Abstract
The prefrontal cortex and the frontoparietal network are associated with a variety of regulatory behaviors. Functional connections between these brain regions and the amygdala are implicated in risk for anxiety disorders. The prefrontal cortex and frontoparietal network are also linked to executive functioning, or behaviors that help orient action towards higher order goals. Where much research has been focused on deleterious effects of under-controlled behavior, a body of work suggests that over-controlled behavior may also pose a risk for internalizing problems. Indeed, while work suggests that high levels of attention shifting may still be protective against internalizing problems, there is evidence that high levels of inhibitory control may be a risk factor for socioemotional difficulties. In the ABCD sample, which offers large sample sizes as well as sociodemographic diversity, we test the interaction between frontoparietal network-amygdala resting state functional connectivity and executive functioning behaviors on longitudinal changes in internalizing symptoms from approximately 10 to 12 years of age. We found that higher proficiency in attention shifting indeed predicts fewer internalizing behaviors over time. In addition, higher proficiency in inhibitory control predicts fewer internalizing symptoms over time, but only for children showing resting state connectivity moderately above the sample average between the frontoparietal network and amygdala. This finding supports the idea that top-down control may not be adaptive for all children, and relations between executive functioning and anxiety risk may vary as a function of trait-level regulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prefrontal cortex (PFC) is a region within the frontal lobe broadly associated with executive functioning and cognitive control (Diamond, 2006; Miller & Cohen, 2001). Functional connections between the PFC and amygdala also implicate the PFC in processes such as emotion regulation (Gaffrey et al., 2021). Transdiagnostic approaches to understanding risk for psychopathology, such as the National Institute of Mental Health’s Research Domain Criteria (RDoC; Cuthbert & Insel, 2013), suggest that these forms of regulatory control mediated by the PFC may be especially relevant when considering risk and protective factors for maladaptive behaviors, such as the attentional biases and rumination often associated with anxiety (Cisler & Koster, 2009; McLaughlin & Nolen-Hoeksema, 2011; McTeague et al., 2016).
Network approaches to understanding human cognition emphasize investigating functional networks within the brain, which are ensembles of brain regions whose activity is highly correlated as measured by imaging methods such as functional magnetic resonance imaging (fMRI). These patterns of activity are apparent both during rest (i.e., during resting state MRI; rsMRI) or during more active tasks (Sylvester et al., 2012). The frontoparietal network has notable spatial as well as conceptual overlap with the PFC, and is associated with flexible control of other brain areas to help orient behaviors towards higher-order goals (Zanto & Gazzaley, 2013). The frontoparietal network includes regions of the brain such as the dorsolateral PFC, the inferior parietal lobe, subregions of the middle cingulate gyrus, and subregions of the precuneus, non-exhaustively (Sylvester et al., 2012).
Conventionally, top-down regulation is viewed as a mechanism for adaptive development, understood as a linear positive relation between levels of regulation and positive outcomes where “more is better”. However, emerging work suggests that it may be possible to have too much of a good thing, and increased levels of inhibitory control, a sub-domain of executive functioning, may exacerbate risk for anxiety disorders (Henderson & Wilson, 2017; Henderson et al., 2015; Thorell et al., 2004; White et al., 2011). In this paper, we examine interactions between two different markers of regulation, resting state functional connectivity between the frontoparietal network and amygdala and behavioral facets of executive functioning, and their relation to reported internalizing symptoms, both concurrently and longitudinally. We conduct this analysis within the Adolescent Brain and Cognitive Development (ABCD) data set (Casey et al., 2018), a large and diverse multi-site longitudinal cohort study. Use of ABCD provides the needed statistical power while also improving the generalizability of any findings to the general population. Furthermore, examining these interrelations in middle childhood rather than adulthood allows for the examination of risk factors for anxiety, prior to the average age of clinical onset and the acute presence of symptoms (Beesdo et al., 2009). Additionally, examining both functional connections and behavioral correlates of the frontoparietal network during a time of rapid and critical development may help to better understand how interactions between patterns of resting state connectivity and inhibitory control with anxiety may relate to this period of heightened plasticity (Casey et al., 2005; Gee et al., 2013; Tottenham & Gabard-Durnam, 2017; Welsh et al., 1991).
The Frontoparietal Network and Emotion Regulation
Neural circuitry between the frontoparietal network and the amygdala is a key functional connection in adaptive socioemotional processes (Etkin et al., 2009; He et al., 2016; Li et al., 2021; Qin et al., 2014; Rodman et al., 2019). The amygdala is often considered a “salience detector,” responding to stimuli that are important for adaptive engagement with one’s environment, including affective stimuli (Adolphs, 2008).
Functional connections between the PFC, broadly construed, and the amygdala evolve over the course of development up to and through young adulthood (Taber-Thomas & Pérez-Edgar, 2015). The amygdala reaches maturity well before the PFC, and during development exerts significant influence over the nature of functional connections between the PFC and amygdala (Tottenham & Gabard-Durnam, 2017; Ulfig et al., 2003). Gee et al. (2013) found that functional connectivity between the PFC and the amygdala in response to fearful faces flips from positive to negative around 10 years of age in a healthy cross-sectional sample. Corresponding with this developmental change is a decrease in amygdala activity in response to fearful faces. These findings suggest that this developmental change in frontoamygdala connectivity may reflect the downregulation of the amygdala in response to fearful stimuli by dampening amygdala reactivity (Gee et al., 2013).
Looking to the frontoparietal network more specifically, the network is often characterized as a flexible system projecting to other brain areas as a mechanism of top down control, including to the amygdala (Cole et al., 2014; Zanto & Gazzaley, 2013). Prior work in adults has found average negative resting state functional connectivity between the frontoparietal network and the PFC reflecting this downregulatory relation, although no work to date has directly examined age-related changes in frontoparietal-amygdala connectivity through childhood and adolescence (Xiao et al., 2018).
Activation within the frontoparietal network has also been associated with emotion regulation. Li et al. (2021) found in a sample of adults that when participants were prompted to implement various emotion regulation strategies, they showed greater activation in the frontoparietal network. Similarly, Rodman et al. (2019) found in children ages 8–17 that emotion regulation, specifically implementing cognitive reappraisal, was associated with increased activation within the frontoparietal network and decreased activation in the amygdala.
