Abstract
During the diagnostic evaluation period for autism or intellectual disability (ID), families of young children are at risk for poor adjustment. The present study aimed to document family quality of life (FQOL), along with associated risk and protective factors, during this critical step of families’ services trajectory. FQOL was measured in a large sample of families of children recently diagnosed with a neurodevelopmental disorder and examined in relation to the type of services received, children’s clinical profile, and family variables. FQOL was related to types of services, children’s challenging behavior, parenting stress, and several aspects of family composition and status. These findings highlight a need for mental health support for parents, coaching interventions for challenging behaviors, and family-centered supports.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The period during which families of children with autism spectrum disorder (ASD) or intellectual disability (ID) have their child assessed, receive a diagnosis, and seek out appropriate interventions can entail major challenges to family functioning, uncertainty, and other stressors for parents (Boshoff et al., 2019; Mello et al., 2021; Moh & Magiati, 2012; Rivard et al., 2014, 2021). Prompt access to assessment and intervention services, the quality of these services and related supports, and how parents experience working with providers can have a strong influence on family adjustment and quality of life during this period, as well as throughout their pathway through services (Crane et al., 2016; Jashar et al., 2019; McCrimmon & Gray, 2020; Rivard, Mello, et al., 2020 ; Rivard, Millau, et al., 2020). In actuality, studies and surveys document extensive waiting lists to access assessment and early interventions, diagnostic evaluations that do not always follow best practices, and several sources of parental dissatisfaction related to lack of support and guidance during the assessment process and following the child’s diagnosis (Austin et al., 2016; Boshoff et al., 2019; Chamak et al., 2011; Crane et al., 2016; Lappé et al., 2018; Legg & Tickle, 2019; Makino et al., 2021; Penner et al., 2015; Reed & Osborne, 2012; Shepherd & Waddell, 2015; Yi et al., 2020). These shortcomings of service provision in relation to families’ needs can exacerbate pre-existing vulnerabilities (e.g., challenges posed by the child’s symptoms, complex care needs, social isolation, concerns about the future) and thus place families at heightened risk for adjustment difficulties and lower quality of life.
To address these concerns, a pediatric clinic for the diagnosis of ASD and ID was recently piloted in an urban center in Québec, Canada (see https://chaireditc.uqam.ca/vcmf/) over the course of six years (2015–2021). Its goals were to develop and evaluate a family centered clinical model for the diagnostic evaluation of young children suspected to have ASD or ID based on best practices in assessment and that would also incorporate strategies to support families during this critical period of their care and service trajectory. The concept of care and service trajectory refers to the sequence of steps that service users (in our case, families) take to gain access to a range of services, supports, and interventions and the transitions between these. It encompasses the objective features of this pathway (e.g., duration, organization) as well users’ subjective experience of it. This idea has been extensively developed in the work of Barelds et al. (2009) and was recently applied specifically to the diagnostic care and service trajectory for ASD and ID by Rivard et al. (2020, 2021). In response to parents’ needs and sources of dissatisfaction frequently raised in studies on families’ experiences during stage of their trajectory (e.g., Boshoff et al., 2019; Crane et al., 2016; Lappé et al., 2018; Makino et al., 2021; Roth et al., 2016), the pilot clinic adopted a model for assessment services that would (1) be based on best practices for the diagnostic evaluation of ID and ASD; (2) involve a multidisciplinary team of professionals who received specialized training and would benefit from resources such as continuing education, supervision, and organizational practices intended to foster expertise and quality of life in the workplace; (3) include mechanisms (i.e., a care navigator) to support parents throughout the assessment process and following the child’s diagnosis until they access public early intervention services; (4) provide parents with informational resources about the assessment process, the child’s diagnosis, and available services; (5) make clinical recommendations and provide guidance on how these recommendations can be applied at home by a specialized interventionist after the diagnosis; and (6) propose different interventions and supports (e.g., parent coaching group) based on the child’s diagnosis while the family awaits access to public services (for more details, see the Method section and Morin, Abouzeid et al., 2020).
Thus, the pilot clinic adopted a family-centered care model that envisions the steps of the evaluation process and related supports prior to, during, and following the diagnosis with the aim of promoting and supporting functioning within the family system and, by extension, positive outcomes for children. A research program implemented in parallel with this clinic sought to document this clinical model, evaluate its implementation and validity, and assess its impact on families’ experience. The outcomes of this project would then drive recommendations for the province’s public health and social services, which are responsible for providing assessment services for children suspected of ASD or ID. In connection with this goal, the present study documented family quality of life (FQOL) during the period following the child’s diagnosis in a large sample of families who received assessment services from the pilot clinic and in families who received these services within the public health and social services system prior to the implementation of the clinic. It additionally sought to identify contextual (i.e., the organization providing assessment services: pilot clinic vs. public agencies), child-related (e.g., challenging behavior or symptoms), or family-related (e.g., income, employment) risk and protective factors in relation to family adjustment (i.e., FQOL).
Families’ Experiences during Diagnostic evaluation
As soon as they begin to have their first concerns of atypical development in their child, families must learn to navigate a complex social and health system to obtain information about their child’s condition and available services while also processing their own feelings and concerns about their future (Brewer, 2018; Lappé et al., 2018; McCrimmon & Gray, 2020). As they progress along this journey, they also become aware of the importance of early intervention and other supports to ensure the best long-term outcomes for their child and the family unit (Rivard et al., 2015, 2021). However, because these services are often contingent on a formal diagnosis, parents may experience contradictory feelings toward the assessment process. On the one hand, they anticipate and experience negative emotions due to its demands on the family (i.e., time, financial resources) and the potential consequences of its outcome; on the other hand, they are also eager to obtain answers and thus access resources that will improve their child’s prognosis (Brewer, 2018; Lappé et al., 2018). Taken together, these elements place additional stress on families who already experience numerous adjustments demands associated with parenting a young child (Gould et al., 2018; Rivard et al., 2014; Whittingham & Coyne, 2019).
Several studies highlight the potential protective influence, in terms of family adjustment and quality of life, of a model for diagnostic services that provides more support during the assessment phase (e.g., availability of information about the assessment process, diagnoses, and available services; Crane et al., 2016; Hennel et al., 2016; Mansell & Morris, 2004; Osborne & Reed, 2008; Renty & Roeyers, 2005; Yi et al., 2020; Zarafshan et al., 2019), fosters positive provider-parent partnership and promotes providers’ expertise (e.g., Boshoff et al., 2019; Lappé et al., 2018; Rivard et al., 2021), and includes access to care navigators (Makino et al., 2021; Roth et al., 2016) and other supports while on a waiting list for services (e.g., parental coaching, emotional support; Crane et al., 2016; DePape & Lindsay, 2015; Ooi et al., 2016; Rivard et al., 2019). However, research has also indicated that the challenges and obstacles to accessing adequate diagnostic evaluation services may disproportionately impact some families, as evidenced by the substantial racial and ethnic disparities documented in children’s age at diagnosis, the quality of diagnostic and intervention services, and parental satisfaction (Bishop-Fitzpatrick & Kind, 2017; Emerson et al., 2016; Fountain et al., 2011; Magaña et al., 2016; Rivard et al., 2020; Stahmer et al., 2019; Zuckerman et al., 2017). A lower quality of the assessment process has also been tied to lower family socioeconomic indicators such as parental education, employment, and income (Mazurek et al., 2014; Moh & Magiati, 2012; Stahmer et al., 2019).
