Abstract
Racial and ethnic disparities in the use of nine common autism-related services among Medicaid-enrolled children with autism spectrum disorder (ASD) were examined, distinguishing between school and other community-based outpatient settings. Using 2012 Medicaid Analytic Extract data, we identified 117,848 continuously enrolled children with ASD. Several racial and ethnic disparities were found, varying by geography. Black, Asian, and Native American/Pacific Islanders received fewer outpatient services compared with white children, but there was no disparity for Latinx children. Black and Asian children received more school-based services than white children. Disparities in case management/care coordination services were largest and present in each minority group. Geographic variation in receipt of services suggests targets for policy intervention to improve access for minorities with ASD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Racial and ethnic disparities are known to exist in access to timely diagnostic services for autism spectrum disorder (ASD) (Mandell et al. 2002). Studies have also examined disparities in the use of autism-related health and education services (Bilaver and Havlicek 2019; Liptak et al. 2008; Magaña et al. 2012, 2016; Smith et al. 2020) as well as subspecialty services (Broder-Fingert et al. 2013). Limitations in English language proficiency has been found to relate to barriers to service access for the Latinx population (Zuckerman et al. 2017). However, most studies that examine disparities in autism-related service use do not distinguish between clinical factors that may affect service use, such as disorder severity, versus factors that reflect unequal treatment. Understanding the source of differences is an important step towards implementing practice or policy solutions to mitigate racial and ethnic inequities.
The Medicaid program is the single largest payer for autism-related health care services. In addition to paying for care for children categorically eligible due to low income, disability, and being in foster care, Medicaid also pays for school-based services for eligible children in most states (Baller and Barry 2016). However, school and other community-based outpatient clinical services (hereafter outpatient) have different purposes in supporting children with ASD; in many cases both may be indicated. Services delivered at school should be designed to facilitate a “free and appropriate education,” (Education for All Handicapped Children’s Act 1975; Individual with Disabilities Education Act 1997, 1990) while outpatient services should be designed to maximize functioning in a broader range of environments, including home. For example, school-based services may not be granted if a child with autism is performing at grade level, even if their social impairments may affect long-term outcomes such as higher educational attainment, employment, and overall family functioning.
Recent studies of racial disparities in the Medicaid program have focused on services delivered through the home and community-based services (HCBS) waiver program. Although previous research on HCBS programs finds they are associated with reduced racial and ethnic disparities in unmet need for services among children with ASD (LaClair et al. 2019), less is known about the extent of disparities for children insured through Medicaid outside of waiver programs or disparities in school-based Medicaid-funded services. Although families of children with ASD may consider specific school and outpatient services interchangeable, procedures to access services in different settings vary. Furthermore, it is unclear how previous research on disparities among Latino children with ASD in the general population (Magaña et al. 2013; Zuckerman et al. 2013, 2014, 2016) applies to children served in the Medicaid program.
Conceptual Model
This study employs the framework of racial and ethnic disparity put forth in the Institute of Medicine’s (IOM) 2003 report, Unequal Treatment (Institute of Medicine 2003), to address gaps in our understanding of disparities in Medicaid-funded autism service use. The IOM framework distinguishes among factors that make up a disparity in health care. Figure 1 presents the framework. Differences between racial groups due to factors reflecting clinical appropriateness, need for service or patient preferences are considered justifiable in the IOM framework (hereafter “need factors”). Factors stemming from the operation of the health care system, legal and regulatory climates, bias, discrimination, and stereotype are conceptualized as unjustifiable differences between groups (hereafter “non-need factors”). We categorized variables available in our data as need or non-need factors and applied methods so that our estimates of disparity reflected the definition put forth by the IOM.
In this study, we focused on nine services that children with ASD most often use and distinguished between school and outpatient services. Based on previous research (Bilaver and Havlicek 2019; Magaña et al. 2013, 2016; Zuckerman et al. 2017), we hypothesized that Latinx and black children would use fewer autism-related services than white children with ASD. We did not specify a priori hypotheses about disparities for Asian or Native American/Pacific Islander children, nor did we state hypotheses regarding the significance or size of specific contributions to disparities as there is not sufficient literature for these groups to make hypotheses. Instead, we used a decomposition analysis to guide post-hoc analyses.
Methods
Participants
Participants for this study were drawn from secondary data reflecting Medicaid claims. We used three files from the 2012 Medicaid Analytic eXtract (MAX) data in order to construct the study sample and measure outcomes: Other Therapy, Inpatient, and Personal Summary. The Other Therapy file includes many service types, such as physician and allied health care professional services, outpatient and clinic, lab, and home health, among others. The Personal Summary file provides information on months of enrollment and categories of eligibility. We also used data from the National Plan and Provider Enumeration System (NPPES) and the Area Health Resource File (AHRF). The NPPES data were used to categorize the type of provider. By using the taxonomy code and classification variable associated with the national provider ID, we identified Medicaid claims billed by a Local Education Agency (LEA) as a part of Medicaid special-education programs. AHRF data were used as the source for county-level indicators of health care resources.
