Abstract
Aims
To determine herpes simplex virus (HSV) DNA positivity in corneal scraping samples obtained from patients with microbial keratitis whose findings were not specific for HSV keratitis and to evaluate these particular cases with respect to clinical features and antiviral treatment results.
Methods
Records of patients with microbial keratitis treated in a tertiary eye care hospital within the 3-year period were evaluated retrospectively. Real-time polymerase chain reaction (PCR) was used to identify HSV DNA. Smear slides were evaluated by light microscopy. Patients with typical presentations and histories of HSV keratitis were excluded.
Results
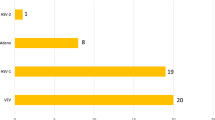
Two hundred and seventy-six eyes of 276 patients were included in the study. HSV-1 DNA was detected in 25 eyes (9%). In these 25 eyes, the initial diagnosis was fungal or bacterial keratitis. The mean symptom duration was 20 ± 14 days (2–60 days). The risk factors were ocular surgery (20%), blepharitis (16%), trauma (8%) and contact lens wear (4%); however, the majority of patients did not have any specific cause for keratitis (52%). Clinical features were variable and not typical for any particular etiology. Culture and microscopic examinations revealed bacteria and/or fungi in 6 patients in addition to herpes infection. Antiviral treatment was successful in 72% of patients.
Conclusion
Herpetic corneal infections can present without typical dendritic or geographic ulcers and may be masked by other infections. Real-time PCR is a useful method for rapid and definitive diagnosis. HSV infection should be considered for microbial keratitis without specific risk factors, with negative culture results and poor response to antimicrobial agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Herpes simplex virus (HSV) is a common worldwide pathogen, and the estimated seropositivity is 90% of the population 50 years or older in the USA [1].
The most characteristic features of HSV infection are their latent status in neural ganglion cell nuclei and various forms of recurrent peripheral herpetic disease [2]. Herpetic epithelial keratitis is one of the causes of corneal blindness, and typical presentations include dendritic or geographical ulcers [3]. In some situations, certain factors, such as delayed diagnosis, topical medications (steroids, preservatives, etc.), ocular trauma or surgical history, may cause clinical features to be atypical [4]. Timely diagnosis and initiation of treatment is crucial to prevent sight-threatening complications in herpetic corneal diseases. In atypical cases, the isolation or identification of HSV-1 is necessary for a definitive diagnosis. Laboratory tests, such as cell cytology, viral antigen detection, nucleic acid detection (polymerase chain reaction) and virus isolation, can be used for diagnosis of HSV infection.
Although viral culture is considered gold standard, besides its low sensitivity compared to polymerase chain reaction (PCR), it is relatively time-consuming and may require a week or longer based on amount of viable virus in the sample [5], whereas PCR process is automated and results can be obtained in just a few hours. PCR is not dependent on the presence of viable virus. Immunofluorescence assay (IFA) for antigen detection is also a rapid test, but it has some disadvantages, including lower sensitivity and subjective interpretation of test results [6, 7].
For HSV detection in corneal scrapings from patients with herpes simplex virus keratitis, several studies confirmed that PCR has proven to be more sensitive (70–100%) than conventional methods such as cell culture (46.2%) and IFA for HSV antigen (78.6–85.7%) [8,9,10,11]. Accurate and rapid diagnosis of herpetic keratitis is important for better patient management and appropriate early treatment. PCR appears to be the most suitable method of choice for identifying HSV DNA and could be helpful in clinical diagnosis of herpetic keratitis [7, 12, 13].
In this study, real-time PCR was used to detect HSV DNA, because it is superior to conventional PCR. Real-time PCR is much faster and less labor-intensive. It has also improved sensitivity and a lower risk of cross-contamination of samples as the whole PCR process from amplification to analysis is performed in a closed-tube system. While standard PCR requires post-PCR analysis such as agarose gel electrophoresis for identifying PCR products by size, it is time-consuming and non-automated. In addition, the primary advantage of real-time PCR is that DNA amplification can be continuously monitored during each cycle by real-time detection of fluorescent PCR products [6, 14, 15].
In this study, we aimed to analyze HSV detection rates in atypical keratitis cases and evaluate these particular cases in terms of clinical features and antiviral treatment results.
Patients and methods
Institutional review board approval was obtained for this study, which adhered to the tenets of the Declaration of Helsinki.
