Abstract
Examined the psychiatric and clinical correlates of loss of previously acquired skills (regression) as reported by parents of youth with autism spectrum disorder (ASD). Study sample comprised 6- to 18-year old (N = 213) children and adolescents with ASD. Parents reported regression in 77 (36%) youth. A more homogeneous subgroup with regression between 18 and 36 months (n = 48) had higher rates of intellectual disability, epilepsy, and special education, more socially restrictive educational settings, and more severe ASD communication deficits and schizophrenia spectrum symptoms than non-regressed youth (n = 136). Similar results were obtained for a more inclusive definition of regression (n = 77). A brief parent report of developmental regression may be a useful clinical indicator of later general functioning.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
A significant minority of youth with autism spectrum disorder (ASD) experience loss of pre-acquired skills during the preschool years. Although rates vary as a function of defining criteria (e.g., age at onset, type of skill) and assessment methodology (e.g., questionnaire, structured interview), a recent meta-analysis of 85 studies puts the rate of developmental regression at 32% with a mean onset of 1.78 years (Barger et al. 2013). Among the most consistent findings is that regression is associated with intellectual disability (ID) and more severe ASD symptoms. Additional evidence of greater risk for aberrant neural function in regression is found in higher rates of epilepsy/seizure disorder (e.g., Hansen et al. 2008; Tuchman and Rapin 1997), atypical brain development prior to the onset of regression (Nordahl et al. 2011), and prodromal developmental disturbances (e.g., Malhi and Singhi 2012). Nevertheless, other research findings about the clinical correlates of developmental regression are mixed, and different assessment strategies result in conflicting conclusions, all of which raise questions about the clinical utility of the routine gathering of such developmental information from parents.
Although much is written about regression in ASD (reviewed by Barger et al. 2013; Matson and Kozlowski 2010; Rogers 2004; Stefanatos 2008), very little research has focused on non-ASD psychiatric co-morbidity. This is surprising as children with ASD are at high risk for co-occurring psychopathology compared with typically developing peers, and at comparable risk for DSM-defined non-ASD psychiatric syndromes as youth referred for outpatient child psychiatric evaluation (e.g., Gadow et al. 2005; Kaat et al. 2013; Simonoff et al. 2008). Given associations of regression with intellectual disability, speech and language dysfunction, and encephalopathy (Barger et al. 2013; Matson and Kozlowski 2010; Rogers 2004; Stefanatos 2008) as well as the well-documented relation of these variables and psychiatric symptoms, it seems reasonable to hypothesize that developmental regression may also be associated with increased risk for psychopathology in youth with ASD.
Prior studies using dimensional symptom scales have generally found no or few differences in severity of psychopathology in developmentally regressed versus non-regressed groups (Hansen et al. 2008; Jones and Campbell 2010; Werner et al. 2005). However, these studies examined emotional and behavioral problems in children under 6 years of age, well before many psychiatric disorders begin to emerge. There are reports of greater severity of psychiatric symptoms and challenging behaviors in regressed youth (e.g., Matson et al. 2010). With regard to psychiatric syndromes, one chart review study found comparable rates of parent-reported mood disorders and aggressive/self-injurious behaviors in regressed and non-regressed youth (Ming et al. 2008), whereas a large-scale online survey recorded lower rates of parent-reported psychiatric diagnoses in regressed versus non-regressed youth (Rosenberg et al. 2011). Findings for family history of psychopathology also fail to show higher rates in regressed youth (Christopher et al. 2004). Collectively, the results of the aforementioned studies are mixed. Moreover, although they provide important information about regression in children with ASD, their diverse samples and methods for assessing regression and behavior problems as well as limited bandwidth of clinical correlates leave many unanswered questions about the value of parent-reported regression in everyday clinical settings.
The primary objective of the present study was to characterize the correlates of parent-reported developmental regression (i.e., psychiatric symptoms and general functioning) in order to validate the clinical utility of this procedure. Parents of children with ASD completed a background questionnaire (development, medical, academic, social, and mental health history) at intake that included a section about loss of pre-existing skills (communication; social interaction and responsiveness; play and imagination; academic or vocational skills; motor skills; and toileting). Because some (but not all) prior studies suggest regression is associated with higher rates of epilepsy, lower IQ, as well as greater ASD severity, we predicted similar associations in the present study. We also examined the psychiatric symptom profile associated with regression as reported by parents using a well-validated measure as well as ecologically valid outcomes such as school functioning and teacher-reported psychiatric symptomatology. Evidence of associations with current clinical status and functioning would support gathering such information at initial referral for developmental evaluation as well as routine clinical care. To the extent that regression demonstrates robust links to clinical outcomes in cross-sectional studies, then it may offer prognostic value to be tested in follow-up studies.
