Abstract
The entire world’s focus has shifted to a digital health management system after the COVID-19 pandemic and crisis management through information systems that provide potential health support and minimize the effects of similar healthcare emergencies. Artificial intelligence (AI) can create alternative techniques such as Clinical Decision Support System (CDSS), which can aid complex scenarios such as large volumes of data, information accuracy, patient turnover, and health management regimes. CDSS uses an AI-based health information system that is helpful, fast, effective, and offers advanced techniques in emergencies and pandemics such as COVID-19. Therefore, it is essential to analyze mechanisms that can influence the degree of health care professionals (HCP) satisfaction and intention to adopt CDSS. Based on DeLone and McLean’s information system success model (D&M and ISSM), the researchers recruited 237 on-duty HCP from three major hospitals in Wuhan, China, in 2021. Data is collected through an online survey questionnaire with the consent of the hospital administration. The empirical findings show the strong influence of IS qualities (system, information, and service quality) and user satisfaction. These findings support the foundation for CDSS adoption in developing countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The flood of patients into hospitals put a strain on healthcare professionals; due to the sudden and rapid outbreak of COVID-19 in China, Wuhan Hongshan Stadium was transformed into an intelligent hospital to accommodate more patients [1, 2]. These global health crises and similar healthcare emergencies which may arise in the future have triggered a search for the healthcare industry and technologies to identify and control pandemics like COVID-19 [3]. Due to limited healthcare facilities, it was hard to locate and track the record of Covid patients [4]. The dramatic rise in the number of COVID-19 patients created grave concern about the satisfaction of HCP in the health sector [5]. Therefore, a centralized decision-based system becomes mandatory to support the safety of HCP and patients. The Clinical Decision Support System (CDSS) implementation is at an early stage, and the developing countries' adoption rate has been prolonged [6]. This study aims to identify the factors that influence CDSS adoption in the public sector hospitals.
World Wide Web (WWW) is the application that allows access to the Internet of Things (IoT). Having 16 billion devices, the IoT is expected to be the biggest category of connected devices [7]. By using IoT advancements, HCP can observe patients in real-time and more efficiently manage their own health conditions through sensor-based health information systems (HIS) [8]. In an IoT device, the DSS communicates through intranets and the internet, analyzes data to generate reports, and operates through internal networks. AI-based intelligent decision support systems (IDSS) execute specific cognitive decision-making processes, according to Burstein and Holsapple [9]. The IDSS can make pre-programmed decisions in predefined situations, like supply chain management, medical diagnostics, manufacturing operations scheduling, agriculture production planning, fraud detection, transaction delay mitigation, and web advisory systems [10]. This study is not concerned with such IDSS since it uses a sample of hospitals to leverage data, reports, and options provided by the compound DSS for daily decisions.
CDSS supports healthcare professionals (HCP) in routine tasks to enhance the quality and safety of healthcare. They are also essential to overlook inefficiencies such as expenditure on, treatment decisions, specialist referrals and diagnostic tests [11]. Previous studies have utilized a Task-Technology Fit (TTF) framework to determine the significance of a clinical decision support system (CDSS) by getting qualitative data [12]. Patni, Sharma [4] studied a machine learning (ML) based model to diagnose the CT images of the chest and cross-examination under the CDSS during the pandemic. These studies utilized a qualitative-based model; therefore, we filled a research gap by conducting our study through surveys (237 participants) and analyzing the level of HCP satisfaction and intention toward adopting CDSS.
Healthcare organizations have implemented specific information systems over the years to integrate technology to reduce medical errors, reduce costs, assist decision making, and facilitate medical solutions [13]. These technologies help HCP to work across the organization and around the globe. One of these inventions is the CDSS, which uses information systems to offer superior health services for patients and solve troublesome problems [14]. Clinical decision-making requires an increasing amount of medical information in emerging nations. Nevertheless, the structure and access to medical information remained poor, frequently leading to incorrect decisions and medical errors [15]. By using CDSS integrated systems to improve work speed and efficiency, HCP will be able to provide better care through high-quality IS [16, 17]. An effective CDSS system assures that system resources can be accessed only by authorized users, often used to ensure data security, biometric technological access, certifications, and smart cards [17].
Research on the factors influencing the adoption of CDSS is critical for practical purposes from the behavioral perspective of HCP. The results obtained through CDSS will provide decision-making support. There are specific problems and challenges relating to internal and external factors concerning the adoption of CDSS [18]. HIS initiatives have failed due to a lack of concern for healthcare workers and end-users while developing health systems [19]. Furthermore, Kabukye, Koch [20] discovered that, while CDSS can improve health care, adoption remains low because their systems do not meet the needs of HCP. This system's primary purpose is to improve patient care quality [21]. However, there is limited research on CDSS healthcare in developing countries, especially after COVID-19, to provide understanding about factors affecting the level of HCP satisfaction.
Our study makes several contributions. First, this study helps assess the influencing factors on the adoption of CDSS by HCP, and in doing so, it responds to a call for research by Aljarboa and Miah [12] to analyze factors that affect the HCP satisfaction and adoption of CDSS system. Second, it adds value to the literature by providing empirical evidence to establish an extension of the Delone & Mclean model, forming a foundation for CDSS adoption in the public sector hospitals. Finally, our research is based on the above-cited call for research which was based on a qualitative survey in two big cities in Saudi Arabia that interviewed only 54 General Practitioners (GPs); our study adds empirical evidence through data collected from 237 healthcare professionals in three public hospitals in Wuhan, China and found out their satisfaction level and CDSS adoption.
