Abstract
Little is known about Young adults with Autism Spectrum Disorder (YA-ASD) health, healthcare and safety needs. This study describes the validation of a health care transition measure for YA-ASD, the Health-Related Independence (HRI). We collected data from caregivers (n = 490) at five Autism Treatment Network sites and compared the psychometric properties of HRI to the gold standard (STARx) and other validated measures. A Confirmatory Factor Analysis and item culling resulted in 30 items addressing six subscales. Content, criterion, and construct validity and internal consistency indicated high validity and reliability for the scale and subscales. HRI is a validated caregiver-report measure of YA-ASD’s self-management, safety, and transition skills. This novel measure will be a useful tool in clinics, intervention development, and research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Interagency Autism Coordinating Committee (IACC) prioritize transition services for young adults with Autism Spectrum Disorder (YA-ASD) as a key area for funding and research within its Strategic Plan for ASD and recommendation for the CARES act of 2019 (IACC 2017). Health Care Transition (HCT) services help YA-ASD prepare for and make the transition from pediatric to adult health care service (American Academy of Pediatrics et al. 2002; White et al. 2018). HCT services are of great importance to YA-ASD as over half of this population has a co-occurring condition and YA-ASD are at increased risk for polypharmacy, multiple health problems, anxiety, depression, and behavioral problems (Muskens et al. 2017; Soke et al. 2018).
Access to HCT services for young adults with special health care needs has shown improvements in access to care, appropriate service utilization, patient satisfaction, health outcomes, and reduced cost burdens to families (Gabriel et al. 2017). Unfortunately, fewer than 20% of YA-ASD receive HCT services and few studies have examined how to improve HCT service provision to YA-ASD (Cheak-Zamora et al. 2013, 2014; Walsh et al. 2017; Shattuck et al. 2018). A systematic review of HCT interventions found that all interventions focused on young adults with physical health conditions such as cystic fibrosis, diabetes, sickle cell disease, and kidney and liver transplants (Betz et al. 2016). None of the interventions identified in the review included YA-ASD.
HCT readiness measurements are an important part of HCT service provision that helps young adults, caregivers, and health care providers assess the young adult’s readiness to transfer to an adult provider (White et al. 2018; Zhang et al. 2014). Both condition-specific and condition-neutral measures of HCT readiness have been developed but none has included a significant number of participants with ASD in the development or validation of the measure. Two of the most popular HCT condition-neutral measures are the Self-management and Transition to Adulthood with Rx = Treatment (STARx) scale and the Transition Readiness Assessment Questionnaire (TRAQ) (Ferris et al. 2015; Sawicki et al. 2009; Zhang et al. 2014). Most of the STARx and TRAQ questions focus on medication management, appointment keeping, and provider interactions. Additionally, the STARx includes subscales related to disease knowledge and resource utilization. The TRAQ includes a few questions on understanding health insurance and life skills but did not develop specific scales or subscales related to these topics. The skills assessed within these measures are needed for a successful transition to adult care but seem most applicable for young adults managing multiple medication and medical appointments. YA-ASD experience additional challenges that these measures do not address (Davis et al. 2014; Kuhlthau et al. 2016).
Due to the unique nature of ASD; providers, caregivers, and YA-ASD themselves report transition experiences and needs that deviate from the experiences of young adults with other special health care needs (Cheak‐Zamora et al. 2015, 2017; Kuhlthau et al. 2016; Weiss et al. 2018). YA-ASD and their caregivers report HCT needs related to sexuality, safety, and self-care skills in addition to medication and appointment management, provider interactions, and YA-ASD-provider communication (Cheak-Zamora et al. 2017; Schwartz et al. 2011). A specific measure of HCT readiness tailored to the needs of this population is essential (Levy and Perry 2011).
This current validation study was part of a larger project that used a mixed-methods approach to develop an HCT measure specific to the needs of YA-ASD and their caregivers- the Health-Related Independence (HRI) measure (Cheak-Zamora et al. 2020). Previous work included YA-ASD interviews and caregiver focus groups to develop measurement concepts and individual items (Cheak-Zamora et al. 2020). Cognitive interviewing and pretesting methods were used to ensure item clarity, translatability, and readability. We define HRI as a holistic understanding of a YA-ASD’s ability to manage their health, health care, and safety needs (Cheak-Zamora et al. 2014, 2019; Golnik et al. 2009; Hess and Straub 2010; Walsh et al. 2017). This paper will describe the large-scale validation of the HRI for YA-ASD Measure- Caregiver version.
Methods
Study Overview
The psychometric evaluation of the HRI measure followed the PROMIS guidelines including a large multi-site data collection effort; Confirmatory Factor Analysis to determine item and model fit; and the inclusion of numerous validated measure used to determine validity, reliability, and interpretability of the final HRI measure (Bevans et al. 2014; HealthMeasures 2013). The HRI development study identified 8 subscales that theoretically contributed to the concept of HRI and 60 individual items (Cheak-Zamora et al. 2020). The eight subscales of HRI included: Physical and mental health challenges and communication; Medication or illness management; Appointments/health care visits; Safety; Relationships and sexuality; Finances/financial management; Self-care/health and lifestyle; and Health success/self-advocacy.