Methods
Participants
Case records for consecutive referrals to a university hospital developmental disabilities specialty clinic located on Long Island, NY, were screened for children who were between 6 and 18 years old (M = 10.7, SD = 3.4) at time of evaluation. Data analyses were limited to youth with a diagnosed ASD and whose case records contained the prerequisite measures. The sample (N = 213) was primarily male (81%) and parent-identified European geographic ancestry/Caucasian/White (85%). A minority (26%) of youth had IQs <70. Most children were receiving some type of intervention, including psychotropic medication (42%) or special education (76%). A subgroup of these youth is described in prior publications (Gadow 2012; Gadow et al. 2016; Kaat et al. 2013). This study was approved by a university Institutional Review Board and appropriate measures were taken to protect child and caregiver confidentiality.
Procedure
Prior to their initial evaluation, parents are asked to complete an assessment battery that includes a DSM-IV-referenced behavior rating scale, i.e., the Child and Adolescent Symptom Inventory-4R (CASI-4R) (Gadow and Sprafkin 2005) and developmental history questionnaire, Parent Questionnaire (Gadow et al. 2008). Parents are also asked to deliver a packet of materials to the school with instructions that requests the youth’s teacher to complete the CASI-4R and the school to provide copies of psycho-educational evaluations to include IQ test results. Schools mailed their information directly to the clinic. Parents’ ratings were completed primarily by the child’s mother (>90%). Intake evaluations included interviews with the children and their caregivers; informal observation of parent–child interaction; and review of the assessment battery.
ASD diagnoses were confirmed by an expert diagnostician and based on five sources of information: (a) comprehensive developmental history, (b) clinician interview with child and caregiver(s), (c) direct observations of the child, (d) the CASI-4R, which includes the symptoms of ASD (DeVincent and Gadow 2009; Gadow et al. 2008), and (e) in most cases (69%) the Autism Diagnostic Observation Schedule (ADOS) (Lord et al. 2000) administered by a certified examiner. The only exceptions were children with a prior well-documented diagnosis of ASD (e.g., prior clinician or school evaluations) who received all of the aforementioned assessments but not the ADOS, and these cases were more likely to have lower IQ scores, current special education services, and more severe ASD communication deficits than the ADOS-assessed group (Gadow and DeVincent 2012).
Measures
Developmental regression. At present there is no consensus definition of regression or widely accepted measure to assess it; however, as noted by Barger et al. (2013) in their meta-analysis of regression research, most investigators conceptualize regression as a loss of previously acquired skills, typically between 18 and 36 months of age. Although regression may involve a wide range of skills, communication is by far the most common followed by social skills. In the present study, parents completed the Parent Questionnaire (Gadow et al. 2008) (described below) which asks “was there a period during which your child seemed to lose skills that s/he acquired earlier, other than during a physical illness?” If “yes”, caregivers are asked to indicate the approximate age of loss of skills. Parents indicated their response for seven skill areas: communication; social interaction and responsiveness; play and imagination; academic or vocational skills; motor skills; and toileting (bladder, bowel, separately).
Psychiatric Symptoms
Informants rated youth’s behavior with either the parent or teacher version the CASI-4R (Gadow and Sprafkin 2005). Individual items bear one-to-one correspondence with DSM-IV symptoms and are rated on a scale from 0 (never) to 3 (very often). Both forms cover the symptoms of attention-deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, generalized anxiety disorder, social phobia, separation anxiety disorder (parent form only), major depressive episode, manic episode, schizophrenia spectrum, and autism spectrum disorder. Symptom severity scores are the sum of all item scores from a specific subscale. For each subscale, informants are asked whether symptoms interfere with social or academic functioning (i.e., impairment). Impairment is also rated on a 4-point scale (impairment severity), and the Impairment Cutoff score is a rating of often or very often. Numerous studies indicate CASI-4R subscales demonstrate satisfactory psychometric properties in youth with ASD. Specifically, individual symptom dimensions evidence satisfactory internal consistency (Cronbach’s alpha), test–retest reliability, convergent and divergent validity with respective measures from a range of relevant assessment instruments and diagnostic procedures in community-based normative and clinic-referred samples, and are minimally correlated with age, gender, IQ, and SES (Gadow and Sprafkin 2015).
