Abstract
Purpose
To evaluate the results of optical biometry using the IOLMaster 500, Lenstar LS 900 and Aladdin in eyes with cataract.
Methods
In 231 eyes of 152 patients with cataract, the measurements of 3 different biometers were retrospectively compared. Paired comparisons were performed for axial length (AL), mean keratometry (mean K) and anterior chamber depth (ACD).
Results
In only 197 of the 231 eyes (85.3%), it was possible to obtain reliable measurements of AL with all the three devices. It was not possible to determine AL in 16 eyes (6.9%) with Lenstar LS 900; in 19 eyes (8.2%) with Aladdin; and in 20 eyes (8.6%) with IOLMaster 500 possibly related to the severity of lens opacification (the corneas had good transparency in the eyes included in the study). There was a statistically significant difference in AL between IOLMaster 500 and the remaining two biometers (P = 0.03). However, the amount of difference was considered clinically not significant (0.04 mm). The mean keratometry (mean K) was determined in 203 eyes (87.9%) with all the three devices. Differences in mean K were between − 0.1 and 0.06 Diopters (D), which were considered neither statistically (P > 0.05) nor clinically significant. The anterior chamber depth (ACD) was determined in 197 eyes (85.28%) with all the three biometers. The differences between the three devices (0.03 to 0.13 mm) were not statistically significant and considered also clinically not significant.
Conclusions
There were no clinically significant differences between these 3 biometers in AL, mean K and ACD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For many years, the immersion A-scan ultrasound biometry was considered the gold standard for measuring axial length (AL) and anterior chamber depth (ACD) in determining the power of the intraocular lenses (IOLs), but since the advent of optical biometers in 1999, these devices have been progressively positioned as the gold standard [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Nevertheless, in case of advanced cataracts with very opaque media, the infrared light may not penetrate and ultrasound measurements may be necessary [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29].
The fact that the AL is determined with a non-contact approach and the corneal power measured with an automated keratometer, makes optical biometry less operator-dependent and more reproducible, thus constituting a valuable tool for the modern cataract surgery. Another advantage over the ultrasound techniques is that it allows rapidly performing multiple measurements of several variables. Today there are several optical biometers available in the market [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. The IOLMaster 500 (Carl Zeiss AG, Oberkochen, Germany) uses partial coherence interferometry (PCI) with a 780 nm laser diode infrared light to measure AL. It employs a lateral slit-illumination to measure the anterior chamber depth (ACD) and determines the keratometry by analyzing 6 reference points in a hexagonal pattern at approximately 2.3 mm of optical zone [3, 10, 18, 19, 22, 24, 25]. The Lenstar LS 900 (Haag-Streit AG, Köniz, Switzerland) measures several dimensions of the eye in a single step. The technology is based on optical low-coherence reflectometry (OLCR), with an 820 nm infrared superluminescent diode. In addition to AL, the unit measures central corneal thickness (CCT), ACD, crystalline lens thickness (LT) and retinal thickness. Keratometry readings are calculated by analyzing the anterior corneal curvature at 32 reference points orientated in 2 circles at approximately the 2.30 mm and 1.65 mm optical zones [3, 6, 7, 20,21,22, 25]. The Aladdin (Topcon, Tokyo, Japan) includes a corneal topographer based on 24 Placido rings. To determine AL, the system uses an infrared superluminescent diode (830 nm wavelength). It uses a slit of light to determine the ACD [3, 8, 15, 22, 25, 27]. The purpose of this study is to evaluate different measurements of three parameters (AL, keratometry, and ACD) obtained using the IOLMaster 500, the Lenstar LS 900 and the Aladdin in eyes with different grades of cataract, and to evaluate the measurement performance of the devices in different stages of cataract, classified according the Lens Opacities Classification System (LOCS) III.
