Abstract
Theory and research suggest that parents’ reactions to children’s emotions play a critical role in teaching children effective emotion regulation (ER) skills, but no studies have directly examined the role that parent emotion socialization plays in the development of ER in children with ADHD. Gaining insight into the causes of impaired ER, particularly in youth with ADHD who are known to have poor ER, has important theoretical and translational significance. The present study is the first to longitudinally examine whether emotion socialization predicts later physiological and adult-reported measures of ER in children with and without ADHD. It also sought to determine if these relations are moderated by ADHD symptoms. Participants were 61 children (31 girls, 30 boys; M = 10.67 years, SD = 1.28) with and without clinically significant ADHD symptoms. At Time 1, parent reports of emotion socialization and parent- and teacher-report of child ADHD symptoms were collected. At Time 2, child ER measures were collected based on parent- and teacher-report and physiological reactivity during an impossible puzzle and a social rejection task. Physiological measures included respiratory sinus arrhythmia and skin conductance level (SCL). Supportive parenting practices were associated with better parent-rated emotion regulation skills for all children and greater SCL reactivity for children with high ADHD symptoms. Non-supportive parenting reactions were associated with greater adult-rated emotional lability for children with high ADHD symptoms. Results highlight the importance of considering multiple aspects of ER, including physiological manifestations. Findings suggest that parents’ use of adaptive emotion socialization practices may serve as a protective factor for children’s ER development and may be particularly critical for youth with ADHD. Our findings support the use of interventions addressing parent emotion socialization to help foster better ER in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Emotion regulation (ER) is a multifaceted construct that involves the initiation, modulation, and expression of emotions (Eisenberg and Spinrad 2004) and is essential for children’s social and emotional well-being. ER involves subjective, physiological, and behavioral responses that vary in the intensity, speed/degree to which they escalate, and extent to which they are modulated to adapt to external circumstances (Bunford et al. 2015). There is growing evidence that children with attention-deficit hyperactivity disorder (ADHD) have significant difficulty regulating their emotions (see Graziano and Garcia 2016; Shaw et al. 2014, for reviews). Little is known, however, about the parental factors that contribute to ER difficulties in children with ADHD and whether these determinants are different than for children without ADHD. Theory and research suggests that parents’ reactions to children’s emotions play a critical socializing role in teaching children effective ER skills (termed emotion socialization; e.g., Denham et al. 2007; Eisenberg et al. 1998). Specifically, parental use of supportive emotion socialization practices may help teach children emotional awareness and understanding, and thus promote better ER (e.g., Cole et al. 2009; Eisenberg et al. 1998). However, to date, no studies have directly examined the role that parent emotion socialization plays in the development of ER in children with ADHD, making this an important potential risk or protective factor to be explored within this at-risk sample.
Role of Emotion Socialization in Children’s Emotional Development
Parents are thought to play a critical role in the development of children’s ER through the process of emotion socialization (e.g., Cole et al. 2009; Hersh and Hussong 2009). When parents respond to children’s emotions, they provide feedback to the child that either encourages/coaches (referred to as supportive reactions) or discourages/dismisses (referred to as non-supportive reactions) the expression of emotion (Gottman et al. 1997). Theory suggests that supportive reactions that validate and legitimize children’s negative feelings help enhance their empathic and prosocial development, and result in children having emotions and behaviors that are relatively regulated and constructive; in contrast, non-supportive responses may heighten or extend arousal, undermine children’s capacities to process and regulate their emotions, and contribute to impaired long-term emotion management due to learning effects (Bryant 1987; Eisenberg et al. 1998; Hoffman 1983). Over time, these non-supportive responses may result in children having inflexible, inconsistent, or unpredictable ways of experiencing emotion (Sanders et al. 2015). Indeed, both cross-sectional (e.g., Lunkenheimer et al. 2007; Ramsden and Hubbard 2002) and longitudinal (Gottman et al. 1996, 1997; Kochanska et al. 2015) data suggest that parent emotion socialization is predictive of children’s ER in typically developing samples, as well as in specific clinical populations (i.e., children with externalizing behavior problems including oppositional defiant disorder [ODD] and conduct disorder, depressed adolescents, and maltreated children; Crowell et al. 2014; Hunter et al. 2011; Kochanska et al. 2015; Shipman et al. 2007). Despite an established link between parent emotion socialization and children’s ER, few longitudinal studies have examined this relation (Gottman et al. 1996, 1997; Kochanska et al. 2015), and these have relied on a single method to measure ER. However, ER is a multi-faceted construct involving subjective, physiological, and behavioral responses (Bunford et al. 2015) requiring examination of multiple aspects of ER. Different measures of ER likely provide distinct information on children’s ER. Physiological measures and behavioral observations of ER behaviors are more task specific, whereas adult-report measures examine ER more globally but are more subject to rater bias. Thus, more research is needed to examine the longitudinal relation between parent emotion socialization and children’s ER using multiple measures of ER.
Importance of Examining Physiological Measures of Emotion Regulation
Researchers argue that children’s autonomic nervous system (ANS) reactivity during stress or challenge reflects physiological manifestations of emotionality and emotion dysregulation (Murray-Close 2013; Porges 2001, 2003). The ANS is comprised of the sympathetic nervous system (SNS), involved in “fight or flight” responses, and the parasympathetic nervous system (PNS), involved in restorative “rest and digest” functions. Polyvagal theory (Porges 2001, 2003) proposes that the PNS plays a critical biological role in adaptive emotion regulation. Respiratory sinus arrhythmia (RSA) is commonly used as a measure of PNS activity and provides an index of vagal influence on the heart based on heart rate variability (Berntson et al. 1997). During a threatening or stressful event, RSA withdrawal is proposed to be adaptive and facilitates efficient mobilization of metabolic resources that support effective coping and responses to the environment. Meta-analysis results support this interpretation for stressful tasks (Graziano and Derefinko 2013), though in ambiguous situations, RSA withdrawal may be inappropriate (e.g., Hastings et al. 2008).
SNS reactivity during stressful situations also may serve as a biological marker of emotional reactivity (El-Sheikh 2005; Hubbard et al. 2002) or sensitivity to environmental feedback (Beauchaine et al. 2001). SNS arousal is typically predominant when individuals are exposed to stressful events (Boucsein 1992). One measure of SNS reactivity is skin conductance level (SCL), a measure of sweat gland activity (see Dawson et al. 2007). In a negative context, increases in SCL are often interpreted as an indicator of greater emotional reactivity (El-Sheikh 2005; Hubbard et al. 2002), whereas a lack of SCL reactivity may suggest insensitivity to punishment or environmental feedback (Murray-Close 2013).
The majority of evidence suggests that adaptive parenting behaviors, including emotion socialization, are directly associated with adaptive physiological regulation in children (Calkins et al. 1998; El-Sheikh 2005; Gottman et al. 1996; Hastings et al. 2008; Miller et al. 2013); however, other work fails to find a direct link (Perry et al. 2012; Scrimgeour et al. 2016). It is possible that the effect of emotion socialization on ANS regulation is not the same for all children and that other child vulnerability factors (e.g., ADHD symptoms) could moderate these effects; however, to our knowledge research has not explored this possibility directly.