The sample was drawn from MAX data from all 50 states and the District of Columbia (DC). It included 165,185 children ages 3–17 as of January 1, 2012 with an ASD diagnosis who were enrolled in the Medicaid program for all 12 months of 2012, were not dually enrolled in the Medicare program (as a result of end stage renal disease), and had access to full rather than partial benefits [as a result of dual eligibility or other state-specific restricted benefit plans (i.e. prescription drugs or pregnancy related services only)]. ASD was identified based on criteria used in previous studies: (Burke et al. 2014; Mandell et al. 2010) having at least two claims with an ASD ICD-9 diagnosis (299.0, 299.8, or 299.8) in the OT file within a 6-month period or one claim in the IP file with an ASD diagnosis. Children ages 0–3 were excluded because these children would have been eligible for services through Early Intervention Programs instead of School-based programs, and we were interested in understanding school-based Medicaid claims.
Additional exclusions were made based on data quality and the amount of missing data. Children in three states (n = 12,033) were excluded from the analysis. Idaho was excluded because most children in the Medicaid program did not have access to full benefits. Colorado was excluded because the race/ethnicity variable was missing in the MAX data. New York was excluded because claims in the OT file did not have associated procedure codes and could not be categorized in the same way as other states. Across the other 46 states and the District of Columbia, another 35,064 children were excluded due to missing or unknown race/ethnicity. Multi-racial was not used as a race category in all states; therefore children listed as multiracial were excluded from the analysis. Finally, a small number of observations (n = 240) were excluded due to missing values in the independent variables central to our analysis. There were 117,848 children included in the final analytic sample. The number of children with ASD in each state ranged from 174 (Hawai’i) to 7889 (Pennsylvania). Most of these children (92%) had some fee for service (FFS) claims during the year although a much smaller percentage (24%) only had FFS claims.
Procedures
We created dependent variables to reflect nine types of autism-related services that children with ASD typically use outside of a hospital or residential care setting: physical therapy, occupational therapy, speech therapy, mental health/social skills/behavior modification, case management/ care coordination, other 1-on-1 therapy or services, other group therapy or services, personal assistant or school aide, or respite care. Both binary and discrete count measures were created. Binary variables were created to indicate any versus no service use during 2012 (0 or 1). The number of claims for each service was treated as a discrete count variable. We identified all services using the procedure code found in the OT file records. The categorization of procedure codes was based on previous autism services research (Mandell et al. 2012). The study authors reviewed and categorized procedure codes uncategorized in the original typology (categorization available upon request). Supplementary Table E1 presents the top five procedure codes in each service category.
We also identified school-based services by identifying all claims where the national provider ID belonged to a LEA. These claims are assumed to be generated through the administration of school-based Medicaid programs. Although we expected at least 44 states to have claims billed by a LEA based on previous research (Baller and Barry 2016), we found only 27 with claims associated with an ASD diagnosis for our study sample. In addition, California and Maine had very low rates of billing by LEAs for any diagnosis within the study population (6% and 2% of study children with ASD, respectively), and thus were excluded. These exclusions were made in order to prevent bias due to systematic underreporting or variation in local billing practices that would affect the data that we had available in the MAX data. These exclusions left 75,200 children across 25 states for the analysis of school-based services. All services had to have either a primary or secondary diagnosis of ASD on the claim in order to be included in the analysis.
The primary independent variable was a five-level combined race/ethnicity variable. Categories include white (white, non-Latinx), black (African American or black, non-Latinx), Asian (Asian, non-Latinx), Native American/Pacific Islander (American Indian, Alaskan Native, Native Hawaiian, Pacific Islander, non-Latinx), and Latinx. White children served as the reference group in the analysis. The MAX data does not identify children by any other racial or ethnic groups aside from multi-racial, which was excluded from the analysis.
Need Factors
We included three types of need factors in the analysis: gender (male vs. female), age (categorized as 3–5 years, 6–8 years, 9–11 years, 12–14 years, and 15–17 years), and ASD-related comorbidities. Comorbidities common among children with ASD that could relate to the need for services were identified based on the clinical expertise of the authors and previous literature (Close et al. 2012; Frazier et al. 2014; Werling and Geschwind 2013). Variables were created from the OT and IP files using ICD-9 codes and HEDIS clinical classification software (Healthcare Cost and Utilization Project-HCUP 2014). Specifically we identified children with at least one claim with a diagnosis of intellectual disability, Attention Deficit Hyperactivity Disorder (ADHD), anxiety disorders, mood disorders, developmental delay, disruptive behavior and conduct disorders, schizophrenia and other psychotic disorders, learning disability, speech-language disorder, and sleep disorder. Supplemental Table E2 presents the ICD-9 codes used to define each comorbidity. Because gender and age could be correlated with unobserved severity, we included both variables as need factors in the analysis.
Non-need Factors
Non-need factors in the IOM framework may include any measured system, provider, or individual level factor that has the potential to impact health care delivery or quality. A four-level category of Medicaid program enrollment and a dichotomous indicator of home and community based waiver participation in January 2012 were the only individual-level non-need factor used in the analysis. Categories of Medicaid program enrollment included foster care, disability, low-income, and other. Several county-level non-need factors from the AHRF were used to reflect local health care characteristics. These included a three-level primary care and mental health care health professional shortage areas (no shortage in county, whole county shortage, partial county shortage). The AHRF includes a nine-level urban–rural continuum code for each county in the US. We created a five-level variable to describe both population density and land-use (metro county with population 1 million or more, metro county with 1 million to 250 K, metro county with less than 250 K, urban county with 20 K or more, completely rural or urban county with less than 20 K). Finally, we included the density of general pediatricians and pediatric specialists per 10 K in the child population as an indicator of health care access, a methodology previously described (Mandell et al. 2010, 2012).
