Abstract
Food consumption in children with ASD, subclinical ASD and with typical development (TD), and their adequacy to dietary recommendations was studied. A school population sample of 77 children with ASD, 40 with subclinical ASD, and 333 with TD participated. Compared to children with TD, pre-schoolers with ASD consumed fewer raw vegetables and less fish and eggs, while primary school children consumed fewer legumes, raw vegetables, citrus fruits, cheese/yogurt and olive oil, and more meat. All groups consumed an excess of sugar but those with ASD consumed even a greater amount than their peers. The higher prevalence of obesity found in primary school children with ASD may be the consequence of a less healthy eating pattern sustained over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism spectrum disorder (ASD) is a neurodevelopmental disability whose prevalence has increased in recent decades. Now affecting 1 in 54 children, ASD is more common in boys than in girls (Maenner et al. 2020). In addition, subclinical ASD affects 2.6% of the school population (Morales-Hidalgo et al. 2017) and 14.5% of the population with risk factors for developmental alterations (very preterm children) (Vermeirsch et al. 2020). Some of the main characteristics of ASD, such as insistence on sameness, inflexible adherence to routines or hyper-or-hypo reactivity to sensory input, may affect subjects’ daily functioning and could contribute to the development of eating disorders. Problems such as food selectivity, food refusal, picky eating and/or mealtime behaviour difficulties are reported in ASD populations with a wide range of impact, from 13 to 80% (Cermak et al. 2010; Marí-Bauset et al. 2014; Nadon et al. 2011a, 2011b; Schreck et al. 2004). These atypical eating behaviours may be related to sensory sensitivity about the type, temperature, texture or colour of food, and affect their consumption and the child’s nutritional intake (Bandini et al. 2010; Castro et al. 2016; Curtin et al. 2015; Johnson et al. 2014; Marí-Bauset et al. 2014; Ranjan and Nasser, 2015; Zimmer et al. 2012).
Other comorbid conditions can also affect the consumption and nutritional intake of the ASD population. Gastrointestinal (GI) symptoms, reported generally as abdominal pain, constipation, and diarrhoea, have been well documented in children with ASD, affecting from 49.3 to 82% of the population. Some authors indicate that children with ASD and GI concerns are at a higher risk of developing eating behaviour problems than those without them (Leader et al. 2020; Mannion et al. 2013; McElhanon 2014; Santocchi et al. 2016). Moreover, many disorders, including attention-deficit/hyperactivity disorder (ADHD), intellectual disabilities and emotional disorders, coexist with ASD, which constitute other factors that may contribute to these eating patterns (Barnhill et al. 2017; Salazar et al. 2015). The combination of all these factors may affect the diet quality, growth and optimal development of children with ASD (Bandini et al. 2017; Barnhill et al. 2017; Matheson and Douglas 2017).
Some authors have studied the consumption of children with ASD compared to those with typical development. In general, they found stronger preferences for energy-dense foods like snacks, sweets, sugary beverages and juice in children with ASD (Berding and Donovan 2018; Evans et al. 2012; Wallace et al. 2020). In contrast, children with ASD tend to eat less from food groups like vegetables (Bandini et al. 2010; Emond et al. 2010; Evans et al. 2012; Ranjan and Nasser 2015), fruit (Chistol et al. 2018; Evans et al. 2012; Schreck et al. 2004; Smith et al. 2020) and dairy products (Herndon et al. 2009; Marí-Bauset et al. 2017; Neumeyer et al. 2018) than children with TD. However, a previous study conducted in Spain found that children with ASD followed a traditional Mediterranean diet and ate more legumes and vegetables than children with TD (Marí-Bauset et al. 2017). So, the studies undertaken to date do not coincide in all their observations, and although some studies have reported that the consumption of vegetables, fruit and dairy products among children with ASD is below that recommended (Al-Thbiany 2017; Diolordi et al. 2014; Webber et al. 2018), other research has not found this deficiency (Evans et al. 2012; Herndon et al. 2009), or has even found contradictory results, as in the case of the protein food group (Herndon et al. 2009; Schreck et al. 2004).
Given that the inadequate consumption of some foods may affect optimal growth in children (Esteban-Figuerola et al. 2019; Marí-Bauset et al. 2017; Sharp et al. 2013), we believe it is important to analyse the degree of dietary imbalance compared to children without ASD and in relation to recommended daily intake in order to assess the degree of risk associated with their eating behaviours.
Therefore, the aim of this study was to investigate the food consumption of a school population with ASD (clinical and subclinical diagnosis) compared to children with TD, and to compare their food consumption to the dietary guidelines. We hypothesise that: (1) the consumption of vegetables, fruit and dairy products will be lower, and the consumption of sweet foods higher, among children with ASD than among those with TD. (2) Children with subclinical ASD will have an eating pattern more similar to those with ASD than to those with TD. (3) We will find the same food consumption characteristics among children with ASD of both preschool and primary school age. (4) For some food groups, like fruit and vegetables, children with ASD will consume less than that recommended in the dietary guidelines.
Material and Methods
Study Design and Sample
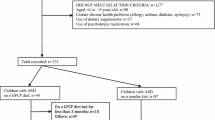
The participants were recruited from the Neurodevelopmental Disorders Epidemiological Research Project (EPINED), which aimed to determine the prevalence of ASD and ADHD (DSM-5 criteria) in a representative school population of preschool and primary school children in the province of Tarragona (Catalonia, Spain). In the first phase of the project, parents and teachers responded to screening tests to detect children at risk of both ASD and ADHD. In the second phase, children identified as at risk for ASD and/or ADHD and a control group without any risk were individually assessed to confirm the diagnoses. From the primary school population of 6894 children in the two age groups (3374 aged 3–6 and 3520 aged 10–12), parents of 3,713 children (895 pre-school age [49.9% boys] and 894 primary school age [46.6% boys]) signed the informed consent form and completed the questionnaires. In the second phase, 760 children were assessed individually, of which 61 were diagnosed with ASD, 43 with subclinical ASD, 259 with ADHD, and 397 had neither ASD nor ADHD. In addition to this sample, 22 children with ASD from clinical services were invited to participate and included in our study (mean age 9.29 years ± 3.7 SD).
The present study excluded children with neurodevelopmental problems other than ASD, those whose parents did not complete the food questionnaires and children who exceeded the age ranges. This resulted in a total sample of 451 participants (199 pre-school children and 251 primary school children), of whom 77 were diagnosed with ASD, 40 were classified as subclinical ASD, and 333 children were classified as controls or children with TD, including children without ASD, subclinical ASD or any other neurodevelopmental disorder (ADHD, intellectual disability).
