Abstract
Whereas previous research on environmental factors implicated in the intergenerational transmission of depression has tended to focus on the role of parenting quality (e.g., harshness), the current study sought to assess whether structural aspects of families may contribute to depression-relevant affective and immune processes in youths. Specifically, the present study examined the role of family routines in linking parental depressive symptoms to youth emotion regulation, a depression-relevant marker of low-grade inflammation, and depressive symptoms in youths. 261 parent-adolescent dyads reported on their own depressive symptoms, family routines, and youths’ emotion regulation abilities. In addition, peripheral blood was drawn from youths to assess levels of the proinflammatory cytokine interleukin 6 (IL-6). Path analyses provided support for a model in which parental depressive symptoms related to fewer family routines, which in turn were associated with higher IL-6 and depressive symptoms in youths as well as marginally associated with worse youth emotion regulation. Moreover, family routines were found to statistically account for part of the association between parent- and youth- depressive symptoms. Together, these results suggest that family routines may represent an additional facet of the family environment that can potentially contribute to the intergenerational transmission of depressive symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression in children and adolescents (hereafter referred to as youths) is a prevalent, recurrent, and frequently chronic disorder, representing a considerable public health burden (Birmaher et al. 2005; Costello et al. 2002). Approximately 20 % of individuals will meet full diagnostic criteria for major depressive disorder at least once by age 18 (Lewinsohn et al. 1993). Once diagnosed, these youths also have a cumulative probability of recurrence of 40 % within 2 years and 70 % within 5 years (Birmaher et al. 1996; Lewinsohn et al. 2000), as well as a two-fold increased chance of developing major depression as adults (Weissman et al. 1999). The extent of youth depression is clearly considerable; moreover, its impact can be tragic. Depression places youths at greater risk for psychiatric comorbidity, substance use, and suicide, the third most common cause of death among individuals aged 10–24 (Angold and Costella 1993; Galaif et al. 2007; Miniño 2010; Rohde et al. 1991). An understanding of the etiology of this disorder in youths is therefore vital to developing and expanding interventions aimed at its prevention and treatment (Howe 2003).
Parental depression is one key factor that predicts risk for youth depression (Goodman et al. 2011; Halligan et al. 2007; Hammen and Brennan 2003), and, as such, it offers valuable insight into pathways that may contribute to the development of the disorder. Here, work on intergenerational transmission mechanisms highlights the significance of environmental factors in conferring risk. Although shared genes certainly play a critical role in depression (Lahey et al. 2011; Sullivan et al. 2000), genetics do not wholly, or even largely, account for risk (Silberg et al. 2010; Singh et al. 2010), such that exposure to parental depression increases risk for youth depression regardless of shared genetic profiles (Tully et al. 2008). This exposure is believed to affect multiple processes relevant to depression in youths, including not only psychological development, but also internal biological processes, such as children’s stress response systems (Del Giudice et al. 2011). This is consistent with a psychoneuroimmunological approach to the study of psychopathology, which emphasizes transactions between the immune and nervous systems in shaping mental and physical health (Raison et al. 2006). To this end, the most prominent models of how environmental factors associated with parental depression lead to youth depression include both psychological and physiological mechanisms (Goodman and Gotlib 1999).
A primary pathway for environmental risk—and subsequent effects on psychological and biological processes—is through impairments in parenting behaviors (Lim et al. 2008). Hammen et al. (2004) found that impoverished parenting behaviors, in the form of greater hostility/control and less warmth/acceptance—in conjunction with greater interpersonal stress—accounted for the links between maternal depression and depression in youths. Drawing on multiple informants, Ge et al. (1994) similarly showed that harsher and more inconsistent disciplinary behaviors by parents mediated the association between parental depressed mood and depressive symptoms in adolescents. Meta-analyses confirm that parents with depression demonstrate significantly more negative parenting behaviors, including more frequent hostile or intrusive behaviors and expressions of negative affect (Lovejoy et al. 2000), and that behaviors relating to parental warmth, withdrawal, aversiveness, and over-involvement are reliably associated with youth depression (McLeod et al. 2007).
Family Routines: an Alternative Factor in the Intergenerational Transmission of Depression?
Although previous work has tended to focus on the quality of family behaviors (such as warmth or harshness), structural aspects of family interactions may also be important to the intergenerational transmission of depression. Specifically, we propose that family routines—by providing organization and predictability to relationships between parents and children—may represent a novel dimension of family life to consider in the context of the intergenerational transmission of depression. Jensen et al. (1983) define family routines as “observable, repetitive behaviors which involve two or more family members and which occur with predicable regularity in the day-to-day and week-to-week life of the family” (p.201). Some examples of family routines include eating meals together, engaging in regularly designated family leisure time, and having coordinated wake and bedtime rituals. Although family routines are not completely independent from indicators of quality (e.g., more harmonious families may better implement routines), these behaviors are believed to primarily act as structuring units, fostering stability by establishing expectations and generating greater predictability within the family (Boyce et al. 1983; Jensen et al. 1983).
This predictability may be consequential for mental health; several lines of research support the notion that experiences that are unpredictable are more closely associated with processes relating to depression—such as learned helplessness, perceived stress, psychological well-being, and physiological stress responses—than experiences that are predictable, regardless of whether the experiences are controllable (Abramson et al. 1978; Sapolsky 1994; Tetrick and LaRocco 1987; Tiggemann and Winefield 1987). For similar reasons, chaotic or capricious parenting practices that undermine predictability are held as maladaptive forms of caregiving (Gardner 1989; Ross and Hill 2002) and may have repercussions for youth depression. For example, Benson et al. (2008) demonstrated that sixth-grade children with mothers who were less consistent with rule-enforcement showed higher levels of both internalizing and externalizing symptoms. Regarding family routines specifically, Brody and Flor (1997) found that children in families with fewer predictable routines had worse behavioral self-control, which in turn was associated with more internalizing and externalizing symptoms.
If family routines may confer risk for youth depression, through what pathways might these associations operate? We propose that family routines may contribute to the intergenerational transmission of depression by shaping two key processes in a biopsychosocial model of depression, specifically, youth cellular inflammatory processes and emotion regulation abilities. To situate this hypothesis, we first describe how family routines may act on inflammation and emotion regulation processes and then review research evidence connecting these mechanisms to depression.
Inflammation and Family Routines
Substantial research points to intimate connections between individuals’ psychological experiences and aspects of the immune system (Cohen and Herbert 1996; Miller et al. 2011; Segerstrom and Miller 2004). Thus, consistent with a psychoneuroimmunological approach, one biological process implicated in the etiology of depression that may be affected by family routines is inflammation. Briefly, when the body’s inflammatory response is acutely activated (such as by infection or injury), proinflammatory cytokines, such as interleukin 1 (IL-1), interleukin 6 (IL-6), and tumor necrosis factor-alpha (TNF-α) are released and help coordinate responses of immune cells to repair tissue damage or destroy the infection (Kiecolt-Glaser and Glaser 2002; Kiecolt-Glaser et al. 2002). While these acute responses are necessary in the short term to protect the body, they can lead to chronic low-grade inflammation if sustained over a long period of time. Low-grade inflammation, in turn, is believed to contribute to a variety of negative physical and mental health outcomes (Fan et al. 2007; Ridker et al. 2000; Sesso et al. 2007).