Quantitative Study Sites
Upon completion of Phase 3, the HRI measure was tested in five Autism Treatment Network (ATN) clinic sites across the U.S. (Missouri, Texas, Ohio, Tennessee, and Pennsylvania), including a children’s hospital, three large academic medical centers, and a large ASD-specific clinic. These specific ATN sites were included to ensure representation of minority populations, rural and urban communities, and communities with varying health care access issues. Each site was charged with recruiting 100 eligible participants, distributing survey instruments and reminders, and providing compensation for participation.
Recruitment and Eligibility for Caregivers
Eligible participants were restricted to English-speaking primary caregivers of a YA-ASD between the ages of 16–25 years of age (Cheak-Zamora et al. 2015; Ferris et al. 2015; Kuhlthau et al. 2016; Nathenson and Zablotsky 2017). YA-ASD diagnosis and age were verified through chart records. ATN sites utilized their network and clinic databases to identify eligible participants. Recruitment methods varied by site and included email, mail, phone, and approach individually before the YA-ASD’s clinical appointments. Study flyers were placed on the sites’ websites and Facebook/Twitter pages. Surveys took between 20–40 min to complete. Most surveys were completed using Research Electronic Data Capture (REDCap) electronic data capture tools (Harris et al. 2009). A small number of caregivers completed the survey in paper format. Participants received a $20 gift card for completing the survey. All sites participated in bi-weekly conference calls during the recruitment period to discuss recruitment goals, develop strategies, problem-solve recruitment, and resolve survey delivery issues.
Measures
Health-related Independence (HRI). The HRI measure was developed for caregiver report of the youth/young adult’s independence level. The measure was comprised of eight subscales and 60 questions. Based on the qualitative data, we theorized the measure subscales would include: Knowledge about medical and mental health conditions; Self-care; Medication management; Healthcare visits; Safety; Sexual health; Healthcare financial management; and Developing goals for future/goal planning. A four-point scale was used for response options. The response options captured the range of assistance YA-ASD would need to complete the skill or task described in the question. This ranged from: “Independent. Can complete task without adult guidance or support” to “Totally dependent on the parent or caregiver to complete task.”
Health Care Transition
The Self-management and Transition to Adulthood with Rx = Treatment (STARx) is a caregiver questionnaire that assesses caregivers’ interpretation of their youths’ HCT readiness. Developed by the University of North Carolina (UNC) School of Medicine, the STARx is a self-administered measure with 3-subscales and 18-questions (Ferris et al. 2015; Zhang et al. 2014). The STARx has been used internationally in hundreds of studies and clinical settings as a diagnosis-neutral HCT measure.
Transfer to an Adult Provider
A single question identifying if young adults had completed the transfer to an adult healthcare provider used to examine construct validity within the HRI. This question was taken from HCT quality improvement measures developed by Got Transition (McManus et al. 2015).
Self-determination
Caregivers also evaluated their young adult’s self-determination using the American Institutes for Research (AIR) Self-Determination measure (Wolman et al. 1994). Self-determination is the ability of a young adult to evaluate their needs, set goals, assess effort, and make decisions among other skills (Chou et al. 2016). The AIR examines the young adult’s capacity to be self-determined (6 questions) and level of opportunity to be self-determined at home (6 questions). The scale score of Self-Determination (range from 12–60) was used in this study. Prior studies have demonstrated adequate reliability and validity for the parent scale (Carter et al. 2009, 2013).
Demographics
As described in Table 2, demographic information was collected on young adults and caregivers. Young adult’s functional/severity level was assessed using a one item question taken from the National Survey of Children’s Health. Specifically this question asks caregivers to rate their, “young adult’s current symptoms of ASD” (Table 2). Young adults' employment and volunteer experience were also evaluated, which are historical indicators of general independence (Paradiz et al. 2018; Shogren et al. 2015; Wehmeyer and Palmer 2003).
Testing of Psychometric Properties of HRI
Confirmatory Factor Analysis (CFA) was used to test the fit of the HRI items to the constructs or topics identified by caregivers of YA-ASD. CFA was also used to test the content validity of the HRI. Because items responses are on a short ordinal scale a robust weighted least square estimator (WLSMV), available in Mplus v8.3, was used to fit the model. The WLSMV estimator does not assume normality and appears to be currently the best choice of estimator for confirmatory models with ordinal or categorical indicators (Flora and Curran 2004; Li 2016). Judging model goodness-of-fit is an important aspect of CFA and numerous descriptive measures of fit have been developed (Tanaka 1993). As the single universally agreed upon fit index is yet to be developed it is customary to consider multiple indices. For this study model, fit-evaluation is based on the Root Mean Square Error of Estimation (RMSEA; MacCallum et al. 1996), the Tucker Lewis Index (TLI; Hu and Bentler 1999), and the standardized root mean square residual (SRMR; Hu and Bentler 1999). Based on recommendations from the cited literature we consider that adequate fit is demonstrated by TLI ≥ 0.95, RMSEA ≤ 0.08, and SRMR < 0.08. Also, because it is customary, the chi-square test of fit is reported, but is given little weight in our evaluations as it is uninformative in large samples, i.e. tends to reject all models. A chi-square difference test appropriate to the WLSMV estimator was performed using the difftest option in Mplus.