Despite these replicated findings linking the frontoparietal network and emotion regulation, associations between the frontoparietal network and anxiety remain less consistent. Amongst adults, work has found negative associations between trait anxiety and resting state functional connectivity between the frontoparietal network and the right amygdala (He et al., 2016). However, other work found that individuals with generalized anxiety disorder had increased connectivity between the frontoparietal network and the amygdala at rest (Etkin et al., 2009). Similarly, in children ranging from 7–9 years, researchers have reported that anxiety symptoms were associated with stronger/more positive connectivity between brain regions included in the frontoparietal network and the left basolateral amygdala, also at rest (Qin et al., 2014). Thus, research is mixed on whether hypo- or hyper-connectivity between the frontoparietal network and the amygdala is implicated in anxiety risk (Etkin et al., 2009; He et al., 2016; Qin et al., 2014). However, these findings suggest that the left amygdala may be more relevant in considering patterns of connectivity that confer risk for anxiety (He et al., 2016; Qin et al., 2014).
Executive Functioning
Both the PFC and the frontoparietal network offer a mechanism of regulation for brain structures, such as the amygdala, and associated behaviors, such as emotion regulation. The processes and behaviors associated with executive functioning are another marker of regulation that allow an individual to flexibly respond to stimuli in the face of competing prepotent responses (Diamond, 2006). Such regulation supports goal attainment, thus proficiency in executive functioning is associated with a host of adaptive behaviors in childhood, including increased school readiness (Fitzpatrick et al., 2014) and more sophisticated theory of mind (Carlson & Moses, 2001). Similar to developmental trajectories of connectivity between regions of the cortex and the amygdala, adult-like proficiency in executive functioning also comes online later in development (Welsh et al., 1991). For the purposes of this paper, we consider executive functioning through the lens of a three-factor model, dividing the broad umbrella term into the dissociable components of set shifting, working memory/updating, and inhibitory control (Miyake et al., 2000). We also note that these subdomains of EF are not necessarily a unitary construct that work in tandem. For example, high levels of proficiency in one domain (i.e., set shifting) may not correlate with high levels of proficiency in another (i.e., inhibitory control; Blackwell et al., 2014).
Prior work has found that increased proficiency in attention shifting operates as a protective mechanism against internalizing problems (Henderson & Wilson, 2017; Henderson et al., 2015; White et al., 2011). A proposed mechanism by which attention shifting may relate to fewer symptoms is that general proficiency may help an individual return to a baseline attentional state after the capture of their attention by a stimulus or event they may deem threatening. The ability to rapidly return to this baseline attentional state may minimize periods of negative affect elicited by the initial threatening stimulus and with repetition, as an individual is able to efficiently navigate between different attentional states, mitigate anxiety risk (Henderson & Wilson, 2017).
However, research is mixed on whether inhibitory control, although also a domain of executive functioning, specifically acts in the same protective fashion. A body of work has found that levels of inhibitory control are inversely related with internalizing symptomatology (Ansari & Derakshan et al., 2011; Basten et al., 2011; Kooijmans et al., 2000; Lengua, 2003; Wolfe & Bell, 2014), consistent with findings for both set shifting and working memory (Basten et al., 2012; Henderson & Wilson, 2017; Henderson et al., 2015; Moran, 2016; White et al., 2011). However, other research has documented that increased inhibitory control may actually act as a risk factor for higher levels of internalizing behaviors (Henderson & Wilson, 2017; Henderson et al., 2015; Thorell et al., 2004; White et al., 2011). This work suggests that high levels of inhibitory control contribute to behavioral rigidity, which acts as the mechanism for these observed relations. Overcontrolled behavior may potentiate any existent maladaptive social behaviors, which may in turn promote negative affect and increase risk for psychopathology (Gunther & Pérez-Edgar, 2021; Henderson & Wilson, 2017; Henderson et al., 2015). Thus, examining interactions between these different markers of behavioral and cognitive control may shed light on the mechanisms by which risk factors for anxiety operate.
Current Study
In the present study we examine resting state connectivity between the frontoparietal network and the amygdala, executive functions (i.e., attention shifting and inhibitory control), and their interaction on longitudinal changes in internalizing symptoms in a multi-site sample of typically-developing children, starting at approximately 10 years of age. Prior work suggests that this may be approximately the age range of a developmental shift from positive to negative connectivity between the PFC and the amygdala (Gee et al., 2013). Although there is currently a paucity of work examining developmental trajectories of connectivity between the frontoparietal network and the amygdala, the available data suggest that this age is a critical time point in which to examine individual differences in connectivity relative to internalizing symptoms due to heightened individual variation in the rate and direction of change (Pérez-Edgar et al., 2020). Thus, this 10-year time point provides the needed variability for the model, setting the foundation for more complex analyses examining potential change over time. We then predict internalizing symptomology through adolescence, when more children may reach symptoms approaching or exceeding clinical threshold (Beesdo et al., 2009).
For these analyses we chose to focus on only attention shifting and inhibitory control. While working memory is also a behavior encompassed by the broader category of executive functions, prior literature does not implicate working memory proficiency in the rigidity or flexibility of affective states as it does attention shifting and inhibitory control (Henderson & Wilson, 2017; Henderson et al., 2015).
There are inconsistent findings regarding resting state connectivity between the frontoparietal network and amygdala within the scope of internalizing symptoms, as well as the associations between executive functions and internalizing symptoms, which may be due to differences in sample age, methodology, or sample sizes, among other possible sources of variability. However, we predict that children showing above average correlations between the frontoparietal network and the amygdala at baseline (roughly age 10), suggesting a lack of downregulation of the amygdala by cortical structures, will show increases in internalizing symptoms longitudinally (from ages 10 through 12) when they also show high inhibitory control, as measured by the Flanker task. Conversely, we hypothesize that high attention shifting, measured in a Dimensional Change Card Sort task, will predict decreases in internalizing symptoms over time, regardless of connectivity, as attention shifting promotes flexibility that may assist an individual in toggling between affective states and thus mitigate risk (Henderson & Wilson, 2017). Finally, we hypothesize that any significant effects of connectivity will be specific to the left amygdala. Prior work suggests that connectivity between the left amygdala and frontoparietal network may be more implicated in anxiety risk as compared to the right amygdala (He et al., 2016; Qin et al., 2014).
Methods
Participants
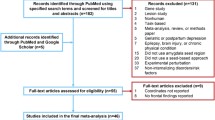
Participants were drawn from the ABCD study, selecting children with usable resting state fMRI data, Flanker data, and Dimensional Change Card Sort data from the NIH toolbox during baseline data collection, in addition to at least one timepoint of usable Child Behavioral Checklist (CBCL; Achenbach & Edelbrock, 1983) responses from either the baseline data point, wave 1, or wave 2. A breakdown of the sample’s demographics can be seen in Table 1.
