Abstract
Purpose
Embryo testing to improve pregnancy outcomes among individuals who are seeking assisted reproduction technologies is increasing. The purpose of this study was to assess decisional factors through in-depth interviews for why women would accept or decline preimplantation genetic testing for aneuploidy (PGT-A) with in vitro fertilization (IVF).
Methods
Semi-structured telephone interviews were conducted with 37 women who were offered PGT-A with IVF during the summer 2017. Interviews lasted on average 40 min and were audio-recorded, transcribed, and analyzed using a content analysis.
Results
Results identified a number of decisional factors related to values about conception, disability, and pregnancy termination, past pregnancy experiences, optimism toward technology, and cost. Other key issues that were identified include the use of expanded carrier screening prior to IVF, maternal age, and limited education about PGT-A due to the complexity about education for IVF alone.
Conclusion
There is a need to develop decision support tools for the increasing choices of genetic testing options for patients seeking IVF. Including patients’ values, past pregnancy experiences and attitudes toward science into the decision-making process may help promote a more informed decision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preimplantation genetic testing for aneuploidy (PGT-A) (previously termed preimplantation genetic screening (PGS)) has been available to patients undergoing the process of in vitro fertilization (IVF) to attempt to improve their reproductive outcomes for nearly 20 years [1]. The utilization of PGT-A was established due to the frequency of aneuploidy among human embryos, which often do not result in a successful outcome or live birth. It has been estimated that approximately 40 to 60% of human embryos are abnormal, and after the age of 40 for females, this number can be as high as 80% [2,3,4]. Possible impacts or results of embryos that have aneuploidy include poor embryonic development, chromosomal abnormalities, miscarriage, or IVF failure [5].
PGT-A involves a trophectoderm biopsy (removal of a few cells from the developing placenta typically on day 5 or 6 of embryo development) and testing those cells for the presence of too few or too many chromosomes. There is some evidence that addition of PGT-A to IVF aids in embryo selection and can increase the potential success of the IVF transfer cycle, or pregnancy rate per transfer [6,7,8]. However, randomized controlled trials that demonstrate conclusive benefits are still needed. Despite limited evidence surrounding the benefits of PGT-A, this technology is routinely offered and its utilization continues to increase among assisted reproductive technology clinics [9,10,11].
The process of patient education for PGT-A is variable across different healthcare clinics with respect to who is involved in the education process and how patient understanding is assessed [12]. Some of the key components recommended for inclusion in patient education include (1) PGT-A cannot change the genetic makeup of the embryo and therefore that PGT-A does not improve the chances of achieving a pregnancy per egg retrieval; (2) PGT-A can aid in certain populations (i.e., advanced maternal age, repeated implantation failure, recurrent miscarriage) increasing the rate of successful implantation (i.e., a pregnancy) and reducing the rate of miscarriage per embryo transfer; and (3) PGT-A is not a perfect test, there are both biological and technological limitations inhibiting routine use of PGT-A [4, 9, 13, 14].
Surprisingly, there is little literature regarding patients’ experiences, attitudes, and understanding of PGT-A with IVF. Only a few studies have described patient perspectives on factors in the decision-making process for the utilization of PGT-A with IVF [13, 15]. Of those factors, cost was identified as the most significant determinant for patients’ decisions, followed by social support and acceptance from friends and family [13, 15]. Some insight can further be gleaned from research on patients’ perspectives on preimplantation genetic diagnosis (PGD), which screens embryos for a single, highly penetrant disease such as Huntington’s disease or spinal muscular atrophy [16]. Determinants when considering PGD include seeking a healthy baby, monetary costs, time and energy, accuracy of the testing, and the logistical decisions and ethical considerations of the disposition of embryos [17]. However, since PGT-A includes embryo testing prior to transfer (i.e., trophectoderm biopsy) and the limited evidence of its effectiveness to improve live birth rates, decisional factors related to why a couple using IVF would accept or decline this procedure may differ. This study fills in this gap. Its aims were to explore in-depth what factors influenced the decision making process to add PGT-A or not, and to describe patient educational experiences of IVF and PGT-A.
