Abstract
Purpose
To analyze the effects of various obstetric and perinatal factors on the severity of retinopathy of prematurity (ROP).
Methods
Infants born at ≤ 32 weeks of gestation, with less than 1500 g gestational weight and having at least stage 1 ROP, were reviewed. Group1A included treatment-requiring ROP (TR-ROP), and group 2A included the remaining patients not requiring treatment. Group 1B included stage 3 ROP cases, and group 2B included the remaining stage 2 or 1 ROP cases. Group 1C included cases with zone III disease, and group 2C the remaining. The control group (group C) was composed of premature infants without ROP. The multiple comparisons were made among groups 1A, 2A, and C; 1B, 2B, and C; 1C, 2C, and C.
Results
A total of 311 infants were included. Group 1A included 34 cases, group 1B 60, group 1C 51, and group C 98. Antenatal steroid administration, gestational diabetes mellitus (GDM), gestational weight (GW), gestational age (GA), sepsis, continuous positive airway pressure (CPAP) time, and invasive mechanical ventilation (MV) time were associated with TR-ROP, stage 3 ROP, and zone I, and II disease (p < 0.05). Pregestational diabetes mellitus (DM) was only associated with stage 3 ROP (p = 0.031). Gestational hypertension was only associated with zone I and II disease (p = 0.034). The use of low-molecular-weight heparin may be protective against stage 3 disease (p = 0.031).
Conclusion
Antenatal steroid administration, GDM, GW, GA, sepsis, CPAP time, and invasive MV time were risk factors for TR-ROP and stage 3 ROP, while pregestational DM was only associated with stage 3 ROP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retinopathy of prematurity (ROP) is a disease of premature babies whose gestational age (GA) is below 32 weeks and gestational weight (GW) is less than 1500 g (g) [1]. However, ROP may also develop in infants older than 32 weeks of gestation [1]. Binocular indirect ophthalmoscopy is the gold standard method for ROP screening. Recently, optic coherence tomography (OCT) has been shown to provide significant findings in many pediatric retinal diseases such as ROP and juvenile X-linked retinoschisis [2]. Subtle retinal alterations, epiretinal membranes, and macular edema are major findings in ROP [3, 4]. In addition to well-established risk factors, including GA, GW, and uncontrolled oxygen therapy, many other risk factors have been analyzed. It has been speculated that apart from the known risk factors, other environmental and genetic factors may be associated with the development and severity of ROP disease [1]. There are several reports on the association of obstetric factors with ROP, including gestational diabetes mellitus (GDM), gestational hypertension (GHT), and antenatal steroid use in pregnant women [5,6,7,8]. The findings are inconsistent and should be further studied. The association of anticoagulant therapy during pregnancy and thrombophilia in pregnant women with ROP has not been studied previously. Perinatal factors related to premature infants have been studied by many authors, but discrepancies still exist regarding the association of oxygen therapy and sepsis with ROP [9, 10] To the best of our knowledge, AlRyalat et al. conducted the research which had included the largest number of perinatal factors associated with ROP, studied in the largest sample of premature infants [11]. The study pointed out the association of the need for prophylactic indomethacin, pneumonia, isolated bowel perforations, sepsis, and receiving ventricular shunt with ROP. Obstetricians as well as neonatologists and ophthalmologists have an important role in the prevention of ROP. However, a few papers emphasized this role. Kindinger and David published a review on the role of obstetrician in the prevention of ROP [12].
The management of ROP requires a multidisciplinary approach involving neonatologists, obstetricians, and ophthalmologists [13]. There is a paucity of data on the relationship between various obstetric factors and ROP. Our aim was to analyze the effects of various obstetric and perinatal factors on the severity of ROP.
Materials and methods
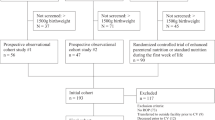
This study was performed in accordance with the Declaration of Helsinki and was approved by The Medical Research Ethics Committee (ATADEK) (2020–16/4). This retrospective study was conducted on premature infants born and cared for at Acibadem Eskisehir Hospital between January 2012 and July 2020. All premature infants were referred to the Eskisehir Osmangazi University Ophthalmology Department for ROP screening. Retinal findings were classified according to the “Revisited International Classification of ROP” [14]. The demarcation line was the only finding in stage 1 ROP cases. Retinal neovascularization developed in stage 3 cases. Zone III disease was defined as cases in which vascularization was not complete only in the residual temporal crescent of the retina. The zone of the disease was defined according to the worst vascularization in either eye at the first screen. The stage of the disease was defined as the worst stage of ROP in either eye at any examination.