2 Literature review and hypothesis development
2.1 Clinical decision support system (CDSS)
CDSS is an electronic system to collect, store, and retrieve patient information, including the history of patients, laboratory test results, billing processes, and other related hospital procedures that can be used in various hospital departments [22]. CDSS is an electronic paperless system that covers all hospital administrative, financial, and clinical procedures [18]; therefore, it is necessary to develop and implement CDSS [23].
DSS are Information Systems (IS) domains that assist and improve organizations' decision-making processes. Numerous structured, semi-structured, and unstructured issues have specific standard criteria [24]. Thus, DSS is an interactive computer-based system designed to assist decision-makers in defining, solving, and determining problems using data and models. It is helpful in various industries, including inventory management, farming, sales optimization, healthcare, and education. CDSS enhances the performance and speed of decision-making activities, promotes learning, and is time-saving. In addition to providing focused clinical information, the CDSS system is expected to provide persistent data and relevant information that will improve human services [25]. Typically, CDSS is a collection of software created to assist healthcare professionals and patients [24].
Moreover, Artificial intelligence can be used to develop alternative techniques known as intelligent decision support systems (IDSS) [4, 26]. When combined with DSS, AI methods such as Intelligent Agents, ML (Machine Learning), Fuzzy Logic, and ANN (Artificial Neural Networks) can help solve complex, real-time problems involving massive amounts of data such as patient health reports. In contrast, CDSS managers and users will analyze such systems accurately [27]. The amount and quality of information available to HCP have an impact patient care outcomes and consistency. Therefore, hospitals have introduced CDSS to provide accurate, timely information to meet organizational needs and improve effectiveness and efficiency at an affordable cost [28, 29].
2.2 CDSS significance and intention to use (IU)
CDS systems incorporate Decision Support Systems (DSS) increasingly in the healthcare sector in developing nations. Underdeveloped countries lacked up-to-date infrastructure and well-trained technical staff to use and manage the information system. The successful implementation of CDSS in such countries depends on factors such as Government support, private investment, and technological infrastructure [30]. In developing countries, several researchers have focused on issues, including political support from the government, active management, and HCP satisfaction [31]. Moreover, researchers also studied complicated software systems and other relevant factors which influence the adoption of CDSS, such as software’s functionality, adequate supply of electricity and internet access, lack of funding, lack of government support for IT use in hospitals and lack of CDSS maintenance [32]. Iskandar, Subramaniam [33] applied ISSM to evaluate the success of implementing the ward cleaning logistics system at Taiwan medical center and identify predictive factors among HCP affecting the intention to use (IU) in the PIS (Poison Information System). Another study analyzed the quality of system influence on HCP satisfaction [34]. Therefore, it is crucial to explore CDSS significance and HCP intention to use CDSS after the Covid-19 pandemic.
2.3 Delone and McLean’s ISSM
Many existing frameworks for the evaluation of information systems (IS) exist; among the most common and valid systems for evaluating IS is DeLone and McLean's ISSM (information system success model) (D&M and ISSM) [35]. ISSM was established by D&M in 1992 and later developed in 2003 [36]. The seven dimensions of ISSM include system quality, service quality, information quality, user satisfaction, system utilization, usefulness, and net benefits [37]. In this study, we addressed the four main aspects such as IS quality: (1) System quality, (2) Information quality, (3) Quality of service, and (4) user satisfaction [38, 39]. ISSM focuses on evaluating the technological features of IS based on user views and describes the technological impact on system use and user satisfaction [40]. Isfahan and Mashhad, Iran’s teaching hospitals, have been analyzed based on ISSM, and the user’s satisfaction with HIS adoption is explored, which indicates the extent to which the user is satisfied with the success of the adoption of the HIS [28, 41].
2.4 Information system service quality (ISQ)
The system quality in literature has been primarily defined using three fundamental characteristics. Measuring success in an information system is difficult because success is not commonly defined explicitly and depends on expectations [42]. In the hospital quality system, we addressed the three main aspects of the quality system: (1) System quality, (2) Information quality, and (3) Quality of service.
2.4.1 Information quality
Information quality is defined as a system in which users believe that the information is accurate, up to date, reliable, complete, understandable, interpretable, and systematic [43, 44]. The quality of information refers to the content and structure of the outputs of the system to ensure that the data is accessible, adequately accurate, meaningful, easy to understand and read, and valuable for completing tasks and decision making [44, 45]. HCP expect CDSS to make quality information available, enabling them to do better work in the treatment, diagnosis, and care delivery [46]. HCP expectations of information output quality are significant in CDSS intention and system evaluation [47].
Improving and sustaining information quality is the fundamental approach of the ISSM. However, limited information, incomplete information, and language that is not understandable could reduce the degree of HCP satisfaction and implementation of the IS [48]. HCP may be able to reduce work time and improve work speed by using integrated systems [16]. HCP care will be indirectly improved by a high-quality IS [17]. Evaluating CDSS adoption based on the HCP satisfaction criterion is of utmost importance to HCP and if the information is incomplete and difficult to analyze may account for the dissatisfaction of HCP [28]. Therefore, based on the above arguments, we hypothesized the following:
Hypothesis 1
Information quality has a significant impact on HCP satisfaction.
2.4.2 System quality
The system's quality can be measured through its simplicity in learning and user-friendliness [49]. System quality is the user's system experience from a technological and operational perspective. Such characteristics have been deemed necessary in several contexts for healthcare IT and IS success [50, 51]. Slow response time and problems in CDSS usage can lead to severe dissatisfaction, eventually leading to a CDS system shutdown [52].
