Abstract
In this study, we explored potential associations among self-injurious behaviors (SIB) and a diverse group of protective and risk factors in children with autism spectrum disorder from two databases: Autism and Developmental Disabilities Monitoring (ADDM) Network and the Autism Speaks-Autism Treatment Network (AS-ATN). The presence of SIB was determined from children’s records in ADDM and a parent questionnaire in AS-ATN. We used multiple imputation to account for missing data and a non-linear mixed model with site as a random effect to test for associations. Despite differences between the two databases, similar associations were found; SIB were associated with developmental, behavioral, and somatic factors. Implications of these findings are discussed in relation to possible etiology, future longitudinal studies, and clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that includes social and communication impairments, and restricted and repetitive patterns of behaviors, interests, or activities (APA 2013). Behavioral disturbances, including self-injurious behaviors (SIB), are frequently reported in ASD (Ando and Yoshimura 1979; Baghdadli et al. 2003; Duerden et al. 2012; Minshawi et al. 2014a; Rattaz et al. 2015; Soke et al. 2016; Weiss 2002).
SIB typically occur without an apparent intent of willful self-harm (Fee and Matson 1992), but unintentional harm is common. SIB are often highly repetitive and rhythmic, and include diverse behaviors, such as head banging, head rubbing, eye poking, hair pulling, and self-biting (MacLean and Symons 2002; Minshawi et al. 2014a; Weiss 2002). The etiology of SIB is not completely understood, however, both biological (e.g., genetic and somatic conditions) and environmental factors (i.e., inability to communicate and interact with others) have been implicated (Carr 1977; Devine 2014; Guess and Carr 1991; Kurtz et al. 2012). In some children with developmental disabilities, SIB may serve a number of functions, including getting attention, avoiding challenging tasks, and self-regulation (Kurtz et al. 2003).
Intensive behavioral and pharmacological interventions that target challenging behaviors, including SIB, may lead to better outcomes in some children with developmental disabilities (Eikeseth 2009; Minshawi et al. 2014b; Richman 2008). However, in general, SIB are difficult to manage and may result in injuries, hospitalizations, death, and exclusion from educational or vocational activities, or admission to residential facilities (Devine 2014; Ianuzzi et al. 2015; Mandell 2008; Minshawi et al. 2014b). Further, SIB have a negative effect on the well-being of other family members and increase the societal costs of services in those with developmental disabilities (Devine 2014; Ianuzzi et al. 2015; Kalb et al. 2012).
In order to improve the management of SIB in ASD, a better understanding of their risk factors is needed, but large epidemiological studies are lacking. Some previous studies on SIB in individuals with ASD failed to find significant associations between SIB and sex, race/ethnicity, developmental regression, or gastrointestinal (GI) problems (Baghdadli et al. 2003; Horovitz et al. 2011; Kozlowski et al. 2012; Lance et al. 2014; Maenner et al. 2012; Wiggins et al. 2009). Significant associations between SIB and low intelligence quotient (IQ) or low adaptive skills have been reported (Ando and Yoshimura 1978; Baghdadli et al. 2003; Duerden et al. 2012). SIB have also been associated with the presence of other psychiatric comorbidities and challenging behaviors (e.g., aggression, anxiety) (Carroll et al. 2014; Kanne and Mazurek 2011), sleep problems, or abnormalities in sensory processing (Duerden et al. 2012; Goldman et al. 2011). In some studies, associations between SIB and child age were found (Baghdadli et al. 2003; Esbensen et al. 2009), while others did not (Duerden et al. 2012; Murphy et al. 2009). In two studies, associations with autism severity were reported (Baghdadli et al. 2003; Rattaz et al. 2015), however, another study did not find such an association (Duerden et al. 2012). The effects of parental or family characteristics on the occurrence of SIB is an area that is understudied. Baghdadli et al. (2003) and Schroeder et al. (2014) did not find an association between parental social class, maternal education and SIB, respectively.
Many of the above studies used small clinical samples. Findings from these small studies may be subject to selection bias, since these studies were more likely to include those with the most severe symptoms or those who can access services. Further, small clinic-based studies may be under-powered and have limited external validity. Large epidemiological studies of a range of risk factors for SIB in a more diverse sample of persons with ASD are needed. IQ and maternal education have been found to modify some associations in those with ASD. For example, the relationship between ratings of autism symptoms and maternal age varied according to the level of maternal education (Hattier et al. 2013). Similarly, Kalkbrenner et al. (2012) found that the association between maternal smoking and ASD was only significant in those with higher IQ. The possibility of an effect modification by IQ or maternal education on the factors associated with SIB have not been considered in studies of SIB in ASD.
The primary goal of this study was to assess factors associated with SIB in two large and distinct national samples of children with ASD, allowing consistency of the findings in two datasets to be examined. Based on results from past studies, the following factors were considered: child variables (e.g., sex, cognitive and adaptive delays, co-occurring conditions). Additionally, we included parent (parental age and maternal education), and family variables (e.g., type of health insurance and census tract median income). A secondary goal was to determine if any associations found were modified by child sex, IQ, or maternal education.
