Abstract
High-mobility group box 1 (HMGB1) plays a key role in the development of acute lung injury (ALI). Propofol, a general anesthetic with anti-inflammatory properties, has been suggested to be able to modulate lipopolysaccharide (LPS)-induced ALI. In this study, we investigated the effects of propofol on the expression of HMGB1 in a rat model of LPS-induced ALI. Rats underwent intraperitoneal injection of LPS to mimic sepsis-induced ALI. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after LPS administration, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. LPS increased wet to dry weight ratio and myeloperoxidase activity in lung tissues and caused the elevation of total protein and cells, neutrophils, macrophages, and neutrophils in bronchoalveolar lavage fluid (BALF). Moreover, HMGB1 and other cytokine levels were increased in BALF and lung tissues and pathological changes of lung tissues were excessively aggravated in rats after LPS administration. Propofol inhibited all the above effects. It also inhibited LPS-induced toll-like receptor (TLR)2/4 protein upexpression and NF-κB activation in lung tissues and human alveolar epithelial cells. Propofol protects rats and human alveolar epithelial cells against HMGB1 expression in a rat model of LPS-induced ALI. These effects may partially result from reductions in TLR2/4 and NF-κB activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Acute lung injury (ALI) is a major consequence of septic shock and contributes to the high morbidity and mortality of sepsis [1]. Previous studies have demonstrated that, after severe injury or infectious challenge, some patients respond by activating pro-inflammatory signaling pathways and overexpressing inflammatory mediators that result in a systemic inflammatory response that culminates in severe shock, multi-organ failure, and death [2]. Despite extensive investigation, the cellular and molecular mechanisms that mediate ALI during septic shock have remained largely unknown. Furthermore, developing effective methods for preventing and/or treating sepsis-induced ALI has proven to be difficult. A growing body of evidence suggests that there is a link between the innate immune response and ALI in several important disease states, including ischemia-reperfusion injury [3], traumatic brain injury [4], and septic shock [5].
High mobility group box 1 (HMGB1) is an evolutionarily conserved protein present in virtually all types of cells, where it functions to stabilize nucleosomal structure and regulate gene expression [6]. Recent evidence suggests that extracellular HMGB1 functions as a danger-associated molecular pattern [7] and is actively secreted by immunologically activated immune cells or passively released from pathologically damaged cells [8]. In vivo neutralization of HMGB1 by specific antibodies protects mice against lethal sepsis [9], as well as lipopolysaccharide (LPS)-induced ALI [10]. In a more clinically relevant animal model of sepsis (induced by cecal ligation puncture, CLP), delayed administration of HMGB1-specific neutralizing antibodies, beginning 24 h after CLP, dose dependently rescue rodents from lethal sepsis [11]. Moreover, targeted inhibition of HMGB1 expression in innate immune cells (e.g., macrophages and dendritic cells) reduces systemic HMGB1 accumulation and similarly rescues mice from sepsis [12]. Taken together, these experimental data establish extracellular HMGB1 as a critical late mediator of experimental sepsis. In vitro studies have demonstrated that the HMGB1-stimulated inflammatory response could be mediated through several pattern-recognition receptors including the receptors for advanced glycation end products [13], toll-like receptor 2 (TLR2) [14], TLR4 [15], and TLR9 [16].
Propofol is an anesthetic agent with sedative properties that modulates innate immunity and pro-inflammatory signaling in sepsis [17, 18]. Propofol administration downregulates sepsis-induced increases in TLR2/4 expression [19, 20], attenuates sepsis-induced NF-κB activity [21], and activates heme oxygenase-1 expression [22]. Previous studies demonstrated that propofol inhibits sepsis-induced ALI in rats [17, 20]. Therefore, we hypothesized that propofol would down-regulate HMGB1 expression and that the inhibition of HMGB1 expression would be associated with the inhibition of TLR2/4 and NF-κB activation by propofol during sepsis. The aim of the present study was to determine whether propofol attenuates ALI by the inhibition of HMGB1 expression in a rat LPS model.
MATERIALS AND METHODS
Materials
Propofol and LPS (Escherichia coli 055:B5) were obtained from Sigma (St. Louis, MO, USA). HMGB1, TNF-α, IL-6, and myeloperoxidase (MPO) enzyme-linked immunosorbent assay (ELISA) kit were obtained from Invitrogen (Carlsbad, CA, USA). Anti-TLR2, anti-TLR4, anti-p-NF-κB p65, and anti-NF-κB p65 antibodies were obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Anti-IκB-α and anti-p-IκB-α antibodies were obtained from Cell Signaling Technology Inc (Beverly, MA, USA).