The inclusion criteria for this study were as follows: (1) infants born at ≤ 32 weeks of gestation, with less than 1500 g GW; (2) follow-up until vascularization was completed and/or therapy, namely intravitreal injection, laser photocoagulation, and surgery, was applied; (3) initial screening at between 4 and 6 weeks of life (4) at least stage 1 ROP; and (5) complete charts. The control group was composed of premature infants without ROP. The controls were born at ≤ 32 weeks of gestation, with less than 1500 g GW, and screened for ROP at between 4 and 6 weeks of life.
Infants meeting any of the following criteria were excluded: (1) genetic diseases or (2) infants who missed the initial screening examination (3) infants who died during follow-up.
To calculate the required number of cases, a priori sample size calculation was performed. The calculation was made using effect size assumption. The effect size conventions level was assumed to be medium (w = 0.3). I type error level was 0.05 and power level was 99%. The total sample size calculated was two hundred and six.
Seven groups of infants were defined. Group 1A included treatment-requiring ROP (TR-ROP), and group 2A included the remaining patients not requiring treatment. Group 1B included stage 3 ROP cases with or without indication for treatment, and group 2B included the remaining stage 2 or 1 ROP cases. Group 1C included cases with zone III disease, and group 2C included the remaining. The control group (group C) was composed of premature infants without ROP.
Perinatal factors, including the baseline characteristics (sex, GW, and GA), the occurrence of bronchopulmonary dysplasia (BPD) and sepsis, and the number of days in which continuous positive airway pressure (CPAP) and/or invasive mechanical ventilation (MV) were used, were recorded.
Obstetric factors, including maternal age, delivery type, the use of antenatal steroids, the application of anticoagulant therapy, the presence of maternal thrombophilia, chronic hypertension, GHT, pregestational diabetes mellitus (DM) and GDM, were recorded. The timing of antenatal steroid administration, namely intramuscular betamethasone (Celestone Chronodose, Schering-Eczacıbası, Luleburgaz, Turkey), was noted. The use of low-molecular-weight heparin (LMWH) [enoxoparin (Oksapar 4000 anti-Xa IU/0.4 ml®, Kocak Farma, Istanbul, Turkey)], 100 mg acetylsalicylic acid (ASA) or their combination was noted.
The obstetric and perinatal factors were compared among groups. The multiple comparisons were made among groups 1A, 2A, and C; 1B, 2B, and C; 1C, 2C, and C.
The data failed the Shapiro–Wilk test for normal distribution; therefore, we compared the continuous clinical characteristics among groups using the nonparametric Kruskal–Wallis H test. We compared the categorical variables among groups using Pearson/Pearson exact chi-square tests. P values < 0.05 were considered statistically significant. Statistical analyses were performed using SPSS statistical software (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.).
Results
One thousand one hundred fifty-five premature infants born were reviewed. Three hundred eleven cases satisfied the inclusion criteria. The mean GW was 1259.94 ± 212.60 g (438–1490), and the mean GA was 29.83 ± 1.89 weeks. The indication for ROP treatment was present in thirty-four infants out of two hundred thirteen cases with different degrees of ROP (15.9%). The mean number of examinations per infants diagnosed with ROP was 4.30 ± 2.05 (2–9). The control group was examined only once.
Group 1A was composed of thirty-four infants, group 1B was composed of sixty stage 3 ROP cases, and group 1C was composed of fifty-one cases with zone III disease. One of the stage 2 zone 2 ROP cases is presented in Fig. 1. The control group was composed of ninety-eight premature infants without ROP.
Table 1 presents the comparison of the obstetric factors among groups 1A, 2A, and C. The use of antenatal steroids, the use of antenatal steroid therapy 0–48 h before birth, and the presence of GDM were significantly higher in group 1A.