The Role of ADHD Symptomatology
Emotion socialization may have particular relevance for children with ADHD who are frequently characterized as emotionally dysregulated (Bunford et al. 2015; Shaw et al. 2014). Specifically, a recent review suggests that children with ADHD have the greatest impairments in emotional lability and emotion regulation skills (Graziano and Garcia 2016). Children with ADHD are rated by parents and teachers as high in negative emotionality and emotion dysregulation (e.g., Seymour et al. 2014; Sjöwall et al. 2013) and display differences, relative to children without ADHD, in ANS reactivity in response to emotion-inducing or cognitively challenging tasks (e.g., Beauchaine et al. 2013; Musser et al. 2013; Ward et al. 2015). In fact, in a previous study using the same sample investigated in the present study, we found that ADHD symptoms were concurrently associated with greater parent-rated negativity and lability, poorer parent-rated ER skills, and blunted RSA withdrawal in response to an experience of social rejection (McQuade and Breaux 2016).
Despite established ER deficits in youth with ADHD, researchers have not directly examined the relation between emotion socialization and ER in this population. However, other types of adaptive parenting behaviors (e.g., warmth, situational advice, responsiveness to distress) have been found to predict ER in youth with ADHD/disruptive behaviors (Duncombe et al. 2012; Melnick and Hinshaw 2000). Given findings in other clinical and non-clinical populations (e.g., Crowell et al. 2014; Gottman et al. 1996, 1997; Hunter et al. 2011; Kochanska et al. 2015; Shipman et al. 2007), it is possible that parent emotion socialization has a similar influence on ER for children with ADHD. However, it is also possible that emotion socialization differentially influences ER outcomes in youth with and without ADHD. For instance, research suggests that there are neurobiological mechanisms underlying emotion dysregulation in children with ADHD (e.g., dysfunction in the amygdala, ventral striatum, and orbitofrontal cortex; see Shaw et al. 2014 for a review); thus, in youth with ADHD, ER may be more strongly influenced by biological factors than by external factors like parenting. On the other hand, evidence suggests that children with ADHD are highly sensitive to their environment, and particularly sensitive to positive reinforcement (Tripp and Wickens 2008). Thus, it is also possible that for children with ADHD, having a parent respond in a supportive and validating manner when they are distressed may have a greater effect on their ER development than for children without ADHD. Some evidence does suggest that adaptive parenting is more protective for children with ADHD than non-ADHD children (e.g., Healey et al. 2011), though no studies have specifically examined implications for ER.
Present Study
The current study is the first to examine how parent emotion socialization relates longitudinally to physiological and adult-reported measures of ER in children with and without elevations in ADHD symptoms. Moreover, this study is the first to examine whether effects of emotion socialization on ER are moderated by ADHD symptom level. A multi-method approach was used to measure ER, including parent- and teacher-report as well as ANS reactivity measured during two failure experiences. One failure experience involved attempts to solve impossible puzzles and the other experience involved rejection by unknown peers. Performance during these tasks was fully standardized to control for individual differences in cognitive or social skills that may influence reactivity. Experiences of failure and rejection may be particularly salient stressors for children in pre-adolescence, when youth are likely to face frequent challenges in school and in social relationships and must respond with effective ER. Given the negative context of these tasks, RSA withdrawal and increased SCL reactivity were expected to be adaptive responses reflective of physiological manifestations of ER and emotional sensitivity (Graziano and Derefinko 2013; Hubbard et al. 2002). Consistent with a developmental psychopathology perspective and the research domain criteria set forth by the National Institute of Mental Health (Franklin et al. 2015; Sanislow et al. 2010), we considered ADHD symptoms dimensionally in our primary analyses. Based on cross-sectional findings, it was hypothesized that supportive parent emotion socialization would be protective and predict better ER, whereas non-supportive parent emotion socialization would be a risk factor for worse ER. In examining the role of ADHD symptoms, two competing hypotheses were considered. If the emotion dysregulation displayed by children with ADHD is due to neurobiological deficits (Shaw et al. 2014), then emotion socialization should have less effect on ER for children with elevated ADHD symptoms. Alternatively, if youth with ADHD display greater sensitivity to their environment (Tripp and Wickens 2008), then adaptive emotion socialization practices may have a larger protective effect for children high in ADHD symptoms.
Method
Participants
Participants included 61 children (31 girls, 30 boys) with and without clinically significant ADHD symptoms, who were 8 to 12 years old (M = 10.67; SD = 1.28) at Time 1 and 9 to 13 years old (M = 11.62, SD = 1.29) at Time 2. Participants were part of a larger study (N = 124) examining social impairment in youth with and without ADHD, and were re-recruited approximately 1 year later to participate in a second study that examined ER capacities. As part of the Time 1 study, an assessment of ADHD was conducted based on a structured and semi-structured clinical interview and symptom and broadband rating scales from parents and teachers (see McQuade et al. 2017 for additional details). Exclusion criteria at Time 1 included a history of autism spectrum disorder, bipolar disorder, or a neurologic condition, an estimated IQ below 80, or diagnostic uncertainty regarding ADHD status. To increase variability in ADHD symptom profiles, children meeting full DSM-5 criteria for ADHD, children with subthreshold clinical elevations, and typically developing children were included in the Time 1 study. Due to proposals that youth with a sluggish cognitive tempo presentation of ADHD do not display emotion dysregulation deficits (Barkley 2015), children with clinical elevations in ADHD symptoms were further excluded from the Time 2 study if they were suspected of this presentation, as defined by having fewer than three symptoms of hyperactivity-impulsivity. Additionally, only families who had provided contact information for participation in future research at Time 1 were re-contacted to participate in Time 2. This resulted in 101 eligible families, with 61 participating. The final sample of children participating at both time points was comprised of 23 children previously assigned a diagnosis of ADHD (13 with the combined presentation, eight with the predominantly inattentive presentation, and two with the predominantly hyperactive-impulsive presentation), seven previously classified as subthreshold ADHD (demonstrating at least four symptoms of inattention and/or hyperactivity-impulsivity in addition to cross-domain impairment), and 31 previously classified as typically developing. Racial distribution was 85% White, 5% Asian, and 7% other or multi-racial; 8% identified as Hispanic or Latino. In this sample, the median household income was $100,000, the average parent education level was 16 years (SD = 1.28), and 77% of parents were married or cohabiting. Children who participated at Time 2 did not significantly differ from those not included at Time 2 on demographic characteristics.
Procedures
The Amherst College institutional review board approved all Time 1 and Time 2 study procedures. For all families, parents provided consent and children provided assent. At Time 1, an assessment of ADHD was conducted and parents (90% mothers) completed relevant rating scales during a single laboratory study visit; teachers completed relevant rating scales through an online survey. Time 2 parent (90% mothers) measures were collected during the first of two laboratory study visits that occurred within the same month (M = 4 days apart) and teachers completed rating scales through an online survey system. Child measures of ANS reactivity during two failure tasks were assessed at the second Time 2 study visit. One research assistant administered the tasks while a second research assistant monitored the physiology equipment. To minimize medication effects, participants taking stimulants (n = 10) discontinued medication on assessment days during both Time 2 study visits; however, three participants taking selective serotonin reuptake inhibitors (SSRI) remained on their medication during the assessments. Families were compensated $75 for participation at Time 1 and $100 for participation at Time 2; teachers were compensated $25 for participation at each time point.
Time 1 Measures
ADHD Symptoms
A parent and teacher completed the Disruptive Behavior Disorder Rating Scale (DBD; Pelham et al. 1992) for each child. Adults rated how often the child displayed each of the DSM-IV ADHD symptoms on a scale from 0 (not at all) to 3 (very much). Symptoms were considered present if endorsed as occurring pretty much (2) or very much (3) by either the parent or teacher. If teacher data was unavailable (n = 7), symptom counts were based on parent-report alone. Informants were asked to rate children’s un-medicated behavior; however, for six children taking stimulant medications, the teacher ratings were based on medicated behavior as the teacher did not have an opportunity to observe the child un-medicated. To index symptom levels dimensionally, ADHD symptom counts (out of 18) were used. The DBD has good reliability and is able to distinguish between clinical and nonclinical children (Pelham et al. 2005). Cronbach’s alpha was 0.95 for parents and 0.94 for teachers in this study.