Methods
The Institutional Review Board at the University of Utah granted approval for the study (IRB no. 98692). A qualitative descriptive design was used to capture and assess experiences among patients who accepted or declined preimplantation genetic testing for aneuploidy (PGT-A) with IVF. A semi-structured interview guide was developed based on a review of literature and expert input. Questions were designed to capture reasons for why PGT-A was important or not with IVF prior to embryo transfer and their experiences and education with the choice (see Table 1 for a list of representative questions).
Recruitment and participants
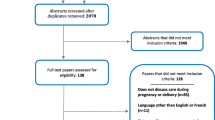
A retrospective medical chart review of women who were offered PGT-A with in vitro fertilization (IVF) between July 2016 and July 2017 was conducted at both an academic medical center clinic and a for profit clinic. Letters were mailed to the potential participants (n = 100, 50 at from each clinic) including an opt-in or opt-out pre-paid postcard to return indicating their interest in participating in this study. Approximately, 30% returned postcards (two of which indicated a choice to opt out). For those who did not return a postcard, one or two attempts were made with a telephone follow-up approximately 2 weeks after the initial letter was mailed. The total response rate, including the five respondents who were unable to be contacted for interviews after opting-in, was 42%. Participants who agreed to an interview were consented over the phone and agreed to have the interview audio recorded. Thirty-seven interviews were conducted in total. On average, interviews lasted 40 min. Each respondent who completed an interview was given a $40 gift card for her participation.
Coding and data analysis
All of the telephone interviews were audio recorded, transcribed by a professional transcription company and verified for accuracy by one of the researchers. A content analysis was used to analyze the transcript data. The data was uploaded into a qualitative software program called Dedoose [18]. A coding template was created based on the interview questions and reading of the first five transcripts. The codes were then systematically applied to the transcripts by one of the researchers (BL), with the ability to use open coding to capture data that may have been missed with the initial development of the codebook [19, 20]. The transcripts and coded data were blinded so that it was unknown who accepted or declined PGT-A. Codes were reviewed and verified independently by another researcher (ER). Once coding was complete, the coded data was separated using the query tool in Dedoose by study group (accepted or declined PGT-A), and then the codes were linked together based on similarity and summarized to identify the most frequently reported codes across and within each of the interviews for both groups of accepters and decliners.
Results
Analysis of the transcript codes revealed a number of factors impacting patients’ decision whether to accept or decline PGT-A with IVF. These include patients’ values and attitudes toward science, conception, disability, and pregnancy termination as well as experience with past pregnancies, maternal age, and costs. These themes are presented below. At the time the interviews were completed, PGS was the terminology used within the clinics so all data that used the term PGS was changed to PGT-A for consistency throughout this paper.
Demographics
Out of the 37 people interviewed, 21 chose to undergo PGT-A and 16 declined PGT-A. The average age of the participant was 37 years old with an age range of 27 to 44 years old. The majority of participants (97%) had health insurance, most were college educated (86%), and a majority (64%) reported household income over $75,000. Only four participants were currently living outside of Utah and four were not married. There were no significant differences between the two groups in demographics. The remaining demographic data, including race/ethnicity, and outcomes of their most recent IVF cycle for all participants are provided in Table 2.
Values about conception, disability, and pregnancy termination
Responses to the questions about why one did or did not elect to undergo PGT-A were strongly related to individual values about conception, disability, and pregnancy termination. Many participants stated that they elected for PGT-A because they did not want to terminate a pregnancy if the fetus was later found to have a chromosomal abnormality. Other participants wanted to avoid having a child with a disability. Three representative quotes capture these frequently expressed views:
We did not want to be in difficult position to decide if we needed to terminate a pregnancy if there was a risk to the embryo of a severe genetic defect
This is going to sound horrible, but we knew that we really wanted to have a healthy baby and that we didn't wanna deal with any Down syndrome or genetic issues. And [if] we didn't do it and then we got stuck in a situation where we had to make a decision about keeping a child or not—we didn't want to be put in that spot.
I might sound shallow, but I wanted to have a healthy baby. I know people that have Down syndrome children and stuff and it's hard. I wasn't a hundred percent sure that I was up for the challenge if that was the case.
