Abstract
Having a consistent source of medical care may facilitate diagnosis of autism spectrum disorders (ASD). This study examined predictors of age of ASD diagnosis using data from the 2011–2012 National Survey of Children’s Health. Using multiple linear regression analysis, age of diagnosis was predicted by race, ASD severity, having a consistent source of care (CSC), and the interaction between these variables after controlling for birth cohort, birth order, poverty level, parental education, and health insurance. While African American children were diagnosed earlier than Caucasians, this effect was moderated by ASD severity and CSC. Having a CSC predicted earlier diagnosis for Caucasian but not African American children. Both physician and parent behaviors may contribute to diagnostic delays in minority children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prevalence of autism spectrum disorders (ASD) has risen immensely in the last 25 years, in large part due to increases in public awareness of parents and healthcare providers (Fountain et al. 2011). The Centers for Disease Control and Prevention (CDC) reported a 78 % increase in ASD diagnosis between the years of 2002 and 2008. Current estimates indicate that one in 68 children, and one in every 42 boys will be diagnosed with an ASD (Centers for Disease Control and Prevention 2014).
ASDs are increasingly costly to both families and society as a whole. The lifetime cost of supporting a person with ASD has been estimated at 2.4 million dollars for patients with intellectual disability, and 1.4 million dollars for those without (Buescher et al. 2014). Societal costs are correspondingly high. Treatment of ASD costs the United States 175 billion dollars per year—more than cancer, stroke, and heart disease combined (Buescher et al. 2014).
Early intervention is particularly important for reducing intellectual, behavioral, and functional impairments (Fountain et al. 2011; Rogers and Vismara 2008). Children who benefit from high-quality, early behavioral intervention have significantly better outcomes than those treated later. They demonstrate better developmental functioning, fewer maladaptive behaviors, lower symptom severity, improved language and socio-emotional skills, reduced intellectual impairment, and higher IQ and Vineland Adaptive Behavior Composite scores both in the short and long term (Eldevik et al. 2009; Rogers and Vismara 2008; Vismara and Rogers 2010). Correspondingly, improvements in IQ in childhood predict better prognosis in peer relationships, education, vocational training, employment, and independent living (Billstedt et al. 2005). As a result, not only is early and accurate diagnosis critical to effective interventions, it can directly minimize functional impairment and, subsequently, associated costs to society.
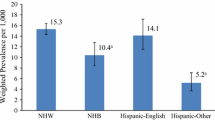
Given the rise in prevalence and visibility of autism, age of initial diagnosis has generally decreased (Hertz-Picciotto and Delwiche 2009). Diagnosis of ASD has historically been influenced by certain demographic variables. Children of privileged and/or Caucasian families have been overrepresented, and families of lower socioeconomic status (SES) and of minority racial and ethnic backgrounds have traditionally been underdiagnosed (Durkin et al. 2010; Fountain et al. 2011). Although community awareness of ASD has begun to reduce these racial and socioeconomic disparities, group differences remain (CDC 2014; Gourdine and Algood 2014; Pedersen et al. 2012; Zuckerman et al. 2013).
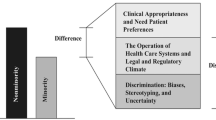
To better understand racial disparities in ASD diagnosis, it is important to evaluate demographic barriers involved in access to healthcare. In the United States, SES proves to be the most powerful determinant of primary health care use, with race being a close and related second (Fiscella et al. 2014). Persons of low SES are at risk for lower quality ambulatory and emergency care (Fiscella et al. 2014), worse overall health (Adler and Rehkopf 2008), higher morbidity and mortality (Adler and Stewart 2010), and they are less likely to have a regular source of care (DeVoe et al. 2007, 2008). Racial health disparities are equally pervasive and persistent in adult (Fiscella et al. 2014) and pediatric care (Flores 2010). Minority children are less likely to have had a recent physician visit (Flores and Lin 2013) or a medical home, which includes having a consistent source of care (CSC; Raphael et al. 2009; Strickland et al. 2009). Similar racial disparities are also observed in mental health care where minority children receive less outpatient mental health care and psychotropic medication than Caucasian children (Cook et al. 2013). These children are also less likely to use mental health services (Coker et al. 2009) or to be referred to specialty care, even after controlling for health insurance status (Kenney et al. 2013). Finally, independent of SES and race, health insurance is also an important determinant of health care use. Uninsured children are less likely to have a usual source of care or to have seen a physician in the recent past, and more likely to have unmet healthcare needs in terms of both treatment and preventative care (Cummings et al. 2009; DeVoe et al. 2009).
Although having health insurance is strongly associated with access to primary care (Cummings et al. 2009), healthcare access does not equate to healthcare utilization (Starfield and Shi 2004). Families that are insured do not necessarily use the services at their disposal due to barriers such as employment, language, education, and location (Chan et al. 2006; Devoe et al. 2007; Zuvekas and Taliaferro 2003). For instance, insured low SES individuals use fewer healthcare services than their higher SES counterparts (Fiscella et al. 2002). Likewise, insured Hispanic and African American children are less likely to receive specialty and mental health care than insured Caucasian children (Kenney et al. 2013). Taking into account confounds between demographic variables and insurance, having a consistent source of medical care may be an equally important, if not better, determinant of health care utilization as health care insurance (Blackwell et al. 2009; DeVoe et al. 2008; Gill et al. 2000; Lillie-Blanton and Hoffman 2005).
In ASD specifically, having a consistent source of medical care may improve the likelihood that pediatricians, who see children regularly for scheduled preventive care visits during their first 3 years of life, notice developmental abnormalities (Pinto-Martin et al. 2008; Sices 2007). Since 2006, the American Academy of Pediatrics (AAP) has implemented guidelines to more accurately screen for developmental abnormalities. Pediatricians are instructed to perform a routine developmental screening at nine, 18, and 24 months, and to conduct an additional autism-specific screening at 18 and 24 months (Bright Futures Steering Committee and Medical Home Initiatives for Children with Special Needs Project Advisory Committee 2006; Johnson and Myers 2007).