Animals
Adult male Sprague–Dawley rats (weighing 250 to 300 g) were provided by the Experimental Animal Center of Shandong University, kept in a 12-h dark/12-h light cycle in a temperature- and humidity-controlled room and fed on standard laboratory diet and water. All procedures were performed in accordance with the Declaration of Helsinki of the World Medical Association. The study was approved by the ethics committee of Shandong Provincial Hospital Affiliated to Shandong University, Jinan, Shandong, China.
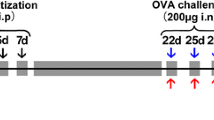
Animal Experimental Design
Animals were randomly divided into six groups and each group contained 20 rats: (1) control group (normal saline, NS), (2) propofol (10 mg/kg) group, (3) LPS group (5 mg/kg), (4) LPS + propofol (1 mg/kg) group, (5) LPS + propofol (5 mg/kg) group, and (6) LPS + propofol (10 mg/kg) group. In another experiments, animals were randomly divided into six groups and each group contained 20 rats: (1) control group (NS), (2) propofol (10 mg/kg) group, (3) HMGB1 group (5 mg/kg), (4) HMGB1 + propofol (1 mg/kg) group, (5) HMGB1 + propofol (5 mg/kg) group, and (6) HMGB1 + propofol (10 mg/kg) group. LPS (5 mg/kg), HMGB1 (5 mg/kg), or vehicle (NS) was intraperitoneally administered to induce ALI [23]. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after LPS injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. The doses of these drugs were on the basis of previous studies and our preliminary experiments [17, 18, 20, 24, 25]. At 24 h after LPS/HMGB1 administration, the rats were sacrificed and samples were collected.
Cell Culture and Treatment
\The human alveolar epithelial cells A549 were obtained from the Typical Species Preservation Center of Wuhan University (Wuhan, Hubei, China). A549 cells were seeded into 6-well plates and were cultured in DMEM supplemented with 10 % FBS, 100 U/mL penicillin, and 100 μg/mL streptomycin at 37 °C in a humidified atmosphere containing 5 % CO2. Cells were grown until 70 % confluence before drug treatments. Cells were divided into four groups: (1) control group (NS), (2) propofol (100 μM) group, (3) LPS group (1 μg/mL), and (4) LPS + propofol (100 μM) group. A549 cells were treated with propofol (100 μM) 24 h after LPS (1 μg/mL) stimulation. The doses of these drugs were on the basis of previous studies and our preliminary experiments [26]. The cell samples were harvested at 24 h after the addition of LPS to analyze the expressions of TLR2, TLR4, p-NF-κB p65, and p-IκB-α.
Lung Wet/Dry Weight Ratio In Vivo
The water content of lungs was determined by calculating the wet/dry weight ratio of lung tissues. The inferior lobe of right lung was excised, rinsed briefly in phosphate-buffered saline (PBS), blotted, and then weighed to obtain the “wet” weight. The lung was then dried at 80 °C for 72 h to obtain the “dry” weight. The wet/dry ratio was calculated by dividing the wet weight by the dry weight.
Determination of Bronchoalveolar Lavage Proteins and Cell Counts
Bronchoalveolar lavage (BAL) was performed by intratracheal injection of 5-mL ice-cold PBS followed by gentle aspiration. The recovery ratio of the fluid was about 90 %. Then, the recovered fluid was pooled and centrifuged at 1200×g for 10 min at 4 °C. Supernatants were preserved for the measurement of total protein concentration by the Bradford method with bovine serum albumin (BSA) as a standard. The cell pellet was re-suspended in 50 μL PBS, and total cells recovered in bronchoalveolar lavage fluid (BALF) were counted. The cell differentiation was determined for 200 cells by examination of the hematoxylin and eosin (H&E)-stained smears.
Cytokine Measurements
The levels of HMGB1, TNF-α, and IL-6 in the supernatants of BALF and lung tissues were measured with a commercially available ELISA kit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions.
MPO Activity Assay
Lung tissues were homogenized in hydroxyethyl piperazine ethanesulfonic acid (pH 8.0) containing 0.5 % cetyltrimethyl ammonium bromide and subjected to three freeze-thaw cycles. The homogenate was centrifuged (4 °C, 12,000×g, 30 min). The MPO activity was assayed using a commercially available ELISA kit (Invitrogen, Carlsbad, CA, USA). Samples were diluted in phosphate citrate buffer (pH 5.0), and the absorbance of the sample was measured at 460 nm using a microplate reader. The specific activity of MPO in the lung is expressed as unit per gram of the tissue.