Case records of 276 patients with presumed microbial keratitis without typical herpetic keratitis history and/or clinical features between December 2014 and January 2018 were analyzed retrospectively. The exclusion criteria are listed in Table 1.
This study was conducted in a tertiary eye care clinic, which is a reference center for microbial keratitis in southern region of Turkey. At this institution, five laboratory examinations are performed routinely for each patients who presented with microbial keratitis: direct microscopic investigation, PCR analysis for HSV DNA, bacteriological culture examination, fungal culture examination and PCR analysis for Acanthamoeba. Patients diagnosed to have HSV keratitis by PCR DNA sequencing from corneal scraping were further analyzed.
Collected data included initial diagnosis, risk factors, symptom duration, previous treatments, lesion features, visual acuity, laboratory investigations, surgical treatments and final examination results.
Cytological examination
Alcohol-fixed smear slides sampled from cornea of the patients were stained with Papanicolaou (Pap). Slides were evaluated by light microscopy in terms of cellularity, presence/absence of intranuclear inclusion and/or multinucleation. Additional findings such as fungal hyphae and bacteria—if present—were noted. (Fig. 1a, b).
a Smear slide revealing cornea epithelial cells (arrowhead); some showing nuclear enlargement and intranuclear inclusions resulting in flu appearance (arrows) (Papanicolaou, × 400). b Cornea epithelial cells showing multinucleation (arrows) are present on smear slide (Papanicolaou, × 400) (Case no. 22 in Table 2)
PCR analysis
Corneal scraping samples from the patients were transferred in PBS (1 ml) to Eppendorf tubes and sent to the laboratory. The presence of HSV DNA in the samples was investigated by real-time PCR. Viral DNA was extracted using Viral Nucleic Acid Extraction Kit (Magnesia, Geneworks Anatolia, İstanbul, Turkey) according to the manufacturer’s instructions by Magnesia 16 auto-extraction instrument system (Anatolia Geneworks, Turkey). Real-time PCR for detection of HSV DNA was performed with HSV 1–2 Genotyping Kit (Bosphore, Anatolia Geneworks, İstanbul, Turkey) by Montania 4896 instrument (Anatolia Geneworks, Turkey). For each patient, 15 µl of PCR Master Mix was transferred to PCR tube and then 10 µl of extract was added. The thermal cycle used for amplification was an initial denaturation at 95 °C for 14.30 min, followed by 50 cycle of 97 °C for 30 s, 60 °C for 90 s and a final step of 22 °C for 5 min.
Treatment
Empirical treatment was conducted using wide-spectrum antibiotic (fortified vancomycin and amikacin) or antifungal (voriconazole) topical regimens initially and was changed according to the laboratory results.
All HSV-positive patients received topical ganciclovir 0.15% antiviral ophthalmic gel (5 times/day until epithelization and then 3 times/day for 7 days). Systemic acyclovir (p.o, 5 × 400 mg) was added to the treatment protocol according to the severity of the disease (limbus involvement, deep corneal layers involvement, progressive corneal melting or anterior chamber inflammation). Treatment regimens were adjusted, tapered and discontinued according to the course of disease. Kidney function tests were performed regularly during the course of systemic acyclovir treatment.
Results
Two hundred and seventy-six eyes of 276 patients with microbial keratitis (not specific for herpes infection) were included in the study. Real-time PCR analyses were positive for HSV in 25 patients (9%). A further analysis was performed for these HSV-positive patients.
The mean patient age was 56 ± 24 years (2–84 years) for 25 patients (15 male, 10 female). All patients were referred from other clinics. The mean symptom duration was 20 ± 14 days (2–60 days). Patient characteristics, laboratory and light microscopy results, and the course of disease are summarized in Table 2.
Three patients (12%) were using topical steroid drops before the initial presentation. The initial clinical diagnoses were fungal keratitis (4 eyes) and bacterial keratitis (21 eyes).
Risk factors were ocular surgery (20%), blepharitis (16%), trauma (8%) and contact lens wear (4%), whereas the majority of patients did not have any specific cause for keratitis (52%).
Clinical features were variable. Epithelial or stromal ulcer infiltrations with well-defined margins were common presentations; rarely, ring infiltrate and satellite lesions were observed (in two patients). Hypopyon was present in 4 patients (Fig. 2a–d).