Methods
Study Design
This is a cross-sectional, secondary analysis of data from a surveillance system and a clinic-based registry of children with ASD. This study was approved by both the Autism and Developmental Disabilities Monitoring (ADDM) Network and the Autism Speaks-Autism Treatment Network (AS-ATN) data sharing committees.
Sample
We included children with ASD from two different samples, the ADDM Network and the AS-ATN. In ADDM, children from all study sites who met the surveillance case definition for ASD during the 2000, 2006, and 2008 surveillance years were included (CDC 2007, 2009, 2012). Data from 2002 and 2004 were excluded, since changes in data collection procedures impacted the reporting of SIB. Data after 2008 were not available at the time of these analyses. The ADDM Network was started by the Centers for Disease Control and Prevention in 2000. It is an active, record-based, multiple site surveillance system for ASD and other developmental disabilities among 8-year-old children in selected areas of the United States. The ADDM methodology has been evaluated and validated by others (Avchen et al. 2011; Bakian et al. 2014; Van Narden Braun et al. 2007) and detailed descriptions of the process for surveillance classification of cases can be found in a number of publications (CDC 2007, 2009, 2012; Rice et al. 2007; Sell et al. 2012; Wiggins et al. 2012). In short, during a given surveillance year, available health records in all sites (e.g., clinician notes, results from standardized tests), and school records in some sites, of a sample of 8-year-old children with specific ICD-9 codes or eligibility for special education services, who lived in different ADDM catchment areas, were screened for trigger words describing social deficits associated with ASD, a documented diagnosis of ASD from a community provider, or an educational eligibility for services under the ASD category. Records that satisfied any of the above criteria were abstracted verbatim. Records from multiple sources for each child were combined to a composite summary that was reviewed by an expert clinician at each ADDM site using an objective coding scheme to decide whether the child met the surveillance definition for ASD based on the Diagnostic and Statistical Manual for Mental Disorders-IV-Edition-Text Revision [DSM-IV-TR] criteria (APA 2000). Census data were linked to the final ADDM dataset. In order to maintain a high quality of data, all sites were required to adhere to a common protocol; ongoing training and quality control checks were implemented for record abstractors and clinician reviewers with a reliability of 90% or greater.
The AS-ATN, initiated by Autism Speaks in 2005, is a network that currently consists of 14 academic health centers in North America. The network maintains a registry of children with ASD diagnosed in any of the participating centers. The details of the AS-ATN registry methodology have been previously published and data from this registry have been used by other researchers in the past (Coury et al. 2009; Kanne et al. 2014; Kuhlthau et al. 2010; Lajonchere et al. 2012; Perrin et al. 2012; Sikora et al. 2012). In summary, families of children, aged 2–18 years, diagnosed with ASD within the preceding 12 months and who planned to receive care in one of the AS-ATN centers were invited to participate in the registry. The diagnosis of ASD was based on clinical judgment based on the DSM-IV-TR criteria and confirmed by the Autism Diagnostic Observation-Schedule (ADOS) (Lord et al. 2000a). Children in foster care or whose parents were not fluent in both written and spoken English were not eligible for the registry. In these analyses, we included all children enrolled in the registry between 2008 and 2012.
Measures
In ADDM, data on SIB and the potential risk factors examined were obtained from available children’s health records in all sites, and school records in some sites. In the AS-ATN registry, data were collected from several instruments, including the AS-ATN demographic form, a modified questionnaire developed from the Parental Concerns Questionnaire (PCQ) (McGrew et al. 2007), as well as standardized tests, such as the Stanford Binet Scales of Intelligence-5th Edition Abbreviated Battery IQ (Roid 2003), the Mullen Scales of Early Leaning (Mullen 1995) and the Vineland Adaptive Behavior Scales (Sparrow et al. 2005).
The outcome of interest in both datasets was SIB (yes/no). In ADDM, SIB were determined by coding of their presence in available records by clinicians trained in the surveillance coding process based on the following definition of SIB: any self-directed behavior that could cause physical harm or a sign or bodily mark of the act, such as picking fingers until bleeding, sucking fingers until chapped, slapping self in face, head banging, etc. In AS-ATN, the presence of SIB was based on a parental questionnaire asking parents whether the child displayed SIB (bangs head, pinches, bites, hits oneself). Though many factors examined were similar in both datasets, some were only evaluated in one dataset. In both datasets, we examined potential associations with sex, race/ethnicity, IQ, adaptive skills, developmental regression, sleep and sensory abnormalities, maladaptive behaviors/co-occurring conditions (aggression, hyperactivity, attention problems, anxiety, mood problems). Child age, severity of ASD, parental age, maternal education, type of health insurance, and the presence of gastrointestinal (GI) disturbances were only examined in the AS-ATN dataset. Severity of ASD was based on ADOS calibrated scores (Gotham et al. 2009; Hus and Lord 2014). IQ and adaptive skills scores were analyzed as continuous in the AS-ATN, since the plots of these variables versus SIB showed continuous distributions. Sleep and GI problems, parental age were examined only in sub-analyses because these variables were only available in specific study years. We assessed potential associations with census tract median income, documentation of a previous diagnosis of ASD in the records, and genetic and neurologic conditions only in the ADDM dataset. Previous diagnosis of ASD in the records was considered a proxy for access to services.