Histological Examination
The right lobes were excised and fixed with 10 % neutral phosphate-buffered formalin, imbedded in paraffin and sliced. After H&E staining, pathological changes of lung tissues were observed under a light microscope. The standard lung injury score was performed by a blinded pathologist to objectively quantify the lung injury.
Western Blot Analysis
Protein concentrations were determined by BCA Protein Assay Kit, and 20 μg proteins was loaded per well on a 10 % sodium dodecylsulfate-polyacrylamide gel and transferred onto polyvinylidene difluoride membrane. After being blocked for 3 h in Tris-buffered saline with 0.1 % Tween 20 (TBST) and 3 % BSA, membranes were incubated overnight at 4 °C with primary antibodies in TBST containing 3 % BSA. Membranes were then washed and incubated with horse radish peroxidase-conjugated secondary antibodies in TBST for 2 h and developed using an ECL detection system. The density of the bands on the membrane was scanned and analyzed with an image analyzer (Lab Works Software, UVP Upland, CA, USA).
Statistical Evaluation
Data are the mean ± standard deviation (SD) of results obtained from 20 rats in each group in vivo and three replicates in vitro. Statistical analysis of the results was carried out by one-way analysis of variance (ANOVA) followed by Tukey’s post hoc test in SPSS 11.0 (Chicago, IL, USA), and P values < 0.05 were considered to be statistically significant.
RESULTS
Effects of Propofol on the Lung Wet/Dry Weight Ratio in Lung Tissues
To evaluate the LPS/HMGB1-induced changes in pulmonary vascular permeability, the lung wet/dry weight ratio in lung tissues was analyzed. As shown in Figs. 1 and 5, the lung wet/dry ratio in lung tissues was significantly increased after LPS/HMGB1 challenge compared with control group. However, propofol administration obviously decreased the wet/dry ratio in lung tissues in a dose-dependent manner (P < 0.05; Figs. 1a and 5a). There were no significant differences of the wet/dry ratio in lung tissues between control and propofol groups.
Propofol reduced the lung wet/dry weight ratio and the MPO activity in LPS-induced ALI rats. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after LPS injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. The lung wet/dry weight ratio (a) and the MPO activity (b) were determined at 24 h after LPS administration. The data are presented as means ± SD (n = 20). *P < 0.05 compared with LPS group; # P < 0.01 compared with LPS group. Prop propofol.
Effects of Propofol on MPO Activity in Lung Tissues
Neutrophils are the major components of inflammatory and immunological reactions in injured lungs. MPO activity in lung tissues is known as a reliable marker of neutrophil infiltration. In this study, MPO activity in the homogenates of lung tissues was detected at 24 h after LPS/HMGB1 administration. As shown in Figs. 1 and 5, LPS/HMGB1 administration significantly increased MPO activity compared with control group. However, propofol treatment apparently decreased MPO activity in lung tissues of LPS/HMGB1-challenged rats in a dose-dependent manner (P < 0.05; Figs. 1b and 5b).
Effects of Propofol on LPS-Mediated Lung Histopathologic Changes
To evaluate the histological changes after propofol treatment in LPS-treated rats, lung tissues were harvested at 24 h after administration of LPS. As shown in Fig. 2a, lung tissues from control group showed a normal structure and no histopathologic changes. In LPS group, histological examination revealed serious lung destruction, as indicated by the H&E assay, which manifest as serious pulmonary edema, hemorrhagia in stroma, alveolar collapse, and massive inflammatory cell infiltration (Fig. 2c). However, propofol treatment effectively alleviated the destruction of lung structure (Fig. 2d). Furthermore, propofol treatment group had a significantly lower lung injury score than control group (P < 0.05; Fig. 2e).
Histologic assessment of the effect of propofol on LPS-induced ALI. Propofol bolus (10 mg/kg) was infused continuously 30 min after LPS injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. Lungs from each experimental group were processed for histological evaluation at 24 h after LPS administration. a Control group, b propofol (10 mg/kg) group, c LPS group, d LPS + propofol (10 mg/kg) group (H&E staining, magnification ×200), and e lung injury index. The data are presented as means ± SD (n = 20).*P < 0.05 compared with LPS group; # P < 0.01 compared with LPS group.