Still, other participants wanted to avoid miscarriages and the emotional consequences of an unsuccessful embryo transfer. For example: “It was bad just following a miscarriage—if my embryos were gonna be abnormal, then I may not want to use them. Just so I don’t keep miscarrying and having that disappointment.”; and “We figured that if we knew that the embryos tested genetically normal, we would have a smaller chance of having to go through another loss.”
Several participants who declined PGT-A said they did so for religious reasons (“We felt like it all conflicted with our religious views.”). Others stated that the genetic testing information was not necessary because they would not terminate a pregnancy. For example “Because we were fine with Down syndrome. We were fine with whatever came about. We only had five embryos to work with, and so we just wanted to give them all a shot.”; and “Just because I guess we look at it as whatever is gonna happen happens.” One person stated that she thought PGT-A harmed the embryo and she did not want to damage them. Finally, some participants expressed preferences for a more “natural” conception with IVF. PGT-A, in contrast, added more “medicalization” to the process such as freezing the embryos and/or intracytoplasmic sperm injection (ICSI). Representative quotes included: “We tried naturally for a couple of years and hadn’t had success. We did a couple rounds IUI because it was more natural and then jumped to IVF as last resort.”; and “We did not want ICSI [ER, i.e., a procedure that forces the sperm into the egg] instead of actual IVF.”
Optimism in science to improve embryo selection
One of the primary differences between those who declined or elected to undergo PGT-A was their opinions about science. Those who chose PGT-A had a more optimistic view of the ability of technological advancements in science to improve their chances of a successful pregnancy. For example, a few quotes included: “Well, you don’t have to do it. We really wouldn’t suggest it.” I said, “Okay, well, then I’ll do it[laughter].”; “My husband said the only way he would do IVF is if we did it [PGT-A]. PGT-A was 100 percent worth it to make sure you are transferring a normal embryo. It was peace of mind for him.”; and “Increase your odds. Especially if you can only transfer one.”
Participants who accepted PGT-A stated that this technology was not only useful for ensuring a healthy baby but also for choosing the sex of the embryo. Although none of the participants stated that she utilized PGT-A for sex selection, almost all participants who accepted PGT-A stated that this was a positive addition to decision-making process. Two representative quotes that captured this attitude included: “Then the added bonus was we thought it would be cool that we could choose the gender.”; and “We had different reasons. My husband wanted to know the gender and I wanted to select the best embryo with the healthiest outcome.”
Of those who declined, many questioned the technology, did not want to do any direct testing on the embryo, or were willing to move forward without the information PGT-A provided. Some quotes that capture these perspectives are: “I read that there’s some controversy on whether or not it is dangerous for the embryos, or if it damages the embryo quality, so we decided not to do that.”; “We were willing to take the gamble to transfer without genetic testing.”; and “None [genetic testing] on the embryos, just testing on us.”
Additional genetic screening of embryos and parents
Another decisional factor that was identified in the interviews was the high use of other types of genetic screening, specifically expanded carrier screening with IVF. It is standard practice to conduct expanded carrier screening with IVF, but some participants appeared to misunderstand the purpose of this testing and used it to make decisions about embryo testing. Of those who declined PGT-A, some participants stated they already did genetic testing and did not need to do additional testing. For example, one participant who declined PGT-A stated “My husband, he did some genetic testing with the lab work to see if he was a carrier of certain things before. That was all we did.”; and “They told us it would just screen for all screenable genetic disorders that we were carriers for, whatever you could catch.” Conversely, participants who opted for PGT-A stated that they wanted more assurance about the health of the embryo. A representative quote included: “Because my husband and I had obviously each had our testing done to see if we had anything that matched up. We didn’t have anything—It made sense to follow this other testing option.” Finally, several participants who used gamete donation reported that genetic testing was conducted on the donor. For example, “I had genetic testing of me and the donor we were using and they did some genetic testing for carriers. That combination, it seemed reasonable to not do genetic testing [PGT-A] with IVF.”