Methods
A retrospective observational study was performed, reviewing the medical records of consecutive patients scheduled for cataract extraction in one or both eyes at Centro Oftalmológico Virgilio Galvis (Floridablanca–Colombia). LOCS III system classification was used to determine the stage of the cataract. Patients were excluded from the study if they had refractive, glaucoma or retinal surgery history, ocular trauma or an active ocular infection or inflammation. In addition, eyes were excluded if corneal opacity was considered to be the cause of a failed measurement with the optical biometers. The same operator made one measurement with each biometer (IOLMaster 500, Lenstar LS 900 and Aladdin) with the standard automatic mode of each system, in the same session. If any of the parameters evaluated was not possible to determine in the first test, a second measurement was performed. No additional attempts were done. Results of AL, average keratometry (mean K) and ACD were analyzed.
Statistical analyses were performed using the statistical software Stata (version 14, StataCorp LLC, College Station, TX, USA), XLSTAT (Addinsoft SARL, Paris, France) and Analyse-it Ultimate Edition (Analyse-it Software Ltd, Microsoft Corporation, Redmond, WA, USA). A p value < 0.05 was deemed statistically significant. To evaluate the normality (Gaussian distribution) of the dataset, the Shapiro–Wilk and Anderson–Darling tests were applied; data were considered normal if the p value was more than 0.05. For data with Gaussian (normal) distribution, the central tendency of each measured parameter was described using the mean, and the statistical dispersion was recorded as the standard deviation (SD). For nonparametric data, both the median and interquartile difference were indicated. For a dataset with Gaussian distribution, the Student’s t test was used to determine if two sets measurements of a given parameter with a pair of biometers were significantly different from each other. In the case of non-normally distributed variables, the Wilcoxon signed-rank test was used.
The linear correlation between measurements with different devices was calculated using the Pearson correlation coefficient (for normally distributed data) of the Spearman’s rank correlation coefficient (for non-normally distributed data).
In order to analyze the agreement between paired measurements of a given parameter (AL, mean K, ACD) with two biometers, the Bland–Altman plot was used [30,31,32,33]. This method is based on the quantification of the agreement between two quantitative measurements by considering the mean (or the median) of the differences between each pair of measurements and determining the limits of agreement. A scatter graph of the differences between the two measurements against the averages of the same two measurements is constructed. The plot of difference against mean also permits to explore any possible association between the discrepancies and the true value (being the best estimate the mean of the two measurements of the same parameter by the two methods). If the average of the differences between the two methods is zero it means that the variability of the differences is only linked to the analytical imprecision of each of the two methods. Three horizontal lines are drawn in the plots indicating the mean of the differences (in the parametric option for data with Gaussian distribution) or the median of the differences (in the nonparametric approach for non-normally distributed dataset), and the upper and lower limits of agreement (LoA). For a dataset with Gaussian distribution, the LoA are defined as the mean difference plus and minus 1.96 times the standard deviation of the differences. For non-normally distributed dataset in order to determine the LoA, the estimation of the 2.5th and 97.5th percentiles of the differences are done. In order to consider two methods of measuring a biological variable as concordant and interchangeable, it is expected that the average difference between two methods is not different from zero, that 95% of the differences are within 1.96 of the Standard deviation of that average (or between the 2.5th and 97.5th percentiles), and that these differences are not clinically important [30,31,32,33].
In order to establish the limits how far apart measurements can be without having clinical significance is a question of judgment of the expert clinician and ideally should be defined in advance to help in the interpretation of the comparison of the different methods [31, 32]. For this study, we deemed that the limits of maximum acceptable differences would be 0.25 D for mean K, 80 microns for AL and 400 microns for ACD, differences that would reflect approximately in a difference of 0.25 D in manifest refraction as a result of the changes in the calculated intraocular lens power.