Systems based on different types of networks and programming languages seem to threaten the advancement of CDDS projects by producing multiple heterogeneous systems in an organization. Therefore, open-source tools, web-based implementation, and approved specifications will help build future applications as part of the system design requirements [53]. The CDSS framework should provide security measures to track user access and confidentiality as security challenges hinder the application and implementation of the healthcare IS [17]. The system quality ISSM approach has demonstrated an impact on consumer satisfaction in e-commerce, particularly in the COVID-19 pandemic. The e-commerce company will improve the system's quality as customer standards demand to increase user satisfaction in the future [48]. The CDSS adoption assessment based on the HCP satisfaction criteria enhances the system quality and improves medical care [28]. Based on the previous literature, our second hypothesis is given below:
Hypothesis 2
System quality has a significant impact on HCP satisfaction.
2.4.3 Service quality
Quality of service is defined as a degree to measures system characteristics such as tangibility, reliability, functionality, interactivity, and understanding [38, 54]. Quality of service is considered to meet or exceed the customer's expectations regarding the service [55]. Moreover, the systematic review identified user support as extremely important for the success of clinical IS projects[56, 57]. A study found that training and user support is one of the main contributors to the success of an IS by HCP in the early and later stages of execution [58]. The lack of satisfaction and use of the EMR by HCP is mainly and strongly due to the poor quality of service. The focus should be on improving service quality in future projects, including HCP support, power infrastructure, training, and technical support [35]. A service quality ISSM-based approach has generally affected user satisfaction in e-commerce, particularly in the COVID-19 pandemic. If the quality of the service is low, customer satisfaction will effect and disturb daily base operations [48]. Therefore, we hypothesized the following:
Hypothesis 3
Service quality has a significant positive impact on HCP satisfaction.
2.5 User satisfaction and intention to use
The acceptance or rejection by users of a system determines the success or failure of the system [59]. The successful implementation is based on the user’s satisfaction [60]. Low level of user satisfaction may reflect anger, dissatisfaction, and stress caused by system inefficiencies [61] Although high satisfaction levels can not only encourage better IS use, but also affect the quality of the working life of the users [27].
Unfortunately, HCP are worried about the purposes of IS and its consequences for their job [62]. System adoption and acceptance of HCP are now considered among the most significant obstacles to the spread of CDSS in the healthcare sector [63]. Vassilios mentioned the satisfaction of the HCP as one of the fundamental approaches for evaluating HIS success. Finally, the author concludes that the HCP satisfaction with the IS could be the most successful evaluation method [27]. These findings specify that the HCP satisfaction with CDSS adoption measurements is paramount among various success factors [27, 64]. Possibly this element is the most common method used to measure success [27, 65].
The various implemented projects that failed were often those in which end users were frustrated, or the core system functions were not adequately utilized [66]. Although most HCP generally believe that technology can help reduce the paper documentation burden and patient database availability in critical situations, they are also quickly disappointed and unhappy when an introduced system or service fails to meet their standards [67]. Consequently, many studies have proposed that user satisfaction is the principal determinant of the user adoption of CDSS [38, 68]. Thus, we proposed the following hypothesis:
Hypothesis 4
User Satisfaction has a significant impact on CDSS adoption intentions.
3 Research methodology
3.1 Participants and procedure
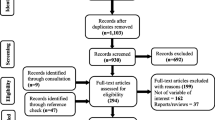
This cross-sectional study was carried out during the COVID-19 pandemic, and data were collected between 27 March 2021 and 24 May 2021. The research population consists of managers, faculty, physicians, and health care professionals HCP (including nurses, chemists, laboratory technicians, administrative support staff, and finance department) who have a comprehensive knowledge of IT and have used the CDSS/HIS/IS. The study was carried out at three public hospitals in Wuhan, Mainland China, and data was collected by filling out a standardized questionnaire about the CDSS adoption intention factors during the COVID-19 pandemic emergency. In hospitals, unrelated individuals are restricted in their mobility, so a web-based questionnaire was used. The questionnaire explained briefly that the objective of the study is to examine AI base CDSS adoption success factors. There are two major sections in the questionnaire: the first section with demographic characteristics of the respondent, including gender, age, experience, education, and position in the hospital. The second part examines CDSS usage intention and its determinants (i.e., IS qualities like information, system, service quality, HCP satisfaction). From a convenience sample of the HCP, we obtained 254 responses out of 270 distributed questionnaires. However, 237 usable responses remained for analysis after the elimination of responses with large quantities of missing data and those from the HCP that are not actual system users. Finally, an analysis with an 87% response rate was found useful. The descriptive statistics of the sample profile are given below.
3.2 Measures
A five-point Likert scale was used to capture perceptions of the success of the system attributes, reflecting system, information, and service quality. A survey designed by Alzahrani, Mahmud [69] was carried out using the D&M IS model for the successful information system (ISSM). An ISSM-based self-administered structured questionnaire was developed to collect data. The questionnaire included five dimensions: information quality, system quality, service quality, HCP satisfaction, and intention to use CDSS. The construct items are given by Appendix A.
The measurement items for the quality of information were adapted from Shaltoni, Khraim [70]. INFQ1, INFQ2, INFQ3, and INFQ4 reflect the relevance, usefulness, accuracy, and comprehensiveness of the information provided by the CDSS. System Quality (four items) was adapted from Pituch and Lee [71] and, more recently, used by Rana, Dwivedi [72] and Shaltoni, Khraim [70]. Service Quality (five items) was adapted from Ismail, Razak [73, 74]. HCP satisfaction has been measured by three adjusted items [73], which SAT1, SAT2, and SAT3 have been designed to fulfill the HCP experience, information worth, and system interactions. The CDSS intention was measured with four items adapted from [75,76,77] and [78], respectively. The questionnaire also contained various questions concerning the pandemic, based on HCP attitudes and knowledge of the CDS system, COVID-19 information, its spread, prevention, control measures, and how it may affect the CDSS, particularly in the current emergency outbreak. The HCP were asked to choose from specific options or write their own opinions. Table 1 presents the demographics of the participants, Table 2 displays the cross loadings, and Table 3 illustrates the confirmatory analysis conducted in this study.
