Abstract
Research with community samples suggests that non-affective features of families, such as the amount of time parents and adolescents spend together, affect depressive symptoms in adolescents. It is possible, however, that spending time with parents not only protects against the onset of depressive symptoms, but also reduces symptoms in adolescents who are already depressed. The current study was designed to test this formulation while also examining whether affective dimensions of family functioning – specifically parental warmth – accounted for or moderated observed associations. Finally, we tested the reverse direction of the associations, examining whether greater severity of depression in adolescents results in parents spending less time with them. Forty-one adolescents (ages 14 to 17 years) who met criteria for a current major depressive episode participated in the present study with one parent. Once each month for six time points, dyads completed reports of depressive symptoms and the amount of time parents and adolescents spent with each other. Participants also completed measures of parental warmth. Results of lagged multilevel modeling indicated that spending more time with a parent predicted fewer depressive symptoms in adolescents at the following assessment relative to their mean; in contrast, greater severity of depressive symptoms did not predict spending less time with a parent at the following assessment. In contrast, parental warmth did not account for or moderate the association between time together and depressive symptoms. These results suggest that non-affective dimensions of family life, specifically spending more time with parents, have beneficial effects on depressive symptoms in adolescents diagnosed with depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Major Depressive Disorder (MDD) in adolescence is a prevalent, recurrent, and frequently devastating illness that places individuals at risk for mental health problems across the lifespan, including increased likelihood of psychiatric and medical comorbidity and risk for suicide (Birmaher et al. 1996; Costello et al. 2002; Galaif et al. 2007). Once they experience MDD, adolescents often have persistent or chronic symptoms that result in substantial impairments in social, academic, and physical health domains (Avenevoli et al. 2015; Kovacs et al. 2016). In this context, identifying factors that can reduce the length or severity of depressive episodes in adolescents who have already experienced the onset of MDD has the potential to reduce disease burden and improve health for adolescents.
Despite increasing autonomy associated with adolescence, parental factors are salient to depressive symptoms in this developmental period (Sheeber et al. 2007). Substantial work suggests that family environments that are characterized by greater conflict and/or less support are related to higher levels of depressive symptoms and to greater likelihood that adolescents will be diagnosed with MDD (Garber et al. 1997; Stice et al. 2004). For example, Schwartz et al. (2013) found that lower levels of maternal support and higher levels of maternal aggressive behavior observed during parent-adolescent interactions predicted the subsequent onset of MDD in adolescents. Most previous work has not considered whether dimensions of parenting behavior continue to be influential after adolescents are already diagnosed with depression, although the frequent involvement of parents in psychotherapy interventions provides theoretical support for the relevant role of parents following the onset of MDD (Restifo and Bögels 2009). These interventions generally focus on increasing parental support, improving communication, and reducing conflict (Restifo and Bögels 2009).
Reflected in these intervention targets is an emphasis on explicitly affective aspects of families. There has been increasing recognition, however, that non-affective features of family environments may also be relevant to adolescents’ psychological symptoms. For example, in one recent cross-sectional study, the extent to which adolescents engaged in family routines (such as eating meals at the same time each night or having a coordinated bedtime ritual) was related to lower levels of depressive symptoms (Manczak et al. 2017). Studies examining other non-affective features of adolescent social experiences, such as frequency of family meals (Fulkerson et al. 2006), family media engagement (Coyne et al. 2014), and attendance at structured after-school programs (Mahoney et al. 2001), have also documented associations with severity of adolescent depressive symptoms. Importantly, these non-affective dimensions may be particularly relevant for treatment; not only might they expand the number of targets for therapy, but they may also be more tolerable, amenable to modification, and easier to disseminate than attempting to target affective dimensions directly.
One non-affective feature of families that may be especially germane is the amount of time parents and teens spend together. (We conceptualize time spent together as being a non-affective dimension because, although interactions between parents and adolescents may be affectively-laden, the number of hours together does not necessitate any specific amount or valence of affective experience.) Studies of community samples suggest that spending more time with family members is associated with lower levels of depressive symptoms in adolescents. For example, Desha et al. (2010) found that spending more time with parents, but not with siblings, was associated with fewer depressive symptoms, with findings replicated in families with average to high socioeconomic status (Crouter et al. 2004) and in girls from Mexican-American families (Zeiders et al. 2015). These associations, however, have not yet been examined in samples of adolescents who are already depressed.