Emotion Socialization
Parents completed the Coping with Children’s Negative Emotions Scale (CCNES; Fabes et al. 1990) as a measure of parent emotion socialization. The CCNES includes 12 hypothetical scenarios in which a child is upset or angry (e.g., “If my child becomes angry because he/she is sick or hurt and can't go to his/her friend's birthday party, I would”). For each scenario parents rate the likelihood on a 7 point Likert scale (1 = Very Unlikely, 7 = Very Likely) that they would respond with six different types of reactions. Reactions can be collapsed into supportive and non-supportive emotion socialization practices. Based on prior studies (Eisenberg et al. 1998; Eisenberg et al. 1996; Fabes et al. 2001), supportive reactions included the Expressive Encouragement Reactions (e.g., “encourage my child to express his/her feelings of anger and frustration”), Emotion-Focused Reactions (e.g., “soothe my child and do something fun with him/her to make him/her feel better about missing the party”), and Problem-Focused Reactions (e.g., “help my child think about ways that he/she can still be with friends”); non-supportive reactions included Punitive Reactions (e.g., “send my child to his/her room to cool off”) and Minimization Reactions (e.g., “tell my child not to make a big deal out of missing the party”). Good reliability has been found for the CCNES (Fabes et al. 2002). Cronbach’s alphas were 0.73 for supportive and 0.78 for non-supportive reactions.
Time 2 Measures
Parent and Teacher Report of Emotion Regulation and Emotional Lability
Parents completed the Emotion Regulation Checklist (ERC; Shields and Cicchetti 1997) and teachers completed the Emotional Control subscale from the Behavior Rating Inventory of Executive Function (BRIEF; Gioia et al. 2000) as measures of children’s emotion dysregulation. On the ERC, parents rated how often their child exhibited a series of behaviors from 1 (rarely/never) to 4 (almost always), with items summed to create two subscale scores. The Emotion Regulation subscale includes eight items that describe the extent to which the child understands and responds appropriately to emotions (e.g., “is able to say when he/she is feeling sad, angry or mad, fearful or afraid”), with higher scores being more adaptive. The Negativity/Lability subscale includes 15 items and describes the extent to which the child displays labile and intense emotions (e.g., “has wild mood swings,”), with lower scores being more adaptive. The ERC has been found to have good reliability (Shields and Cicchetti 1995). Cronbach’s alphas for the current sample were 0.90 for Negativity/Lability and 0.72 for Emotion Regulation. On the BRIEF, teachers rated the frequency of behaviors as never (1) sometimes (2) or often (3) occurring. The Emotional Control subscale includes 9 items that assess children’s emotional lability and emotional explosiveness (e.g., “overreacts to small problems,” “mood changes frequently”). A T-score based on gender and age norms was derived, with higher scores indicating more impairment. Gioia et al. (2000) report high internal consistency and test-retest reliability for teacher report on the BRIEF. Cronbach’s alpha for the current sample was 0.94 for the Emotional Control scale.
The parent-rated ERC Negativity/Lability subscale and the teacher-rated BRIEF Emotional Control subscale both measure emotion lability and had a moderately strong correlation with each other, r (46) = 0.49; therefore, they were standardized and averaged to create a single measure of Emotional Lability. Prior research suggests that the ERC Emotion Regulation and Negativity/Lability subscales represent distinct components of ER (Shields and Cicchetti 1997), and teacher-rated Emotional Control was weakly correlated with parent report of Emotion Regulation, r (46) = −0.19, so the ERC Emotion Regulation subscale was considered as a separate measure of children’s ER.
Physiological Reactivity
Children completed an impossible puzzle task modified from prior research (Hoza et al. 2001) and a social rejection task modified from the chatroom interaction task (Silk et al. 2012) in counterbalanced order. In the puzzle task, participants were presented with three puzzles, one at a time, that each displayed a 20 × 20 letter matrix. In each puzzle they were asked to find three nonsense words. After completing a practice puzzle, the three test puzzles were presented. Only the first word in the first puzzle was actually hidden in the word matrix; the remaining eight words were impossible to find. Children had 2 min to complete each puzzle and were given verbal feedback about the number of words found at the end of 2 min. As a manipulation check, after the task children rated how hard they thought the puzzles were on a 1 (not at all) to 5 (very much) scale and how many words they were able to find on a 1 (none) to 7 (all) scale.
In the social rejection task, children were told that they would be interacting with other peers through an online chat program. They first answered questions and had their picture taken to create a profile; next, they were presented with a series of age and gender-matched fictitious profiles and were asked to select the peers they most wanted to chat with. During the social rejection task, children were seated at a laptop computer and told that they had been matched with two of the peers they had selected at the first study visit. Children were then told that there would be an initial round in which each child would have a chance to choose who they would like to chat with about various topics. The task was programmed so that the other two virtual peers always were selected to make their choices first in consecutive rounds, and the participant was not chosen for 80% of the topics. A large X appeared on the picture of the player not chosen. As a manipulation check, after completion of the social rejection task participants were asked to rate how much they thought the peers liked them on a 1 (not at all) to 5 (very much) scale and how often they were chosen by the peers on a 1 (never) to 7 (all the time) scale. Children also rated on a 1 (not at all) to 5 scale (very much) scale how “sad” and how “angry” they felt directly before each task was introduced and then again directly afterwards. At the end of the assessment children were debriefed with a parent present.
Baseline RSA and SCL were measured during a 3 min period of rest when children viewed a silent video of fish swimming; baselines occurred prior to the introduction of each task. For the impossible puzzle task, RSA and SCL arousal were assessed while children attempted to solve the last two puzzles, when all words were impossible to find (4.0 min). For the social rejection task, RSA and SCL arousal were recorded while the virtual peers made their choices and the participant was repeatedly not chosen (4.5 min).Footnote 1 RSA and SCL arousal were measured with an ambulatory physiology system (Biolog UFI 3991). RSA was assessed with an EKG: three electrodes were placed in a bipolar configuration on the left and right rib cage and the sternum. Interbeat intervals were extracted, and data was visually inspected for movement or measurement artifacts and edited using CardioEdit software to correct for outliers (Brain-Body Center 2007). RSA was calculated in CardioBatch based on procedures outlined by Porges (1985). A frequency band consistent with the spontaneous respiration of adolescents (0.12 to 1.00 Hz) was used to control for spontaneous breathing. Amplitude of RSA was calculated based on the natural logarithm of the variances of 30-s epochs, which were averaged. RSA is reported in ln(ms)2 units. SCL was measured with two Ag/AgCl electrodes attached to the palmer surface of the middle phalanges of the second and third fingers on the non-dominant hand. SCL was quantified as the average electrical conductance in microsiemens. Given high correlations between the two baselines and between arousal during each task (rs > 0.55), RSA and SCL arousal at baseline and during stress tasks were calculated by averaging the two measurements. RSA reactivity (RSA-R) and SCL reactivity (SCL-R) were then calculated as the difference between baseline arousal and arousal during the tasks (reactivity = task arousal – baseline arousal). Positive RSA-R values indicate an increase in PNS activity (RSA activation) and negative values indicate a decrease in PNS activity (RSA withdrawal). Positive SCL-R values indicate an increase in SNS activity; negative values indicate a decrease in SNS activity.