Validation and Internal Consistency Analysis
Criterion validity was evaluated by examining correlations between HRI total and subscale scores and the current gold-standard for HCT measurement of young adults with special health care needs- the STARx measure. Construct validity was assessed in several ways. Young adults who had successfully transitioned to an adult provider would be expected, on average, to have higher HRI scores and so these groups were compared with respect to HRI total and subscale scores. HRI scores were correlated with scores from the AIR self-determination instrument, and examined by age groups (16–17 years, 18–20 years, and 21–25 years of age) with expectation that older YA-ASD and those with higher self-determination will generally have greater independence (Cheak-Zamora et al. 2019. Finally, initial reliability was assessed by examining internal consistency. Internal consistency of the final scales was estimated using Coefficient Alpha (Cronbach 1951). The authors followed the analysis and reporting recommendation described in the PROMIS Instrument Development and Validation Scientific Standards (HealthMeasures 2013).
Floor and Ceiling Effects
The HRI scales were also evaluated for floor and ceiling effects (Terwee et al. 2007). Floor and ceiling effects occur when a large proportion of subjects have the highest or lowest possible score indicating lack of distinguishability and responsiveness of the measure.
Results
Sample
The third version of the HRI measure was administered to 510 caregivers of YA-ASD distributed across the five ATN sites. The development of the measure and revision of previous versions was a multi-year process based on YA-ASD, caregiver, and clinician input (Cheak-Zamora et al. 2020). Thirty-seven cases were excluded from the analysis due to incomplete responses. The majority of the caregivers were mothers (88%) with an average age of 50 years (SD = 7). The caregiver’s YA-ASD of survey respondents were primarily male (79%), Caucasian (86%), and non-Hispanic (93%), with a mean age of 18 years (SD = 2) and range of 16–25 years. Other caregiver demographics and YA-ASD condition-specific characteristics are presented in Table 1.
Confirmatory Factor Analysis
An initial confirmatory factor analysis included all 60 items allocated to the originally conceived eight factors of HRI. Although model fit was adequate, a review by experts and stakeholders concluded that the instrument was much too long and some items reflected concepts more general than HRI. The review process resulted in a consensus to exclude items comprising two of the factors, developing goals and self-care, were not sufficiently focused on health care transition or overall health, and should not be included in a health-related independence measure. Further debate streamlined HRI measure to 30 items addressing six constructs with between four and six and six items per construct/subscale (Table 2). A second CFA was carried out on the reduced item set. The existence of a factor structure is supported by the implausibility of the null model: Chi-square = 86, 950 on 435 degrees of freedom. A model with six correlated factors exhibited good model fit to the data as judged by RMSEA = 0.067, TLI = 0.989 and SRMR = 0.035 (Table 3). Furthermore, all standardized factor loadings were greater than 0.80. The inter-factor correlations were very strong (all > 0.7) and so a model with a single second-order factor was also fit. In the second order model, the factor correlations are conceptually a consequence of the first-order factors themselves being facets of a single more general concept (HRI). Although a chi-square difference test between first and second order models was statistically significant (p < 0.001, df = 9), the loss in goodness-of-fit with the second-order factor model is slight: All indices still fall within the accepted ranges for an adequate model. The standardized loadings of the individual item loadings remained at 0.8 or higher, and standardized loadings of the first-order factors on a single second-order factor are all 0.87 or greater. The reasonably good fit of the second order supports the use of both subscales and an overall score for the HRI tool.
Criterion Validity
The STARx served as our gold standard for the HCT measure for young adults with special health care needs based on its extensive validation and use in the literature. All correlations between HRI and STARx were statistically significant (p < 0.001) and in the expected direction. The strength of the correlation met and exceeded the standard of 0.70 in all appropriate comparisons. HRI Health Care Finance score was not strongly correlated with the STARx scale score or subscale scores but this was to be expected as the STARx does not ask questions related to insurance or finance knowledge. Correlations between all scales and subscales of the HRI and STARx scales were presented in Table 4.
Construct Validity
External validity was also established by comparing HRI scales for YA-ASD who transferred to an adult provider versus YA-ASD being cared for by a pediatrician (Table 5). For all scale scores, the difference was statistically significant and in the expected direction. Specifically, HRI scores and subscale means were higher for the transferred group than for the group that remained with a pediatrician.