Pregnancy history and maternal age
Many of the individuals who opted for PGT-A stated that they had failed previous transfers and wanted more explanation of why they were miscarrying. For example, “I knew that because of my age, I wanted to make sure the quality of the embryos were there.”; “I’d had two miscarriages. The second miscarriage, they genetically tested. They wanted to know why I was miscarrying.”; and “I ended up having a miscarriage. He said it was probably an abnormal embryo. With our next IVF cycle, we decided to have those embryos tested just to keep from miscarrying.” Others stated that because of their age and that they had not been pregnant before, they opted for PGT-A to ensure everything was chromosomally normal. “Yeah. It very much seemed like it was a protocol. Like, you are this age, you’re at this level, we should do this. I was like, okay. I guess we’re doing it.”; and “I guess since for me I think I’m already older, so it’s safer to do the test than just having IVF with no checking.” For those who declined, some of the reasons included that even though they were older, they did not have a previous miscarriage history, a family history of genetic conditions, or were unwilling to discard an embryo based on the result. Some quotes included: “It seemed reasonable to not do genetic testing on the first time with IVF.”; “We didn’t feel like there were any huge risk factors that we knew about.”; “I had no problems getting pregnant with them before. We just didn’t feel like it was a necessity.” and “I just felt like that I wasn’t in a place where I could just throw my embryos away if there was something wrong with them.”
Costs
All participants stated that financial burden of IVF and PGT-A was a significant decisional factor in the choice. In general, those who declined PGT-A stated that they did not want to pay the additional costs. For those that opted for PGT-A, many stated cost-effective calculations relating to pay and possible success of the procedure. For example: “Not willing to pay for IVF without knowing if it was a viable embryo.”; “Lets pick the best one if [we’re] paying this much already.”; and “So the cost of PGT-A testing was instead of transferring all those normal embryos—or those day 5 embryos that all made it—those nine of them—they PGT-A test them and it obviously played out in our favor.” The additional cost of PGT-A also allowed some participants to choose the sex of the embryo. “Let’s pay another five grand more to make sure that our embryos are good, and as a signing bonus, I mean we’re paying this much money, let’s pick the sex that we want.” Finally, for a few participants, the costs were one of the reasons IVF was their last option. (“Just the extra cost.” [reason for declining]; “It was a lot of extra money to have it done.”; and “It was just more costly and didn’t know if that would change our mind about transferring them.”)
Education about PGT-A
Questions were asked about the type of education received about PGT-A. The rationale for asking about education in relation to the decision making process for PGT-A is that it gives more context to how this was offered and how it may or may not influence choices. In general, most of the participants stated that education was provided verbally, (but a few mentioned a brochure to follow-up the verbal communication) and in conjunction with all other information provided prior to IVF. For example: “We were just told that it was to make sure that all the chromosomes were there.”; “They talked about that a little bit, but that wasn’t a huge thing they talked about. There was just a little bit of information given.”; and “Basically just talking about it’s like chromosome testing. There’s not much details. It’s like telling us to go read out the booklet more.” Other representative quotes included:
Maybe just a few sentences. I don’t think it was much. I think what I understood was that this helps us not to go through potential miscarriages, but it identifies which embryo has the biggest chances of surviving. That’s all I needed to know actually.
Never heard about it till actually we were working on the IVF treatments. The doctors and the nurses kinda suggested it just, again, because of my age, the risk for having abnormalities were a little bit higher. We were told that the chances of getting pregnant and continuing on with pregnancy was higher if we test those embryos to make sure they all had 46 chromosomes.
Discussion
This is one of the few studies to conduct an in-depth, descriptive assessment through interviews among both patients who accepted or declined PGT-A. Understanding the factors that contribute to the decision-making process of patients can help providers to incorporate this information and improve the education provided and the shared decision making process. In turn, patient experience and satisfaction may increase as a result of more informed decision-making. This study identified several determinants in the decision-making process of why a patient accepted or declined PGT-A with IVF. These included personal values toward conception, disability and pregnancy termination, trust in science, use of other genetic testing, pregnancy history and maternal age, and costs.