Analytic Plan
A series of regression analyses were conducted in Mplus version 7 (Muthén and Muthén 1998–2012) to examine if Time 1 parent emotion socialization practices predicted Time 2 measures of children’s ER and if Time 1 ADHD symptomatology moderated these associations. Supportive and non-supportive emotion socialization practices were considered in separate models, as were each ER measure. Given evidence that baseline physiological arousal is systematically related to reactivity (Graziano and Derefinko 2013), baseline physiological arousal (RSA or SCL) prior to the task was included as a covariate in relevant models.Footnote 2 Predictor variables were mean centered prior to creating interaction terms. For significant interactions, ADHD symptoms simple slopes were calculated at 0 ADHD symptoms (10th percentile), 4 ADHD symptoms (50th percentile; referred to as moderate ADHD symptoms) and 16 ADHD symptoms (90th percentile; referred to as high ADHD symptoms). Maximum likelihood robust estimator was used to address missing dataFootnote 3 and variable skew. Unstandardized coefficients are presented below based on the recommendations of Hayes (2013).
Results
Preliminary Analyses
Descriptive statistics and intercorrelations between variables are presented in Table 1. Participants demonstrated a significant decrease in RSA and increase in SCL during the tasks (ps < 0.001), suggesting that, on average, children evidenced physiological reactivity reflected in PNS withdrawal and SNS activation. Children’s post-task evaluations indicated that they understood that they were unsuccessful on the impossible puzzle task. Children rated the puzzles’ difficulty as “quite a bit hard” (M = 4.29, SD = 0.67) and reported that they found “hardly any words” (M = 1.69, SD = 0.57). Additionally, on average, participants reported that the other peers in the chat task liked them “just a little” (M = 2.24, SD = 0.66) and that they were chosen “not very often” (M = 2.79, SD = 0.67), suggesting understanding of the task.Footnote 4 During both tasks, children reported a significant increase in self-reported feelings of anger and sadness from pre to post-rejection (ps < 0.02), suggesting a negative emotional reaction. Child-reported post-task evaluations did not significantly correlate with ADHD symptoms (rs = 0.06–0.21, ps > 0.21).
Do Parental Emotion Socialization Practices Longitudinally Predict Children’s ER?
Results are displayed in Tables 2 and 3. Parents’ use of more supportive emotion socialization significantly predicted higher parent-rated Emotion Regulation at Time 2. No other significant effects of emotion socialization emerged for supportive or non-supportive reactions.
Do ADHD Symptoms Moderate the Relation between Parental Emotion Socialization and Children’s ER?
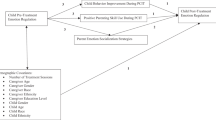
A significant interaction was found between ADHD symptoms and supportive emotion socialization in predicting SCL-R. Simple slopes indicated that when children had high ADHD symptoms, greater supportive practices were associated with significantly greater SCL-R, b = 1.37, SE = 0.61, p = 0.03. This relation was not found for children with moderate, b = 0.13, SE = 0.28, p = 0.64, or low, b = −0.28, SE = 0.27, p = 0.29, ADHD symptoms. As shown in Fig. 1a, children with moderate or no ADHD symptoms demonstrated moderate SCL-R, regardless of parent emotion socialization level. However, children with high ADHD symptoms evidenced low SCL-R when parents demonstrated low rates of supportive practices but comparatively high SCL-R when parents were high in supportive practices. ADHD symptoms did not moderate the relation between supportive emotion socialization practices and the other ER measures.
a ADHD symptoms moderating the relation between supportive emotion socialization practices and SCL-R. SCL-R = task arousal – baseline arousal, averaged across the two tasks. b ADHD symptoms moderating the relation between non-supportive emotion socialization practices and parent- and teacher-reported Emotional Lability
With regard to non-supportive emotion socialization, there was a significant interaction between non-supportive practices and child ADHD symptoms in predicting Emotional Lability. Simple slopes analyses revealed that non-supportive practices significantly predicted greater Emotional Lability for children with moderate, b = 0.30, SE = 0.12, p = 0.01, and high, b = 0.82, SE = 0.27, p < 0.01, levels of ADHD symptoms. This relation was not found for children with low ADHD symptoms, b = 0.13, SE = 0.11, p = 0.27. As shown in Fig. 1b, children with high ADHD symptoms displayed relatively low Emotional Lability when parents were low in non-supportive reactions; however, when parents were high in use of non-supportive responses, they displayed high levels of Emotional Lability. Children with moderate ADHD symptoms also displayed more emotional lability when parents used high levels of non-supportive reactions; however, these children were still lower in Emotional Lability than children with high levels of ADHD symptoms. Children with no ADHD symptoms displayed low levels of Emotional Lability regardless of parental non-supportive reactions. ADHD symptoms did not significantly moderate the relation between non-supportive practices and the other ER measures.Footnote 5
Follow-Up Tests of Robustness
Given the number of analyses being run, a false discovery rate-controlling analysis (Benjamini and Hochberg 1995, 2000) was conducted as a follow-up test of the robustness of effects; false discovery rate controlling analysis is designed to control the expected proportion of false discoveries (i.e., Type I Error). To conduct a false-discovery rate analysis, all observed p-values were ordered sequentially from low (p 1) to high (p m), where m represents the total number (28) of p-values. We then identified the largest k such that p k < 0.05 * k/m. The adjusted alpha of 0.05*k/m was 0.023. All significant results had p-values below this adjusted alpha, suggesting that the main effect of supportive emotion socialization predicting parent-rated Emotion Regulation, the interaction of supportive emotion socialization practices and ADHD symptoms predicting SCL-R, and the interaction of non-supportive emotion socialization practices and ADHD symptoms predicting parent- and teacher-rated Emotional Lability were all robust findings.
Given prior research suggesting that demographic variables such as child sex, age, family SES (as measured by family income), and child ethnicity are related to ER, additional follow-up tests of robustness were conducted to examine if the pattern of significant effects were consistent when controlling for significant demographic effects. Preliminary analyses indicated that child ethnicity and race were not significantly associated with the primary study variables. Child sex was significantly correlated with Emotional Lability, r(59) = 0.27, p = 0.04, such that males had greater Emotion Lability than females. Age was significantly correlated with RSA-R, r(49) = −0.26, p < 0.05. Household income was significantly correlated with SCL-R, r(56) = −0.34, p = 0.01. Including these covariates in relevant models did not change the pattern of significant effects.
Additionally, we examined if including comorbid internalizing symptoms from the Child Behavior Checklist (Achenbach and Edelbrock 1991) or ODD symptoms from the DBD as covariates changed the pattern of significant effects. The main effect of supportive reactions on parent-rated Emotion Regulation remained significant controlling for comorbid internalizing symptoms; however, when controlling for comorbid ODD symptoms this relation became non-significant, b = 0.21, SE = 0.14, p = 0.13. It should be noted, however, that while the main effect became non-significant this was due to the SE increasing (likely due to the confound between ADHD and ODD symptoms), and that the regression coefficient in fact increased in magnitude. The interaction between supportive reactions and SCL-R and between non-supportive reactions and Emotional Lability remained significant when controlling for comorbid internalizing or ODD symptoms.
Discussion
This is the first study to longitudinally examine whether parents’ emotion socialization strategies predict multiple indices of ER and whether child ADHD symptoms moderate these relations. The results of the present study address several gaps in the literature regarding the role of parents in the development of children’s ER, especially among youth with ADHD. Results suggest that supportive parent emotion socialization practices are associated with parent-rated emotion regulation skills; in addition, results suggest that for certain indices of ER, effects differ for children with elevations in ADHD symptoms. Specifically, children high in ADHD symptoms appear to be more susceptible to parental use of emotion socialization practices – both supportive and non-supportive. There also were differences in the pattern of effects across measures of ER, highlighting the importance of measuring ER in multiple ways. Specifically, relations between emotion socialization and parent-rated emotion regulation skills were not moderated by ADHD symptomatology, whereas relations for adult-rated emotional lability and SCL-R were.