Since a high number of variables were included in these analyses, we first estimated the variance inflation factor (VIF) and the tolerance for each variable to assess multicollinearity. None of the variables had a VIF >10 or a tolerance <0.10 (Cheng et al. 2010). Because of missing data on important variables (e.g., IQ and adaptive behaviors), we imputed missing data using the fully conditional specification (FCS) technique (Janssen et al. 2010; Langkamp et al. 2010; Lee and Carlin 2010; Rubin 1987; Van Buuren 2007). We used Proc MI in SAS to impute 10 datasets within each site to account for within site correlation. We used PROC GLIMMIX (SAS® version 9.3, Cary, NC) with an alpha level of 0.05 to assess the associations between SIB and the above factors in each imputed dataset using a non-linear mixed model because SIB was categorized (yes/no). Site was included as a random effect to account for between-site variability. Results from the 10 imputed datasets were combined using Rubin’s formula to obtain the final results (Rubin 1987). Effect modification by child sex and IQ were assessed in ADDM, while in AS-ATN, child sex, IQ, and maternal education were evaluated, using the same analytical approach described above. We primarily reported results from multiple imputation analyses.
Results
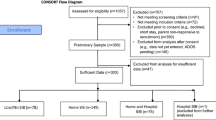
A total of 8065 participants were included in ADDM analyses and 5102 in the main AS-ATN analyses; 4615 in the first AS-ATN sub-analysis (GI and sleep problems) and 3017 in the second AS-ATN sub-analysis (parental age). The characteristics of participants are presented in Table 1.
In both datasets, SIB were significantly associated with child characteristics of impairment in adaptive behavior, developmental regression, maladaptive behaviors (e.g., aggression, hyperactivity, anxiety), sleep problems, and abnormalities in sensory processing. No significant associations were reported with child sex or race/ethnicity. In AS-ATN, SIB were significantly associated with younger child age, lower maternal education attainment, or having public health insurance, but no associations were found with GI problems, severity of ASD, or parental age. In ADDM, a significant relationship was found with lower median income in the census tract, previous diagnosis in the records, neurologic conditions, but not with genetic conditions (Table 2). No significant effect modifications by child IQ or sex were observed in either dataset nor by maternal education in AS-ATN. In general, findings from multiple imputation analyses were consistent with those from complete case analyses concerning the directionality and the significance of the associations, except in few cases (adaptive impairment and developmental conditions in ADDM; maternal age, other health insurance, and severity of ASD in the AS-ATN). Results from complete case analyses are included in the supplemental table.
Discussion
We found similarities in the results for both samples, despite differences between the two datasets (samples, way SIB were assessed, age of the participants, and methods of data collection of the different factors examined), which supports the validity of these findings.
In line with previous studies (Carroll et al. 2014; Matson et al. 2008; Rao and Landa 2014; Schroeder et al. 2014), SIB were related to behavioral factors (i.e., aggression, hyperactivity, anxiety, and mood problems). The causal nature and direction of these associations could not be determined from the cross-sectional data in our study. It is possible that these associations are due to a shared etiology. SIB and other challenging behaviors may all be the result of deficits in inhibitory mechanisms secondary to a lack of impulse control. Emotional dysregulation has been found to be among the factors that may explain this lack of impulse control (Prizant and Laurent 2011; Quek et al. 2012). Further, reporting bias may also explain these associations, as parents of children with SIB may consider these children as being “difficult” and report the presence of these other challenging behaviors. The associations between SIB and other challenging behaviors suggest that clinicians should inquire about SIB when there is a parent report of other challenging behaviors.
Similar to results reported by others (Baghdadli et al. 2003; Duerden et al. 2012), we found significant relationships between low adaptive or cognitive skills and SIB, though the association with low IQ was not statistically significant in the AS-ATN dataset. These associations support past findings that having limited social and communication skills, as in those with low IQ or low adaptive scores, may lead to self-injury, since these children may use SIB as a way of communication (Devine 2014). Further, in some children with limited adaptive skills, SIB may reflect frustration, since these children have limitations in their abilities to independently perform important activities of daily living and communicate their needs. The loss of previously-acquired skills (e.g., communication or social skills) in children who experience developmental regression may increase the likelihood of these children to use SIB as a way of communication and may explain the association between SIB and developmental regression.