Effects of Propofol on the Concentration of Total Protein and the Inflammatory Cell Counts in BALF
To examine the effects of propofol on LPS/HMGB1-induced pulmonary inflammation, the concentration of total protein and the numbers of inflammatory cells, such as neutrophils and macrophages, in BALF were analyzed at 24 h after LPS/HMGB1 injection. As shown in Figs. 3 and 6, after LPS/HMGB1 challenging, the concentration of total protein and the numbers of total cells, neutrophils, and macrophages significantly increased compared with control group. However, this increase was apparently attenuated by propofol treatment in a dose-dependent manner (P < 0.05; Fig. 3 and 6).
Effects of propofol on the total protein concentration and the numbers of total cells, neutrophils, and macrophages in BALF. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after LPS injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. BALF was collected at 24 h after LPS administration to measure the total protein concentration (a) and the numbers of total cells (b), neutrophils (c), and macrophages (d). The data are presented as means ± SD (n = 20). *P < 0.05 compared with LPS group; # P < 0.01 compared with LPS group. Prop propofol.
Effects of Propofol on the Concentrations of Pro-Inflammatory Cytokines in BALF and Lung Tissues
To further evaluate the anti-inflammatory action of propofol, the concentrations of pro-inflammatory cytokines TNF-α, IL-6, and HMGB1in BALF and lung tissues were analyzed at 24 h after LPS/HMGB1 administration by ELISA. As illustrated in Figs. 4, 5, 6, and 7, the concentrations of TNF-α, IL-6, and HMGB1 in BALF and lung tissues significantly increased in LPS/HMGB1 group. However, propofol treatment markedly decreased the levels of TNF-α, IL-6, and HMGB1compared to those in LPS/HMGB1 group in a dose-dependent manner (P < 0.05; Figs. 4 and 7).
Propofol inhibited LPS-induced expressions of TNF-α, IL-6, and HMGB1 in BALF and lung tissues. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after LPS injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. BALF and lung tissues were collected at 24 h after LPS administration to analyze the inflammatory cytokines TNF-α (a, d), IL-6 (b, e), and HMGB1 (c, f). The data are presented as means ± SD (n = 20). *P < 0.05 compared with LPS group; # P < 0.01 compared with LPS group. Prop propofol.
Propofol reduced the lung wet/dry weight ratio and the MPO activity in HMGB1-induced ALI rats. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after HMGB1 injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. The lung wet/dry weight ratio (a) and the MPO activity (b) were determined at 24 h after HMGB1 administration. The data are presented as means ± SD (n = 20). *P < 0.05 compared with HMGB1 group; # P < 0.01 compared with HMGB1 group. Prop propofol.
Effects of propofol on the total protein concentration and the numbers of total cells, neutrophils, and macrophages in BALF. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after HMGB1 injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. BALF was collected at 24 h after HMGB1 administration to measure the total protein concentration (a) and the numbers of total cells (b), neutrophils (c), and macrophages (d). The data are presented as means ± SD (n = 20). *P < 0.05 compared with HMGB1 group; # P < 0.01 compared with HMGB1 group. Prop propofol.
Propofol inhibited HMGB1-induced expressions of TNF-α and IL-6 in BALF and lung tissues. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after HMGB1 injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. BALF and lung tissues were collected at 24 h after HMGB1 administration to analyze the inflammatory cytokines TNF-α (a, b) and IL-6 (c, d). The data are presented as means ± SD (n = 20). *P < 0.05 compared with HMGB1 group; # P < 0.01 compared with HMGB1 group. Prop propofol.
Effects of Propofol on the Expressions of TLR2 and TLR4 in Lung Tissues
In this study, the expressions of TLR2 and TLR4 in lung tissues were detected by Western blotting. As shown in Fig. 8, the levels of TLR2 and TLR4 proteins showed significant increases in LPS group at 24 h after LPS administration. However, this increase was apparently attenuated by propofol treatment in a dose-dependent manner (P < 0.05; Fig. 8a, b).
Propofol inhibited the expressions of TLR2 and TLR4 and the phosphorylation of NF-κB p65 and IκB-α in lung tissues. Propofol bolus (1, 5, or 10 mg/kg) was infused continuously 30 min after LPS injection, followed by infusion at 5 mg/(kg · h) through the left femoral vein cannula. At 24 h after LPS administration, the expressions of TLR2 (a) and TLR4 (b) and the phosphorylation of NF-κB p65 (c) and IκB-α (d) were detected by Western blotting. The data are presented as means ± SD (n = 20). *P < 0.05 compared with LPS group; # P < 0.01 compared with LPS group. Prop propofol.