Previous studies investigating family adjustment in ASD in general, but also specifically on the diagnostic period, have mainly focused on parenting stress and negative outcomes (e.g., caregiver burden or poor mental health; Mello et al., 2019). In contrast, there has been less attention to other elements of family functioning beyond parents’ mental health, or on protective factors. However, a family outcomes perspective on research in this field, which suggests an emphasis on family-oriented data such as FQOL indicators, has been emerging in recent years. Indeed, a growing number of scholars underscore the importance of studying the role of access to ASD-related services in FQOL. At this time, there have been few empirical studies in this direction, and fewer still that specifically examine the early stages of families’ care and service trajectory (i.e., as families seek out a diagnosis) and factors that could promote family functioning and well-being in this crucial period.
FQOL in ASD and ID
There exist a range of definitions for FQOL, which is acknowledged to vary cross-culturally (Fung et al., 2021). However, there is consensus that it describes the extent to which the family’s needs are met and its members enjoy their life together, can interact as a family, and have opportunities to pursue activities that are important to their well-being (Turnbull et al., 2004). In contrast to the typical focus on child outcomes, the assessment of FQOL aims to understand needs more comprehensively at the family level. This represents a progression within disability research toward family-centered care and family-centered data in acknowledgement of the essential role that families play in the well-being of the child (Zeng et al., 2020). Family functioning in the context of having a child with a disability can be examined across a range of domains such as family interactions, perceived emotional and material resources, and supports in relation to this disability. When evaluated at a specific moment in families’ care and service trajectories, FQOL can also help researchers identify risk and protective factors that may act on family systems and, consequently, better understand which services are most beneficial during important transitional periods in the life of a child with a disability.
The study of FQOL in the field of ASD has been gaining momentum (for systematic reviews, see Eapen & Guan 2016; Vasilopoulou & Nisbet, 2016). However, there remains a need for studies of specific age ranges or time periods in relation to ASD services conducted on a large scale (but see Mello et al., 2019). In particular, families who recently received a diagnosis of ASD for their child are especially likely to experience poor FQOL and need of family-centered supports (Corcoran et al., 2015). The scientific literature has identified risk and protective factors in relation to the child’s clinical profile and the family’s situation. For instance, among children’s developmental and clinical profile variables, lower FQOL has been associated with a higher severity of autism symptoms (Alhazmi, Petersen & Donald, 2018; Dardas & Ahmad 2014; Mello et al., 2019; Pozo et al., 2014; Schlebusch et al., 2017Wang et al., 2018), higher rates of challenging behavior (McStay et al., 2014; Pozo et al., 2014; Vasilopoulou & Nisbet, 2016), and lower levels of adaptive behavior and intellectual functioning (Gardiner & Iarocci, 2015; Mello et al., 2019). Furthermore, families with higher household incomes (Alhazmi et al., 2018;Dardas & Ahmad 2014; Gardiner & Iarocci, 2015; Lu et al., 2015; Schlebusch et al., 2017) and part- or full-time employment for parents(Dardas & Ahmad, 2014; Kuru & Piyal, 2018; Vasilopoulou & Nisbet, 2016), are comprised of two parents (Mas et al., 2016; Schlebusch et al., 2017), have fewer children, and have lower levels of parenting stress (Dardas & Ahmad, 2014; Hsiao et al., 2017) tend to have higher FQOL outcomes. Previous work has also noted that immigrant status and language may be connected to the quality of the diagnostic period (Zuckerman et al., 2017), however the link between these family characteristics and FQOL has been less studied. Based on evidence that families who were born in another country or speak a different language than the host country show lower satisfaction and report a lower quality of services, we hypothesized that these families may also report lower FQOL during the diagnostic period. Furthermore, to date, few studies have considered systemic or organizational (i.e., contextual) factors such as the type of services received in a specific period of the care and service trajectory (e.g., in this case the diagnostic period) in connection to FQOL, despite repeated suggestions that FQOL measures be included in program evaluation initiatives.
Objectives
The primary objective of the present study was to examine whether the use of family-centered diagnostic evaluation services from the pilot clinic were associated with higher FQOL than what families typically experience within the existing public system (for more details on diagnostic evaluation practices in this province, see Collège des Médecins du Québec et Ordre des psychologues du Québec, 2012). Because the pilot clinic adopted a model that specifically sought to address sources of parental dissatisfaction and incorporated several practices found to promote family well-being in previous studies, it was hypothesized that families who made use of its services would report higher FQOL across all dimensions than those who received a diagnosis within the public system, even after taking into account child- and family-related variables associated with FQOL (H1). The second goal of the study was to promote a better understanding of FQOL in families of children who recently underwent diagnostic evaluation for suspected ASD or ID, as well as the risk and protective factors associated with this outcome at this critical moment in their care and service trajectory. This was accomplished by assessing a range of dimensions of FQOL in a large sample of families (who received different evaluation services, see H1) along with information about children’s clinical profiles and important family variables. Specifically, we hypothesized that families whose children have less severe autism symptoms (H2), display lower rates of challenging behavior (H3), and have higher levels of adaptive behavior (H4) and intellectual functioning (H5) would report higher FQOL. It was also expected that FQOL would be higher in families presenting the following characteristics: higher income (H6), parental employment (H7), two-parent household composition(H8), fewer children (H9), lower parental stress (H10), native to Canada (H11), and speaking either English or French at home (H12).
Method
Participants
Participants were 547 families who had recently received free diagnostic evaluation services either from the existing public network of hospitals and social and health services agencies mandated to provide this service (Public System, n = 288) or from a pilot assessment clinic implemented to address some challenges within this network (Pilot Clinic, n = 259). All had been referred for suspicion of ASD or ID to either of these which specialize in the evaluation of children suspected of having these conditions. Because evaluations were completed in English or French, parents’ ability to speak either language was a criterion for inclusion in the present study. Across the entire sample, 93.8% of children received a diagnosis of ASD, 1.6% were diagnosed with ID, and 4.6% were diagnosed with another neurodevelopmental disorder (e.g., language disorder, global developmental delay [GDD]). They were mostly boys (80%) and aged between 1.6 and 7.1 years (M = 4.1, SD = 0.9) at the time of the diagnosis. Children from the pilot clinic were slightly older (M = 4.4, SD = 1.1) than those evaluated in the public system (M = 3.8, SD = 0.6; t(539) = -7.63, p < .001), but no differences were observed between the two samples in terms of children’s sex (80% boys in both groups, χ²(1) = 0.00, p = .986).
Tables 1 and 2 summarize families’ and children’s characteristics for both groups. Most families were nuclear (i.e., two-parent families), but a greater proportion of pilot clinic service users were single-parent families. The majority (75.7%) of families had household incomes in brackets below CAD90,000 and, thus, below the mean household income in the province where the study was conducted (CAD98,700). Half of all mothers, and over 80% of fathers, were employed. Children who were assessed through the pilot clinic, rather than in the public system, tended to have lower autism symptom severity scores and to score higher on measures of intellectual quotient (IQ) and adaptive behavior. Their parents also tended to display lower levels of parenting stress than those of children assessed within the public system.
