Abstract
Purpose
To evaluate the in vitro efficacy of three commercial ophthalmic solutions (gatifloxacin, levofloxacin and gentamicin) against cysts of Acanthamoeba species.
Design
Experimental study
Methods
Acanthamoeba cysts belonging to genotypes T3, T4 and T5 were incubated with three ophthalmic solutions for different periods of time; 1, 24, 48 and 72 h at 37 °C. After incubation, treated cysts were stained with trypan blue and counted to express the percent of growth inhibition. Additionally, the viability of treated cysts was assessed by culturing them in PYG medium at 30 °C for 72 h as well as on non-nutrient agar plates at 30 °C for 1 month.
Results
Acanthamoeba cysts of all genotypes were susceptible to gentamicin and gatifloxacin after exposure for 1 h and 24 h, respectively, and for levofloxacin, cysts of all genotypes were resistant to levofloxacin even after 72 h of incubation. Gentamicin and gatifloxacin showed statistically highly significant difference (P < 0.001), and levofloxacin showed statistically significant difference (P < 0.05) in comparison to non-treated control.
Conclusions
Gentamicin and gatifloxacin were highly effective against Acanthamoeba cysts. Although our results should be confirmed in animal models, this result will guide the choice of the appropriate ophthalmic drugs for early treatment of eye infection caused by Acanthamoeba spp.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Free-living amoebae of the genus Acanthamoeba are the worldwide distribution in a variety of habitats such as soil, water and even in the air [1]. There are two forms in their life cycle, a vegetative trophozoite stage and a highly resistant cyst stage. Trophozoite can develop into protective cyst form when environmental conditions become adverse. Based on the variation of nucleotide sequences of the Diagnostic fragment 3 (DF3) region of the 18S rRNA gene, Acanthamoeba spp. have been classified into 20 genotypes, T1–T20 [2]. Acanthamoeba species can cause serious infections, granulomatous amoebic encephalitis (GAE) which is rare but high fatality rate in immunocompromised persons and amoebic keratitis (AK) in immunocompetent persons, which can result in poor vision or blindness if delay in diagnosis and inadequate treatment. In developing countries, AK has been reported in people previously suffering from corneal ulcers and having contact with contaminated water and soil, even without wearing contact lenses [3]. In Thailand, AK cases have been reported among both contact lens users and non-contact lens users. Twenty-four AK cases occurred in Thailand between 1996 and 2006 [4, 5], of which five were reported in 1999 [6]. Misdiagnosis of AK is common because signs and symptoms are not specific and can mimic bacteria, fungal or viral keratitis [1] together with lacking of consensus of AK diagnosis, these lead to AK remains significant. Therefore, AK treatment depends on clinicians’ experience. At present, the first-line drugs for AK are biguanides, such as chlorhexidine and PHMB, and diamidines such as propamidine isethionate and neomycin. Although the treatment of AK often requires a combination of biguanides and diamidines [7], not all AK cases are cured with these [8]. Trophozoites are usually susceptible to biocides including therapeutic drugs. The major problem for AK treatment is therefore, unable to eliminate cyst stage completely [9]. Various therapeutic drugs have been studied in vitro by focusing on cysticidal efficacy, as effectiveness is essential for subsequent studies in vivo therapy of Acanthamoeba keratitis [10,11,12]. However, their protocols have not been standardized for using and no eyedrops preparations are commercially available. Moreover, there are no fully effective against all strains in the available treatments. Therefore, it is necessary to study new therapeutic agents to be the alternative drugs for AK treatment.
The aim of this study was to evaluate the in vitro efficacy of three commercially available ophthalmic solutions (gatifloxacin, levofloxacin and gentamicin) against cysts of three Acanthamoeba strains, Thailand isolates. These ophthalmic drugs are usually used to treat keratitis caused by bacteria. Chlorhexidine, first-line AK treatment, was used as a reference drug. This study will guide the choice of drug to treat early stages of eye disease caused by Acanthamoeba spp.
Methods
Acanthamoeba strains and cysts preparation
Three environmental strains of Acanthamoeba were examined: GenBank accession numbers KT897271 (T3), KT897265 (T4) and KT897268 (T5) [13]. Each strain was cultured onto non-nutrient agar plates which were seeded with 5 µL of heat-killed Escherichia coli and incubated at 30 °C for 3 weeks. The cysts were harvested by washing plates with phosphate buffered saline (PBS) and decanted into 15 mL tubes which were centrifuged at 3000 rpm for 5 min. The supernatant was discarded and 0.5% sodium dodecyl sulfate (SDS) added for 10 min to lyse immature cysts and then the tubes were centrifuged at 3000 rpm for 5 min. The SDS was washed out twice using PBS. Finally, cysts were counted with a hemocytometer and standardized to a concentration of 20 × 104 cysts/mL.