In a previous study, Gebhart et al. (2016) identified cost, social support, and partner and provider influences as determinants for the inclusion of PGT-A by surveying patients online [15]. This study found cost as an influential factor, thus reinforcing earlier findings. Social support was also a factor, but this was not discussed frequently in these interviews. However, this study also identified additional novel factors that many participants discussed, specifically, how personal values influenced the choice about whether or not to add PGT-A to IVF. For example, the most common reasons expressed by the participants who elected PGT-A with IVF was to avoid a miscarriage and the need to avoid future decisions about pregnancy termination as well as desire to avoid or decrease the likelihood to have a child with disabilities. Interestingly, almost all participants who elected PGT-A also mentioned sex selection. In contrast, participants in the online study of factors influencing decisions for PGT-A, 89% reported that gender identification was not important and did not influence the decision making process [15].
The results of this study also expand the quantitative findings of Gebhart et al. (2016) by identifying why those who declined adding PGT-A would not add it to IVF. The primary reason was that additional genetic information would not impact decisions to continue a pregnancy and that they were concerned that genetically testing the embryos would risk the success of the transfer, thus, again highlighting the importance of values toward pregnancy and disability as significant influences. Similar research on decision making around pre-implantation genetic diagnosis (PGD) stated that couples made decisions about PGD with IVF through four active phases of dynamic decision-making in which couples often revert back and forth [21]. However, unlike PGT-A, most couples in PGD are aware of their genetic risk status and contemplation about the decision to undergo PGD involved reflections on values toward parenthood, not necessarily pregnancy outcomes. The couples during the contemplation stage of decision making for PGD reported asking themselves if whether they want to become parents or not as why they would add PGD. In this study, all of the participants expressed the need to become parents. As such, providers who are offering PGT-A may be faced with different decisional factors than couples contemplating PGD and promoting accurate education about PGT-A should be taking into consideration for this context.
Our findings indicate that patients may not accurately understand PGT-A and its limits, and that there is a need to improve the education process regarding PGT-A with IVF. For example, a common response among women who declined PGT-A with their IVF treatment was that previous genetic testing of the parents had eliminated their risk for certain genetic conditions and/or that PGT-A was not needed or would not provide any additional information. This may suggest patients’ misunderstanding because an increased risk of aneuploidy is often not “carried” by a parent and each pregnancy carries a certain amount a risk to have aneuploidy occur by chance, relative to a woman’s age. Similarly, participants who elected PGT-A had highly positive views toward technology and science for improving IVF outcomes. Thus, educating patients about the limitations of this technology are needed to prevent positive views of technology inhibiting understanding of the real benefits of PGT-A. PGT-A is not a perfect test, and there are both biological and technological limitations that inhibit PGT-A from being diagnostic. For example, PGT-A removes cells from the trophectoderm (where the placenta would develop) and not from the inner mass cells (where the fetus would develop), and thus, it is an estimate of the likelihood that the embryo would have mosicasim. Additionally, certain deletions/duplications of chromosome material or other genetic changes, that can affect health outcomes, cannot be identified with this technology.
Current recommendations from national fertility societies still question the value of PGT-A as a universal screening test for all IVF patients [9]. Until more conclusive evidence is generated through randomized controlled trials, thorough education and counseling must be provided to address limitations, risks of errors, and lack of evidence that it improves live-birth rates [22]. This study also highlights the importance of this pre-test education in that in most participants, there were some misconceptions and gaps in knowledge about PGT-A and how it differs from other genetic testing offered with IVF.
Several reasons may account for this educational gap. Although many of the participants stated that PGT-A was discussed verbally in the context of other general information with IVF, it can be difficult for patients to understand the complexities of genetic testing, especially given the emotional impacts of the IVF process [23]. Moreover, although clinicians may be providing accurate education about PGT-A, highly optimistic views toward science in general may cause barriers to adequate patient comprehension about the risks and benefits of this genetic testing [24]. Finally, it is possible that how participants understand information about PGT-A is closely connected with their values and other beliefs about risk estimates and probabilities for success. None of the participants reported how such issues were discussed, or considered, although these are often used in decision support tools when dealing with multiple choices for healthcare utilization such as PGT-A [25]. Indeed, individual’s previous experiences and values are unique and influence the decision-making process as are individual’s knowledge and actual risk estimates for embryo transfers. Thus, to address this educational gap, a decision aid to support patient informed decision may be warranted. In addition, for individuals considering adding PGT-A to their IVF treatment, there is a need to explore, consider, and identify the emotional impacts that information from PGT-A can elicit prior determining whether to add PGT-A to IVF.