Referral to specialty care is subsequently recommended for children who use no spontaneous two-word phrases by 2 years of age or who display language or social regressions (Barbaresi et al. 2006). Although similar guidelines were recommended earlier by the American Academy of Neurology (Filipek et al. 2000), surveillance was the AAP recommendation until 2006. The 2006 AAP guidelines were developed to ensure widespread adoption by outlining implementation strategies for various primary care settings (King et al. 2010).
Even with regular primary care and an appropriate specialty care referral, however, the road to diagnosis is often an arduous one. Reports of diagnostic experiences by parents highlight the difficulty in obtaining a definite diagnosis (Goin-Kochel et al. 2006; Keenan et al. 2010). Both symptom heterogeneity and physician uncertainity contribute to diagnostic delays (Goin-Kochel et al. 2006). Although half of parents recall concerns dating back to the first years of life (Zwaigenbaum et al. 2013), there may be a gap of several years between first noticing developmental delays and the confirmation of a diagnosis (Sansosti et al. 2012; Shattuck et al. 2009).
Both physician and parent factors influence diagnosis. Lack of universal screening by primary care practitioners (PCP) may contribute to diagnostic delays. A study by Dosreis et al. (2006) revealed that, while 44 % of the sampled doctors served ASD patients, only 8 % regularly screened for the disorder. Meanwhile, relying on parents to elicit concerns also has consequences. In a controlled trial of ASD screening in primary care, 75 % of parents with children who screened positive for an ASD had not suspected it (Pinto-Martin et al. 2008). Despite these hindrances, consultation with PCPs still remains the crucial first step in the diagnostic process. Most parents express their initial concerns to their child’s pediatrician and rely on the advice they receive to determine follow-up (Barbaresi et al. 2006). Given the importance of primary care in identifying symptoms and referring to specialists, the goal of the current study was to determine whether having a CSC predicted timeliness of ASD diagnosis.
The study tested the following hypotheses. We anticipated that families without a CSC would have children diagnosed at a later age. Given documented disparities in medical practice for ASD, we also expected that children of color would be diagnosed later than their Caucasian peers. With the implication that more severe symptoms would be recognized earlier, we expected autism severity to be negatively related to age of diagnosis. Finally, we posited that the impact of having a CSC on age of diagnosis would depend on both race and autism severity. Given that children with mild forms of ASD tend to wait considerably longer for a diagnosis (Fountain et al. 2011), we presumed that having a CSC would facilitate diagnosis of more severe forms of ASD but not of mild ASD. We also expected the effect of a CSC to be moderated by racial disparities such that being from an ethnic or racial minority would minimize the benefits of a CSC on timeliness of ASD diagnosis.
Since other demographic variables may impact age of ASD diagnosis (Herlihy et al. 2014), we controlled for poverty level, parental education, current health insurance status, and whether children were born before or after the implementation of the 2006 AAP screening guidelines (hereafter referred to as birth cohort). We also included birth order under the assumption that first-time parents would likely recognize ASD later due to less familiarity with typical child development (Fountain et al. 2011).
Methods
Participants
Data were obtained from the CDC National Survey of Children’s Health (NSCH) 2011. The sample consisted of parents or guardians of children between the ages of 0 and 17 (M = 8.85, SD = 5.237). The adult in the household most knowledgeable about the child’s health was asked to complete the phone survey. In total, 96,677 child-level interviews were conducted. Of the respondents, 69.5 % were mothers, 21.8 % were fathers, and 8.3 % were other family members or guardians. Of children old enough to receive an ASD diagnosis, 2-years old or older, 1.7 % of children in the sample had an ASD (N = 1624). Twenty-one percent of parents reported receiving the diagnosis from their child’s PCP; the rest received the diagnosis from a variety of specialists. Table 1 contains additional demographic information about the sample of children with ASD. Table 2 includes information about the survey respondents: parents and guardians.
Procedures
The national cross-sectional survey was conducted via random-digit-dialed telephones, both landline and mobile, between February 2011 and June 2012, using the sampling frame of the National Immunization Survey (CDC 2013). The overall response rate to the survey was 23 %; the completion rate was 54.1 % for landline and 41.2 % for mobile phone interviews (Visser et al. 2014). The interview was based on previous surveys conducted by the CDC in 2003 and 2007 using similar questions and methods (Blumberg et al. 2012).
Measures
Publicly available data files and methodology reports from the 2011–2012 National Survey of Children’s Health were used to test research questions. The purpose of the NSCH was to collect information on children’s health, including physical and mental health status, access to health care, information on the child’s family, neighborhood, and social context (CDC 2013). Collected demographic information included child sex, race and ethnicity, parental education, primary language spoken in the home, and poverty level.
As part of the survey, the responding parent was asked whether the selected child had any of the following diagnoses: Attention Deficit Disorder or Attention Deficit Hyperactive Disorder, depression, anxiety problems, behavior or conduct problems, autism, Asperger’s Disorder, pervasive development disorder, or other ASD, any developmental delay, intellectual disability or mental retardation, or Tourette Syndrome.
The current study focused on the answers of parents who answered affirmatively to: “Does [CHILD’S NAME] currently have autism or autism spectrum disorder?” Subsequently, parents were asked, “How old was [CHILD’S NAME] when you were first told by a doctor or other health care provider that (he/she) had [CONDITION]?” and “Would you describe (his/her) condition as mild, moderate, or severe?” The other question of interest was: “Is there a place that [CHILD’S NAME] USUALLY goes when [he/she] is sick or you need advice about [his/her] health?” hereafter referred to as CSC.
Statistical Analysis
Prior to running the multiple linear regression, we checked for and confirmed that the assumptions of linearity, normality, and multicollinearity of multiple linear regression had not been violated. A hierarchical multiple linear regression analysis was used to examine the relative contributions of birth cohort, birth order, poverty level, parental education, insurance status, race, ASD severity, and CSC on age of initial ASD diagnosis. We also examined all two- and three-way interactions among race, ASD severity, and CSC on age of diagnosis.