Similarly, we compared the HRI scale to a validated self-determination scale, the AIR self-determination scale, to assess construct validity. The research team hypothesized that YA-ASD with higher levels of self-determination would be associated with higher HRI scale scores.
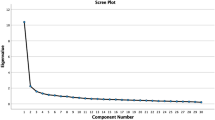
Associations between the HRI scale scores and AIR self-determination scale scores represent another source of construct validity (Table 6). All correlations are positive and statistically significant. Finally, HRI scale scores were examined by age groups to measure sensitivity to changes in age. Figure 1 shows a significant dose–response to age category.
Internal Consistency
The internal consistency for the scale score and all subscales had Cronbach’s alphas that exceeded 0.9. Item total correlations over all items and subscales had a range of 0.71 to 0.89 with an average of 0.82. Calculating Coefficient Alpha for each scale with item deletion did not reveal any opportunities to improve internal consistency by removing items This was an indication of very good internal consistency (Clark and Watson 1995). Summary statistics for the total scale scores, internal consistency estimates (coefficient alpha) and the standard error of measurement (SEM) were presented in Table 7.
Floor and Ceiling Effects
No floor or ceiling effect was observed for the HRI scale score and four of the six subscale scores. The Health Insurance Knowledge subscale had a significant floor effect as described in Table 7. After review of the results and consultation with our expert panel, we concluded that the floor effect for Health Insurance Knowledge subscale is not an indicator of poor content validity (Terwee et al. 2007). Rather similar to findings from other HCT studies, it appears that this topic area is rarely discussed in society, in particular with young adults and those with disabilities (Ferris et al. 2012; Sawicki et al. 2009). The floor effects within this subscale represent the lack of attention given to health insurance education in the YA-ASD population. Further, there is no evidence that the reliability of this subscale was in question since it is highly likely that with education, a portion of YA-ASD would gain health insurance knowledge and skills.
Discussion
The 2017 Report to Congress: Young Adults and Transitioning Youth with ASD advocates for the development and validation of functional outcome measures for YA-ASD (IACC 2017). The current study responded to this identified need by validating the first HCT measurement for YA-ASD. Specifically, the HRI measure examined what YA-ASD and caregivers constitute as positive HCT and independence-related outcomes, as well as skills needed to successfully transition to adult care. The HRI is a brief, 5 to 10 min, caregiver-administered survey that provides a holistic evaluation of the YA-ASD’s ability to manage their health, health care, and safety needs.
The PROMIS guidelines were used to develop the initial concept, subscales, and initial item pool of the HRI measure and conduct a large-scale validation study of the measure. In the first phases of this process, qualitative methods were used to obtain an in-depth understanding of caregiver and YA-ASD transition needs (Cheak-Zamora et al. 2020). These themes were then used to develop HRI scale, subscales, and individual items in a team-based approach with caregivers, clinicians, and autism researchers. Additional cognitive interviews and pilot testing clarified individual questions, answer choices, and formatting of the measure. Finally, the HRI measure was implemented in five Autism Treatment Network (ATN) clinics throughout the country to test the psychometric properties of the caregiver-version of the HRI measure.
A reasonable fit for the second-order factor model supports the use of the measure with a total scale score and six construct-specific subscale scores. The absence of extreme ceiling and floor effects within the HRI measure and most subscales indicate that there is no clumping of scores at the high and low ends of the scoring range. Thus we are confident in the measures variability and ability to detect positive and negative changes in independence over time. The HRI measure was shown to have strong internal consistency with alpha estimates exceeding recommended levels in both the full-scale and subscales. This further supports the use of the full-scale score and subscales in future work. The survey appears to be well tolerated as less than 40 (7%) participants started the survey, but quit before completing the HRI measure.
The significant criterion validity results confirm that the HRI and the STARx are measuring similar HCT and independence subscales. The STARx has been used in hundreds of studies within young adult populations with various disabilities making it an important comparison measure (Ferris et al. 2015). For subscales in which HRI and STARx covered similar concepts, subscale correlations were significant and exceeded correlation standards. Similar correlations were observed when comparing STARx and HRI overall scale scores. These findings indicate the strength of the HRI measure in not only assessing independence but also HCT readiness. The health care system is in great need of measures to assess independence and HCT readiness for YA-ASD as no measure previously existed (IACC 2017; Levy and Perry 2011; Walsh et al. 2017). The HRI’s ability to address the unique HCT readiness and independence needs of YA-ASD will provide a great service to primary and specialty health care services.
The transition from pediatric to adult care and self-determination skills are key outcomes for YA-ASD. This study used a validated self-determination measure and a one-item question assessing the transfer status of the YA-ASD (i.e. had the YA-ASD transferred from a pediatric to an adult provider) to examine construct validity of the HRI measure. As hypothesized, higher HRI scores were strongly correlated with increased self-determination and the transfer to an adult provider. These results increased our confidence that current HRI score is highly predictive of future transition success and the ability to perform autonomous and independent activities.