Adult-Report of Emotion Regulation
The results of the present study suggest that supportive emotion socialization parenting practices serve to promote better parent-rated emotion regulation skills in children approximately 1 year later. These findings converge with the larger body of longitudinal parenting research which has found a relation between general parenting practices and children’s ER (e.g., Graziano et al. 2010; Hoffman et al. 2006). They also extend the limited body of longitudinal research examining the relation between parent emotion socialization practices and children’s ER in typically developing children (Gottman et al. 1996, 1997; Kochanska et al. 2015) by suggesting that when parents are high in supportive emotion socialization practices children may display better understanding and responses to emotions 1 year later.
Interestingly, there were no main effects of non-supportive parenting practices predicting children’s ER in daily life. However, other work does suggest that the use of non-supportive emotion socialization practices is associated with poorer ER (Lunkenheimer et al. 2007), poorer socioemotional functioning (Jones et al. 2002) and greater externalizing problems (Tao et al. 2010). One difference that may account for this discrepancy is that prior studies used emotion dismissing coding rather than parent self-report of emotion socialization to assess non-supportive reactions. It is possible that parents are less likely to report their own use of non-supportive reactions and that coded behavioral observation may yield different results. This will be an important possibility for future research to explore in ADHD samples.
Although no main effects were found for non-supportive emotion socialization practices on any measure of child ER, non-supportive practices were predictive of parent and teacher reports of emotional lability for youth with high levels of ADHD. Specifically, for children with high ADHD symptomatology, having parents who used more non-supportive emotion socialization practices was a risk factor for greater emotional lability. This finding suggests that children with high ADHD symptomatology might be at increased risk for the deleterious effects of having a parent dismiss or invalidate their negative emotions, resulting in more labile emotions and intense emotional reactions in daily life. This finding is particularly concerning given that previous research has found that parents of children with ADHD possess risk factors for using non-supportive parenting practices. Specifically, these parents experience greater psychopathology (e.g., Middleton et al. 2009), which has been associated with use of more non-supportive emotion socialization practices (Breaux et al. 2016). Investigation of the processes leading to differences in parents’ emotion socialization responses will be an important area for future studies to explore.
It is noteworthy that results were not consistent across the two measures of adult-rated ER. There were main effects of emotion socialization on emotion regulation skills but not on children’s emotional lability. It is possible that the Emotion Regulation scale represents a set of skills that are largely acquired through parenting practices, which influence all children, not just those with ADHD. In contrast, emotional lability has been found to be an aspect of emotion dysregulation that may specifically characterize children with ADHD (Martel 2009; McQuade and Breaux 2016). Consequently, children high in ADHD symptoms may be predisposed to emotional lability, which may be further exacerbated when parents use non-supportive reactions. These negative reactions to emotions may model a negative and reactive response style, which may be particularly detrimental if children are already vulnerable to emotion lability. In contrast, children without ADHD symptoms may possess the internal capacities to appropriately regulate their emotional reactions and thus are not affected by non-supportive parenting practices.
Physiological Measures of Emotion Regulation
Our findings are the first to consider whether parent emotion socialization and child ADHD symptoms interact to predict physiological manifestations of emotionality and ER in children. Our current findings suggest that for children with high levels of ADHD symptoms, more supportive emotion socialization practices predict an increase in SCL-R in response to negative stressors. In contrast, children high in ADHD symptoms whose parents use low levels of supportive practices displayed low SCL-R. Low SCL-R in response to negative stressors and challenge has been proposed to suggest an insensitivity to punishment (Beauchaine et al. 2001) and a failure to experience normative levels of fear (Ortiz and Raine 2004). Indeed, some evidence suggests that children with ADHD may display a lack of SNS arousal or reactivity, which may reflect a specific biological vulnerability in this population (Beauchaine et al. 2001; Crowell et al. 2006; Musser et al. 2013). In the context of negative failure, it may be expected that children will have a negative emotional reaction, reflected in increased SCL-R. Indeed, children with zero or moderate levels of ADHD symptoms displayed moderate SCL-R, regardless of parent supportive practices. For youth high in ADHD symptoms, highly supportive parenting may help children with ADHD have greater emotional sensitivity to environmental stressors.
In contrast, emotion socialization practices were not predictive of RSA-R in the present study. Other researchers also have failed to find a direct link between emotion socialization and RSA-R (Perry et al. 2012; Scrimgeour et al. 2016). However, others have found significant effects (Gottman et al. 1996). Differences across studies may be accounted for by differences in the specific context in which RSA-R is evoked or the age of participants. A varied range of tasks have been used to assess RSA-R, and to our knowledge, none have specifically examined reactivity to standardized failure tasks. Research suggests that there are differential associations between RSA-R and adjustment depending on the specific context in which RSA is assessed (Obradović et al. 2011), highlighting the importance of considering children’s physiological reactivity in a range of contexts. Further, the few studies finding links between parenting practices and RSA-R have used preschool samples (Calkins et al. 1998; Gottman et al. 1996; Hastings et al. 2008). It is possible that there is a critical period when parenting practices influence RSA-R, with parenting no longer having the same effect in late childhood/early adolescence. It also is possible that RSA-R is strictly reflective of a biological vulnerability and is therefore less strongly influenced by parenting practices. To further advance our findings it will be important for researchers to consider how emotion socialization relates to children’s physiological reactivity across a range of contextual factors and in different developmental periods. Comparison of findings to studies examining reactivity to non-threatening situations or when performance is not standardized may be particularly useful in elucidating when certain patterns of physiological regulation are maladaptive.
Limitations
The findings of the present study should be interpreted with several limitations in mind. First, emotion socialization was based on parents’ self-report, which is subject to possible defensiveness or positive bias. Future studies should use a multi-method assessment of emotion socialization, including observational measures. Second, although we used a multi-method approach to assess ER, it is still possible that issues of shared method variance influenced results. Specifically, parent report was used in the combined parent and teacher measure of ADHD symptoms, the assessment of emotion socialization, and the adult-report measures of children’s ER. Third, while the analyses were longitudinal in nature, ER was only examined at Time 2; thus, we could not control for initial levels of ER or examine changes over time in ER. Fourth, we excluded children suspected of having a sluggish cognitive tempo of ADHD from the present sample; thus, the present findings do not generalize to all children with ADHD. Although some theoretical discussions argue that individuals with a sluggish cognitive tempo do not display emotion dysregulation deficits (Barkley 2015), emerging evidence suggests they may also have ER challenges (e.g., Becker et al. 2016). Thus, future research should consider examining the role of emotion socialization in the ER profiles of children with sluggish cognitive tempo. Fifth, our sample was relatively small. Thus, we were unable to examine whether effects may be further moderated by additional factors such as child sex, age, or comorbidity; we also were not sufficiently powered to detect small magnitude effects. Finally, our sample primarily consisted of white families from a fairly high socioeconomic level and with mothers as primary caregivers. Therefore, results may not generalize to all children or parents. Given evidence that emotion socialization practices have differential effects for families of different ethnicities (e.g., Keller and Otto 2009; Lugo-Candelas et al. 2016), it is important for future research to be conducted with a larger, more diverse sample in order to examine whether processes differ across demographic characteristics.