The results of this study also confirmed previous reports of associations of SIB with abnormalities in sensory processing (Duerden et al. 2012, 2014) and sleep problems (Goldman et al. 2011; Sikora et al. 2012). Children with sensory disturbances may use SIB as a mechanism to regulate arousal (hypo or hyper arousal) and under these circumstances, SIB may play a function of autoregulation. As suggested by others, it is also possible that SIB are consequences of alterations in pain sensitivity secondary to structural abnormalities in the somatosensory system (Duerden et al. 2014). In their study, Goldman et al. (2011) reported that the association between SIB and sleep problems was the strongest among all the behaviors evaluated. The mechanism explaining the relationship between SIB and sleep problems is complex and not completely understood and a reverse association is also a possibility (Symons et al. 2000). Nevertheless, studies have shown that improvement in sleep has led to less SIB and repetitive behaviors in some children (Malow et al. 2014; Schreck et al. 2004).
Unlike studies done elsewhere: Baghdadli et al. (2003) in France and Schroeder et al. (2014) in Peru, we found significant associations with four factors related to socioeconomic status (SES): lower maternal level of education or having public health insurance in AS-ATN, lower median income in the census tract or having a previous diagnosis of ASD in the records in the ADDM network. It is possible that children from families with low SES are more likely to receive services if they have SIB and this may explain the documentation of SIB in their records. On the other hand, because disparities in access to ASD specialized services based on individual (Irvin et al. 2012; Liptak et al. 2008) and community factors (Thomas et al. 2012) have been reported in the United States, it is also possible that children from families with low SES are less likely to access specialized services that may address associated factors that impact SIB (e.g., sensory, sleep). Mothers with low educational attainment may also have limited coping skills or understanding of child’s development (Yu et al. 2002). Since these results have not been reported previously, these findings need to be evaluated in future studies.
A few variables were only available in one dataset. In AS-ATN, we found an association of SIB with younger chronological age, which is similar to findings from others (Baghdadli et al. 2003; Esbensen et al. 2009). This age effect may reflect the general developmental maturation with age, or differences in the duration of interventions received between younger and older children. Further, though these analyses were adjusted for study year, this age effect might also suggest high reporting of SIB in the most recent cohort of children with ASD because of an increase in awareness of co-occurring conditions, including SIB. Similar to others, we also did not find significant associations with GI problems or severity of ASD (Duerden et al. 2012; Maenner et al. 2012; Nikolov et al. 2009). In ADDM, we found a positive association of SIB with the presence of neurologic conditions, such as seizure disorders or cerebral palsy, as have others (Viscidi et al. 2014). While neurologic conditions are associated with developmental regression, our findings were still significant after controlling for developmental regression.
This study has several strengths, including large samples of children with ASD from two national datasets, diverse factors tested, the ability to assess consistency of the findings in two different datasets, use of multiple imputation to account for missing data, and exploration of effect modification. However, it has some limitations. We examined a set of factors potentially related to SIB that were retrospectively collected. Variables such as perinatal and neonatal factors, metabolic diseases, factors related to the physical and social environments of the child (quality of social interaction with caregivers, exposure to environmental toxins, parental psychiatric conditions) or the types of interventions received that might be related to SIB, were not available in our datasets. These findings may have been influenced by a selection bias since only families who were fluent in English, had access to specialized care, and agreed to be part of the registry were included in the AS-ATN and in the ADDM Network, sites are not selected to include representative samples of children with ASD. Therefore, these findings might not be representative of all the children with ASD, and might not be generalizable to the entire nation. In AS-ATN, the presence of co-occuring conditions was based on parental responses, while in ADDM, they were documented by a review of the child’s records. This difference in methods of ascertainment may explain the differences in the proportion of co-occuring conditions between the two databases. As mentioned, due to the cross-sectional design of this study, we cannot infer the temporal relationship between SIB and other behavioral factors. Multiple testing may also have influenced our findings because of the high number of statistical tests. We did not adjust for multiple comparisons because of the exploratory nature of the study and the consequences of false negative findings (Goldman 1998; Greenland 2008).
Despite these limitations, results from this analysis of two different datasets found significant associations between SIB and behavioral (aggression, hyperactivity, anxiety) developmental (adaptive behaviors, IQ, regression), and somatic (sensory abnormalities, sleep problems) factors. The consistency of our findings in two distinct datasets shows the robustness of these results and mitigates against chance alone as the explanation. Overall, though, the findings from this study require confirmation in future longitudinal studies, they are in line with past findings and also support recommendations for a comprehensive and multidisciplinary approach to evaluating and treating SIB in ASD (Isaksen et al. 2013; Minshawi et al. 2014b). In providing a comprehensive assessment of children with SIB, clinicians could identify causative or exacerbating conditions that can be managed through available interventions. Similarly, early intervention provided by clinicians could target some of the factors associated with SIB (sleep, abnormalities in sensory processing, adaptive skills), since such interventions might lead to prevention or amelioration of SIB in some children. Researchers can use these data to inform future studies, which could examine other factors (e.g., prenatal and perinatal factors, metabolic factors), in addition to those included in this study and employ longitudinal designs, allowing evaluation of temporal relationships over the life course between SIB and other factors in individuals with ASD.