Clinical Correlates
The Parent Questionnaire (Gadow et al. 2008) obtains information about four domains of variables: Child characteristics were age, gender (male = 0, female = 1), ethnicity (White = 0, non-White = 1), and IQ ≥ 70 (no = 0, yes = 1). IQ scores were obtained from school evaluations. Family characteristics were maternal education using Hollingshead (1975) criteria, income level (1–6), single parent (no = 0, yes = 1), and family history of psychopathology (no = 0, yes = 1). For the latter, parents indicated from a list of 16 disorders whether any members of the child’s family (first and second degree relatives) had the problem and whether the relative was “on the mother’s [or father’s] side of the family”. Medical characteristics were ever hospitalized for a non-psychiatric medical condition (no = 0, yes = 1), number of non-psychiatric medical conditions (1 of 7 types of child medical conditions, e.g., seizures, asthma, emergency room visits), any medical condition (no = 1, yes = 1), number of pregnancy complications, which included eight types of prenatal (e.g., high blood pressure, Rh incompatibility, gestational diabetes) and nine types of peri- or postnatal (e.g., premature delivery, cesarean section, infant oxygen) birth complications, any pregnancy complication (no = 0, yes = 1), number of prior pregnancies, and epilepsy/seizure disorder (no = 0, yes = 1). Treatment characteristics were early childhood special education (n = 0, yes = 1), currently receiving special education (no = 0, yes = 1), degree of social integration with non-special education peers (0–5), and lifetime and current psychotropic medication for an emotional or behavioral disorder (no = 0, yes = 1).
Statistical Analyses
Separate Chi square tests (categorical variables) and t tests (continuous variables) were conducted to examine differences between groups with and without developmental regression. At present, it is not known whether more broad or restrictive definitions of regression evidence closer links to clinical markers. Thus, we consider both a conventional/homogeneous definition for primary analyses and more inclusive definition for secondary analyses. The more restrictive and widely adopted criteria for developmental regression are loss of previously acquired communication and social skills between 18 and 36 months of age (Barger et al. 2013), whereas the more broadly based definition disregards age of onset and type of skill (referred to here as full inclusion grouping strategy).
To be as informative as possible, this study utilizes a large archival dataset to describe the child, family, and treatment characteristics that distinguish regressed from non-regressed youth with ASD. To balance concern of Type one and Type two errors, we adopted a more conservative p value of <0.025. We also report effect size, Cohen’s d for continuous variables and odds ratio for binary variables, to complement traditional null hypothesis testing and aid in interpretation of results. We believe this better suits the exploratory nature of this study relative to other approaches (i.e., simply restricting the number of variables). Consequently, our findings should be considered hypothesis generating rather than confirmatory.
As previously noted, ID is commonly associated with developmental regression, and correlates of the latter could be misidentified as correlates of the former. However, the high rate of co-occurrence supports the possibility that developmental regression shares common factors with ID (i.e., factors that lead to developmental regression likely result in ID and vice versa). Thus, statistical control of ID (i.e., covariation) is not indicated because it may inadvertently control for effects of developmental regression (c.f., Dennis et al. 2009). Thus, to provide insight into whether correlates of regression in the primary analyses are potentially better accounted for by ID (IQ <70), we conducted additional secondary analyses that compared regressed and non-regressed youth just among individuals without ID.
Results
Developmental Regression
Parents indicated that 77 (36%) and 136 (64%) youth, respectively, did and did not experience developmental regression according to the full inclusion grouping strategy. The more restrictive criteria for developmental regression (primary analysis) was met by 48 of the 77 regressed youth after excluding cases for whom caregivers did not indicate the month of regression (n = 14); cases for whom caregivers reported regression occurred after 36 months (n = 12); and cases for whom caregivers reported only bladder/bowel function (n = 3).
This resulted in a final sample of 48 youth with and 136 without regression for the main analyses. All but one of these 48 youth experienced regression in communication or social skills by 36 months. The distribution of regressed skills by 36 months was as follows: communication (n = 17/36%), social (n = 10/21%), or both (n = 20/42%). Of these youth, 20 (46%) had IQs <70, which is consistent with previous findings that ID and regression are strongly but not perfectly correlated.