Effects of Propofol on LPS-Induced NF-κB Activation in Lung Tissues
Western blot analysis was used to determine the phosphorylation of NF-κB p65 and IκB-α, which reflected the activation of NF-κB in lung tissues. As shown in Fig. 8, LPS administration significantly increased the phosphorylation of NF-κB p65 and IκB-α, as compared with control group. However, propofol treatment markedly decreased the phosphorylation of NF-κB p65 and IκB-α induced by LPS in a dose-dependent manner (P < 0.05; Fig. 8c, d). These results showed that propofol could inhibit NF-κB activation in LPS-induced ALI rats.
Effects of Propofol on the Expressions of TLR2 and TLR4 in A549 Alveolar Epithelial Cells
To further examine the anti-inflammatory mechanistic basis of propofol, we investigated the effects of propofol on TLR2 and TLR4 expressions in A549 alveolar epithelial cells. Similar to what we observed in animal experiments, TLR2 and TLR4 protein upexpressions were dramatically increased in cells stimulated with LPS. However, these increases were markedly inhibited by propofol treatment (P < 0.05; Fig. 9a, b).
Propofol inhibited the expressions of TLR2 and TLR4 and the phosphorylation of NF-κB p65 and IκB-α in LPS-stimulated A549 alveolar epithelial cells. A549 cells were treated with propofol (100 μM) 24 h after LPS (1 μg/mL) stimulation. The expressions of TLR2 (a) and TLR4 (b) and the phosphorylation of NF-κB p65 (c) and IκB-α (d) were detected by Western blotting. Data are presented as means ± SD from three independent experiments. *P < 0.05 compared with LPS group; # P < 0.01 compared with LPS group. Prop propofol.
Effects of Propofol on LPS-Induced NF-κB Activation in A549 Alveolar Epithelial Cells
Propofol was found to inhibit LPS-induced NF-κB activation in our animal experiments. We also examine whether this inhibitory effect of propofol happens to alveolar epithelial cells. As shown in Fig. 9, we found that LPS greatly enhanced the phosphorylation of NF-κB p65 and IκB-α, which reflected the activation of NF-κB. However, treatment of propofol inhibited the LPS-induced NF-κB activation in A549 alveolar epithelial cells (P < 0.05; Fig. 9c, d).
DISCUSSION
In this study, we evaluated the protective effects of propofol in a model of LPS-induced ALI in rats. Consistent with previous studies [27], propofol administration attenuated lung inflammatory injury after LPS, as revealed by decreased elevation of the lung wet to dry weight ratio, total cells, neutrophils, macrophages, and MPO activity, associated with reduced lung histological damage. In addition, we also found that propofol post-treatment markedly inhibited the release of HMGB1 and other pro-inflammatory cytokines in a model of LPS-induced ALI in rats. Furthermore, propofol significantly inhibited LPS-induced TLR2/4 protein upexpression and NF-κB activation in lung tissues and in LPS-stimulated A549 alveolar epithelial cells.
Previous studies have shown that propofol can inhibit the inflammatory responses and mitigate endotoxin-induced ALI [24, 28]. As is already known, the etiologies of ALI are complex, and additional mechanisms by which propofol affords protection in LPS-induced lung injury are needed to be further investigated. Evidence suggests that HMGB1 plays a critical role in the progression of ALI. HMGB1-based therapeutic strategy may be more meaningful in ALI, because HMGB1 is a late inflammatory mediator; this will give us a much broader intervention window. Therefore, the current study aimed to test the hypothesis that propofol can alleviate LPS-induced ALI through preventing the expression of HMGB1.
Clinical and experimental studies have shown that ALI is an early and fatal complication of septic shock [1] and that the TLR2/4-mediated NF-κB activation signaling pathway could be an early molecular event leading to ALI during septic shock [29, 30]. Previous studies have shown that propofol significantly increased survival in CLP rat and the mechanisms involved in down-regulating the expression of TLR2/4 and blunting NF-κB activation in the lung [17, 19–21]. To evaluate our hypothesis, we examined pulmonary inflammation in LPS-induced ALI with or without propofol treatment. We observed that the pulmonary inflammation was significantly increased in a rat LPS model. However, propofol administration significantly inhibited pulmonary inflammation by inhibiting the TLR2/4 expressions in a rat LPS model. Previous studies have shown that propofol administration significantly blunted NF-κB activation in septic rat [18, 21]. NF-κB is a critical transcription factor in TLR-mediated signaling pathways [31] and plays a critical role in regulation of the expression of a number of genes, including inflammatory cytokines such as HMGB1, TNF-α, and IL-1β [32–35]. In this study, we demonstrated that propofol would down-regulate HMGB1 expression in LPS-induced ALI model and that the inhibition of HMGB1 expression would be associated with the inhibition of TLR2/4 and NF-κB activation by propofol during sepsis. An important limitation of the current study is that LPS is not equivalent to sepsis. In this study, we only investigated the effects of propofol on LPS-induced ALI in a rat model; a further study to investigate the protective effects of propofol on sepsis-induced ALI in clinical studies is needed.