There are several reasons why simply spending more time with parents may be important for depressed adolescents. One possibility is that spending more time with a parent leads adolescents to structure their day more productively (Brody and Flor 1997). Another possibility is that a parent who is present signals the availability of support (Spagnola and Fiese 2007). This exposure may provide more opportunities for adolescents to disclose problems to their parent without being prompted directly (Kerr and Stattin 2000), with child disclosure relating to less severe depressive symptoms in prior work (Bacchini et al. 2010). Additionally, spending more time together also increases the likelihood that adolescents will have joint positive experiences with their parent, such as by engaging in pleasant activities (McHale et al. 2001) or that it precludes adolescents from engaging in other riskier behaviors during that time (Milkie et al. 2015).
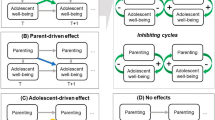
Thus, it is possible that spending time with parents not only protects against the onset of depressive symptoms, but also facilitates symptom improvement in adolescents who are already depressed. The current study was designed to test this formulation while also testing whether effects were specific to non-affective features of families. In addition, we tested the direction of the associations, examining whether parents of more depressed adolescents are less willing to spend time together. We recruited adolescents diagnosed with a current episode of depression at baseline and assessed them monthly over a five-month period (see Fig. 1). We hypothesized that adolescents would exhibit fewer depressive symptoms (relative to their average) at the monthly assessment following an assessment at which parents and adolescents report spending more time together than average. We also tested whether these associations would be due to, or differ as a function of, affective dimensions of parenting (i.e., parental warmth). Finally, we examined the reverse sequencing of associations, hypothesizing that adolescent depressive symptoms at one monthly assessment would not predict how much time parents and adolescents report spending together at the following assessment.
Conceptual Figure for Examining the Associations Between Time Spent Together and Adolescent Depressive Symptoms. Note: Solid arrows indicate primary conceptual model in which time spent together predicts adolescents’ depressive symptoms; dashed arrows indicate ‘reverse direction’ model in which adolescents’ depressive symptoms predict time spent together
Methods
Participants
Forty-one adolescents (ages 14 to 17 years) who met criteria for a current major depressive episode participated in the present study with one parent who was identified as the primary caregiver. Participants who were native speakers of English were recruited through media advertisements and flyers posted in an academic medical school, community mental health clinics, and throughout the community. Two-hundred-twenty individuals completed an initial phone screen, and 61 adolescents completed an in-person assessment, of which 41 adolescents met inclusionary and exclusionary criteria and participated in subsequent time points. Participating adolescents were required to meet DSM-IV criteria for a current episode of MDD, which was assessed using the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS; Joan et al. 1996). Exclusionary criteria included meeting criteria for bipolar disorder, a psychotic disorder, or substance dependence, or having a lifetime history of major medical problems, including severe head injury.
Thirty girls and 11 boys participated with 38 mothers and 3 fathers. Adolescents were on average 15.59 years old at baseline (SD = 1.07) and parents were on average 50.71 years old (SD = 6.91). Fifteen percent of participants identified as Hispanic/Latino ethnic status. Regarding racial identity, 68% of families identified as Caucasian, 22% identified as Asian American, 7% identified as Black/African American, and 12% identified as “other” (with participants able to endorse multiple identities). Parents had on average at least a two-year college degree and 79% were married.
Ethical Considerations
Parents provided written consent and adolescents provided written assent, overseen by the Institutional Review Board at Stanford University.
Procedure
Adolescents and their parents participated in an initial laboratory session (T1) during which current diagnosis of MDD was confirmed using the K-SADS. All interviews were conducted by trained research staff (symptom and diagnostic reliability κ > 0.9) with final diagnostic decisions made by a licensed psychologist. During this visit, parents and adolescents also separately completed a measure of the adolescent’s depressive symptoms and the amount of time they spent together (described below). Parents and adolescents then repeated these measures every month for five additional time points (T2-T6) through private emailed questionnaire links, resulting in six total assessments. At time points 2–6, parents and adolescents also completed questionnaires assessing parenting dimensions of warmth in their relationship with the adolescent. To limit the possibility of shared reporter bias, we analyzed adolescents’ reports of depressive symptoms (based on the assumption that they are experts concerning their own symptomatology) and parents’ reports of time together and of relationship quality variables (to reduce the possibility that more severely depressed adolescents might inaccurately perceive having less warm or available parents). Importantly, however, the results of these analyses are unchanged if we use the average of parent and adolescent reports for each variable. To avoid confusion, we describe measures below only for the participants whose data were analyzed (i.e., parent versus adolescent).