Clinical Features
Developmentally regressed and non-regressed groups did not differ in terms of most of child, family, medical, or treatment characteristics; however, a larger percentage of the regressed group obtained IQ scores below 70, had a seizure disorder, was currently receiving special education, and was less likely to be in a classroom with typically developing peers (Table 1). When we limited our sample to youth with IQ ≥70, the regressed group continued to have significantly higher rates of epilepsy (p < .01) but not current special education (p = .10) than the non-regressed group (Supplemental Table A, available online).
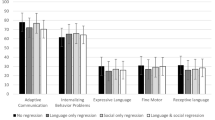
Severity of ASD
The regressed group was rated as having more severe ASD symptoms according to both parents’ and teachers’ CASI-4R ratings; however, group differences were significant for only communication deficits (Table 2), and effect sizes were in the moderate range. Social deficits and perseverative behaviors were not related to regression. When we limited our sample to youth with IQ ≥70, severity of ASD communication deficits remained higher in regressed compared to non-regressed youth when rated by parents (p = .01) but not teachers. This nonsignificant result for teacher ratings may reflect that teachers reported lower levels of communication deficits compared to parents in both groups (Supplemental Table A, available online).
Severity of Co-Occurring Psychiatric Symptoms
Parents’ CASI-4R ratings indicated that regressed youth were reported to evidence greater severity of schizophrenia spectrum disorder symptoms (p < .02, Cohen’s d = 0.41) (Table 3). Teachers’ ratings were not significant for any non-ASD psychiatric symptom dimension. When we limited our sample to youth with IQ ≥70, parent-rated schizophrenia spectrum symptoms remained significantly elevated in regressed compared to non-regressed youth (p < .01) (Supplemental Table A, available online).
Given the heterogeneity of the schizophrenia spectrum phenotype, we conducted exploratory item-level analyses to examine the association of regression with specific schizophrenia spectrum disorder symptoms. Chi-squared tests compared binary symptom endorsement by parents and teachers, separately, of regressed versus non-regressed youth (Supplementary Table B, available online). Parent ratings’ indicated significantly greater endorsement of disorganized behavior (p = .02, OR = 2.57) and avolition symptoms (p = .02, OR = 2.77) for regressed youth compared to those without regression. When restricted to youth without ID, findings were similar: parents more often endorsed strange behavior (p = .01; OR = 4.23) and avolition (p = .04; OR = 3.13) for youth with regression than without.
Impairment from Co-Occurring Psychiatric Symptoms
We also examined whether the two groups differed in terms of impairment in social or academic functioning for each CASI-4R psychiatric disorder separately (Supplemental Table C, available online). Consistent with the symptom severity ratings, the regressed group was more impaired by schizophrenia spectrum symptoms than the non-regressed group by parents (p < .01, OR = 3.22) and teachers (p < .01, OR = 3.02). When we limited our sample to youth with IQ ≥70, rates of parent-rated and teacher-rated schizophrenia impairment symptoms were elevated in the regressed group (OR >1.0), but below threshold for statistical significance (Supplemental Table A, available online).
Alternative Grouping Strategy
Secondary analyses were also conducted for the entire study sample using the full inclusion subgrouping strategy: developmental regression (n = 77) and no regression (n = 136). In terms of clinical features (Supplemental Table D, available online), severity of ASD symptoms (Supplemental Table E, available online), and severity of non-ASD symptoms (Supplemental Table F, available online), results for the full inclusion strategy were highly similar to those of the more restrictive grouping strategy; however, as might be expected, there was modest variation in effect sizes across measures. The two notable exceptions were that parents’ rated symptom severity of attention-deficit/hyperactivity disorder inattention (p = .004) and generalized anxiety disorder (p = .011) as more severe for regressed youth.
Discussion
The present study examined the case records of consecutive referrals obtained during routine intake evaluation to a developmental disabilities specialty clinic who were diagnosed with ASD according to DSM-IV criteria as to whether parent report of regression provided useful information about clinical course. Approximately one-third of cases were reported to have experienced some type of developmental regression, one-fourth between 18 and 36 months of age, typically in speech and language, which is consistent with rates reported by others (Barger et al. 2013). Youth who were reported to have experienced regression were more likely to have intellectual disability and more severe ASD communication deficits than peers with ASD but without reported regression. In line with prior research demonstrating a relation between developmental regression and seizure disorder (reviewed by Matson and Kozlowski 2010; Stefanatos 2008), children with a history of regression (23%) were more likely to have a diagnosis of epilepsy than the non-regressed group (6%). The relation between seizure disorder and autism has been reported for many years (reviewed by El Achkar and Spence 2015), and epileptiform processes may contribute to regression (Besag and Blackmon 2014) or ASD more generally (Blackmon 2015), but research is mixed. Epilepsy in ASD is also associated with ID (Berg and Plioplys 2012), which may explain their co-occurrence (Amiet et al. 2008), and possibly the relation of epilepsy with developmental regression (Viscidi et al. 2013). We address this topic in a companion publication that involves a much larger sample of youth with ASD (but includes those from the present study) as well as a comparison group of neuro-atypical, non-ASD youth (Weber and Gadow 2016).