To calculate the effect of the 2006 AAP guidelines on age of diagnosis, we split the data set into two birth cohorts, pre- and post-2006. We first calculated year of birth based on the child’s age at time of interview. Since survey date was not available in the current dataset, a 2-year birth range was estimated based on the data collection date range: 2011–2012. The variable was then dummy coded into pre- and post-2006 birth years, using pre-2006 as the reference group.
Birth order was originally coded categorically as only child, first born, second born, third born, and fourth born. For the purpose of this study, this variable was dichotomized and dummy coded into first born/only child, and younger sibling. To examine the effect of health insurance, we constructed contrast codes to compare insured to uninsured children, and publicly insured to privately insured children.
Household income was collected during the survey but not available in the public dataset. Instead, income was translated into percentage of the Federal Poverty Level (FPL). The continuous variable was originally coded on a four-point Likert scale from 1 representing “0–99 % FPL” to 4 representing “400 % FPL or greater.” In the current study, this item was reverse coded and centered on the mean to facilitate interpretation. Parental education was measured using three categories: “less than high school,” “high school,” and “more than high school.” The highest level of education of either parent or guardian was chosen to estimate the effect of parental education. The variable was subsequently dummy coded, using the most common educational level as the reference group: more than high school.
Both race and ASD severity were dummy coded, using Caucasian and mild ASD as reference groups, respectively. Information about child race was derived from a variable that coded race as follows: Hispanic, White non-Hispanic, Black non-Hispanic (referred to as African American in text), and multiracial/other non-Hispanic. The multiracial/other category consisted of children who reported more than one race (multiracial) or only one race category of Asian, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander (other) (CDC 2013).
Consistent source of care was categorically coded 0 for having no CSC, and 1 for having a CSC. The outcome variable, age of initial ASD diagnosis, was originally collected in both months and years. To facilitate analysis, cases measured in years were recalculated in terms of months. Cases that listed age of diagnosis as 0 months were coded as missing. Given that most diagnoses of ASD do not occur before 1 year of age (Matson et al. 2008), cases that listed age of diagnosis as occurring before 1 year old were recoded as 12 months.
Results
The optimal linear combination of birth cohort, birth order, poverty level, parental education, insurance status, race, ASD severity, and CSC, and the interaction of the latter three variables accounted for 16 % of the variance in age of initial diagnosis, adjusted R 2 = 0.16, F(24, 1533) = 13.38, p < .001. Birth cohort, birth order, poverty level, race, and ASD severity all independently predicted age of diagnosis. Average age of diagnosis was 64.65 months (SD = 41.03). While birth cohort predicted age of ASD diagnosis, children born in or after 2006 were significantly younger (M = 4.15, SD = 0.936) than children born before 2006 (M = 11.52, SD = 3.29), t(1622) = 33.83, p < .001.
The direction of the race predictor was not in the expected direction. While we assumed that Caucasian children would be diagnosed earliest, given racial disparities in diagnosis, being of Hispanic descent significantly predicted earlier diagnosis (b = −25.83, 95 % CI [−50.62, −1.04], p < .05). On average, ethnic minority children (Hispanic M = 57.06, SD = 37.00; African American M = 50.89, SD = 35.76; multiracial/other M = 58.05, SD = 38.78) were diagnosed earlier than Caucasian children in the sample (M = 68.24, SD = 41.95).
We also found that condition severity predicted diagnosis age, with moderate ASD being diagnosed earlier than mild and severe forms of autism (Moderate ASD: b = −24.94, 95 % CI [−44.52, −5.37], p < .05). In terms of control variables, being a younger sibling significantly predicted earlier diagnosis (b = −11.44, 95 % CI [−15.72, −7.17], p < .001). Neither parental education, health insurance status nor CSC independently predicted age of diagnosis, p > .05.
Main effects were qualified by three-way interactions, such that the effect of one predictor on age of initial diagnosis was dependent on the levels of the two other predictors in the interaction. Two of the six three-way interaction terms were statistically significant, both of which involved African American children (CSC × Moderate ASD × AA: t(1) = 2.58 95 % CI [5.12, 37.55], p < .05; CSC × Severe ASD × AA: t(1) = 2.10, 95 % CI [1.46, 44.60], p < .05). None of the two-way interactions between CSC and race or between CSC and ASD proved significant, p > .05.
The three-way interaction indicated that the effect of having a CSC depended on race and ASD severity. Contrary to our hypothesis, having a CSC was not consistently predictive of earlier diagnosis. In African American families, children who had a CSC were diagnosed later than those without (Fig. 1). In contrast, while Caucasian children were diagnosed later than Hispanic and African American counterparts in general, those with a CSC were diagnosed earlier than those without, regardless of ASD severity (Fig. 2). Of note, diagnostician type significantly differed by race, χ2(33, N = 1577) = 73.8, p < .001. While only 18.7 % of Caucasian children were diagnosed in primary care, 36.8 % of African American children were diagnosed by a PCP. Results of the multiple regression model are presented in Table 3.
Discussion
The goal of the current study was to examine the effects of birth cohort, birth order, poverty level, parental education, health insurance, race, ASD severity and CSC, and the interactions between race, ASD severity, and CSC on age of initial ASD diagnosis. We predicted that, after controlling for birth cohort, birth order, poverty level, parental education, and health insurance, having a CSC would be associated with younger age at time of initial diagnosis. We expected that autism severity would independently influence age of diagnosis, such that more severe symptomatology would yield earlier diagnosis. We also anticipated that children of minority racial or ethnic categories would be diagnosed later than Caucasian children. Finally, we predicted that the relationship between having a CSC and age of diagnosis would depend on both race and ASD severity.