Table 2 presents the comparison of the obstetric factors among groups 1B, 2B, and C. The use of LMWH was significantly higher in group 2B, while the use of antenatal steroids, the use of antenatal steroid therapy 0–48 h before birth, the presence of pregestational DM, and GDM were significantly higher in group 1B.
Table 3 presents the comparison of the obstetric factors among groups 1C, 2C, and C. The use of antenatal steroid therapy, the use of antenatal steroid therapy 0–48 h before birth, GHT, and GDM were significantly higher in group 2C.
Table 4 presents the comparison of the perinatal factors among groups 1A, 2A, and C. The GW, GA, sepsis frequency, CPAP time, and invasive MV time were significantly different.
Table 5 presents the comparison of the perinatal factors among groups 1B, 2B, and C. The GW, GA, sepsis frequency, CPAP time, and invasive MV time were significantly different.
Table 6 presents the comparison of the perinatal factors among groups 1C, 2C, and C. The GW, GA, BPD, sepsis frequency, CPAP time, and invasive MV time were significantly different.
Discussion
In the current study including three hundred eleven infants, 8 perinatal and 8 obstetric risk factors for ROP were analyzed. To the best of our knowledge, this was the research which included the largest number of risk factors for ROP in one study. Antenatal steroid administration, GDM, GW, GA, sepsis, CPAP time, and invasive MV time were found to be associated with TR-ROP, and stage 3 ROP. Pregestational DM was found to be associated with stage 3 ROP in which treatment is commonly indicated. The use of LMWH was found to lower the risk of stage 3 disease. On the other hand, the use of antenatal steroids, GHT, GDM, GW, GA, sepsis occurrence, CPAP therapy, and MV ventilation times were associated with halting vascularization in zone 3.
Prolonged and/or uncontrolled oxygen use, GA and GW are the major risk factors for ROP development [1]. The risk of severe ROP increases as GA decreases [1]. We reviewed infants of ≤ 32 weeks GA and < 1500 g GW in whom mild-to-severe ROP developed. The mean GW was not different between group 1A (TR-ROP) and 2A, whereas there was a one-week difference in the mean GA. The group 1C neonates (zone 3 disease) and group 2B neonates (stage 1 and 2 disease) were significantly larger than neonates in the other groups. We evaluated the effect of oxygen therapy on the severity of ROP. ROP severity was especially associated with the MV time. Consistent with our study, Chaves-Samaniego et al. concluded that MV time must be taken into account when predicting the need for ROP treatment [15]. The duration of CPAP therapy increased the risk of stage 3 disease and zone I and zone II disease. Although the duration of CPAP therapy failed to reach a statistical significance between group 1A and 2A, statistical significance was found between TR-ROP and control cases. Similar to our finding, Arima et al. reported that CPAP therapy was highly associated with TR-ROP [9]. Contrary to our results regarding the duration of oxygen therapy, BPD and surfactant therapy were not associated with ROP severity. In many studies, sepsis was found to increase the risk of ROP [16], but Wang et al. stated that there were inconsistent findings among different studies [10]. In the current study, sepsis was significantly more frequent in cases with stage 3 disease than in those with milder stages. The sepsis rate was also higher in group 1A cases (38%) compared to group 2A cases (15%), but the difference between these two groups failed to reach statistical significance. The sepsis rate was significantly higher in TR-ROP, when compared to control infants.