Chemicals
Four antimicrobial agents were tested: chlorhexidine (Sigma-Aldrich, USA) was prepared at the commercially available concentrations (0.02%) and used as reference drug, and three ophthalmic solutions, 0.3% gentamicin (3 mg/mL) (Seng Thai Pharmaceutical Laboratory, Bangkok, Thailand), 0.3% gatifloxacin (3 mg/mL) (Allergan Sales, TX, USA) and 0.5% levofloxacin (5 mg/mL) (Santen Pharmaceutical Laboratory, Osaka, Japan).
Evaluation of the cysticidal activity
Qualification assays
Experiments for eyedrops testing on cysts were performed in the sterile microtube. Briefly, 100 µL of each of calibrated Acanthamoeba strain (20 × 104 cysts/mL) was incubated with 100 µL of each eyedrop for 1, 24, 48 and 72 h at 37 °C, each in duplicate. After incubation, the suspension was washed twice with PBS to eliminate residual drugs and resuspended with 100 µL PBS. The cyst viability was examined by taking 20 µL of sample into NNA medium coated with heated E. coli and incubated at 30 °C, examining the samples every day by microscope for 1 month. The remaining content was then cultured in 500 µL axenically PYG medium containing 50 µg/mL enrofloxacin (General Drugs House, Bangkok, Thailand) and incubated at 30 °C for 72 h in 96-well microtiter plate and examined by inverted microscope. The presence of trophozoite was considered as drug-resistant strain.
Quantification assays
For growth inhibition evaluation, 100 µL of treated cysts of each eyedrop were stained with 100 µL 0.4% trypan blue for 10 min, unstained cysts were viable and stained cysts were nonviable [14]. Viable and nonviable cysts were then counted using the hemocytometer at 1, 24, 48 and 72 h. The percent of growth inhibition was calculated: Percent of growth inhibition = a − b/a × 100 (a mean number of non-treated cysts, b is the mean number of treated cysts) [15].
All assays, both qualification and quantification were repeated five times, each in duplicate, for each strain. In addition, control containing cysts treated with 0.02% chlorhexidine gluconate as a reference drug control and cysts in PBS as non-treated control were performed to the same procedure. The effect of eyedrops on cysts for morphological observation was examined by a light microscope (× 40).
Data analysis
Data management and analysis were made using SPSS version 19.0 for Windows. Cyst number was calculated as mean ± SD and percent of growth inhibition. The mean numbers were analyzed by using analysis of variance (ANOVA) followed by the Tukey test for post hoc comparisons.
Results
Cysticidal activity assays
The efficacy of three ophthalmic drugs (0.3% gentamicin, 0.3% gatifloxacin and 0.5% levofloxacin) was evaluated for their cysticidal activity against three Acanthamoeba strains at different time points (1, 24, 48, 72 h). After incubation, the viability was determined using trypan blue staining and counting for growth inhibition calculation. The results showed that Acanthamoeba cysts of all strains were susceptible to gentamicin and gatifloxacin when incubated for at least 1 and 24 h, respectively. Levofloxacin was the least effective of the three drugs tested. No genotypes were completely killed, even after 72 h incubation. The results of growth inhibition are shown in Fig. 1, and mean number of cysts (mean ± SD) after exposure to drugs are shown in Table 1. After statistical analysis, gentamicin and gatifloxacin showed highly statistically significant difference (P < 0.001) and levofloxacin showed statistically significant difference (P < 0.05) as compared with non-treated control. Gentamicin was the most effective ophthalmic drugs against cysts of all three genotypes of Acanthamoeba in our study (P < 0.001).