Birth cohort was an important predictor of ASD diagnosis. Children born in or after 2006 (the year AAP guidelines were published) were diagnosed on average 35 months earlier than those born between 1994 and 2005. Compared to the 2014 CDC report, which reported an average age of diagnosis at 53 months for children born pre-AAP implementation, this suggests a noteworthy improvement in the diagnostic process (CDC 2014). However, while this may indicate that nationwide implementation of ASD screening guidelines improved screening and precipitated diagnosis, children in the later cohort were also significantly younger. Given that children born in or after 2006 were so young, they may represent the optimally diagnosed. As a result, interpretation of this effect should be made cautiously. Moreover, research on the success of AAP guideline implementation has produced mixed evidence. While most primary care practices increased their structured screening of ASD, referral of children who screened positive was inconsistent. In a study examining outcomes of the AAP screening guidelines, King et al. (2010) found that more than one-third of children who failed the screen were not referred to specialty care. Moreover, doctors that did refer patients to specialists found that many families failed to follow-up with recommended referrals (King et al. 2010). Consequently, conclusions drawn from the considerable effect size of the cohort predictor may not be solely attributable to AAP guideline implementation. Instead, we can speculate that increases in parental and physician awareness of ASD have also contributed to earlier identification and diagnosis seeking (Fountain et al. 2011; Hertz-Picciotto and Delwiche 2009). We can also postulate that age differences contributed to the magnitude of the measured effect.
Two other covariates significantly predicted age of ASD diagnosis. First, being a younger sibling was associated with earlier diagnosis. Parents’ familiarity with early warning signs of ASD likely explains this effect. Second, poverty level predicted diagnostic age, such that more impoverished children were diagnosed later than wealthier children. As suggested by the literature, families of lower SES are less likely to have a regular source of care and to receive routine medical supervision (DeVoe et al. 2007, 2008) even after controlling for health insurance (Fiscella et al. 2002). Moreover, families of lower SES may encounter additional economic and environmental barriers following referral to specialty care, given an increased likelihood of financial difficulties to afford medical copayments, time off work, and childcare for other family members (Kuhlthau et al. 2004). Consequently, the main effect of poverty level may reflect both pre- and post-consultation disparities. In contrast, while we expected that parental education would have an impact on diagnostic age, the current sample was better educated than that of the average United States citizen, which may explain the lack of anticipated findings.
In terms of interaction effects, the relationship between having a CSC and age of initial diagnosis depended on race. While having a CSC prompted earlier ASD diagnosis in Caucasian children, it delayed diagnosis for African American children. This racial disparity in children who have a CSC suggests two possibilities: race-based differences in practitioner and/or parent behavior.
One theory is that these two groups may be treated differently by physicians when first reporting ASD symptoms. That is, physicians may not refer African American children to specialists at the same rate or with the same speed as they refer other patients. Given that PCPs were only responsible for one-fifth of ASD diagnoses in the sample, and that this number is likely to be an overestimate because parents may be recalling first concern by any medical professional, we can assume that a majority of children were referred to, and eventually diagnosed by, a specialist: psychologist, psychiatrist or other. Racial disparities in referral practices are well documented and have been stable over decades, indicating a reliable difference in referral practices across medical specialty and time (Cook et al. 2009; Murphy et al. 2009; Harstad et al. 2013; Steyerberg et al. 2007). This disparity has also been documented in child healthcare (Boss et al. 2011; Mayer et al. 2004; Shields et al. 2004; Toomey et al. 2013; Zimmerman 2005).
Diagnostic disparities seen in the literature were also observed in the current sample. Diagnostician type significantly differed by race. While only one in five Caucasian children were diagnosed in primary care, over a third of African American children were diagnosed by a primary physician. This latter percentage is much larger than the average estimated in Goin-Kochel et al.’s (2006) study of sources of final, confirmatory ASD diagnoses, which estimated that only 15 % of ASD diagnoses were determined by a pediatrician or general physician, a team of professionals or another health practitioner. Although errors in parent recall of diagnostic timing may have influenced our results, we may nonetheless conclude with some caution that slower or less frequent referrals to the appropriate specialist may have delayed diagnosis of African American children presenting to their regular physician with moderate and severe ASD symptoms. This finding is concerning considering that children with more severe symptomatology ASD are likely to display more noticeable pathological symptoms.
While discrimination in referral practice may be one factor that influences decisions to refer to specialty care, primary care physicians may also be slower to recognize ASD in minority children due to differences in ASD presentations. Sell et al. (2012) found that African American children had higher rates of object preoccupations and inflexible routines, while Caucasian children demonstrated more unusual sensory stimuli preoccupations and abnormal motor development. Becerra et al. (2014) found that ethnic minority children were more likely to display ASD phenotypes with severe emotional outbursts and impaired expressive language than Caucasian children. Consequently, primary care physicians trained to identify typical or common ASD presentations may overlook minority children displaying phenotypic differences.
Nonetheless, the above explanation fails to explain why African American children with moderate and severe ASD who had a CSC were diagnosed later than their counterparts who had no regular place of medical care. One possibility is that children without a CSC tend to come from poorer homes that qualify for programs such as Head Start, which mandate regular tracking of developmental and educational progress of students. Likewise, minority children without a CSC may be more likely to attend low-cost Medicaid-eligible clinics that mandate Early and Periodic Screening, Diagnosis, and Treatment (EPSDT). In fact, Daniels and Mandell (2013) found that children from states with higher EPSDT compliance rates were diagnosed earlier than those with lower compliance.
However, the sample demonstrated no significant difference in poverty level between African American children who have a CSC those who do not. African American children from families that earned 0–199 % of the FPL were equally as likely to endorse having a CSC as children in the 200–400 % group (94.05 vs. 95 % respectively). This therefore minimizes the chance that African American children without a CSC were more likely to benefit from EPSDT or other federally mandated public program screenings.
Given that income differences are unlikely to fully explain diagnostic disparities in the current study, we may posit that primary physicians simply may not be recognizing the appropriate warning signs in African American children. The most recent CDC prevalence report reveals that Non-Hispanic White children were 30 % more likely to receive an ASD diagnosis than non-Hispanic Black children. However, of those diagnosed with an ASD, only 25 % of White children were classified in the range of intellectual disability, compared to 48 % of non-Hispanic Black children and 38 % of Hispanic children (CDC 2014). Following this logic, minority children may be suspected of having an intellectual disability or other psychopathology before the ASD diagnosis is eventually decided.