Data Analysis
Disparity was measured using a three-step process concordant with the IOM definition which has been used throughout the health services literature (Cook et al. 2010, 2012; McGuire et al. 2006). The process includes (1) model estimation, (2) transformation of the distribution of need factors for racial and ethnic minorities, and (3) prediction. All analyses were performed using Stata 15.1.
Model Estimation
Separate logistic regression models were fit to estimate the log odds of ever receiving each of the autism-related services described above, and negative binomial regression was used to estimate the log of total services. The main specification for each model included race, the need and non-need factors described above, and state fixed effects. In some models state fixed effects could not be included due to problems of perfect prediction and convergence.
Transformation of Distribution of Need Factors
Transformation is the step in the process that creates IOM concordant estimates by adjusting the allowable differences between racial and ethnic groups before predicting the disparity. Transformation was done using the rank-and-replace method (Cook et al. 2010), the method most commonly used to create IOM concordant estimates (Cook et al. 2010, 2012; McGuire et al. 2006). The process involves equalizing the need factors between two groups by ranking observations according to the sum of the predicted value of the need factors and then replacing the prediction of the nth-ranked minority child with the nth-ranked white child. The process creates a counterfactual in which the need factors of the minority children are equal to that of white children, while non-need factors are allowed to vary.
Prediction
After equalizing the need factor related predictions between minority and white children, predicted service use of the counterfactual population was then calculated for each racial and ethnic group and compared to predicted service use among white children. The difference between minority and white in predicted mean service use is the IOM-concordant measure of disparity. Standard errors for the IOM concordant disparities were calculated using 1000 bootstrapped replicates (Efron 1979).
In post-hoc analyses of our primary logistic model, we used the Fairlie (2005) decomposition method and stratified analyses to examine the contribution of potentially modifiable drivers of disparities. The Fairlie method is an extension of the Oaxaca-Blinder decomposition model (Blinder 1973; Oaxaca 1973) applied to nonlinear binary outcome models. Because a randomly selected white subsample is used to estimate the contributions, the process is repeated with 1,000 randomly selected samples and results averaged. We used the Stata program developed by Ben Jann (2008) and random ordering of variables to address path dependence as described by Fairlie (2017). The choice of variables for the stratified analysis was based on the result of the decomposition. Specifically, we stratified the primary IOM concordant estimates of service use by whether the child lived in a metropolitan county with population over 250 K (large metro) versus other counties (small metro or non-metro). The dichotomous version of the urban–rural continuum code has been described elsewhere and used for policy decisions (Hart et al. 2005).
In addition to the post-hoc analyses informed by the decomposition, several sensitivity analyses were performed to assess our assumptions about sample selection criteria and variable choice. First, we ran our primary analysis on the subset of children with only FFS claims during 2012. Second, we assessed whether our criteria related to having an ASD diagnosis on the service claim was too strict. For example, children with ASD could be receiving some of the services included in our analysis as a result of comorbid conditions. We ran our primary analysis by include all claims of a particular service type regardless of the diagnosis (primary or secondary) on the claim. Finally, we assessed whether our results were robust to our conceptualization of gender as a need factor. If differences by gender reflect unjustified differential treatment within the health care system, gender should be considered a non-need factor. We tested the robustness of our primary analysis to a different assumption by interacting gender and race as a non-need factor in the analysis.
Results
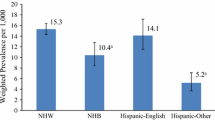
Descriptive statistics for the study population by race/ethnicity are presented in Table 1. Among Medicaid enrolled children with ASD in the analytic sample, 64% were white, 18% black, 14% Latinx, 2% Asian, and 2% Native American/Pacific Islander. The percentage of children with co-occurring conditions ranged from 34.5% (ADHD) to 3.0% (Schizophrenia and other psychotic disorders) and in many cases varied substantially across race/ethnicity. Most children with ASD were enrolled in Medicaid due to disability (50.7%) and through a waiver program (59.5%), although there was considerable variation by race/ethnicity in some categories. For example, 11.5% of black children were enrolled through foster care compared with 4% of Latinx, 2% of Asian, 7.5% of Native American/Pacific Islander, and 8.1% of white children. Similarly, 51.1% of black children were enrolled in a waiver program compared with 66.3% Latinx, 70.7% of Asian, 68.7% of Native American/Pacific Islander, and 59.7% of white children.
More than 70% of Medicaid enrolled children with ASD in each race/ethnicity group billed at least one autism-related service outside of school (Supplementary Figure E2). The number of service claims outside of school ranged from an average of 24 for black children to 35 for Asian children (Supplementary Figure E3). The percentage of children with school-based services was much lower, and ranged from 21% of Native American/Pacific Islander to 31% of Asian children. The average number of school-based claims ranged from 7 to 10 per year.
Table 2 presents the unadjusted differences and IOM concordant disparities in the percentage of service use. Differences described as disparities are those where the minority children receive fewer services that white children, and this is assumed to represent a disadvantage for the minority child. IOM concordant estimates of outpatient service use revealed disadvantage for black, Asian, and Native American/Pacific Islander children compared with white children. Black children had rates of service use that were 5.2 percentage points lower than white children, while Asian children had rates 2.6 percentage points lower and Native American/Pacific Islander children had rates 3.7 percentage points lower. There were no significant disparities in use of school-based services. In contrast, black and Asian children had a rate of school-based service use that was 5.6 and 4.8 percentage points higher than white children respectively.