Results
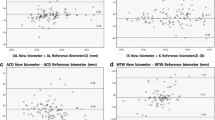
Out of 241 eyes with ocular biometry measurements available with the three devices, 238 eyes of 152 patients met the inclusion criteria but since 7 eyes were excluded due to missing data, only 231 eyes were finally analyzed. Three additional eyes were not included as they were not evaluable because of corneal opacity. Demographic information of participants is shown in Table 1. About 51.5% were left eyes (n = 119) and 48.5% right eyes (n = 112). In only 197 of the 231 eyes (85.3%), it was possible to obtain reliable measurements of AL with all the three devices. The average of AL in those eyes was 23.40 ± 1.45 mm for Lenstar LS 900; 23.40 ± 1.43 mm for Aladdin, and 23.36 ± 1.44 mm for the IOLMaster 500 (Table 2). A statistically significant differences were found when comparing IOLMaster 500 versus Lenstar LS 900 and IOLMaster 500 versus Aladdin, with an average of 0.04 mm ± 0.26 shorter measurements with IOLMaster 500 than with Lenstar LS 900 (P < 0.001), for the 197 eyes with both measurements, and 0.04 mm ± 0.13 shorter measurements with IOLMaster 500 than with Aladdin (P < 0.001), for the 191 eyes with both measurements. Those differences were considered non-clinically significant, according to the criteria previously defined. Figure 1 shows Bland–Altman plots for the agreement between the biometers for axial length. The paired correlations for AL were above 99.5%. It was not possible to measure the AL with one or more of the three devices in 34 eyes (14.7%): in 16 eyes (6.9%) with Lenstar LS 900; in 19 eyes (8.2%) with Aladdin and in 20 eyes (8.6%) with IOLMaster 500 (Table 3). The differences in the failed measurement rate between the three systems were not statistically significant. An association between the impossibility of measuring the AL with any biometer and the degree of cataract was found for nuclear color and subcapsular opacity (P = 0.0001 and P = 0.002, respectively). Failed measurements were much more frequent in cataract with LOCS III classification higher than 6.0 for nuclear color and nuclear opalescence (Table 3). The association of failures of measurements of AL with posterior subcapsular cataract was less consistent (Table 3).
Bland–Altman plots showing the agreements according to paired comparison among the three biometers on axial length measurements. (All the differences were considered non-normally distributed according to Shapiro–Wilk and Anderson–Darling tests, and thus, the medians of the differences are indicated in the central red lines). Both the means and the medians of the differences (mean/median) were very close to zero (not significant bias): − 0.04/− 0.03 mm, < − 0.001/− 0.01 mm and − 0.04/− 0.03 mm between IOLMaster 500 and Lenstar, Lenstar and Aladdin and IOLMaster 500 and Aladdin, respectively. Differences were considered not clinically significant
The mean K was determined in 203 eyes (87.9% of the total group) with all the three devices. It was not possible to measure it in 4 eyes (2%) with Lenstar LS 900; 7 eyes (3.4%) with Aladdin; and 11 eyes (5.4%) with IOLMaster 500. In 6 eyes, the mean K could not be determined with 2 biometers.
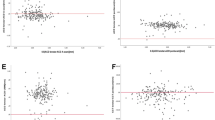
The mean K measurements were 43.95 ± 1.6 Diopters (D) for Lenstar LS 900; 43.91 ± 1.63 D for Aladdin; and 44.00 ± 1.66 D for IOLMaster 500. Paired correlation between the three biometers was 97%, and no statistically significant differences (P > 0.05) were found between the three biometers (Table 2). Figure 2 shows the agreement between the mean K values measured with the three biometers (Bland and Altman plots).
Bland–Altman plots showing the agreements according to paired comparison among the three biometers on mean keratometry measurements. (All the differences were considered non-normally distributed according to Shapiro–Wilk and Anderson–Darling tests, and thus, the medians of the differences are indicated in the central red lines). Both the means and the medians of the differences (mean/median) were very close to zero (not significant bias): − 0.04/− 0.03 D, 0.06/0.07 D and − 0.1/− 0.1 D between Lenstar and IOLMaster 500, Lenstar and Aladdin and Aladdin and IOLMaster 500, respectively. Differences were considered not clinically significant
The ACD measurement could be performed with all the three devices in 197 eyes (85.3% of the total group). It was not possible to measure ACD in 2 eyes (1%) with Lenstar LS 900, 3 eyes (1.5%) with Aladdin and in 5 eyes (2.5%) with the IOLMaster 500. In 24 eyes, the ACD could not be determined with 2 biometers. The mean depth of the anterior chamber (from the epithelium) in eyes with the three measurements was 3.1 ± 0.41 mm for the Lenstar LS 900; 3.1 ± 0.35 mm for the Aladdin; and 3.0 ± 0.41 mm for the IOLMaster 500 (Table 2). The paired correlations were above 83% being higher among the IOLMaster 500 and the Aladdin (93%). No statistically significant differences were found, except for IOLMaster 500 vs Lenstar LS 900 (P = 0.02) with an average difference of 0.13 ± 0.23 mm. Figure 3 shows the agreement between the ACD values measured with the three biometers (Bland and Altman plots).