Developmental regression was also associated with functional impairment as the regressed group was more likely to be receiving special education services and in more socially restrictive settings than non-regressed youth. In general, our results are similar with the findings of prior investigations (Barger et al. 2013; Matson and Kozlowski 2010; Rogers 2004; Stefanatos 2008); nevertheless, as previously noted, for most variables the extant literature is mixed for more broadly defined ASD (e.g., Jones and Campbell 2010). Parent report of regression obtained from a brief intake questionnaire appears to be a useful indicator of later functioning. This having been said, different strategies for assessing and defining regression will likely yield different results, and definitive conclusions will require longitudinal designs (see below).
Unexpectedly, there was little evidence that parent-reported developmental regression was associated with any of a wide range of psychiatric symptoms in youth with ASD. This is noteworthy as all of the clinical correlates examined in this study were previously found to be associated with psychiatric symptom severity or impairment in youth with ASD (Gadow et al. 2008, 2016). There was one exception, schizophrenia spectrum symptoms, and this was evident for both severity (parents’ ratings) and impairment (teachers’ and parents’ ratings), and effect sizes were moderate (Cohen 1988). Specifically, parents of regressed youth endorsed schizophrenia spectrum disorder symptoms of disorganized behavior and avolition significantly more often than those of non-regressed youth. Previous findings indicate that these symptoms, as is the case with developmental regression, evidence low to moderate correlations (0.30 < r < 0.50) with ASD symptom severity, whereas positive symptoms and for the most part disorganized thinking do not (r < 0.30) (Gadow 2013). There is some preliminary evidence that co-occurring schizophrenia spectrum traits may identify a clinically relevant sub-group within the broader ASD phenotype, and children with parent-rated impairing schizophrenia spectrum traits (versus unimpaired peers with ASD) have higher rates of ID (Gadow 2012; Gadow and DeVincent 2012). However, associations of specific schizophrenia spectrum disorder symptoms with regression did not differ when youth with ID were excluded from analyses, further supporting the unique association of regression with clinical course beyond cognitive ability. Although others have reported more severe global ratings of psychiatric symptoms and challenging behavior in regressed versus non-regressed youth with ASD (e.g., Matson et al. 2010), we were unable to locate other comparable studies of DSM-defined symptoms or syndromes.
Some of the variables found to be associated with parent-reported developmental regression in this study are associated with lower IQ and are interrelated (e.g., Berg and Plioplys 2012; Gadow and DeVincent 2012; Guilmatre et al. 2009; Mikhail et al. 2011; Sahoo et al. 2011). Nevertheless, it is important to add approximately one-half of youth with parent-reported regression had IQs ≥70. When we limited our analyses to youth with IQ ≥70, the regressed group had significantly higher rates of epilepsy and more severe schizophrenia spectrum and ASD communication deficit symptoms than non-regressed youth. Thus, these aspects of regression do not appear attributable to intellectual deficits in regressed youth, per se. On the other hand, utilization of special education classes and teacher-rated markers (communication deficits, schizophrenia spectrum impairment) did not relate to regression among youth with IQ ≥70. It may be that IQ deficits account for poor functioning in structured environments, such as the school environment, where regressed youth are less ably differentiated from non-regressed youth with ASD.
As expected, our results show that different criteria for scoring parent reports result in different rates of regression, but correlates of regression were generally consistent between the broad and narrow operationalization (i.e., comparable effect sizes). In other words, efforts to enhance homogeneity really did not result in better regression group differentiation and therefore greater clinical utility, but this is a topic that warrants further study.