Socio-demographic information was reported by the parents. Socio-economic status was estimated using the Hollingshead Index (Hollingshead, 2011). EPINED was approved by the Research and Ethics Committee of the Sant Joan University Hospital (13-10-31/10proj5) and by the Catalan Department of Education. Written consent forms were obtained from the children’s parents and the children and schools agreed to take part in the study.
Psychological Assessment, Diagnostic Procedure and ASD Case Definition
In the first phase, parents completed the Childhood Autism Spectrum Test (CAST; Scott et al. 2002) and teachers the EduTEA questionnaire (https://psico.fcep.urv.cat/Q4/EduTEA; Morales-Hidalgo et al. 2017) to screen for the risk of ASD.
In the second phase, ASD was diagnosed using the DSM-5 criteria from the Autism Diagnostic Observation Schedule, Second Edition (ADOS-2; Lord et al. 2012) and the Autism Diagnostic Interview-Revised (ADI-R; Rutter et al. 2003). Autism severity was determined based on the ADOS cut-off points described by Gotham et al. (2009; i.e. ≤ 3 non ASD, 4–5 ASD, 6–10 autism). In terms of ASD case definition, diagnoses were considered positive when the child’s score reached or exceeded the threshold in all the ADI-R diagnostic algorithm domains and in the ADOS-2 calibrated score of severity (score ≥ 4), or when a consensus in diagnosis was reached by two trained researchers (psychologist and psychiatrist with experience with ASD) based on the information from the two instruments. The ASD diagnosis was considered subclinical when the child obtained subthreshold scores in both the ADI-R and ADOS-2 and a clinical consensus was also reached.
The Wechsler Scales of Intelligence for preschool and primary school children (WPPSI-IV, Wechsler Preschool and Primary Scale of Intelligence; and WISC-IV, Wechsler Intelligence Scales for Children (Wechsler, 2003, 2012) were used to assess cognitive function. To collect data on the presence of ADHD diagnosis and assess the compliance with DSM-5 diagnostic criteria, the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-PL; Kaufman et al. 1997) interview was administered to the families. All diagnoses and tests were performed by trained psychologists and psychiatrists.
Anthropometric Measures
In the second phase, anthropometric measurements were taken by a certificated dietitian in accordance with the International Society for the Advancement of Kinanthropometry (ISAK) protocols. A SECA® stadiometer accurate to 0.1 mm (PERILB-STND) was used to measure height (cm), and TANITA scales (BC 420SMA) to measure weight (kg). Subjects’ body mass index (BMI) (kg/m2) was obtained based on the international World Health Organization Chard Growth Standards (from birth to 5 years of age and children/teenagers 5–19 years of age (de Onis et al. 2007; World Health Organization [WHO] 2007).
Food Consumption and the Healthy Eating Index
The participants’ parents reported their children’s eating habits and the weekly frequency of food consumption using the food frequency questionnaires (FFQ) validated in Spanish adolescents and consisting of 45 items (Trinidad et al. 2008) and the FFQ validated in preschool children with 41 items (Esteban-Figuerola et al. 2020). The questionnaires yielded data on servings/day, servings/week, and grams/day. Grams/day of food consumption was calculated based on the items in the daily consumption frequency questionnaire according to the reference gram ration for each item and age group (Agència de Salut Pública de Catalunya 2005), and in agreement with the experts in this field from our research group (Arija et al. 1996a, b; Jardí et al. 2019a, b; Aparicio et al. 2015).
Items were classified into the following seven main food groups and 23 subgroups: (1) Starch group: 1—Savoury cereals and tubers (bread, pasta, rice, potatoes, breakfast cereals); 2—sweet cereals (biscuits, pastries, cookies); 3—legumes; 4—nuts; (2) Vegetable group: 5—boiled vegetables, 6—raw vegetables; (3) Fruit group: 7—citrus fruit, 8—other fruit, 9—preserved fruit, 10—natural fruit juice (mostly orange juice), 11—commercial fruit juice; (4) Dairy products group: 12—cheese and yogurt, 13—milk, 14—dairy desserts; (5) Fat group: 15—olive oil; (6) Protein group (also includes legumes): 16—poultry (chicken, turkey, etc.), 17—red and processed meat (beef, pork, etc.), 18—oily fish, 19—white fish, 20—seafood, 21—eggs; (7) Sweets/Sugary Beverages group: 22—sweets, 23—sugary beverages.
The average servings/day (s/d) or servings/week (s/w) per food group was compared with the recommended Spanish dietary/eating guidelines (R-DG) of the Spanish Society of Community Nutrition (Sociedad Española de Nutrición Comunitaria [SENC] 2018).
Diet quality was also estimated using the Spanish Quality Diet Index (SQDI) proposed by Norte Navarro and Ortiz Moncada (2011) based on the food recommendations of the SENC (2004). The SQDI includes nine food groups based on their nutritional quality. So, meat, fish and eggs were re-grouped into a single group, and sweets and sweet cereals also were grouped into a single group. The consumption of each group by serving was compared to the recommended consumption and scored 0–100. The final index scores were classified as ≥ 80 points ‘healthy’, 50–79 points ‘needs to improve’ and ≤ 49 points ‘unhealthy’.
Statistical Analysis
All variables were described and compared by age group and diagnosis (ASD, subclinical ASD and control/TD). ANOVA and Chi-square analyses were used to compare quantitative and qualitative variables, respectively. Prior to their application, we confirmed the normality of the variables and the criteria for the application of the statistical tests. The significance level for all statistical comparisons was set at P < 0.05. Data were analysed using SPSS Statistics 25.0.
Results
Table 1 shows the subjects’ sociodemographic, psychological, and anthropometrical characteristics by age (preschool or primary school children) and by ASD diagnosis (ASD, subclinical and control). There were significantly more boys on the autism spectrum (ASD and subclinical level) than girls. Between 80 and 85% of the sample were autochthons, and no clear differences in socioeconomic status were found between the autism spectrum groups and the children with TD. Around 25% of the pre-school and primary school children with ASD fell within the unhealthy diet group. BMI values were higher in primary school children with ASD than with TD, but these significant differences were not observed in the pre-school group. The mean IQ score was in the normal range for all groups, but TD children exhibited the highest IQs. ASD severity (ADOS-2) was low-moderate. Comorbidity between ASD and ADHD was high and increased in relation to age. ADHD was not present in children with TD because we excluded subjects with other neurodevelopmental disorders from the control sample.
