J Hum Genet. 2011;89(4):572–9. https://doi.org/10.1016/j.ajhg.2011.09.006.
Kalfa N, Fukami M, Philibert P, Audran F, Pienkowski C, Weill J, et al. Screening of MAMLD1 mutations in 70 children with 46,XY DSD: identification and functional analysis of two new mutations. PLoS One. 2012;7(3):e32505. https://doi.org/10.1371/journal.pone.0032505.
Funding
This work was supported by the Guangdong Science and Technology project (grant number 2012B031800077).
Author information
Authors and Affiliations
Contributions
• Sinian Pan and Shili Guo: Formal analysis, funding acquisition, investigation,; methodology, writing original draft
• Liting Liu: Supervision, validation
• Xiaoyuan Yang and Hanmei Liang: Review and editing
Corresponding author
Ethics declarations
Ethics statement
The Research Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University approved the collection of tissue samples for research.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
We identified a patient with a novel heterozygous mutation in the NR5A1 gene, c.630delG (p.Y211Tfs*85).
The NR5A1 c.630delG p.Y211Tfs*85 mutation could effectively downregulate the transcriptional activation of the AMH and STAR.
This novel frameshift mutation resulted in a decreased protein expression of SF-1.
Rights and permissions
About this article
Cite this article
Pan, S., Guo, S., Liu, L. et al. Functional study of a novel c.630delG (p.Y211Tfs*85) mutation in NR5A1 gene in a Chinese boy with 46,XY disorders of sex development. J Assist Reprod Genet 37, 477–486 (2020). https://doi.org/10.1007/s10815-019-01676-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01676-7