Bland–Altman plots showing the agreements according paired comparison among the three biometers on ACD measurements (all the differences were considered non-normally distributed according to Shapiro–Wilk and Anderson–Darling tests, and thus, the medians of the differences are indicated in the central red lines). The means and the medians (mean/median) of the differences were: 0.13/0.08 mm, 0.03/0.01 mm and 0.1/0.07 mm between Lenstar and IOLMaster 500, Lenstar and Aladdin and Aladdin and IOLMaster 500, respectively. Differences were considered not clinically significant
The differences between the three biometers with regard to axial length and mean keratometry were very close to zero, showing no significant bias.
The differences in ACD between Lenstar and IOLMaster 500 (mean 0.13 mm, median 0.08 mm) and between Aladdin and IOLMaster 500 (mean 0.1 mm, median 0.07 mm) showed systematic errors. However, they were deemed not clinically significant.
There were not clear non-uniform differences, i.e., tendencies to increase or diminish the difference between devices in the extreme values of any given parameter measured.
Discussion
Currently cataract surgery reaches very good results; however, in order to meet or exceed the ever-increasing modern patient expectations, usually very high, precise IOL power calculations are a critical element. It is essential that the data entered in biometric formulas (mean K, ACD and AL, among others) are very accurate. Presently, optical biometry has become the gold standard [3, 25]; however, it is important to determine if all of the available devices are equally reliable. We found an excellent clinical correlation between three instruments of modern optical biometry (IOLMaster 500, Lenstar LS 900 and Aladdin). A statistically significant differences in the measurement of the AL were found between the IOLMaster 500 (shorter) and the other two optical biometers, Lenstar LS 900 and Aladdin (longer measurements), but only of about 0.04 mm. That would imply a discrepancy of around 0.12 D in the residual refractive error, which was considered according to our judgment, not clinically significant. Similar differences were found by Hoffer et al. and recently by Shammas et al. [18, 22] being also the measurement from the Lenstar LS900 the longer one. Buckhurst et al. [6] found also a small difference (0.06 mm) in AL measurements between the IOLMaster (version 5 software) and Lenstar LS900, which was also considered not clinically significant. In contrast with these findings, other groups have found that the AL measurements with Lenstar LS 900 were shorter than those with the IOLMaster, but again, the difference was likewise deemed not clinically significant [7, 17, 20]. Other studies have found differences that were not considered clinically significant by comparing the IOLMaster (v5.4) versus Aladdin and the IOLMaster 500 versus Aladdin in AL measurements [8, 15, 22, 26, 27].
When comparing ACD measured by IOLMaster 500 and Lenstar LS900, small statistically significant differences (around 0.1 mm) but also not significant differences (0 mm) have been reported, all of them considered clinically not significant [10, 20, 22]. No statistically significant differences have been reported between ACD measurements performed with the IOLMaster 500 and Aladdin instruments [8].
