ABSTRACT
D-limonene epoxidation generates (+)-limonene epoxide, an understudied compound in the pharmacologically point of view. Herein, we investigated the anti-inflammatory and antinociceptive potentialities of (+)-limonene epoxide and suggested a mechanism of action. The anti-inflammatory potential was analyzed using agents to induce paw edema, permeability, and myeloperoxidase (MPO) activity. Pro-inflammatory cytokines and cell migration of peritoneal cells were also assessed. Antinociceptive effects were evaluated by writhing test induced by acetic acid, formalin, and hot plate assays and contribution of opioid pathways. Pretreated animals with (+)-limonene epoxide showed reduced carrageenan-induced paw edema in all doses (25, 50, and 75 mg/kg) (P < 0.05). At 75 mg/kg, it suppressed edema provoked by compound 48/80, histamine, prostaglandin E2, and serotonin and reduced permeability determined by Evans blue and MPO activity. It also reduced leukocytes, neutrophils, and IL-1β levels in the peritoneal cavity in comparison with carrageenan group (P < 0.05). (+)-Limonene epoxide diminished abdominal contortions induced by acetic acid (78.9%) and paw licking times in both 1 (41.8%) and 2 (51.5%) phases and a pretreatment with naloxone (3 mg/kg) reverted the antinociceptive action in morphine- and (+)-limonene epoxide-treated groups (P < 0.05). Additionally, it enlarged response times to the thermal stimulus after 60 and 90 min. In conclusion, (+)-limonene epoxide inhibited release/activity of inflammatory mediators, vascular permeability, migration of neutrophils and displayed systemic and peripheral analgesic-dependent effects of the opioid system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Between 1981 and 2010, 1073 new chemical entities (New Chemical Entities—NCEs) were approved as drug by the Food and Drug Administration (FDA) of the USA and 64% of them are natural, derived, or synthesized molecules based on natural compounds. The interest in molecular modeling, combinatorial chemistry, and other chemical synthesis techniques associated with products from nature and medicinal chemistry are responsible for the most new therapeutic agents against infections (fungal, bacterial, or parasitic), disease vectors, cancer, dyslipidemia, immunomodulation, and inflammatory disorders [1–7].
Inflammation can be defined as a fundamental defense reaction of the body against invasion of pathogens or injury. It is characterized as a matrix for enzyme activation, mediator release, extravasation, cell migration, tissue breakdown, and repair [8]. Pain, redness, swelling, and loss of function are classic signs of inflammation that are produced by inflammatory agents, such as nitric oxide, prostaglandins, bradykinin, serotonin, histamine, and leukotrienes [9]. Some of them act as neuromodulators, generating sustained activation of nociceptors and sensitization of primary and higher order neurons involved in pain transmission [10].
In general, the medication therapy used to treat inflammation and their signals is base on non-steroidal anti-inflammatory drugs (NSAIDs). These drugs are effective in a wide range of process conditions that involves pain and inflammation. However, they can induce gastrointestinal effects, water retention, liver and kidney toxicity, and skin allergic phenomena when chronically used. There is also the risk of NSAIDs to trigger asthma attacks due to non-selective inhibition of constitutive isoform (COX-1) and inducible (COX-2) of the enzyme cyclooxygenase (COX) [11]. In this context, natural, derived, or synthesized molecules based on natural compounds emerge as new therapeutic options that allow the development and introduction of effective and safer pharmaceutical alternatives to treat pain and inflammatory correlated conditions.
Among derivatives of medicinal plants, it is important to highlight biological activities of mixtures of essential oils, which are constituted, among other compounds, by terpenes [12, 13]. Limonene (4-isoprenyl-1-methyl-cyclohexene), for example, is a monocyclic monoterpene found in essential oils of several species of aromatic plants, such as Lippia alba and Artemisia dracunculus, and is present in the essential oils of citric fruits as lemon, orange, and tangerine [14]. Due to its citrus odor, limonene is widely used as fragrance in perfumes, soaps, food, and beverages and is listed in the Code of Federal Regulations as generally recognized as safe (GRAS) for a flavoring agent and can be found in common food items [15].
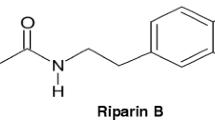
Studies demonstrated biological effects of limonene, including anti-inflammatory, gastroprotective [16], chemopreventive against breast, lung, skin and liver [17], antinociceptive, and hypoglycemic [14, 18]. In view of its low water solubility and tendency to autoxidation and polymerization, limonene became a suitable industrial by-product for bioconversions with high-value commercial purposes [18]. From this perspective, the epoxidation reaction of (+)-limonene was performed with m-chloroperbenzoic acid, which is used in the epoxidation of unfunctionalized olefins. Limonene double bond (C=C) of is nucleophilic and react with this peracid, which acts as an electrophile [19] resulting in the generation of (+)-limonene epoxide (Fig. 1). Thus, the present study investigated the antinociceptive and anti-inflammatory potential of (+)-limonene epoxide in mice and suggested a possible mechanism of action for its therapeutic action.
MATERIAL AND METHODS
Drugs and Reagents
Some drugs and reagents used (λ-carrageenan, histamine, serotonin, compound 48/80, prostaglandin E2, Evans blue, acetic acid, and formaldehyde) were purchased from Sigma Chemical (St. Louis, MO, EUA). Heparin, indomethacin, and morphine were obtained from Merck (São Paulo, SP, Brazil). All drugs were dissolved in sterile 0.9% NaCl (vehicle). A mixture of cis and trans (+)-limonene epoxide was prepared as described by [20], and emulsified with 0.05% Tween 80 (Sigma Chem. Co. St. Louis, MO, EUA) dissolved in 0.9% saline (vehicle).