4 Results
4.1 Data analysis
The research was performed on SmartPLS 3.2.8 [79] and IBM SPSS Statistics 22. However, SmartPLS was primarily used for data analysis because PLS-SEM has higher predictive power than SEM-dependent factors [80]. Researchers in information systems, social sciences, and business management often use this technique for their research [81]. The partial least squares (PLS) method was used to analyze the research model with SmartPLS 3.2.8 [82]. The measuring model is tested for its validity and reliability following the two-stage analytical process [69, 83]. The hypothesis is subsequently evaluated, and the structural model estimates the path coefficient [84]. To assess the significance of the path coefficients and the loadings, a bootstrapping mechanism with 5,000 re-samples was used. The PLS-SEM goal focuses on endogenous variables and aims to optimize the variance described [69, 84].
4.2 Measurement model
Reflective indicators were used to test the measurement model's reliability and validity. A composite reliability (CR) measure has been proposed as a better measure of reliability than Cronbach's alpha, since PLS does not require all indicators to be equally reliable [85], which in other software is a limitation. As shown in Table 4, most items have an outer load above 0.70 to assess the reliability of latent variables. However, some items with lower outer loads are retained because they contribute to content validity [86].
Considering that the minimum limit of 0.40 is an appropriate value for loading items [87], none of the items had to be excluded since all loadings were above 0.4. In addition, high composite reliability scores above 0.8 were seen in all the constructs. The values ranged confirming adequate reliability [85]. The Cronbach’s alpha and rho_A values and Table 5 discriminant validity were also relatively high and well above the benchmarks set in the literature.
To assess the validity of the construct, both convergent and discriminant validity [88] suggestions have been made, and 0.5 or above has been identified as an appropriate value of the Average Variance Extracted (AVE) [89]. As a result, AVE values for all constructs were larger than 0.5 and ranged from 0.502 to 0.765, confirming convergent validity and evaluating discriminant validity [88].
4.3 Structural model
The authors assessed the structural model in three stages (Solano Acosta, 2018); as a first step, each latent variable was given an R2 value. Second, the redundancy check for Q2 was determined using the Blindfolding feature, which assesses the consistency of predictive significance. A sample of 5000 bootstraps was used to make the same number of observations as the original sample for standard errors and t-values [90]. F2 values of effect size were used to check the interaction impact. Chin [91] proposed 0.67 for significant, 0.33 for moderate strong, and 0.19 for weak R-square benchmarking values. The Figure 1 displays R-square variance inside the constructs, path coefficient values, and t-values in parentheses. The three independent variables (INFQ β = 0.273, SYSQ β = 0.248, SERVQ β = 0.334) explained a 52% variance in satisfaction (β = 0.528) in turn explained 27.9% variance in intention to use.
In Table 6, INFQ had a significant positive impact on SAT (t = 4.779, p = < 0.001). SYSQ had a significant positive relationship with SAT (t = 3.705, p < 0.001). SERQ also had a significant positive effect on SAT (t = 7.243, p < 0.001). Moreover, SAT (t = 8.238, p < 0.001) had a significant positive effect on the intention to use.
4.4 Model strength and quality
F2 values of 0.02, 0.15, and 0.35 suggest that the interaction term on the criterion variable is low, medium, or high. A Q2 value greater than zero means that the model has ethical predictive relevance [92].
The values for F2 were calculated from the results of the measuring model, while the Q2 values were calculated via the Blindfolding function under the SmartPLS software tab. In Table 7 the relationship paths from INFQ to SAT (F2 = 0.065), SYSQ to SAT (F2 = 0.080) and SERQ to SAT (F2 = 0.130) are obvious from the statistics, since F2 values are below the minimum threshold of 0.02. With an F2 value of 0.387, which is significantly high, SAT and IU were the strongest interactions. All relationships met the minimum literature criterion of having Q2 values above zero. Table 8 displays the t-values and p-values showing that INFQ, SYSQ and SERVQ indicate a significantly positive relationship with satisfaction (t = 3.589, p = 0.000), (t = 4.331, p = 0.000) and (t = 5.019, p = 0.000). The relationships with t-values well above 1.96 thresholds and p-values of less than 0.05 have proven important. According to the thumb rule of t-value for a two-tailed test, t = 1.96, all hypotheses are supported.
5 Discussion
The purpose of this study was to evaluate the role of HCP satisfaction in determining the relationship between IS qualities and intention to use CDSS. A better-quality system creates an environment of CDSS successful implementation; HCP level of satisfaction, and through this mechanism, adoption of CDSS is facilitated. The continuity of safety and patient care in organizations that rely heavily on computerized health care systems requires zero downtime and business continuity protocols [93]. Previous studies affirm that user satisfaction in measuring CDSS adoption is significant [59, 64]. The results of the studies have shown that satisfaction is a valuable criterion for determining the CDSS system adoption [48].
This study supports the recent findings of Aljarboa and Miah [12] work on CDSS. According to Table 6, our IS qualities highly influence HCP satisfaction with adopting CDSS. This study developed hypotheses and established a correlation between CDSS adoption, information quality, and HCP satisfaction, as represented by H1. Previous researchers have supported these conclusions [35]. Wibowo [94] also found that information quality has a dominant influence on HCP satisfaction because information quality relates to the delivery of information about the stages that must be passed by the HCP. An information system of high quality will contribute indirectly to HCP quality of care [17].