Diagnostic evaluation settings
Pilot Clinic
The logic model adopted by the pilot clinic was developed with the purpose of assisting families who were on the waiting list for assessment services within the public network of health and social services (e.g., hospitals and specialized agencies mandated with the diagnostic evaluation of ASD, ID, or GDD) in Montreal (Quebec, Canada). This pilot initiative sought to develop and test, over a 6-year period, a clinical model that would support the assessment of ASD and ID in early childhood according to best practices, carried out efficiently (in terms of duration, referral process, and service coordination) by a multidisciplinary team. It also included family support mechanisms intended to facilitate the assessment process and to promote family members’ adjustment during this difficult period. To this end, each family was assigned to a care navigator who would accompany them until their child was enrolled in public intervention services. This person informed and supported families throughout the evaluation process and had regular postdiagnostic follow-up sessions with them until they secured the appropriate interventions for their child’s diagnosis. Additionally, families were offered postdiagnostic information and support meetings to help them understand and adjust to their child’s diagnosis, regular follow-up phone calls by the care navigator, guidance in applying for grants and subsidies, suggestions for behavioral interventions from a behavior analyst, peer support groups for parents, and an information toolkit on treatments and resources available within the community.
Public System
Other children and families who participated in the present study were assessed prior to the implementation of the pilot clinic in 2015. Instead, they received diagnostic evaluation within the public health and social services system, according to provincial guidelines for the assessment of ASD and ID (Collège des Médecins du Québec et Ordre des psychologues du Québec, 2012). These services were provided by area hospitals or affiliated assessment clinics specialized in ASD and ID.
Measures
Family Quality of Life
FQOL was assessed through the Beach Center Family Quality of Life scale (Hoffman et al., 2006; French translation and validation by Rivard et al., 2017). Respondents use a 5-point Likert scale to rate their level of satisfaction with 25 aspects of family life organized into five subscales: Family Interaction, Parenting, Emotional Well-being, Physical/Material Well-being, and Disability-related Support. Higher scores represent higher FQOL. The original instrument had acceptable to excellent subscale (α = 0.74–90) and good full-scale internal consistency (α = 0.88) along with good convergent validity and test-retest reliability (Hoffman et al., 2006). The French translation demonstrated acceptable to good internal consistency across subscales (α = 0.72–82) and excellent internal consistency at the full-scale level (α = 0.90; Rivard et al., 2017). The instrument also had acceptable to good internal consistency across subscales in the present study (α = 0.63-0.82) and excellent internal consistency for the full scale (α = 0.91).
Intellectual functioning
Three measures of intellectual functioning were used to assess intellectual functioning based on characteristics of the child (i.e., age, level of cooperation, verbal communication): the Wechsler Preschool and Primary Scale of Intelligence – Fourth Edition (WPPSI-IV; Wechsler 2012), the Bayley Scales of Infant & Toddler Development III (BSID-III; Bayley, 2006), and the Leiter International Performance Scale (Leiter-3; Roid et al., 2013). The WPPSI-IV full-scale IQ, the BSID-III Cognitive Composite, or the Leiter non-verbal IQ (all M = 100, SD = 15), as applicable for each child, were retained as indicators of intellectual functioning in the present study. These measures had internal consistencies ranging from acceptable to excellent (WPPSI-IV: α = 0.71–94, Soares & McCrimmon 2013; BSID-III: α = 0.83–94, Albers & Grieve 2007; Leiter-3: α = 0.96, Kranzler & Floyd 2013).
Children’s intellectual functioning was assessed with the most appropriate standardized test for their chronological age and for which a baseline score could be obtained. For most participants, the WPPSI-IV, which is normed for children aged 2 years 6 months to 7 years, was administered. The BSID-III, a developmental measure widely used, was administrated for the younger children. For children with limited expressive or receptive language skills, a non-verbal assessment of intellectual functioning was deemed more appropriate. The Leiter-3 is a nonverbal standardised test designed to assess IQ regardless of a person’s verbal or motor abilities (Roid et al., 2013). These three measures provide standardized scores with a mean of 100 and a standard deviation of 15. Different studies have been conducted to examine the relation between those three instruments (see for examples Bayley, 2006; Kalkastabakken et al., 2021).
Adaptive behavior
Children’s adaptive behavior was evaluated with the Parent/Primary Caregiver Form (ages 0–5) of the Adaptive Behavior Assessment System (earlier cohorts: ABAS-II, Harrison & Oakland 2003; later cohorts: ABAS-III, Harrison & Oakland 2015). Respondents rate behaviors corresponding to 10 skill areas on a scale from 0 (is not able) to 3 (always/almost always); together, these 10 skills areas combine to form the Global Adaptive Composite (GAC) which was used in the present study. The two forms demonstrated excellent internal consistency (α > 0.90; in the present, study α = 0.92), as well as test-retest reliability and convergent validity (Harrison & Oakland, 2003, 2015).
Challenging behavior and emotional difficulties
Participants obtained a diagnosis within the public system completed the 30-item Social Competence and Behavior Evaluation scale (SCBE-30; LaFrenière & Dumas 1996). This scale is used to assess social competence and difficulties based on behavioral and emotional characteristics observed in children ages 30–78 months. A three-factor structure, corresponding to Social Competence, Anger-Aggression (i.e., externalizing problems), and Anxiety-Withdrawal (i.e., internalizing problems), was observed in four distinct samples (one in Quebec, three in the United States). These three subscale scores and General Adaptation, a global score, were used in analyses (M = 50, SD = 10). These scores have good to excellent internal consistency (α = 0.79-0.91; in the present study, global adaptation α = 0.87) and good interrater reliability and test-retest reliability over a six-month period (LaFrenière & Dumas, 1996).
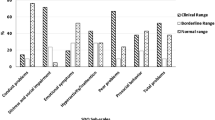
The pilot clinic administered a comparable measure, the preschool version (ages 1.5-5) of parent-reported Child Behavior Checklist (CBCL; Achenbach & Rescorla 2000). Respondents rate items describing various behaviors on a scale ranging from 0 (not true) to 2 (very true or often true). CBCL measure a wide range of potential behavioral and emotional difficulties corresponding to seven syndrome scores: Emotionally reactive, Anxious/Depressed, Somatic complaints, Withdrawn, Sleep problems, Attention problems, and Aggressive behavior. Scores from the first four syndromes can be combined to form a broadband measure of internalizing difficulties whereas the latter two (i.e., excluding Sleep problems) combine into externalizing difficulties. For the present study, the scores for Internalizing Problems and Externalization Problems, as well as the global score, Total Problems, were retained (M = 50, SD = 10). The CBCL has been used in several studies to evaluate behavioral and emotional difficulties in children with ASD (e.g., Hoffmann et la., 2016) Several studies have documented the reliability and validity of these scales (α = 0.90-0.97; in the present study, Total problems α = 0.95; Achenbach & Rescorla 2001; Ivanova et al., 2010; Rescorla et al., 2012, 2014). Moderate correlations between the CBCL and the SCBE-30 have been observed in previous studies, indicating the convergent validity of these two measures of challenging behavior (LaFrenière et al., 1992).
Parenting stress
Third edition of the Parenting Stress Index – Short Form (PSI-SF; Abidin 1995) was completed by parents. Respondents rate a series of 36 statements describing their perceptions of parenting their child on a 5-point Likert scale. The measure yields a Total Stress global score and three subscale scores: Parenting Distress (difficulties related to one’s role as a parent), Parent-Child Dysfunctional Interaction (perception of interactions with their child), and Difficult Child (perceived challenges related to the child’s characteristics or behaviors). Previous studies suggest that these three subscales reflect different experiences of parenting stress and are differentially associated to factors such as the child’s behaviors and functioning (see Mello et al., 2021), and thus suggest that subscale scores should be analyzed separately. Internal consistency for the full scale and the three subscales ranges from good to excellent (α = 0.80-0.91; in the present study α = 0.79-0.92).