Measures
Depressive Symptoms
Adolescents completed a modified version of the PHQ-9 (Kroenke et al. 2001; Richardson et al. 2010). The PHQ-9 is a well-validated measure probing the presence of each DSM symptom of depression in the past two weeks on a scale of 0= “not at all” to 3= “nearly every day” and has been used in clinical adolescent populations (Richardson et al. 2010). The item assessing suicidality was omitted out of concern for adequately managing risk without face-to-face contact; psychomotor changes were assessed using two items reflecting psychomotor agitation and retardation separately. Scores on all items were summed and internal reliability on this measure was high (α = 0.80, current sample).
Time Together
At each assessment, parents responded to two items created for the present study assessing the number of hours per day they estimated spending with their adolescent: “on an average weekday over the past two weeks, how much awake time did you spend in close proximity to your child?” and “on an average weekend day over the past two weeks, how much awake time did you spend in close proximity to your child?” Parents were provided with the examples: “This might include being in the car together or being in the same room or general area within your home.” Responses to weekend and weekday items were combined by taking the weighted average ((5*weekday hours +2*weekend hours)/7), resulting in the average number of hours per day parents reported spending with their adolescent for each time point. Although the specific wording of these items is unique to the current study, this approach is consistent with previous research assessing parents’ perceptions of time spent with their adolescent children that used single-item questions and averaged across weekdays and weekends (Dubas and Gerris 2002).
Parental Warmth
Parents also completed the Parenting Styles and Dimensions Questionnaire Warmth subscale (Robinson et al. 1995), which consists of 11 items probing aspects of warmth and involvement with their child and has demonstrated reliability and validity (Olivari et al. 2013) (α = 0.89, current sample). Items were rated on a 1 (“almost never”) to 5 (“very often”) scale.
Demographic Characteristics
Participant age and parental education level (coded as 1 = less than high school diploma, 2 = GED/high school diploma, 3 = some college, 4 = two-year college degree, 5 = four-year college degree, 6 = master’s degree, 7 = professional degree, and 8 = doctorate), along with dummy codes indicating participant sex (coded as 0 = female, 1 = male), parent sex (0 = female, 1 = male), parent marital status (0 = married, 1 = single/divorced/widowed), and racial/ethnic minority status (0 = majority, 1 = minority), were assessed and included in secondary analyses.
Data Analytic Strategy
For our primary analyses, we tested the hypothesis that parents’ reports of spending more time with their adolescents would predict lower levels of depressive symptoms in adolescents at the next assessment relative to the participant’s average. To test this hypothesis, we conducted a series of multilevel models to estimate fixed effects using Hierarchical Linear and Nonlinear Modeling (HLM) software (Version 6.08; Raudenbush et al. 2004). For our initial model, at Level-1, adolescents’ depressive symptoms scores were modeled by the prior assessments’ time together variable (person-centered) and a random error term, representing the within-person portion of the model. A random effect term was included in the Level 2 model of the intercept. Following recommendations outline by Kraemer (2015), we first tested our model without any covariates to reduce potential model bias and to examine the generalizability of variable associations. The model is presented below:
The main coefficient of interest was the term indicating slope of the lagged time together variable. A significant coefficient term would indicate that changes in the amount of time parents and adolescents spend together (compared to their average) predicted adolescents’ depressive symptoms at the following month’s assessment.
Next, to examine whether demographic characteristics or linear trends in depressive symptoms might account for any observed associations, we added an assessment time point variable at Level 1 (indicating the time point for data collection with baseline = 0), as well as covariates of participant age, participant sex, parent sex, parent marital status, parent education, and participant minority status at Level 2 models of the intercept and slopes of Level 1 predictors.