References
American Psychiatric Association (APA). (2000). Diagnostic and statistical manual of mental disorders (4th ed-text revision). Washington, DC: American Psychiatric Publishing.
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders (5th edn.). Washington, DC: American Psychiatric Publishing.
Ando, H., & Yoshimura, I. (1979). Comprehension skill levels and prevalence of maladaptive behaviors in autistic and mentally retarded children. Child Psychiatry and Human Development, 9, 131–136.
Avchen, R. N., Wiggins, L., Devine, O., Van Naarden Braun, K., Rice, C., et al. (2011). Evaluation of a records-review surveillance system used to determine the prevalence of autism spectrum disorders. Journal of Autism and Developmental Disorders, 41, 227–236.
Baghdadli, A., Grisi, C., & Aussillloux, C. (2003). Risk factors for self-injurious behaviors among 222 young children with autistic disorders. Journal of Intellectual Disability Research, 47, 622–627.
Bakian, A. V., Bilder, D. A., Carbone, P. S., Hunt, T. D., Petersen, B., et al. (2014). Brief Report: Independent validation of autism spectrum disorders case status in the Utah Autism and Developmental Disabilities Monitoring (ADDM) Network site. Journal of Autism and Developmental Disorders, 45, 873–880.
Carr, E. (1977). The motivation of self-injurious behavior: A review of some hypotheses. Psychological Bulletin, 84, 800–816.
Carroll, D., Hallett, V., McDougle, C., Aman, M. G., McCracken, J. T., et al. (2014). Examination of aggression and self-injurious in children with autism spectrum disorders and serious behaviors problems. Child and Adolescent Psychiatric Clinics of North America, 23, 57–72.
Centers for Disease Control and Prevention (CDC) (2007). Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 6 sites, 2000. Mortality Morbidity Weekly Report Surveillance Summaries, 56, 1–20.
Centers for Disease Control and Prevention (CDC) (2009). Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 14 sites, 2006. Mortality Morbidity Weekly Report Surveillance Summaries, 58, 1–20.
Centers for Disease Control and Prevention (CDC) (2012). Prevalence of autism spectrum disorders—Autism and Developmental Disabilities Monitoring Network, 11 sites, 2008. Mortality Morbidity Weekly Report Surveillance Summaries, 61, 1–19.
Centers for Disease Control and Prevention (CDC) (2014). Prevalence of autism spectrum disorders among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. Mortality Morbidity Weekly Report Surveillance Summaries, 63, 1–21.
Cheng, J., Edwards, L., Maldonado-Molina, M., Komro, K., & Muller, K. (2010). Real longitudinal data analysis for real people: Building a good enough mixed model. Statistics in Medicine, 20, 504–520.
Coury, D., Jones, N., Klatka, K., Winklosky, B., & Perrin, J. M. (2009). Health care for children with autism: The Autism Treatment Network. Current Opinion in Pediatrics, 21, 828–832.
Devine, D. (2014). Self-injurious behaviors in autistic children: A neuro-developmental theory of social and environment isolation. Psychopharmacology, 231, 979–997.
Duerden, E., Card, D., Roberts, S. W., Mak-Fan, K., Chakravarty, M., et al. (2014). Self-injurious behaviors are associated with alterations in the somatosensory system in children with autism spectrum disorder. Brain Structure and Function, 219, 1251–1261.
Duerden, E., Oakley, H., Mak-Fan, K., McGrath, P., Taylor, M., et al. (2012). Risk factors associated with self-injurious behaviors in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42, 2460–2470.
Eikeseth, S. (2009). Outcomes of comprehensive psycho-educational interventions for young children with autism spectrum disorders. Research in Developmental Disabilities, 30, 158–178.
Esbensen, A., Seltzer, M. M., Lam, K. S., & Bodfish, J. W. (2009). Age-related differences in restricted repetitive behaviors in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39, 57–66.
Fee, V. E., & Matson, J. L. (1992). Definition, classification, and taxonomy. In J. K. Luiselli, J. L. Matson & N. Singh (Eds.), Self-injurious behavior: Analysis, assessment, and treatment (pp. 3–20). New York: Springer-Verlag.
Goldman, S. (1998). Multiple comparisons explained. American Journal of Epidemiology, 147, 807–811.
Goldman, S., McGrew, S., Johnson, K., Richdale, A., Clemons, T., et al. (2011). Sleep is associated with problem behaviors in children and adolescents with autism spectrum disorders. Research in Autism Spectrum Disorders, 5, 1223–1229.