Clinical Implications
Despite these limitations, the present study has important clinical implications. Specifically, our findings support the use of interventions targeting supportive parent emotion socialization (e.g., Havighurst et al. 2010) and suggest that such interventions may foster better ER in children. Several groups of researchers have added an emotion socialization/coaching module to behavioral intervention programs for preschoolers with ADHD symptoms and found that such interventions hold promise for improving children’s emotion knowledge and functioning and reducing children’s ADHD symptoms and oppositional defiance (Chronis-Tuscano et al. 2016; Havighurst et al. 2013; Herbert et al. 2013); however, these studies have focused on preschool children and have not directly examined the efficacy of the interventions in decreasing emotion dysregulation. The findings of this study suggest that adding an emotion socialization module to behavioral training for older children with ADHD may be effective in reducing emotion dysregulation in this at-risk population; this is a promising avenue for future research to explore.
Notes
In order to further minimize continued physiological arousal after children completed the first stressor task, the task was followed by an additional 3 min period of rest. Children were then provided with an external excuse for why the task was challenging (i.e., due to a research assistant mistake) and then completed a 3 min distractor task.
The pattern of significant effects was consistent when also including dummy coded variables of stimulant medication use and SSRI use as covariates.
Missing data can be seen based on the sample sizes presented in Table 1. Teachers did not complete the BRIEF for 14 children. Physiological reactivity data were treated as missing for one child due to extreme behavior problems. Due to equipment failure, RSA data was missing for four additional participants.
Two participants indicated suspicion that the impossible puzzle task was rigged and two other participants indicated suspicion that the social rejection task was rigged during the debriefing procedure; however, these subjects reported that they were unsure if their suspicion was correct while they completed the task. Treating reactivity data for these participants as missing did not change the pattern of results; hence, their data was retained in the final analyses.
Analyses were also run with ADHD diagnosis as a dichotomous variable; all significant interactions remained and no new results emerged. Given that the current sample includes children with subthreshold ADHD, using ADHD symptomatology as a moderator was viewed as a more appropriate measurement approach.
References
Achenbach, T. M., & Edelbrock, C. (1991). Child behavior checklist. Burlington: University of Vermont Research Center for Children, Youth and Families.
Barkley, R. A. (2015). Concentration deficit disorder (sluggish cognitive tempo). In R. A. Barkley (Ed.), Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (pp. 81–115). New York: Guilford Press.
Beauchaine, T. P., Katkin, E. S., Strassberg, Z., & Snarr, J. (2001). Disinhibitory psychopathology in male adolescents: Discriminating conduct disorder from attention-deficit/hyperactivity disorder through concurrent assessment of multiple autonomic states. Journal of Abnormal Psychology, 110, 610–624. doi:10.1037/0021-843X.110.4.610.
Beauchaine, T. P., Gatzke-Kopp, L., Neuhaus, E., Chipman, J., Reid, M. J., & Webster-Stratton, C. (2013). Sympathetic-and parasympathetic-linked cardiac function and prediction of externalizing behavior, emotion regulation, and prosocial behavior among preschoolers treated for ADHD. Journal of Consulting and Clinical Psychology, 81, 481493. doi:10.1037/a0032302.
Becker, S. P., Leopold, D. R., Burns, G. L., Jarrett, M. A., Langberg, J. M., Marshall, S. A., et al. (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 163–178. doi:10.1093/jpepsy/jst058.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological), 57, 289–300. doi:10.2307/2346101.
Benjamini, Y., & Hochberg, Y. (2000). On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics, 25, 60–83. doi:10.2307/1165312.
Berntson, G. G., Bigger, J. T., Eckberg, D. L., Grossman, P., Kaufmann, P. G., Malik, M., et al. (1997). Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology, 34, 623–648. doi:10.1111/j.1469-8986.1997.tb02140.x.
Boucsein, W. (1992). Electrodermal activity. New York: Plenum Press.
Brain-Body Center. (2007). CardioEdit=CardioBatch [computer software]. Chicago: University of Illinois.
Breaux, R. P., Harvey, E. A., & Lugo-Candelas, C. I. (2016). The role of parent psychopathology in emotion socialization. Journal of Abnormal Child Psychology, 44, 731–743. doi:10.1007/s10802-015-0062-3.
Bryant, B. K. (1987). Mental health, temperament, family, and friends: Perspectives on children’s empathy and social perspective taking. In N. Eisenberg & J. Strayer (Eds.), Empathy and its development (pp. 245–270). Cambridge: Cambridge University Press.
Bunford, N., Evans, S. W., & Wymbs, F. (2015). ADHD and emotion dysregulation among children and adolescents. Clinical Child and Family Psychology Review, 18, 185–217. doi:10.1007/s10567-015-0187-5.
Calkins, S. D., Smith, C. L., Gill, K. L., & Johnson, M. C. (1998). Maternal interactive style across contexts: Relations to emotional, behavioral, and physiological regulation during toddlerhood. Social Development, 7, 350–369. doi:10.1111/1467-9507.00072.
Chronis-Tuscano, A., Lewis-Morrarty, E., Woods, K. E., O’Brien, K. A., Mazursky-Horowitz, H., & Thomas, S. R. (2016). Parent–child interaction therapy with emotion coaching for preschoolers with attention-deficit/hyperactivity disorder. Cognitive and Behavioral Practice, 1, 62–78. doi:10.1016/j.cbpra.2014.11.001.
Cole, P. M., Dennis, T. A., Smith-Simon, K. E., & Cohen, L. H. (2009). Preschoolers’ emotion regulation strategy understanding: Relations with emotion socialization and child self-regulation. Social Development, 18, 324–352. doi:10.1111/j.1467-9507.2008.00503.x.
Crowell, S. E., Beauchaine, T. P., Gatzke-Kopp, L., Sylvers, P., Mead, H., & Chipman-Chacon, J. (2006). Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. Journal of Abnormal Psychology, 115, 174–178. doi:10.1037/0021-843X.115.1.174.
Crowell, S. E., Baucom, B. R., Yaptangco, M., Bride, D., Hsiao, R., McCauley, E., & Beauchaine, T. P. (2014). Emotion dysregulation and dyadic conflict in depressed and typical adolescents: Evaluating concordance across psychophysiological and observational measures. Biological Psychology, 98, 50–58. doi:10.1016/j.biopsycho.2014.02.009.
Dawson, M. E., Schell, A. M., & Filion, D. L. (2007). The electrodermal system. In J. T. Cacioppo, L. G. Tassinary, G. G. Berntson, J. T. Cacioppo, L. G. Tassinary, & G. G. Berntson (Eds.), Handbook of psychophysiology (3rd ed., pp. 159–181). New York: Cambridge University Press. doi:10.1017/CBO9780511546396.007.
Denham, S. A., Bassett, H. H., & Wyatt, T. (2007). The socialization of emotional competence. In J. E. Grusec, P. D. Hastings, J. E. Grusec, & P. D. Hastings (Eds.), Handbook of socialization: Theory and research (pp. 614–637). New York: Guilford Press.
Duncombe, M. E., Havighurst, S. S., Holland, K. A., & Frankling, E. J. (2012). The contribution of parenting practices and parent emotion factors in children at risk for disruptive behavior disorders. Child Psychiatry & Human Development, 43, 715–733. doi:10.1007/s10578-012-0290-5.
Eisenberg, N., & Spinrad, T. L. (2004). Emotion-related regulation: Sharpening the definition. Child Development, 75, 334–339. doi:10.1111/j.1467-8624.2004.00674.x.
Eisenberg, N., Fabes, R. A., & Murphy, B. C. (1996). Parents' reactions to children's negative emotions: Relations to children's social competence and comforting behavior. Child Development, 67, 2227–2247. doi:10.2307/1131620.
Eisenberg, N., Cumberland, A., & Spinrad, T. L. (1998). Parental socialization of emotion. Psychological Inquiry, 9, 241–273. doi:10.1207/s15327965pli0904_1.