Insurance type may be another factor implicated in race-based differences in the diagnosis of children with a CSC. Access to outpatient specialty care has been shown to be limited for publicly insured children, likely due to specialists’ reluctance to accept public health insurance (Bisgaier and Rhodes 2011). However, comparison of public versus private health insurance failed to demonstrate significant differences in age of ASD diagnosis in our sample.
Another possibility is that the difference between groups lies at the patient rather than at the physician level. First, a CSC may mean different things across demographic groups. African Americans and Latinos are more likely to identify an emergency department as their primary source of care (Baker et al. 1994). Since patients who rely on emergency services tend to have 25 % fewer physician visits, this may explain the observed race-based discrepancy in children with a CSC (Baker et al. 1994).
Second, patient perception of discrimination may also promote consultation delays. In general, African, Hispanic and Asian American patients report more perceived provider discrimination and poorer health than Caucasians (Lee et al. 2009). Perceived discrimination has been shown to predict a variety of negative health behaviors. Perceived bias is related to underutilization of medical care even after controlling for socio-demographic characteristics, health care access, and physical and mental health (Burgess et al. 2008). It has also been tied to delays of medical tests and treatments (Casagrande et al. 2007; Facione and Facione 2007; Wagner and Abbott 2007), avoidance of preventative services (Trivedi and Ayanian 2006), and avoidance of alternative care options (Bazargan et al. 2005). As a result, minority patients treated by doctors they perceive as discriminatory may delay ASD consultation for their child in an attempt to avoid anticipated bias.
Third, diagnostic delays for minority children with a CSC may reflect differences in both parental initiation of diagnosis and in referral attendance. Minority parents have been shown to follow through with referrals to specialists at a lower rate than Caucasian parents (Zuckerman et al. 2011), a difference that has also been established in regards to autism referral attendance (Kalb et al. 2012). Minority parents may face more socioeconomic, scheduling, and transportation barriers to visit specialists (Broder-Fingert et al. 2013; Kalb et al. 2012). They may also hold different beliefs about the importance or seriousness of specialty consultations and are more likely to have had prior negative experiences in specialty care (Broder-Fingert et al. 2013). Another possibility is that parents of different backgrounds self-refer for autism diagnosis at disparate rates. Carr and Lord (2013) found that African American mothers with lower education reported less negative impact related to having a child with ASD than Caucasian mothers. Feeling less caregiver burden may result in later diagnosis seeking by African American parents.
While this study replicates others in underscoring the importance of demographic variables in ASD diagnosis, it is novel in its exposition of race and autism severity as moderators of the effect of having a CSC on age of diagnosis. Any existing differential medical practices across race and ASD type must be addressed to prevent further delays in diagnosis and treatment, as must the possible influence of discrepant parent behavior on delayed diagnosis seeking. In terms of strengths, this study has strong external validity given its sample size and demographic variety. The NSCH is the only survey of its kind to collect such extensive child health information on the national level.
The results of the study must also be considered within the context of several study limitations. First, the survey relies on retrospective recall and parent-report of ASD severity. Parents may have rated severity in a subjective manner, likely influenced by intellectual disability and behavioral problems, rather than having received a severity rating by a diagnostician. Similarly, age of ASD diagnosis was parent-reported and therefore subject to recall error or to confusion with age of first concern elicited by a healthcare professional. Given the possibility that minority children may have received an intellectual disability (ID) diagnosis before being diagnosed with ASD, earlier diagnosis of Hispanic and African American children may actually reflect age of ID diagnoses or special needs concerns.
The CSC variable also reflects parent report and may therefore be confounded by parent interpretation of a CSC. Of importance, the lack of a measure of CSC and insurance status preceding diagnosis limits the generalizability of our findings. Relatedly, the finding that health insurance type did not predict age of diagnosis must be interpreted with caution given that only 2 % of the sample was uninsured. Finally, the survey response rate of 23 % suggests that respondents may reflect a sample of convenience.
Statistical analyses of the model indicated a moderate effect size, which suggests that other factors contributed to age of diagnosis. Besides those variables studied, physician training has been identified as an important variable in ASD diagnosis (Fiscella et al. 2014; Fountain et al. 2011; Heidgerken et al. 2005). Differences in training of physicians serving primarily Caucasian versus African American populations may elucidate group differences, especially given different phenotypic expressions of ASD seen in the literature (Becerra et al. 2014; Sell et al. 2012). Implicit and explicit bias of physicians serving minority patients would also be worthwhile to study. Likewise, understanding how perceived discrimination plays into consultation delays would be an equally important factor to research. Lastly, more research is needed to clarify the intrapersonal factors involved in diagnosis seeking. Understanding which symptom led to referral (social, behavioral, intellectual), which person initiated the evaluation based on suspicion (parent, teacher or physician), and which tool and health professional confirmed the diagnosis would help to elucidate the diagnostic process and its predictors.
Determining deterrents to diagnosis, whether bias-based or not, is vital to reducing the gap between perception of ASD symptoms and confirmation of diagnosis. Timely diagnosis affords its recipients the specialized services that optimize outcomes (Fountain et al. 2011; Rogers and Vismara 2008). In addition, training physicians to recognize ASD symptoms in minority children and to practice nondiscriminatory referrals may help remedy racial disparities in the effect of having a CSC on age at diagnosis. Minimizing racial disparities may in turn decrease patient-based treatment delays associated with perceived discrimination and lower referral attendance to specialty care. Also, given that a considerable percent of children who are flagged do not complete follow-ups, health education of parents about the importance of specialty care must be emphasized.
One model that is increasingly popular and facilitates coordination of both preventive care and specialty referrals is the medical home (American Academy of Pediatrics 2005). Having a medical home has been shown to significantly improve care coordination and specialty care follow-through, and to in turn decrease unmet needs for children with special health care needs (Boudreau et al. 2014). Given recent provisions in the 2010 Patient Protection and Affordable Care Act that support implementation of the medical home model on a larger scale, we may be able to look forward to more regular health care utilization and better care coordination by families that have thus far been unable to access care (National Academy of State Health Policy 2010).