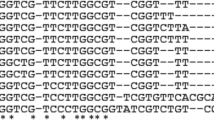
In the present study, treated cysts were inoculated into PYG medium and on NNA medium overlaid with heated E. coli for qualification viability tests. The results from NNA culture corresponded to PYG culture; gentamicin and gatifloxacin were highly effective against Acanthamoeba cysts of all genotypes after exposure 1 h and 24 h, respectively. In contrast, levofloxacin had the least effectiveness against all three genotypes. Even after incubation with this drug for 72 h, cysts of all three genotypes were capable of yielding trophozoites in the viability test. Figure 2 showed the results of Acanthamoeba cysts of genotype T4 treated with each eyedrop for 72 h and then cultured in PYG medium. After observation by inverted microscope (× 20), the results revealed there were no excysted trophozoites in samples treated with 0.02% chlorhexidine, 0.3% gentamicin and 0.3% gatifloxacin, but presented in sample treated with 0.5% levofloxacin. The other two strains, T3 and T5 genotypes, also revealed the same results (data not shown). The altered morphology with cytoplasm destruction after 24 h of incubation with each effective eyedrop, chlorhexidine, gatifloxacin and gentamicin is shown in Fig. 3.
Discussion
Our study has presented the susceptibility of cysts of three genotypes (T3, T4 and T5) of Acanthamoeba to three commercially available drugs. The results showed that gentamicin and gatifloxacin showed statistically highly significant difference (P < 0.001) and levofloxacin showed statistically significant difference (P < 0.05) as compared with non-treated control. Of these three drugs, gentamicin was the most effective drug (P < 0.001). Gentamicin and gatifloxacin killed cysts of all three genotypes within 1 and 24 h, respectively. In the case of levofloxacin, no genotypes were completely killed, even after 72 h of incubation. These drugs are primarily known for killing bacteria, but some of them have shown activity against Acanthamoeba spp. both in vitro and in clinical treatment [10, 16,17,18]. As used by us in vitro, drugs were diluted to 50% of their supplied concentration. In clinical use, drugs applied to the eye will also be diluted, and eventually flushed out, by the production of lachrymal fluid [19]. Gentamicin is a member of the aminoglycoside group, to have high efficacy against Acanthamoeba cyst by inhibiting protein synthesis [20]. We found that 0.3%gentamicin (3 mg/mL) has cysticidal activity after only 1 h. Another study has found that a lower concentration of gentamicin was also effective against clinical and environmental strains of Acanthamoeba [16]. The mean minimum cysticidal concentration (MCC) at 30 °C in all tested strains was 0.193 mg/mL and 0.029 mg/mL at 37 °C (range 0.031–1 mg/mL) after incubation for 48 h. In addition, they found that environmental strains were more sensitive than clinical strains to gentamicin [16]. However, another study reported that gentamicin was clinically ineffective at 5 mg/mL but the drug’s mean MCC was 13.33 mg/mL (range 10–20 mg/mL) after exposure to clinical strains for 24 h [10]. Gatifloxacin affected the morphology of cysts belonging to genotypes T3, T4 and T5 after 24 h. In this study, levofloxacin was the least effective of the three drugs tested against cysts, despite 72 h of incubation. Levofloxacin may require more incubation time to kill Acanthamoeba cyst. Levofloxacin is in the same group as gatifloxacin but produced different results. The possible explanation for this difference is the structure of gatifloxacin, fourth-generation fluoroquinolones, was modified by substitution of a methoxy group at position 8 of the quinolone ring, which allows for simultaneous inhibition of both DNA gyrase and topoisomerase IV. This modification was made to increase the efficacy against microorganisms more than the third-generation form, such as levofloxacin [21]. No previous study has reported the use of this agent alone in vitro. However, it was successful at 5 mg/mL as part of combined drug treatment of bacterial coinfection in an Acanthamoeba keratitis case [22].
We have presented data showing that commercially available ophthalmic drugs differ in their ability to kill Acanthamoeba cysts. Three different genotypes of Acanthamoeba were selected based on their potential to be pathogenic strains that can cause keratitis [1]. Although our results should be confirmed in vivo studies, gentamicin and gatifloxacin may be the optimum choices for treating the early stages of eye infection caused by Acanthamoeba spp. However, not only the efficacy of drugs should be considered in AK treatment, but also issues relating to the duration of treatment and the effects of dilution by the lachrymal fluid.