IOM concordant disparities in specific services varied considerably by type of service and race/ethnicity. The only type of services that consistently found minority disadvantage in the IOM concordant estimate were physical therapy, occupational therapy, and case management/care coordination services where only the latter had statistically significant disparities in three of four racial groups. Specifically, disparities in case management/care coordination ranged from 1.9 percentage points lower (black) to 8.3 percentage points lower (Asian). IOM concordant disparities were found in the use of 1-on-1 therapy or counselling services, and personal assistant or school aide services in three of the four race/ethnicity groups. Only Native American/Pacific Islander children had a disparity in speech therapy (−3.1%). In contrast, all other minority groups had significantly higher rates of speech therapy compared with white children.
IOM concordant disparities in the number of billed services are presented in Supplementary Table E3. Estimates for black children continue to reveal disadvantage in the number of billed services outside of school [mean −2.1, standard error (SE) 0.4] while there was no significant difference in the number of billed services between Latinx and Native American/Pacific Islander compared with white children. Asian children had significantly more outpatient services billed (mean 7.1, SE 1.5). Only Latinx children had a significant IOM concordant disparity in the average number of school-based services (mean −0.9, SE 0.3). IOM concordant mean numbers of billed case management and care coordination services revealed significant disadvantage in all four minority groups.
Decomposition
Table 3 presents the decomposition of outpatient service disparities for the three groups with significant IOM disparities in our primary logistic model. The coefficient describes the change in the minority white gap due to racial differences in the distribution of the variable and the percentage describes the coefficient as a percent of the minority-white gap. For example, 7.7% of the difference between black and white children in outpatient services use was accounted for by differences in the distribution of urban–rural county of residence. Put another way, if the distribution of urban–rural county of residence classification between black and white children were equalized, the difference in outpatient service use would be 7.7% smaller. State fixed effects accounted for the largest percentage of the minority-white gap indicating a significant contribution of unknown state characteristics.
Post-hoc Analysis
Table 4 presents the results of the IOM concordant estimates of service use stratified by large metro vs. small metro or non-metro county classification status. The disparity in outpatient service use for black children was driven largely by children living in large metro counties where the disparity compared to white children was −6.0% compared with a higher percentage of black children using services in small metro or non-metro counties (2.6%). The opposite was true for Native American/Pacific Islander children where only those living outside of large metro counties had a disparity (−7.5%). Although there were no overall disparities in school-based services we did find two significant disparities in the stratified analysis, both among children living in small metro or non-metro counties. Black children living in these areas had rates of school-based service use that were 4.4 percentage points lower than white children, while Latinx children had rates that were 6.8 percentage points lower.
Sensitivity Analyses
Three sensitivity analyses were performed for our main analysis of outpatient services and school-school based services (Supplementary Table E4). Among black and Native American/Pacific Islander children, outpatient disparities remained in estimates that included children with only FFS claims. Latinx children on the other hand had a large disparity (−6.0%) when children with only FFS claims were used to estimate outpatient service use. There were no new disparities in estimates for school based services although most of the differences in service use increased when based on children with only FFS claims.
Analysis 2 examined the impact of relaxing the diagnosis requirement on the service claims such that any claim for that type of service was used to measure disparities. For black–white and Native American/Pacific Islander–white outpatient disparities the size of the disparity decreased but remained statistically significant (−2.8% black–white and −1.7% Native American/Pacific Islander–white, p < 0.001). With respect to school-based services, a new Native American/Pacific Islander–white emerged when using claims with any diagnosis (−9.5%). Analysis 3 treated gender as a non-need factor. There were no substantive differences with this assumption.
Discussion
Significant racial and ethnic disparities in autism-related services were found among Medicaid enrolled children with ASD. Black, Asian, and Native American/Pacific Islanders received fewer outpatient, autism-related services compared with white children, but there was no disparity among Latinx children. There were no disparities in school-based services. To our surprise black and Asian children received more services than white children in the school setting. Disparities in case management/care coordination services were largest; there was a significant 8.3, 7.3, and 1.9 percentage point disparity for Asian, Latinx, and black children respectively. In stratified analyses, we found a disparity for black children (6 percentage points) in outpatient services for children living in large metro areas.
Our empirical strategy attempts to identify the origin of differences in received services. While the metro status of the county in which a child lives is associated with disparities, the measured characteristics including those captured in state-level fixed effects do not fully explain the differences we observe. Consistent with the IOM definition, we expect that unmeasured factors such as bias and discrimination, including interpersonal and structural racism, contribute to disparities. Structural racism refers to “the totality of ways in which societies foster racial discrimination through mutually reinforcing systems of housing, education, employment, earnings, benefits, credit, media, health care, and criminal justice”(Bailey et al. 2017). In this study, the downstream effects of structural racism may manifest in a variety of contexts including the school system, the Medicaid program, and the healthcare system. Although we could not identify differences in school billing practices in this study, the racial disparities that we observe could be a downstream consequence of structural racism in housing such that schools in poorer neighborhoods are incentivized to make up revenue gaps by billing Medicaid. In addition to structural barriers that promote racial disparities in service use, families bring with them the legacy of these experiences that may affect their preferences to pursue services to support their children with ASD.