Any interference with the transmission of light can affect the results with these optical devices, especially the AL measurement. Therefore, depending on the density and location, cataracts can interfere measurements. Hill et al. [11] in 2008 reported failed measurements of AL in 7.4 and 3.7% in a group of 54 eyes using the composite mean value of 5 and 20 measurements, respectively, with the IOLMaster version 5 software. In a study published in 2009, using the IOLMaster version 5 software and Lenstar LS900 Buckhurst et al. [6] found that in 9 to 10% of the eyes the AL measurement failed. Epitropoulos in a more recent study found that it was not possible to acquire AL measurement in 16.2, 7.6 and 15.2% of eyes for the composite mean value of the standard 5 composite measurements with the IOLMaster 500, the composite mean value of 20 measurements with the IOLMaster 500, and Lenstar LS 900, respectively [7]. In addition, while the Lenstar LS 900 and the composite mean value of 5 measurements with the IOLMaster 500 methods were able to acquire AL measurements successfully in 30% of eyes with a cataract nuclear color graded > 5.0, the composite mean value of 20 measurements with the IOLMaster 500 was able to acquire AL measurements successfully in 60% of eyes with that grade of nuclear cataract [7]. In 2011, Mylonas et al. [16] reported that in 9.8% of the eyes it was not possible to obtain AL measurements with the IOLMaster V.5 and in 11.8% of the eyes with the Lenstar LS900. Most of those eyes had posterior subcapsular cataract grade 4.0 or greater according to LOCS III classification. McAlinden et al. [15] found that failure rate for the IOLMaster (v5.4) was 37.8%, and for the Lenstar LS 900 it was 35.5% when examining Chinese public hospital cataract patients. They found a statistically significant association between acquisition rates and increasing severity of posterior subcapsular cataracts with the IOLMaster and Lenstar LS 900. More than half of all eyes (51.5%) had posterior subcapsular changes more advanced than stage 3.5. The percentages of those eyes that had failed AL lectures were 46.3% with the IOLMaster and 43.0% with Lenstar LS 900 [15].
In a new study by the same group of researchers, they used a new swept-source optical coherence tomography-based biometer (OA-2000, Tomey, Nagoya, Japan) and compared it with the IOLMaster (v5.4) and Aladdin devices [27]. Overall, the failure rate of AL measurement was 0% for the OA-2000, 36.1% for the IOLMaster and 13.5% for the Aladdin. In addition, although 72 eyes had a stage greater than 3.5 of posterior subcapsular cataract, the OA-2000 could obtain measurements in all the eyes, while the IOLMaster obtained a failed measurement in 91.7% of these eyes, and the Aladdin in 59.7% of them [27]. For nuclear color stage higher than 3.5, the percentages of unobtainable measurements were 89.6% for the IOLMaster and 46.8% for the Aladdin [27]. In 2005, Freeman et al. [12] had already reported that the IOLMaster failed to acquire AL measurement in approximately about 20% in cataracts with subcapsular opacity higher to 3.5. The authors did not explain exactly what version they used; it was most probably version 5 software, since the IOLMaster 500 was released around 2009. It is striking that the percentage of non-obtainable measurements was much lower than that reported with the same instrument by Mcalinden et al. in eyes of similar characteristics.
We used the standard composite mean value of 5 measurements with IOLMaster 500. We found similar performance with the three biometers (failure rate between 6.9 and 8.6%) comparable to the 5-composite measurements reported by Hill et al., Buckhurst et al., and Mylonas et al. [15, 27] but slightly lower than those results by Epitropoulos. On the other hand, the rate of unobtainable measurements in the present study was much lower than those reported from two studies in China by McAlinden et al. even when analyzing separately eyes with advanced stages of cataract. In the present study in the subgroup of eyes with stage 4.0 or greater of nuclear color, the failure measurement rates were 12.8% for IOLMaster 500 and 11.0% for Lenstar LS 900. In the subgroup of eyes with stage 4.0 or grater of posterior subcapsular opacity, they were 16.7% and 11.9%, respectively. The differences in the percentage with the IOLMaster could be related to the fact that McAlinden et al. used a previous version of the instrument, but we do not have a possible explanation for the differences using the Lenstar LS 900. McAlinden et al. indicated that logistic regression analysis showed a statistically significant association between acquisition rates and increasing severity of posterior subcapsular cataracts with the IOLMaster, but no association was found between acquisition rates and cortical or nuclear cataracts with either device.
In our series, no association was found between cortical grade of cataract according to LOCS III and the failure of the determination of AL and not clear association was found with posterior subcapsular opacity. On the other hand, both nuclear color and nuclear opalescence were directly related to a higher probability of failure, but the effect was noticeable when the stage was 6.0 or more advanced. Between 33.3 and 55.6% of the eyes with nuclear color higher than 6.0, and between 30.7 and 46.2% with nuclear opalescence higher than 6.0, had a failed measurement of the axial length.