Table 2 shows food group consumption in grams/day (g/d) and servings/day (s/d) or servings/week (s/w) by diagnosis status (ASD, subclinical ASD and TD), age, and recommended consumption. The consumption of children with ASD was similar to that of children with subclinical ASD in most food groups, including starches, dairy products, vegetables, fruit and fats. However, preschool children with ASD consumed fewer protein groups like legumes, fish (white fish) and eggs, and more sweets than pre-schoolers with subclinical ASD. Primary school children with ASD also consumed fewer legumes, but had a higher consumption of red and processed meat, commercial juices and sweets than those with subclinical ASD.
No differences were found between the diets of children with ASD (ASD and subclinical ASD) and that of children with TD in most food groups, including the starch, vegetable, fruit and dairy product,. However, some differences were found by age and food subgroups. Pre-schoolers with ASD consumed significantly fewer proteins and specifically lower g/d and servings of fish (both white and oily) and eggs. The primary school children with ASD consumed less in the subgroup of legumes, citrus fruit and natural fruit juices, cheese/yogurt and fat, and higher in other fruit, meats and sweets. The consumption of children with subclinical ASD was only significantly different from those of children with TD for raw vegetables and sweets in preschool children. At this age, preschool children with ASD consumed fewer raw vegetables than those with TD, a trend also observed in primary school children with ASD.
We also studied how the children's food consumption compared to dietary guidelines (R-DG) (Table 2), and found that, in general, the children have adequate consumption, or close to the R-DG, for the starch (although lower than the R-DG for legumes and nuts, and higher for sweet cereals), dairy, visible fats and protein groups (although lower than the R-DG for eggs). In contrast, all of the children consumed much fewer vegetables and fruits and more sweet foods and sugary beverages than recommended. However, according to the R-DG, in some food groups the consumption of children with ASD put them at higher risk for the development of diet-related issues than those of TD children. For example, children with ASD consumed even fewer raw vegetables and more sweets than TD children. In addition, at the preschool age, they deviate from the recommendations consuming less fish and eggs than TD children. And primary school children with ASD deviate even more from the recommendations consuming fewer legumes, citrus fruits, natural fruit juices and olive oil, and more meat than did TD children.
Discussion
This study describes food consumption and compliance with the dietary guidelines in a school population sample (3–6 years and 10–12 years) of children with ASD (clinical and subclinical diagnosis) and TD. Although a poorer quality diet was reported for the children with ASD than for the subclinical and control sample, all of the groups need to improve their diet. Differential intakes of some types of food were found among children with ASD compared to those with TD, as well as a higher consumption of sweets, possibly related to the organoleptic characteristics of these foods and the idiosyncrasy of this pathology.
Food Consumption Differences Between Children with ASD and TD
To our knowledge, this is the first study to compare the food consumption of children with subclinical ASD and ASD, and subclinical ASD and TD. The analysis comparing the food consumption of subclinical ASD and ASD subjects yielded few differences overall. However, differences were found between the subclinical ASD and TD subjects. Among the differences found, it is striking that in both age groups, children with subclinical ASD tend to consume more legumes than children with ASD or even with TD, and this is the one group that reached the recommended number of servings. The consumption of legumes is recommended by public health agencies around the world on the basis that they are a good source of protein, fibre, and several micronutrients, including iron and zinc (Venn et al. 2012). In our study, the lowest consumption of legumes was found among children with ASD, in contrast to the data presented by Marí-Bauset et al. (2017), which was also collected from a Spanish population in a Mediterranean environment. The joint analysis of the consumption of sweets/beverages was not differently significant between groups but favourably children with subclinical ASD consumed fewer sweets than children with ASD. Other differences in food consumption between subclinical ASD and other groups are related to age group. Preschool children with subclinical ASD had higher consumption in the protein groups than ASD children in the same age group, specifically related to the reduced consumption of fish and eggs, while primary school children with subclinical ASD consumed less meats than those with ASD. Our data did not support the hypothesis of a consistent eating pattern within the broad autism phenotype. We did not find a progression in food consumption according to the level of severity of ASD (from diagnostic to subclinical). Only in raw vegetables did preschool children with ASD and subclinical ASD consume significantly less than children with TD, and the same trend was observed among primary school children. However, although a low degree of acceptance of vegetables has been referred to in several studies with ASD children (Chistol et al. 2018; Dickerson Mayes and Zickgraf 2019; Tsujigushi et al. 2020), the small sample size of subclinical ASD children and the non-generalisation with other foods does not allow us to draw conclusions in this case.
We found that the differences between children along the entire autism disorder spectrum and those with TD occur mainly with children diagnosed with ASD and not with the subclinical ASD group. However, although it should be noted that the consumption of most food groups is quite similar between children with ASD and those with TD, some interesting peculiarities emerged when comparing food subgroups. Our data were not consistent with those of Marí-Bauset et al. (2017), who, also in Spain, found a healthy eating index for children with ASD and no significant differences in the food variety score. In the current study, differences between food subgroups may be related to the sensory characteristics of the food, which, together with the clinical characteristics of children with ASD, such as disordered sensorial processing, inflexible adherence to routines and gastrointestinal disturbances (Cemark et al. 2010; Hubbart et al. 2014; Ranjan and Nasser 2015; Santocchi et al. 2016; Smith et al. 2020), may give rise to the food preferences and aversions typical in this population (Emond et al. 2010; Evans et al. 2012; Graf-Myles et al. 2013; Liu et al. 2016). In addition, as mentioned in Schreck and Williams (2006), along with the diagnostic characteristics of autism, family food preferences could also influence the food selection of the children.