Baseline data collection occurred when participants were an average of 119.52 months old (SD = 7.49, approximately 9.96 years), data collection for wave 1 occurred approximately 1 year later (Mage = 131.68 months, SD = 7.71, approximately 10.97 years) and data collection for wave 2 occurred approximately 1 year after wave 1 data collection (Mage = 143.95 months, SD = 7.71, approximately 12.00 years).
Resting State Connectivity
Data in this study were collected across 21 sites with 29 3 T scanners, including Siemens Prisma, General Electric 750, and Phillips (Casey et al., 2018). Participants completed 3–4 resting state scans at 5 min each to maximize data quality and minimize loss due to motion artifacts (Casey et al., 2018). Full details for scanning protocols and parameters can be found in Casey et al. (2018). The average motion during the resting state scans for the study sample was 0.22 mm (SD = 0.20 mm; Casey et al., 2018).
Our variables of interest were the resting state correlation between the frontoparietal network and the left amygdala, and the resting state correlation between the frontoparietal network and the right amygdala, both at baseline. Functional networks and subcortical structures were both defined by the Gordon atlas (Gordon et al., 2016). ABCD provides correlations as z-scores for analysis (Hagler et al., 2019).
Inhibitory Control
Our metric of inhibitory control was the Flanker task from the NIH toolbox, administered at baseline data collection (Zelazo et al., 2013). In the Flanker task, participants are asked to indicate the directionality (left/right) of a centrally presented stimulus, in the presence of surrounding “flanker” stimuli that are pointing in either the same or opposite direction. In this task, the child must inhibit the prepotent response to respond with the directionality of the majority of the stimuli, instead focusing on the center stimulus which may be in a conflicting direction (Luciana et al., 2018; Weintraub et al., 2013; Zelazo et al., 2013).
The score derived by NIH toolbox incorporates both reaction time and accuracy, each on a scale of 0–5, for a total maximum score of 10, when the participant was at least 80% accurate in their responses. For those below this threshold, only accuracy was used in the score (Weintraub et al., 2013; Zelazo et al., 2013). Further details on this scoring calculation can be found in Zelazo et al. (2013). The age corrected score as computed by NIH toolbox was used in analyses, meaning that the score generated is based on a comparison to the scores of other children of the same age. For example, an age-corrected score of 100 indexes that a child performed at the mean level for their age. An age-corrected score of 115 indexes that a child preformed 1SD above the mean level for their age, and an age-corrected score of 85 indexes that a child performed 1SD below the mean level for their age (NIH Toolbox, n.d.).
Attention Shifting
Our metric of attention shifting was the Dimensional Change Card Sort (DCCS) task from the NIH toolbox, also administered at baseline data collection (Zelazo et al., 2013). In this task, participants are given two target cards, for example a blue rabbit and a red boat. They are then given additional cards, for example cards with red rabbits and blue boats. They are first asked to sort these cards by one dimension, for example by color. They then switch and are asked to sort by the other dimension, for example by shape. The iteration of this task used in the NIH toolbox includes a practice block, a pre-switch block (one rule set), a post-switch box (switching to the second rule set) and finally a mixed block. Only individuals who got at least 4 correct trials on the post-switch block moved onto the mixed block (Dick et al., 2019). In the mixed block, the dimension on which the individual is asked to sort (shape or color) changes on a pseudorandom basis (Luciana et al., 2018).
The scoring incorporates both reaction time and accuracy, each on a scale of 0–5, for a total maximum score of 10, when the participant was at least 80% accurate in their responses. For those below this threshold, only accuracy was used in the score (Dick et al., 2019). As above, further details on this scoring calculation can be found in Zelazo et al. (2013). Like the Flanker task, the age-corrected score was used, where the individual’s score was standarized (M = 100, SD = 15) to performance among individuals their own age.
Internalizing Symptoms
Our analysis focused upon internalizing symptoms as reported by the child’s parent on the CBCL (Achenbach & Edelbrock, 1983) at baseline, wave 1, and wave 2. While prior research has focused heavily on symptoms of anxiety, and anxiety disorders are indeed seen in children as young as preschool-age (Franz et al., 2013), onset can also be as late as adolescence or adulthood depending on the type of anxiety disorder (Beesdo et al., 2009). The community sampling of the ABCD study provides a cohort that is generally healthy. In addition, these data were collected when the children were fairly young. Thus, there was little likelihood that many children in this sample, albeit at some level of risk for anxiety, would display symptoms at or near a clinical threshold. Measuring internalizing behaviors, a broader classification that includes symptoms of anxiety, offers greater analytic variability and a better developmental match with the sample (Beesdo et al., 2009). While internalizing symptoms also encompass behaviors associated with depression, and there are high degrees of comorbidity, anxiety emerges earlier in development than depression. It is more likely that the behaviors captured in this sample by the internalizing subscale are more likely to reflect emerging anxiety-linked processes (Beesdo et al., 2007).
Furthermore, in these analyses we use count of reported behaviors rather than T scores to reflect the subclinical nature of the sample, maximize analytic variability, and mitigate skew. Within our sample, the distribution of internalizing behaviors was characteristic of a non-clinical, community sample (Fig. 1).
Puberty
There are documented relations between pubertal status and both structural and functional brain development (Dai & Scherf, 2019). Because our sample was at an age where puberty is a relevant consideration, yet not central to our research question, both assigned sex and puberty were entered into all models as covariates.
Pubertal status was measured via using child report on the Pubertal Development Scale (Petersen et al., 1988). From these responses, a category score was derived (Cheng et al., 2021). This metric produced a category for male-assigned and female-assigned participants, separately. To consider these metrics as a single variable, categories were Z-scored within male and female participants and collapsed. A histogram of Z-scored puberty can be seen in Fig. 2.
Data Analysis
All statistical analyses were conducted in R version 3.6.2. First, we examined correlations between our variables of interest to characterize their interrelations.
Multilevel modeling (Snijders & Bosker, 2011) was used to assess trajectories of internalizing symptoms across ages 10, 11, and 12 years as a function of frontoparietal network-amygdala connectivity, executive functioning, and their interaction at age 10 years. All multilevel models were fit using the nlme package in R (Pinheiro et al., 2022). We ran two separate multilevel models, one using the Flanker score as our metric of inhibitory control and the other using DCCS score as our metric of attention shifting. In the model for inhibitory control, attention shifting was entered as a covariate, and vice versa. For all models, internalizing symptoms, Flanker/DCCS score, and network to ROI correlations were Z-scored. Additionally, puberty and sex assigned at birth were entered as covariates in all models. To account for the sampling and testing scheme of the ABCD study, data were nested by scanner ID, family, and participant as nested random intercepts. Age was entered as a random slope. Participants included in the model all had complete executive functioning, resting state, puberty, and assigned sex data. Any missing repeated measures in internalizing behaviors were accounted for via Restricted Maximum Likelihood (REML; Pinheiro et al., 2022).