By promoting greater predictability and stability, family routines may affect youth inflammatory processes. Indeed, predictability has been identified as a key dimension of experiences that moderates stress responding, such that more predictable experiences evoke lower physiological responses (Sapolsky 1994). In addition, greater structural regularity may foster cohesion and facilitate a less frenzied environment that results in fewer experiences of acute stress (Jensen et al. 1983). In line with these possibilities, greater family chaos has been shown to interact with lower socioeconomic status to predict higher levels of low-grade inflammation in adolescents (Schreier et al. 2014). In contrast, greater utilization of routines within families of children with asthma has been found to predict decreases in mitogen-stimulated production of the asthma-relevant cytokine interleukin 13 over an 18-month period (Schreier and Chen 2010). The extent to which daily family routines may be linked to cytokines associated with depression in a medically healthy population remains unclear, however.
Inflammation as Pathway to Youth Depression
Several converging findings suggest that inflammation and depression are closely linked. First, individuals with depression who are otherwise medically healthy have been found to have elevated levels of proinflammatory cytokines and acute-phase proteins (Dowlati et al. 2010; Ford and Erlinger 2004; Gimeno et al. 2008; Herbert and Cohen 1993; Howren et al. 2009; Liu et al. 2012; Maes et al. 1995; Suarez et al. 2003). In particular, individuals with depression have higher levels of IL-1, IL-6, TNF-α, and C-reactive protein (CRP). Second, rates of depression are disproportionately elevated for individuals with inflammatory diseases (Bruce 2008). For example, depression is recognized as frequently comorbid with cardiovascular disease (McConnell et al. 2005) and children with asthma have a two-fold higher prevalence of depressive/anxiety symptoms compared to children without asthma (Katon et al. 2007). Third, stimulation of the inflammatory response, such as by injecting healthy individuals with a bacterial endotoxin or administering cytokine-therapy for the treatment of cancers and certain infections, induces low mood and other depressive symptoms (Eisenberger et al. 2010; Raison et al. 2006). Together, these results are consistent with the theory that proinflammatory processes may not only result from—but may actually contribute to—the development of depression (Cicchetti et al. 1999; Felger and Lotrich 2013; Raison and Miller 2011). Consequently, by affecting youths’ inflammatory profiles, disruptions in family routines may increase risk for depression as well.
Emotion Regulation and Family Routines
Impairments in family routines may also confer risk for depression by affecting psychological processes, such as emotion regulation abilities. As defined by Thompson (2013), emotion regulation encompasses “the extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, especially their intensive and temporal features, to accomplish one’s goals” (pp. 27–28). The developmental theory of emotion regulation posits that one’s utilization of these processes grows out of consistent family behaviors early in life (Fox and Calkins 2003). Thus, it is possible that family routines may exert a stabilizing force for youths that facilitates better emotion regulation abilities even into adolescence.
Here, parent-child contact is believed to be the initial method of affective regulation for infants (Field 1996; Fox and Calkins 2003; Gross and Thompson 2006). Through sensitive, predictable responding by parents, infants are thought to begin the process of developing a repertoire of emotion regulation strategies, solidifying over time to engender better coping as children grow older (Calkins 1994). As youths become more independent in late childhood and adolescence, the family context continues to provide important models, behaviors, and reinforcements for emotion regulation skills and expectations (Morris et al. 2007; Valentiner and Holahan 1994).
One such source of continued family influence may be family routines. In families characterized by stable patterns of interpersonal routines, youth may have clearer expectations for their own behavior and for the roles, dependability, and support of other family members, facilitating self-regulation. Indeed, routinized behavior has been associated with better self-control in samples of both Caucasian and African American adolescents (Brody and Flor 1997; Fiese and Kline 1993; Jensen et al. 1983). By extension, it is possible that the regulation of emotions may be similarly associated with family routines.
Emotion Regulation as Pathway to Youth Depression
Perhaps not surprisingly, the selection and utilization of emotion regulation strategies is one prominent mechanism robustly linked with depression (Berking et al. 2008). In adults, individuals with current, as well as remitted, depression show a range of specific emotion regulation deficits, including a lack of inhibition of negative material, less use of reappraisal of situations, greater rumination, and greater use of emotional suppression (Joormann and Gotlib 2010). Impairments are also found with regard to depression in youths (Cole et al. 2008). For example, less inhibition of negative stimuli and greater reliance on emotional suppression have been demonstrated in samples of adolescents who are depressed (Betts et al. 2010). Additionally, Silk et al. (2003) found that depressive symptoms were correlated with emotion regulation strategies that were less effective at reducing negative affect (such as rumination and denial) in the daily lives of adolescents, as well as with greater emotional intensity and lability. For these reasons, emotion regulation is believed to be a key risk factor for the development of depression in youths, such that an inability to reduce sad affect or distress in appropriate ways presages the development of the disorder and may be seen as an important diathesis (Kovacs et al. 2008).
The Present Study
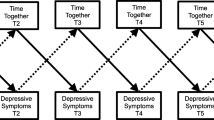
The present work sought to test the role of family routines in the intergenerational transmission of depressive symptoms via effects on emotion regulation processes and a biomarker of inflammation. As displayed in a schematic model of our hypotheses in Fig. 1, we predicted that parents who were experiencing higher levels of depressive symptoms would be less able to provide a predictable family environment for their children, which would be reflected in fewer family routines. In turn, we hypothesized that, for youths, fewer family routines would be related to higher levels of the proinflammatory cytokine IL-6 in circulation and to poorer emotion regulation abilities in youth—two markers related to key components of risk that we anticipated would be associated with youth depressive symptoms. Finally, we predicted that fewer family routines would be related to higher levels of depressive symptoms in youths, both directly and indirectly through IL-6 and emotion regulation abilities.
Method
Adolescent children (ages 13–16) and their parents were recruited through advertisements in local media into a larger study on cardiovascular functioning and family characteristics. As per our recruitment strategy, interested, eligible families responded to our advertisements. If there were multiple children in a family who were eligible to participate, the families decided amongst themselves which youth participated. All participants were required to be free of chronic and acute illness and to be fluent in English. Two-hundred-sixty-one dyads composed of one adolescent and one parent from each family participated. Seventy-six percent of parents were mothers and 53 % of children were female. Youths were on average 14.53 years old (SD = 1.07) and parents were on average 45.83 years old (SD = 5.50). Forty-nine percent of children identified as being of European descent, 36 % identified as being of Asian descent, 5 % identified as being of Latin American descent, 5 % identified as being of African descent, and 5 % identified as “other.” Average family income was in the $50,000–74,999 Canadian dollars range and parents had on average some college education. Seventy-one percent of parents were married, 18 % were divorced, and 11 % were single.