In addition, we observed specific differences in dietary patterns by age. We found an evolutionary change in dietary protein sources: preschool children with ASD consumed less protein groups than TD children (− 35.3 g; − 22.5%) (p = 0.002), and this is opposite to the consumption of primary school children (22.5 g; 11.7%) (p = 0.058), which is related to the high consumption of meats in this age group. Vissoker et al. (2018), working with a group of preschool children, and Malhi et al. (2017), with children between 4 and 10 years old, found that ASD children consume less protein food groups than TD children. However, neither Williams et al. (2005) nor Diolordi et al. (2014) found any differences with samples of a wide age range (2–12 years old and 6–9.5 years old, respectively). In our study, the lower consumption of protein found in preschool children with ASD was due to the reduced consumption of fish and eggs. In different cultural settings, Al-Farsi et al. (2013) also found a lower consumption of fish, eggs, legumes and vegetables in Egyptian ASD preschool children than in TD preschool children, and Hertz-Picciotto et al. (2010) found a lower consumption of fish in Californian ASD preschool children than in TD children. The reduced consumption of fish could be related to the particular smell and flavour of fish or to its bones (Chistol et al. 2018; Diolordi et al. 2014). In contrast, Zhu et al. (2020) in China and other authors in the USA (Berding and Donovan 2018; Graf-Myles et al. 2013) found only a lower consumption of dairy in ASD preschool children compared to their TD peers, which is not supported by our data. Unlike some of these authors, the children with autism in our sample were not reported to follow intentional diets, such as casein-free diets. We found that primary school children with ASD consumed less cheese and yogurt than their peers with TD, which does not coincide with the lesser consumption of dairy described by Marí-Bauset et al. (2017) in Spanish children aged 6 to 9. Furthermore, the high consumption of meats within the protein food groups found in the sample of 10–11 years old in our study is not consistent with the data of other researchers, in which the consumption of meat was lower in children with ASD (Diolordi et al. 2014; Vissoker et al. 2019) or was the same in ASD and TD children (Zhu et al. 2020). Our data are similar to those of Huxham (2012), who found that in the UK 69.2% of children with ASD had preferences for processed meat products. Apart from these age differences in the consumption of proteins, primary school children with ASD also consumed fewer citrus fruits and less natural fruit juice, which in our country comes mainly from citrus fruit (oranges). This reduced consumption may be related to the acidic taste of these fruits, which may make them less accepted by children with ASD who present higher oral sensory sensitivity (Cermak et al. 2010; Chistol et al. 2018). On the other hand, the consumption of other fruits was higher in primary school children with ASD, which means that overall, no significant differences were detected in the total consumption of fruits. The higher consumption of non-citrus fruits could be related to their sweet and savoury taste (Diolordi et al. 2014; Schreck et al. 2004). The preference for these tastes may also be one reason for the higher consumption of sweets and commercial fruit juices in ASD children compared to the other diagnosis groups. Most studies have considered fruit consumption as a global value without differentiating fruit types. So, like us, the meta-analysis by Esteban et al. (2019) did not find any differences in overall fruit consumption, although only three studies could be analysed. However, other authors (Araujo et al. 2018; Evans et al. 2012; Smith et al. 2020; Vissoker et al. 2019; Zhu et al. 2020) found that fruit and vegetables were the least consumed foods among children with ASD. To promote the acceptance of fruit and vegetables, a recent study (Chung et al. 2020) physically changed these foods, improving impaired sensory processing and consequently increasing their consumption in children with ASD. In the fat group, primary school children with ASD consumed less olive oil than their peers with TD. We think that this slight decrease in oil consumption may be associated with a stronger dislike of stews; however, olive oil consumption is very common in Spain and specifically in the Mediterranean region, and we have not found other studies including this analysis to date.
Regardless of age group, children with ASD consumed fewer raw vegetables. These foods are characterised by strong flavours and tough textures, which make them less accepted by children with ASD (Chistol et al. 2018; Dickerson et al. 2019; Tsujigushi et al. 2020). Another possible reason for this food selectivity may be gastrointestinal disturbances, as described in Santocchi et al. (2016). Other authors (Al-Farsi et al. 2013; Bandini et al. 2010; Diolordi et al. 2014; Vissoker et al. 2019; Wallace et al. 2020; Zhu et al. 2020) have also observed a reduced consumption of vegetables, but they did not explore subgroups within vegetables. Only Al-Thbiany et al. (2017) described non-significant differences in raw and boiled vegetable consumption between children with ASD and TD. Lastly, and in agreement with previous data (Berding and Donovan 2018; Evans et al. 2012; Vissoker et al. 2019; Wallace et al. 2020), we found that the children with ASD consumed more sweets and sweetened beverages than children with TD. This excessive consumption has often been attributed to these children’s preference for sweet flavours (Schreck et al. 2004), but Wallace et al. (2020) found that among children with ASD, emotional over-eating was related to the increased consumption of sweet foods. This eating behaviour linked to negative emotions like anxiety may have both immediate and eventual health effects. On the other hand, the diet of children with ASD in our study, rich in simple sugars, added sugars and saturated fatty acids and low in fibre and antioxidants, may have consequences at the neurological level. This dietary pattern, as described Martínez Leo and Segura Campos (2020) in a neurobiological model, favours the dysbiosis of the gut microbiota and, through a series of systemic repercussions, facilitates the neuroinflammation process.
Diets of ASD and TD Children and Their Alignment with Recommendations
We compared our subjects’ food consumption with the serving/days recommended in the dietary guidelines to evaluate the degree of dietary adequacy. In general, we observed that the children in the different subject groups met the R-DG in terms of average values in the starch (with a lower consumption of legumes in children with ASD), dairy, oil (with a lower consumption in children with ASD), and protein groups (with lower fish and egg consumption in preschool children with ADS). The adequate consumption of these food groups ensures an adequate average supply of energy, proteins, carbohydrates, fats and MUFAs, calcium, fat-soluble vitamins and some minerals in the children.
However, we also observed some risky dietary behaviours among the children due to their very low consumption of legumes (between 0.19 and 0.31 s/w vs 2–4 s/w R-DG), vegetables (between 1.08 and 1.49 s/d vs 2–3 s/d R-DG) and fruit (between 1.36 and 1.74 s/d vs 2–3 s/d R-DG), and their higher consumption of sweet foods and sugary beverages (4.17–7.65 s/d vs occasionally R-DG), sweet cereals (between 0.86 and 1.33 s/d vs occasionally R-DG) compared to the R-DG.
Like other authors, we also observed that children with ASD generally consume a lower quantity of some foods than the R-DG in some food groups, almost all coinciding with a reduced consumption of fruits and vegetables (Araujo et al. 2018; Berding and Donovan 2018; Diolordi et al. 2014; Evans et al 2012; Graf-Myles et al. 2013; Malhi et al. 2017; Sharp et al. 2013), but not the other food groups. However, our study did not reveal a lower consumption of dairy products or protein than that recommended in the dietary guidelines, nor a reduced consumption in children with ASD in relation to TD children, though other authors have observed a lower consumption of dairy products among children with ASD (Al-Thbiany et al. 2017; Berding and Donovan 2018; Diolordi et al 2014; Graf-Myles et al. 2013; Malhi et al. 2017; Marí-Bauset et al. 2017) proteins (Al-Thbiany et al. 2017; Malhi et al. 2017; Sharp et al. 2013), and fish (Al-Thbiany et al. 2017; Berding and Donovan 2018). Nevertheless, the samples used in most studies come from a clinical population, which may represent a greater severity of autism than in this study (severity in ADOS is low). In our sample, only the preschool children with ASD failed to meet the recommendations for fish consumption, while the fish consumption habits of all the other groups aligned with the guidelines.