This investigation has several strengths to include a relatively large sample of youth with ASD who exhibited the full range of ASD severity; a practical, cost-effective parent report of developmental regression; a relatively broad range of commonly studied child, family, medical, and treatment characteristics; a well-validated measure of co-occurring psychiatric symptoms; and examination of different criteria for developmental regression. Nevertheless, findings are subject to several qualifications. Consistent with its primary objective, this study focuses on clinic referrals and results may not generalize to community-based samples. Information about developmental regression was obtained retrospectively from parent report and therefore subject to recall bias and likely underestimates the rate of true regression (Ozonoff et al. 2010; Rogers 2004; Stefanatos 2008). However, our research was designed to examine the clinical utility of parent-reported regression as a marker of more severe clinical course and not the relative construct validity of different strategies for measuring regression (e.g., structured interview, longitudinal videotaping) (Goldberg et al. 2003), variables that may impact parental ratings (e.g., age of youth, birth order) (De Giacomo and Fombonne 1998), or their potential implications for nosology or models of pathogenesis (e.g., Matson et al. 2010; Richler et al. 2006; Rogers 2004). Scoring algorithms that include other variables such as abrupt versus gradual onset (Goldberg et al. 2003) may improve clinical utility of parent reports of regression. We also considered comparing communication regression versus social regression groups, but there were too few youth with the latter for meaningful analyses. Although we examined the relation between developmental regression and a range of clinically relevant variables in youth without ID, the results of these analyses must be considered tentative pending replication in larger samples. The present study is cross-sectional, and prospective, longitudinal designs are better suited for examining the prognostic significance of early developmental characteristics for later outcome. Future research should examine different practical procedures for eliciting important information about early development from caregivers in everyday clinical settings and strategies for parsing patients according to regression as well as the relative contribution of reports of regression in comparison with a wider range of youth and early developmental characteristics as predictors of later outcome (e.g., genetic background). Comparison with referred youth with other diagnosed psychiatric disorders would inform differential diagnosis and with typically developing toddlers and preschoolers would help establish the value of early parent report of regression as a potential clinical marker for ASD.
Conclusion
The findings of the present study support the clinical utility of asking parents about their child’s early developmental history during initial diagnostic evaluations, specifically perception of developmental regression, as a history of regression indicates increased risk for a more impacted clinical course (e.g., intellectual disability, epilepsy, ASD communication deficits, schizophrenia spectrum symptoms, special education, and social exclusion in special education services), and owing to its typical age of onset, may be of value in procurement of early intervention, which is a widely recognized clinical imperative. This may be particularly relevant in countries or geographic regions where routine access to standardized cognitive testing is limited. Furthermore, owing to the early onset of regression, it may also be of value in early detection where clear ASD symptoms have yet to present or the child’s caregivers are unaware of them.
References
Amiet, C., Gourfinkel-An, I., Bouzamondo, A., Tordjman, S., Baulac, M., Lechat, P. & Cohen, D. (2008). Epilepsy in autism is associated with intellectual disability and gender: Evidence from a meta-analysis. Biological Psychiatry, 64(7), 577–582.
Barger, B.D., Campbell, J.M., & McDonough, J.D. (2013). Prevalence and onset of regression within autism spectrum disorders: A meta-analytic review. Journal of Autism and Developmental Disorders, 43(4), 817–828.
Berg, A. T., & Plioplys, S. (2012). Epilepsy and autism: Is there a special relationship? Epilepsy & Behavior, 23(3), 193–198.
Besag, F. C., & Blackmon, K. (2014). Comments on Hughes JR. A review of recent reports on autism: 1000 studies published in 2007. Epilepsy & Behavior 2008, 13:425–437.
Blackmon, K. (2015). Structural MRI biomarkers of shared pathogenesis in autism spectrum disorder and epilepsy. Epilepsy & Behavior, 47, 172–182.
Christopher, J. A., Sears, L. L., Williams, P. G., Oliver, J., & Hersh, J. (2004). Familial, medical and developmental patterns of children with autism and a history of language regression. Journal of Developmental and Physical Disabilities, 16(2), 163–170.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd edn.). Mahwah, NJ: Lawrence Erlbaum.
De Giacomo, A., & Fombonne, E. (1998). Parental recognition of developmental abnormalities in autism. European Child and Adolescent Psychiatry, 7(3), 131–136.
Dennis, M., Francis, D. J., Cirino, P. T., Schachar, R., Barnes, M. A., & Fletcher, J. M. (2009). Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. Journal of the International Neuropsychological Society, 15(3), 331–343.
DeVincent, C. J., & Gadow, K. D. (2009). Relative clinical utility of three child symptom inventory-4 scoring algorithms for differentiating children with autism spectrum disorder versus attention-deficit hyperactivity disorder. Autism Research, 2(6), 312–321.
El Achkar, C. M., & Spence, S. J. (2015). Clinical characteristics of children and young adults with co-occurring autism spectrum disorder and epilepsy. Epilepsy & Behavior, 47, 183–190.