References
Adler, N. E., & Rehkopf, D. H. (2008). US disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health, 29, 235–252.
Adler, N. E., & Stewart, J. (2010). Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of the New York Academy of Sciences, 1186(1), 5–23.
American Academy of Pediatrics Council on Children with Disabilities. (2005). Care coordination in the medical home: Integrating health and related systems of care for children with special health care needs. Pediatrics, 116(5), 1238.
Baker, D. W., Stevens, C. D., & Brook, R. H. (1994). Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. Journal of the American Medical Association, 271(24), 1909–1912.
Barbaresi, W. J., Katusic, S. K., & Voigt, R. G. (2006). Autism: A review of the state of the science for pediatric primary health care clinicians. Archives of Pediatrics and Adolescent Medicine, 160(11), 1167–1175.
Bazargan, M., Norris, K., Bazargan-Hejazi, S., Akhanjee, L., Calderon, J. L., Safvati, S. D., & Baker, R. S. (2005). Alternative healthcare use in the under-served population. Ethnicity & Disease, 15, 531–539.
Becerra, T. A., von Ehrenstein, O. S., Heck, J. E., Olsen, J., Arah, O. A., Jeste, S. S., et al. (2014). Autism spectrum disorders and race, ethnicity, and nativity: A population-based study. Pediatrics, 134(1), e63–e71.
Billstedt, E., Gillberg, I. C., & Gillberg, C. (2005). Autism after adolescence: Population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders, 35(3), 351–360.
Bisgaier, J., & Rhodes, K. V. (2011). Auditing access to specialty care for children with public insurance. New England Journal of Medicine, 364(24), 2324–2333.
Blackwell, D. L., Martinez, M. E., Gentleman, J. F., Sanmartin, C., & Berthelot, J. M. (2009). Socioeconomic status and utilization of health care services in Canada and the United States: Findings from a binational health survey. Medical Care, 47(11), 1136–1146.
Blumberg, S. J., Foster, E. B., Frasier, A. M., Satorius, J., Skalland, B. J., Nysse-Carris, K. L., et al. (2012). Design and operation of the National Survey of Children’s Health, 2007: Program and collection procedures. (Vital and Health Statistics No. 55). Hyattsville, MD: Centers for Disease Control and Prevention National Center for Health Statistics.
Boss, E. F., Smith, D. F., & Ishman, S. L. (2011). Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. International Journal of Pediatric Otorhinolaryngology, 75(3), 299–307.
Boudreau, A. A., Goodman, E., Kurowski, D., Perrin, J. M., Cooley, W. C., & Kuhlthau, K. (2014). Care coordination and unmet specialty care among children with special health care needs. Pediatrics, 133(6), 1046–1053.
Bright Futures Steering Committee, & Medical Home Initiatives for Children With Special Needs Project Advisory Committee. (2006). Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics, 118(1), 405–420.
Broder-Fingert, S., Shui, A., Pulcini, C. D., Kurowski, D., & Perrin, J. M. (2013). Racial and ethnic differences in subspecialty service use by children with autism. Pediatrics, 132(1), 94–100.
Buescher, A. V. S., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics, 168(8), 721–728.
Burgess, D. J., Ding, Y., Hargreaves, M., van Ryn, M., & Phelan, S. (2008). The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. Journal of Health Care for the Poor and Underserved, 19(3), 894–911.
Carr, T., & Lord, C. (2013). Longitudinal study of perceived negative impact in African American and Caucasian mothers of children with autism spectrum disorder. Autism, 17(4), 405–417.
Casagrande, S. S., Gary, T. L., LaVeist, T. A., Gaskin, D. J., & Cooper, L. A. (2007). Perceived discrimination and adherence to medical care in a racially integrated community. Journal of General Internal Medicine, 22(3), 389–395.
Centers for Disease Control and Prevention. (2014). Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report, Surveillance Summaries, 63(2), 6–21.
Centers for Disease Control and Prevention National Center for Health Statistics. (2013). State and Local Area Integrated Telephone Survey: 2011-2012 National Survey of Children’s Health [Data file]. http://www.cdc.gov/nchs/slaits/nsch.htm.
Chan, L., Hart, L. G., & Goodman, D. C. (2006). Geographic access to health care for rural Medicare beneficiaries. Journal of Rural Health, 22(2), 140–146.
Coker, T. R., Elliott, M. N., Kataoka, S., Schwebel, D. C., Mrug, S., Grunbaum, J. A., et al. (2009). Racial/ethnic disparities in the mental health care utilization of fifth grade children. Academic Pediatrics, 9(2), 89–96.
Cook, N. L., Ayanian, J. Z., Orav, E. J., & Hicks, L. S. (2009). Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation, 119(18), 2463–2470.
Cook, B. L., Barry, C. L., & Busch, S. H. (2013). Racial/Ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Services Research, 48(1), 129–149.
Cummings, J. R., Lavarreda, S. A., Rice, T., & Brown, E. R. (2009). The effects of varying periods of uninsurance on children’s access to health care. Pediatrics, 123(3), e411–e418.
Daniels, A. M., & Mandell, D. S. (2013). Children’s compliance with American Academy of Pediatrics’ well-child care visit guidelines and the early detection of autism. Journal of Autism and Developmental Disorders, 43(12), 2844–2854.
DeVoe, J. E., Baez, A., Angier, H., Krois, L., Edlund, C., & Carney, P. A. (2007). Insurance + access ≠ health care: Typology of barriers to health care access for low-income families. The Annals of Family Medicine, 5(6), 511–518.
DeVoe, J. E., Petering, R., & Krois, L. (2008). A usual source of care: Supplement or substitute for health insurance among low-income children? Medical Care, 46(10), 1041–1048.
DeVoe, J. E., Tillotson, C. J., & Wallace, L. S. (2009). Children’s receipt of health care services and family health insurance patterns. The Annals of Family Medicine, 7(5), 406–413.