Our data are consistent with those of most studies conducted with children from developed countries, in which the consumption of sweet food products and sugary drinks is much higher than the recommended occasional consumption (Araujo et al. 2018; Berding and Donovan 2018; Evans et al. 2012; Sharp et al. 2013). It has been well established that a higher consumption of sugary products is associated with the development of obesity, type 2 diabetes mellitus and cardiovascular diseases (Ludwing et al. 2018; Makarem et al. 2018; WHO 2015).
In general, a dietary pattern with a low content of fibres from legumes, nuts, fruits and vegetables is related to a decreased feeling of satiety during meals (Clark and Slavin 2013). This, together with an excess intake of high energy density food, such as sweet cereals, sweets and sugary drinks, constitute an eating pattern of high energy intake in all children. However, it is important to note that this high-risk eating pattern is more pronounced among children with ASD, since their specificities in the consumption of some food groups leads them to an eating pattern that diverges even further from the R-DG. This is the case of the reduced consumption of legumes, raw vegetables, some types of fruit, and fish (in preschool children) and the higher consumption of sweets among children with ASD compared to children with TD.
This pattern coincides with the higher percentage of obesity observed in children with ASD versus TD children (preschool: 16.7% vs 7.0%; p = 0.240; primary school: 29.3% vs 19.3%; p = 0.046). Other authors have also observed this relationship between the eating patterns in ASD subjects and the higher prevalence of obesity (Araujo et al. 2018; Evans et al. 2012).
Strengths and Limitations
One of the strengths of the design of this study is that the participants come from a representative school sample from a Spanish province. The two-phase design allowed us to detect both children at risk and not at risk of ASD, all of whom underwent the diagnostic procedure, which yielded three groups: ASD, subclinical ASD and TD. In addition, the study of two age groups allowed us to explore differences related to age. Most published studies come from clinical samples, so it is difficult to include children with subclinical ASD and children with TD with equivalent age and geographical characteristics. However, our results cannot be generalised for ASD and subclinical ASD, because the number of subjects in these age subgroups was not very high.
At a methodological level, the diagnostic procedure for ASD was very rigorous, and both validated techniques and questionnaires were used to determine the anthropometric and nutritional variables, specifically, the CFCA has been validated in the Spanish population for both age groups participating in the study.
Conclusion
The consumption habits of children with ASD, subclinical ASD and TD present no differences in the major food groups. However, the consumption of some food subgroups is different between children with ASD and TD and undergoes changes with age. Preschool children with ASD eat fewer raw vegetables, fish, and eggs, and primary school children with ASD consume fewer legumes, raw vegetables, citrus fruits and natural juices, cheese and yogurt and olive oil and more meat (red and processed meat) than children with TD. Both age groups with ASD consumed more sugar than the TD group. None of the children met the recommended dietary guidelines for fruit, vegetables, legumes or eggs, but children with ASD diverged even further from the recommendations than the TD group. Their eating pattern (poor in legumes, fruit, vegetables, and rich in sugary cereals, red and processed meat, sweets and sugary drinks) puts them at higher risk of developing obesity than TD children. Children in general, and especially children with autism, would benefit from the promotion of a healthy diet. It would be interesting to confirm the health risk that their eating habits may have through follow-up studies.
References
Agència de Salut Pública de Catalunya. (2005). La alimentación saludable en la etapa escolar. Barcelona: Agència de Salut Pública de Catalunya. Generalitat de Catalunya. Retrieved April 4, 2020 from https://es.calameo.com/read/000784569c7c9f5e80645.
Al-Farsi, Y. M., Waly, M. I., Deth, R. C., Al-Sharbati, M. M., Al-Shafaee, M., Al-Farsi, O., et al. (2013). Impact of nutrition on serum levels of docosahexaenoic acid among Omani children with autism. Nutrition, 29(9), 1142–1146. https://doi.org/10.1016/j.nut.2013.03.009
Al-Thbiany, A., Farghal, S., Al-Harbi, G., Abduallah, M., Al-Rehaly, R., Al-Johani, G., et al. (2017). Assessment of some nutritional risk factors that predispose to autism among preschool & school Saudi children living in AL-Madinah Al-Monawarah city. Journal of Studies and Searches of Specific Education, 3(1), 133–145.
Aparicio, E., Canals, J., Pérez, S., & Arija, V. (2015). Dietary intake and nutritional risk in Mediterranean adolescents in relation to the severity of the eating disorder. Public Health Nutrition, 18(8), 1461–1473. https://doi.org/10.1017/S1368980014002043
Araujo, A., Almeida, P., Alves, L., Carvalho, W., Zagmignan, A., Rodrigues de Oliveira, B., et al. (2018). Consumption of ultra-processed foods and nutritional status of children with autism spectrum disorder. Revista Brasileira em Promoção da Saúde. Retrieved from https://core.ac.uk/download/pdf/235419963.pdf.
Arija, V., Salas Salvadó, J., Fernández-Ballart, J., Cucó, G., & Martí-Henneberg, C. (1996a). Consumption, dietary habits and nutritional status of the Reus (IX) population. Evolution of food consumption, energy and nutrient intake and relationship with the socioeconomic and cultural level, 1983–1993. Medicina Clinica, 106(5), 174–179.
Arija, V., Salas Salvadó, J., Fernández-Ballart, J., Cucó, G., & Martí-Henneberg, C. (1996b). Food consumption, habits, and nutritional status of the population of Reus (VIII). Evolution of energy and nutrient intake from 1983 to 1993. Medicina Clínica (Barcelona), 106(2), 45–50.