New devices based on swept-source optical coherence tomography have been recently marketed, as the already-mentioned OA-2000, the IOLMaster 700 (Carl Zeiss AG, Oberkochen, Germany) and the Argos (Movu Inc., Santa Clara, CA, USA). They seem to have a better performance than the previously available instruments in terms of unobtainable measurement rates [23,24,25,26,27,28,29].
In spite of these higher success rates in the measurements, it is very likely that there will be still some cases of very dense cataracts that cannot be examined with an optical biometer. In those cases, in order to perform intraocular lens power calculation, the utilization of ultrasonic immersion biometry is required.
With regard to mean K the differences in the present study were very small, and they were neither statistically nor clinically significant.
Comparing ACD measurements using IOLMaster 500 and Lenstar LS 900, a small statistically significant difference was found, but with no relevant clinical importance. (Using the Haigis formula, its impact would be around 0.08 D in manifest refraction).
As mentioned earlier, how much difference between two measurements of a given biological parameter can be tolerated without being considered to have clinical significance is a matter of clinical judgment. No statistical method can answer that question. The differences in AL and ACD that we found did not reach clinical significance according to our previously defined criteria. The performance in any degree of LOCS III classification for cataracts was slightly better with Lenstar LS 900 followed by Aladdin and IOLMaster 500, although there were not statistically significant differences. The performance of the three devices in different degrees of cataract was thus comparable.
Conclusion
The IOLMaster 500, Lenstar LS 900 and Aladdin showed very similar results of AL, mean K and ACD. We found, however, some statistically significant differences in AL and ACD measurements.
References
Haigis W, Lege B, Miller N, Schneider B (2000) Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefes Arch Clin Exp Ophthalmol 238:765–773
Kiss B, Findl O, Menapace R, Wirtitsch M, Drexler W, Hitzenberger CK et al (2002) Biometry of cataractous eyes using partial coherence interferometry: clinical feasibility study of a commercial prototype I. J Cataract Refract Surg 28:224–229
Nazm N, Chakrabarti A (2017) Update on optical biometry and intraocular lens power calculation. TNOA J Ophthalmic Sci Res 55:196–210
Holzer MP, Mamusa M, Auffarth GU (2009) Accuracy of a new partial coherence interferometry analyser for biometric measurements. Br J Ophthalmol 93:807–810
Sahin A, Hamrah P (2012) Clinically relevant biometry. Curr Opin Ophthalmol 23:47–53
Buckhurst PJ, Wolffsohn JS, Shah S, Naroo SA, Davies LN, Berrow EJ (2009) A new optical low coherence reflectometry device for ocular biometry in cataract patients. Br J Ophthalmol 93:949–953
Epitropoulos A (2014) Axial length measurement acquisition rates of two optical biometers in cataractous eyes. Clin Ophthalmol 8:1369–1376
Mandal P, Berrow EJ, Naroo SA, Wolffsohn JS, Uthoff D, Holland D et al (2014) Validity and repeatability of the Aladdin ocular biometer. Br J Ophthalmol 98:256–258
Salouti R, Nowroozzadeh MH, Zamani M, Ghoreyshi M, Salouti R (2011) Comparison of the ultrasonographic method with 2 partial coherence interferometry methods for intraocular lens power calculation. Optometry 82:140–147
Shajari M, Lehmann UC, Kohnen T (2016) Comparison of corneal diameter and anterior chamber depth measurements using 4 different devices. Cornea 35:838–842
Hill W, Angeles R, Otani T (2008) Evaluation of a new IOLMaster algorithm to measure axial length. J Cataract Refract Surg 34:920–924
Freeman G, Pesudovs K (2005) The impact of cataract severity on measurement acquisition with the IOLMaster. Acta Ophthalmol Scand 83:439–442
Rajan MS, Keilhorn I, Bell JA (2002) Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye (Lond) 16:552–556