When compared with white children, black children with ASD were 5.3% less likely to use outpatient autism related services but 5.6% more likely to use school-based services, a result driven by children living in large metro areas. One hypothesis to explain this substitution effect would be easier access and availability of school-based services compared with outpatient services in large metro counties with large concentrations of minority children. Although obtaining an individualized education plan to receive school-based services can be challenging for families (MacLeod et al. 2017; Salembier and Furney 1997), at least the process typically occurs in the building where a child attends school and requires no additional family travel. A second hypothesis is that the school context, including racial composition and fiscal resources, are associated with the propensity to place minority children in special education and possibly bill Medicaid for school-based services. There is a significant body of literature that has documented a higher likelihood of special education placement among minority children (National Research Council 2002; Zhang et al. 2014); however, recent studies have challenged this finding after more fully controlling for socioeconomic correlates, school context, and type of disability (Fish 2019; Morgan et al. 2017; Schussler et al. 2016). It is possible that the pattern of greater service use among black children stems in part from this legacy as well as variation in school-based Medicaid billing practices. Future research should examine the contribution of school context including racial composition and fiscal resources on disparities.
The other racial and ethnic groups in the study had mixed findings. Overall, there were no significant disparities in outpatient or school-based autism-related services among Latinx children; Latinx children were 0.6% more likely to receive outpatient services and just as likely to receive school-based service compared with white children. There were different patterns among Asian and Native American/Pacific Islander children. Asian children were less likely to receive outpatient services (−2.6%) but 4.8% more likely to receive school-based services compared with white children. Native American/Pacific Islander children had a disparity in the likelihood of outpatient services (−3.7%) but were equally likely to receive school-based services compared with white children. Although our overall findings did not support our hypothesis of widespread disparities across outpatient services among Latinx children, we did find disparities in occupational therapy consistent with some prior literature (Bilaver and Havlicek 2019; Harstad et al. 2013; Irvin et al. 2012; Magaña et al. 2016). However, we also found an increased likelihood of speech therapy, mental health/social skills/behavior modification services, and 1 on 1 therapy or counseling services not consistent with previous estimates in the general population (Bilaver and Havlicek 2019; Magaña et al. 2016). Although population-level research on service use among Asian, Native American, and Pacific Islander children with ASD is extremely limited, evidence from California’s Department of Developmental Services found greater per-person non-medical spending (including respite and day services) among Asian and “other” race/ethnicity children than Latinx and black children (Leigh et al. 2016). Qualitative studies of Asian immigrant parents of children with ASD reveal the influence of unique cultural, religious, and environmental factors that may influence service utilization (Shorey et al. 2020; Wang and Casillas 2013) as well as the challenges that limited language proficiency presents when trying to access quality autism-related services (Zuckerman et al. 2014). Our mixed findings for these groups of children suggest a more complex dynamic that requires further study to understand why population average patterns should increase use of some services but not others.
To our knowledge, disparities in case management/care coordination services for children with ASD have not been documented previously. The claims for children with ASD in this category of service consisted largely of both case management and target case management services. Case management refers broadly to services used to support recipients find medical or other services necessary for the treatment of a health condition while targeted case management (TCM) refers to services restricted to a specific groups of recipients (Binder 2008). There is a long history of legislative and regulatory action around the use of case management and TCM in the Medicaid program beginning in 1981. On March 3, 2008, a CMS rule became effective that clarified the use of TCM in both Medicaid waiver and non-waiver programs (Rosenbaum 2008). The rule was expected to reduce federal Medicaid expenditures by $1.28 billion between fiscal year (FY) 2008 and FY 2012 (Binder 2008). Because TCM refers to specific groups of recipients it is possible that certain racial and ethnic groups are overrepresented, and therefore less likely to receive TCM as a result of the rule change compared with white children. Future research needs to examine the extent to which inequitable use of case management and/or TCM contributes to disparities, as it is critical that all children with ASD have equal access to this important service.
Our findings must be interpreted within the context of a health system which has documented disparities in receiving an ASD diagnosis for racial and ethnic minorities. The Autism and Developmental Disabilities Monitoring (ADDM) Network, a collaboration tracking the number and characteristics of children with ASD across 16 US sites, has reported higher rate of white children identified with ASD than black or Latinx children, although black and white prevalence has equalized in the most recent report.(CDC 2018; Maenner 2020) This discrepancy may mean that minority children have more delays to diagnosis and fewer diagnoses overall and that those with fewer functional limitations are less likely to be diagnosed in racial/ethnic minority children. Our analysis cannot untangle systemic biases in assigning comorbidities, for example the potentially increased likelihood of a black child of receiving a diagnosis of intellectual disability or behavioral problems. It is also possible that these racial discrepancies impact case identification for ASD through diagnostic substitution, and therefore strategies to address racial inequities in diagnoses and supportive services must take a broad approach across developmental disabilities. Standardizing the diagnostic process for school-aged children and assigning appropriate services ought to include ready access to school-based and medically-based multidisciplinary assessment professionals in order to reduce disparities in diagnostic service access and avoid implicit biases.
This reality makes our empirical strategy all the more important. By controlling for comorbid conditions that may be associated with more significant limitations, we attempted to measure disparities after accounted for variation by race/ethnicity in these factors. Higher levels of functioning, however, may not be well distinguished by comorbidities. In our analysis, if the white population included more children with autism and no intellectual disability, this may explain why these children received fewer in-school services than minority children with ASD, as they may not have qualified for school-based services despite the general autism designation. For example, a child with autism who is at grade level, but who struggles with social nuance and relationships may not qualify for speech therapies in school, versus a child with autism who struggles with simple requesting or answering questions.