Antenatal steroids have been used in women at risk of preterm labor. This treatment decreases the risk of mortality and morbidity in premature births [17]. There are inconsistent publications about the effects of antenatal steroids on ROP. Karna et al. showed that the use of antenatal steroids had no significant effect on the development of severe ROP [18]. In a study by Smith et al., single or multiple courses of antenatal steroids did not prevent severe ROP [7]. In a systematic review and meta-analysis, antenatal steroid administration was associated with a reduced risk of severe ROP [8]. It is well known that antenatal steroids decrease the risk of respiratory distress syndrome and the requirement of oxygen therapy [17]. These effects may reduce the risk of severe ROP development, since prolonged supplemental oxygen is a risk factor for ROP development. On the other hand, antenatal steroids may improve preterm survival [17]. This may increase the ROP incidence since more premature patients will survive. In the current study, antenatal steroids were associated with TR-ROP, while their early use two days prior to birth was associated with halting retinal vascularization. Our finding was inconsistent with the previous literature [8]. The BPD occurrence was similar among groups, while the duration of MV was significantly longer in our TR-ROP cases. The higher incidence of antenatal steroid administration in severe ROP cases may be an indication of prematurity. This could be an independent explanation for the higher development of severe ROP in these cases. However, the mean GW was similar among groups 1A (TR-ROP) and 2A (1191 vs 1213 g). The difference in the mean GA was only one week (28. vs 29.4 weeks). Based on our results, we speculated that antenatal steroids could have halted retinal vascularization. Based on our literature search, we found two possible independent explanations for the association of ROP and antenatal steroids. Antenatal betamethasone use has been shown to increase vascular reactivity to endothelin-1 in an in vitro study [19]. Second, antenatal steroid exposure in the late preterm period was associated with reduced cord blood neurotrophin-3 [20]. This reduction may prevent neuroretinal development, which is mandatory for the termination of retinal vascularization [21].
GDM and hypertension are known risk factors for premature delivery [22, 23]. GDM also raises the risk of GHT [22]. The incidence of gestational DM has been reported to be approximately 10% in the USA, while variable values between 7 and 17% have been reported [24]. Hypertensive disorders in pregnancy complicate 3–8% of all pregnancies [25]. In the current study, twenty-seven out of two hundred thirteen infants (12.7%) were born to women with GDM. The incidence was over 20% in severe ROP cases. Hypertension was diagnosed in over 10% of patients in all of our groups. Several studies have evaluated the relationship between GDM and ROP. In some papers, GDM was an independent risk factor for ROP severity, while no association has been found in others [26, 27]. Kaempf et al. showed that higher mean blood glucose levels were associated with both mild and severe ROP [28]. Opara et al. found that the strength of the association between GDM and ROP increased with increasing severity of ROP [29]. Tunay et al. found GDM to be a risk factor for ROP in premature neonates with a GW of 1500 g or more [30]. On the other hand, in a systematic review and meta-analysis by Razak and Faden, GDM was not a risk factor for ROP [27]. In our study, GDM was significantly associated with TR-ROP and stage 3 ROP. Garg et al. reported a relationship between hyperglycemia and ROP [31]. They conducted a study on rat retinal Müller and mesangial cells and suggested that VEGF protein expression increases in hyperglycemia. This is a possible reason for the higher ROP in premature infants born to women with GDM. The association of GHT disorders and ROP is controversial. Many studies concluded no significant association, but larger avascular areas in the retina were associated with maternal hypertension in a study by Zayed et al. [32, 33]. In the current study, increased GHT was found to be associated with zone I and II disease (p = 0.034), but no association was shown between group 1A (TR-ROP) and 1B.
LMWH and ASA are the most commonly considered anticoagulants for use in pregnant women. The risk of deep venous thrombosis, prosthetic heart valves, central venous sinus thrombosis, and recurrent pregnancy loss are major indications for anticoagulant use in pregnant women [34]. Acquired and inherited thrombophilias are common etiologies for an increased risk of thrombotic diseases, spontaneous abortions, and premature birth [34]. In the current study, maternal thrombophilia was slightly more frequent in severe ROP cases but failed to reach statistical significance. This may be due to the inheritance of some genes associated with the risk of severe ROP from pregnant women with thrombophilia. Aydin et al. reported that the prevalence of the factor V Leiden polymorphism was higher in ROP cases [35]. On the other hand, the use of LMWH was more frequently used in group 2A (ROP not requiring treatment) and 2B (stage 1 and 2 ROP) cases, but the difference was not statistically significant. We only obtained a statistically significant difference in the use of LMWH between stage 3 cases and the other ROP patients. In several studies, women receiving LMWH and/or aspirin had lower rates of premature birth [34, 36]. Anticoagulant therapy, especially LMWH, may be associated with larger GAs (28.1 weeks in group 1B vs 29.7 weeks in group 2B). This may be the reason for the increase in the occurrence of stage 3 disease in cases not receiving LMWH therapy.