Gotham, K., Pickles, A., & Lord, C. (2009). Standardizing ADOS-G scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39, 693–705.
Greenland, S. (2008). Multiple comparisons and association selection in general epidemiology. International Journal of Epidemiology, 37, 430–434.
Guess, D., & Carr, E. G. (1991). Emergence and maintenance of stereotypy and self-injury. American Journal on Mental Retardation, 96, 299–319.
Hattier, M., Matson, J., Belva, B., & Adams, H. (2013). The effects of informant age and education on childhood ASD. Research in Autism Spectrum Disorders, 7, 398–404.
Horovitz, M., Matson, J., Rieske, R., Kozolowski, A., & Sipes, M. (2011). The relationship between race and challenging behaviors in infants and toddlers with autistic disorder and pervasive developmental disorder-not otherwise specified. Developmental Neurorehabilitation, 14, 208–214.
Hus, V., & Lord, C. (2014). The Autism Diagnostic Observation Schedule, Module 4: Revised algorithm and standardized severity scores. Journal of Autism and Developmental Disorders, 44, 1996–2012.
Ianuzzi, D., Cheng, E., Broder-fingert, S., & Bauman, M. (2015). Emergency department utilization by individuals with autism. Journal of Autism and Developmental Disorders, 45, 1096–1102.
Irvin, D., McBee, M., Boyd, B., Hume, K., & Odom, S. (2012). Child and family factors associated with the use of services for preschoolers with autism spectrum disorders. Research in Autism Spectrum Disorders, 6, 565–572.
Isaksen, J., Bryn, V., Diseth, T., Heiberg, A., Schjolberg, S., et al. (2013). Children with autism spectrum disorders—The importance of medical investigations. European Journal of Paediatric Neurology, 17, 68–76.
Janssen, K., Donders, A. R., Harrell, F., Vergouwe, Y., Chen, Q., et al. (2010). Missing covariate data in medical research: To impute is better than ignore. Journal of Clinical Epidemiology, 63, 721–727.
Kalb, L. G., Stuart, E., Freedman, B., Zablotsky, B., & Vasa, R. (2012). Psychiatric-related emergency department visits among children with an autism spectrum disorder. Pediatric Emergency Care, 28, 1269–1275.
Kalkbrenner, A., Braun, J., Durkin, M., Maenner, M., Cunniff, C., et al. (2012). Maternal smoking during pregnancy and the prevalence of autism spectrum disorders, using data from the Autism and Developmental Disabilities Monitoring Network. Environmental Health Perspectives, 120, 1042–1048.
Kanne, S. M., & Mazurek, M. (2011). Aggression in children and adolescents with ASD: Prevalence and risk factors. Journal of Autism and Developmental Disorders, 41, 926–937.
Kanne, S. M., Mazurek, M., Sikora, D., Bellando, J., Branum-Martin, L., et al. (2014). The Autism Impact Measure: Initial development of a new tool for treatment outcome measurement. Journal of Autism and Developmental Disorders, 44, 168–179.
Kozlowski, A., Matson, J., & Rieske, R. (2012). Gender effects on challenging behaviors in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 6, 958–964.
Kuhlthau, K., Orlich, F., Hall, T., Sikora, D., Kovacs, E., et al. (2010). Health-related quality of life in children with autism spectrum disorders: Results from the Autism Treatment Network. Journal of Autism and Developmental Disorders, 40, 721–729.
Kurtz, P., Chin, M., Huete, J., & Cataldo, M. (2012). Identification of emerging of self-injurious behaviors in young children: A preliminary study. Journal of Mental Health Research in Intellectual Disabilities, 1, 260–285.
Kurtz, P., Chin, M., Huete, J., Tarbox, R., O’Connor, J., et al. (2003). Functional analysis and treatment of self-injurious behaviors in young children: A Summary of 30 cases. Journal of Applied Behavior Analysis, 36, 205–219.
Lajonchere, C., Jones, N., Coury, D., & Perrin, J. M. (2012). Leadership in health care, research, quality improvement for children and adolescents with autism spectrum disorders: The Autism Treatment Network and Autism Intervention. Pediatrics, 130, 1–9.
Lance, E., York, J., Lee, L. C., & Zimmerman, A. W. (2014). Association between regression and self-injurious behaviors among children with ASD. Research in Developmental Disabilities, 35, 408–413.
Langkamp, D., Lehman, A., & Lemeshow, S. (2010). Techniques for handling missing data in secondary analyses of large surveys. Academic Pediatrics, 10, 205–210.
Lee, K., & Carlin, J. (2010). Multiple imputation for missing data: Fully conditional specification versus multivariate normal imputation. American Journal of Epidemiology, 171, 624–632.