Results
Pearson correlations revealed significant associations between many variables of interest. Of note, resting state connectivity between the frontoparietal network and the left or right amygdala was not significantly associated with our core measures of internalizing symptoms, attention shifting, and inhibitory control (Table 2).
The multilevel model examining the interaction of resting state frontoparietal-amygdala, inhibitory control, and age on repeated measures of internalizing symptoms found a significant two-way interaction between inhibitory control and resting state connectivity between the frontoparietal network and the left amygdala, b = -0.74, p = 0.049 (Table 3). The Johnson-Neyman technique was used to probe the interaction and identify the range of values of frontoparetal and amygdala connectivity at which the association between inhibitory control and internalizing symptoms was significant. This analysis found that when the z-scored correlation between the frontoparietal network and left amygdala was inside the interval [0.07, 0.44] for the observed data, the slope between inhibitory control and internalizing symptoms was significant and negative (Fig. 3). To characterize this region of significance, 4077 individuals or approximately 46% of the sample fell within this range.
The multilevel model examining the interaction of resting state frontoparietal-amygdala, attention shifting, and age on repeated measures of internalizing symptoms found a significant negative main effect of attention shifting on number of internalizing symptoms, b = -0.13, p = 0.04 (Table 4).
Discussion
In this study, we examined the interaction of resting state frontoparietal-amygdala connectivity, executive functioning performance (inhibitory control and attention shifting), and age on repeated measures of internalizing symptoms. We were motivated by work suggesting that high levels of attention shifting may be protective against the development of anxiety disorders, but inhibitory control may be a risk factor for anxiety disorders, particularly for children at temperamental or familial risk (Henderson & Wilson, 2017; Henderson et al., 2015; White et al., 2011). We hypothesized that high inhibitory control, along with above average frontoparietal-amygdala resting state connectivity, would relate to increases in internalizing behaviors over time, reflecting overcontrol as a mechanism for exacerbated symptoms. We also hypothesized that high attention shifting would relate to decreases in internalizing behaviors over time, regardless of frontoparietal-amygdala connectivity. Finally, we hypothesized that any significant effects of connectivity would be specific to connectivity with the left amygdala, given prior data on anxiety risk (He et al., 2016; Qin et al., 2014).
Our findings did not fully align with our hypotheses. For our model with inhibitory control, we found that children with correlations between the frontoparietal network and left amygdala that were between 0.07 standard deviations above the mean and 0.44 standard deviations above the mean had a significant negative relation between inhibitory control and internalizing symptoms. That is, children with connectivity between these brain areas that were moderately above the average had lower internalizing symptoms if they had higher inhibitory control, but this relation did not vary as a function of child age. Children with either connectivity over 0.44 standard deviations above the mean or below average connectivity between the frontoparietal network and the left amygdala showed no significant associations between inhibitory control and internalizing symptoms. While these findings do not support our hypothesis of high levels of inhibitory control as a potential risk factor for psychopathology, it does support the idea that high inhibitory control may only be protective for some children. These data suggest that children who display trait-level regulation that is slightly above average, but are not overregulated, can benefit from a buffering effect. Once the level of regulation becomes extreme, inhibitory control is no longer a potent buffer against internalizing symptoms. Our hypothesis pertaining to attention shifting was mostly supported, in that we found that greater levels of attention shifting was associated with fewer internalizing symptoms, regardless of connectivity. However, there were no significant effects of age.
These findings also in part mirror the literature looking at the broader attentional mechanisms of proactive and reactive control. Proactive control, also referred to as planful control, refers to goal-driven behaviors that maintain action towards a higher-order outcome and encompasses behaviors such as attention shifting (Fox et al., 2020). Reactive control, on the other hand, refers to “just in time” cognitive control strategies (Filippi et al., 2021) and encompasses behaviors such as inhibitory control during a Go/No-go task or flanker task (Fox et al., 2020; Xie et al., 2017). Mirroring research on associations from inhibitory control and set shifting to internalizing behaviors and/or anxiety symptoms, work with proactive and reactive control similarly finds that high levels of reactive control may relate to greater anxiety risk/more anxiety symptoms, while high levels of proactive control may relate to fewer anxiety symptoms and thus confer some protection against anxiety disorders (i.e. Filippi et al., 2021; Fox et al., 2020; Schmid et al., 2015; Valadez et al., 2022). While our findings did not immediately support the idea of inhibitory/reactive control as a risk factor, we did see that greater performance on a task traditionally considered an assessment of proactive control was associated with fewer internalizing symptoms.
We highlight that the ABCD study features a community sample, displaying relatively normative levels of attention shifting and inhibitory control, as well as internalizing symptoms. Thus, due to the natural undersampling at the extremes of these behaviors, analyses may not have been able to detect any effects specifically associated with extreme levels of attention shifting or inhibitory control. Future research may seek to strategically sample children at the extreme profile of putative over- or under-control to better understand capture any non-linear relations with executive functioning (Northoff & Tumati, 2019).
A large range of sociodemographic and psychosocial diversity is included in the ABCD sample. Prior work has suggested that structural components of the developmental environment may relate to the development of executive functions (e.g. Arán-Filippetti & Richaud De Minzi, 2012; Fields et al., 2021; Raver et al., 2013), where children experiencing forms of early life stress may have impairments in inhibitory control and working memory, and may show either impairments or enhancements in attention shifting. Stressful or uncertain developmental environments may also contribute to increased risk for psychopathology (Cohodes et al., 2020 for review). Future research should examine interactions with these contextual factors to better understand how markers of potential environmental risk and buffering may relate to the associations noted here.
We also note that much theory pertaining to connectivity between the PFC/frontoparietal network and amygdala is predicated on the notion of a developmental “shift” from positive to negative connectivity between these brain regions during childhood, especially in response to emotional tasks (Gee et al., 2013). However, the majority of human work in this sub-domain of study has been conducted cross sectionally. Bloom et al. (2021) recently found in an accelerated longitudinal design, using multiverse analyses that test the robustness of a finding as a function of different analytic decisions, that this developmental trajectory may be less robust than previously understood. The ABCD data set will enable follow-up studies to examine trajectories of frontoparietal network-amygdala connectivity from 10 years of age and onward through adolescence, and how these trajectories may relate to interactions with executive functioning in relation to psychopathology. Trajectory analyses (i.e., growth-curve models) will be necessary to characterize fronto-amygdala connectivity within a true longitudinal sample to understand if, and how, these patterns of connectivity may change over time as well as how these trajectories may relate to socioemotional adaptation/maladaptation.