Procedure
Participants were recruited from two larger longitudinal projects on families’ experiences leading up to and following their child’s diagnosis and their perceptions of quality of the services they received after this diagnosis (e.g., early intensive behavioral intervention). At a postdiagnostic follow-up meeting, a member of the clinical staff from the participating organizations provided parents with a flyer containing information about the relevant research projects. Parents who consented to participate in the study agreed to be contacted by the research team. Almost all study questionnaires were completed over the course of an individual meeting between a research assistant (a doctoral student in psychology trained in child assessment) and the family. However, for the subsample who was assessed at the pilot clinic, intellectual functioning measures and the ABAS were completed by a psychologist employed at the clinic, who also assisted parents in completing the CBCL. For the Public System sample, the measure of challenging behavior (SCBE) was completed by a staff member (e.g., early intervention therapist) who knew the child well. The Beach FQOL scale, as well as the PSI, were primarily completed by the child’s mother (93.8%).
Statistical analyses
Mean FQOL scores were computed for each subscale and for the complete scale. Subscale scores were compared to each other using paired-samples t-tests with a Bonferroni correction to maintain the familywise Type I error rate at 0.05. Independent-samples t-tests were used to compare mean FQOL levels between the two subsamples (i.e., Pilot Clinic and Public System). Potential contextual, family, and child-related risk and protective factors were entered as predictors in a set of regressions using full-information maximum likelihood estimation, which retains all cases even in the presence of missing data (see Enders 2010). Household income and parent’s education were treated as ordinal variables. Deviation effect coding was used for categorical predictors: the resulting regression coefficients reflect the difference in average FQOL scores between a given category and the overall mean. The measure of intellectual functioning used for each child (WPPSI, BSID-III, or Leiter) and challenging behavior measures (SCBE or CBCL) were standardized to yield a single IQ score and Internalizing, Externalizing, and Total Problems scores, respectively.
Results
Table 3 presents mean FQOL scores for each subscale and overall for both subsamples and for the entire study sample. Most families reported positive or neutral evaluations of their FQOL across all five subscales. On average, families rated their Physical/Material Well-being highest, followed by Disability-related Support, then Parenting; the lowest scores were observed for Emotional Well-being and Family Interaction. In both subsamples, the general ordering of subscale scores was similar, with Physical/Material Well-being receiving higher ratings than other subscale scores. In the Public System sample, FQOL ratings did not differ between the Parenting, Emotional Well-being, and Disability-related Support subscales, but were higher than for Family Interaction. In the Pilot Clinic sample, both Emotional Well-being and Family Interaction were rated lower than other subscales. Most notably, families who were diagnosed at the pilot clinic had significantly higher FQOL, overall and for each subscale, than families diagnosed within the public system.
The results of the regressions predicting FQOL are displayed in Table 4. The organization providing diagnostic services was a significant predictor of FQOL, which indicates that differences between the two samples remain significant when controlling for differences in other predictors (see Tables 1 and 2). Of all child-related factors, only challenging behavior and emotional difficulties were related to FQOL. Specifically, families of children displaying higher levels of internalizing problems reported better FQOL in terms of Family Interaction. However, when considering global scores, families of children with more challenging behavior overall (Total Problems) reported lower FQOL on the Family Interaction and Emotional Well-being dimensions. A few family characteristics were also associated with FQOL. Having more children was associated with lower Parenting and Physical Well-being FQOL. Additionally, when compared the average family, stepfamilies had lower overall Family Interaction and Parenting FQOL. Higher household incomes were predictive of lower FQOL on the Disability-related Support subscale specifically, while speaking a language other than French or English at home was associated with higher FQOL in terms of Family Interaction. Families in which the father was unemployed reported significantly lower FQOL for Parenting, Emotional Well-being, and overall FQOL. Conversely, families in which the mother was unemployed reported higher Parenting FQOL. Finally, parenting stress was associated with FQOL: higher scores on the Parenting Distress and Difficult Child subscales were associated with lower overall, Emotional Well-being, Parenting, and Family Interaction FQOL. Scores on the Parenting Distress subscale were also associated with lower Physical Well-being FQOL.
Discussion
To date, very few empirical studies have documented FQOL in families of children with ASD in general, and fewer still have examined the risk and protective factors for this family-centered outcome or how it manifests during the period of families’ care and service trajectory associated with diagnostic evaluations. Indeed, most research conducted on this topic has tended to group together families of children who differ widely in age and who are at different moments in their care and services trajectory (e.g., diagnostic evaluation, early intervention, primary and secondary school), which obscures important differences in the various stages and transitions of a complex journey. The experiences of families differ vastly depending on where they are on their pathway, for instance in terms of how they perceive their child’s diagnosis and how fluently they can interact with the complex network of services potentially available to them. Importantly, how families perceive the early stages of their care and service trajectory, that is, when they suspect their child has ASD, may shape the remainder of this trajectory and their lives as a family (Boshoff et al., 2019; Brewer, 2018). A better understanding of FQOL at this important juncture could better inform the types of services and supports to provide to assist families. With this goal in mind, the present study contributed to our understanding of FQOL of families of children recently diagnosed with ASD by identifying differences attributable to service delivery contexts, vulnerable domains of FQOL, and specific risk and protective factors for family functioning during this period. The primary goal of the study was to evaluate if a family-centered approach to diagnostic evaluation, namely the logic model adopted by the pilot clinic to address previously documented sources of parental dissatisfaction, could address challenges to FQOL during a critical period of families’ care and service trajectories.
First, the present study emphasized the role that service provision modalities and contexts, and, by extension, family supports, can play on FQOL. Considerable challenges to accessing diagnostic evaluation and related services have been observed within the public health and social services system in several countries (Austin et al., 2016; Boshoff et al., 2019; Crane et al., 2016; Lappé et al., 2018; Penner et al., 2015; Rivard et al., 2019). In the present study, a pilot clinic was implemented in response to these observations and sought to integrate features known to be valued by families such as access to information, regular contact and follow-up with a knowledgeable staff member, and a range of support programs. Overall, results indicated that the clinical model proposed by the pilot clinic could serve as a protective factor for FQOL relative to typical experiences within the existing network of public health and social services. This was the case even when accounting for differences in child- or family-related characteristics between the two samples.
Second, this study helped to identify areas of family functioning that may require additional support during the diagnostic period. This stage of families’ care and service trajectory places several adjustment demands on parents, who must gather information about available services and their effectiveness while also responding to the challenges posed by their child’s symptoms or behavioral difficulties. In addition to adapting to this new reality, parents may also experience difficult emotions (e.g., Corcoran et al., 2015; McCrimmon & Gray, 2020; Rivard et al., 2019). These observations from earlier studies were echoed in the results of the present study, where Emotional Well-being and Family Interaction were the two lowest-rated dimensions of FQOL. These findings underscore the importance of providing psychological support to parents at this very critical phase of a family’s care and service trajectory. There is evidence that parents’ mental health (e.g., stress) and socio-emotional difficulties in their children may have a bidirectional influence over time (e.g., Dieleman et al., 2017; Rodriguez et al., 2019; Zaidman-Zait et al., 2014). Thus, promoting parental adjustment may also be beneficial to children and, by extension, the entire family system.