Animals
Adult male Swiss mice (Mus musculus Linnaeus, 1758) were obtained from the animal facilities of the Universidade Federal do Piauí (UFPI), Teresina, Brazil. They were kept in well-ventilated cages under standard conditions of light (12:12-h light/dark cycle) and temperature (23 ± 2 °C) and were housed with free access to commercial rodent stock diet (Purina, Campinas, Brazil). Animals were randomly divided into groups (n = 5/group) before the studies.
Evaluation of Anti-inflammatory Effects
Mice were pretreated intraperitoneally with 0.05% Tween 80 dissolved in 0.9% saline (vehicle) or (+)-limonene epoxide (25, 50, and/or 75 mg/kg). Indomethacin (10 mg/kg) was used as reference drug.
Paw Edema Induced by Carrageenan
The animals were randomly divided into six groups (n = 5), and edema was induced by injection of 50 μL of a suspension of carrageenan (500 μg/paw) in vehicle solution into the right hind paw (group II). Mice were pretreated with vehicle (group I, untreated control), indomethacin 10 mg/kg (group III, reference drug), or (+)-limonene epoxide (25, 50, and 75 mg/kg for groups IV, V, and VI, respectively). Paw volume was measured before (V 0) and at 1, 2, 3, and 4 h after carrageenan treatment (V t ) using a plethysmometer (Panlab, Barcelona, Spain). The effect of pretreatment was calculated as percent inhibition of edema relative to the paw volume of the vehicle group using the following formula [21, 22].
Paw Edema Induced by Other Phlogistic Agents
Paw edema was also induced by the compound 48/80 (12 μg/paw), serotonin (1% w/v), histamine (100 ng/paw), or PGE2 (3 nmol/paw). Animals were pretreated 1 h before of each phlogistic agent with vehicle or (+)-limonene epoxide (75 mg/kg). Paw volume was measured before (V 0) and 0.5, 1, 1.5, and 2 h after the stimulus as described below.
Permeability Induced by the Compound 48/80 and Myeloperoxidase Activity
Animals were pretreated 1 h before of each phlogistic agent with vehicle or (+)-limonene epoxide (75 mg/kg). Vascular permeability was evaluated 30 min after the administration of the compound 48/80 by the Evan’s blue test [23]. It was injected 2.5% Evans blue (25 mg/kg) intravenously through retro orbital plexus 30 min before the compound 48/80. Paw was collected, weighed, and placed in glass tubes containing a solution of formamide (1 mL/paw) at 37 °C for 72 h to extract the dye. The amount of dye was measured at 630 nm using a standard curve of Evans blue.
Afterwards, paw tissue was homogenized in potassium phosphate buffer containing 0.5% hexadecyltrimethyl ammonium bromide and centrifuged at 4500 rpm for 15 min at 4 °C. The pellet was resuspended, and activity of MPO was determined at 450 nm using o-dianisidine dihydrochloride and 1% hydrogen peroxide [24]. One unit of MPO was defined as the amount of MPO capable of breaking 1 mmol of peroxide/min and data were reported in units per milligram of tissue (U/mg tissue).
Cell Migration and Measurement of Cytokines
Mice received vehicle or (+)-limonene epoxide (75 mg/kg) 60 min before the administration of carrageenan (250 μL in 500 μg/cavity). Animals were euthanized (sodium pentobarbital 150 mg/kg, i.p.) 4 h after carrageenan administration. Peritoneal cavity was washed with 1.5 mL of phosphate-buffered saline (PBS). Total cell counting was performed in a Neubauer chamber. Differential cell counting (total 100 cells) was performed on slides prepared in cytocentrifuge and stained with hematoxylin. Results were presented as number of cells per milliliter of peritoneal exudate.
Concentrations of tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) were determined by enzyme-linked immunosorbent assay (ELISA) using commercially available kits following the manufacturer’s instructions (DuoSet ELISA development kit R&D Systems, Minneapolis, MN, EUA). Results were expressed as cytokine picograms per milligram of tissue inducer (pg/mg protein) [25].
Evaluation of Antinociceptive Effects
Negative control group received 0.05% Tween 80 dissolved in 0.9% saline (vehicle). Experimental group mice received (+)-limonene epoxide 75 mg/kg intraperitoneally. Positive control group was subcutaneously injected with morphine (5 mg/kg, s.c.).
Writhing Test Induced by Acetic Acid
Mice received 0.05% Tween 80, dissolved in 0.9% saline (vehicle) or (+)-limonene epoxide (75 mg/kg) or morphine 60 min before administration of 0.6% acetic acid (10 mL/kg, i.p.). After 10 min, number of constrictions was recorded during 20 min, including abdominal muscle contraction and extension of hind paw [26].
Formalin Test
Mice received 0.05% Tween 80, dissolved in 0.9% saline (vehicle) or (+)-limonene epoxide (75 mg/kg) or morphine 60 min before administration of 2.5% formalin (20 μL/paw). Animals were observed for 5 min after formalin injection, which corresponds to a direct chemical stimulation of nociceptors (phase 1 of the inflammatory process). Phase 2 involves inflammatory mediator release and was observed from 20 to 25 min after formalin injection [27].
Evaluation of Opioid Pathways Participation in the Antinociceptive Effect of (+)-Limonene Epoxide
The mice received 0.05% Tween 80, dissolved in 0.9% saline (vehicle) or naloxone (3 mg/kg, s.c.; opioid antagonist). After 30 min, it was administered (+)-limonene epoxide (75 mg/kg) or morphine (opioid agonist). One hour later, it was administered 2.5% formalin (20 μL/paw). Licking times from 0 to 5 min were recorded.