The results also demonstrated the HRI’s responsiveness to differences in the YA-ASD’s age. Figure 1 indicated an increase in HRI score with increases in age category. The measures sensitivity to changes in age was similar to those indicated in condition-neutral HCT measures- STARx, TRAQ, and UNC TRxANSITION (Ferris et al. 2012, 2015; Sawicki et al. 2009). Improved HRI scores with age fits with the assumption that skill related to decision making, independence, and transition readiness improve with age (Ferris et al. 2015, 2012; Sawicki et al. 2009). The ability of the measure to distinguish between developmental ages within a wide age range will assist in the creation of age-appropriate interventions. As with the STARx, further research utilizing the HRI will enable researchers and practitioners to develop age-based standardized scores for YA-ASD. Further research and implementation of the HRI, particularly utilizing standardized scores, will improve our ability to identify clinically meaningful changes in scores and predictive models for a successful transfer to an adult provider.
The STARx, TRAQ, and UNC TRxANSITION are the predominate condition-neutral measures of HCT (Ferris et al. 2012, 2015; Sawicki et al. 2009). While each of these measures have contributed significantly to the field, HRI has many strengths over the current measures. Content validity was the primary measure of validity for the current measures and none examined construct validity against a gold-standard. Within this study, we were able to fully examine the psychometric properties of the HRI across five clinical settings within the U.S. with a large sample size of nearly 500 caregiver participants.
The HRI shares many of the same subscales as the current HCT measures in the field. Each of the measures have subscales or question sets related to condition knowledge, medication management, and participation in the health care visit (Ferris et al. 2015; Sawicki et al. 2009; Zhang et al. 2014). Similar to the HRI, the TRAQ and UNC TRxANSITION include several questions about health insurance knowledge (Ferris et al. 2012; Sawicki et al. 2009). While some questions within these subscales are similar, the HRI assesses a wider range of health-related skills and knowledge for both physical and mental health needs, along with communication skills that may be more challenging for YA-ASD.
The HRI further extends on previous measures by including subscales related to safety and sexual health. Concerns related to safety and sexual vulnerability have been well documented in the literature (Cheak-Zamora et al. 2017; Cheak-Zamora and Teti 2015; IACC 2017). Safety concerns were keys themes for both YA-ASD and caregivers in the qualitative study in which the HRI measure was built. While caregivers talked more about sexual safety, YA-ASD discussed the need for sexual health education and relationship development skills (Cheak-Zamora et al. 2019; Teti et al. 2019). While the UNC TRxANSITION includes a subscale on reproduction, the majority of questions relate the effect of a medical condition on the individual’s ability to reproduce (Ferris et al. 2012). While this is important for some conditions, ASD-related concerns included understanding pregnancy, protection, consent, and how to differentiate between friendship and romantic relationships. Similarly, safety concerns for individuals with ASD and their caregivers centered on being alone, using the internet, interaction with law enforcement, and elopement. Caregivers provided examples in which the lack of these skills/abilities resulted in physical and psychological harm to their children and adolescents. No other measure examines overall safety of young adults with special health care needs.
With the successful validation, the HRI measure can serve as a learning and evaluation tool for both medical providers and caregivers to examine promotion of YA-ASD independence. HRI results will allow the medical team to tailor activities and material needed to improve YA-ASD’s transition readiness during and after the medical visit. HCT measures for other populations have been shown to improve the frequency and quality of health care provider’s conversations with families about increasing independence, guardianship issues, and preparing for the transfer to an adult doctor (Betz et al. 2016; Gabriel et al. 2017; Hess and Straub 2010). In pilot testing the HRI, caregivers reported the survey was a reminder of the topics they should be addressing to assist YA-ASD to successfully transition into adulthood. Implementation of the HRI measure in health care clinics or support services will increase both caregiver and system-level supports to enhance YA-ASD independence.
The HRI measure can improve the development and assessment of future interventions. As stated in the 2017 Report to Congress current interventions and programs cannot be tested due to the lack of validated measures to examine intended outcomes (IACC 2017; Zhang et al. 2014). The current study fills this gap by providing a measure to examine the efficacy of future transition planning programs and health or independence-related interventions for youth and YA-ASD. Similarly, the subscales within the HRI measure can be used separately to examine interventions that focus on one or more of the six subscales identified as important to caregivers and YA-ASD in previous qualitative studies (Cheak-Zamora and Teti 2015; Kuhlthau et al. 2016; Teti et al. 2019).
There are several limitations to the study. While previous HCT measures have been developed for both caregivers and young adults with special health care needs, this study conducted the initial validation of the HRI utilizing caregiver report only. This study did not include YA-ASD self-report in the validation portion of the study due to limited resources and the inability to include YA-ASD with intellectual disabilities and significant communication limits (Johnson et al. 2009; Lerner et al. 2012; Stratis and Lecavalier 2015). Similar to other measures of HCT, our goal was to ensure the psychometric properties of one version of the HRI before testing multi-rater versions (Ferris et al. 2012, 2015; Sawicki et al. 2009). The use of caregiver report in this study should not make little of the need for and importance of YA-ASD voices. Multi-rater reports of HRI in which both the caregiver and YA-ASD provide their assessment of independence are ideal. A separate validation of a young adult self-report version of the HRI is ongoing but is outside the scope of this study.