Third, the present study shed light on risk and protective factors for FQOL associated family and child characteristics, irrespective of service provision context. In contrast with other studies, autism severity was not associated with reduced FQOL in parents (Dardas & Ahmad, 2014; Pozo et al., 2014; Schlebusch et al., 2017; Vasilopoulou & Nisbet, 2016; Wang et al., 2018). This could be specific to age group and the specific measure of autism symptoms (i.e., CARS) included in the present study. Similarly, neither IQ nor adaptive behavior were predictive of FQOL, which is consistent with an observation by Vaz et al., (2021) that caregivers of children with ASD with and without co-occurring ID did not differ in their general quality of life (but see Gardiner & Iarocci 2015; Mello et al., 2019). However, complex associations between challenging behavior and emotional difficulties on the one hand, and FQOL on the other hand, were observed. Overall, behavioral problems were associated with lower scores on the Family Interaction and Emotional Well-being domains of FQOL (see also Hall & Graff 2012; McStay et al., 2014; Pozo et al., 2014). These findings indicate that, in addition to direct psychological support, parents may benefit from coaching programs that can better equip them to respond to challenging behaviors as early as the diagnostic phase and the subsequent waiting period for early intervention. It is worth noting that internalized difficulties (e.g., being shy or anxious) were paradoxically associated with higher FQOL in one of the same domain of Family Interaction. It may be these problems are less disruptive to family functioning than externalized behaviors, which are also more noticeable by others outside the family and thus more likely to result in social isolation and decreased social support. Furthermore, externalized behavior problems also have more negative repercussions on siblings (see Rochefort et al., 2022; Rixon et al., 2021). Nevertheless, supports provided to children and families during this period of family life should also help address internalizing behaviors.
Some family characteristics were also linked to FQOL. For instance, having more children was associated with lower Parenting FQOL (see Mello et al., 2019). This observation makes sense given that this dimension of FQOL reflects adults’ perception of having the time and resources to care for children. Furthermore, having a child with a neurodevelopmental disorder has repercussions for the child’s siblings (Corcoran et al., 2015; Walton, 2016). Compared to other types of families, stepfamilies had lower overall FQOL and in terms of Family Interaction and Parenting. However, the data gathered in this study do not include whether parents remarried before or after the birth of the child with a neurodevelopmental disorder. The latter case may present additional difficulties for the stepparent or in terms of shared custody. Different parent-child relationships or parenting styles in stepfamilies could also contribute to explain those differences.
Surprisingly, higher household incomes were associated with lower FQOL on the Disability-related Support dimension specifically, which is inconsistent with the literature (e.g., Dardas & Ahmad 2014; Lu et al., 2015; Schlebusch et al., 2017). In the present study, we also tested the possibility of non-linear associations between income and this dimension of FQOL, however results were consistent only with a linear, negative association between these two variables. Schlebusch et al., (2017) noted that FQOL was connected to parents’ perception of their financial resources, which extends beyond annual household income. It should be noted that all families in the present study were entitled to a range of free services (e.g., assessment, intervention) in relation to neurodevelopmental disorders, however these services present limitations such as extensive waiting lists. Lower-income families cannot bypass these difficulties by paying out of pocket for private services: when they finally access free, public services, they may appreciate these to a greater extent than families who could potentially avail themselves of other options (Rivard et al., 2021). Additionally, to the extent that some grants and subsidies are made available to families on the basis of need (i.e., income-based allocation), higher-income households may experience dissatisfaction at not receiving some forms of assistance available to other families (unless they elect to pay for these within the private sector).
Families in which the father was unemployed reported lower FQOL overall and in the Parenting and Emotional Well-being domains (see also Kuru & Piyal 2018; Schlebusch et al., 2017; Vasilopoulou & Nisbet, 2016). In contrast, families in which the mother was unemployed reported higher Parenting FQOL. Compared to mothers who work, those who do not may perceive that they have more time and energy to care for their child. Relatedly, parenting stress, specifically in the Parenting Distress and Difficult Child domains, was associated with lower FQOL. This was observed in other studies (e.g., Dardas & Ahmad 2014; Hsiao et al., 2017). Contrary to the extant literature, which suggests an association between immigration status or language and quality of diagnostic services (Zuckerman et al., 2017), in the present study parents’ country of origin and language spoken at home were not linked to lower FQOL. In fact, speaking a language other than English or French at home was linked to higher FQOL on the Family Interaction subscale. A possible explanation for this finding is that preserving the family’s mother tongue from a foreign country (whether or not they are first-generation immigrants) could be an indicator of a family culture that focuses on strong family ties and engagement with, as well as support from, one’s ethnocultural community. This may also be due to the allocation of public resources (e.g., subsidies and increased intervention support at home) to families who present certain risk factors (e.g. allophone population).
Limitations and future directions
One of the limitations of the present study stems from the fact that participants were not randomly assigned to receive diagnostic evaluation from either the public system or the pilot clinic. Data for the two samples were collected at different points in time, i.e., before and after the implementation of the pilot clinic in 2015, which could have led to potential time or cohort effects. To the extent possible, the present study adopted analytical methods that controlled for several characteristics of children and families that differed between the two samples. However, in the absence of random assignment, parents and children within the two groups may differ ways that were not directly assessed in the context of this study and thus could not be accounted for in the interpretation of results. Future studies seeking to test family-centered service delivery models should adopt random allocation of participants when feasible. These two different clinical contexts used different assessments of challenging behavior and emotional difficulties, as well as different respondents (i.e., either a parent or a staff member) to complete these assessments. An additional limitation is that standardized measures of intellectual functioning were selected on a case-by-case basis to account for children’s age and development (including verbal ability). It would not have been realistic to ask the diagnostic assessment teams in the two clinical contexts to modify their professional practices for the purpose of this study. However, various studies have previously documented the convergence of these different instruments, such that scores obtained with one or another instrument of the same construct, used in similar situations, can be understood to communicate similar information about the child’s developmental and clinical profile. However, some authors have raised concerns about the comparability of IQ scores obtained with different tests (Bünger et al., 2021). One final limitation to consider is that, because diagnostic evaluations took place in English or French only, all participants in the present study were fluent in one or both languages. The results of the present study cannot be generalized to other linguistic populations.
Conclusions
The findings of the present study underscore the importance of providing diagnostic services based on a family-centered model that gives direct support to families during the diagnostic period, beginning with the first suspicions of atypical development in their child and ending with the provision of appropriate interventions. Indeed, this is a stage in family life where parents experience a number of stressors and typically receive few formal supports. In addition to diagnostic evaluation services provided according to best practices, the findings of the present study suggest several pathways to better supporting families. Promising avenues include mental health support to parents as early as the diagnostic evaluation phase, coaching interventions that assist parents in managing challenging behaviors in their child, and related supports for families presenting other risk factors (e.g., respite care for larger families or vocational counseling for parents seeking employment).