Hot Plate Assay
Mice received 0.05% Tween 80, dissolved in 0.9% saline (vehicle) or (+)-limonene epoxide (75 mg/kg) or morphine (5 mg/kg, s.c., positive control). Measurements were performed before in time zero and 30, 60, 90, and 120 min after the treatment with a cutting time of 45 s to prevent the development of paw lesions [28]. Each animal was placed on a hot plate (55 ± 1 °C) (Model FEP-361, Insight, São Paulo, Brazil) and reaction time was noted as paw licking or jumping and response latency.
Statistical Analysis
In order to determine differences between groups, data (mean ± S.E.M.) were compared by one-way analysis of variance (ANOVA) followed by Student Newman-Keuls test (P < 0.05) using GraphPad Prism® software.
RESULTS
Anti-inflammatory Effects of (+)-Limonene Epoxide
Paw Edema Induced by Carrageenan in Mice
With exception for doses of 25 mg/kg after 1 and 2 h of treatment (P < 0.05), all doses (25, 50, and 75 mg/kg) and times (1, 2, 3, and 4 h) analyzed reduced carrageenan-induced paw edema significantly [25 mg/kg at 3 and 4 h: 53.1 and 80.9%; 50 mg/kg: 74.1, 41.6, 71.6, and 92.8%; 75 mg/kg: 82.7, 84.4, 86.4, and 64.3%, respectively] (P < 0.05) (Table 1). Interestingly, doses of 50 and 75 mg/kg were similar or more active than indomethacin (P < 0.05). For next steps, the dose of 75 mg/kg was chosen to detail additional aspects related to the anti-inflammatory and analgesic mechanisms of (+)-limonene epoxide.
Paw Edema Induced by Compound 48/80, Histamine, Prostaglandin E2, and Serotonin
The compound (+)-limonene epoxide at 75 mg/kg reduced significantly the paw edema induced in all protocols and times (30, 60, 90, and 120 min) when compared with paw edema inducer groups, respectively: (a) compound 48/80: 38.4, 50.0, 54.0, and 70% (Fig. 2a); (b) histamine: 36.8, 72.4, and 58.7% (Fig. 2b), but it was not observed early reduction of edema in the first 30 min; (c) PGE2: 31.0, 33.5, 40.0, and 25.0% (Fig. 2c); (d) serotonin: 34.8, 92.0, 34.0, and 19.6% (P < 0.05). Indomethacin (10 mg/kg) was used as reference drug and showed significant reduction of paw edema of mice in all analysis performed (Fig. 2a–d) (P < 0.05).
Effects of (+)-limonene epoxide (75 mg/kg) on paw edema induced by compound 48/80 (a), histamine (b), prostaglandin E2 (c), and serotonin (d). Results are expressed as mean ± standard error of measurement (S.E.M.) (n = 5 animals/group). Indomethacin was used as drug reference (10 mg/kg). *P < 0.05 compared to vehicle (0.05% Tween 80 dissolved in 0.9% saline) by ANOVA followed by Student Newman-Keuls test; **P < 0.05 compared to the paw edema inducer group (48/80, histamine, PGE2, or serotonine) by ANOVA followed by Student Newman-Keuls test.
Permeability Induced by Compound 48/80, Peritonitis Induced by Carrageenan and Levels of Myeloperoxidase Activity, TNF-α, and IL-1β
Animals treated with (+)-limonene epoxide (75 mg/kg) revealed reduction in extravasation of Evans blue (0.176 ± 0.02 μg/mg) when compared with compound 48/80-treated mice (0.215 ± 0.01 μg/mg) and vehicle (0.04 ± 0.004 μg/mg) (P < 0.05).
Figure 3a shows the influence of (+)-limonene epoxide on MPO activity followed by paw edema induced by carrageenan. Mice paw homogenates from (+)-limonene epoxide-treated animals at 75 mg/kg showed reduction (64%) in MPO activity (36.0 ± 4.8 Units of MPO/mg tissue) in comparison with carrageenan group (99.7 ± 9.3 Units of MPO/mg tissue) and in similar extents to those found with indomethacin (25.1 ± 9.3 Units of MPO/mg tissue) (P < 0.05).
Effects of (+)-limonene epoxide (75 mg/kg) on myeloperoxidase activity from paw tissue (a), cellular migration of inflammatory peritoneal cells (b), and levels of interleukin-1β and tumor necrosis factor-α from peritonitis (c) induced by carrageenan. Results are expressed as mean ± standard error of measurement (S.E.M.) (n = 5 animals/group). Indomethacin was used as drug reference (10 mg/kg). *P < 0.05 compared to vehicle (0.05% Tween 80 dissolved in 0.9% saline) by ANOVA followed by Student Newman-Keuls test; **P < 0.05 compared to the paw edema inducer group by ANOVA followed by Student Newman-Keuls test.
Pretreatment with (+)-limonene epoxide also reduced total number of leukocytes (5.03 ± 0.38 × 103/mL) and neutrophils (3.76 ± 0.27 × 103/mL) in the peritoneal cavity of mice in comparison with animals from carrageenan group, whose counting showed intense cellular infiltration 4 h after such stimulus (15.22 ± 1.84 and 6.06 ± 0.61 × 103/mL) and significant increasing when compared to the vehicle (0.69 ± 0.10 and 0.16 ± 0.02 × 103/mL, respectively) (P < 0.05). Indomethacin (10 mg/kg) also reduced cell migration of inflammatory cells (leukocytes, 5.02 ± 0.33 × 103/mL; neutrophils, 2.39 ± 0.23 × 103/mL) (P < 0.05) (Fig. 3b).