Procedure
As part of a laboratory visit, parents and youths provided written consent and assent before independently completing a series of questionnaires, described below. In addition, peripheral blood was drawn from youths. Covariates potentially related to independent or dependent variables, including age, gender, ethnicity, and waist circumference, were also assessed.
Measures
Depressive Symptoms
Parents and youths independently completed the Center for Epidemiological Studies Depression Scale Short Form (CESD; Bjorgvinsson et al. 2013). This widely-used self-report depression screen probes for the frequency of ten depressive symptoms over the course the previous week and is appropriate for use with both adolescents and adults (Bradley et al. 2010; Mojtabai and Olfson 1999). Its reliability and validity have been established in clinical as well as community samples, showing convergence with other self-report measures of depression and with clinical diagnoses of major depressive disorder (Anderson et al. 1994; Bjorgvinsson et al. 2013). Higher scores on this measure indicate greater depressive symptomatology (α = 0.81 for parents; α = 0.72 for youths, current sample).
Family Routines
Parents and youths also independently completed the Family Routines Inventory (Jensen et al. 1983), a 20-item measure probing for how regularly family members engage in specific behavioral routines in any given week. Participants were asked to rate how much various behaviors are a routine in their family, such as “Children do the same things every morning as soon as they wake up” or “Family has certain ‘family time’ each week when they do things together at home.” Responses follow a 4-point scale from almost never to always with specific frequencies provided as guides (for example, 3–5 days a week or most weekdays, depending on whether the item is appropriate across the week or for weekdays only). This scale has been shown to have good test-retest reliability and validity (Jensen et al. 1983) and to converge with other measures of child routines (Sytsma et al. 2001). Higher scores on this inventory indicate family environments characterized by greater regularity of family routines (α = 0.85 for parents; α = 0.79 for youths, current sample). In the present study, youth and parent scores were significantly correlated (r = 0.33, p < 0.001); consequently, reports were standardized and then averaged to create a single, more reliable indicator of family routines. This approach of combining parent and youth reports creates a more reliable indicator of behaviors as they actually occur at home (Epstein 1979), such that each respondent can supplement the limits to the recall and responses of the other regarding a shared context. In addition, it reflects the importance of considering the family as a unit (rather than only the parent’s or youth’s appraisal).
Youth Emotion Regulation
Parents reported on their child’s perceived emotion regulation abilities by completing a shortened version of the Emotion Regulation Checklist (Shields and Cicchetti 1997). They rated six statements on a 4-point scale to indicate the extent to which emotion regulation abilities were characteristic of their child, including “Is able to delay gratification” and “Can recover quickly from things that upset or distress him/her.” Higher scores on this measure reflect more adaptive emotion regulation skills (α = 0.75, current sample).
Inflammatory Biomarker
Peripheral blood was drawn from youths using antecubital venipucture into serum separator (SST) tubes. Serum was harvested by centrifugation at 1200 g for 10 min and was then frozen at −30 °C until assays were performed. Circulating levels of interleukin 6 (IL-6) were assessed in the lab using high sensitivity ELISA kits (R&D Systems, Minneapolis, MN). This system has a lower detection threshold of 0.07 pg/ mL. Intra- and interassay coefficients of variation were less than 10 %. This marker was selected because elevations in IL-6 (and other pro-inflammatory cytokines) are believed to play a role in the pathogenesis of depression (Raison et al. 2006) and have been shown to be elevated in individuals with major depressive disorder (Dowlati et al. 2010; Liu et al. 2012). IL-6 values were log transformed prior to analysis to normalize the distribution.
Covariates
Demographic characteristics of youth age, gender, and ethnicity were assessed and retained as covariates. Ethnicity was represented using a set of dummy codes to create contrasts between being of European descent, Asian descent, or other descent. Youth waist circumference was additionally included as a covariate for analyses with IL-6 to control for the potential contribution of adiposity to inflammatory processes (i.e., to be sure that obesity was not accounting for potential links between IL-6 and youth depressive symptoms). As a measure of adiposity, waist circumference has been shown to be a better predictor of chronic inflammation than body mass index (Festa et al. 2001; Hermsdorff et al. 2010).
Statistical Plan
Descriptive statistics and zero-order correlations between study variables were computed. Following this, path analyses were conducted to simultaneously test direct and indirect pathways linking the constructs of interest. We aimed to (a) test a scenario involving the role of routines as a link between parental depression and child depression, while (b) simultaneously testing the mechanisms through which routines might confer risk, both directly and indirectly through associations with emotion regulation and IL-6 production. Path analyses were conducted using the Mplus software (version 6.12, Muthén & Muthén 2007) and used maximum likelihood estimation with robust standard errors. Given that only 3 % missing data was observed, imputation was unnecessary. Model fit was evaluated using several statistics: overall model fit was assessed by examining the chi-square test of fit, in which a nonsignificant value indicates acceptable fit, the Comparative Fit Index (Bentler 1990), in which a value above 0.90 is considered acceptable (Bentler and Bonett 1980), and the root-mean-square error of approximation (RMSEA), for which a value less than 0.08 is considered indicative of a reasonable fit (Browne and Cudeck 1992). Comparisons between nested models were evaluated using the chi-square test of difference, in which a nonsignificant value indicates that both models are of equivalent fit (and thus the more parsimonious model should be used), while a significant value indicates the nested model is a worse fit for the data (Schermelleh-Engel and Moosbrugger 2003). Although we hypothesized specific associations between our variables (as displayed in the schematic), we began by testing a full model in which all paths were specified and then compared this to models in which paths were increasingly eliminated based on their statistical significance, stopping once the fit of the nested model was worse than the one prior. This approach allows us to determine whether the best-fitting model for our data is or is not consistent with our hypothesized model. Specific parameters of path analyses are described below and standardized coefficients (betas) are presented in all path analysis results.
Results
Descriptive statistics and intercorrelations for study variables are presented in Tables 1 and 2. There were several significant correlations between demographic covariates and study variables. Specifically, families with older children endorsed fewer routines, as did families of European descent. In contrast, families of Asian descent endorsed more routines. IL-6 levels were negatively associated with child age, but positively associated with waist circumference. Boys and youths of European descent reported lower levels of depressive symptoms.
Next, path analyses were conducted. Parent and youth depressive symptoms, routines, emotion regulation, and IL-6 variables were included in the path analyses. Across all models, each of these variables was regressed onto covariates of age, gender, and dummy codes representing being of European descent, Asian descent, or neither European nor Asian descent. IL-6 was additionally regressed onto waist circumference. The direct paths specified in the full model (Model A) were links from parental depressive symptoms to family routines, emotion regulation, IL-6, and youth depressive symptoms, from family routines to emotion regulation, IL-6, and youth depressive symptoms, from emotion regulation to IL-6 and youth depressive symptoms, and from IL-6 to youth depressive symptoms. These pathways were specified based on previous research examining connections between aspects of family life and youth psychobiological functioning, as reviewed above. In addition to the significance of direct effects, the path analysis results also indicated significance levels of each possible indirect effect.