We then tested whether including parental warmth diminishes or modifies the association between time together and depressive symptoms. Thus, we modeled depressive symptom scores by lagged time together and lagged parental warmth scores. We did not include demographic covariates in this or other follow-up analyses because there was no evidence of associations between these variables and depressive symptoms. We then modeled depressive symptom scores by lagged time together, parental warmth, and their interaction term to test whether the association between time and depressive symptoms differs as a function of the affective quality of the relationship with the parent.
Although the lagged nature of the models makes a reverse-direction explanation less likely, we nonetheless tested the possibility that observed associations might be accounted for by parents spending less time with more depressed adolescents by examining a model in which we predicted time together from adolescent’s depressive symptoms at the previous assessment (person-centered, Level 1).
Missing data was observed for less than 5% of the expected observations. Because HLM is robust to missing data at Level 1, we did not perform any data imputation.
Results
Descriptive statistics and bivariate correlations for all variables are presented in Table 1. Averaged across all days of the week, parents and adolescents in this study spent 4.71 h together per day, consistent with previous work finding that mothers spent an average of 4.61 h per day with their teenage children (Dubas and Gerris 2002). Of note, minority status was positively associated with time together, indicating that racial or ethnic minority families reported spending more time with their children than families of Caucasian adolescents. In addition, families who spent more time together also reported higher levels of parental warmth.
Does Spending More Time Together Predict fewer Depressive Symptoms?
Although bivariate correlations — ignoring within person differences — suggested that time together was not associated with concurrent depressive symptoms, the results of our initial model predicting adolescents’ depressive symptoms scores from time spent together reported at the previous assessments (Table 2) indicated that after an assessment in which adolescents spent more time than average with their parent, they reported significantly lower than average depressive symptoms at the following assessment (b = −0.49, SE = 0.13, p < 0.001). Follow-up analyses that adjusted for linear trends and demographic factors indicated that although there was a trend-level simple effect of assessment time point (b = −0.69, SE = 0.37, p = 0.066), there was no evidence that linear trends or demographic variables accounted for associations between time together and depressive symptoms, or that they predicted the slope of the effect of time together on depressive symptoms (ps > 0.10). The pattern of results were the same when centering the time together variable on the mean of all participants as when centering on the individual participant’s mean.
Does Parental Warmth Account for Associations with Depressive Symptoms?
To examine the possibility that associations between time spent together and depressive symptoms might simply reflect a finding that more optimal parenting predicts fewer adolescent depressive symptoms, we added lagged parental warmth as a covariate in our model, which did not reveal significant effects on depressive symptoms of parental warmth at the previous assessment (b = −0.06, SE = 0.07, p = 0.422; Table 3). Associations with time together and depressive symptoms remained significant (b = −0.51, SE = 0.14, p < 0.001).
Does Parental Warmth Moderate the Association between Time Together and Depressive Symptoms?
It is also possible that parental warmth moderates the association between time together and depressive symptoms. As presented in Table 3, there was no evidence of an interactive effect of warmth and time together on symptoms (b = −0.01, SE = 0.01, p = 0.441).
Do more Depressive Symptoms Predict Less Time Together?
Finally, to rule out the reverse direction of associations, we modeled time spent together by depressive symptom scores at the previous assessment (Table 3). This analysis indicated that parents did not spend less time with their adolescent as the adolescent’s depressive symptoms increased (b = −0.02, SE = 0.04, p = 0.575).
Taken together, these results suggest that (a) spending more time with a parent predicts fewer adolescent depressive symptoms a month later; (b) these associations are not accounted for by demographic features nor reverse directionality; and (c) these associations are specific to time spent together rather than simply reflecting more optimal parenting quality as indexed by parental warmth.
Discussion
The present results indicate that spending more time with a parent predicts lower subsequent levels of depressive symptoms in depressed adolescents. Specifically, we found that adolescents reported lower levels of depressive symptoms the month after an assessment in which they spent more time than average with their parent, with effects not due to overall linear trends in depressive symptoms, participants’ demographic characteristics, or parents spending less time with adolescents who are more depressed. Notably, parental warmth did not account for or moderate the association between time and depressive symptoms, supporting the formulation that time spent with a parent may be important for the functioning of depressed teens regardless of the affective quality of the relationship.