Intraperitoneal administration of carrageenan induced an evident increase in IL-1β (1046.0 ± 34.5 pg/mL) and TNF-α (155.6 ± 22.9 pg/ml) levels in the peritoneal exudate (Fig. 3c). Pretreatment with (+)-limonene epoxide reduced IL-1β (750.0 ± 79.9 pg/mL) levels (P < 0.05), but it did not alter TNF-α (155.3 ± 14.4 pg/mL) concentration when compared to the carrageenan group.
Antinociceptive Effects of (+)-Limonene Epoxide
Abdominal Contortions Test Induced by Acetic Acid
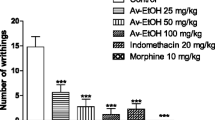
The compound (+)-limonene epoxide (75 mg/kg) reduced (78.9%) the number of contortions (12.0 ± 5.3, Fig. 4a) in comparison with vehicle group (56.4 ± 8.9). Morphine was also greatly efficient to block pain induced by acetic acid (0.2 ± 0.4) (P < 0.05).
Effects of (+)-limonene epoxide (75 mg/kg) on writhing’s number induced by acetic acid (a), paw licking time induced by formalin [(b) phase 1, (c) phase 2], and on latency of hind paw licking elicited following a thermal stimulus (d). Results are expressed as mean ± standard error of measurement (S.E.M.) (n = 5 animals/group). Morphine was used as drug reference (5 mg/kg). Naloxone (3 mg/kg) was used to antagonize the opioid system. *P < 0.05 compared to vehicle (0.05% Tween 80 dissolved in 0.9% saline) by ANOVA followed by Student Newman-Keuls test; **P < 0.05 between Formalin + Limonene epoxide and Formalin + Limonene epoxide + Naloxone compared by ANOVA followed by Student Newman-Keuls test.
Involvement of Opioid System
In the formalin test, the (+)-limonene epoxide reduced paw licking time in both phases 1 and 2 evaluated, showing reduction of 41.8% (41.8 ± 5.7 s) and 51.5% (34.1 ± 12.1 s) when compared to the vehicle group (71.9 ± 9.1 and 70.4 ± 11.1 s), respectively (Fig. 4b, c). As expected, morphine (5 mg/kg) also decreased significantly the licking time in both phases (phase 1, 5.5 ± 1.6 s; phase 2, not detected). Naloxone (3 mg/kg), an antagonist of opioid system, reverted the antinociceptive action in morphine- and (+)-limonene epoxide-treated groups (P < 0.05).
Animals pretreated with (+)-limonene epoxide increased response times to the thermal stimulus after 60 min (25.2 ± 1.1 s) and 90 min (18.4 ± 1.2 s) following administration when compared to the time zero (8.6 ± 3.2 and 7.4 ± 3.4 s, respectively) (P < 0.05). Statistically significant outcomes were seen with morphine in all intervals analyzed (Fig. 4d).
DISCUSSION
Inflammation and pain are cause or consequence of most diseases and have associated in virtually all human disorders, such as autoimmune, gastrointestinal, neurodegenerative, and respiratory diseases, cancers, and infections [9, 28, 29]. In this context, the process of pain can be a pathophysiological consequence of various morbidities and their consequences. These can lead to disabilities, impairing quality of life and psychosocial and economic effects [30]. To relieve pain to turn the treatment of a disease a less traumatic process is a critical approach and the search for new pharmacological tools has a long history in the pharmaceutical sciences. In last years, D-limonene epoxidation generated (+)-limonene epoxide, an understudied compound in the pharmacologically point of view. Recent results showed its antioxidant [31], anxiolytic [32], and anthelmintic [33] properties. Herein, we are described the first in vivo evidences for its anti-inflammatory and antinociceptive activities.
Carrageenan-induced paw edema in rodents is a well-established model for screening molecules with anti-inflammatory activity. Carrageenan is a linear sulfated polysaccharide derived from red algae with robust inflammatory properties. After the injection of carrageenan, the edema is established for 4 h, and it can last up to 96 h [34–36]. Intermediary (50 mg/kg) and high acute doses (75 mg/kg) of (+)-limonene epoxide were capable to reduce paw edema, with inhibition percentage values of paw swelling superior than positive control indomethacin in some intervals of the study. Based on these findings, the dose of 75 mg/kg was selected to detail additional aspects related to the anti-inflammatory and analgesic mechanisms of (+)-limonene epoxide.
Following the carrageenan injection on the rat’s paw, some mediators are sequentially released in the early phase (0–1 h), including histamine, serotonin, and bradykinin, whose releasing raises vascular permeability in later phases (1–6 h), there are intensification in the production of prostaglandins by activation of cyclooxygenase-2, release of nitric oxide, and strong infiltration of neutrophils [37–40]. So, to elucidate the mechanism of action for (+)-limonene epoxide, we induced paw edema by compound 48/80, serotonin, histamine, and prostaglandin E2.
The compound 48/80 acts on mast cell degranulation of inflammatory mediators accumulated into cytoplasmic vesicles, causing the release of histamine, serotonin, leukotrienes, and a variety of cytokines that are associated with inflammatory events [41]. Histamine and serotonin are the principal mediators involved in the dextran-induced paw edema, and their release is a result of mast cell degranulation [37]. Prostaglandins, on the other hand, are immediately synthesized and released in substantial quantities in sites of inflammation. They act in vasodilation, induce production of pro-inflammatory cytokines, including IL-1β and TNF-α, and chemoatract various inflammatory molecules for leukocytes [39]. In all protocols performed, (+)-limonene epoxide at 75 mg/kg was able to minimize the inflammatory process, suggesting it might suppress edema formation by the inhibition of inflammatory mediator substances. Subsequently, the (+)-limonene epoxide action was assessed on vascular permeability induced by compound 48/80, measurement of MPO, and levels of IL-1β and TNF-α (Fig. 5).