Study limitations
This study is limited by the relatively small sample size and use of only two IVF healthcare centers. Because only female participants were identified and offered to participate in the study, the experience of male partners using PGT-A was not explored. Additionally, this was a qualitative descriptive research study with self-selected participants. The views of those who declined to participate in the interview are not represented. The majority of women who participated had education beyond an associate’s degree, identified as Caucasian, higher socioeconomic status, and insured. This population may have better access to IVF treatments and the views of other populations may have not been captured. Further, participants self-selected to participate in interviews, and as such, this sample may have more experience and knowledge about genetics and, as such, chose to participate. It is unknown the demographics of those that choose not to participate. Future research will need to include more diverse samples to assess if more patients remember the offer of PGT-A.
Conclusion
More and more women are electing to pursue IVF and genetic testing, including PGT-A [26]. Identifying ways to inform and educate patients about the purpose, benefits, limitations, and impacts of PGT-A is essential. It will be important that patients’ healthcare providers help in facilitating the decision-making process for IVF and the consideration of the addition of genetic testing. Development of a decision-making tool to use in addition to provider’s information may further help address these concerns and potentially allow patients to better consider genetic testing options with IVF treatments. For example, discussing patients’ values about for conception, pregnancy, and disability may help promote more informed decision-making. Future studies could develop or evaluate a decision-making tool to assist patients to reflect on personal values while navigating genetic testing with IVF treatment as well as inclusion of more diverse groups.
References
Rubio C, Rodrigo L, Mir P, Mateu E, Peinado V, Milán M, et al. Use of array comparative genomic hybridization (array-CGH) for embryo assessment: clinical results. Fertil Steril. 2013;99(4):1044–8.
Fragouli E, Wells D, Whalley KM, Mills JA, Faed MJW, Delhanty JDA. Increased susceptibility to maternal aneuploidy demonstrated by comparative genomic hybridization analysis of human MII oocytes and first polar bodies. Cytogenet Genome Res. 2006;114(1):30–8.
Bielanska M, Tan SL, Ao A. High rate of mixoploidy among human blastocysts cultured in vitro. Fertil Steril. 2002;78(6):1248–53.
Dahdouh EM, Balayla J, Audibert F, Genetics Committee, Wilson RD, Audibert F, et al. Technical Update: Preimplantation Genetic Diagnosis and Screening. J Obstet Gynaecol Can. 2015;37(5):451–63.
Scott RT Jr, Ferry K, Su J, Tao X, Scott K, Treff NR. Comprehensive chromosome screening is highly predictive of the reproductive potential of human embryos: a prospective, blinded, nonselection study. Fertil Steril. 2012;97(4):870–5.
Brezina PR, et al. Evaluation of 571 <em>in vitro</em> fertilization (IVF) Cycels and 4,873 embryos using 23-chromosome single nucleotide polymorphism (SNP) microarray preimplantation genetic screening (PGS). Fertil Steril. 2012;97(3):S23–4.
Forman EJ, Tao X, Ferry KM, Taylor D, Treff NR, Scott RT. Single embryo transfer with comprehensive chromosome screening results in improved ongoing pregnancy rates and decreased miscarriage rates. Hum Reprod. 2012;27(4):1217–22.
Besser AG, Mounts EL. Counselling considerations for chromosomal mosaicism detected by preimplantation genetic screening. Reprod BioMed Online. 2017;34(4):369–74.
Penzias A et al. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109(3):429–436. https://doi.org/10.1016/j.fertnstert.2018.01.002.
Harper JC, Wilton L, Traeger-Synodinos J, Goossens V, Moutou C, SenGupta SB, et al. The ESHRE PGD consortium: 10 years of data collection. Hum Reprod Update. 2012;18(3):234–47.