The anesthetic concentration of propofol used for clinical medication is less than 5 mg/kg/h to provide satisfactory sedation [36]. In addition to its anesthetic properties, a safe range of doses of propofol is neuroprotective against ischemia reperfusion [37, 38] and has cardiovascular benefits against oxidative stress [39, 40]. However, abuse of propofol treatment causes severe complications in patients with critical illness and is called propofol infusion syndrome [41]. In this study, we found that propofol treatment (1, 5, and 10 mg/kg) attenuated LPS-induced ALI in dose-dependent manner. Because of toxicity of systemic propofol, we think that propofol treatment (5 mg/kg) was better than other treatment groups and should be explored further in larger animals and more relevant sepsis models in a path to human trials.
In summary, the present study provided evidence that propofol improves LPS-induced ALI accompanied with decreased HMGB1 expression. The mechanisms are, at least in part, through the down-regulation of TLR2/4 expressions and inhibition of NF-κB pathway.
References
Su, C.F., S.J. Kao, and H.I. Chen. 2012. Acute respiratory distress syndrome and lung injury: pathogenetic mechanism and therapeutic implication. World Journal Critical Care Medicine 1: 50–60.
Castellheim, A., O.L. Brekke, T. Espevik, M. Harboe, and T.E. Mollnes. 2009. Innate immune responses to danger signals in systemic inflammatory response syndrome and sepsis. Scandinavian Journal of Immunology 69: 479–491.
Jing, H., J. Yao, X. Liu, H. Fan, F. Zhang, Z. Li, X. Tian, and Y. Zhou. 2014. Fish-oil emulsion (omega-3 polyunsaturated fatty acids) attenuates acute lung injury induced by intestinal ischemia-reperfusion through adenosine 5′-monophosphate-activated protein kinase-sirtuin1 pathway. Journal of Surgical Research 187: 252–261.
Song, Z., X. Zhao, Y. Gao, M. Liu, M. Hou, H. Jin, and Y. Cui. 2015. Recombinant human brain natriuretic peptide ameliorates trauma-induced acute lung injury via inhibiting JAK/STAT signaling pathway in rats. Journal Trauma Acute Care Surgery 78: 980–987.
Lin, W.C., C.W. Chen, Y.W. Huang, L. Chao, J. Chao, Y.S. Lin, and C.F. Lin. 2015. Kallistatin protects against sepsis-related acute lung injury via inhibiting inflammation and apoptosis. Scientific Reports 5: 12463.
Lu, B., C. Wang, M. Wang, W. Li, F. Chen, K.J. Tracey, and H. Wang. 2014. Molecular mechanism and therapeutic modulation of high mobility group box 1 release and action: an updated review. Expert Review of Clinical Immunology 10: 713–727.
Agalave, N.M., and C.I. Svensson. 2015. Extracellular high-mobility group box 1 protein (HMGB1) as a mediator of persistent pain. Molecular Medicine 20: 569–578.
Wang, H., M.F. Ward, and A.E. Sama. 2014. Targeting HMGB1 in the treatment of sepsis. Expert Opinion on Therapeutic Targets 18: 257–268.
Wang, H., O. Bloom, M. Zhang, J.M. Vishnubhakat, M. Ombrellino, J. Che, A. Frazier, H. Yang, S. Ivanova, L. Borovikova, K.R. Manogue, E. Faist, E. Abraham, J. Andersson, U. Andersson, P.E. Molina, N.N. Abumrad, A. Sama, and K.J. Tracey. 1999. HMG-1 as a late mediator of endotoxin lethality in mice. Science 285: 248–251.
Lutz, W., and J. Stetkiewicz. 2004. High mobility group box 1 protein as a late-acting mediator of acute lung inflammation. International Journal of Occupational Medicine and Environmental Health 17: 245–254.
Yang, H., M. Ochani, J. Li, X. Qiang, M. Tanovic, H.E. Harris, S.M. Susarla, L. Ulloa, H. Wang, R. DiRaimo, C.J. Czura, J. Roth, H.S. Warren, M.P. Fink, M.J. Fenton, U. Andersson, and K.J. Tracey. 2004. Reversing established sepsis with antagonists of endogenous high-mobility group box 1. Proceedings of the National Academy of Sciences of the United States of America 101: 296–301.