The standardized path coefficients for the full model are presented in Fig. 1. For clarity, contributions of demographic covariates are not presented. Overall, Model A had acceptable fit, where Χ 2[4, N = 260] = 6.47, ns; CFI = 0.976, and RMSEA = 0.049. The simultaneous estimation of direct effects was largely consistent with the theoretical model, such that there was a significant direct path from parental depressive symptoms to family routines (β = −0.20, 95 % CI [−0.30, −0.10]), p < 0.01, and to emotion regulation abilities (β = −0.19, 95 % CI [−0.31, −0.06], p < 0.01). Significant direct paths also existed to child depressive symptoms from family routines (β = −0.20, 95 % CI [−0.33, −0.07], p < 0.01), emotion regulation abilities (β = −0.17, 95 % CI [−0.29, −0.04], p < 0.01), and IL-6 (β = 0.14, 95 % CI [0.02, 0.25], p < 0.05). Direct paths between parental depressive symptoms and child depressive symptoms (β = −0.11, 95 % CI [−0.02, 0.23], p < 0.10), family routines and emotion regulation abilities (β = 0.11, 95 % CI [−0.02, 0.25], p < 0.10), and family routines and IL-6 levels (β = −0.12, 95 % CI [−0.24, 0.01], p < 0.10) were marginally significant. The paths from parental depressive symptoms to youth IL-6 and from emotion regulation to IL-6 were nonsignificant (β = 0.04, 95 % CI [−0.10, 0.17], ns and β = −0.05, 95 % CI [−0.20, 0.09], ns, respectively).
Tests of indirect effects are presented in Table 3. These reveal a significant indirect pathway from parent depressive symptoms to youth depressive symptoms through family routines (β = 0.04, 95 % CI [0.00, 0.08], p < 0.05). In addition, there were marginally significant indirect pathways from parental depressive symptoms to youth depressive symptoms through emotion regulation abilities (β = 0.03, 95 % CI [−0.01, 0.07], p < 0.10) and from parental depressive symptoms to youth IL-6 levels through family routines (β = 0.02, 95 % CI [0.00, 0.04], p < 0.10).
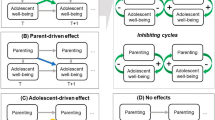
To probe for the best fitting model, we next compared Model A to a trimmed model that retained pathways originally shown to be significant or marginally significant (Model B). Given our focus on the hypothesized role of family routines in conferring aspects of risk, we opted to retain marginally significant pathways as well as significant pathways in order to further probe connections between family routines and youth emotion regulation and between routines and youth IL-6 levels, which were marginally significant in the first model. (We also tested a model in which only significant paths were retained, described below as Model C.) Overall, Model B had acceptable fit as well, where Χ 2[6, N = 260] = 6.61, ns; CFI = 0.993, and RMSEA = 0.021. An examination of the chi-square test of difference suggested that this trimmed, nested model (Model B) was equivalent in fit to the Model A (Χ 2 diff [2, N = 260] = 0.235, ns), and thus superior. This determination is further supported by comparing the values of the CFI and RMSEA across the models, as well.
As displayed in Fig. 2, direct paths from parental depressive symptoms to family routines (β = −0.20, 95 % CI [−0.30, −0.10], p < 0.01) and to emotion regulation abilities (β = −0.18, 95%CI [−0.31, −0.06], p < 0.01) were significant. As before, direct paths to child depressive symptoms from family routines (β = −0.20, 95 % CI [−0.33, −0.07], p < 0.01), emotion regulation abilities (β = −0.17, 95 % CI [−0.29, −0.04], p < 0.01), and IL-6 (β = 0.14, 95 % CI [0.02, 0.26], p < 0.05) were also significant. In contrast to Model A, the path from family routines to IL-6 was statistically significant in Model B (β = −0.13, 95 % CI [−0.26, −0.01], p < 0.05). Direct paths between parental depressive symptoms and child depressive symptoms (β = −0.11, 95 % CI [−0.02, 0.23], p < 0.10) and between family routines and emotion regulation abilities (β = 0.11, 95 % CI [−0.02, 0.24], p < 0.10) were marginally significant.
Similar to Model A, tests of indirect effects revealed a significant indirect path from parental depressive symptoms to youth depressive symptoms through family routines (β = 0.04, 95 % CI [0.00, 0.08], p < 0.05). There were also marginally significant indirect effects of parental depressive symptoms on youth depressive symptoms through emotion regulation abilities (β = 0.03, 95 % CI [−0.01, 0.07], p < 0.10) and of parental depressive symptoms on youth IL-6 levels through family routines (β = 0.02, 95 % CI [0.01, 0.05], p < 0.10).
We next compared the trimmed model retaining both marginal and significant paths (Model B) to a model in which only the significant paths were retained from the full model (Model C). Here, Χ 2[9, N = 260] = 16.75, n.s.; CFI = 0.924, and RMSEA = 0.058, indicating adequate fit. A comparison of this model to the prior model (Model B) using the chi-square test of difference indicated that the model retaining both marginal and significant paths (Model B) was superior in fit to the model retaining significant paths only (Model C) (Χ 2 diff [3, N = 260] = 10.045, p < 0.05). Consequently, Model B (retaining both marginal and significant paths) was the best fitting model for our data and we did not test any further nested models.
For Model C, all specified paths were significant, such that there were significant paths from parental depressive symptoms to family routines (β = −0.20, 95 % CI [−0.30, −0.10], p < 0.01) and to emotion regulation abilities (β = −0.21, 95 % CI [−0.34, −0.08], p < 0.01). Paths from family routines, emotion regulation, and IL-6 levels to child depressive symptoms were also significant (β = −0.22, 95 % CI [−0.36, −0.09], p < 0.01; β = −0.19, 95 % CI [−0.31, −0.06], p < 0.01; and β = 0.14, 95 % CI [0.02, 0.27], p < 0.05, respectively).
Tests of indirect effects revealed that there were significant indirect paths from parent depressive symptoms to child depressive symptoms through both family routines and emotion regulation abilities, (β = 0.04, p < 0.05, 95 % CI [0.00, 0.08], and β = 0.04, p < 0.05, 95 % CI [0.00, 0.08], respectively).
Discussion
As researchers and clinicians seek to understand and thwart the intergenerational transmission of depression between parents and children, they increasingly turn to modifiable characteristics of the family environment that may confer risk (Connell and Dishion 2008; Valdez et al. 2010). While previous work has tended to focus on the quality of parenting characteristics, such as parental warmth or harshness, the current work sought to test a model in which structural aspects such as routines within families may contribute to key immunologic and affective processes. In keeping with a biopsychosocial conceptualization of the intergenerational transmission of depression (Goodman and Gotlib 1999; Raison et al. 2006), the results of the present study suggest that the utilization of family routines may play a role in multiple risk processes, consistent with our hypothesized model. Specifically, we found that, in the best fitting model of risk, family routines were significantly associated with both parent- and youth-depressive symptoms, youths’ levels of a biomarker of low-grade inflammation, IL-6, and had a marginally significant association with youths’ emotion regulation abilities. Furthermore, our model revealed that a statistically significant portion of the observed link between parent- and youth- depressive symptoms (22 %) was accounted for by fewer family routines.