The strengths of this study include the evaluation of sixteen variables, including eight obstetric and eight perinatal factors, among groups with different ROP severities and the relatively large number of premature infants included. Premature infants ≤ 32 weeks GA and < 1500 g GW in whom ROP developed were included. This study group enabled us to make some relevant comments about the associations of variables other than GA and GW on ROP severity. There are several limitations related to the inclusion criteria, variables, and statistical analyses. GA and GW are well-known risk factors for ROP, and our aim was not to compare these variables. If we could have included infants ≤ 30 weeks GA, the groups would have been more uniform, which would have improved our analysis of obstetric factors and perinatal factors other than GA and GW. OCT under topical anesthesia could be routinely applied in all of our cases, and this could add valuable data to our study groups [3, 4, 37]. However, the difficulties of its application in neonates, especially with ROP, prevented us to perform OCT in all premature infants. Intraventricular hemorrhage has been proposed as one of the risk factors for severe ROP [38]. We could also have involved this factor, but the medical charts lacked this information. Although the number of cases included was relatively large, the number of patients was not sufficient to perform binary logistic regression analysis of sixteen parameters.
In conclusion, antenatal steroid administration, GDM, GW, GA, sepsis, CPAP time, and invasive MV time were found to be associated with TR-ROP and stage 3 ROP, while pregestational DM was only found to be associated with stage 3 ROP. The use of LMWH was postulated to be a possible protective factor against stage 3 disease. Based on our findings, collaboration between pediatric ophthalmologists, neonatologists, and obstetricians may help ophthalmologists to identify the riskier premature infants. This collaborative approach to ROP could improve ROP outcomes by timely diagnosing TR-ROP. We would like to point out the importance of obstetricians as well as neonatologists and ophthalmologists in the prevention and early treatment of ROP. Further studies are required that should include more infants with smaller GA compared to the current study to support our findings.
Availability of data and material
All the authors have full control of all primary data and agree to allow the International Ophthalmology to review their data upon request.
References
Kim SJ, Port AD, Swan R, Campbell JP, Chan RVP, Chiang MF (2018) Retinopathy of prematurity: a review of risk factors and their clinical significance. Surv Ophthalmol 63:618–637. https://doi.org/10.1016/j.survophthal.2018.04.002
Galantuomo MS, Fossarello M, Cuccu A et al (2016) Rebound macular edema following oral acetazolamide therapy for juvenile X-linked retinoschisis in an Italian family. Clin Ophthalmol 10:2377–2382. https://doi.org/10.2147/OPTH.S114568
Cernichiaro-Espinosa LA, Olguin-Manriquez FJ, Henaine-Berra A, Garcia-Aguirre G, Quiroz-MercadoH M-C (2016) New insights in diagnosis and treatment for Retinopathy of Prematurity. Int Ophthalmol 36:751–760. https://doi.org/10.1007/s10792-016-0177-8
Anwar S, Nath M, Patel A, Lee H, Brown S, Gottlob I, Proudlock FA (2020) Potential utility of foveal morphology in preterm infants measured using hand-held optical coherence tomography in retinopathy of prematurity screening. Retina (Philadelphia, Pa.) 40:1592–1602. https://doi.org/10.1097/IAE.0000000000002622
Au SC, Tang SM, Rong SS, Chen LJ, Yam JC (2015) Association between hyperglycemia and retinopathy of prematurity: a systemic review and meta-analysis. Sci Rep 5:9091. https://doi.org/10.1038/srep09091
Chan PY, Tang SM, Au SC et al (2016) Association of gestational hypertensive disorders with retinopathy of prematurity: a systematic review and meta-analysis. Sci Rep 6:30732. https://doi.org/10.1038/srep30732