References
Siddiqui R, Khan NA (2012) Biology and pathogenesis of Acanthamoeba. Parasit Vectors 5:1–13
Corsaro D, Walochnik J, Köhsler M, Rott MB (2015) Acanthamoeba misidentification and multiple labels: redefining genotypes T16, T19, and T20 and proposal for Acanthamoeba micheli sp. nov. (genotype T19). Parasitol Res 114:2481–2490
Garg G, Kalra P, Joseph J (2017) Non-contact lens related Acanthamoeba keratitis. Indian J Ophthalmol 65:1079–1086
Jongwutiwes S, Pariyakanok L, Charoenkorn M, Yagita K, Endo T (2000) Heterogeneity in cyst morphology within isolates of Acanthamoeba from keratitis patients in Thailand. Trop Med Int Health 5:335–340
Wanachiwanawin D, Booranapong W, Kosrirukvongs P (2012) Clinical features of Acanthamoeba keratitis in contact lens wearers and non-wearers. Southeast Asian J Trop Med Public Health 43:549–556
Kosrirukvongs P (1999) Treatment of Acanthamoeba keratitis with chlorhexidine. Ophthalmology 106:798–802
Rahimi F, Hashemian SMN, Tafti MF et al (2015) Chlorhexidine monotherapy with adjunctive topical corticosteroids for Acanthamoeba keratitis. J Ophthalmic Vis Res 10:106–111
Lim N, Goh D, Bunce C (2008) Comparison of polyhexamethylene biguanide and chlorhexidine as monotherapy agents in the treatment of Acanthamoeba keratitis. Am J Ophthalmol 145:130–135
Lorenzo-Morales J, Khan NA, Walochnik J (2015) An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite 22:1–20
Ghani MKA, Hoon STG, Nordin A, Hashim PNM, Suboh Y, Rahim NA (2011) In vitro susceptibility test for Acanthamoeba species isolated from clinical specimens against chlorhexidine, propamidine isethionate, gentamicin and chloramphenicol. Int Med J 18:146–148
Sunada A, Kimura K, Nishi I (2014) In vitro evaluations of topical agents to treat Acanthamoeba keratitis. Ophthalmology 121:2059–2065
Ortillés Á, Belloc J, Rubio E (2017) In-vitro development of an effective treatment for Acanthamoeba keratitis. Int J Antimicrob Agents 50:325–333
Thammaratana T, Laummaunwai P, Boonmars T (2016) Isolation and identification of Acanthamoeba species from natural water sources in the northeastern part of Thailand. Parasitol Res 115:1705–1709
Polat ZA, Vural A, Ozan F, Tepe B, Özcelik S, Cetin A (2008) In vitro evaluation of the amoebicidal activity of garlic (Allium sativum) extract on Acanthamoeba castellanii and its cytotoxic potential on corneal cells. J Ocul Pharmacol Ther 24:8–14
Palmas C, Wakelin D, Gabriele F (1984) Transfer of immunity against Hymenolepis nana in mice with lymphoid cells or serum from infected donors. Parasitol 89:287–293
Noradilah SA, Kamel Mohamed AG, Anisah N, Noraina AR, Yusof S (2014) The effectiveness of gentamicin against Acanthamoeba cysts in vitro. Mal J Med Health Sci 8:51–54
Junejo SA, Lodhi AA, Ahmed M, Kumar M, Kamal M (2013) Efficacy of gatifloxacin in acute bacterial corneal ulcer. Pak J Med Sci 29:2–7
Martín-Navarro CM, López-Arencibia A, Arnalich-Montiel F, Valladares B, Piñero JE, Lorenzo-Morales J (2013) Evaluation of the in vitro activity of commercially available moxifloxacin and voriconazole eye-drops against clinical strains of Acanthamoeba. Graefes Archi Clin Exp Ophthalmol 251:2111–2117
Durairaj C (2017) Ocular pharmacokinetics. Handb Exp Pharmacol 242:31–55
Siddiqui R, Aqeel Y, Khan NA (2016) The development of drugs against Acanthamoeba infections. Antimicrob Agents Chemother 60:6441–6450
Lorenzo JC, Francis SM (2011) Clinical use of gatifloxacin ophthalmic solution for treatment of bacterial conjunctivitis. Clin Ophthalmol 5:495–502
Kim EC, Kim MS (2009) Bilateral Acanthamoeba keratitis after orthokeratology. Cornea 29:680–682
Acknowledgements
This study was supported in part by Grants from the following: Faculty of Medicine and the Commission on Higher Education, Khon Kaen University; and the Thailand Research Fund (MRG6080065).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thongseesuksai, T., Wongwai, P., Boonmars, T. et al. Evaluating the in vitro efficacy of gatifloxacin, levofloxacin and gentamicin against Acanthamoeba cysts. Int Ophthalmol 40, 361–368 (2020). https://doi.org/10.1007/s10792-019-01188-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01188-4