Future work in ABCD will continue to follow these trajectories of internalizing symptoms. While the literature is mixed regarding the average age of onset for anxiety disorders, prior work generally finds that children older than the range of this sample, and likely closer to late teens/early twenties, will show potentiated internalizing symptoms and clinical anxiety (de Lijster et al., 2017; Regier et al., 1998; Rhebergen et al., 2017). A strength of this study is that the current sample allowed us to capture changes in internalizing symptoms prior to clinical onset for most children, however further insight could be gleaned by examining how symptoms may increase later in development. Additionally, both models had trend-level interactions when including the child’s age (Age x Flanker x Frontoparietal-right amygdala correlation b < 0.01, p = 0.08; Age x DCCS x Frontoparietal-right amygdala correlation b < 0.001, p = 0.05) so continued sampling may reveal that executive functioning, frontoparietal-amygdala connectivity, and/or their interaction relate to changes in the number of internalizing symptoms over time. Thus, it will be critical to continue studying these trajectories to better understand how these potential mechanisms may contribute to clinical levels of risk, and whether the associations between measures change over time. Furthermore, where a notable body of work has studied changes in task-based PFC-amygdala connectivity and how these patterns may change with age (e.g., Bloom et al., 2021; Gee et al., 2013), very little work has examined age-related changes in resting state frontoparietal-amygdala connectivity longitudinally, which provide needed information regarding within-person patterns of risk for psychopathology.
These findings should be interpreted within the context of current methodological limitations. Work suggests that there may be age-related differences in cognitive state while an individual is instructed to “rest” during a scan. Indeed, for a younger child, a resting state scan is a task within itself to suppress movement or conversation, thus eliciting greater levels of cognitive control. In turn, resting state network analyses may reflect this heightened state of cognitive control. Inconsistencies in prior work may in part stem from this unstructured task, and findings should be interpreted in the context that the actual “task” of laying still in a scanner may vary systematically with child age, or other individual differences (Camacho et al., 2020). Additionally, we note that parcellation is an important methodological decision (Bryce et al., 2021) and these results are specific to brain regions as functionally defined by the Gordon atlas (Gordon et al., 2016). However, had a different parcellation been used to define ROIs, there would be the potential for results different from what is reported in this manuscript. It is also possible that other networks or network edges may similarly moderate the relation between executive functioning and anxiety, such as the executive control network (Geiger et al., 2015). Future work should take network-based approaches with the aim of exploring other networks and how they may relate to anxiety risk. Future work in other large data sets should also explore the specificity of these reported findings, to test whether these associations are specific to executive functioning or may apply to more broad cognitive processes.
Finally, we present these findings within the context of a recent publication by Marek et al. (2022) that highlights replicability issues in MRI work that seeks to link brain function to behavioral phenotypes, even in “large” samples like ABCD. However, the use of resting state functional connectivity as well as behavioral data from the NIH toolbox may help with replicability (Marek et al., 2022). Future work should seek to replicate these analyses in other larger data sets to bolster the validity of findings. Furthermore, our analysis was based upon correlations between the frontoparietal network and the amygdala. Because of this approach, we are not able to disentangle what component brain areas/nodes of the frontoparietal network may be driving the strength or directionality of correlations with each hemisphere of the amygdala.
Taken together, these data suggest that both inhibitory control and attention shifting may be important moderators for anxiety risk over time. While inhibitory control may operate differently across children as a function of neural markers of regulation, as captured by resting state frontoparietal-amygdala connectivity, attention shifting may be more widely protective against internalizing symptoms. Understanding these differential relations between forms of executive functioning and internalizing symptoms, especially in the context of brain connectivity, may help inform interventions and provide greater specificity in who may benefit.
Data Availability
Data can be obtained through the Adolescent Brain Cognitive Development (ABCD) Study’s Data Exploration and Analysis Portal (DEAP).
References
Achenbach, T. M., & Edelbrock, C. S. (1983). Manual for the child behavioral checklist and revised child behavior profile. University of Vermont.
Adolphs, R. (2008). Fear, faces, and the human amygdala. Current Opinion in Neurobiology, 18, 166–172. https://doi.org/10.1016/j.conb.2008.06.006
Ansari, T. L., & Derakshan, N. (2011). The neural correlates of impaired inhibitory control in anxiety. Neuropsychologia, 49, 1146–1153. https://doi.org/10.1016/j.neuropsychologia.2011.01.019
Arán-Filippetti, V., & Richaud de Minzi, M. C. (2012). A structural analysis of executive functions and socioeconomic status in school-age children: cognitive factors as effect mediators. The Journal of Genetic Psychology, 173(4), 393–416.