The second hypothesis concerns the effect of system quality on HCP satisfaction. Based on these findings, system quality positively affects the HCP satisfaction. The outcome of our hypothesis is thus consistent with previous research [95, 96]. An effective CDSS assures that system resources can be accessed only by approved users; thus, the findings support that system quality attributes are crucial for user satisfaction [97] and to intention to adopt CDSS [52].
Results also support the third hypothesis that service quality significantly influences HCP satisfaction. Our findings are in line with previous studies [98, 99] that contradict earlier research in the healthcare sector, which has advocated for a greater focus on service quality to improve HCP satisfaction and, as a result, achieve system success [35, 98]. The dissatisfaction with this area, emphasized in multiple researches, has been identified as a barrier to using electronic health records (EHR) and the primary cause for HCP abandoning them [17]. As a broad technological characteristic of the HIS/CDSS, timely high-speed system access has been identified as a significant efficiency aspect [100]. HCP adoption of the system and its successful deployment are less likely when the system response time is slow [101]. The IS quality dimensions and the ISSM approach has impacted user satisfaction and information system in e-commerce, particularly in the current COVID-19 pandemic [48].
The fourth hypothesis in this study is the effect of an HCP satisfaction on intention to use, which significantly influence the CDSS adoption. Technological change needs to address HCP satisfaction [102, 103]; as a result, what motivates people to use the technical system, technology varies based on their expectations needs, and values [104]. As a result, hospital administration should give enough training to raise user awareness and understanding of the relevance of CDSS and its significant implications, as well as implement and deploy CDSS. According to Lee, Ramayah [14], the more uneasy people are about the technology, the less likely they are to implement it. Consequently, the hypothesis of our study shows factors influencing the intentions to adopt CDSS. The findings of this research would be valued for the effective implementation of CDSS in public sector hospitals. Hence, IT plans, and roadmaps are required by government and hospital administration to ensure that the deployment of integrated CDSS goes smoothly. To achieve positive benefits from CDSS, it is important to communicate this roadmap to all stakeholders. If HCP satisfaction, government policies and infrastructure that meet all IS criteria for CDSS, should all contribute to a successful CDSS implementation. Finally, HCP participation in all phases of the CDSS development cycle is critical for delivering a high-quality CDSS.
6 Practical implication
Apart from a load of HCP activities, the knowledge codification required by CDSS allows medical and non-medical personnel access to a broader level of knowledge in organizations. [102, 105]. Furthermore, HCP are concerned about a loss of privacy, increased workload and costs, medical liability, and inadequate usability, particularly regarding the medical record system. [102]. This could result in satisfaction or dissatisfaction among healthcare workers, affecting their intentions to use the system. In this regard, the government should establish policies that contain a unique set of rules and plans to pursue the goal of CDSS adoption, which will result in hospitals implementing CDSS [30, 106].
7 Conclusion
This study aimed to investigate the change in HCP satisfactory level toward the success of CDSS in a developing country. The primary goal of this research is to determine the critical factors influencing CDSS adoption in public hospitals in the light of the D&M and ISSM framework after the COVID-19 pandemic. We have seen that a Clinical Decision Support System using AI is beneficial, fast, and reliable. The number of cases increases exponentially during pandemics such as COVID-19, making it impossible to diagnose each patient manually. As AI came into trend later, it wasn’t used efficiently in earlier pandemics, so these are very useful for areas where there are still low levels of HCP satisfaction and intention to use CDSS. As a result, we can assure that the designed system meets the needs HCP satisfaction. The results of our study indicate that all our independent variables positively influence the success of CDSS. The findings imply that HCP satisfaction is an essential factor for the success of CDSS.
7.1 Limitations and suggestions for future research
This study has some limitations, even though it has contributed to theory and practice. It's a cross-sectional study involving just HCP, so extra attention is recommended when applying the findings to another cadre, industry, or business type. Future research could increase the generalizability of this study, which was conducted in Wuhan, the outbreak's epicenter, such as collecting samples from other regions where COVID-19 is currently in a highly infectious phase, and HCP are likely to face satisfaction, safety, and CDSS challenges.
Further study on CDSS adoption may be undertaken with the roles of management and leadership behavior on how hospital leaders' actions can affect employee behaviors in adopting the technology. Furthermore, this study is based on the D&M and ISSM frameworks. Further research should be conducted using different contexts such as the Human Organization Technology (HOT) Fit model to understand CDSS adoption better.
Data availability statement
The manuscript data has not associated, and data will be available on request.