Smith LM, Qureshi N, Chao CR (2000) Effects of single and multiple courses of antenatal glucocorticoids in preterm newborns less than 30 weeks’ gestation. J Matern Fetal Med 9:131–135
Yim CL, Tam M, Chan HL et al (2018) Association of antenatal steroid and risk of retinopathy of prematurity: a systematic review and meta-analysis. Br J Ophthalmol 102:1336–1341. https://doi.org/10.1136/bjophthalmol-2017-311576
Arima M, Tsukamoto S, Fujiwara K, Murayama M, Fujikawa K, Sonoda KH (2017) Late onset circulatory collapse and continuous positive airway pressure are useful predictors of treatment-requiring retinopathy of prematurity: a 9-year retrospective analysis. Sci Rep 7:3904. https://doi.org/10.1038/s41598-017-04269-5
Wang X, Tang K, Chen L, Cheng S, Xu H (2019) Association between sepsis and retinopathy of prematurity: a systematic review and meta-analysis. BMJ Open 9:e025440. https://doi.org/10.1136/bmjopen-2018-025440
AlRyalat SA, Al Oweidat K, Al-Amer A et al (2020) Perinatal events predicting retinopathy of prematurity in extremely pre-term infants. J Neonatal Perinatal Med 13:261–266. https://doi.org/10.3233/NPM-190336
Kindinger LM, David AL (2019) The role of the obstetrician in the prevention of retinopathy of prematurity. Semin Perinatol 43:323–332. https://doi.org/10.1053/j.semperi.2019.05.003
Gilbert CE, Dawes L, Wise M, Darlow BA (2019) Obstetric strategies to reduce blindness from retinopathy of prematurity in infants born preterm. Acta Obstet Gynecol Scand 98:1497–1499. https://doi.org/10.1111/aogs.13684
International Committee for the Classification of Retinopathy of Prematurity (2005) The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 123:991–999. https://doi.org/10.1001/archopht.123.7.991
Chaves-Samaniego MJ, García Castejón M, Chaves-Samaniego MC et al (2020) Risk calculator for retinopathy of prematurity requiring treatment. Front Pediatr 8:529639. https://doi.org/10.3389/fped.2020.529639
Huang J, Tang Y, Zhu T, Li Y et al (2019) Cumulative evidence for association of sepsis and retinopathy of prematurity. Medicine (Baltimore) 98:e17512. https://doi.org/10.1097/MD.0000000000017512
Kemp MW, Newnham JP, Challis JG, Jobe AH, Stock SJ (2016) The clinical use of corticosteroids in pregnancy. Hum Reprod Update 22:240–259. https://doi.org/10.1093/humupd/dmv047
Karna P, Muttineni J, Angell L, Karmaus W (2005) Retinopathy of prematurity and risk factors: a prospective cohort study. BMC Pediatr 5:18. https://doi.org/10.1186/1471-2431-5-18
Lee JH, Zhang J, Massmann GA, Figueroa JP (2014) Antenatal betamethasone increases vascular reactivity to endothelin-1 by upregulation of CD38/cADPR signaling. J Dev Orig Health Dis 5:56–62. https://doi.org/10.1017/S2040174413000512
Hodyl NA, Crawford TM, McKerracher L, Lawrence A, Pitcher JB, Stark MJ (2016) Antenatal steroid exposure in the late preterm period is associated with reduced cord blood neurotrophin-3. Early Hum Dev 101:57–62. https://doi.org/10.1016/j.earlhumdev.2016.03.016
Tremblay S, Miloudi K, Chaychi S et al (2013) Systemic inflammation perturbs developmental retinal angiogenesis and neuroretinal function. Invest Ophthalmol Vis Sci 54:8125–8139. https://doi.org/10.1167/iovs.13-12496
Lende M, Rijhsinghani A (2020) Gestational diabetes: overview with emphasis on medical management. Int J Environ Res Public Health 17:9573. https://doi.org/10.3390/ijerph17249573
Bernardes TP, Zwertbroek EF, Broekhuijsen K et al (2019) Delivery or expectant management for prevention of adverse maternal and neonatal outcomes in hypertensive disorders of pregnancy: an individual participant data meta-analysis. Ultrasound Obstet Gynecol 53:443–453. https://doi.org/10.1002/uog.20224
Mishra S, Rao CR, Ab S (2016) Trends in the diagnosis of gestational diabetes mellitus. Scientifica (Cairo) 2016:5489015. https://doi.org/10.1155/2016/5489015
Naderi S, Tsai SA, Khandelwal A (2017) Hypertensive disorders of pregnancy. Curr Atheroscler Rep 19:15. https://doi.org/10.1007/s11883-017-0648-z