The research team did not collect HRI data over multiple time points, thus test–retest reliability was not estimated. The study findings showed that the HRI met reliability standards as it was able to distinguish between different groups of patients, but this study was not able to ensure HRI’s temporal stability. Future studies are needed to examine test–retest reliability within the HRI. Lastly, this study utilized data collection sites in five autism-clinics through the U.S. to improve response rates of typically underrepresented populations such as racial/ethnic minorities and low-income families. Although the diversity within our data is an improvement on many autism-specific national surveys, our data is not representative of the nation as a whole. Additionally, targeted efforts are needed to recruit and retain underrepresented populations in future studies.
Conclusion
The study aimed to identify the health care transition needs of young adults with ASD and their caregivers by developing and testing a measure tailored to their needs. This article describes the development and validation of the Health-Related Independence (HRI) measure using a large-scale multisite data collection process. The process resulted in a validated caregiver-administered measure of YA-ASD’s ability to manage their health, health care, and safety needs. The HRI is the first measure of its kind and will improve the health and transition success of YA-ASD.
Following established criteria for measurement propriety development, this study demonstrated the HRI measure has adequate internal consistency and content, criterion and construct validity (HealthMeasures 2013). The authors further present HRI mean and standard deviation differences by important indicators and outcomes (i.e. transfer to an adult provider, self-determination, and age) to establish clinically meaningful deviations and potential changes in scores. Future studies are needed to examine changes in HRI over time and define clinically meaningful cut points.
As described in the 2017 Report to Congress: Young Adults and Transitioning Youth with ASD, the HRI measure fills a large gap in the need for validated measures of transition-related outcomes for YA-ASD (IACC 2017). The HRI measure has the potential to improve clinical care by giving providers a quick low-resource measure of YA-ASD transition readiness and provide age and stage-appropriate guidance. The measure can be easily implemented into health care or other services systems without considerable training or cost. Caregivers can utilize HRI results to educate their YA-ASD and improve opportunities for independence at home. Additionally, the HRI is an important research tool as it is the first validated assessment of transition intervention success.
Clinicians and caregivers should strive to incorporate the HRI measure into their bi-annual and annual assessment within health care, school, and other services settings. Although the focal area of the HRI measure is health care needs, the measure covers important concepts related to safety, sexual safety and health, among other topics. Increasing independence in one area of life has been shown to increase independence in other areas of life. Implementation of the HRI can improve collaboration across health care, home, and community settings and improve YA-ASD independence overall.
References
American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians-American Society of Internal Medicine. (2002). A consensus statement on health care transitions for young adults with special health care needs. Pediatrics, 110(6), 1304–1306.
Betz, C. L., O’Kane, L. S., Nehring, W. M., & Lobo, M. L. (2016). Systematic review: Health care transition practice service models. Nursing Outlook, 64(3), 229–243. https://doi.org/10.1016/j.outlook.2015.12.011.
Bevans, M., Ross, A., & Cella, D. (2014). Patient-Reported Outcomes Measurement Information System (PROMIS): Efficient, standardized tools to measure self-reported health and quality of life. Nursing Outlook, 62(5), 339–345.
Carter, E. W., Lane, K. L., Cooney, M., Weir, K., Moss, C. K., & Machalicek, W. (2013). Parent assessments of self-determination importance and performance for students with autism or intellectual disability. American Journal on Intellectual and Developmental Disabilities, 118(1), 16–31.
Carter, E. W., Owens, L., Trainor, A. A., Sun, Y., & Swedeen, B. (2009). Self-determination skills and opportunities of adolescents with severe intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 114(3), 179–192. https://doi.org/10.1352/1944-7558-114.3.179.
Cheak-Zamora, N., Teti, M., & Tait, A. (2020). Development and initial-testing of a health-related independence measure for autistic young adults as reported by caregivers. Autism in Adulthood (in press).
Cheak-Zamora, N. C., Farmer, J. E., Mayfield, W. A., Clark, M. J., Marvin, A. R., Law, J. K., et al. (2014). Health care transition services for youth with autism spectrum disorders. Rehabilitation Psychology, 59(3), 340.
Cheak-Zamora, N. C., & Teti, M. (2015). “You think it’s hard now… It gets much harder for our children”: Youth with autism and their caregiver’s perspectives of health care transition services. Autism, 19(8), 992–1001.
Cheak-Zamora, N. C., Teti, M., & First, J. (2015). ‘Transitions are scary for our kids, and they’re scary for us’: Family member and youth perspectives on the challenges of transitioning to adulthood with autism. Journal of Applied Research in Intellectual Disabilities, 28(6), 548–560.