References
Khan ZH, Siddique A, lee CW (2020) Robotics utilization for healthcare digitization in global COVID-19 Management. Int J Environ Res Public Health 17(11):3819
Zeng Z, Chen P-J, Lew AA (2020) From high-touch to high-tech: COVID-19 drives robotics adoption. Tour Geogr 22(3):724–734
Khanchi I, Ahmed E, Sharma HK (2020) Automated framework for real-time sentiment analysis. In: 5th international conference on next generation computing technologies (NGCT-2019)
Patni JC et al (2022) COVID-19 pandemic diagnosis and analysis using clinical decision support systems. Cyber intelligence and information retrieval. Springer, pp 267–277
Parr J (2020) Pneumonia in China: lack of information raises concerns among Hong Kong health workers. 2020, British Medical Journal Publishing Group
Khuram S et al (2018) Essential factors for adopting hospital information system: a case study from Pakistan, pp 1–12
Ericsson (2016) Ericsson-mobility-report
Son J, Kim Y, Zhou S (2022) Alerting patients via health information system considering trust-dependent patient adherence. Inf Technol Manage 23(4):245–269
Burstein F, Holsapple CW (2008) Handbook on decision support systems. Springer Verlag, Berlin
Power DJ (2018) A Brief History of Decision Support Systems. 2007 August 20, 2018]; Available from: http://DSSResources.COM/history/dsshistory.html
Cresswell K et al (2013) Computerised decision support systems for healthcare professionals: an interpretative review. J Innov Health Inf 20(2):115–128
Aljarboa S, Miah SJ (2022) An Integration of UTAUT and task-technology fit frameworks for assessing the acceptance of clinical decision support systems in the context of a developing country. In: Proceedings of sixth international congress on information and communication technology. Springer
Ahmadi H, Nilashi M, Ibrahim O (2015) Organizational decision to adopt hospital information system: an empirical investigation in the case of Malaysian public hospitals. Int J Med Inform 84(3):166–188
Lee HW, Ramayah T, Zakaria N (2012) External factors in hospital information system (HIS) adoption model: a case on Malaysia. J Med Syst 36(4):2129–2140
Delpierre C et al (2004) A systematic review of computer-based patient record systems and quality of care: more randomized clinical trials or a broader approach? Int J Qual Health Care 16(5):407–416
Sagiroglu O, Ozturan MJ (2006) Implementation difficulties of hospital information systems. Inf Technol J 5(5):892–899
Farzandipour M et al (2020) Technical requirements framework of hospital information systems: design and evaluation. BMC Med Inform Decis Mak 20(1):61
Masrom M, Rahimly A (2015) Overview of data security issues in hospital information systems. Pac Asia J Assoc Inf Syst 7(4):5
Teixeira L, Ferreira C, Santos BS (2012) User-centered requirements engineering in health information systems: a study in the hemophilia field. Comput Methods Progr Biomed 106(3):160–174
Kabukye JK et al (2017) User requirements for an electronic medical records system for oncology in developing countries: a case study of Uganda. In: AMIA annual symposium proceedings. American Medical Informatics Association
Vafaei A et al (2010) Views of users towards the quality of hospital information system in training hospitals
Handayani PW, Hidayanto AN, Budi I (2018) User acceptance factors of hospital information systems and related technologies: Systematic review. Inform Health Soc Care 43(4):401–426
Kelkar S (2010) Hospital information systems: a concise study. PHI Learning Pvt. Ltd
Sutton RT et al (2020) An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med 3(1):17
Kelly-Cirino CD et al (2019) Importance of diagnostics in epidemic and pandemic preparedness. BMJ Glob Health 4(Suppl 2):e001179
Bahl S et al (2021) Bioengineering technology in context of COVID-19 pandemic: potential roles and applications. J Ind Integr Manage 6(02):193–207
Aggelidis VP, Chatzoglou PD (2008) Methods for evaluating hospital information systems: a literature review. EuroMed J Bus 3(1):99–118
Saghaeiannejad-Isfahani S et al (2014) A survey on the users’ satisfaction with the hospital information systems (HISs) based on DeLone and McLean’s model in the medical-teaching hospitals in Isfahan City. Acta Inform Med 22(3):179–182
Shahzad K, Jianqiu Z, Zia MA, Shaheen A, Sardar T (2021) Essential factors for adopting hospital information system: a case study from Pakistan. Int J Comput Appl 43(1):26–37
Ahmad N, Waqas M, Zhang X (2021) Public sector employee perspective towards adoption of E-government in Pakistan: a proposed research agenda. Data Inf Manage 5(1):119–124
Sultan F et al (2014) Development of an in-house hospital information system in a hospital in Pakistan. Int J Med Inf 83(3):180–188
Lucas H (2008) Information and communications technology for future health systems in developing countries. Soc Sci Med 66(10):2122–2132
Iskandar YHP et al (2020) Predicting healthcare professionals’ intention to use poison information system in a Malaysian public hospital. Health Inf Sci Syst 8(1):6
Wei K-M et al (2017) Using an updated Delone and McLean model to assess the success of implementing the ward cleaning logistics system in a medical center. J Stat Manage Syst 20(5):965–976
Tilahun B, Fritz F (2015) Modeling antecedents of electronic medical record system implementation success in low-resource setting hospitals. BMC Med Inform Decis Mak 15(1):61
DeLone W, William HJ (1992) Determinants of success for computer usage in small firms. MIS Quart 3(1):60
Pimentel L et al (2017) Impact of health policy changes on emergency medicine in maryland stratified by socioeconomic status. West J Emerg Med 18(3):356–365
Delone WH, McLean ER (2003) The DeLone and McLean model of information systems success: a ten-year update. J Manag Inf Syst 19(4):9–30
DeLone WH, McLean ER (1992) Information systems success: The quest for the dependent variable. Inf Syst Res 3(1):60–95
Otieno GO et al (2008) Measuring effectiveness of electronic medical records systems: towards building a composite index for benchmarking hospitals. Int J Med Inform 77(10):657–669