Previous research has found that time with parents is associated with fewer depressive symptoms in community samples of adolescents (Desha et al. 2010); the current study is the first, however, to find similar associations, prospectively, in a sample of adolescents diagnosed with clinically significant depression. There are several possible explanations for these beneficial effects. For example, the mere presence of a parent may convey continued support for the adolescent even during difficult times, providing a supportive buffer for stress and impairment. Notably, this availability of support may function differently than demonstrated support captured by parental warmth. Another possibility is that spending time with a parent—and potentially engaging in tasks together—may help to minimize ruminative processes in adolescents and facilitate greater behavioral activation, two processes identified as potent mechanisms of psychotherapy for depression (Jacobson et al. 2001; Watkins et al. 2007).
In the current study, parental warmth did not account for the associations between time together and adolescents’ subsequent depressive symptoms, nor did the strength of that association vary depending on levels of parental warmth. It is possible that whereas impairments experienced by depressed teens render them less perceptive of, and less responsive to, subtle changes in warmth in their parents, time together remains more noticeable and potent even during depressive episodes.
The fact that we did not find that adolescents’ depressive symptoms predict the amount of time spent with parents suggests that any interpersonal deficits associated with depression (e.g., Joiner and Timmons 2002) do not affect parents’ willingness to spend time with their adolescent. This absence of a predictive effect of depressive symptoms on time together with parents is encouraging for youth outcomes; specifically, it does not appear to be the case that adolescents who are most in need of support from parents are not able to access it.
The current findings have important clinical implications. Whereas traditional psychotherapies often attempt to modify affective aspects of parent-child relationships, such as reducing conflict and increasing parental warmth, our results underscore the importance of also considering non-affective dimensions. Indeed, encouraging families to spend more time together may be particularly amenable to intervention, easy to include in existing treatments, and possible to disseminate in even non-clinical contexts. Further, such efforts may be more cost-effective, more easily tolerated, and less socially stigmatizing than more traditional psychotherapeutic or pharmacological interventions for youth depression. Of course, certain families may be limited by structural constraints that prevent parents from spending greater time with their children; however, by expanding the number of possible treatment targets, it increases the likelihood possible least some interventions may be successful for families.
It is important to acknowledge limitations of the current work and to advance future directions for research. One limitation is the relatively small sample size; it will be important to replicate these results with larger samples. It is possible that the lack of associations with parental warmth are due to inadequate power to detect those effects; indeed, although our power to detect a medium effect size was .98, our power to detect a small effect was only .18. The sample size also prevented us from adequately examining demographic differences in associations. In addition, the primary variables that we used to assess time spent with an adolescent should be validated more formally in future studies, perhaps by using more frequent assessment periods, real-time monitoring, or detailed ratings. It is difficult to know, for example, if the two-week windows included holiday vacations during which families might spend more time together or if very high levels of time together signal less adaptive processes like family enmeshment. We also cannot determine which specific parent-child experiences, out of the range of possible explanations, account for the observed associations between time together and depressive symptoms. It is also possible that other variables, such as family members’ schedules, contribute to our findings. Direct manipulation of time together in a randomized-control context would provide stronger support for our interpretations of the findings. Similarly, additional assessments of other forms of affective dimensions of parenting would improve future work. We should also note that families were recruited from both clinical and non-clinical settings in the local community, with a mixture of youth who were and who were not seeking treatment. While this composition of our sample means that the findings may not be generalizable to a specific population of adolescents with depression, we think that it increases generalizability to depressed adolescents in the community. Finally, we only examined time spent with the primary caregiver, which was overwhelmingly the participant’s mother; future studies should examine time spent with all caregivers as well as with friends, siblings, and romantic partners to determine whether time with different social partners similarly predicts depressive symptoms in depressed teens.
Despite these limitations, however, the current study provides a strong test of associations between time spent with parents and changes in depressive symptoms in adolescents diagnosed with MDD. By utilizing repeated assessments, examining prospective associations, and testing reverse directionality, our findings suggest that spending more time with a parent predicts experiencing fewer depressive symptoms a month later, and that similar associations are not accounted for by parental warmth. Taken together, this work suggests that non-affective dimensions of family life, specifically spending more time with parents, has beneficial associations with depressive symptomatology even in adolescents diagnosed with MDD.