The concurrent analysis of school and outpatient services begs a provocative question about how school-based services are financed nationally. Part B of the IDEA covers funding for the education of all children with disabilities. These federal funds are intended to support, for example, children with autism to access education, which in many cases includes creating a behavioral plan and engaging in regular occupational and speech therapy services. However, educational funding is only in small part from the federal government; local school districts fund the majority. Therefore disparities in community resources for education may explain why some schools utilize the family medical insurance to cover education access instead of relying purely on educational funds. In most circumstances, this would have the negative impact of prohibiting families from accessing outpatient therapeutic services due to insurance limits on the quantity of services. Therefore, the observed increased access of school-based services may represent another type of hidden disparity for minority children. A detailed exploration about how special education and related services are financed, specifically autism-related services, would bolster support for children with disabilities in and out of the school system.
There are several limitations related to our analysis. First, claims data do not allow for clinical confirmation of the ASD diagnosis. Based on a previous validation study, the strategy that we employed is associated with a positive predictive value of 87.4% (Burke et al. 2014). Second, although the MAX data reflect a relatively harmonized claims database, quality control in all fields is lacking and led us to exclude some states from the analysis. For example, standard documentation and anomaly reports did not include information about the procedure code anomaly that we encountered in the New York state data. Data quality may also have impacted the categorization of service settings and types. Although we expected 44 states to have school-based Medicaid claims, we only found such claims in 27 states and excluded another two from the analysis based on an unbelievably low percentage of claims. Regarding service type categorization, we used multiple variables to help to identify relevant procedure codes, but we recognize that such a data driven procedure is subject to unmeasurable error. Finally, although the IOM definition includes patient preferences and discrimination, our data lacked specific measures of both. With respect to discrimination, our measured county-level characteristics only address the pathway between racism and discrimination and inadequate healthcare; however, racism can affect health care seeking behavior and thus service utilization for children with ASD through many other pathways not measured in this study (Bailey et al. 2017).
Balancing these limitations are the size and scope of our sample, our ability to examine multiple racial and ethnic groups, and our ability to examine school and outpatient settings in the same sample.
Conclusion
Within the Medicaid program, disparities in autism-related service use exists across all minority racial and ethnic groups although there is significant variation by type of service. School-based services are an important source of services for children with ASD and disparities in outpatient services appear to be ameliorated in school settings. Geographic variation in disparities suggest potential targets for policy intervention to achieve equal access to services.
References
Bailey, Z. D., Krieger, N., Agénor, M., Graves, J., Linos, N., & Bassett, M. T. (2017). Structural racism and health inequities in the USA: evidence and interventions. Lancet (London, England), 389(10077), 1453–1463. https://doi.org/10.1016/S0140-6736(17)30569-X.
Baller, J. B., & Barry, C. L. (2016). State variation in school-based disability services financed by Medicaid. Journal of Disability Policy Studies, 27(3), 148–157. https://doi.org/10.1177/1044207316637545.
Bilaver, L. A., & Havlicek, J. (2019). Racial and ethnic disparities in autism-related health and educational services. Journal of Developmental and Behavioral Pediatrics: JDBP. https://doi.org/10.1097/DBP.0000000000000700.
Binder, C. (2008). Medicaid targeted case management benefits (CRS Report for Congress No. RL34426).
Blinder, A. S. (1973). Wage discrimination: reduced form and structural estimates. The Journal of Human Resources, 8(4), 436–455. https://doi.org/10.2307/144855.
Broder-Fingert, S., Shui, A., Pulcini, C. D., Kurowski, D., & Perrin, J. M. (2013). Racial and ethnic differences in subspecialty service use by children with autism. Pediatrics, 132(1), 94–100. https://doi.org/10.1542/peds.2012-3886.
Burke, J. P., Jain, A., Yang, W., Kelly, J. P., Kaiser, M., Becker, L., et al. (2014). Does a claims diagnosis of autism mean a true case? Autism: The International Journal of Research and Practice, 18(3), 321–330. https://doi.org/10.1177/1362361312467709.
CDC. (2018, April 26). Racial and ethnic differences in children identified with ASD. Centers for Disease Control and Prevention. Retrieved March 13, 2020 from https://www.cdc.gov/ncbddd/autism/addm-community-report/differences-in-children.html.
Close, H. A., Lee, L.-C., Kaufmann, C. N., & Zimmerman, A. W. (2012). Co-occurring conditions and change in diagnosis in autism spectrum disorders. Pediatrics, 129(2), e305-316. https://doi.org/10.1542/peds.2011-1717.
Cook, B. L., McGuire, T. G., Lock, K., & Zaslavsky, A. M. (2010). Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health Services Research, 45(3), 825–847. https://doi.org/10.1111/j.1475-6773.2010.01100.x.
Cook, B. L., McGuire, T. G., & Zaslavsky, A. M. (2012). Measuring racial/ethnic disparities in health care: methods and practical issues. Health Services Research, 47(3 Pt 2), 1232–1254. https://doi.org/10.1111/j.1475-6773.2012.01387.x.
Education for All Handicapped Children’s Act. (1975). Pub. L. No. 94–142.
Efron, B. (1979). Bootstrap methods: another look at the jackknife. The Annals of Statistics, 7(1), 1–26. https://doi.org/10.1214/aos/1176344552.
Fairlie, R. W. (2005). An extension of the Blinder-Oaxaca decomposition technique to logit and probit models. Journal of Economic and Social Measurement, 30(4), 305–316.