References
Abidin, R. R. (1995). Parenting Stress Index: Manual (3rd ed.). Psychological Assessment Resources
Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA preschool forms and profiles. University of Vermont, Research Center for Children, Youth, & Families
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles. University of Vermont, Research Center for Children, Youth, & Families
Albers, C. A., & Grieve, A. J. (2007). Review of Bayley Scales of Infant and Toddler Development-Third Edition. Journal of Psychoeducational Assessment, 25(2), 180–190. https://doi.org/10.1177/0734282906297199
Austin, J., Manning-Courtney, P., Johnson, M. L., Weber, R., Johnson, H., Murray, D., Ratliff-Schaub, K., Tadlock, A. M., & Murray, M. (2016). Improving access to care at autism treatment centers: A system analysis approach. Pediatrics, 137(Supplement 2), S149–S157. https://doi.org/10.1542/peds.2015-2851M
Bishop-Fitzpatrick, L., & Kind, A. J. H. (2017). A scoping review of health disparities in autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(11), 3380–3391. https://doi.org/10.1007/s10803-017-3251-9
Boshoff, K., Gibbs, D., Phillips, R. L., Wiles, L., & Porter, L. (2019). A meta-synthesis of how parents of children with autism describe their experience of advocating for their children during the process of diagnosis. Health & Social Care in the Community, 27(4), e143–e157. https://doi.org/10.1111/hsc.12691
Brewer, A. (2018). “We were on our own”: Mothers’ experiences navigating the fragmented system of professional care for autism. Social Science & Medicine, 215, 61–68. https://doi.org/10.1016/j.socscimed.2018.08.039
Bünger, A., Grieder, S., Schweizer, F., & Grob, A. (2021). The comparability of intelligence test results: Group- and individual-level comparisons of seven intelligence tests. Journal of School Psychology, 88, 101–117. https://doi.org/10.1016/j.jsp.2021.09.002
Chamak, B., Bonniau, B., Oudaya, L., & Ehrenberg, A. (2011). The autism diagnostic experiences of French parents. Autism: The International Journal of Research and Practice, 15(1), 83–97. https://doi.org/10.1177/1362361309354756
Collège des médecins du Québec et Ordre des psychologues du Québec (OPQ) (2012). Les troubles du spectre de l’autisme, l’évaluation clinique, lignes directrices.https://www.ordrepsy.qc.ca/documents/26707/63191/spectre-de-lautism)
Corcoran, J., Berry, A., & Hill, S. (2015). The lived experience of US parents of children with autism spectrum disorders: A systematic review and meta-synthesis. Journal of Intellectual Disabilities, 19(4), 356–366. https://doi.org/10.1177/1744629515577876
Crane, L., Chester, J. W., Goddard, L., Henry, L. A., & Hill, E. (2016). Experiences of autism diagnosis: A survey of over 1000 parents in the United Kingdom. Autism, 20(2), 153–162. https://doi.org/10.1177/1362361315573636
Dardas, L. A., & Ahmad, M. M. (2014). Quality of life among parents of children with autistic disorder: A sample from the Arab world. Research in Developmental Disabilities, 35(2), 278–287. https://doi.org/10.1016/j.ridd.2013.10.029
DePape, A. M., & Lindsay, S. (2015). Parents’ experiences of caring for a child with autism spectrum disorder. Qualitative Health Research, 25(4), 569–583. https://doi.org/10.1177/1049732314552455
Dieleman, L. M., De Pauw, S. S., Soenens, B., Beyers, W., & Prinzie, P. (2017). Examining bidirectional relationships between parenting and child maladjustment in youth with autism spectrum disorder: A 9-year longitudinal study. Development and Psychopathology, 29(4), 1199–1213
Eapen, V., & Guan, J. (2016). Parental Quality of Life in Autism Spectrum Disorder: Current Status and Future Directions. Acta Psychopathologica, 2(1), https://doi.org/10.4172/2469-6676.100031
Emerson, N., Morrell, H., & Neece, C. (2016). Predictors of Age of Diagnosis for Children with Autism Spectrum Disorder: The Role of a Consistent Source of Medical Care, Race, and Condition Severity. Journal of Autism and Developmental Disorders, 46. https://doi.org/10.1007/s10803-015-2555-x
Enders, C. K. (2010). Applied missing data analysis. Guilford Press
Fountain, C., King, M. D., & Bearman, P. S. (2011). Age of diagnosis for autism: Individual and community factors across 10 birth cohorts. Journal of Epidemiology & Community Health, 65(6), 503–510. https://doi.org/10.1136/jech.2009.104588
Gardiner, E., & Iarocci, G. (2015). Family quality of life and ASD: The role of child adaptive functioning and behavior problems. Autism Research, 8. https://doi.org/10.1002/aur.1442
Gould, E. R., Tarbox, J., & Coyne, L. (2018). Evaluating the effects of Acceptance and Commitment Training on the overt behavior of parents of children with autism. Journal of Contextual Behavioral Science, 7, 81–88. https://doi.org/10.1016/j.jcbs.2017.06.003
Hall, H. R., & Graff, J. C. (2012). Maladaptive behaviors of children with autism: Parent support, stress, and coping. Issues in Comprehensive Pediatric Nursing, 35(3–4), 194–214. https://doi.org/10.3109/01460862.2012.734210
Harrison, P. L., & Oakland, T. (2003). Adaptive Behavior Assessment System-Second Edition. The Psychological Corporation. https://doi.org/10.1016/B978-0-12-373586-7.X0001-X
Harrison, P. L., & Oakland, T. (2015). Adaptive Behavior Assessment System – Third Edition. Western Psychological Services
Hennel, S., Coates, C., Symeonides, C., Gulenc, A., Smith, L., Price, A. M., & Hiscock, H. (2016). Diagnosing autism: Contemporaneous surveys of parent needs and paediatric practice. Journal of Paediatrics and Child Health, 52(5), 506–511
Hoffmann, W., Weber, L., König, U., Becker, K., & Kamp-Becker, I. (2016). The role of the CBCL in the assessment of autism spectrum disorders: An evaluation of symptom profiles and screening characteristics. Research in Autism Spectrum Disorders, 27, 44–53. https://doi.org/10.1016/j.rasd.2016.04.002
Hoffman, L., Marquis, J., Poston, D., Summers, J. A., & Turnbull, A. (2006). Assessing family outcomes: Psychometric evaluation of the beach center family quality of life scale. Journal of Marriage and Family, 68(4), 1069–1083. https://doi.org/10.1111/j.1741-3737.2006.00314.x
Hsiao, Y. J., Higgins, K., Pierce, T., Whitby, P. J. S., & Tandy, R. D. (2017). Parental stress, family quality of life, and family-teacher partnerships: Families of children with autism spectrum disorder. Research in Developmental Disabilities, 70, 152–162. https://doi.org/10.1016/j.ridd.2017.08.013
Ivanova, M. Y., Achenbach, T. M., Rescorla, L. A., Harder, V. S., Ang, R. P., Bilenberg, N., Bjarnadottir, G., Capron, C., De Pauw, S. S. W., Dias, P., Dobrean, A., Doepfner, M., Duyme, M., Eapen, V., Erol, N., Esmaeili, E. M., Ezpeleta, L., Frigerio, A., Gonçalves, M. M., & Verhulst, F. C. (2010). Preschool psychopathology reported by parents in 23 societies: Testing the seven-syndrome model of the child behavior checklist for ages 1.5-5. Journal of the American Academy of Child and Adolescent Psychiatry, 49(12), 1215–1224. https://doi.org/10.1016/j.jaac.2010.08.019