References
Avenevoli, S., Swendsen, J., He, J., Burstein, M., & Merikangas, K. (2015). Major depression in the National Comorbidity Survey–Adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 54(1), 37–44.e2. https://doi.org/10.1016/j.jaac.2014.10.010.
Bacchini, D., Concetta Miranda, M., & Affuso, G. (2010). Effects of parental monitoring and exposure to community violence on antisocial behavior and anxiety/depression among adolescents. Journal of Interpersonal Violence, 26(2), 269–292. https://doi.org/10.1177/0886260510362879.
Birmaher, B., Ryan, N., Williamson, D., Brent, D., Kaufman, J., Dahl, R., et al. (1996). Childhood and adolescent depression: A review of the past 10 years. Part I. Journal of the American Academy of Child & Adolescent Psychiatry, 35(11), 1427–1439.
Brody, G., & Flor, D. (1997). Maternal psychological functioning, family processes, and child adjustment in rural, single-parent, African American families. Developmental Psychology, 33(6), 1000–1011. https://doi.org/10.1037/0012-1649.33.6.1000.
Costello, E., Pine, D., Hammen, C., Plotsky, P., Weissman, M., et al. (2002). Development and natural history of mood disorders. Biological Psychiatry, 52, 529–542.
Coyne, S., Padilla-Walker, L., Fraser, A., Fellows, K., & Day, R. (2014). Media time = family time. Journal of Adolescent Research, 29(5), 663–688. https://doi.org/10.1111/j.1467-954X.2005.00517.x.
Crouter, A., Head, M., McHale, S., & Tucker, C. (2004). Family time and the psychosocial adjustment of adolescent siblings and their parents. Journal of Marriage and Family, 66(1), 147–162. https://doi.org/10.1111/j.0022-2445.2004.00010.x-i1.
Desha, L., Nicholson, J., & Ziviani, J. (2010). Adolescent depression and time spent with parents and siblings. Social Indicators Research, 101(2), 233–238. https://doi.org/10.1007/s11205-010-9658-8.
Dubas, J., & Gerris, J. (2002). Longitudinal changes in the time parents spend in activities with their adolescent children as a function of child age, pubertal status and gender. Journal of Family Psychology, 16(4), 415–426. https://doi.org/10.1037//0893-3200.16.4.415.
Fulkerson, J., Story, M., Mellin, A., Leffert, N., Neumark-Sztainer, D., & French, S. (2006). Family dinner meal frequency and adolescent development: Relationships with developmental assets and high-risk behaviors. Journal of Adolescent Health, 39(3), 337–345. https://doi.org/10.1016/j.jadohealth.2005.12.026.
Galaif, E., Sussman, S., Newcomb, M., & Locke, T. (2007). Suicidality, depression, and alcohol use among adolescents: A review of empirical findings. International Journal of Adolescent Medical Health, 19(1), 27–35.
Garber, J., Robinson, N., & Valentiner, D. (1997). The relation between parenting and adolescent depression: Self-worth as a mediator. Journal of Adolescent Research, 12(1), 12–33.
Jacobson, N., Martell, C., & Dimidjian, S. (2001). Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice, 8, 255–270.
Joan, K., Birmaher, B., Brent, B., Rao, U., & Ryan, N. (1996). The schedule for affective disorders for school-aged children. Pittsburg: University of Pittsburgh Medical Center.
Joiner, T., & Timmons, K. (2002). Depression in its interpersonal context. In I. H. Gotlib & C. Hammen (Eds.), Handbook of Depression (pp. 322–339). New York: Guilford Press.
Kerr, M., & Stattin, H. (2000). What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpretation of monitoring. Developmental Psychology, 36(3), 366–380. https://doi.org/10.1037//0012-1649.36.3.366.
Kovacs, M., Obrosky, S., & George, C. (2016). The course of major depressive disorder from childhood to young adulthood: Recovery and recurrence in a longitudinal observational study. Journal of Affective Disorders, 203, 374–381. https://doi.org/10.1016/j.jad.2016.05.042.
Kraemer, H. (2015). A source of false findings in published research studies. JAMA Psychiatry, 72(10), 961. https://doi.org/10.1001/jamapsychiatry.2015.1178.