Bandini, L. G., Anderson, S. E., Curtin, C., Cermak, S., Evans, E. W., Scampini, R., et al. (2010). Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics, 157(2), 259–264. https://doi.org/10.1016/j.jpeds.2010.02.013
Bandini, L. G., Curtin, C., Phillips, S., Anderson, S. E., Maslin, M., & Must, A. (2017). Changes in food selectivity in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(2), 439–446. https://doi.org/10.1007/s10803-016-2963-6
Barnhill, K., Gutierrez, A., Ghossainy, M., Marediya, Z., Marti, C. N., & Hewitson, L. (2017). Growth status of children with autism spectrum disorder: A case-control study. Journal of Human Nutrition and Dietetics, 30(1), 59–65. https://doi.org/10.1111/jhn.12396
Berding, K., & Donovan, S. M. (2018). Diet can impact microbiota composition in children with autism spectrum disorder. Frontiers in Neuroscience, 12, 515. https://doi.org/10.3389/fnins.2018.00515
Castro, K., Faccioli, L. S., Baronio, D., Gottfried, C., Perry, I. S., & Riesgo, R. (2016). Feeding behavior and dietary intake of male children and adolescents with autism spectrum disorder: A case-control study. International Journal of Developmental Neuroscience: the Official Journal of the International Society for Developmental Neuroscience, 53, 68–74. https://doi.org/10.1016/j.ijdevneu.2016.07.003
Cermak, S. A., Curtin, C., & Bandini, L. G. (2010). Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association, 110(2), 238–246. https://doi.org/10.1016/j.jada.2009.10.032
Chistol, L. T., Bandini, L. G., Must, A., Phillips, S., Cermak, S. A., & Curtin, C. (2018). Sensory sensitivity and food selectivity in children with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48(2), 583–591. https://doi.org/10.1007/s10803-017-3340-9
Chung, L., Law, Q., & Fong, S. (2020). Using physical food transformation to enhance the sensory approval of children with autism spectrum disorders for consuming fruits and vegetables. Journal of Alternative and Complementary Medicine, 26(11), 1074–1079. https://doi.org/10.1089/acm.2020.0215
Clark, M. J., & Slavin, J. L. (2013). The effect of fiber on satiety and food intake: A systematic review. Journal of the American College of Nutrition. https://doi.org/10.1080/07315724.2013.791194
Curtin, C., Hubbard, K., Anderson, S. E., Mick, E., Must, A., & Bandini, L. G. (2015). Food selectivity, mealtime behavior problems, spousal stress, and family food choices in children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(10), 3308–3315. https://doi.org/10.1007/s10803-015-2490-x.
de Onis, M., Onyango, A. W., Borghi, E., Siyam, A., Nishida, C., & Siekmann, J. (2007). Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization, 85(9), 660–667. https://doi.org/10.2471/blt.07.043497
Dickerson Mayes, S., & Zickgraf, H. (2019). Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Research in Autism Spectrum Disorders, 64, 76–83. https://doi.org/10.1016/j.rasd.2019.04.002
Diolordi, L., del Balzo, V., Bernabei, P., Vitiello, V., & Donini, L. M. (2014). Eating habits and dietary patterns in children with autism. Eating and Weight Disorders, 19(3), 295–301. https://doi.org/10.1007/s40519-014-0137-0
Emond, A., Emmett, P., Steer, C., & Golding, J. (2010). Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics, 126(2), e337–e342. https://doi.org/10.1542/peds.2009-2391
Esteban-Figuerola, P., Canals, J., Fernández-Cao, J. C., & Arija Val, V. (2019). Differences in food consumption and nutritional intake between children with autism spectrum disorders and typically developing children: A meta-analysis. Autism, 23(5), 1079–1095. https://doi.org/10.1177/1362361318794179
Esteban-Figuerola, P., Jardí, C., Canals, J., & Arija Val, V. (2020). Validación de un cuestionario corto de frecuencia de consumo alimentario en niños pequeños. Nutrición Hospitalaria, 37(1), 101–113. https://doi.org/10.20960/nh.02670
Evans, E. W., Must, A., Anderson, S. E., Curtin, C., Scampini, R., Maslin, M., & Bandini, L. (2012). Dietary patterns and body mass index in children with autism and typically developing children. Research in Autism Spectrum Disorders, 6(1), 399–405. https://doi.org/10.1016/j.rasd.2011.06.014
Gotham, K., Pickles, A., & Lord, C. (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705. https://doi.org/10.1007/s10803-008-0674-3
Graf-Myles, J., Farmer, C., Thurm, A., Royster, C., Kahn, P., Soskey, L., Rothschild, L., & Swedo, S. (2013). Dietary adequacy of children with autism compared with controls and the impact of restricted diet. Journal of Developmental and Behavioral Paediatrics, 34(7), 449–459. https://doi.org/10.1097/DBP.0b013e3182a00d17
Herndon, A. C., DiGuiseppi, C., Johnson, S. L., Leiferman, J., & Reynolds, A. (2009). Does nutritional intake differ between children with autism spectrum disorders and children with typical development? Journal of Autism and Developmental Disorders, 39(2), 212–222. https://doi.org/10.1007/s10803-008-0606-2
Hertz-Picciotto, I., Green, P. G., Delwiche, L., Hansen, R., Walker, C., & Pessah, I. N. (2010). Blood mercury concentrations in CHARGE Study children with and without autism. Environmental Health Perspectives, 118(1), 161–166. https://doi.org/10.1289/ehp.0900736
Hollingshead, A. B. (2011). Four factor index of social status. Yale Journal of Sociology, 8, 21–52.
Hubbard, K. L., Anderson, S. E., Curtin, C., Must, A., & Bandini, L. G. (2014). A comparison of food refusal related to characteristics of food in children with autism spectrum disorder and typically developing children. Journal of the Academy of Nutrition and Dietetics, 114(12), 1981–1987. https://doi.org/10.1016/j.jand.2014.04.017
Huxham, L. (2012). Feeding problems and current dietary practices in children with autism spectrum disorder in England [Doctoral Thesis, University of Stellenbosch]. Retrieved from http://scholar.sun.ac.za/handle/10019.1/20190.
Jardí, C., Aranda, N., Bedmar, C., & Arija, V. (2019a). Excess nutritional risk in infants and toddlers in a Spanish city. International Journal for Vitamin and Nutrition Research, 89(3–4), 210–220. https://doi.org/10.1024/0300-9831/a000530
Jardí, C., Aranda, N., Bedmar, C., Ribot, B., Elias, I., Aparicio, E., et al. (2019b). Consumption of free sugars and excess weight in infants. A longitudinal study. Anales de Pediatría, 90(3), 165–172. https://doi.org/10.1016/j.anpedi.2018.03.018
Johnson, C. R., Turner, K., Stewart, P. A., Schmidt, B., Shui, A., Macklin, E., et al. (2014). Relationships between feeding problems, behavioral characteristics and nutritional quality in children with ASD. Journal of Autism and Development Disorders, 44, 2175–2184. https://doi.org/10.1007/s10803-014-2095-9.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. https://doi.org/10.1097/00004583-199707000-00021
Leader, G., Tuohy, E., Chen, J. L., Mannion, A., & Gilroy, S. P. (2020). Feeding problems, gastrointestinal symptoms, challenging behavior and sensory issues in children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(4), 1401–1410. https://doi.org/10.1007/s10803-019-04357-7
Liu, X., Liu, J., Xiong, X., Yang, T., Hou, N., Liang, X., et al. (2016). Correlation between nutrition and symptoms: Nutritional survey of children with autism spectrum disorder in Chongqing, China. Nutrients, 8(5), 294. https://doi.org/10.3390/nu8050294
Lord, C., Rutter, M., DiLavore, P., Risi, S., Gotham, K., & Bishop, S. (2012). Autism diagnostic observation schedule (ADOS) (2nd ed.). Beaverton: Western Psychological Corporation.