Ebnehoseini Z et al (2019) Determining the hospital information system (HIS) success rate: development of a new instrument and case study. Open Access Maced J Med Sci 7(9):1407–1414
Van Der Meijden MJ et al (2003) Determinants of success of inpatient clinical information systems: a literature review. J Am Med Inform Assoc 10(3):235–243
Acton T et al (2009) DeLone & McLean success model as a descriptive tool in evaluating the use of a virtual learning environment
Gable GG, Sedera D, Chan T (2008) Re-conceptualizing information system success: the IS-impact measurement model. J Assoc Inf Syst 9(7):18
Torkzadeh G, Doll WJ (1999) The development of a tool for measuring the perceived impact of information technology on work. Omega 27(3):327–339
Kimiafar K et al (2014) Prioritizing factors influencing nurses’ satisfaction with hospital information systems: a fuzzy analytic hierarchy process approach. Comput Inform Nurs 32(4):174–181
Otieno OG et al (2007) Nurses’ views on the use, quality and user satisfaction with electronic medical records: questionnaire development. J Adv Nurs 60(2):209–219
Dirgantari PD et al (2020) Level of use and satisfaction of e-commerce customers in Covid-19 pandemic period: an information system success model (ISSM) approach. Indones J Sci Technol 5(2):86–95
Petter S, McLean ER (2009) A meta-analytic assessment of the DeLone and McLean IS success model: an examination of IS success at the individual level. Inf Manage 46(3):159–166
Hayrinen K, Saranto K, Nykanen P (2008) Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform 77(5):291–304
Huryk LA (2010) Factors influencing nurses’ attitudes towards healthcare information technology. J Nurs Manag 18(5):606–612
Smith D, Morris A, Janke J (2011) Nursing satisfaction and attitudes with computerized software implementation: a quasi-experimental study. Comput Inform Nurs 29(4):245–250
Tieu L et al (2015) Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Int Res 17(12):e275
Lin F, Fofanah SS, Liang D (2011) Assessing citizen adoption of e-Government initiatives in Gambia: a validation of the technology acceptance model in information systems success. Gov Inf Quart 28(2):271–279
Parasuraman A, Zeithaml VA, Berry LL (1988) Servqual: a multiple-item scale for measuring consumer perc. J Retail 64(1):12
Gruber D et al (2009) Factors influencing outcomes of clinical information systems implementation: a systematic review. Comput Inform Nurs 27(3):151–163
He J (2014) Technology adoption in Hospitals–the roles of system integration and technology support
Lee TT et al (2008) Two-stage evaluation of the impact of a nursing information system in Taiwan. Int J Med Inform 77(10):698–707
Saleem N et al (2017) Significance of user participation in a hospital information system success: insights from a case study. Health Care Manag (Frederick) 36(2):199–205
Ajami S, Mohammadi-Bertiani Z (2012) Training and its impact on hospital information system (HIS) success. J Inf Technol Softw Eng 2(112)
Brown SA et al (2002) Do I really have to? User acceptance of mandated technology. Eur J Inf Syst 11(4):283–295
Stevenson JE et al (2010) Nurses’ experience of using electronic patient records in everyday practice in acute/inpatient ward settings: A literature review. Health Inf J 16(1):63–72
Bush M et al (2009) The alignment of information systems with organizational objectives and strategies in health care. Int J Med Inform 78(7):446–456
Kaplan B, Harris-Salamone KD (2009) Health IT success and failure: recommendations from literature and an AMIA workshop. J Am Med Inform Assoc 16(3):291–299
Aggelidis VP, Chatzoglou PD (2012) Hospital information systems: Measuring end user computing satisfaction (EUCS). J Biomed Inf 45(3):566–579
Nour M (2007) Physicians’ use of and attitudes toward electronic medical record system implemented at a teaching hospital in saudi arabia. J Egypt Public Health Assoc 82(5–6):347–364
Chisolm DJ et al (2010) Clinician perceptions of an electronic medical record during the first year of implementaton in emergency services. Pediatr Emerg Care 26(2):107–110
Ives B, Olson MH, Baroudi JJ (1983) The measurement of user information satisfaction. Commun ACM 26(10):785–793
Alzahrani AI et al (2019) Modelling digital library success using the DeLone and McLean information system success model. J Librarians Inf Sci 51(2):291–306
Shaltoni AM et al (2015) Exploring students’ satisfaction with universities’ portals in developing countries: a cultural perspective. Int J Inf Learn Technol 32(2):82–93
Pituch KA, Lee Y-K (2006) The influence of system characteristics on e-learning use. Comput Educ 47(2):222–244
Rana NP et al (2015) Investigating success of an e-government initiative: validation of an integrated IS success model. Inf Syst Front 17(1):127–142
Ismail NZ et al (2012) E-learning continuance intention among higher learning institution students’ in Malaysia. Proc Soc Behav Sci 67:409–415
Chen Y-H, Chengalur-Smith IJTI, Education H (2015) Factors influencing students’ use of a library Web portal: applying course-integrated information literacy instruction as an intervention. Int Higher Educ 26:42–55
Hsu C-L, Lin JCC (2010) A study of the adoption behaviour for in-car GPS navigation systems. Int J Mob Commun 8(6):603–624
Mayeh M, Ramayah T, Popa SJJU (2014) The role of absorptive capacity in the usage of a complex information system: the case of the enterprise information system. J Univ Comput Sci 20(6):826–841
Calisir F, Gumussoy CA, Bayram A (2009) Predicting the behavioral intention to use enterprise resource planning systems. Manage Res News 32(7):597–613
Shih Y-Y, Huang S-S (2009) The actual usage of ERP systems: an extended technology acceptance perspective. J Res Pract Inf Technol 41(3):263
Ringle CM, Wende S, Becker JM (2015) SmartPLS 3. SmartPLS GmbH, Boenningstedt. J Serv Sci Manage 10(3):32–49
Sarstedt M et al (2016) Estimation issues with PLS and CBSEM: Where the bias lies! J Bus Res 69(10):3998–4010
Kline RB (2005) Principles and practice of structural equation modeling, 2nd edn. Guilford publications