That parental depressive symptoms were related to fewer family routines is consistent with prior work documenting depression-related impairments in other aspects of caregiving, such as more intrusive interactions and greater hostility toward children (Ge et al. 1994; Lovejoy et al. 2000). As such, this work extends an understanding of the taxonomy of caregiving deficits that may exist when a parent is depressed. Multiple different depressive symptoms may contribute to this particular impairment. For example, parents may find it more difficult to access the energy for engaging in consistent interactions with their children due to motivational declines or sleep disturbance (Goyal et al. 2007). Even if attempted, those interactions may be less reinforcing, as greater anhedonia may result in parents deriving less satisfaction or pleasure from spending time regularly with their child (Lovejoy et al. 2000; Pizzagalli 2014). It is also possible that if interactions with a depressed parent are more aversive, youths, too, may be less willing to participate in family routines.
In turn, families with fewer routines have youths with riskier phenotypes. In the current study, fewer family routines was associated with higher IL-6 levels in youths and showed a trend-level association with worse emotion regulation, in line with the proposal that less predictable family behaviors may undermine structure and regularity and relate to depression-relevant affective and immunologic processes (Abramson et al. 1978; Boyce et al. 1983).
That IL-6 was significantly related to youth depressive symptoms echoes the findings that individuals with depression show elevations in this biomarker, reaffirming links between psychopathology and inflammation even in adolescence (Gabbay et al. 2009; Miller and Cole 2012). Although there was not evidence that IL-6 accounted for the association between family routines and youth depressive symptoms (contrary to our predictions), there was a marginally significant indirect effect of family routines accounting for part of the link between parental depressive symptoms and youth IL-6. This finding is consistent with previous work attesting to associations between impairments in caregiving and youth inflammation (Miller and Chen 2010; Repetti et al. 2011). Indeed, given that inflammation is implicated not only in depressive disorders but also in a variety of physical health disorders, such as heart disease and certain cancers (Heikkilä et al. 2008; Ridker et al. 2000), this pathway from parental depression and family routines to youth inflammation may have important implications for offspring’s health in the future if sustained over the long term. For example, previous work has shown that children raised in abusive or dysfunctional family environments show elevations in forms of cancers, chronic lung disease, skeletal fracture, ischemic heart disease, and liver disease (Felitti et al. 1998). It is possible that the absence of family routines, if it encourages repeated activation of the inflammatory processes that give rise to higher IL-6, may over time impact both physical and mental health.
With regard to emotion regulation, there was a significant pathway from parental depressive symptoms to youth emotion regulation and a marginally significant pathway from family routines to emotion regulation abilities, suggesting that youths exposed to parental symptomatology or who have more chaotic home environments may have less support for learning adaptive coping strategies (Repetti et al. 2002), resulting in weaker development of emotion regulation skills and more emotional lability that confer risk for depression (Morris et al. 2007; Thompson et al. 2012). There was also a marginally significant indirect effect in which emotion regulation abilities accounted for part of association between youth depressive symptoms and parental depressive symptoms, highlighting the importance of affective processes for intergenerational transmission.
These pathways through family routines, emotion regulation, and IL-6 may represent broad risk for a range of mental and physical health problems, but they also show particular connections to youth depression. Here, we found that not only were there direct effects between family routines and youth depressive symptoms, there was also a significant indirect effect in which parental depressive symptoms related to youth depressive symptoms through family routines. In this way, routines appear to be one mechanism that confers risk for the intergenerational transmission of depressive symptoms. Although the size of this effect is small, it may nonetheless represent an important risk factor (Prentice and Miller 1992). Indeed, even small changes in depressive symptoms or subsyndromal depression may result in notable impairment for individuals (Rapaport and Judd 1998). Furthermore, given that adolescence represents a time of increasing vulnerability for the onset of major depressive disorder (e.g., Burke et al. 1991), it is possible that family factors that contribute to risk during this period will have a more substantial impact than at other developmental periods. However, further work is needed to test this possibility directly.
There are several limitations to acknowledge in the present work. First, the study was cross-sectional in nature, making it impossible to determine directionality or causality. For example, it is possible that higher youth depressive symptoms may lead to fewer routines or may take a toll on parental mental health, rather than the reverse. Future longitudinal work will be important for determining the time course and direction of these pathways. Second, parent and youth depressive symptoms were assessed at the symptom-level using short self-report inventories, rather than clinician-administered measures or more comprehensive, multidimensional assessments. However, the CES-D has been shown to converge with clinician diagnoses and is commonly used in clinical settings, including primary care (Bjorgvinsson et al. 2013; Fischer et al. 2003). Thus, although it is brief, the measure represents an important real-world tool for the diagnosis and treatment of depressive symptoms. Moreover, a dimensional (vs. categorical) approach to depression acknowledges the substantial toll that even subthreshold depressive symptoms can take on psychosocial functioning (Rapaport and Judd 1998). Future work would also benefit from observational or daily diary assessment of other constructs such as family routines or emotion regulation, as well as youth reports of emotion regulation.
There are also limitations regarding the study sample. For example, the current study was conducted in a city in which the majority of the citizens are of European or Asian descent, which was reflected in the low numbers of participants of Latin American or African descent, limiting generalizability. Additionally, the sample was drawn from the community and required that participants not take medication for chronic health issues. Thus, no participants included in the study were on long-term psychotropic medication, which likely contributed to the generally low levels of depressive symptoms observed in parents and youths. However, if anything, restricted range should attenuate the magnitude of associations (Wiberg and Sundström 2009), underestimating the contribution of family routines to these pathways. Rather, that these associations emerge in normative family environments suggest that they may represent a persistent source of influence on youths across the spectrum of functioning.
The current research also raises several important issues deserving of future study. Examinations of interventions aimed at cultivating family routines will be particularly fruitful for determining causal pathways and for testing additional implications. For example, although the focus of the current project was on how family routines may affect youths, additional research should consider how the implementation of family routines may impact parents with depression. Might consistently engaging with their children around dinners or homework serve as a form of behavioral activation that lessens depressive symptomatology in parents? Or might it represent an additional burden for parents that saps already limited energetic resources? Longitudinal work will be especially important for clarifying these potential effects and for examining other parent and child characteristics that may contribute to the generation or maintenance of family routines, including assessments of family quality.
Another interesting topic for future work would be to examine how systems outside of the home may influence family routines and youth mental health. For example, certain religious communities have regular patterns of worship that may add consistency to weekly family behaviors, while schools can differ in whether class schedules are consistent or variable across days of the week. It would be interesting to see whether such community-level structures might relate to youth mental health as well or how other types of regularly-occurring family behaviors would relate to these outcomes. With regards to this last point, the current work was guided by the conceptualization of family routines provided by Jensen et al. (1983). However, other types of behaviors, such as family prayer, seasonal vacations, or holiday traditions could be considered family traditions or rituals and should be investigated in the future.