El-Sheikh, M. (2005). The role of emotional responses and physiological reactivity in the marital conflict-child functioning link. Journal of Child Psychology and Psychiatry, 46, 1191–1199. doi:10.1111/j.1469-7610.2005.00418.x.
Fabes, R. A., Eisenberg, N., & Bernzweig, J. (1990). The coping with Children’s negative emotions scale: Procedures and scoring. Available from authors. Tempe: Arizona State University.
Fabes, R. A., Leonard, S. A., Kupanoff, K., & Martin, C. L. (2001). Parental coping with children's negative emotions: Relations with children's emotional and social responding. Child Development, 72, 907–920. doi:10.1111/1467-8624.00323.
Fabes, R. A., Poulin, R. E., Eisenberg, N., & Madden-Derdich, D. A. (2002). The coping with Children’s negative emotions scale (CCNES): Psychometric properties and relations with children’s emotional competence. Marriage & Family Review, 34, 285–310. doi:10.1300/J002v34n03_05.
Franklin, J. C., Jamieson, J. P., Glenn, C. R., & Nock, M. K. (2015). How developmental psychopathology theory and research can inform the research domain criteria (RdoC) project. Journal of Clinical Child and Adolescent Psychology, 44, 280–290. doi:10.1080/15374416.2013.873981.
Gioia, G. A., Isquith, P. K., Guy, S. C., & Kenworthy, L. (2000). Behavior rating inventory of executive function: BRIEF. Odessa: Psychological Assessment Resources.
Gottman, J. M., Katz, L. F., & Hooven, C. (1996). Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology, 10, 243–268. doi:10.1037/0893-3200.10.3.243.
Gottman, J. M., Katz, L. F., & Hooven, C. (1997). Meta-emotion: How families communicate emotionally. Mahwah: Psychology Press.
Graziano, P., & Derefinko, K. (2013). Cardiac vagal control and children’s adaptive functioning: A meta-analysis. Biological Psychology, 94, 22–37. doi:10.1016/j.biopsycho.2013.04.011.
Graziano, P. A., & Garcia, A. (2016). Attention-deficit hyperactivity disorder and children’s emotion dysregulation: A meta-analysis. Clinical Psychology Review, 46, 106–123. doi:10.1016/j.cpr.2016.04.011.
Graziano, P. A., Keane, S. P., & Calkins, S. D. (2010). Maternal behaviour and children’s early emotion regulation skills differentially predict development of children’s reactive control and later effortful control. Infant and Child Development, 19, 333–353. doi:10.1002/icd.670.
Hastings, P. D., Sullivan, C., McShane, K. E., Coplan, R. J., Utendale, W. T., & Vyncke, J. D. (2008). Parental socialization, vagal regulation and preschoolers’ anxious difficulties: Direct mothers and moderated fathers. Child Development, 1, 45–64. doi:10.1111/j.1467-8624.2007.01110.x.
Havighurst, S. S., Wilson, K. R., Harley, A. E., Prior, M. R., & Kehoe, C. (2010). Tuning in to kids: Improving emotion socialization practices in parents of preschool children–findings from a community trial. Journal of Child Psychology and Psychiatry, 51, 1342–1350. doi:10.1111/j.1469-7610.2010.02303.x.
Havighurst, S. S., Wilson, K. R., Harley, A. E., Kehoe, C., Efron, D., & Prior, M. R. (2013). Tuning into kids: Reducing young children’s behavior problems using an emotion coaching parenting program. Child Psychiatry & Human Development, 44, 247–264. doi:10.1007/s10578-012-0322-1.
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press.
Healey, D. M., Flory, J. D., Miller, C. J., & Halperin, J. M. (2011). Maternal positive parenting style is associated with better functioning in hyperactive/inattentive preschool children. Infant and Child Development, 20, 148–161. doi:10.1002/icd.682.
Herbert, S. D., Harvey, E. A., Roberts, J. L., Wichowski, K., & Lugo-Candelas, C. I. (2013). A randomized controlled trial of a parent training and emotion socialization program for families of hyperactive preschool-aged children. Behavior Therapy, 44, 302–316. doi:10.1016/j.beth.2012.10.004.
Hersh, M. A., & Hussong, A. M. (2009). The association between observed parental emotion socialization and adolescent self-medication. Journal of Abnormal Child Psychology, 37, 493–506. doi:10.1007/s10802-008-9291-z.
Hoffman, M. L. (1983). Affective and cognitive processes in moral internalization. In E. T. Higgins, D. N. Ruble, & W. W. Hartup (Eds.), Social cognition and social development: A sociocultural perspective (pp. 236–274). Cambridge: Cambridge University Press.
Hoffman, C., Crnic, K. A., & Baker, J. K. (2006). Maternal depression and parenting. Implications for children’s emergent emotion regulation and behavioral functioning. Parenting: Science and Practice, 6, 271–295. doi:10.1207/s15327922par0604_1.
Hoza, B., Waschbusch, D. A., Owens, J. S., Pelham, W. E., & Kipp, H. (2001). Academic task persistence of normally achieving ADHD and control boys: Self-evaluations, and attributions. Journal of Consulting and Clinical Psychology, 69, 271–283. doi:10.1037/0022-006X.69.2.271.
Hubbard, J. A., Smithmyer, C. M., Ramsden, S. R., Parker, E. H., Flanagan, K. D., Dearing, K. F., et al. (2002). Observational, physiological, and self-report measures of children’s anger: Relations to reactive versus proactive aggression. Child Development, 73, 1101–1118. doi:10.1111/1467-8624.00460.
Hunter, E. C., Katz, L. F., Shortt, J. W., Davis, B., Leve, C., Allen, N. B., & Sheeber, L. B. (2011). How do I feel about feelings? Emotion socialization in families of depressed and healthy adolescents. Journal of Youth and Adolescence, 40, 428–441. doi:10.1007/s10964-010-9545-2.
Jones, S., Eisenberg, N., Fabes, R. A., & MacKinnon, D. P. (2002). Parents’ reactions to elementary school children’s negative emotions: Relations to social and emotional functioning at school. Merrill-Palmer Quarterly, 48, 133–159. doi:10.1353/mpq.2002.0007.
Keller, H., & Otto, H. (2009). The cultural socialization of emotion regulation during infancy. Journal of Cross-Cultural Psychology, 40, 996–1011. doi:10.1177/0022022109348576.
Kochanska, G., Brock, R. L., Chen, K. H., Aksan, N., & Anderson, S. W. (2015). Paths from mother-child and father-child relationships to externalizing behavior problems in children differing in electrodermal reactivity: A longitudinal study from infancy to age 10. Journal of Abnormal Child Psychology, 43, 721–734. doi:10.1007/s10802-014-9938-x.
Lugo-Candelas, C. I., Harvey, E. A., Breaux, R. P., & Herbert, S. D. (2016). Ethnic differences in the relation between parental emotion socialization and mental health in emerging adults. Journal of Child and Family Studies, 25, 922–938. doi:10.1007/s10826-015-0266-8.
Lunkenheimer, E. S., Shields, A. M., & Cortina, K. S. (2007). Parental emotion coaching and dismissing in family interaction. Social Development, 16, 232–248. doi:10.1111/j.1467-9507.2007.00382.x.
Martel, M. M. (2009). Research review: A new perspective on attention-deficit hyperactivity disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry, 50, 1042–1051. doi:10.1111/j.1469-7610.2009.02105.x.
McQuade, J. D., & Breaux, R. P. (2016). Are elevations in ADHD symptoms associated with physiological reactivity and emotion dysregulation in children? Journal of Abnormal Child Psychology. Advanced Online Publication. doi:10.1007/s10802-016-0227-8.