Gadow, K. D. (2012). Schizophrenia spectrum and attention-deficit/hyperactivity disorder symptoms in autism spectrum disorder and controls. Journal of the American Academy of Child and Adolescent Psychiatry, 51(10), 1076–1084.
Gadow, K. D. (2013). Association of schizophrenia spectrum and autism spectrum disorder (ASD) symptoms in children with ASD and clinic controls. Research in Developmental Disabilities, 34(4), 1289–1299.
Gadow, K. D., DeVincent, C., & Schneider, J. (2008). Predictors of psychiatric symptoms in children with an autism spectrum disorder. Journal of Autism and Developmental Disorders, 38, 1710–1720.
Gadow, K. D., & DeVincent, C. J. (2012). Comparison of children with autism spectrum disorder with and without schizophrenia spectrum traits: Gender, season of birth, and mental health risk factors. Journal of Autism and Developmental Disorders, 42(11), 2285–2296.
Gadow, K. D., DeVincent, C. J., Pomeroy, J., & Azizian, A. (2005). Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism: The international journal of research and practice, 9(4), 392–415.
Gadow, K. D., Perlman, G., Ramdhany, L., & de Ruiter, J. (2016). Clinical correlates of co-occurring psychiatric and autism spectrum disorder (ASD) symptom-induced impairment in children with ASD. Journal of Abnormal Child Psychology, 44, 129–139.
Gadow, K. D., Schwartz, J., DeVincent, C. J., Strong, G., & Cuva, S. (2008). Clinical utility of autism spectrum disorder scoring algorithms for the Child Symptom Inventory. Journal of Autism and Developmental Disorders, 38(3), 419–427.
Gadow, K. D., & Sprafkin, J. (2005). Child and Adolescent Symptom Inventory–4R. Stony Brook. NY: Checkmate Plus.
Gadow, K. D., & Sprafkin, J. (2015). The Symptom Inventories: An annotated bibliography. Stony Brook, NY: Checkmate Plus. http://www.checkmateplus.com.
Goldberg, W. A., Osann, K., Filipek, P. A., Laulhere, T., Jarvis, K., Modahl, C. & Spench, M. A. (2003). Language and other regression: Assessment and timing. Journal of Autism and Developmental Disorders, 33(6), 607–616.
Guilmatre, A., Dubourg, C., Mosca, A. L., Legallic, S., Goldenberg, A., Drouin-Garraud, V., … & Campion, D (2009). Recurrent rearrangements is synaptic and neurodevelopmental genes and shared biologic pathways in schizophrenia, autism, and mental retardation. Archives of General Psychiatry, 66(9), 947–956.
Hansen, R. L., Ozonoff, S., Krakowiak, P., Angkustsiri, K., Jones, C., Deprey, L. J., & Hertz-Picciotto, I. (2008). Regression in autism: Prevalence and associated factors in the CHARGE study. Ambulatory Pediatrics, 8(1), 25–31.
Hollingshead AB. (1975). Four Factor Index of Social Status. Unpublished working paper from the Department of Sociology. New Haven, CT, Yale University, Retrieved from http://www.academia.edu/927771/ Four_Factor_Index_of_Social_Status.
Hughes, J. R. (2009) Update on autism: A review of 1300 reports published in 2008. Epilepsy & Behavior. Epilepsy & Behavior 16, 569–589.
Hughes, J. R. (2009) Update on autism: A review of 1300 reports published in 2008. Epilepsy & Behavior. Epilepsy & Behavior 40, 37–41.
Jones, L. A., & Campbell, J. M. (2010). Clinical characteristics associated with language regression for children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(1), 54–62.
Kaat, A. J., Gadow, K. D., & Lecavalier, L. (2013). Psychiatric symptom impairment in children with autism spectrum disorders. Journal of Abnormal Child Psychology, 41(6), 959–969.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H. Jr., Leventhal, B. L., DiLavore, P. C., & Rutter, M. (2000). The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223.
Malhi, P., & Singhi, P. (2012). Regression in children with autism spectrum disorders. Indian Journal of Pediatrics, 79(10), 1333–1337.
Matson, J. L., & Kozlowski, A. M. (2010). Autistic regression. Research in Autism Spectrum Disorders, 4(3), 340–345.
Matson, J. L., Wilkins, J., & Fodstad, J. C. (2010). Children with autism spectrum disorders: A comparison of those who regress vs. those who do not. Developmental Neurorehabilitation, 13(1), 37–45.