Myeloperoxidase is an abundant enzyme found in azurophilic granules of neutrophils, whose contents are released after their activation within the phagosome or in the extracellular space. The MPO activity is directly proportional to neutrophil chemotaxis and infiltration in inflamed tissues [42, 43]. (+)-Limonene epoxide reduced appreciably the permeability assessed by Evans blue and myeloperoxidase activity. Since MPO is an indirect marker of tissue neutrophil infiltration, its decline indicates less neutrophil infiltration [44] and such findings were confirmed by failure or impairment of leukocyte and neutrophil migration to the peritoneal cavity.
From the histological point of view, the inflammatory process involves a complex series of events, in which it is included vasodilation post-capillaries that leads to increased permeability and blood proteins flow, exudation of fluid and plasma, and migration of polymorphonuclear leukocytes [45]. This latter phenomenon is essential factor in the acute inflammatory process and considered as the first line of cellular defense [37, 46].
Carrageenan-induced peritonitis technique allows the quantification of leukocytes that migrate into the peritoneal cavity by action of chemotactic agents. This migration is sensitive to non-steroidal anti-inflammatory, such as indomethacin [47]. Such peri- tonitis involves exudation and production of mediators such as nitric oxide and cytokines (IL-1β and TNF-α) (LIMA et al., 2012). Then, the effect of (+)-limonene epoxide was evaluated on levels of IL-1β and TNF-α in the peritoneal exudate of mice with carrageenan-induced peritonitis.
Compound (+)-limonene epoxide diminished concentrations of IL-1β but TNF-α levels were not altered. IL-1β is released primarily by monocytes, macrophages, and mast cells as well as by nonimmune cells, from keratinocytes, fibroblasts, synoviocytes, endothelial, neuronal, and glial cells (Schwann cells, microglia, and astrocytes), during cell injury, infection, invasion, and inflammation. So, overproduction of IL-1β is implicated in the pathophysiological changes that occur during different disease states, such as rheumatoid arthritis, neuropathic pain, inflammatory bowel disease, osteoarthritis, vascular disease, multiple sclerosis, and Alzheimer’s and Parkinson’s diseases [48, 49].
The antinociceptive action of (+)-limonene epoxide was also investigated since mediators produced in inflammation sites can produce pain by activation or sensitization of nociceptors adjacent to the injured tissue. IL-1β, IL-6, and TNF-α are pro-inflammatory cytokines found to increase the production of substance P and PGE2 in a number of neuronal and glial cells, contribute to the development of neuropathic pain behavior following a peripheral nerve injury, and induce tactile allodynia and thermal hyperalgesia [48, 50].
The abdominal contortions technique induced by acetic acid is a visceral pain model with its high sensitivity and low specificity very used to evaluate the antinociceptive activity of new drugs [34, 51, 52]. The local irritation caused by intraperitoneal administration of such agent triggers the release of mediators, such as bradykinin, substance P and PGs, as well as cytokines such as IL-1β, TNF-α, and IL-8. These mediators activate chemosensitive nociceptors, which contribute to the development of inflammatory pain and vascular permeability. Certainly, (+)-limonene epoxide inhibited mice nociceptive response to acetic acid in a significant manner by suppression of inflammatory pain through the inhibition of release/activity of inflammatory mediators [34] which declined vascular permeability during the initial exudative inflammation [37]. Its inhibition may contribute to the reduction of edema formation and to decrease the migration of neutrophils.
Next, additional hot plate studies were carried out to verify central effects of (+)-limonene epoxide. Jumping or licking paws are indicative of response to thermic nociceptive stimulation. Diminution of such parameters is interpreted as antinociceptive effect [10], implying that (+)-limonene may act as an analgesic substance after 60 and 90 min.
The formalin test is used as a more specific pain inducer and triggers two distinct periods with different nociceptive mechanisms. Response in the first stage is a consequence from immediate release of the excitatory amino acids glutamate and aspartate and intense increase in activity of primary afferent fibers. On the other hand, reactions in the second stage result from the extensive activation of primary afferent neurons in a low and continuous way by sensory neuropeptides like substance P at the spinal cord [53]. Opioid analgesics, such as morphine, suppress both early and late phases of the formalin test, while NSAIDs mainly act on the late and peripheral inflammatory [54]. So, it was shown that (+)-limonene epoxide as well as morphine alleviated both phases, suggesting possible peripheral and central antinociceptive mechanisms of the semisynthetic terpene. This hypothesis was supported by the reversion of the analgesic action of (+)-limonene epoxide in animals pretreated with naloxone, an antagonist of receptor 2 opioid. So, findings with formalin test corroborated those results obtained with the hot plate method and amplified the time for lickings.
CONCLUSIONS
In conclusion, (+)-limonene epoxide inhibited inflammation in mice due to its inhibition of release/activity of inflammatory mediators, declined vascular permeability, decreases migration of neutrophils, and displayed systemic and peripheral analgesic-dependent effects on the opioid system. Since it presents great advantages due to its biodegradable characteristics, readiness of production, and economic viability to obtain them on an industrial scale, it arises as a promising molecule to treat inflammation and pain-related disorders.
REFERENCES
Butler, M.S. 2014. The role of natural product chemistry in drug discovery. Journal of Natural Products 67: 2141–2153.