Cheak-Zamora, N. C., Teti, M., Maurer-Batjer, A., & Koegler, E. (2017). Exploration and comparison of adolescents with autism spectrum disorder and their caregiver’s perspectives on transitioning to adult health care and adulthood. Journal of pediatric psychology, 42(9), 1028–1039.
Cheak-Zamora, N. C., Teti, M., Maurer-Batjer, A., O’Connor, K. V., & Randolph, J. K. (2019). Sexual and relationship interest, knowledge, and experiences among adolescents and young adults with autism spectrum disorder. Archives of sexual Behavior, 48(8), 2605–2615.
Cheak-Zamora, N. C., Yang, X., Farmer, J. E., & Clark, M. (2013). Disparities in transition planning for youth with autism spectrum disorder. Pediatrics, 131(3), 447–454.
Chou, Y.-C., Wehmeyer, M. L., Palmer, S. B., & Lee, J. (2016). Comparisons of self-determination among students with autism, intellectual disability, and learning disabilities: A multivariate analysis. Focus on Autism and Other Developmental Disabilities, 32(2), 124–132. https://doi.org/10.1177/1088357615625059.
Clark, L. A., & Watson, D. (1995). Constructing validity: Basic issues in objective scale development. Psychological Assessment, 7(3), 309.
Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334.
Davis, A. M., Brown, R. F., Taylor, J. L., Epstein, R. A., & McPheeters, M. L. (2014). Transition care for children with special health care needs. Pediatrics, 134(5), 900.
Ferris, M., Cohen, S., Haberman, C., Javalkar, K., Massengill, S., Mahan, J. D., et al. (2015). Self-management and transition readiness assessment: Development, reliability, and factor structure of the STARx questionnaire. Journal of Pediatric Nursing, 30(5), 691–699.
Ferris, M. E., Harward, D. H., Bickford, K., Layton, J. B., Ferris, M. T., Hogan, S. L., et al. (2012). A clinical tool to measure the components of health-care transition from pediatric care to adult care: The UNC TRxANSITION Scale. Renal Failure, 34(6), 744–753.
Flora, D. B., & Curran, P. J. (2004). An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods, 9(4), 466.
Gabriel, P., McManus, M., Rogers, K., & White, P. (2017). Outcome evidence for structured pediatric to adult health care transition interventions: A systematic review. The Journal of Pediatrics, 188, 263–269.e15. https://doi.org/10.1016/j.jpeds.2017.05.066.
Golnik, A., Ireland, M., & Borowsky, I. W. (2009). Medical homes for children with autism: A physician survey. Pediatrics, 123(3), 966–971.
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381.
HealthMeasures. (2013). PROMIS instrument development and validation scientific standards. Version 2.0. Retrieved November 1, 2019, from https://www.healthmeasures.net/images/PROMIS/PROMISStandards_Vers2.0_Final.pdf.
Hess, J. S., & Straub, D. M. (2010). Brief report: Preliminary findings from a pilot health care transition education intervention for adolescents and young adults with special health care needs. Journal of Pediatric Psychology, 36(2), 172–178.
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55.
Interagency Autism Coordinating Committee (IACC). (2017). Interagency Autism Coordinating Committee Strategic Plan for Autism Spectrum Disorder (ASD) Research—2016 Update. U.S. Department of Health and Human Services Interagency Autism Coordinating. Retrieved from https://iacc.hhs.gov/publications/strategic-plan/2017/.
Johnson, S. A., Filliter, J. H., & Murphy, R. R. (2009). Discrepancies between self-and parent-perceptions of autistic traits and empathy in high functioning children and adolescents on the autism spectrum. Journal of Autism and Developmental Disorders, 39(12), 1706–1714.
Kuhlthau, K. A., Delahaye, J., Erickson-Warfield, M., Shui, A., Crossman, M., & van der Weerd, E. (2016). Health care transition services for youth with autism spectrum disorders: Perspectives of caregivers. Pediatrics, 137(Supplement 2), S158–S166. https://doi.org/10.1542/peds.2015-2851N.
Lerner, M. D., Calhoun, C. D., Mikami, A. Y., & De Los Reyes, A. (2012). Understanding parent–child social informant discrepancy in youth with high functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(12), 2680–2692.
Levy, A., & Perry, A. (2011). Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders, 5(4), 1271–1282.
Li, C. (2016). (2016) Confirmatory factor analysis with ordinal data: Comparing robust maximum likelihood and diagonally weighted least squares. Behavioral Research, 48, 936–949. https://doi.org/10.3758/s13428-015-0619-7.
MacCallum, R. C., Browne, M. W., & Sugawara, H. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1(2), 130–149.
McManus, M., White, P., Barbour, A., Downing, B., Hawkins, K., Quion, N., et al. (2015). Pediatric to adult transition: A quality improvement model for primary care. Journal of Adolescent Health, 56(1), 73–78.