Jashar, D. T., Fein, D., Berry, L. N., Burke, J. D., Miller, L. E., Barton, M. L., & Dumont-Mathieu, T. (2019). Parental perceptions of a comprehensive diagnostic evaluation for toddlers at risk for autism spectrum disorder. Journal of Autism and Developmental Disorders, 49(5), 1763–1777. https://doi.org/10.1007/s10803-018-3851-z
Kranzler, J. H., & Floyd, R. G. (2013). Assessing intelligence in children and adolescents: A practical guide. Guilford Press
Kuru, N., & Piyal, B. (2018). Perceived social support and quality of life of parents of children with autism. Nigerian Journal of Clinical Practice, 21(9), 1182–1189. https://doi.org/10.4103/njcp.njcp_13_18
LaFrenière, P. J., & Dumas, J. E. (1996). Social competence and behavior evaluation in children ages 3 to 6 years: The short form (SCBE-30). Psychological Assessment, 8(4), 369377. https://doi.org/10.1037/1040-3590.8.4.369
LaFrenière, P. J., Dumas, J. E., Capuano, F., & Dubeau, D. (1992). Development and validation of the Preschool Socioaffective Profile. Psychological Assessment, 4(4), 442–450. https://doi.org/10.1037/1040-3590.4.4.442
Lappé, M., Lau, L., Dudovitz, R. N., Nelson, B. B., Karp, E. A., & Kuo, A. A. (2018). The diagnostic odyssey of autism spectrum disorder. Pediatrics, 141(Supplement 4), S272–S279. https://doi.org/10.1542/peds.2016-4300C
Legg, H., & Tickle, A. (2019). UK parents’ experiences of their child receiving a diagnosis of autism spectrum disorder: A systematic review of the qualitative evidence. Autism, 23(8), 1897–1910. https://doi.org/10.1177/1362361319841488
Lu, M., Yang, G., Skora, E., Wang, G., Cai, Y., Sun, Q., & Li, W. (2015). Self-esteem, social support, and life satisfaction in Chinese parents of children with autism spectrum disorder. Research in Autism Spectrum Disorders, 17, 70–77. https://doi.org/10.1016/j.rasd.2015.05.003
Magaña, S., Parish, S. L., & Son, E. (2016). Functional severity and Latino ethnicity in specialty services for children with autism spectrum disorder. Journal of Intellectual Disability Research: JIDR, 60(5), 424–434. https://doi.org/10.1111/jir.12293
Makino, A., Hartman, L., King, G., Wong, P. Y., & Penner, M. (2021). Parent experiences of autism spectrum disorder diagnosis: A scoping review. Review Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s40489-021-00237-y
Mansell, W., & Morris, K. (2004). A survey of parents’ reactions to the diagnosis of an autistic spectrum disorder by a local service: Access to information and use of services. Autism, 8(4), 387–407
Mazurek, M. O., Handen, B. L., Wodka, E. L., Nowinski, L., Butter, E., & Engelhardt, C. R. (2014). Age at first autism spectrum disorder diagnosis: The role of birth cohort, demographic factors, and clinical features. Journal of Developmental & Behavioral Pediatrics, 35(9), 561–569. https://doi.org/10.1097/DBP.0000000000000097
McCrimmon, A. W., & Gray, S. M. (2020). A systematic review of factors relating to parental satisfaction with the diagnostic process for autism spectrum disorder. Review Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s40489-020-00224-9
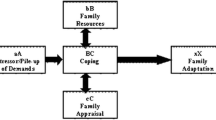
McStay, R. L., Trembath, D., & Dissanayake, C. (2014). Stress and family quality of life in parents of children with autism spectrum disorder: Parent gender and the double ABCX model. Journal of Autism and Developmental Disorders, 44(12), 3101–3118. https://doi.org/10.1007/s10803-014-2178-7
Mello, C., Rivard, M., Morin, D., Patel, S., & Morin, M. (2021). Symptom severity, internalized and externalized behavioral and emotional problems: Links with parenting stress in mothers of children recently diagnosed with autism. Journal of Autism and Developmental Disorders, 1–14. https://doi.org/10.1007/s10803-021-05131-4
Mello, C., Rivard, M., Terroux, A., & Mercier, C. (2019). Quality of life in families of young children with autism spectrum disorder. American Journal on Intellectual and Developmental Disabilities, 124(6), 535–548. https://doi.org/10.1352/1944-7558-124.6.535
Moh, T. A., & Magiati, I. (2012). Factors associated with parental stress and satisfaction during the process of diagnosis of children with autism spectrum disorders. Research in Autism Spectrum Disorders, 6(1), 293–303. https://doi.org/10.1016/j.rasd.2011.05.011
Morin, M., Abouzeid, N., Rivard, M., Morin, D., Bolduc, M., Blanchard-Beauchemin, M., & et Mercier, C. (2020). Guide d’implantation d’un programme d’évaluation diagnostique du trouble du spectre de l’autisme, de la déficience intellectuelle et du retard global de développement auprès d’enfants de 0 à 5 ans. Laboratoire Épaulard, Département de psychologie, Université du Québec à Montréal. https://12a37703-c89e-45e0-b8ba-09b35c1f987d.filesusr.com/ugd/ec40b5_f3d5151eb2274f19bf57e60aee33e228.pdf
Ooi, K. L., Ong, Y. S., Jacob, S. A., & Khan, T. M. (2016). A meta-synthesis on parenting a child with autism. Neuropsychiatric Disease and Treatment. https://doi.org/10.2147/NDT.S100634
Osborne, L. A., & Reed, P. (2008). Parents’ perceptions of communication with professionals during the diagnosis of autism. Autism, 12(3), 309–324. https://doi.org/10.1177/1362361307089517
Penner, M., Rayar, M., Bashir, N., Roberts, S. W., Hancock-Howard, R. L., & Coyte, P. C. (2015). Cost-effectiveness analysis comparing pre-diagnosis autism spectrum disorder (ASD)-targeted intervention with Ontario’s autism intervention program. Journal of Autism and Developmental Disorders, 45(9), 2833–2847. https://doi.org/10.1007/s10803-015-2447-0
Pozo, P., Sarriá, E., & Brioso, A. (2014). Family quality of life and psychological well-being in parents of children with autism spectrum disorders: A double ABCX model. Journal of Intellectual Disability Research: JIDR, 58(5), 442–458. https://doi.org/10.1111/jir.12042
Reed, P., & Osborne, L. A. (2012). Diagnostic practice and its impacts on parental health and child behaviour problems in autism spectrum disorders. Archives of Disease in Childhood, 97(10), 927–931. https://doi.org/10.1136/archdischild-2012-301761
Renty, J., & Roeyers, H. (2005). Students with autism spectrum disorder in special and general education schools in Flanders. The British Journal of Development Disabilities, 51(100), 27–39. https://doi.org/10.1179/096979505799103795
Rescorla, L. A., Achenbach, T. M., Ivanova, M. Y., Bilenberg, N., Bjarnadottir, G., Denner, S., Dias, P., Dobrean, A., Döpfner, M., Frigerio, A., Gonçalves, M., Guðmundsson, H., Jusiene, R., Kristensen, S., Lecannelier, F., Leung, P. W. L., Liu, J., Löbel, S. P., Machado, B. C., & Verhulst, F. C. (2012). Behavioral/emotional problems of preschoolers: Caregiver/teacher reports from 15 societies. Journal of Emotional and Behavioral Disorders, 20(2), 68–81. https://doi.org/10.1177/1063426611434158
Rescorla, L. A., Bochicchio, L., Achenbach, T. M., Ivanova, M. Y., Almqvist, F., Begovac, I., Bilenberg, N., Bird, H., Dobrean, A., Erol, N., Fombonne, E., Fonseca, A., Frigerio, A., Fung, D. S. S., Lambert, M. C., Leung, P. W. L., Liu, X., Marković, I., Markovic, J., & Verhulst, F. C. (2014). Parent-teacher agreement on children’s problems in 21 societies. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology American Psychological Association Division, 53(4), 627–642. https://doi.org/10.1080/15374416.2014.900719. 43