Liptak, G., Benzoni, L., Mruzek, D., Nolan, K., Thingvoll, M., et al. (2008). Disparities in diagnosis and access to health services for children with autism: Data from the National Survey of Children’s Health. Journal of Developmental and Behavioral Pediatrics, 29, 152–160.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H., Leventhal, B. L., et al. (2000a). “The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism”. Journal of Autism and Developmental Disorders, 30, 205–223.
MacLean, W. E. Jr., & Symons, F. (2002). Self-injury behaviors in infancy and young childhood. Infants and Young Children, 14, 31–41.
Maenner, M., Arneson, C., Levy, S., Kirby, R., Nicholas, J., et al. (2012). Brief report: Association between behavioral features and gastrointestinal problems among children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 42, 1520–1525.
Malow, B. A., Adkins, K. W., Reynolds, A., Weiss, S.K., Loh, A., Fawkes, D., Katz, T., et al. (2014). Parent-based sleep education for children with autism spectrum disorders. Journal Autism and Developmental Disorders, 44, 216–228.
Mandell, D. (2008). Psychiatric hospitalization among children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38, 1059–1065.
Matson, J., Cooper, C., Malone, C., & Moskow, S. (2008). The relationship of self-injurious behaviors and other maladaptive behaviors among individuals with severe and profound intellectual disabilities. Research in Developmental Disabilities, 29, 141–148.
McGrew, S., Malow, B., Henderson, L., Wang, L., Song, Y., et al. (2007). Developmental and behavioral questionnaire for autism spectrum disorders. Pediatric Neurology, 37, 108–116.
Minshawi, N., Hurtwitz, S., Morriss, D., & McDougle, C. (2014b). Multidisciplinary assessment and treatment of self-injurious behaviors in autism spectrum disorders and intellectual disability: Integration of psychological and biological theory and approach. Journal of Autism and Developmental Disorders, 45, 1541–1568.
Minshawi, N., Hurwitz, S., Fodstad, J., Biebl, S., Morris, D., et al. (2014a). The association between self-injurious behaviors and autism spectrum disorders. Psychology Research and Behavior Management, 7, 125–136.
Mullen, E. (1995). Mullen scales of early learning. Circle Pines, MN: American Guidance Service Inc.
Murphy, O., Healy, O., & Leader, G. (2009). Risk factors for challenging behaviors among 157 children with autism spectrum disorders in Ireland. Research in Autism Spectrum Disorders, 3, 474–482.
Nikolov, R., Bearss, K., Lettinga, J., Erickson, C., Rodowski, M., et al. (2009). Gastrointestinal symptoms in a sample of children with pervasive developmental disorders. Journal of Autism and Developmental Disorders, 39, 405–413.
Perrin, J. M., Coury, D. M., Jones, N., & Lajonchere, C. (2012). The Autism Treatment Network and Autism Intervention Research Network on physical health: Future directions. Pediatrics, 130, 198–201.
Prizant, B. M., & Laurent, A. (2011). Behavior is not the issue: An emotional regulation perspective on problem behavior-Part one of part-two article. Autism Spectrum Quarterly, 1, 29–30.
Quek, L. H., Sofronoff, K., Sheffield, J., White, A., & Kelly, A. (2012). Co-occurring anger in young people with Asperger’s syndrome. Journal of Clinical Psychology, 68, 1142–1148.
Rao, P., & Landa, R. (2014). Association between severity of behavioral phenotype comorbid attention deficit hyperactivity disorder symptoms in children with autism spectrum disorder. Autism: The International Journal of Research and Practice, 18, 272–280.
Rattaz, C., Michelon, C., & Baghdadli, A. (2015). Symptom severity as a risk factor for self-injurious behaviours in adolescents with autism spectrum disorders. Journal of Intellectual Disability Research, 59, 730–740.
Rice, C., Baio, J., Van Naarden Braun, K., Doernberg, N., Meaney, J., et al. (2007). A public health collaboration for the surveillance of autism spectrum disorders. Pediatric and Perinatal Epidemiology, 21, 179–190.
Richman, D. (2008). Early intervention and prevention of self-injurious behaviours exhibited by young children with developmental disabilities. Journal of Intellectual Disability Research, 52, 3–17.
Roid, G. (2003). Stanford-binet intelligence scales (5th edn.). Itasca, IL: Riverside Publishing.
Rubin, D. B. (1987). Multiple imputation for nonresponse in surveys. J. New York: Wiley and Sons.
Schreck, K. A., Mulick, J. A., & Smith, A. F. (2004). Sleep problems as possible predictors of intensified symptoms of autism. Research in Developmental Disabilities, 25, 57–66.
Schroeder, S., Marquis, J. G., Reese, R. M., Richman, D., Mayo-Ortega, L., et al. (2014). Risk factors for self-injurious, aggression, stereotyped behavior among young children at risk for intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 119, 351–370.
Sell, N. K., Giarelli, E., Blum, N., Hanlon, A., & Levy, S. (2012). A comparison of Autism Spectrum Disorder DSM-IV criteria and associated features among African American and White children in Philadelphia County. Disability and Health Journal, 5, 9–17.