Balunas, M.J., and A.D. Kingnorn. 2005. Drug discovery from medicinal plants. Life Sciences 78: 431–441.
Srivastava, A.S., J.K. Negi, M. Gupta Kumar, and S.P.S. Khanuja. 2005. Plant-based anticancer molecules: a chemical and biological profile of some important leads. Bioorganic & Medicinal Chemistry 13: 5892–5908.
Farias, D.F., T.M. Souza, M.P. Viana, B.M. Soares, A.P. Cunha, I.M. Vasconcelos, N.M. Ricardo, P.M.P. Ferreira, V.M.M. Melo, and A.F.F.U. Carvalho. 2013. Antibacterial, antioxidant, and anticholinesterase activities of plant seed extracts from Brazilian semiarid region. BioMed Research International 2013: 1–9.
Pereira, J.B.A., M.M. Rodrigues, I.R. Morais, C.R.S. Vieira, J.P.M. Sampaio, M.G. Moura, M.F.M. Damasceno, J.N. Silva, I.B.F. Calou, F.A. Deus, A.P. Peron, M.C. Abreu, G.C.G. Militão, and P.M.P. Ferreira. 2005. O papel terapêutico do Programa Farmácia Viva e das plantas medicinais no centro-sul piauense. Revista Brasileira de Plantas Medicinais 17: 550–561.
Simoes, E.R.B., E.A. Santos, M.C. Abreu, J.N. Silva, N.M.F. Nunes, M.P. Costa, O.D.L. Pessoa, C. Pessoa, and P.M.P. Ferreira. 2015. Biomedical properties and potentiality of Lippia microphylla Cham. and its essential oils. Journal of Intercultural Ethnopharmacology 4: 256–263.
Ferreira, P.M.P., D.P. Bezerra, J.N. Silva, M.P. Costa, J.R.O. Ferreira, N.M.N. Alencar, I.S.T. Figueiredo, A.J. Cavalheiro, C.M.L. Machado, R. Chammas, A.P.N.N. Alves, M.O. Moraes, and C. Pessoa. 2016. Preclinical anticancer effectiveness of a fraction from Casearia sylvestris and its component Casearin X: in vivo and ex vivo methods and microscopy examinations. Journal of Ethnopharmacology 186: 270–279.
Jukanti, R., G. Devaraj, R. Devaraj, and S. Apte. 2011. Drug targeting to inflammation: studies on antioxidant surface loaded diclofenac liposomes. International Journal of Pharmaceutics 414: 179–185.
Zygmunt, M., G. Chłoń-Rzepa, and J. Sapa. 2014. Analgesic and anti-inflammatory activity of 7-substituted purine-2,6-dione. Pharmacological Reports 66: 996–1002.
Silva, J.C., S.R.G.L. Saraiva, R.G. Oliveira-Júnior, and J.R.G.S. Almeida. 2013. Experimental models for evaluation of antinociceptive activity of natural products: a review. Brazilian Journal of Pharmacognosy 94: 18–23.
Quintans-Júnior, L.J., A.G. Guimarães, M.T. Santana, B.E.S. Araújo, F.V. Moreira, L.R. Bonjardim, A.S.S. Araújo, J.S. Siqueira, A.R. Antoniolli, M.A. Botelho, J.R.G.S. Almeida, and M.R.V. Santos. 2011. Citral reduces nociceptive and inflammatory response in rodents. Brazilian Journal of Pharmacognosy. 21: 497–502.
Burt, S. 2004. Essential oils: their antibacterial properties and potential applications in foods—a review. International Journal of Food Microbiology 94: 223–253.
Raut, J.S., and S.M. Karuppayil. 2014. A status review on the medicinal properties of essential oils. Industrial Crops and Products 62: 260–264.
Amaral, J.F., M.I. Silva, M.R. Neto, P.F. Neto, B.A. Moura, C.T. Melo, F.L. Araújo, P.F. Vasconcelos, S.M. Vasconcelos, and F.C. Sousa. 2007. Antinociceptive effect of the monoterpene R-(+)-limonene in mice. Biological and Pharmaceutical Bulletin 30: 1217–1220.
Sun, J. 2007. D-Limonene: safety and clinical applications. Alternative Medicine Review 12: 259–264.
Rozza, A.L., T.M. Moraes, H. Kushima, A. Tanimoto, M.O. Marques, T.M. Bauab, C.A. Hiruma-Lima, and C.H. Pellizzon. 2011. Gastroprotective mechanisms of Citrus lemon (Rutaceae) essential oil and its majority compounds limonene and β-pinene: involvement of heat-shock protein-70; vasoactive intestinal peptide; glutathione; sulfhydryl compounds; nitric oxide and prostaglandin E2. Chemico-Biological Interactions 189: 82–89.
Murali, R., and S. Ramalingam. Antidiabetic effect of d-limonene, a monoterpene in streptozotocin-induced diabetic rats. Biomedicine & Preventive Nutrition 2:269–275.
Maróstica-Júnior, M.R., and G.M. Pastore. 2007. Biotransformation of limonene: a review of the main metabolic pathways. Quimica Nova 30: 382–387.
Von Honlleben, M.L.A., and C.M. Schuch. 1997. Activating agents of the hydrogen peroxide in the epoxidation of unfunctionalized alkenes. Quimica Nova 20: 58–71.
Thomas, A.F., and Y. Bessiére. 1989. Limonene. Natural Products Reports 291–309.
Winter, C.A., E.A. Risley, and G.W. Nuss. 1962. Carrageenan-induced oedema in the hind paw of rat as an assay for anti-inflammatory activity. Proceedings of the Society for Experimental Biology and Medicine 111: 544–547.