Slit lamp images of two patients are presented as initial and final examination. Case 21, a ring-like infiltration with feathery margin and deep vascularization is shown, b healing with scar and vascularization at the end of treatment course. Case 19. c Well-defined peripheral ulcer and deep infiltration is shown. d Complete resolution after treatment
In addition to HSV infection, other microorganisms (bacteria and/or fungi) were detected in 6 patients (24%) via culture or direct microscopic examination. Real-time PCR analysis was negative for Acanthamoeba in all corneal specimens. Visual prognosis was not predictable in these mixed infected patients, while one patient with bacteria and fungi had excellent outcome (patient number 8 in Table 2), other one patient went to evisceration (patient number 6 in Table 2).
Cytological examination was also performed on corneal smear samples. Typical cytomorphological features of herpes infection with intranuclear inclusions alone (2/25) and with multinucleated giant cells (8/25), were demonstrated in 10 of 25 (40%) patients. These findings supported the diagnosis of herpetic keratitis in these patients.
Mean healing time was 54 ± 38 days (10–200 days). At the end of the follow-up, 18 patients (72%) showed favorable responses to antiviral treatment (topical and/or oral); their inflammation subsided and ulcers healed. In 7 patients, the disease was not controlled with medical treatment alone and amniotic membrane transplantation (5 patients) or tectonic keratoplasty (1 patient) was required. Unfortunately, 1 patient experienced evisceration because of uncontrolled cornea-scleral lysis and perforation.
Visual acuity values were in low levels at first visit (majority of patients had hand motion vision). In course of treatment, none of the vision values reduced. At the final visit, visual acuity had increased two or more line in 4 patients (16%).
Discussion
Herpes simplex keratitis is one of the challenges in ophthalmology because of diagnostic and treatment difficulties. Diagnosis is commonly based on clinical features and repeated disease history. Atypical presentations have been observed in HSV keratitis, which may mimic other infections [14,15,16,17]. For these cases, clinician suspicion has a critical role in prognosis. Diagnosis can be difficult, especially in later stages of the disease. When repeated culture or cytological examinations are unable to detect any causative agent or there is no response to empirical antimicrobial treatments, HSV infection may be responsible for the clinical picture.
Atypical herpes keratitis may be underestimated. In a clinical study, the corneal explant buttons of patients with clinically atypical and typical herpetic stromal keratitis were evaluated for the presence of HSV DNA; the frequencies of HSV DNA were comparable in the atypical and typical groups (25% and 37%, respectively) [18].
In this study, HSV infection was detected in 9% of microbial keratitis cases that did not have typical features of herpetic keratitis. Because of geographical and sociocultural factors (subtrophic climate and agricultural works), bacterial or fungal keratitis was the principal confusions in the initial phase.
Initial clinical features were variable, including round- or feathery-margin ulcers with stromal infiltration and satellite or ring infiltrates. Patients had been using various topical medications (antibiotics, antifungals, steroids) before presentation. Mean symptom duration (time to diagnosis) was 20 days that may be explained with all patients referred form other clinics and who treated with various diagnoses before presentation. Delayed diagnosis may be cause of permanent changes in corneal tissue and visual disability. Super-infections and toxicity caused by the prolonged use of ineffective medications may be responsible for atypical clinical presentations. Visual prognosis was poor in cases that presented late. Unfortunately, corneal perforation developed in one case.
Risk factor evaluation can be helpful for a definitive diagnosis in the majority of microbial keratitis cases, such as contact lens use, trauma with organic matter or chronic blepharitis. However, patients with atypical herpetic keratitis may not have such risk factors. In our series, half of the patients did not have any specific risk factor; therefore, we recommend considering herpes infection in situations where there is no definitive risk factor for keratitis.
Isolation or identification of HSV from corneal specimens is necessary for the diagnosis of atypical cases. Cytology is a quick and simple method to determine cytological changes in HSV-infected cells, such as multinucleated giant cells and intranuclear inclusions [19]. However, this method has lower sensitivity (57%) and specificity [8]. Similarly, we observed these cytological features in 40% of corneal specimens. Cytological examination is cost-effective when compared with molecular diagnostic tests, but expert interpretation is important for reliable results. On the other hand, molecular diagnosis by PCR is generally accepted valuable and reliable laboratory diagnostic test to confirm herpetic ocular diseases, especially in atypical herpetic keratitis [3, 16, 18].