Basten, U., Stelzel, C., & Fiebach, C. J. (2011). Trait anxiety modulates the neural efficiency of inhibitory control. Journal of Cognitive Neuroscience, 23(10), 3132–3145. https://doi.org/10.1162/jocn_a_00003
Basten, U., Stelzel, C., & Fiebach, C. J. (2012). Trait anxiety and the neural efficiency of manipulation in working memory. Cognitive, Affective, and Behavioral Neuroscience, 12, 571–588. https://doi.org/10.3758/s13415-012-0100-3
Beesdo, K., Bittner, A., Pine, D. S., Stein, M. B., Hofler, M., Lieb, R., & Wittchen, H. (2007). Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Archives of General Psychiatry, 64(8), 903–912. https://doi.org/10.1001/archpsyc.64.8.903
Beesdo, K., Knappe, S., & Pine, D. S. (2009). Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. The Psychiatric Clinics of North America, 32(3), 483–524. https://doi.org/10.1016/j.psc.2009.06.002
Blackwell, K. A., Chatham, C. H., Wiseheart, M., & Munakata, Y. (2014). A developmental window into trade-offs in executive function: The case of task switching versus response inhibition in 6-year-olds. Neuropsychologia, 62, 356–364. https://doi.org/10.1016/j.neuropsychologia.2014.04.016
Bloom, P. A., VanTieghem, M., Gabard-Durnam, L., Gee, D. G., Flannery, J., Caldera, C., Goff, B., Telzer, E. H., Humphreys, K. L., Fareri, D. S., Shapiro, M., Algharazi, S., Bolger, N., Aly, M., & Tottenham, N. (2021). Age-related change in task-evoked amygdala-prefrontal circuitry: A multiverse approach with an accelerated longitudinal cohort aged 4–22 years. Human Brain Mapping. https://doi.org/10.1002/hbm.25847
Bryce, N. V., Flournoy, J. C., Moreira, J. F. G., Rosen, M. L., Sambook, K. A., Mair, P., & McLaughlin, K. A. (2021). Brain parcellation selection: An overlooked decision point with meaningful effects on individual differences in resting-state functional connectivity. NeuroImage, 243, 118487. https://doi.org/10.1016/j.neuroimage.2021.118487
Camacho, M. C., Quiñones-Camacho, L. E., & Perlman, S. B. (2020). Does the child brain rest?: An examination and interpretation of resting cognition in developmental cognitive neuroscience. Neuroimage, 212, 116688. https://doi.org/10.1016/j.neuroimage.2020.116688
Carlson, S. M., & Moses, L. J. (2001). Individual differences in inhibitory control and children’s theory of mind. Child Development, 72(4), 1032–1053. https://doi.org/10.1111/1467-8624.00333
Casey, B. J., Cannonier, T., Conley, M. I., Cohen, A. O., Barch, D. M., Heitzeh, M. M., Soules, M. E., Teslovich, T., Dellarco, D. V., Garavan, H., Orr, C. A., Wager, T. D., Banich, M. T., Speer, N. K., Sutherland, M. T., Riedel, M. C., Dick, A. S., Bjork, J. M., Thomas, K. M., & Dale, A. M. (2018). The Adolescent Brain Cognitive Development (ABCD) study: Imaging acquisition across 21 sites. Developmental Cognitive Neuroscience, 32, 43–54. https://doi.org/10.1016/j.dcn.2018.03.001
Casey, B. J., Tottenham, N., Liston, C., & Durston, S. (2005). Imaging the developing brain: What have we learned about cognitive development? TRENDS in Cognitive Sciences, 9(3), 104–110. https://doi.org/10.1016/j.tics.2005.01.011
Cheng, T. W., Magis-Weinberg, L., Guazzelli Williamson, V., Ladouceur, C. D., Whittle, S. L., Herting, M. M., Uban, K. A., Byrne, M. L., Barendse, M. E. A., Shirtcliff, E. A., & Pfeifer, J. H. (2021). A researcher’s guide to the measurement and modeling of puberty in the ABCD study at baseline. Frontiers in Endocrinology, 12, 608575. https://doi.org/10.3389/fendo.2021.608575
Cisler, J. M., & Koster, E. H. W. (2010). Mechanisms of attentional biases towards threat in anxiety disorders: an integrative review. Clinical Psychology Review, 30(2), 203–216. https://doi.org/10.1016/j.cpr.2009.11.003
Cohodes, E. M., Kitt, E. R., Baskin-Sommers, A., & Gee, D. G. (2020). Influences of early-life tress on frontolimbic circuitry: Harnessing a dimensional approach to elucidate the effects of heterogeneity in stress exposure. Developmental Psychobiology, 1–20. https://doi.org/10.1002/dev.21969
Cole, M., Repovs, G., & Anticevic, A. (2014). The frontoparietal control system: a central role in mental health. The Neuroscientist, 20(1), 652–664. https://doi.org/10.1177/1073858414525995
Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 1–8.
Dai, J., & Scherf, K. S. (2019). Puberty and functional brain development in humans: Convergence in findings? Developmental Cognitive Neuroscience, 39, 100690. https://doi.org/10.1016/j.dcn.2019.100690
de Lijster, J. M., Dierckx, B., Utens, E. M., Verhulst, F. C., Zieldorff, C., Dieleman, G. C., & Legerstee, J. S. (2017). The age of onset of anxiety disorders. Canadian Journal of Psychiatry, 62(4), 237–246. https://doi.org/10.1177/0706743716640757
Diamond, A. (2006). The early development of executive functions. In E. Bialystok & F. Craik (Eds.), Lifespan Cognition: Mechanisms of Change (pp. 70–95). Oxford University Press.
Dick, A. S., Garcia, N. L., Pruden, S. M., Thompson, W. K., Hawes, S. W., Sutherland, M. T., Reidel, M. C., Laird, A. R., & Gonzalez, R. (2019). No evidence for a bilingual executive function advantage in the ABCD study. Nature Human Behaviour, 3(7), 692–701. https://doi.org/10.1038/s41562-019-0609-3
Etkin, A., Prater, K. E., Schatzberg, A. F., Menon, V., & Greicius, M. D. (2009). Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Archives of general psychiatry, 66(12), 1361–1372. https://doi.org/10.1001/archgenpsychiatry.2009.104
Fields, A., Bloom, P. A., VanTieghem, M., Harmon, C., Choy, T., Camacho, N. L., Gibson, L., Umbach, R., Heleniak, C., & Tottenham, N. (2021). Adaptation in the face of adversity: Decrements and enhancements in children’s cognitive control behavior following early caregiving instability. Developmental Science, 24(6), e13133. https://doi.org/10.1111/desc.13133
Filippi, C. A., Suber, A., Ravi, S., Haas, S., Troller-Renfree, S. V., Fox, N. A., Leibenluft, E., & Pine, D. S. (2021). Developmental changes in the association between cognitive control and anxiety. Child Psychiatry and Human Development. https://doi.org/10.1007/s10578-021-01150-5
Fitzpatrick, C., McKinnon, R. D., Blair, C. B., & Willoughby, M. T. (2014). Do preschool executive function skills explain the school readiness gap between advantaged and disadvantaged children? Learning and Instruction, 30, 25–31. https://doi.org/10.1016/j.learninstruc.2013.11.003
Fox, N. A., Buzzell, G. A., Morales, S., Valadez, E. A., Wilson, M., & Henderson, H. A. (2020). Understanding the emergence of social anxiety in children with behavioral inhibition. Biological Psychiatry, 89, 681–689. https://doi.org/10.1016/j.biopsych.2020.10.004
Franz, L., Angold, A., Copeland, W., Costello, E. J., Towe-Goodman, N., & Egger, H. (2013). Preschool anxiety disorders in pediatric primary care: prevalence and comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry, 52(12), 1294–1303. https://doi.org/10.1016/j.jaac/2013.09.008
Gaffrey, M. S., Barch, D. M., Luby, J. L., & Petersen, S. E. (2021). Amygdala functional connectivity is associated with emotion regulation and amygdala reactivity in 4-to 6-year-olds. Journal of the American Academy of Child & Adolescent Psychiatry, 60(1), 176–185.