McQuade, J. D., Mendoza, S. A., Larsen, K. L., & Breaux, R. P. (2017). The nature of social positive illusory bias: Reflection of social impairment, self-protective motivation, or poor executive functioning? Journal of Abnormal Child Psychology, 45, 289–300. doi:10.1007/s10802-016-0172-6.
Melnick, S. M., & Hinshaw, S. P. (2000). Emotion regulation and parenting in AD/HD and comparison boys: Linkages with social behaviors and peer preference. Journal of Abnormal Child Psychology, 28, 73–86. doi:10.1023/A:1005174102794.
Middleton, M., Scott, S. L., & Renk, K. (2009). Parental depression, parenting behaviours, and behaviour problems in young children. Infant and Child Development, 18, 323–336. doi:10.1002/icd.598.
Miller, J. G., Chocol, C., Nuselovici, J. N., Utendale, W. T., Simard, M., & Hastings, P. D. (2013). Children’s dynamic RSA change during anger and its relations with parenting, temperament, and control of aggression. Biological Psychology, 92, 417–425. doi:10.1016/j.biopsycho.2012.12.005.
Murray-Close, D. (2013). Psychophysiology of adolescent peer relations I: Theory and research findings. Journal of Research on Adolescence, 23, 236–259. doi:10.1111/j.1532-7795.2012.00828.x.
Musser, E. D., Galloway-Long, H. S., Frick, P. J., & Nigg, J. T. (2013). Emotion regulation and heterogeneity in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 52, 163–171. doi:10.1016/j.jaac.2012.11.009.
Muthén, L. K., & Muthén, B. O. (1998-2012). Mplus User’s Guide (Seventh ed.). Los Angeles: Muthén & Muthén.
Obradović, J., Bush, N. R., & Boyce, W. T. (2011). The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: The role of laboratory stressors. Development and Psychopathology, 23, 101–114. doi:10.1017/S0954579410000672.
Ortiz, J., & Raine, A. (2004). Heart rate level and antisocial behavior in children and adolescents: A meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 154–162. doi:10.1097/00004583-200402000-00010.
Pelham, W. E., Gnagy, E. M., Greenslade, K. E., & Milich, R. (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 31, 210–218. doi:10.1097/00004583-199203000-00006.
Pelham Jr., W. E., Fabiano, G. A., & Massetti, G. M. (2005). Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34, 449–476. doi:10.1207/s15374424jccp3403_5.
Perry, N. B., Calkins, S. D., Nelson, J. A., Leerkes, E. M., & Marcovitch, S. (2012). Mothers' responses to children's negative emotions and child emotion regulation: The moderating role of vagal suppression. Developmental Psychobiology, 54, 503–513. doi:10.1002/dev.20608.
Porges, S. W. (1985). U.S. Patent No. 4,510,944. Washington, DC: U.S. Patent and Trademark Office.
Porges, S. W. (2001). The polyvagal theory: Phylogenetic substrates of a social nervous system. International Journal of Psychophysiology, 42, 123–146. doi:10.1016/S0167-8760(01)00162-3.
Porges, S. W. (2003). The polyvagal theory: Phylogenetic contributions to social behavior. Physiology & Behavior, 79, 503–513. doi:10.1016/S0031-9384(03)00156-2.
Ramsden, S. R., & Hubbard, J. A. (2002). Family expressiveness and parental emotion coaching: Their role in children’s emotion regulation and aggression. Journal of Abnormal Child Psychology, 30, 657–667. doi:10.1023/A:1020819915881.
Sanders, W., Zeman, J., Poon, J., & Miller, R. (2015). Child regulation of negative emotions and depressive symptoms: The moderating role of parental emotion socialization. Journal of Child and Family Studies, 24, 402–415. doi:10.1007/s10826-013-9850-y.
Sanislow, C. A., Pine, D. S., Quinn, K. J., Kozak, M. J., Garvey, M. A., Heinssen, R. K., et al. (2010). Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology, 119, 631–639. doi:10.1037/a0020909.
Scrimgeour, M. B., Davis, E. L., & Buss, K. A. (2016). You get what you get and you don’t throw a fit!: Emotion socialization and child physiology jointly predict early prosocial development. Developmental Psychology, 52, 102–116. doi:10.1037/dev0000071.
Seymour, K. E., Chronis-Tuscano, A., Iwamoto, D. K., Kurdziel, G., & MacPherson, L. (2014). Emotion regulation mediates the association between ADHD and depressive symptoms in a community sample of youth. Journal of Abnormal Child Psychology, 42, 611–621. doi:10.1007/s10802-013-9799-8.
Shaw, P., Stringaris, A., Nigg, J., & Leibenluft, E. (2014). Emotional dysregulation and attention-deficit/hyperactivity disorder. The American Journal of Psychiatry, 171, 276–293. doi:10.1176/aapi.ajp.2013.1307066.
Shields, A. M., & Cicchetti, D. (1995, March). The development of an emotion regulation assessment battery: Reliability and validity among at-risk grade-school children. Indianapolis: Poster presented at the biennial meeting of the Society for Research in Child Development.
Shields, A., & Cicchetti, D. (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33, 906–916. doi:10.1037/0012-1649.33.6.906.
Shipman, K. L., Schneider, R., Fitzgerald, M. M., Sims, C., Swisher, L., & Edwards, A. (2007). Maternal emotion socialization in maltreating and non-maltreating families: Implications for children’s emotion regulation. Social Development, 16, 268–285. doi:10.1111/j.1467-9507.2007.00384.x.
Silk, J. S., Stroud, L. R., Siegle, G. J., Dahl, R. E., Lee, K. H., & Nelson, E. E. (2012). Peer acceptance and rejection through the eyes of youth: Pupillary, eyetracking and ecological data from the chatroom interact task. Social Cognitive and Affective Neuroscience, 7, 93–105. doi:10.1093/scan/nsr044.
Sjöwall, D., Roth, L., Lindqvist, S., & Thorell, L. B. (2013). Multiple deficits in ADHD: Executive dysfunction, delay aversion, reaction time variability, and emotional deficits. Journal of Child Psychology and Psychiatry, 54, 619–627. doi:10.1111/jcpp.12006.
Tao, A., Zhou, Q., & Wang, Y. (2010). Parental reactions to children’s negative emotions: Prospective relations to Chinese children’s psychological adjustment. Journal of Family Psychology, 24, 135–144. doi:10.1037/a0018974.
Tripp, G., & Wickens, J. R. (2008). Research review: Dopamine transfer deficit: A neurobiological theory of altered reinforcement mechanisms in ADHD. Journal of Child Psychology and Psychiatry, 49, 691–704. doi:10.1111/j.1469-7610.2007.01851.x.
Ward, A. R., Alarcón, G., Nigg, J. T., & Musser, E. D. (2015). Variation in parasympathetic dysregulation moderates short-term memory problems in childhood attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology, 43, 1573–1583. doi:10.1007/s10802-015-0054-3.
Acknowledgements
We are grateful to the families and teachers who generously participated in this study. We would like to acknowledge Rose Miller, Elizabeth Mathias, Angelina Gomez, Taylor Penzel, and Kristy Larsen for their important role in collecting this data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all parents included in the study; assent was obtained from all children included in the study.
Rights and permissions
About this article
Cite this article
Breaux, R.P., McQuade, J.D., Harvey, E.A. et al. Longitudinal Associations of Parental Emotion Socialization and Children’s Emotion Regulation: The Moderating Role of ADHD Symptomatology. J Abnorm Child Psychol 46, 671–683 (2018). https://doi.org/10.1007/s10802-017-0327-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-017-0327-0