This study had some limitations because of its retrospective design, as we did not have knowledge regarding the status of corneal sensation, which may be helpful for documentation. Further investigations with a larger number of cases are needed to confirm the results of this study.
In clinically atypical herpetic keratitis, virus may be a primary trigger or a secondary contributor of disease. Early antiherpetic treatments should be considered if empirical treatment does not effectively control keratitis. PCR analysis is a useful method for quickly identifying HSV keratitis, as it provides a timely diagnosis for the accurate management of atypical cases.
References
Bradley H, Markowitz LE, Gibson T et al (2014) Seroprevalence of herpes simplex virus types 1 and 2: United States, 1999–2010. J Infect Dis 209:325–333
Whitley RJ, Roizman B (2001) Herpes simplex virus infections. Lancet 357:1513–1518
Tsatsos M, MacGregor C, Athanasiadis I et al (2016) Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Exp Ophthalmol 44:824–837
Beyer CF, Arens MQ, Hill JM et al (1989) Penetrating keratoplasty in rabbits induces latent HSV-1 reactivation when corticosteroids are used. Curr Eye Res 8:1323–1329
Hudu SA, Alshrari AS, Syahida A et al (2016) Cell culture, technology: enhancing the culture of diagnosing human diseases. J Clin Diagn Res 10:1–5
Hwang KA, Ahn JH, Nam JH (2018) Diagnosis of viral infection using real-time polymerase chain reaction. J Bacteriol Virol 48:1–13
Azher TN, Yin XT, Tajfirouz D et al (2017) Herpes simplex keratitis: challenges in diagnosis and clinical management. Clin Ophthalmol 11:185–191
Subhan S, Jose RJ, Duggirala A et al (2004) Diagnosis of herpes simplex virus-1 keratitis: comparison of Giemsa stain, immunofluorescence assay and polymerase chain reaction. Curr Eye Res 29:209–213
Farhatullah S, Kaza S, Athmanathan S, Garg P et al (2004) Diagnosis of herpes simplex virus-1 keratitis using Giemsa stain, immunofluorescence assay, and polymerase chain reaction assay on corneal scrapings. Br J Ophthalmol 88:142–144
Barrado L, Suarez MJ, Pérez-Blázquez E et al (2014) Could polymerase chain reaction tests on conjunctival swabs be useful to diagnose herpetic keratitis? Enferm Infecc Microbiol Clin 32:28–30
El-Aal AM, El Sayed M, Mohammed E et al (2006) Evaluation of herpes simplex detection in corneal scrapings by three molecular methods. Curr Microbiol 52:379–382
Taravati P, Lam D, Van Gelder RN (2013) Role of molecular diagnostics in ocular microbiology. Curr Ophthalmol Rep 1:1–13
Satpathy G, Behera HS, Sharma A et al (2018) A 20-year experience of ocular herpes virus detection using immunofluorescence and polymerase chain reaction. Clin Exp Optom 101:648–651
Mackay M (2004) Real-time PCR in the microbiology laboratory. Clin Microbiol Infect 10:190–212
Kalezic T, Mazen M, Kuklinski E et al (2018) Herpetic eye disease study: lesson learned. Curr Opin Ophthalmol 29:340–346
Koizumi N, Nishida K, Adachi W et al (1999) Detection of herpes simplex virus DNA in atypical epithelial keratitis using polymerase chain reaction. Br J Ophthalmol 83:957–960
Tei M, Nishida K, Kinoshita S (1996) Polymerase chain reaction of herpes simplex virus in tear fluid from atypical herpetic epithelial keratitis after penetrating keratoplasty. Am J Ophthalmol 122:732–735
Garweg JG, Russ CE, Shellhorn M et al (2003) HSV-1 antigens and DNA in the corneal explant buttons of patients with non-herpetic or clinically atypical herpetic stromal keratitis. Graefe’s Arch Clin Exp Ophthalmol 241:734–739
Kaye S, Choudhary A (2006) Herpes simplex keratitis. Prog Retin Eye Res 25:355–380
Funding
This study was funded by government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest for this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Erdem, E., Harbiyeli, İ.İ., Öztürk, G. et al. Atypical herpes simplex keratitis: frequency, clinical presentations and treatment results. Int Ophthalmol 40, 659–665 (2020). https://doi.org/10.1007/s10792-019-01226-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01226-1