Muskens, J. B., Velders, F. P., & Staal, W. G. (2017). Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: A systematic review. European Child & Adolescent Psychiatry, 26(9), 1093–1103. https://doi.org/10.1007/s00787-017-1020-0.
Nathenson, R. A., & Zablotsky, B. (2017). The transition to the adult health care system among youths with autism spectrum disorder. Psychiatric Services, 68(7), 735–738.
Paradiz, V., Kelso, S., Nelson, A., & Earl, A. (2018). Essential self-advocacy and transition. Pediatrics, 141(Supplement 4), S373–S377. https://doi.org/10.1542/peds.2016-4300P.
Sawicki, G. S., Lukens-Bull, K., Yin, X., Demars, N., Huang, I.-C., Livingood, W., et al. (2009). Measuring the transition readiness of youth with special healthcare needs: Validation of the TRAQ—transition readiness assessment questionnaire. Journal of Pediatric Psychology, 36(2), 160–171. https://doi.org/10.1093/jpepsy/jsp128.
Schwartz, L., Tuchman, L., Hobbie, W., & Ginsberg, J. (2011). A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child: Care, Health And Development, 37(6), 883–895.
Shattuck, P. T., Lau, L., Anderson, K. A., & Kuo, A. A. (2018). A national research agenda for the transition of youth with autism. Pediatrics, 141(Supplement 4), S355–S361.
Shogren, K. A., Wehmeyer, M. L., Palmer, S. B., Rifenbark, G. G., & Little, T. D. (2015). Relationships between self-determination and postschool outcomes for youth with disabilities. The Journal of Special Education, 48(4), 256–267.
Soke, G. N., Maenner, M. J., Christensen, D., Kurzius-Spencer, M., & Schieve, L. A. (2018). Prevalence of co-occurring medical and behavioral conditions/symptoms among 4- and 8-year-old children with autism spectrum disorder in selected areas of the United States in 2010. Journal of Autism and Developmental Disorders, 48(8), 2663–2676. https://doi.org/10.1007/s10803-018-3521-1.
Stratis, E. A., & Lecavalier, L. (2015). Informant agreement for youth with autism spectrum disorder or intellectual disability: A meta-analysis. Journal of Autism and Developmental Disorders, 45(4), 1026–1041.
Tanaka, J. S. (1993). Multifaceted conceptions of fit in structural equation models. In K. A. Bollen & J. S. Long (Eds.), Testing structural equation models. Newbury Park, CA: Sage.
Terwee, C. B., Bot, S. D., de Boer, M. R., van der Windt, D. A., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42.
Teti, M., Cheak-Zamora, N., Bauerband, L., & Maurer-Batjer, A. (2019). A qualitative comparison of caregiver and youth with autism perceptions of sexuality and relationship experiences. Journal of Developmental & Behavioral Pediatrics, 40(1), 12–19.
Walsh, C., Jones, B., & Schonwald, A. (2017). Health care transition planning among adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(4), 980–991.
Wehmeyer, M. L., & Palmer, S. B. (2003). Adult Outcomes for students with cognitive disabilities three-years after high school: The impact of self-determination. Education and Training in Developmental Disabilities, 38(2), 131–144.
Weiss, J. A., Isaacs, B., Diepstra, H., Wilton, A. S., Brown, H. K., McGarry, C., et al. (2018). Health concerns and health service utilization in a population cohort of young adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(1), 36–44.
White, P. H., Cooley, W. C., & American Academy of Pediatrics, American Academy of Family Physicians. (2018). Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics, 142(5), e20182587.
Wolman, J., Campeau, P., Dubois, P., Mithaug, D., & Stolarski, V. (1994). AIR self-determination scale and user guide (p. 26). Palo Alto, CA: American Institute for Research.
Zhang, L. F., Ho, J. S., & Kennedy, S. E. (2014). A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatrics, 14(1), 4. https://doi.org/10.1186/1471-2431-14-4.
Funding
Funding was provided by Department of Defense Autism Idea Development Award No. W81XWH-14-1-0604.
Author information
Authors and Affiliations
Contributions
NCZ conceptualized the study, conducted some data analysis, and wrote the manuscript; GP conducted the quantitative analysis and contributed to writing the manuscript; ALM assisted in conceptualizing and contributed to the writing the manuscript; DB contributed to conceptualizing the study and contributed to the writing; JF helped with conceptualization of the study and some writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Department of Defense, U.S. Army Medical Research and Development Command (USAMRDC) Office of Research Protections, Human Research Protection Office (HRPO) Study number Proposal AR130405) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheak-Zamora, N., Petroski, G., La Manna, A. et al. Validation of the Health-Related Independence for Young Adults with Autism Spectrum Disorder Measure- Caregiver Version. J Autism Dev Disord 51, 2036–2046 (2021). https://doi.org/10.1007/s10803-020-04690-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-020-04690-2