Bhutta E, Kausar S, Rehman A (2019) Factors affecting the performance of market committees in Punjab, Pakistan: an empirical assessment of performance through smart pls mediation analysis. J Agric Res 57(3):189–197
Anderson JC, Gerbing DW (1988) Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull 103(3):411
Hair JF Jr et al (2014) Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur Bus Rev 26(2):106–121
Hair J et al (2017) An updated and expanded assessment of PLS-SEM in information systems research. Ind Manag Data Syst 117(3):442–458
Hair JF, Ringle CM, Sarstedt M (2014) PLS-SEM: indeed a silver bullet. J Mark Theory Pract 19(2):139–152
Hair JF et al (2014) A Primer on partial least squares structural equation modeling (PLS-SEM). SAGE Publications Inc, California, p 307
Fornell C, Larcker DF (1981) Structural equation models with unobservable variables and measurement error: algebra and statistics. J Mark Res 18(3):382–388
Van der Wee M et al (2015) Identifying and quantifying the indirect benefits of broadband networks for e-government and e-business: a bottom-up approach. Telecommun Policy 39(3–4):176–191
Hair JF, Ringle CM, Sarstedt M (2013) Partial least squares structural equation modeling: rigorous applications, better results and higher acceptance. Long Range Plan 46(1–2):1–12
Chin WW (1998) The partial least squares approach to structural equation modeling. Modern Methods Bus Res 295(2):295–336
Chin W (1998) The partial least squares approach to structural equation modeling. In: Marcoulides GA (ed) Lawrence Erlbaum Associates, Mahwah
Wager KA, Lee FW, Glaser JP (2017) Health care information systems: a practical approach for health care management. John Wiley & Sons, New Jersey
Wibowo WA (2013) Pengaruh system quality, information quality, dan service quality terhadap user satisfaction website Lion Airlines dan Sriwijaya Airlines. J Strat Pemasar 1(1)
Cheung CS et al (2013) Factors associated with adoption of the electronic health record system among primary care physicians. JMIR Med Inf 1(1):e2766
Bossen C, Jensen LG, Udsen FW (2013) Evaluation of a comprehensive EHR based on the DeLone and McLean model for IS success: approach, results, and success factors. Int J Med Inform 82(10):940–953
Ghahramani N et al (2009) User satisfaction with computerized order entry system and its effect on workplace level of stress. J Med Syst 33(3):199–205
Choi W et al (2013) Information system success model for customer relationship management system in health promotion centers. Healthc Inform Res 19(2):110–120
Susnita TAJJ (2020) Pengaruh kualitas pelayanan dan kepuasan pelanggan terhadap loyalitas pelanggan pada hotel Libra kadipaten Kabupaten Majalengka. JITK (Jurnal Ilmu Pengetahuan dan Teknologi Komputer) 3(1):73–84
Mohan J, Yaacob RRR (2004) The Malaysian Telehealth Flagship Application: a national approach to health data protection and utilisation and consumer rights. Int J Med Inf 73(3):217–227
Berg M (2001) Implementing information systems in health care organizations: myths and challenges. Int J Med Inform 64(2–3):143–156
Salahuddin L et al (2020) Safe use of hospital information systems: an evaluation model based on a sociotechnical perspective. Behav Inf Technol 39(2):188–212
Ahmed F et al (2022) Supportive leadership and post-adoption use of MOOCs: the mediating role of innovative work behavior. J Org End User Comput (JOEUC) 34(1):1–23
Waqas M, Ahmad N, Wu J (2021) Adoption of e-services and quality of life among older consumers in China. Data Inf Manage 5(1):125–130
Prasad P, Prasad AJHR (1994) The ideology of professionalism and work computerization: an institutionalist study of technological change. Hum Relat 47(12):1433–1458
Klöcker P, Bernnat R, Veit D (2014) Implementation through force or measure? How institutional pressures shape national ehealth implementation programs
Acknowledgements
This research is supported by the National Natural Science Foundation of China (Project Number 72072167 and 72071193).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology done by NA. Validation and formal analysis done by FA. Investigation, resources, and draft preparation done by NuA. Writing, review, and editing done by XY. Project administration and funding acquisition done by DS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix A: Questionnaire
Appendix A: Questionnaire
1.1 System quality (information system and service quality)
-
1.
The AI-based CDSS that I am using is user friendly.
-
2.
The work flow is improved by AI-based CDSS.
-
3.
The AI-based CDSS that I am using is easy to use.
-
4.
The AI-based CDSS responds quickly enough.
-
5.
The information that I get from AI-based CDSS is complete.
-
6.
The information that I get from AI-based CDSS is on time.
-
7.
The quality of the information that I get from AI-based CDSS is valid.
-
8.
The information from AI-based CDSS is useful for decision making.
-
9.
Service quality support provided by AI-based CDSS is sufficient.
-
10.
The AI-based CDSS has provided me with the assistance I need.
-
11.
Training on the use of AI-based CDSS is sufficient.
-
12.
There is always someone to turn to if we need help with the AI-based CDSS.
-
13.
Clinically critical decisions are supported by the AI-based CDSS.
1.2 User (HCP) satisfaction
-
14.
Using AI-based CDSS has been a pleasant experience for me.
-
15.
I am very satisfied with the information I receive through AI-based CDSS.
-
16.
AI-based CDSS has helped to provide reliable services.
-
17.
Overall, my interaction with AI-based CDSS is very satisfying.
1.3 Intention to adopt CDSS
-
18.
I intend to use AI-based CDSS to do my work.
-
19.
I will return to AI-based CDSS often.
-
20.
I intend to use AI-based CDSS frequently to get services.
-
21.
Given the opportunity, I will use AI-based CDSS.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahmad, N., Du, S., Ahmed, F. et al. Healthcare professionals satisfaction and AI-based clinical decision support system in public sector hospitals during health crises: a cross-sectional study. Inf Technol Manag (2023). https://doi.org/10.1007/s10799-023-00407-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s10799-023-00407-w