Silva, R.O., M.S. Salvadori, F.B.M. Sousa, M.S. Santos, N.S. Carvalho, D.P. Sousa, B.S. Gomes, F.A. Oliveira, A.L.R. Barbosa, R.M. Freitas, R.N. De Almeida, and J.R. Medeiros. 2014. Evaluation of the anti-inflammatory and antinociceptive effects of myrtenol, a plant derived monoterpene alcohol, in mice. Flavour and Fragrance Journal 29: 184–192.
Radu, M., and J. Chernoff. 2013. An in vivo assay to test blood vessel permeability. Journal of Visualized Experiments 16, e50062.
Bradley, P.P., D.A. Priebat, R.D. Christensen, and G. Rothstein. 1982. Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. Journal of Investigative Dermatology 78: 206–209.
Molins, B., M. Mesquida, R.W. Lee, V. Llorenç, L. Pelegrín, and A. Adán. 1954. Regulatory T cell levels and cytokine production in active non-infectious uveitis: in vitro effects of pharmacological treatment. Clinical & Experimental Immunology 179: 529–538.
Koster, R., M. Anderson, and E.I. Debeer. 1959. Acetic acid for analgesic screening. Federation Proceedings 18: 412–418.
Fasmer, O.G. Berge, and K. Hole. 1985. Changes in nociception after lesions of descending serotonergic pathways induced with 5,6-dihydroxytryptamine. Different effects in the formalin and tail-flick tests. Neuropharmacology 24: 729–734.
Eddy, N.B., and D. Leimbach. 1953. Synthetic analgesics. II. Dithienylbutenyl and dithienylbutylamines. Journal of Pharmacology and Experimental Therapeutics 107: 385–393.
McCubrey, J.A., S.L. Abrams, T.L. Fitzgerald, L. Cocco, A.M. Martelli, G. Montalto, M. Cervello, A. Scalisi, S. Candido, M. Libra, and L.S. Steelman. 2015. Roles of signaling pathways in drug resistance, cancer initiating cells and cancer progression and metastasis. Advances in Biological Regulation 57: 75–101.
Talwar, S., K. Nandakumar, P.G. Nayak, P. Bansal, J. Mudgal, V. Mor, C.M. Rao, and R. Lobo. 2011. Anti-inflammatory activity of Terminalia paniculata bark extract against acute and chronic inflammation in rats. Journal of Ethnopharmacology 134: 323–328.
Almeida, A.A.C., R.B.F. Carvalho, O.A. Silva, D.P. Sousa, and R.M. Freitas. 2014. Potential antioxidant and anxiolytic effects of (+)-limonene epoxide in mice after marble-burying test. Pharmacology, Biochemistry and Behavior 118: 69–78.
Almeida, A.A.C., J.P. Costa, R.B.F. Carvalho, D.P. Sousa, and R.M. Freitas. 2012. Evaluation of acute toxicity of a natural compound (+)-limonene epoxide and its anxiolytic-like action. Brain Reseach 1448: 56–62.
Moraes, J., A.A.C. Almeida, M.R.M. Brito, T.H.C. Marques, L.C. Lima, D.P. Sousa, E. Nakano, R.Z. Mendonça, and R.M. Freitas. 2013. Antihelmintic activity of a natural compound (+)-limonene epoxide against Schistosoma mansoni. Planta Medica 79: 253–258.
Ribeiro, R.V., R.M.L. Silva, J.C. Silva, and D.T.O. Martins. 2010. Antiinflammatory, antinociceptive and antipyretic effects of hydroethanolic extract from Macrosiphonia velame (A. St.-Hil.) M. Arg. in animal models. Brazilian Journal of Pharmaceutical Sciences 46: 515–523.
Chakrabarty, A., K.E. Mccarson, and P.G. Smith. 2011. Hypersensitivity and hyperinnervation of the rat hind paw following carrageenan-induced inflammation. Neuroscience Letters 495: 67–71.
Silva, R.O., S.R.B. Damasceno, I.S. Silva, V.G. Silva, C.F.C. Brito, A.E.A. Teixera, G.B.L. Nunes, C.A. Camara, J.M.B. Filho, S.J.C. Gutierrez, R.A. Ribeiro, M.H.L.P. Souza, A.L.R. Barbosa, R.M. Freitas, and J.V.R. Medeiros. 2015. Riparin A, a compound from Aniba riparia, attenuates the inflammatory response by modulation of neutrophil migration. Chemico-Biological Interactions 229: 55–63.
Lo, T.N., A.P. Almeida, and M.A. Beaven. 1982. Dextran and carrageenan evoke different inflammatory responses in rat with respect to composition of infiltrates and effect of indomethacin. Journal of Pharmacology and Experimental Therapeutics 222: 261–267.
Silva, M.G., F.S. Oliveira, L.J. Quintans-Júnior, O.M.L. Thenio, and M.F.M. Diniz. 2005. Investigação de efeito analgésico central e anti-inflamatório de Conocliniopsis prasiifolia (DC) RM King and H Robinson em roedores. Acta Farmaceutica Bonaerense 24: 533–537.
Damasceno, S.R.B., F.R.A.M. Oliveira, N.S. Carvalho, C.F.C. Brito, I.S. Silva, F.B.M. Sousa, R.O. Silva, D.P. Sousa, A.L.R. Barbosa, R.M. Freitas, and J.R. Medeiros. 2014. Carvacrol acetate, a derivative of carvacrol, reduces nociceptive and inflammatory response in mice. Life Sciences 94: 58–66.