Additional work should also consider other forms of youth psychopathology. For example, future work might examine associations between parental depression, family routines, and youth ADHD or anxiety disorders. Previous work has shown that maternal depression is associated with broad risk for youth mental health disorders (Goodman et al. 2011). Thus, it is possible that impairments in family routines may confer risk for other forms of psychopathology. Relatedly, future work should also consider whether there might be forms of youth psychopathology for which the cultivation of family routines would be contraindicated. For example, would it be possible for families to become overly rigid about family interactions in ways that then undermine healthy youth functioning?
Despite these limitations and unanswered questions, the current work has several notable strengths and important implications. First, the present study examined a novel, integrative model for the transmission of depressive symptoms, reflecting the interconnections of social, biological, and psychological processes in the context of youth psychopathology. In doing so, it drew on multiple reporters and a multi-method approach, reducing the likelihood that associations amongst variables were due to shared method variance. Second, it highlighted a dimension of family life that may be particularly conducive to modification through behavioral interventions. Promoting the cultivation of family routines may be safer, more cost effective, more palatable, and more easily disseminated than other types of interventions for depression such as specialized therapies or prescriptions for psychotropic medications, which require extensive training and expertise on the part of the care provider. Lastly, by testing multiple outcome variables, such as emotion regulation and IL-6, the current study has implications for theoretical models of the biological and psychological processes involved in youth depression. In sum, the results of this study suggest that family routines may be an important factor to consider in terms of youth mental and physical health and their underlying processes.
References
Abramson, L. Y., Seligman, M. E. P., & Teasdale, J. D. (1978). Learned helplessness in humans: critique and reformulation. Journal of Abnormal Psychology, 87, 49–74.
Anderson, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10, 77–84.
Angold, A., & Costella, E. J. (1993). Depressive comorbidity in children and adolescents: empirical, theoretical, and methodological issues. American Journal of Psychiatry, 150, 1779–1791.
Benson, M. J., Buehler, C., & Gerard, J. M. (2008). Interparental hostility and early adolescent problem behavior: spillover via maternal acceptance, harshness, inconsistency, and intrusiveness. The Journal of Early Adolescence, 28, 428–454.
Bentler, P. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246.
Bentler, P., & Bonett, D. (1980). Significance tests and goodness- of-fit in analysis of covariance structures. Psychological Bulletin, 88, 588–606.
Berking, M., Orth, U., Wupperman, P., Meier, L. L., & Caspar, F. (2008). Prospective effects of emotion-regulation skills on emotional adjustment. Journal of Counseling Psychology, 55, 485–494.
Betts, J., Gullone, E., & Allen, J. S. (2010). An examination of emotion regulation, temperament, and parenting style as potential predictors of adolescent depression risk status: a correlational study. British Journal of Developmental Psychology, 27, 473–485.
Birmaher, B., Ryan, N. D., Williamson, D. E., Brent, D. A., Kaufman, J. A., Dahl, R. E., et al. (1996). Childhood and adolescent depression: a review of the past 10 years. Part I. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1427–1439.
Birmaher, B., Ryan, N. D., Williamson, D. E., Brent, D. A., & Kaufman, J. A. (2005). Childhood and adolescent depression: a review of the past 10 years, part II. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1575–1583.
Bjorgvinsson, T., Kertz, S. J., Bigda-Peyton, J. S., McCoy, K. L., & Aderka, I. M. (2013). Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment, 20, 429–436.
Boyce, W. T., Jensen, E. W., & James, S. A. (1983). The family routines inventory: theoretical origins. Social Science & Medicine, 17, 193–200.
Bradley, K. L., McGrath, P. J., Brannen, C. L., & Bagnell, A. L. (2010). Adolescents’ attitudes and opinions about depression treatment. Community Mental Health Journal, 46, 242–251.
Brody, G. H., & Flor, D. L. (1997). Maternal psychological functioning, family processes, and child adjustment in rural, single-parent, African American families. Developmental Psychology, 33, 1000–1011.
Browne, M. W., & Cudeck, R. (1992). Alternate ways of assessing model fit. Sociological Methods & Research, 21, 230–258.
Bruce, T. O. (2008). Comorbid depression in rheumatoid arthritis: pathophysiology and clinical implications. Current Psychiatry Reports, 10, 258–264.
Burke, K. C., Burke Jr., J. D., Rae, D. S., & Regier, D. A. (1991). Comparing age at onset of major depression and other psychiatric disorers by birth cohorts in five US community populations. Archives of General Psychiatry, 48, 789–795.
Calkins, S. D. (1994). Origins and outcomes of individual differences in emotion regulation. Monographs of the Society for Research in Child Development, 59, 53–72.
Cicchetti, D., Wollman, E., Vitkovic, L., & Yirmiya, R. (1999). Cytokines and depression: fortuitous or causative association? Molecular Psychiatry, 4, 1–5.
Cohen, S., & Herbert, T. (1996). Health psychology: psychological factors and physical disease from the perspective of human psychoneuroimmunology. Annual Review of Psychology, 47, 113–142.
Cole, P. M., Luby, J., & Sullivan, M. W. (2008). Emotions and the development of childhood depression: bridging the gap. Child Development Perspectives, 2, 141–148.
Connell, A. M., & Dishion, T. J. (2008). Reducing depression among at-risk early adolescents: three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology, 22, 574–585.
Costello, E. J., Pine, D. S., Hammen, C., March, J. S., Plotsky, P. M., Weissman, M. M., et al. (2002). Development and natural history of mood disorders. Biological Psychiatry, 52, 529–542.
Del Giudice, M., Ellis, B. J., & Shirtcliff, E. A. (2011). The adaptive calibration model of stress responsivity. Neuroscience & Biobehavioral Reviews, 35, 1562–1592.
Dowlati, Y., Herrmann, N., Swardfager, W., Liu, H., Sham, L., Reim, E. K., & Lanctôt, K. L. (2010). A meta-analysis of cytokines in major depression. Biological Psychiatry, 67, 446–457.
Eisenberger, N. I., Inagaki, T. K., Mashal, N. M., & Irwin, M. R. (2010). Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain, Behavior, and Immunity, 24, 558–563.
Epstein, S. (1979). The stability of behavior: on predicting most of the people much of the time. Journal of Personality and Social Psychology, 37, 1097–1126.
Fan, X., Pristach, C., Liu, E. Y., Freudenreich, O., Henderson, D. C., & Goff, D. C. (2007). Elevated serum levels of C-reactive protein are associated with more severe psychopathology in a subgroup of patients with schizophrenia. Psychiatry Research, 149, 267–271.
Felger, J. C., & Lotrich, F. E. (2013). Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience, 246, 199–229.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A., Edwards, V. J., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14, 245–258.
Festa, A., D’Agostino, R., Williams, K., Karter, A. J., Mayer-Davis, E. J., Tracy, R. P., & Haffner, S. M. (2001). The relation of body fat mass and distribution to markers of chronic inflammation. International Journal of Obesity, 25, 1407–1415.