Kroenke, K., Spitzer, R., & Williams, J. (2001). The Phq-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613.
Mahoney, J., Schweder, A., & Stattin, H. (2001). Structured after-school activities as a moderator of depressed mood for adolescents with detached relations to their parents. Journal of Community Psychology, 30(1), 69–86. https://doi.org/10.1002/jcop.1051.
Manczak, E., Williams, D., & Chen, E. (2017). The role of family routines in the intergenerational transmission of depressive symptoms between parents and their adolescent children. Journal of Abnormal Child Psychology, 45, 643–656. https://doi.org/10.1007/s10802-016-0187-z.
McHale, S., Crouter, A., & Tucker, C. (2001). Free- time activities in middle childhood: Links with adjustment in early adolescence. Child Development, 72(6), 1764–1778.
Milkie, M., Nomaguchi, K., & Denny, K. (2015). Does the amount of time mothers spend with children or adolescents matter? Journal of Marriage and Family, 77(2), 355–372. https://doi.org/10.2307/352718.
Olivari, M., Tagliabue, S., & Confalonieri, E. (2013). Parenting style and dimensions questionnaire: A review of reliability and validity. Marriage & Family Review, 49(6), 465–490. https://doi.org/10.1080/01494929.2013.770812.
Raudenbush, S. W., Bryk, A. S., Cheong, Y. F., Congdon, R., & du Toit, M. (2004). HLM 6 for Windows [Computer software]. Lincolnwood: Scientific Software International, Inc.
Restifo, K., & Bögels, S. (2009). Family processes in the development of youth depression: Translating the evidence to treatment. Clinical Psychology Review, 29(4), 294–316.
Richardson, L., McCauley, E., Grossman, D., McCarty, C., Richards, J., Russo, J., et al. (2010). Evaluation of the patient health questionnaire-9 item for detecting major depression among adolescents. Pediatrics, 126(6), 1117–1123. https://doi.org/10.1542/peds.2010-0852.
Robinson, C., Mandleco, B., Olsen, S., & Hart, C. (1995). Authoritative, authoritarian, and permissive parenting practices: Development of a new measure. Psychological Reports, 77, 819–830.
Schwartz, O., Byrne, M., Simmons, J., Whittle, S., Dudgeon, P., Yap, et al. (2013). Parenting during early adolescence and adolescent-onset major depression. Clinical Psychological Science, 2(3), 272–286. https://doi.org/10.1001/archpsyc.65.12.1377.
Sheeber, L., Davis, B., Leve, C., Hops, H., & Tildesley, E. (2007). Adolescents' relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology, 116(1), 144–154.
Spagnola, M., & Fiese, B. (2007). Family routines and rituals. Infants & Young Children, 20(4), 284–299. https://doi.org/10.1097/01.iyc.0000290352.32170.5a.
Stice, E., Ragan, J., & Randall, P. (2004). Prospective relations between social support and depression: Differential direction of effects for parent and peer support? Journal of Abnormal Psychology, 113(1), 155–159. https://doi.org/10.1037/0021-843X.113.1.155.
Watkins, E., Scott, J., Wingrove, J., Rimes, K., Bathurst, N., Steiner, H., et al. (2007). Rumination-focused cognitive behaviour therapy for residual depression: A case series. Behaviour Research and Therapy, 45(9), 2144–2154.
Zeiders, K., Updegraff, K., Umaña-Taylor, A., McHale, S., & Padilla, J. (2015). Familism values, family time, and Mexican-origin young adults' depressive symptoms. Journal of Marriage and Family, 78(1), 91–106. https://doi.org/10.1016/j.jadohealth.2013.06.008.
Acknowledgements
Support for this research was provided by National Institute of Mental Health grants R37-MH101495, K01-MH106805, and T32-MH019938, and by the Klingenstein Third Generation Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Manczak, E.M., Ordaz, S.J., Singh, M.K. et al. Time Spent with Parents Predicts Change in Depressive Symptoms in Adolescents with Major Depressive Disorder. J Abnorm Child Psychol 47, 1401–1408 (2019). https://doi.org/10.1007/s10802-019-00526-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-019-00526-5