Dosreis, S., Weiner, C. L., Johnson, L., & Newschaffer, C. J. (2006). Autism spectrum disorder screening and management practices among general pediatric providers. Journal of Developmental and Behavioral Pediatrics, 27(2), S88–S94.
Durkin, M. S., Maenner, M. J., Meaney, F. J., Levy, S. E., DiGuiseppi, C., Nicholas, J. S., et al. (2010). Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a U.S. cross-sectional study. PLoS ONE, 5(7), 1–8.
Eldevik, S., Hastings, R. P., Hughes, J. C., Jahr, E., Eikeseth, S., & Cross, S. (2009). Meta-analysis of early intensive behavioral intervention for children with autism. Journal of Clinical Child and Adolescent Psychology, 38(3), 439–450.
Facione, N. C., & Facione, P. A. (2007). Perceived prejudice in healthcare and women's health protective behavior. Nursing Research, 56(3), 175–184.
Filipek, P. A., Accardo, P. J., Ashwal, S., Baranek, G. T., Cook, E. H., Dawson, G., et al. (2000). Practice parameter: Screening and diagnosis of autism Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology, 55(4), 468–479.
Fiscella, K., Franks, P., Doescher, M. P., & Saver, B. G. (2002). Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Medical Care, 40(1), 52–59.
Fiscella, K., Franks, P., Gold, M. R., & Clancy, C. M. (2014). Inequality in quality: Addressing socioeconomic, racial, and ethnic disparities in health care. Policy Perspectives, 283(19), 2579–2584.
Flores, G. (2010). Technical report: Racial and ethnic disparities in the health and health care of children. Pediatrics, 125(4), e979–e1020.
Flores, G., & Lin, H. (2013). Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: Has anything changed over the years? International Journal for Equity in Health, 12(10), 9276-12.
Fountain, C., King, M. D., & Bearman, P. S. (2011). Age of diagnosis for autism: Individual and community factors across 10 birth cohorts. Journal of Epidemiology and Community Health, 65(6), 503–510.
Gill, J. M., Mainous, A. G, I. I. I., & Nsereko, M. (2000). The effect of continuity of care on emergency department use. Archives of Family Medicine, 9(4), 333.
Goin-Kochel, R. P., Mackintosh, V. H., & Myers, B. J. (2006). How many doctors does it take to make an autism spectrum diagnosis? Autism, 10(5), 439–451.
Gourdine, R. M., & Algood, C. L. (2014). Autism in the African American population. In V. B. Patel, V. R. Preedy, & C. R. Martin (Eds.), Comprehensive guide to autism (pp. 2455–2467). New York, NY: Springer.
Harstad, E., Huntington, N., Bacic, J., & Barbaresi, W. (2013). Disparity of care for children with parent-reported autism spectrum disorders. Academic Pediatrics, 13(4), 334–339.
Heidgerken, A. D., Geffken, G., Modi, A., & Frakey, L. (2005). A survey of autism knowledge in a health care setting. Journal of Autism and Developmental Disorders, 35(3), 323–330.
Herlihy, L. E., Brooks, B., Dumont-Mathieu, T., Barton, M. L., Fein, D., Chen, C. M., & Robins, D. L. (2014). Standardized screening facilitates timely diagnosis of autism spectrum disorders in a diverse sample of low-risk toddlers. Journal of Developmental and Behavioral Pediatrics, 35(2), 85–92.
Hertz-Picciotto, I., & Delwiche, L. (2009). The rise in autism and the role of age at diagnosis. Epidemiology, 20, 84–90.
Johnson, C. P., & Myers, S. M. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215.
Kalb, L. G., Freedman, B., Foster, C., Menon, D., Landa, R., Kishfy, L., & Law, P. (2012). Determinants of appointment absenteeism at an outpatient pediatric autism clinic. Journal of Developmental and Behavioral Pediatrics, 33(9), 685–697.
Keenan, M., Dillenburger, K., Doherty, A., Byrne, T., & Gallagher, S. (2010). The experiences of parents during diagnosis and forward planning for children with autism spectrum disorder. Journal of Applied Research in Intellectual Disabilities, 23(4), 390–397.
Kenney, G. M., Coyer, C., & Anderson, N. (2013). Racial and ethnic differences in access to care and service use for children with coverage through Medicaid and Children’s Health Insurance Program: A summary. Urban Institute. http://www.urban.org/publications/412780.html.
King, T. M., Tandon, S. D., Macias, M. M., Healy, J. A., Duncan, P. M., Swigonski, N. L., et al. (2010). Implementing developmental screening and referrals: Lessons learned from a national project. Pediatrics, 125(2), 350–360.
Kuhlthau, K., Nyman, R. M., Ferris, T. G., Beal, A. C., & Perrin, J. M. (2004). Correlates of use of specialty care. Pediatrics, 113(3), e249–e255.
Lee, C., Ayers, S. L., & Kronenfeld, J. J. (2009). The association between perceived provider discrimination, health care utilization, and health status in racial and ethnic minorities. Ethnicity & Disease, 19(3), 330.
Lillie-Blanton, M., & Hoffman, C. (2005). The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Affairs, 24(2), 398–408.
Matson, J. L., Wilkins, J., & Gonzalez, M. (2008). Early identification and diagnosis in autism spectrum disorders in young children and infants: How early is too early? Research in Autism Spectrum Disorders, 2(1), 75–84.
Mayer, M. L., Skinner, A. C., & Slifkin, R. T. (2004). Unmet need for routine and specialty care: Data from the National Survey of Children with Special Health Care Needs. Pediatrics, 113(2), e109–e115.
Murphy, M. M., Simons, J. P., Ng, S. C., McDade, T. P., Smith, J. K., Shah, S. A., et al. (2009). Racial differences in cancer specialist consultation, treatment, and outcomes for locoregional pancreatic adenocarcinoma. Annals of Surgical Oncology, 16(11), 2968–2977.
National Academy of State Health Policy. (2010). Long term services and supports and chronic care coordination: Policy advances enacted by the Patient Protection and Affordable Care Act. http://www.ncsl.org/research/health/the-medical-home-model-of-care.aspx.