Field, T. (1996). Attachment and separation in young children. Annual Review of Psychology, 47, 1–22.
Fiese, B. H., & Kline, C. A. (1993). Development of the family ritual questionnaire: initial reliability and validation studies. Journal of Family Psychology, 6, 290–299.
Fischer, L. R., Wei, F., Solberg, L. I., & Rush, W. A. (2003). Treatment of elderly and other adult patients for depression in primary care. Journal of the American Geriatrics Society, 51, 1554–1562.
Ford, D. E., & Erlinger, T. P. (2004). Depression and c-reactive protein in US adults. Archives of Internal Medicine, 164, 1010–1014.
Fox, N. A., & Calkins, S. D. (2003). The development of self-control of emotion: intrinsic and extrinsic influences. Motivation and Emotion, 27, 7–27.
Gabbay, V., Klein, R. G., Alonso, C. M., Babb, J. S., Nishawala, M., De Jesus, G., et al. (2009). Immune system dysregulation in adolescent major depressive disorder. Journal of Affective Disorders, 115, 177–182.
Galaif, E. R., Sussman, S., Newcomb, M., & Locke, T. F. (2007). Suicidality, depression, and alcohol use among adolescents: A review of empirical findings. International Journal of Adolescent Medicine and Health, 19, 27–35.
Gardner, F. E. M. (1989). Inconsistent parenting: is there evidence for a link with children’s conduct problems? Journal of Abnormal Child Psychology, 17, 223–233.
Ge, X., Conger, R. D., Lorenz, F. O., & Simmons, R. L. (1994). Parents’ stressful life events and adolescent depressed mood. Journal of Health and Social Behavior, 35, 28–44.
Gimeno, D., Kivimäki, M., Brunner, E. J., Elovainio, M., De Vogli, R., Steptoe, A., et al. (2008). Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychological Medicine, 39, 413.
Goodman, S. H., & Gotlib, I. (1999). Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490.
Goodman, S. H., Rouse, M. H., Connell, A. M., Broth, M. R., Hall, C. M., & Heyward, D. (2011). Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review, 14, 1–27.
Goyal, D., Gay, C. L., & Lee, K. A. (2007). Patterns of sleep disruption and depressive symptoms in new mothers. The Journal of Perinatal & Neonatal Nursing, 21, 123–129.
Gross, J. J., & Thompson, R. A. (2006). Emotion regulation: Conceptual foundations. In J. J. Gross (Ed.), Handbook of emotion regulation (Vol. 3, p. 24). New York: Guilford Press.
Halligan, S. L., Murray, L., Martins, C., & Cooper, P. J. (2007). Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. Journal of Affective Disorders, 97, 145–154.
Hammen, C., & Brennan, P. (2003). Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry, 60, 253–248.
Hammen, C., Shih, J. H., & Brennan, P. A. (2004). Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology, 72, 511–522.
Heikkilä, K., Harris, R., Lowe, G., Rumley, A., Yarnell, J., Gallacher, J., et al. (2008). Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes & Control, 20, 15–26.
Herbert, T. B., & Cohen, S. (1993). Depression and immunity: a meta-analytic review. Psychological Bulletin, 113, 472–486.
Hermsdorff, H. H. M., Zulet, M. Á., Puchau, B., & Martínez, J. A. (2010). Central adiposity rather than total adiposity measurements are specifically involved in the inflammatory status from healthy young adults. Inflammation, 34, 161–170.
Howe, G. (2003). Next-generation trials for the prevention of depression: lessons from longitudinal epidemiology and developmental psychopathology. Prevention & Treatment, 6, 1–12.
Howren, M. B., Lamkin, D. M., & Suls, J. (2009). Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosomatic Medicine, 71, 171–186.
Jensen, E. W., James, S. A., Boyce, W. T., & Hartnett, S. A. (1983). The family routines inventory: development and validation. Social Science & Medicine, 4, 201–211.
Joormann, J., & Gotlib, I. H. (2010). Emotion regulation in depression: relation to cognitive inhibition. Cognition & Emotion, 24, 281–298.
Katon, W., Lozano, P., Russo, J., McCauley, E., Richardson, L., & Bush, T. (2007). The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. Journal of Adolescent Health, 41, 455–463.
Kiecolt-Glaser, J. K., & Glaser, R. (2002). Depression and immune function: central pathways to morbidity and mortality. Journal of Psychosomatic Research, 53, 873–876.
Kiecolt-Glaser, J., McGuire, L., Robles, T. F., & Glaser, R. (2002). Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology. Annual Review of Psychology, 53, 83–107.
Kovacs, M., Joormann, J., & Gotlib, I. H. (2008). Emotion (dys) regulation and links to depressive disorders. Child Development Perspectives, 2, 149–155.
Lahey, B., van Hulle, C., Singh, A., Waldman, I., & Rathouz, P. (2011). Higher-order genetic and enviornment structure of prevalent forms of child and adolescent psychopathy. Archives of General Psychiatry, 68, 1–9.
Lewinsohn, P. M., Rohde, P., Seeley, J. R., & Fischer, S. A. (1993). Age-cohort changes in the lifetime occurrence of depression and other mental disorders. Journal of Abnormal Psychology, 102, 110–120.
Lewinsohn, P. M., Rohde, P., Seeley, J. R., Klein, D. N., & Gotlib, I. H. (2000). Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. American Journal of Psychiatry, 157, 1584–1591.
Lim, J., Wood, B. L., & Miller, B. D. (2008). Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology, 22, 264–273.
Liu, Y., Ho, R. C.-M., & Mak, A. (2012). Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. Journal of Affective Disorders, 139, 230–239.
Lovejoy, M. C., Graczyk, P. A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior: a meta-analytic review. Clinical Psychology Review, 20, 561–592.
Maes, M., Meltzer, H. Y., Bosmans, E., Bergmans, R., Vandoolaeghe, E., Ranjan, R., & Desnyder, R. (1995). Increased plasma concentrations of interleukin-6, soluable interleukin-6, soluable interleukin-2, and transferrin receptor in major depression. Journal of Affective Disorders, 34, 301–309.
McConnell, S., Jacka, F. N., Williams, L. J., Dodd, S., & Berk, M. (2005). The relationship between depression and cardiovascular disease. International Journal of Psychiatry in Clinical Practice, 9, 157–167.
McLeod, B. D., Weisz, J. R., & Wood, J. J. (2007). Examining the association between parenting and childhood depression: a meta-analysis. Clinical Psychology Review, 27, 986–1003.
Miller, G. E., & Chen, E. (2010). Harsh family climate in early life presages the emergence of a proinflammatory phenotype in adolescence. Psychological Science, 21, 848–856.
Miller, G. E., & Cole, S. W. (2012). Clustering of depression and inflammation in adolescents previously exposed to childhood adversity. Biological Psychiatry, 72, 34–40.
Miller, G. E., Chen, E., & Parker, K. J. (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137, 959–997.
Miniño, A. (2010). Mortality among teenagers aged 12–19 years: United States, 1996–2006 (No. 37) (pp. 1–8). Hyattsville: National Center for Health Statistics Data Brief.