Pereira, L.P., K.E.S. Da Silva, R.O. Da Silva, A.M.S. Assreuy, and M.G. Pereira. 2012. Anti-inflammatory polysaccharides of Azadirachta indica seed tegument. Brazilian Journal of Pharmacognosy 22: 617–622.
Silva, R.O., F.B.M. Sousa, S.R.B. Damasceno, N.S. Carvalho, V.G. Silva, F.R.M.A. Oliveira, D.P. Sousa, K.S. Aragão, A.L.R. Barbosa, R.M. Freitas, and J.V.R. Medeiros. 2014. Phytol, a diterpene alcohol, inhibits the inflammatory response by reducing cytokine production and oxidative stress. Fundamental & Clinical Pharmacology 28: 455–464.
Santos, J., P.C. Yang, J.D. Soderholm, M. Benjamin, and M.H. Perdue. 2001. Role of mast cells in chronic stress induced colonic epithelial barrier dysfunction in the rat. Gut 48: 630–636.
Pereira, J.G., J.X. Mesquita, K.S. Aragão, A.X. Franco, M.H.L.P. Souza, T.V. Brito, J.M. Dias, R.O. Silva, J.R. Medeiros, J.S. Oliveira, C.M.W.S. Abreu, R.C.M. De Paula, A.L.R. Barbosa, and A.L.P. Freitas. 2014. Polysaccharides isolated from Digenea simplex inhibit inflammatory and nociceptive responses. Carbohydrate Polymers 108: 17–25.
Silva-Filho, S.E., F.M.Z. Silva-Comar, L.A.M. Wiirzler, R.J. Pinho, R. Grespan, C.A. Bersani-Amado, and R.K.N. Cuman. 2014. Effect of camphor on the behavior of leukocytes in vitro and in vivo in acute inflammatory response. Tropical Journal of Pharmaceutical Research 13: 2031–2037.
Nuzzo, D., P. Picone, L. Caruana, S. Vasto, A. Barrera, C. Caruso, and M. Di Carlo. 2014. Inflammatory mediators as biomarkers in brain disorders. Inflammation 37: 639–648.
Brito, T.V., Prudêncio, A.B. Sales, F.C. Vieira Júnior, S.J.N. Candeira, A.X. Franco, K.S. Aragão, R.A. Ribeiro, M.H.L.P. Souza, L.S. Chaves, A.L.P. Freitas, J.R. Medeiros, and A.L.R. Barbosa. 2013. Anti-inflammatory effect of a sulphated polysaccharide fraction extracted from the red algae Hypnea musciformis via the suppression of neutrophil migration by the nitric oxide signalling pathway. Journal of Pharmacy and Pharmacology 65: 724–733.
González, C.P., R.S. Veja, M. González-Chávez, M.A.Z. Sánchez, and S.P. Gutiérrez. 2013. Antiinflammatory activity and composition of Senecio salignus Kunth. BioMed Research International 2013: 1–4.
Zhang, J.M., and J. An And. 2007. Cytokines, inflammation, and pain. International Anesthesiology Clinics 45: 27–37.
Ren, K., and R. Torres. 2009. Role of interleukin-1β during pain and inflammation. Brain Research Reviews 60: 57–64.
Carvalho, V., L. Fernandes, T. Conde, H. Zamith, R. Silva, A. Surrage, V. Frutuoso, H. Castro-Faria-Neto, and F. Amendoeira. 2013. Antinociceptive activity of Stephanolepis hispidus skin aqueous extract depends partly on opioid system activation. Marine Drugs 11: 1221–1255.
Lima, S.M.A., L.C.C. Araújo, M.M. Sitônio, A.C.C. Freitas, S.L. Moura, M.T. Correia, D.J.N. Malta, and T. Gonçalves-Silva. 2012. Anti-inflammatory and analgesic potential of Caesalpinia ferrea. Brazilian Journal of Pharmacognosy 22: 169–175.
Sowemimo, A., M. Onakoy, M.S. Fageyinbo, and T. Fadoju. 2012. Studies on the anti-inflammatory and anti-nociceptive properties of Blepharis maderaspatensis leaves. Brazilian Journal of Pharmacognosy 23: 830–835.
Shin, D.J., C.W. Jeong, S.H. Lee, and M.H. Yoon. 2011. Receptors involved in the antinociception of intrathecal melatonin in formalin test of rats. Neuroscience Letters 494: 207–210.
Mansouri, M.T., B. Naghizadeh, and B. Ghorbanzadeh. 2014. Involvement of opioid receptors in the systemic and peripheral antinociceptive actions of ellagic acid in the rat formalin test. Pharmacology, Biochemistry and Behavior 120: 43–49.
ACKNOWLEDGEMENTS
We wish to thank the Federal Brazilian agency “Conselho Nacional de Desenvolvimento Científico e Tecnológico” (CNPq) for financial support in the form of grants (#473167/2012-3) and fellowships.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were approved by the Committee on Animal Research at the UFPI (Process no. 091/2014) and followed the Brazilian (Colégio Brasileiro de Experimentação Animal—COBEA) and International Standards on the care and use of experimental animals (Directive 2010/63/EU of the European Parliament and of the Council).
Conflict of Interest
The authors declare that there are no conflicts of interest.
Additional information
Rivelilson Mendes de Freitas (In Memoriam)
Rights and permissions
About this article
Cite this article
de Almeida, A.A.C., Silva, R.O., Nicolau, L.A.D. et al. Physio-pharmacological Investigations About the Anti-inflammatory and Antinociceptive Efficacy of (+)-Limonene Epoxide. Inflammation 40, 511–522 (2017). https://doi.org/10.1007/s10753-016-0496-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0496-y