Rivard, M., Lépine, A., Mercier, C., & Morin, M. (2015). Quality determinants of services for parents of young children with autism spectrum disorders. Journal of Child and Family Studies, 24(8), 2388–2397. https://doi.org/10.1007/s10826-014-0041-2
Rivard, M., Mercier, C., Mestari, Z., Terroux, A., Mello, C., & Bégin, J. (2017). Psychometric properties of the Beach Center Family Quality of Life in French-speaking families with a preschool-aged child diagnosed with autism spectrum disorder. American Journal on Intellectual and Developmental Disabilities, 122(5), 439–452. https://doi.org/10.1352/1944-7558-122.5.439
Rivard, M., Millau, M., Magnan, C., Mello, C., & Boulé, M. (2019). Snakes and ladders: Barriers and facilitators experienced by immigrant families when accessing an autism spectrum disorder diagnosis. Journal of Developmental and Physical Disabilities, 31(4), 519–539. https://doi.org/10.1007/s10882-018-9653-6
Rivard, M., Mello, C., Mercier, C., Lefebvre, C., Millau, M., Morin, M., Morin, D., Abouzeid, N., & Chatenoud, C. (2020a). Development of a questionnaire to assess the quality of service trajectories in autism spectrum disorder from families’ perspective. Journal of Applied Research in Intellectual Disabilities, 33(6), 1500–1511. https://doi.org/10.1111/jar.12777
Rivard, M., Millau, M., Mello, C., Clément, C., Mejia-Cardenas, C., Boulé, M., & Magnan, C. (2020b). Immigrant families of children with autism disorder’s perceptions of early intensive behavioral intervention services. Journal of Developmental and Physical Disabilities, 1–19. https://doi.org/10.1007/s10882-020-09764-8
Rivard, M., Patrick, C., Mello, C., Morin, D., & Morin, M. (2021). The diagnostic trajectory in autism and intellectual disability in Quebec: Pathways and parents’ perspective. BMC Pediatrics, 21(1), 393. https://doi.org/10.1186/s12887-021-02864-0
Rivard, M., Terroux, A., Parent-Boursier, C., & Mercier, C. (2014). Determinants of stress in parents of children with autism spectrum disorders. Journal of Autism & Developmental Disorders, 44(7), 1609–1620. https://doi.org/10.1007/s10803-013-2028-z
Rochefort, C., Paradis, A., Rivard, M., & Dewar, M. (2022, in revision). Siblings of Individuals with Developmental Disabilities: A Scoping Review Using Trauma Theory
Rodriguez, G., Hartley, S. L., & Bolt, D. (2019). Transactional relations between parenting stress and child autism symptoms and behavior problems. Journal of Autism and Developmental Disorders, 49(5), 1887–1898. https://doi.org/10.1007/s10803-018-3845-x
Roid, G. H., Miller, L., Pomplun, M., & Koch, C. (2013). Leiter International Performance Scale- Third Edition. Western Psychological Services
Roth, B. M., Kralovic, S., Roizen, N. J., Spannagel, S. C., Minich, N., & Knapp, J. (2016). Impact of autism navigator on access to services. Journal of Developmental & Behavioral Pediatrics, 37(3), 188–195. https://doi.org/10.1097/DBP.0000000000000261
Schlebusch, L., Dada, S., & Samuels, A. E. (2017). Family quality of life of South African families raising children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(7), 1966–1977. https://doi.org/10.1007/s10803-017-3102-8
Shepherd, C. A., & Waddell, C. (2015). A qualitative study of autism policy in Canada: Seeking consensus on children’s services. Journal of Autism and Developmental Disorders, 45(11), 3550–3564. https://doi.org/10.1007/s10803-015-2502-x
Soares, M. A., & McCrimmon, A. W. (2013). Test review: Wechsler Preschool and Primary Scale of Intelligence, Fourth Edition: Canadian. Canadian Journal of School Psychology, 28(4), 345–351. https://doi.org/10.1177/0829573513497343
Stahmer, A. C., Vejnoska, S., Iadarola, S., Straiton, D., Segovia, F. R., Luelmo, P., Morgan, E. H., Lee, H. S., Javed, A., Bronstein, B., Hochheimer, S., Cho, E., Aranbarri, A., Mandell, D., Hassrick, E. M., Smith, T., & Kasari, C. (2019). Caregiver voices: Cross-cultural input on improving access to autism services. Journal of Racial and Ethnic Health Disparities, 6(4), 752–773. https://doi.org/10.1007/s40615-019-00575-y
Vasilopoulou, E., & Nisbet, J. (2016). The quality of life of parents of children with autism spectrum disorder: A systematic review. Research in Autism Spectrum Disorders, 23, 36–49
Vaz, S., Thomson, A., Cuomo, B., Falkmer, T., Chamberlain, A., & Black, M. H. (2021). Co-occurring intellectual disability and autism: Associations with stress, coping, time use, and quality of life in caregivers. Research in Autism Spectrum Disorders, 84, 101765
Walton, K. M. (2016). Risk factors for behavioral and emotional difficulties in siblings of children with autism spectrum disorder. American Journal on Intellectual and Developmental Disabilities, 121(6), 533–549
Wang, Y., Xiao, L., Chen, R. S., Chen, C., Xun, G. L., Lu, X. Z., Shen, Y. D., Wu, R. R., Xia, K., & Zhao, J. P. (2018). Social impairment of children with autism spectrum disorder affects parental quality of life in different ways. Psychiatry Research, 266, 168–174. https://doi.org/10.1016/j.psychres.2018.05.057
Wechsler, D. (2012). Wechsler Preschool and Primary Scale of Intelligence (4th ed.). Pearson
Whittingham, K., & Coyne, L. (2019). Acceptance and commitment therapy: The clinician’s guide for supporting parents. Academic Press
Yi, H., Siu, Q. K. Y., Ngan, O. M. Y., & Chan, D. F. Y. (2020). Parents’ experiences of screening, diagnosis, and intervention for children with autism spectrum disorder. American Journal of Orthopsychiatry, 90(3), 297–311. https://doi.org/10.1037/ort0000433
Zaidman-Zait, A., Mirenda, P., Duku, E., Szatmari, P., Georgiades, S., Volden, J., Zwaigenbaum, L., Vaillancourt, T., Bryson, S., & Smith, I. (2014). Examination of bidirectional relationships between parent stress and two types of problem behavior in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(8), 1908–1917
Zarafshan, H., Mohammadi, M. R., Abolhassani, F., Motevalian, S. A., Sepasi, N., & Sharifi, V. (2019). Current status of health and social services for children with autism in Iran: Parents’ perspectives. Iranian Journal of Psychiatry, 14(1), 76–83
Zeng, S., Hu, X., Zhao, H., & Stone-MacDonald, A. K. (2020). Examining the relationships of parental stress, family support and family quality of life: A structural equation modeling approach. Research in Developmental Disabilities, 96, 103523. https://doi.org/10.1016/j.ridd.2019.103523
Zuckerman, K. E., Lindly, O. J., Reyes, N. M., Chavez, A. E., Macias, K., Smith, K. N., & Reynolds, A. (2017). Disparities in diagnosis and treatment of autism in Latino and non-Latino white families. Pediatrics, 139(5), https://doi.org/10.1542/peds.2016-3010
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
conflicts of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rivard, M., Morin, D., Coulombe, P. et al. The Diagnostic Period for Autism: Risk and Protective Factors for Family Quality of Life in Early Childhood. J Autism Dev Disord 53, 3755–3769 (2023). https://doi.org/10.1007/s10803-022-05686-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05686-w