Mojtabai, R., & Olfson, M. (1999). Major depression in community-dwelling middle-aged and older adults: prevalence and 2- and 4-year follow-up symptoms. Psychological Medicine, 34, 623–634.
Morris, A. S., Silk, J. S., Steinberg, L., Myers, S. S., & Robinson, L. R. (2007). The role of the family context in the development of emotion regulation. Social Development, 16, 361–388.
Muthén, L. K.., & Muthén, B. O. (2007). Mplus User's Guide (Sixth Edition). Los Angeles, CA: Muthén & Muthén.
Pizzagalli, D. A. (2014). Depression, stress, and anhedonia: toward a synthesis and integrated model. Annual Review of Clinical Psychology, 10, 393–423.
Prentice, D. A., & Miller, D. T. (1992). When small effects are impressive. Psychological Bulletin, 112, 160–164.
Raison, C. L., & Miller, A. H. (2011). Is depression an inflammatory disorder? Current Psychiatry Reports, 13, 467–475.
Raison, C. L., Capuron, L., & Miller, A. H. (2006). Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends in Immunology, 27, 24–31.
Rapaport, M. H., & Judd, L. L. (1998). Minor depressive disorder and subsyndromal depressive symptoms: functional impairment and response to treatment. Journal of Affective Disorders, 48, 227–232.
Repetti, R. L., Taylor, S. E., & Seeman, T. (2002). Risky families: family social environments and mental and physical health of offspring. Psychological Bulletin, 128, 330–366.
Repetti, R. L., Robles, T. F., & Reynolds, B. (2011). Allostatic processes in the family. Development and Psychopathology, 23, 921–938.
Ridker, P. M., Hennekens, C. H., Buring, J. E., & Rifai, N. (2000). C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. The New England Journal of Medicine, 342, 836–843.
Rohde, P., Lewinsohn, P. M., & Seeley, J. R. (1991). Comorbidity of unipolar depression: II. Comorbidity with other mental disorders in adolescents and adults. Journal of Abnormal Psychology, 100, 214–222.
Ross, L. T., & Hill, E. M. (2002). Childhood unpredictability, schemas for unpredictability, and risk taking. Social Behavior and Personality: An International Journal, 30, 453–474.
Sapolsky, R. M. (1994). Individual differences and the stress response. Seminars in Neuroscience, 6, 261–269.
Schermelleh-Engel, K., & Moosbrugger, H. (2003). Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods of Psychological Research, 8, 23–74.
Schreier, H., & Chen, E. (2010). Longitudinal relationships between family routines and biological profiles among youth with asthma. Health Psychology, 29, 82–90.
Schreier, H., Roy, L., Frimer, L., & Chen, E. (2014). Family chaos and adolescent inflammatory profiles: the moderating role of socioeconomic status. Psychosomatic Medicine, 76, 460–467.
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin, 130, 601–630.
Sesso, H. D., Wang, L., Buring, J. E., Ridker, P. M., & Gaziano, J. M. (2007). Comparison of interleukin-6 and C-reactive protein for the risk of developing hypertension in women. Hypertension, 49, 304–310.
Shields, A. M., & Cicchetti, D. (1997). Emotion regulation among school-age children: the development and validation of a new criterion Q-sort scale. Developmental Psychology, 33, 906–916.
Silberg, J. L., Maes, H., & Eaves, L. J. (2010). Genetic and environmental influences on the transmission of parental depression to children’s depression and conduct disturbance: an extended children of twins study. Journal of Child Psychology and Psychiatry, 51, 734–744.
Silk, J. S., Steinberg, L., & Morris, A. S. (2003). Adolescents’ emotion regulation in daily life: links to depressive symptoms and problem behavior. Child Development, 74, 1869–1880.
Singh, A. L., D’Onofrio, B. M., Slutske, W. S., Turkheimer, E., Emery, R. E., Harden, K. P., et al. (2010). Parental depression and offspring psychopathology: a children of twins study. Psychological Medicine, 41, 1385–1395.
Suarez, E., Krishan, R. R., & Lewis, J. G. (2003). The relation of severity of depressive symptoms to monocyte-associated proinflammatory cytokines and chemokines in apparently healthy men. Psychosomatic Medicine, 65, 362–368.
Sullivan, P., Neale, M., & Kendler, K. (2000). Genetic epidemiology of major depression: review and meta-analysis. American Journal of Psychiatry, 157, 1552–1562.
Sytsma, S. E., Kelley, M. L., & Wymer, J. H. (2001). Development and initial validation of the child routines inventory. Journal of Psychopathology and Behavioral Assessment, 23, 241–251.
Tetrick, L. E., & LaRocco, J. M. (1987). Understanding, prediction, and control as moderators of the relationships between perceived stress, satisfaction, and psychological well-being. Journal of Applied Psychology, 72, 538–543.
Thompson, R. A. (2013). Emotion regulation: a theme in search of definition. Monographs of the Society for Research in Child Development, 25–52.
Thompson, R. J., Mata, J., Jaeggi, S. M., Buschkuehl, M., Jonides, J., & Gotlib, I. H. (2012). The everyday emotional experience of adults with major depressive disorder: examining emotional instability, inertia, and reactivity. Journal of Abnormal Psychology, 121, 819–829.
Tiggemann, M., & Winefield, A. H. (1987). Predictability and timing of self-report in learned helplessness experiments. Personality and Social Psychology Bulletin, 13, 253–264.
Tully, E. C., Iacono, W. G., & McGue, M. (2008). An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. American Journal of Psychiatry, 165, 1148–1154.
Valdez, C. R., Mills, C. L., Barrueco, S., Leis, J., & Riley, A. W. (2010). A pilot study of a family-focused intervention for children and families affected by maternal depression. Journal of Family Therapy, 33, 3–19.
Valentiner, D. P., & Holahan, C. J. (1994). Social support, appraisals of event controllability, and coping: an integrative model. Journal of Personality and Social Psychology, 66, 1094–1102.
Weissman, M. M., Wolk, S., Goldstein, R. B., Moreau, D., Adams, P., Greenwald, S., et al. (1999). Depressed adolescents grown up. Journal of the American Medical Academy, 281, 1707–1713.
Wiberg, M., & Sundström, A. (2009). A comparison of two approaches to correction of restriction of range in correlation analysis. Practical Assessment, Research, & Evaluation, 14, 1–9.
Acknowledgments
Support for this research was provided by the Canadian Institutes of Health Research grant 97872, National Heart, Lung, and Blood Institute grant R01 HL108723, National Institute on Drug Abuse grant P30 DA027827 and National Institute of Mental Health grant F31 MH105092.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement on the Welfare of Animals
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Manczak, E.M., Williams, D. & Chen, E. The Role of Family Routines in the Intergenerational Transmission of Depressive Symptoms between Parents and their Adolescent Children. J Abnorm Child Psychol 45, 643–656 (2017). https://doi.org/10.1007/s10802-016-0187-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10802-016-0187-z