Gee, D. G., Humphreys, K. L., Flannery, J., Goff, B., Telzer, E. H., Shapiro, M., Hare, T. A., Bookheimer, S. Y., & Tottenham, N. (2013). A developmental shift from positive to negative connectivity in human amygdala-prefrontal circuitry. Journal of Neuroscience, 33(10), 4584–4593. https://doi.org/10.1523/JNEUROSCI.3446-12.2013
Geiger, M. J., Domschke, K., Isper, J., Hattingh, C., Baldwin, D. S., Lochner, C., & Stein, D. J. (2015). Altered executive control network resting-state connectivity in social anxiety disorder. The World Journal of Biological Psychiatry, 17(1), 47–57. https://doi.org/10.3109/15622975.2015.1083613
Gordon, E. M., Laumann, T. O., Adeyemo, B., Huckins, J. F., Kelley, W. M., & Petersen, S. E. (2016). Generation and evaluation of a cortical area parcellation from resting-state correlations. Cerebral Cortex, 26, 288–303. https://doi.org/10.1093/cercor/bhu239
Gunther, K. E., & Pérez-Edgar, K. (2021). Dopaminergic associations between behavioral inhibition, executive functioning, and anxiety in development. Developmental Review, 60, 100966. https://doi.org/10.1016/j.dr.2021.100966
Hagler, D. J., Hatton, S. N., Cornejo, M. D., Makowski, C., Fair, D. A., Dick, A. S., Sutherland, M. T., Casey, B. J., Barch, D. M., Harms, M. P., Watts, R., Bjork, J. M., Garavan, H. P., Hilmer, L., Pung, C. J., Sicat, C. S., Kuperman, J., Bartsch, H., Xue, F., & Dale, A. M. (2019). Image processing and analysis methods for the Adolescent Brain Cognitive Development Study. NeuroImage, 202, 116091. https://doi.org/10.1016/j.neuroimage.2019.116091
He, Y., Xu, T., Zhang, W., & Zuo, X. (2016). Lifespan anxiety is reflected in human amygdala cortical connectivity. Human Brain Mapping, 37, 1178–1193. https://doi.org/10.1002/hbm.23094
Henderson, H. A., Pine, D. S., & Fox, N. A. (2015). Behavioral inhibition and developmental risk: A dual-processing perspective. Neuropsychopharmacology, 40, 207–224. https://doi.org/10.1038/npp.2014.189
Henderson, H. A., & Wilson, M. J. G. (2017). Attention processes underlying risk and resilience in behaviorally inhibited children. Current Behavioral Neuroscience Reports, 4, 99–106. https://doi.org/10.1007/s40473-017-0111-z
Kooijmans, R., Scheres, A., & Oosterlaan, J. (2000). Response inhibition and measures of psychopathology: A dimensional analysis. Child Neuropsychology, 6(3), 145–184. https://doi.org/10.1076/chin.6.3.175.3154
Lengua, L. J. (2003). Associations among emotionality, self-regulation, adjustment problems, and positive adjustment in middle childhood. Applied Developmental Psychology, 24, 595–618. https://doi.org/10.1016/j.appdev.2003.08.002
Li, W., Yang, P., Ngetich, R. K., Zhang, J., Jin, Z., & Li, L. (2021). Differential involvement of frontoparietal network and insula cortex in emotion regulation. Neuropsychologia, 161, 107991. https://doi.org/10.1016/j.neuropsychologia.2021.107991
Luciana, M., Bjork, J. M., Nagel, B. J., Barch, D. M., Gonzalez, R., Nixon, S. J., & Banick, M. T. (2018). Adolescent neurocognitive development and impacts of substance use: Overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Developmental Cognitive Neuroscience, 32, 67–79. https://doi.org/10.1016/j.dcn.2018.02.006
Marek, S., Tervo-Clemmens, B., Calabro, F. J., Montez, D. F., Kay, B. P., Hatoum, A. S., Donohue, M. R., Foran, W., Miller, R. L., Hendrickson, T. J., Malone, S. M., Kandala, S., Feczko, E., Miranda-Dominguez, O., Graham, A. M., Earl, E. A., Perrone, A. J., Cordova, M., Doyle, O., & Dosenbach, N. U. (2022). Reproducible brain-wide association studies require thousands of individuals. Nature, 603, 654–660. https://doi.org/10.1038/s41586-022-04492-9
McLaughlin, K. A., & Nolen-Hoeksema, S. (2011). Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy, 49(3), 186–193. https://doi.org/10.1016/j.brat.2010.12.006
McTeague, L. M., Goodkind, M. S., & Etkin, A. (2016). Transdiagnostic impairment of cognitive control in mental illness. Journal of Psychiatric Research, 83, 37–46. https://doi.org/10.1016/j.jpsychires.2016.08.001
Miller, E. K., & Cohen, J. D. (2001). An integrative theory of prefrontal cortex function. Annual Review of Neuroscience, 24, 167–202.
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology, 41(1), 49–100. https://doi.org/10.1006/cogp.1999.0734
Moran, T. P. (2016). Anxiety and working memory capacity: A meta-analysis and narrative review. Psychological Bulletin, 142(8), 1–34. https://doi.org/10.1037/bul0000051
NIH Toolbox. (n.d.). Health measures. https://www.healthmeasures.net/score-and-interpret/interpret-scores/nih-toolbox
Northoff, G., & Tumati, S. (2016). Average is good, extremes are bad - Non-linear inverted U-shaped relationship between neural mechanisms and functionality of mental features. Neuroscience and Biobehavioral Reviews, 104, 11–25. https://doi.org/10.1016/j.neubiorev.2019.06.030
Pérez-Edgar, K., Vallorani, A., Buss, K. A., & LoBue, V. (2020). Individual differences in infancy research: Letting the baby stand out from the crowd. Infancy, 25, 438–457. https://doi.org/10.1111/infa.12338
Petersen, A.C., Crockett, L., Richards, M., & Boxer, A. (1988). A self-report measure of pubertal status: reliability, validity, and initial norms. Journal of Youth and Adolescence, 17(2), 117–33. https://doi.org/10.1007/BF01537962
Pinheiro, J., Bates, D., DebRoy, S., Sarkar, D., & R Core Team. (2022). nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1–155. https://CRAN.R-project.org/package=nlme
Qin, S., Young, C. B., Duan, X., Chen, T., Supekar, K., & Menon, V. (2014). Amygdala subregional structure and intrinsic functional connectivity predicts individual differences in anxiety during early childhood. Biological Psychiatry, 75, 892–900. https://doi.org/10.1016/j.biopsych.2013.10.006
Raver, C. C., Blair, C., Willoughby, M., & The Family Life Project Key Investigators. (2013). Poverty as a predictor of 4-year-olds’ executive function: new perspectives on models of differential susceptibility. Developmental Psychology, 49(2), 292–304.