Fairlie, R. W. (2017). Addressing path dependence and incorporating sample weights in the nonlinear Blinder-Oaxaca decomposition technique for logit, probit and other nonlinear models. SIEPR (Stanford Insitute for Economic Policy Research Discussion Paper No. 17-013). Retrieved December 5, 2017 from https://siepr.stanford.edu/research/publications/addressing-path-dependence-and-incorporating-sample-weights-nonlinear-blinder.
Fish, R. E. (2019). Standing out and sorting in: exploring the role of racial composition in racial disparities in special education. American Educational Research Journal, 56(6), 2573–2608. https://doi.org/10.3102/0002831219847966.
Frazier, T. W., Georgiades, S., Bishop, S. L., & Hardan, A. Y. (2014). Behavioral and cognitive characteristics of females and males with autism in the Simons simplex collection. Journal of the American Academy of Child and Adolescent Psychiatry, 53(3), 329-340.e1–3. https://doi.org/10.1016/j.jaac.2013.12.004.
Harstad, E., Huntington, N., Bacic, J., & Barbaresi, W. (2013). Disparity of care for children with parent-reported autism spectrum disorders. Academic Pediatrics, 13(4), 334–339. https://doi.org/10.1016/j.acap.2013.03.010.
Hart, L. G., Larson, E. H., & Lishner, D. M. (2005). Rural definitions for health policy and research. American Journal of Public Health, 95(7), 1149–1155. https://doi.org/10.2105/AJPH.2004.042432.
Healthcare Cost and Utilization Project-HCUP. (2014). Clinical classifications software 2014. Agency for Healthcare Research and Quality.
Individual with Disabilities Education Act. (1990). Pub. L. No. 101-476.
Individual with Disabilities Education Act. (1997). Pub. L. No. 101-157.
Institute of Medicine. (2003). Unequal treatment: confronting racial and ethnic disparities in health care. In B. D. Smedley, A. Y. Stith, & A. R. Nelson (Eds.). Washington DC: National Academies Press.
Irvin, D. W., McBee, M., Boyd, B. A., Hume, K., & Odom, S. L. (2012). Child and family factors associated with the use of services for preschoolers with autism spectrum disorder. Research in Autism Spectrum Disorders, 6(1), 565–572. https://doi.org/10.1016/j.rasd.2011.07.018.
Jann, B. (2008). FAIRLIE: Stata module to generate nonlinear decomposition of binary outcome differentials. Boston College Department of Economics. Retrieved December 5, 2017 from https://ideas.repec.org/c/boc/bocode/s456727.html.
LaClair, M., Mandell, D. S., Dick, A. W., Iskandarani, K., Stein, B. D., & Leslie, D. L. (2019). The effect of Medicaid waivers on ameliorating racial/ethnic disparities among children with autism. Health Services Research, 54(4), 912–919. https://doi.org/10.1111/1475-6773.13176.
Leigh, J. P., Grosse, S. D., Cassady, D., Melnikow, J., & Hertz-Picciotto, I. (2016). Spending by California’s department of developmental services for persons with autism across demographic and expenditure categories. PLoS ONE, 11(3), e0151970. https://doi.org/10.1371/journal.pone.0151970.
Liptak, G. S., Benzoni, L. B., Mruzek, D. W., Nolan, K. W., Thingvoll, M. A., Wade, C. M., & Fryer, G. E. (2008). Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children’s Health. Journal of Developmental and Behavioral Pediatrics: JDBP, 29(3), 152–160. https://doi.org/10.1097/DBP.0b013e318165c7a0.
MacLeod, K., Causton, J. N., Radel, M., & Radel, P. (2017). Rethinking the individualized education plan process: voices from the other side of the table. Disability and Society, 32(3), 381–400. https://doi.org/10.1080/09687599.2017.1294048.
Maenner, M. J. (2020). Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 Sites, United States, 2016. MMWR. Surveillance Summaries, 69. https://doi.org/https://doi.org/10.15585/mmwr.ss6904a1.
Magaña, S., Lopez, K., Aguinaga, A., & Morton, H. (2013). Access to diagnosis and treatment services among latino children with autism spectrum disorders. Intellectual and Developmental Disabilities, 51(3), 141–153. https://doi.org/10.1352/1934-9556-51.3.141.
Magaña, S., Parish, S. L., Rose, R. A., Timberlake, M., & Swaine, J. G. (2012). Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellectual and Developmental Disabilities, 50(4), 287–299. https://doi.org/10.1352/1934-9556-50.4.287.
Magaña, S., Parish, S. L., & Son, E. (2016). Functional severity and Latino ethnicity in specialty services for children with autism spectrum disorder. Journal of Intellectual Disability Research: JIDR, 60(5), 424–434. https://doi.org/10.1111/jir.12293.
Mandell, D. S., Listerud, J., Levy, S., & Pinto-Martin, J. (2002). Race differences in the age at diagnosis among Medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 41(12), 1447–1453. https://doi.org/10.1097/00004583-200212000-00016.
Mandell, D. S., Morales, K. H., Xie, M., Polsky, D., Stahmer, A., & Marcus, S. C. (2010). County-level variation in the prevalence of Medicaid-enrolled children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(10), 1241–1246. https://doi.org/10.1007/s10803-010-0982-2.