Mikhail, F. M., Lose, E. J., Robin, N. H., Descartes, M. D., Rutledge, K. D., Rutledge, S. L., & Carroll, A. J. (2011). Clinically relevant single gene or intragenic deletions encompassing critical neurodevelopmental genes in patients with developmental delay, mental retardation, and or autism spectrum disorders. American Journal of Medical Genetics Part A, 155(10), 2386–2396.
Ming, X., Brimacombe, M., Chaaban, J., Zimmerman-Bier, B., & Wagner, G. C. (2008). Autism spectrum disorders: Concurrent clinical disorders. Journal of Child Neurology, 23(1), 6–13.
Nordahl, C. W., Lange, N., Li, D. D., Barnett, L. A., Lee, A., Buonocore, M. H., & Amaral, D. G. (2011). Brain enlargement is associated with regression in preschool-age boys with autism spectrum disorders. Proceedings of the National Academy of Sciences of the United States of America, 108(5), 20195–20200.
Ozonoff, S., Iosif, A. M., Baguio, F., Cook, I. C., Hill, M. M., Hutman, T., & Young, G. S. (2010). A prospective study of the emergence of early behavioral signs of autism. Journal of the American Academy of Child & Adolescent Psychiatry, 49(3), 256–266.
Richler, J. L., Luyster, R., Risi, S., Hsu, W. L., Dawson, G., Bernier, R., & Lord, C. (2006). Is there a ‘regressive phenotype’ of autism spectrum disorder associated with the measles-mumps-rubella vaccine? A CPEA study. Journal of Autism and Developmental Disorders, 36(3), 299–316.
Rogers, S. J. (2004). Developmental regression in autism spectrum disorders. Mental Retardation and Developmental Disabilities Research Reviews, 10(2), 139–143.
Rosenberg, R. E., Kaufmann, W. E., Law, J. K., & Law, P. A. (2011). Parent report of community psychiatric comorbid diagnoses in autism spectrum disorders. Autism Research and Treatment, (ID 405849). doi:10.1155/2011/405849.
Sahoo, T., Theisen, A., Rosenfeld, J. A., Lamb, A. N., Ravnan, J. B., Schultz, R. A., & Shaffer, L. G. (2011). Copy number variants of schizophrenia susceptibility loci are associated with a spectrum of speech and developmental delays and behavior problems. Genetics in Medicine, 13(10), 868–880.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47(8), 921–929.
Stefanatos, G. A. (2008). Regression in autistic spectrum disorders. Neuropsychology Review, 18(4), 305–319.
Tuchman, R. F., & Rapin, I. (1997). Regression in pervasive developmental disorders: Seizures and epileptiform electroencephalogram correlates. Pediatrics, 99(4), 560–566.
Viscidi, E. W., Triche, E. W., Pescosolido, M. F., McLean, R. L., Joseph, R. M., et al. (2013). Clinical characteristics of children with autism spectrum disorder and co-occurring epilepsy. PLoS one, 8(7), e67797. doi:10.1371/journal.pone.0067797.
Weber, B. J., & Gadow, K. D. (2016). Relation of psychiatric symptoms with epilepsy, asthma, and allergy in youth with ASD vs. psychiatry referrals. Journal of Abnormal Child Psychology. doi:10.1007/s10802-016-0212-2.
Werner, E., Dawson, G., Munson, J., & Osterling, J. (2005). Variation in early developmental course in autism and its relation with behavioral outcome at 3–4 years of age. Journal of Autism and Developmental Disorders, 35(3), 337–350.
Funding
This study was supported, in part, by the Matt and Debra Cody Center for Autism and Developmental Disabilities.
Author Contributions
Dr. Gadow conceived of the study, designed the data collection instrument, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Perlman and Ms. Weber carried out the data analyses, helped draft the initial manuscript, and approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.D. Gadow: Shareholder, Checkmate Plus, publisher of the Child and Adolescent Symptom Inventory; G. Perlman: This author has no conflicts of interest relevant to this article to disclose; and R. Weber: This author has no conflicts of interest relevant to this article to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gadow, K.D., Perlman, G. & Weber, R.J. Parent-Reported Developmental Regression in Autism: Epilepsy, IQ, Schizophrenia Spectrum Symptoms, and Special Education. J Autism Dev Disord 47, 918–926 (2017). https://doi.org/10.1007/s10803-016-3004-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-016-3004-1