Mohamed S, Murray JC, Dagle JM, Colaizy T (2013) Hyperglycemia as a risk factor for the development of retinopathy of prematurity. BMC Pediatr 13:78. https://doi.org/10.1186/1471-2431-13-78
Razak A, Faden M (2021) Association of maternal diabetes mellitus with preterm infant outcomes: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 106:271–277. https://doi.org/10.1136/archdischild-2020-320054
Kaempf JW, Kaempf AJ, Wu Y, Stawarz M, Niemeyer J, Grunkemeier G (2011) Hyperglycemia, insulin and slower growth velocity may increase the risk of retinopathy of prematurity. J Perinatol 31:251–257. https://doi.org/10.1038/jp.2010.152
Opara CN, Akintorin M, Byrd A, Cirignani N, Akintorin S, Soyemi K (2020) Maternal diabetes mellitus as an independent risk factor for clinically significant retinopathy of prematurity severity in neonates less than 1500g. PLoS ONE 15:e0236639. https://doi.org/10.1371/journal.pone.0236639
Tunay ZÖ, Özdemir Ö, Acar DE, Öztuna D, Uraş N (2016) Maternal diabetes as an independent risk factor for retinopathy of prematurity in infants with birth weight of 1500 g or more. Am J Ophthalmol 168:201–206. https://doi.org/10.1016/j.ajo.2016.05
Garg R, Agthe AG, Donohue PK, Lehmann CU (2003) Hyperglycemia and retinopathy of prematurity in very low birth weight infants. J Perinatol 23:186–194. https://doi.org/10.1038/sj.jp.7210879
Ge G, Zhang Y, Zhang M (2021) Pregnancy-induced hypertension and retinopathy of prematurity: a meta-analysis. Acta Ophthalmol. https://doi.org/10.1111/aos.14827.Advanceonlinepublication.10.1111/aos.14827
Zayed MA, Uppal A, Hartnett ME (2010) New-onset maternal gestational hypertension and risk of retinopathy of prematurity. Invest Ophthalmol Vis Sci 51:4983–4988. https://doi.org/10.1167/iovs.10-5283
Leaf RK, Connors JM (2017) The role of anticoagulants in the prevention of pregnancy complications. Clin Appl Thromb Hemost 23:116–123. https://doi.org/10.1177/1076029615615972
Aydin H, Gunay M, Celik G, Gunay BO, Aydin UT, Karaman A (2016) Evaluation of Factor V Leiden, Prothrombin G20210A, MTHFR C677T and MTHFR A1298C gene polymorphisms in retinopathy of prematurity in a Turkish cohort. Ophthalmic Genet 37:415–418. https://doi.org/10.3109/13816810.2015.1126611
Visser L, de Boer MA, de Groot CJM et al (2017) Low dose aspirin in the prevention of recurrent spontaneous preterm labour–the APRIL study: a multicenter randomized placebo controlled trial. BMC Pregnancy Childbirth 17:223. https://doi.org/10.1186/s12884-017-1338-0
Gursoy H, Bilgec MD, Erol N, Basmak H, Colak E (2016) The macular findings on spectral-domain optical coherence tomography in premature infants with or without retinopathy of prematurity. Int Ophthalmol 36:591–600. https://doi.org/10.1007/s10792-016-0176-9
Chang JW (2019) Risk factor analysis for the development and progression of retinopathy of prematurity. PLoS ONE 14:e0219934. https://doi.org/10.1371/journal.pone.0219934
Acknowledgements
The paper is edited for proper language by AJE editors. Certificate Verification Key is 3695-38C9-3424-574F-61DE.
Author information
Authors and Affiliations
Contributions
All of the authors meet all four of the following conditions: 1. Make substantial contributions to conception and design, and/or acquisition of data, and/or analysis and interpretation of data; 2. Participate in drafting the article or revising it critically for important intellectual content; 3. Give final approval of the version to be submitted; 4. Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any financial conflicts of interest related to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozgur Gursoy, O., Gurer, H.G., Yildiz Eren, C. et al. The association of various obstetric and perinatal factors with retinopathy of prematurity. Int Ophthalmol 42, 2719–2728 (2022). https://doi.org/10.1007/s10792-022-02260-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02260-2