Ludwig, D. S., Hu, F. B., Tappy, L., & Brand-Miller, J. (2018). Dietary carbohydrates: Role of quality and quantity in chronic disease. British Medical Journal, 361, 2340. https://doi.org/10.1136/bmj.k2340
Maenner, M. J., Shaw, K. A., Baio, J., Washington, A., Patrick, M., DiRienzo, M., et al. (2020). Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. Morbidity and Mortality Weekly Report. Survellance Summaries, 69(4), 1–12.
Makarem, N., Bandera, E. V., Nicholson, J. M., & Parekh, N. (2018). Consumption of sugars, sugary foods, and sugary beverages in relation to cancer risk: A systematic review of longitudinal studies. Annual Review of Nutrition, 38(1), 17–39. https://doi.org/10.1146/annurev-nutr-082117-051805
Malhi, P., Venkatesh, L., Bharti, B., & Singhi, P. (2017). Feeding problems and nutrient intake in children with and without autism: A comparative study. The Indian Journal of Pediatrics, 84(4), 283–288. https://doi.org/10.1007/s12098-016-2285-x
Mannion, A., Leader, G., & Healy, O. (2013). Comorbidity in autism spectrum disorder: A literature review. Research in Autism Spectrum Disorders, 7(12), 1595–1616. https://doi.org/10.1016/j.rasd.2013.09.006
Marí-Bauset, S., Llopis-González, A., Zazpe, I., Marí-Sanchis, A., & Suárez-Varela, M. (2017). Comparison of nutritional status between children with autism spectrum disorder and typically developing children in the Mediterranean Region (Valencia, Spain). Autism, 21(3), 310–322. https://doi.org/10.1177/1362361316636976
Marí-Bauset, S., Zazpe, I., Mari-Sanchis, A., Llopis-González, A., & Suárez-Varela, M. (2014). Evidence of the gluten-free and casein-free diet in autism spectrum disorders: A systematic review. Journal of Child Neurology, 29(12), 1718–1727. https://doi.org/10.1177/0883073814531330
Martínez Leo, E. E., & Segura Campos, M. R. (2020). Effect of ultra-processed diet on gut microbiota and thus its role in neurodegenerative diseases. Nutrition, 71, 110609. https://doi.org/10.1016/j.nut.2019.110609
Matheson, B. E., & Douglas, J. M. (2017). Overweight and obesity in children with Autism Spectrum Disorder (ASD): A critical review investigating the development, and maintenance of this relationship. Review Journal of Autism and Developmental Disorders, 4, 4142–4156. https://doi.org/10.1007/s40489-017-0103-7
McElhanon, B. O., McCracken, C., Karpen, S., & Sharp, W. G. (2014). Gastrointestinal symptoms in autism spectrum disorder: A meta-analysis. Pediatrics, 133(5), 872–883. https://doi.org/10.1542/peds.2013-3995
Morales-Hidalgo, P., Hernández-Martínez, C., Voltas, N., & Canals, J. (2017). EDUTEA: A DSM-5 teacher screening questionnaire for autism spectrum disorder and social pragmatic communication disorder. International Journal of Clinical and Health Psychology, 17(3), 269–281. https://doi.org/10.1016/j.ijchp.2017.05.002
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011a). Association of sensory processing and eating problems in children with autism spectrum disorders. Autism Research and Treatment. https://doi.org/10.1155/2011/541926
Nadon, G., Feldman, D. E., Dunn, W., & Gisel, E. (2011b). Mealtime problems in children with autism spectrum disorder and their typically developing siblings: A comparison study. Autism, 15(1), 98–113. https://doi.org/10.1177/1362361309348943
Neumeyer, A. M., Cano Sokoloff, N., McDonnell, E. I., Macklin, E. A., McDougle, C. J., Holmes, T. M., et al. (2018). Nutrition and bone density in boys with autism spectrum disorder. Journal of the Academy of Nutrition and Dietetics, 118(5), 865–877. https://doi.org/10.1016/j.jand.2017.11.006
Norte Navarro, A. I., & Ortiz Moncada, R. (2011). Calidad de la dieta española según el índice de alimentación saludable. [Spanish diet quality according to the healthy eating index]. Nutrición Hospitalaria, 26(2), 330–336. https://doi.org/10.1590/S0212-16112011000200014
Ranjan, S., & Nasser, J. A. (2015). Nutritional status of individuals with autism spectrum disorders: Do we know enough? Advances in nutrition (Bethesda, Md.), 6(4), 397–407. https://doi.org/10.3945/an.114.007914
Rutter, M., Le Couteur, A., & Lord, C. (2003). Autism diagnostic interview revised (ADI-R). Beaverton: Western Psychological Services.