Németh J, Fekete O, Pesztenlehrer N (2003) Optical and ultrasound measurement of axial length and anterior chamber depth for intraocular lens power calculation. J Cataract Refract Surg 29:85–88
McAlinden C, Wang Q, Pesudovs K, Yang X, Bao F, Yu A et al (2015) Axial Length Measurement Failure Rates with the IOLMaster and Lenstar LS 900 in Eyes with Cataract. PLoS ONE 10:e0128929
Mylonas G, Sacu S, Buehl W, Ritter M, Georgopoulos M, Schmidt-Erfurth U (2011) Performance of three biometry devices in patients with different grades of age-related cataract. Acta Ophthalmol 89:e237
Stattin M, Zehetner C, Bechrakis NE, Speicher L (2015) Comparison of IOL-Master 500 vs. Lenstar LS900 concerning the calculation of target refraction: a retrospective analysis. Ophthalmologe 112:444–450
Shammas HJ, Ortiz S, Shammas MC, Kim SH, Chong C (2016) Biometry measurements using a new large-coherence-length swept-source optical coherence tomographer. J Cataract Refract Surg 42:50–61
Akman A, Asena L, Güngör SG (2016) Evaluation and comparison of the new swept source OCT-based IOLMaster 700 with the IOLMaster 500. Br J Ophthalmol 100:1201–1205
Goebels S, Pattmöller M, Eppig T, Cayless A, Seitz B, Langenbucher A (2015) Comparison of 3 biometry devices in cataract patients. J Cataract Refract Surg 41:2387–2393
Gao R, Chen H, Savini G, Miao Y, Wang X, Yang J et al (2017) Comparison of ocular biometric measurements between a new swept-source optical coherence tomography and a common optical low coherence reflectometry. Sci Rep 7:2484
Hoffer KJ, Shammas HJ, Savini G (2010) Comparison of 2 laser instruments for measuring axial length. J Cataract Refract Surg 36:644–648
Hua Y, Qiu W, Xiao Q, Wu Q (2018) Precision (repeatability and reproducibility) of ocular parameters obtained by the Tomey OA-2000 biometer compared to the IOLMaster in healthy eyes. PLoS ONE 13:e0193023
Kunert KS, Peter M, Blum M, Haigis W, Sekundo W, Schütze J et al (2016) Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer versus partial coherence interferometry and optical low-coherence reflectometry. J Cataract Refract Surg 42:76–83
Turczynowska M, Koźlik-Nowakowska K, Gaca-Wysocka M, Grzybowski A (2016) Effective ocular biometry and intraocular lens power calculation. European Ophthalmic Review 10:94–100
Hoffer KJ, Shammas HJ, Savini G, Huang J (2016) Multicenter study of optical low-coherence interferometry and partial-coherence interferometry optical biometers with patients from the United States and China. J Cataract Refract Surg 42:62–67
McAlinden C, Wang Q, Gao R, Zhao W, Yu A, Li Y, Guo Y, Huang J (2017) Axial length measurement failure rates with biometers using swept-source optical coherence tomography compared to partial-coherence interferometry and optical low-coherence interferometry. Am J Ophthalmol 173:64–69
Higashiyama T, Mori H, Nakajima F, Ohji M (2018) Comparison of a new biometer using swept-source optical coherence tomography and a conventional biometer using partial coherence interferometry. PLoS ONE 13:e0196401
Savini G, Hoffer KJ, Shammas HJ, Aramberri J, Huang J, Barboni P (2017) Accuracy of a new swept-source optical coherence tomography biometer for IOL power calculation and comparison to IOLMaster. J Refract Surg 33:690–695
Altman DG, Bland JM (1983) Measurement in medicine: the analysis of method comparison studies. Statistician 32:307–317
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160
Giavarina D (2015) Understanding Bland Altman analysis. Biochem Med (Zagreb) 25:141–151
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they do not have any conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethical committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ortiz, A., Galvis, V., Tello, A. et al. Comparison of three optical biometers: IOLMaster 500, Lenstar LS 900 and Aladdin. Int Ophthalmol 39, 1809–1818 (2019). https://doi.org/10.1007/s10792-018-1006-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-1006-z