Sikora, D. M., Johnson, K., Clemons, T., & Katz, T. (2012). The association between sleep problems and daytime behaviors in children of different ages with autism spectrum disorders. Pediatrics, 130, 83–90.
Soke, GN., Rosenberg, SA., Hamman, R., Fingerlin, T., Robinson, C. et al. (2016). Brief report: Prevalence of self-injurious behaviors among children with Autism Spectrum Disorder—A population-based study. Journal of Autism and Developmental Disorders, 46, 3607–3614.
Sparrow, S. S., Cicchetti, D. V., & Balla, D. A. (2005). The Vineland adaptive behavior scales-2 (survey form). Circle Pines, MN: American Guidance Service.
Symons, F., Davis, M., & Thompson, T. (2000). Self-injurious behavior and sleep disturbance in adults with developmental disabilities. Research in Developmental Disabilities, 21, 115–123.
Thomas, P., Zahorodny, W., Peng, B., Soyeon, K., Nisha, J., et al. (2012). The association of autism diagnosis with socioeconomic status. Autism: The International Journal of Research and Practice, 16, 201–213.
Van Buuren, S. (2007). Multiple imputation of discrete and continuous data by Fully Conditional Specification. Statistical Methods in Medical Research, 16, 219–242.
Van Naarden Braun, K., Pettygrove, S., Daniels, J., Miller, L., Nicholas, J., et al. (2007). Evaluation of a methodology for a collaborative multiple source surveillance network for autism spectrum disorders-autism and developmental disabilities monitoring network, 14 sites, United States, 2002. MMWR, 56, 29–40.
Viscidi, E., Johnson, A. L., Spence, S. J., Buka, S. L., Morrow, E. M., et al. (2014). The Association between epilepsy, autistic symptoms and maladaptive behaviors in children with autism spectrum disorder. Autism: The International Journal of Research and Practice, 18, 996–1006.
Weiss, J. (2002). Self-injurious behaviors in autism: A literature review. Journal on Developmental Disabilities, 9, 129–143.
Wiggins, L., Baio, J., Schieve, L., Lee, L. C., Nicholas, J., et al. (2012). Retention of autism spectrum diagnoses by community professionals: Findings from the Autism and Developmental Disabilities Monitoring Network, 2000, 2006. Journal of Developmental and Behavioral Pediatrics, 33, 387–395.
Wiggins, L., Rice, C., & Baio, J. (2009). Developmental regression in children with autism spectrum disorders identified by a population-based surveillance system. Autism: The International Journal of Research and Practice, 13, 357–374.
Yu, S. H., Park, C. H., & Schwalberg, R. H. (2002). Factors associated with smoking cessation among US pregnant women. Maternal and Child Health Journal, 6, 89–97.
Acknowledgements
We acknowledge CDC ADDM project personnel, ADDM projects coordinators, clinician reviewers, abstractors, data managers, and ADDM investigators at each site who contributed to the ADDM surveillance project and data collection. We acknowledge AS-ATN project coordinators and all families who provided data into the AS-ATN registry. This Network activity was supported by Autism Speaks and cooperative agreement UA3 MC11054 through the U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program to the Massachusetts General Hospital. This work was conducted through the Autism Speaks-Autism Treatment Network.
Author contributions
Dr. Gnakub N. Soke conceptualized and drafted the original proposal of the study, carried out the analyses, drafted the original manuscript, revised the manuscript, and approved the submission of the final manuscript; Drs. Steven A. Rosenberg, Richard F. Hamman supervised the initial manuscript, reviewed and revised the manuscript and approved the submission of the final manuscript; Drs. Cordelia Robinson and Ann Reynolds supervised the initial manuscript, contributed to data acquisition, reviewed and revised the manuscript and approved the submission of the final manuscript; Drs. Tasha Fingerlin and Carolyn DiGuiseppi supervised the initial manuscript, supervised the analyses, reviewed and revised the manuscript and approved the submission of the final manuscript; Drs. Maureen S. Durkin and Lisa Wiggins played prominent roles in reviewing and revising the manuscript and approved the submission of the final version; Drs. Laura Carpenter, Ellen Giarelli, and Li-Ching Lee reviewed and revised the manuscript and approved the submission of the final version provided feed-back on.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with ethical standards of the institutional and /or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study is a secondary data analysis of unidentified data previously collected in a surveillance system. Therefore, formal consent is not required.
Additional information
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The views expressed in this publication do not necessarily reflect the views of Autism Speaks, Inc.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Soke, G., Rosenberg, S., Hamman, R. et al. Factors Associated with Self-Injurious Behaviors in Children with Autism Spectrum Disorder: Findings from Two Large National Samples. J Autism Dev Disord 47, 285–296 (2017). https://doi.org/10.1007/s10803-016-2951-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-016-2951-x