Brezina PR, Ke RW, Kutteh WH. Preimplantation genetic screening: a practical guide. Clin Med Insights Reprod Health. 2013;7:37–42.
McGowan ML, Burant CJ, Moran R, Farrell R. Patient education and informed consent for preimplantation genetic diagnosis: health literacy for genetics and assisted reproductive technology. Genet Med. 2009;11(9):640–5.
Brezina PR, Kutteh WH, Bailey AP, Ke RW. Preimplantation genetic screening (PGS) is an excellent tool, but not perfect: a guide to counseling patients considering PGS. Fertil Steril. 2016;105(1):49–50.
Committee, E.P.C.S. ESHRE preimplantation genetic diagnosis consortium: data collection III (may 2001). Hum Reprod. 2002;17(1):233–46.
Gebhart MB, Hines RS, Penman A, Holland AC. How do patient perceived determinants influence the decision-making process to accept or decline preimplantation genetic screening? Fertil Steril. 2016;105(1):188–93.
Chang J, Boulet SL, Jeng G, Flowers L, Kissin DM. Outcomes of in vitro fertilization with preimplantation genetic diagnosis: an analysis of the United States assisted reproductive technology surveillance data, 2011–2012. Fertil Steril. 2016;105(2):394–400.
Genoff Garzon MC, Rubin LR, Lobel M, Stelling J, Pastore LM. Review of Patient Decision-Making Factors and Attitudes Regarding Preimplantation Genetic Diagnosis. Clin Genet. 2017; https://doi.org/10.1111/cge.13174.
Dedoose. Dedoose Version 7.0.23: Web application for managing, analyzing, and presenting qualitative and misxed method reearch data. Los Angelos: SocioCultural research Consutlants, LLC; 2016.
Miles M, Huberman AM, Saldana J. Qualitative data analysis: A methods sourcebook. 3rd ed. Los Angeles: Sage; 2014.
Rothwell, E., et al. Experiences among women with positive prenatal expanded carrier screening results. J Genet Couns, 2016.
Hershberger PE, Gallo AM, Kavanaugh K, Olshansky E, Schwartz A, Tur-Kaspa I. The decision-making process of genetically at-risk couples considering preimplantation genetic diagnosis: Initial findings from a grounded theory study. Soc Sci Med. 2012;74(10):1536–1543.https://doi.org/10.1016/j.socscimed.2012.02.003.
Practice Committee of Society for Assisted Reproductive Technology, Practice Committee of American Society for Reproductive Medicine. Preimplantation genetic testing: a practice committee opinion. Fertil Steril. 2008;90(5 Suppl):S136–43. https://doi.org/10.1016/j.fertnstert.2008.08.062.
Ying L, Wu LH, Loke AY. The effects of psychosocial interventions on the mental health, pregnancy rates, and marital function of infertile couples undergoing in vitro fertilization: a systematic review. J Assist Reprod Genet. 2016;33(6):689–701. https://doi.org/10.1007/s10815-016-0690-8.
Garrett N, Sharot T. Optimistic update bias holds firm: three tests of robustness following Shah et al. Conscious Cogn. 2017;50:12–22.
Stacey, D., et al. Decision aids for people facing health treatment or screening decisions. In Cochrane Database Syst Rev. 2011.
Collins SC, Xu X, Mak W. Cost-effectiveness of preimplantation genetic screening for women older than 37 undergoing in vitro fertilization. J Assist Reprod Genet. 2017;34:1515. https://doi.org/10.1007/s10815-017-1001-8.
Acknowledgements
The authors would like to thank the University of Utah Graduate Program in Genetic Counseling and the Creative Research Grant program for their support for this research. We would like to thank the Utah Center in Excellence in Ethical, Legal and Social Implications (HG009037) and the Center for Clinical and Translational Science program (1UL1TR001067) for their partial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lamb, B., Johnson, E., Francis, L. et al. Pre-implantation genetic testing: decisional factors to accept or decline among in vitro fertilization patients. J Assist Reprod Genet 35, 1605–1612 (2018). https://doi.org/10.1007/s10815-018-1278-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1278-2