Regier, D. A., Rae, D. S., Narrow, W. E., Kaelber, C. T., & Schatzberg, A. F. (1998). Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. British Journal of Psychiatry, 173, 24–28. https://doi.org/10.1192/S0007125000293483
Rhebergen, D., Aderka, I. M., van der Steenstraten, I. M., van Balkom, A. L. J. M., van Oppen, P., Stek, M. L., Comijs, H. C., & Batelaan, N. M. (2017). Admixture analysis of age of onset in generalized anxiety disorder. Journal of Anxiety Disorders, 50, 47–51. https://doi.org/10.1016/j.janxdis.2017.05.003
Rodman, A. M., Jenness, J. L., Weissman, D. G., Pine, D. S., & McLaughlin, K. A. (2019). Neurobiological Markers of Resilience to Depression Following Childhood Maltreatment: The Role of Neural Circuits Supporting the Cognitive Control of Emotion. Biological Psychiatry, 86, 464–473. https://doi.org/10.1016/j.biopsych.2019.04.033
Schmid, P. C., Kleiman, T., & Amodio, D. M. (2015). Neural mechanisms of proactive and reactive cognitive control in social anxiety. Cortex, 70, 137–145. https://doi.org/10.1016/j.cortex.2015.05.030
Snijders, T. A., & Bosker, R. J. (2011). Multilevel analysis: An introduction to basic and advanced multilevel modeling. Sage.
Sylvester, C. M., Corbetta, M., Raichle, M. E., Rodebaugh, T. L., Schlaggar, B. L., Sheline, Y. I., Zorumski, C. F., & Lenze, E. J. (2012). Fumctional network dysfunction in anxiety and anxiety disorders. Trends in Neurosciences, 35(9), 527–535. https://doi.org/10.1016/j.tins.2012.04.012
Taber-Thomas, B., & Pérez-Edgar, K. (2015). Brain development in emerging adulthood. In J. Arnett (Ed.), Oxford Handbook of Emerging Adulthood (pp. 126–141). Oxford University Press.
Thorell, L. B., Bohlin, G., & Rydell, A. (2004). Two types of inhibitory control: Predictive relations to social functioning. International Journal of Behavioral Development, 28(3), 193–203. https://doi.org/10.1080/01650250344000389
Tottenham, N., & Gabard-Durnam, L. J. (2017). The developing amygdala: A student of the world and a teacher of the cortex. Current Opinion in Psychology, 17, 55–60. https://doi.org/10.1016/j.copsyc.2017.06.012
Ulfig, N., Setzer, M., & Bohl, J. (2003). Ontogeny of the human amygdala. Annals of the New York Academy of Sciences, 985(1), 22–33.
Valadez, E. A., Morales, S., Buzzell, G. A., Troller-Renfree, S. V., Henderson, H. A., Chronis-Tuscano, A., Pine, D. S., & Fox, N. A. (2022). Development of Proactive Control and Anxiety Among Behaviorally Inhibited Adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. https://doi.org/10.1016/j.jaac.2022.04.012
Weintraub, S., Dikmen, S. S., Heaton, R. K., Tulsky, D. S., Zelazo, P. D., Bauer, P. J., Carlozzi, N. E., Slotkin, J., Blitz, D., Wallner-Allen, K., Fox, N. A., Beaumont, J. L., Mungas, D., Nowinski, C. J., Richler, J., Deocampo, J. A., Anderson, J. E., Manly, J. J., Borosh, B., … Gershon, R. C. (2013). Cognition assessment using the NIH Toolbox. Neurology, 80(11 Suppl 3), S54–S64. https://doi.org/10.1212/WNL.0b013e3182872ded
Welsh, M. C., Pennington, B. F., & Groisser, D. B. (1991). A normative-developmental study of executive function: A window on prefrontal function in children. Developmental Neuropsychology, 7(2), 131–149. https://doi.org/10.1080/87565649109540483
White, L. K., McDermott, J. M., Degnan, K. A., Henderson, H. A., & Fox, N. A. (2011). Behavioral Inhibition and anxiety: The moderating roles of inhibitory control and attention shifting. Journal of Abnormal Child Psychology, 39, 735–747. https://doi.org/10.1007/s10802-011-9490-x
Wolfe, C. D., & Bell, M. A. (2014). Brain electrical activity of shy and non-shy preschool-aged children during executive function tasks. Infant and Child Development, 23(3), 259–272. https://doi.org/10.1002/icd.1858
Xiao, T., Zhang, S., Lee, L., Chao, H. H., van Dyck, C., & Li, C. R. (2019). Exploring Age-Related Changes in Resting State Functional Connectivity of the Amygdala: From Young to Middle Adulthood. Frontiers in Aging Neuroscience, 10, 209. https://doi.org/10.3389/fnagi.2018.00209
Xie, L., Ren, M., Cao, B., & Li, F. (2017). Distinct brain responses to different inhibitions: Evidence from a modified Flanker Task. Nature Scientific Reports, 7, 6657. https://doi.org/10.1038/s41598-017-04907-y
Zanto, T. P., & Gazzaley, A. (2013). Fronto-parietal network: Flexible hub of cognitive control. Trends in Cognitive Sciences, 17(12), 602–603.
Zelazo, P. D., Anderson, J. E., Richler, J., Wallner‐Allen, K., Beaumont, J. L., & Weintraub, S. (2013). II. NIH Toolbox Cognition Battery (CB): Measuring executive function and attention. Monographs of the Society for Research in Child Development, 78(4), 16–33.
Funding
This study was funded by the National Science Foundation Graduate Research Fellowship Grant No. DGE1255832 (to KEG) and the National Institute on Drug Abuse T32 DA017629 (to DP). The content is the sole responsibility of the authors and does not necessarily represent the official position of any funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gunther, K.E., Petrie, D., Pérez-Edgar, K. et al. Relations Between Executive Functioning and Internalizing Symptoms Vary as a Function of Frontoparietal-amygdala Resting State Connectivity. Res Child Adolesc Psychopathol 51, 775–788 (2023). https://doi.org/10.1007/s10802-023-01025-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-023-01025-4