2011/12 National Survey of Children’s Health. Maternal and Child Health Bureau in collaboration with the National Center for Health Statistics. 2011/12 NSCH SPSS Indicator Data Set prepared by the Data Resource Center for Child and Adolescent Health, Child and Adolescent Health Measurement Initiative. www.childhealthdata.org.
Pedersen, A., Pettygrove, S., Meaney, F. J., Mancilla, K., Gotschall, K., Kessler, D. B., et al. (2012). Prevalence of autism spectrum disorders in Hispanic and non-Hispanic white children. Pediatrics, 129(3), e629–e635.
Pinto-Martin, J. A., Young, L. M., Mandell, D. S., Poghosyan, L., Giarelli, E., & Levy, S. E. (2008). Screening strategies for autism spectrum disorders in pediatric primary care. Journal of Developmental & Behavioral Pediatrics, 29(5), 345–350.
Raphael, J. L., Guadagnolo, B. A., Beal, A. C., & Giardino, A. P. (2009). Racial and ethnic disparities in indicators of a primary care medical home for children. Academic Pediatrics, 9(4), 221–227.
Rogers, S. J., & Vismara, L. A. (2008). Evidence-based comprehensive treatments for early autism. Journal of Clinical Child and Adolescent Psychology, 37(1), 8–38.
Sansosti, F. J., Lavik, K. B., & Sansosti, J. M. (2012). Family experiences through the autism diagnostic process. Focus on Autism and Other Developmental Disabilities, 27(2), 81–92.
Sell, N. K., Giarelli, E., Blum, N., Hanlon, A. L., & Levy, S. E. (2012). A comparison of autism spectrum disorder DSM-IV criteria and associated features among African American and white children in Philadelphia County. Disability and Health Journal, 5(1), 9–17.
Shattuck, P. T., Durkin, M., Maenner, M., Newschaffer, C., Mandell, D. S., Wiggins, L., et al. (2009). Timing of identification among children with an autism spectrum disorder: Findings from a population-based surveillance study. Journal of the American Academy of Child & Adolescent Psychiatry, 48(5), 474–483.
Shields, A. E., Comstock, C., & Weiss, K. B. (2004). Variations in asthma care by race/ethnicity among children enrolled in a state Medicaid program. Pediatrics, 113(3), 496–504.
Sices, L. (2007). Developmental screening in primary care: The effectiveness of current practice and recommendations for improvement. Commonwealth Fund. www.commonwealthfund.org.
Starfield, B., & Shi, L. (2004). The medical home, access to care, and insurance: A review of evidence. Pediatrics, 113(4), 1493–1498.
Steyerberg, E. W., Neville, B., Weeks, J. C., & Earle, C. C. (2007). Referral patterns, treatment choices, and outcomes in locoregional esophageal cancer: A population-based analysis of elderly patients. Journal of Clinical Oncology, 25(17), 2389–2396.
Strickland, B. B., Singh, G. K., Kogan, M. D., Mann, M. Y., van Dyck, P. C., & Newacheck, P. W. (2009). Access to the medical home: New findings from the 2005–2006 National Survey of Children with Special Health Care Needs. Pediatrics, 123(6), e996–e1004.
Toomey, S. L., Chien, A. T., Elliott, M. N., Ratner, J., & Schuster, M. A. (2013). Disparities in unmet need for care coordination: The national survey of children’s health. Pediatrics, 131(2), 217–224.
Trivedi, A. N., & Ayanian, J. Z. (2006). Perceived discrimination and use of preventive health services. Journal of General Internal Medicine, 21(6), 553–558.
Vismara, L. A., & Rogers, S. J. (2010). Behavioral treatments in autism spectrum disorder: What do we know? Annual Review of Clinical Psychology, 6, 447–468.
Visser, S. N., Danielson, M. L., Bitsko, R. H., Holbrook, J. R., Kogan, M. D., Ghandour, R. M., et al. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United states, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 34–46.
Wagner, J., & Abbott, G. (2007). Depression and depression care in diabetes relationship to perceived discrimination in African Americans. Diabetes Care, 30(2), 364–366.
Zimmerman, F. J. (2005). Social and economic determinants of disparities in professional help-seeking for child mental health problems: Evidence from a national sample. Health services research, 40(5 pt 1), 1514–1533.
Zuckerman, K. E., Mattox, K., Donelan, K., Batbayar, O., Baghaee, A., & Bethell, C. (2013). Pediatrician identification of Latino children at risk for autism spectrum disorder. Pediatrics, 132(3), 445–453.
Zuckerman, K. E., Nelson, K., Bryant, T. K., Hobrecker, K., Perrin, J. M., & Donelan, K. (2011). Specialty referral communication and completion in the community health center setting. Academic Pediatrics, 11(4), 288–296.
Zuvekas, S. H., & Taliaferro, G. S. (2003). Pathways to access: Health insurance, the health care delivery system, and racial/ethnic disparities, 1996–1999. Health Affairs, 22(2), 139–153.
Zwaigenbaum, L., Bryson, S., & Garon, N. (2013). Early identification of autism spectrum disorders. Behavioural Brain Research, 251, 133–146.
Author Contributions
Mrs. Emerson designed the study, conducted the statistical analysis, analyzed the data, wrote the initial draft of the paper, and participated in revising the manuscript and addressing the reviewers' comments. Dr. Morrell assisted with manuscript development, provided guidance on statistical analysis, and participated in revising the manuscript and addressing the reviewers' comments. Dr. Neece assisted with manuscript development, provided guidance on statistical analysis, and participated in revising the manuscript and addressing the reviewers' comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Emerson, N.D., Morrell, H.E.R. & Neece, C. Predictors of Age of Diagnosis for Children with Autism Spectrum Disorder: The Role of a Consistent Source of Medical Care, Race, and Condition Severity. J Autism Dev Disord 46, 127–138 (2016). https://doi.org/10.1007/s10803-015-2555-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-015-2555-x