Mandell, D. S., Xie, M., Morales, K. H., Lawer, L., McCarthy, M., & Marcus, S. C. (2012). The interplay of outpatient services and psychiatric hospitalization among Medicaid-enrolled children with autism spectrum disorders. Archives of Pediatrics and Adolescent Medicine, 166(1), 68–73. https://doi.org/10.1001/archpediatrics.2011.714.
McGuire, T. G., Alegria, M., Cook, B. L., Wells, K. B., & Zaslavsky, A. M. (2006). Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Services Research, 41(5), 1979–2005. https://doi.org/10.1111/j.1475-6773.2006.00583.x.
Morgan, P. L., Farkas, G., Hillemeier, M. M., & Maczuga, S. (2017). Replicated evidence of racial and ethnic disparities in disability identification in U.S. schools. Educational Researcher, 46(6), 305–322. https://doi.org/10.3102/0013189X17726282.
National Research Council. (2002). Minority students in special and gifted education. Washington, DC: The National Academies Press. https://doi.org/10.17226/10128.
Oaxaca, R. (1973). Male–female wage differentials in urban labor markets. International Economic Review, 14(3), 693–709. https://doi.org/10.2307/2525981.
Rosenbaum, S. (2008). The CMS Medicaid targeted case management rule: implications for special needs service providers and programs—advancingstates.org. Center for Health Care Strategies. Retrieved April 9, 2020 from http://www.advancingstates.org/hcbs/article/cms-medicaid-targeted-case-management-rule-implications-special-needs-service-providers.
Salembier, G., & Furney, K. S. (1997). Facilitating participation: parents’ perceptions of their involvement in the IEP/transition planning process. Career Development for Exceptional Individuals, 20(1), 29–42. https://doi.org/10.1177/088572889702000103.
Schussler D. L., Morgan P. L., Farkas G., Cook M., Strassfeld N. M., Hillemeier M. M., Pun W. H. (2016). Are black children disproportionately overrepresented in special education? A best-evidence synthesis—Paul L. Morgan, George Farkas, Michael Cook, Natasha M. Strassfeld, Marianne M. Hillemeier, Wik Hung Pun, Deborah L. Schussler, 2017. Exceptional children. http://journals.sagepub.com/doi/https://doi.org/10.1177/0014402916664042
Shorey, S., Ng, E. D., Haugan, G., & Law, E. (2020). The parenting experiences and needs of Asian primary caregivers of children with autism: a meta-synthesis. Autism: The International Journal of Research and Practice, 24(3), 591–604. https://doi.org/10.1177/1362361319886513.
Smith, K. A., Gehricke, J.-G., Iadarola, S., Wolfe, A., & Kuhlthau, K. A. (2020). Disparities in service use among children with autism: a systematic review. Pediatrics, 145(Suppl 1), S35–S46. https://doi.org/10.1542/peds.2019-1895G.
Wang, H.-T., & Casillas, N. (2013). Asian American parents’ experiences of raising children with autism: multicultural family perspective. Journal of Asian and African Studies, 48(5), 594–606. https://doi.org/10.1177/0021909612467421.
Werling, D. M., & Geschwind, D. H. (2013). Sex differences in autism spectrum disorders. Current Opinion in Neurology, 26(2), 146–153. https://doi.org/10.1097/WCO.0b013e32835ee548.
Zhang, D., Katsiyannis, A., Ju, S., & Roberts, E. (2014). Minority representation in special education: 5-year trends. Journal of Child and Family Studies, 23(1), 118–127. https://doi.org/10.1007/s10826-012-9698-6.
Zuckerman, K. E., Mattox, K., Donelan, K., Batbayar, O., Baghaee, A., & Bethell, C. (2013). Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics, 132(3), 445–453. https://doi.org/10.1542/peds.2013-0383.
Zuckerman, K. E., Sinche, B., Mejia, A., Cobian, M., Becker, T., & Nicolaidis, C. (2014). Latino parents’ perspectives on barriers to autism diagnosis. Academic Pediatrics, 14(3), 301–308. https://doi.org/10.1016/j.acap.2013.12.004.
Zuckerman, K. E., Lindly, O. J., & Sinche, B. (2016). Parent beliefs about the causes of learning and developmental problems among children with autism spectrum disorder: results from a national survey. American Journal on Intellectual and Developmental Disabilities, 121(5), 432–447. https://doi.org/10.1352/1944-7558-121.5.432.
Zuckerman, K. E., Lindly, O. J., Reyes, N. M., Chavez, A. E., Macias, K., Smith, K. N., & Reynolds, A. (2017). Disparities in diagnosis and treatment of autism in Latino and non-Latino white families. Pediatrics, 139(5), e20163010. https://doi.org/10.1542/peds.2016-3010.
Acknowledgments
The authors acknowledge funding from the Health Resources and Services Administration (R40MC288550100) and would like to thank Dr. Benjamin Lê Cook for his methodological guidance.
Author information
Authors and Affiliations
Contributions
LB conceived of the study, participated in its design, performed the statistical analysis, and drafted the manuscript; SS participated in the interpretation of the data and helped to draft the manuscript; DM participated in the design of the study, interpretation of the data, and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This project was determined to be exempt by the institutional review board at Northwestern University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bilaver, L.A., Sobotka, S.A. & Mandell, D.S. Understanding Racial and Ethnic Disparities in Autism-Related Service Use Among Medicaid-Enrolled Children. J Autism Dev Disord 51, 3341–3355 (2021). https://doi.org/10.1007/s10803-020-04797-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-020-04797-6