Ye, C., J.G. Choi, S. Abraham, H. Wu, D. Diaz, D. Terreros, P. Shankar, and N. Manjunath. 2012. Human macrophage and dendritic cell-specific silencing of high-mobility group protein B1 ameliorates sepsis in a humanized mouse model. Proceedings of the National Academy of Sciences of the United States of America 109: 21052–21057.
van Beijnum, J.R., W.A. Buurman, and A.W. Griffioen. 2008. Convergence and amplification of toll-like receptor (TLR) and receptor for advanced glycation end products (RAGE) signaling pathways via high mobility group B1 (HMGB1). Angiogenesis 11: 91–99.
Park, J.S., F. Gamboni-Robertson, Q. He, D. Svetkauskaite, J.Y. Kim, D. Strassheim, J.W. Sohn, S. Yamada, I. Maruyama, A. Banerjee, A. Ishizaka, and E. Abraham. 2006. High mobility group box 1 protein interacts with multiple toll-like receptors. American Journal of Physiology - Cell Physiology 290: C917–C924.
Kim, S., S.Y. Kim, J.P. Pribis, M. Lotze, K.P. Mollen, R. Shapiro, P. Loughran, M.J. Scott, and T.R. Billiar. 2013. Signaling of high mobility group box 1 (HMGB1) through toll-like receptor 4 in macrophages requires CD14. Molecular Medicine 19: 88–98.
Hirata, Y., H. Kurobe, M. Higashida, D. Fukuda, M. Shimabukuro, K. Tanaka, Y. Higashikuni, T. Kitagawa, and M. Sata. 2013. HMGB1 plays a critical role in vascular inflammation and lesion formation via toll-like receptor 9. Atherosclerosis 231: 227–233.
Bao, H.G., and S. Li. 2011. Effects of propofol on the outcomes of rats with sepsis. Journal of Surgical Research 168: e111–e115.
Song, X.M., Y.L. Wang, J.G. Li, C.Y. Wang, Q. Zhou, Z.Z. Zhang, and H. Liang. 2009. Effects of propofol on pro-inflammatory cytokines and nuclear factor kappaB during polymicrobial sepsis in rats. Molecular Biology Reports 36: 2345–2351.
Chiu, W.T., Y.L. Lin, C.W. Chou, and R.M. Chen. 2009. Propofol inhibits lipoteichoic acid-induced iNOS gene expression in macrophages possibly through downregulation of toll-like receptor 2-mediated activation of Raf-MEK1/2-ERK1/2-IKK-NFkappaB. Chemico-Biological Interactions 181: 430–439.
Ma, L., X.Y. Wu, L.H. Zhang, W.M. Chen, A. Uchiyama, T. Mashimo, and Y. Fujino. 2013. Propofol exerts anti-inflammatory effects in rats with lipopolysaccharide-induced acute lung injury by inhibition of CD14 and TLR4 expression. Brazilian Journal of Medical and Biological Research 46: 299–305.
Wang, T., X.Y. Wei, B. Liu, L.J. Wang, and L.H. Jiang. 2015. Effects of propofol on lipopolysaccharide-induced expression and release of HMGB1 in macrophages. Brazilian Journal of Medical and Biological Research 48: 286–291.
Liang, C., J. Cang, H. Wang, and Z. Xue. 2013. Propofol attenuates cerebral ischemia/reperfusion injury partially using heme oxygenase-1. Journal of Neurosurgical Anesthesiology 25: 311–316.
Shen, W., J. Gan, S. Xu, G. Jiang, and H. Wu. 2009. Penehyclidine hydrochloride attenuates LPS-induced acute lung injury involvement of NF-kappaB pathway. Pharmacological Research 60: 296–302.
Chu, C.H., D. David Liu, Y.H. Hsu, K.C. Lee, and H.I. Chen. 2007. Propofol exerts protective effects on the acute lung injury induced by endotoxin in rats. Pulmonary Pharmacology & Therapeutics 20: 503–512.
Li, S., H. Bao, L. Han, and L. Liu. 2010. Effects of propofol on early and late cytokines in lipopolysaccharide-induced septic shock in rats. Journal Biomedical Research 24: 389–394.
Wei, L., H. Matsumoto, and H. Yamaguchi. 2013. Propofol attenuates lipopolysaccharide-induced monocyte chemoattractant protein-1 production through p38 MAPK and SAPK/JNK in alveolar epithelial cells. Journal of Anesthesia 27: 366–373.
Zhao L.L., Hu G.C., Zhu S.S., Li J.F. and Liu G.J. 2014. Propofol pretreatment attenuates lipopolysaccharide-induced acute lung injury in rats by activating the phosphoinositide-3-kinase/Akt pathway. Brazilian Journal of Medical and Biological Research.