Salazar, F., Baird, G., Chandler, S., Tseng, E., O’sullivan, T., Howlin, P., et al. (2015). Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2283–2294. https://doi.org/10.1007/s10803-015-2361-5
Santocchi, E., Guiducci, L., Fulceri, F., Billeci, L., Buzzigoli, E., Apicella, F., et al. (2016). Gut to brain interaction in Autism Spectrum Disorders: A randomized controlled trial on the role of probiotics on clinical, biochemical and neurophysiological parameters. BMC Psychiatry, 16, 183. https://doi.org/10.1186/s12888-016-0887-5
Schreck, K. A., & Williams, K. (2006). Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Research in Developmental Disabilities, 27(4), 353–363. https://doi.org/10.1016/j.ridd.2005.03.005
Schreck, K. A., Williams, K., & Smith, A. F. (2004). A comparison of eating behaviors between children with and without autism. Journal of Autism and Developmental Disorders, 34(4), 433–438. https://doi.org/10.1023/b:jadd.0000037419.78531.86
Scott, F. J., Baron-Cohen, S., Bolton, P., & Brayne, C. (2002). The CAST (Childhood Asperger Syndrome Test): Preliminary development of a UK screen for mainstream primary-school-age children. Autism, 6(1), 9–31. https://doi.org/10.1177/1362361302006001003
Sharp, W. G., Berry, R. C., McCracken, C., Nuhu, N. N., Marvel, E., Saulnier, C. A., et al. (2013). Feeding problems and nutrient intake in children with autism spectrum disorders: A meta-analysis and comprehensive review of the literature. Journal of Autism and Developmental Disorders, 43(9), 2159–2173. https://doi.org/10.1007/s10803-013-1771-5
Smith, B., Rogers, S. L., Blissett, J., & Ludlow, A. K. (2020). The relationship between sensory sensitivity, food fussiness and food preferences in children with neurodevelopmental disorders. Appetite, 150, 104643. https://doi.org/10.1016/j.appet.2020.104643
Sociedad Española de Nutrición Comunitaria. (2018). Guía de Alimentación Saludable para Atención Primaria y colectivos ciudadanos. La alimentación saludable en la etapa escolar. Planeta. Retrieved April 4, 2020 from https://www.nutricioncomunitaria.org/es/noticia/guia-alimentacion-saludable-ap.
Trinidad Rodríguez, I., Fernández Ballart, J., Cucó Pastor, G., Biarnés Jordà, E., & Arija Val, V. (2008). Validación de un cuestionario de frecuencia de consumo alimentario corto: reproducibilidad y validez. Nutrición Hospitalaria, 23(3), 242–252. Retrieved January 19, 2021 from http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0212-16112008000300011&lng=es&tlng=es.
Tsujiguchi, H., Miyagi, S., Nguyen, T., Hara, A., Ono, Y., Kambayashi, Y., et al. (2020). Relationship between autistic traits and nutrient intake among Japanese children and adolescents. Nutrients, 12(8), 2258. https://doi.org/10.3390/nu12082258
Venn, B., Thies, F., & O’Neil, C. (2012). Whole grains, legumes, and health. Journal of Nutrition and Metabolism, 2012, 903767. https://doi.org/10.1155/2012/903767
Vermeirsch, J., Verhaeghe, L., Casaer, A., Faes, F., Oostra, A., & Roeyers, H. (2020). Diagnosing autism spectrum disorder in toddlers born very preterm: Estimated prevalence and usefulness of screeners and the autism diagnostic observation schedule (ADOS). Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-020-04573-6
Vissoker, R. E., Berger, D., Latzer, Y., & Gal, E. (2018). Food selectivity, gastrointestinal symptoms and urine organic acids in autism spectrum disorder: A pilot study. Current Nutrition & Food Science, 14, 171–179. https://doi.org/10.2174/1573401313666170525133604.
Vissoker, R. E., Latzer, Y., Stolar, O., Rabenbach, A., & Gal, E. (2019). Eating problems and patterns among toddlers and young boys with and without autism spectrum disorders. Research in Autism Spectrum Disorders, 59, 1–9. https://doi.org/10.1016/j.rasd.2018.12.001
Wallace, G. L., Richard, E., Wolff, A., Nadeau, M., & Zucker, N. (2020). Increased emotional eating behaviors in children with autism: Sex differences and links with dietary variety. Autism. https://doi.org/10.1177/1362361320942087
Webber, A., Sinha, S., Robinson, C., & Gray, H. L. (2018). Associations among diet variety, mealtime behaviors, and diet quality in children with autism spectrum disorder. Journal of Nutrition Education and Behavior, 50(7), S27. https://doi.org/10.1016/j.jneb.2018.04.071
Wechsler, D. (2003). Wechsler intelligence scale for children—Fourth Edition (WISC-IV). San Antonio, TX: The Psychological Corporation.
Wechsler, D. (2012). Wechsler preschool and primary scale of intelligence—Fourth Edition (WPPSI-IV). San Antonio, TX: The Psychological Corporation.
Williams, K. E., Gibbons, B. G., & Schreck, K. A. (2005). Comparing selective eaters with and without developmental disabilities. Journal of Developmental and Physical Disabilities, 17(3), 299–309. https://doi.org/10.1007/s10882-005-4387-7
World Health Organization. (2007c). WHO Growth Standards: Head Circumference-for-Age, Arm Circumference-for-Age, Triceps Skinfold-for-Age and Subscapular Skinfold-for-Age: Methods and Development. Geneva: World Health Organization. Retrieved January 2, 2020 from https://www.who.int/childgrowth/standards/second_set/technical_report_2.pdf?ua=1.
World Health Organization. (2015). Guideline: sugars intake for adults and children. Geneva, World Health Organization. Retrieved June 10, 2020 from https://www.who.int/publications/i/item/9789241549028.
Zhu, J., Guo, M., Yang, T., Lai, X., Tang, T., Chen, J., et al. (2020). Nutritional status and symptoms in preschool children with autism spectrum disorder: A two-center comparative study in Chongqing and Hainan province, China. Frontiers in Pediatrics, 8, 469. https://doi.org/10.3389/fped.2020.00469
Zimmer, M. H., Hart, L. C., Manning-Courtney, P., Murray, D. S., Bing, N. M., & Summer, S. (2012). Food variety as a predictor of nutritional status among children with autism. Journal of Autism and Developmental Disorders, 42(4), 549–556. https://doi.org/10.1007/s10803-011-1268-z
Acknowledgments
The authors are grateful to the URV English Service for the review of the manuscript
Funding
This study was supported by Spain’s Ministry of Economy and Competitiveness and the European Regional Development Fund (ERDF) [Grant PSI2015-64837-P]; by the Catalan Government’s Department of Universities, Research and Information Society and the European Social Fund (FSE), [Grant 2019FI_B2_00148]; and by Spain’s Ministry of Science, Innovation and Universities and the European Regional Development Fund (ERDF) [Project RTI2018-097124-B-I00].
Author information
Authors and Affiliations
Contributions
Study concept and design: JC-S. Material preparation, data collection and analysis were performed by JC-S, PE-F and PM-H. The first draft of the manuscript was written by JC-S, PE-F and VA All authors reviewed the manuscript for important intellectual content and approved the final version to be published. JC-S is the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Canals-Sans, J., Esteban-Figuerola, P., Morales-Hidalgo, P. et al. Do Children with Autism Spectrum Disorders Eat Differently and Less Adequately than Those with Subclinical ASD and Typical Development? EPINED Epidemiological Study. J Autism Dev Disord 52, 361–375 (2022). https://doi.org/10.1007/s10803-021-04928-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-021-04928-7