Gokcinar, D., V. Ergin, A. Cumaoglu, A. Menevse, and A. Aricioglu. 2013. Effects of ketamine, propofol, and ketofol on proinflammatory cytokines and markers of oxidative stress in a rat model of endotoxemia-induced acute lung injury. Acta Biochimica Polonica 60: 451–456.
Feng, G., B. Sun, and T.Z. Li. 2015. Daidzein attenuates lipopolysaccharide-induced acute lung injury via toll-like receptor 4/NF-kappaB pathway. International Immunopharmacology 26: 392–400.
Tianzhu, Z., and W. Shumin. 2015. Esculin inhibits the inflammation of LPS-induced acute lung injury in mice via regulation of TLR/NF-kappaB pathways. Inflammation 38: 1529–1536.
Kawasaki, T., and T. Kawai. 2014. Toll-like receptor signaling pathways. Frontiers in Immunology 5: 461.
Chang, Y., X. Huang, Z. Liu, G. Han, L. Huang, Y.C. Xiong, and Z. Wang. 2013. Dexmedetomidine inhibits the secretion of high mobility group box 1 from lipopolysaccharide-activated macrophages in vitro. Journal of Surgical Research 181: 308–314.
Liu, Z., J. Zhang, X. Huang, L. Huang, S. Li, and Z. Wang. 2013. Magnesium sulfate inhibits the secretion of high mobility group box 1 from lipopolysaccharide-activated RAW264.7 macrophages in vitro. Journal of Surgical Research 179: e189–e195.
Liu, Z., Y. Chang, J. Zhang, X. Huang, J. Jiang, S. Li, and Z. Wang. 2013. Magnesium deficiency promotes secretion of high-mobility group box 1 protein from lipopolysaccharide-activated macrophages in vitro. Journal of Surgical Research 180: 310–316.
Yang, Q., X. Liu, Z. Yao, S. Mao, Q. Wei, and Y. Chang. 2014. Penehyclidine hydrochloride inhibits the release of high-mobility group box 1 in lipopolysaccharide-activated RAW264.7 cells and cecal ligation and puncture-induced septic mice. Journal of Surgical Research 186: 310–317.
Mackenzie, N., and I.S. Grant. 1987. Propofol for intravenous sedation. Anaesthesia 42: 3–6.
Shao, H., J. Li, Y. Zhou, Z. Ge, J. Fan, Z. Shao, and Y. Zeng. 2008. Dose-dependent protective effect of propofol against mitochondrial dysfunction in ischaemic/reperfused rat heart: role of cardiolipin. British Journal of Pharmacology 153: 1641–1649.
Li, J., B. Han, X. Ma, and S. Qi. 2010. The effects of propofol on hippocampal caspase-3 and Bcl-2 expression following forebrain ischemia-reperfusion in rats. Brain Research 1356: 11–23.
Karashima, Y., M. Oike, S. Takahashi, and Y. Ito. 2002. Propofol prevents endothelial dysfunction induced by glucose overload. British Journal of Pharmacology 137: 683–691.
Wang, B., T. Luo, D. Chen, and D.M. Ansley. 2007. Propofol reduces apoptosis and up-regulates endothelial nitric oxide synthase protein expression in hydrogen peroxide-stimulated human umbilical vein endothelial cells. Anesthesia and Analgesia 105: 1027–1033. Table of contents.
Vasile, B., F. Rasulo, A. Candiani, and N. Latronico. 2003. The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Medicine 29: 1417–1425.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (NSF 30872433).
Author Contributions
Xiaoyan Wang: conception, design, analysis, and interpretation of data; writing the manuscript.
Gongming Wang: conception, design, analysis, and interpretation of data; writing the manuscript.
Chengxiao Liu: analysis and interpretation of data; writing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were performed in accordance with the Declaration of Helsinki of the World Medical Association. The study was approved by the ethics committee of Shandong Provincial Hospital Affiliated to Shandong University, Jinan, Shandong, China.
Conflicts of Interest
The authors report no proprietary or commercial interest in any product mentioned, or concept discussed, in this article.
Rights and permissions
About this article
Cite this article
Wang, X., Liu, C. & Wang, G. Propofol Protects Rats and Human Alveolar Epithelial Cells Against Lipopolysaccharide-Induced Acute Lung Injury via Inhibiting HMGB1 Expression. Inflammation 39, 1004–1016 (2016). https://doi.org/10.1007/s10753-016-0330-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0330-6