Abstract
Severe acute pancreatitis is a life threatening disease with a high rate of mortality, but its treatments are still controversial. The purpose of this study is to investigate the potential effects of calcium binding protein S100A12 on severity evaluation and curative effect of severe acute pancreatitis induced by caerulein and lipopolysaccharide in mice. Intraperitoneal injection of 50 μg/kg caerulein for seven times (every interval time was an hour) and intraperitoneal injection of 10 mg/kg lipopolysaccharide for once to establish acute pancreatitis mice models. One hundred sixty specific pathogen-free imprinting control region (ICR) female mice were randomly divided into the control group (group A, normal saline), the mild group (group B, caerulein), the severe group (group C, caerulein + lipopolysaccharide), and the intervention group (group D, S100A12 recombinant antibodies + caerulein + lipopolysaccharide); each group had 40 mice. We sampled the blood at 8, 12, and 24 h after the beginning of building animal models. In each period of time, we respectively detected the serum S100A12, amylase (AMY), C-reactive protein (CRP), interleukin (IL-1β, IL-6), and tumor necrosis factor (TNF-α) levels. In addition, we observed and scored the pancreas and lungs histopathology of the mice. In each same period of time compared with group C, serum AMY, CRP, IL-1β, IL-6, TNF-α levels of group D were significantly decreased (p < 0.05). In each same period of time compared with group B and group C, serum S100A12 concentration of group D was significantly decreased (p < 0.05), and the pancreas and lungs histopathology were also much improved. These observations demonstrate that S100A12 recombinant antibodies were able to significantly reduce the severity of acute pancreatitis induced by caerulein and lipopolysaccharide in mice. Serum S100A12 may serve as a useful marker for disease severity and curative effect in mice with severe acute pancreatitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute pancreatitis is the most common pancreatic lesion and its morbidity rate is also showing a trend of rising year by year [1]. Mild acute pancreatitis is a self-limited disease; the prognosis is good, but about 25 % of the patients have severe acute pancreatitis, and the fatality rate is as high as 10–30 % [2, 3]. Once the disease process is initiated, its severity is largely determined by a complex network of activated inflammatory mediators. Inhibiting these mediators and suppressing the extensive inflammatory response may provide a specific therapeutic opportunity.
In the present study, researchers found that in many diseases, such as angiocardiopathy [4–8], inflammatory bowel disease [9–12], acute and chronic lung diseases [13–15], Alzheimer’s disease [16], glomerular nephritis [17], diabetes mellitus type 2 [18], rheumatism [19–21], Kawasaki disease [22, 23], etc., S100A12 had a highly specific expression and played an important role in regulating the inflammation. Nowadays, a number of studies have demonstrated that S100A12 is not a housekeeping protein, but a protein that has selective expressions in the condition of different cell types and cell cycle, and it is closely related to inflammation.
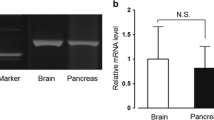
S100A12 is one of the members of the S100 protein family [24]. The gene S100A12 is located in human chromosome 1q21, between S100A8 and S100A9, its code calcium binding protein S100A12, which exists in the form of covalent dimers. At present, the study found that S100A12 has two Ca2+ binding sites—C terminal and N terminal. These two sites are the important basis that show S100A12 differs from other members of the S100 family (as shown in Fig. 1) [25].
S100A12 is made up of four α-helixes, two L-rings, and one hinge area. L-rings are Ca2+ binding sites. There is an α-helix before and after each L-ring. HII and HIII are connected by a hinge area. L1 is a nonconservative structure (also known as pseudo EF hand); L2 is a conservative structure (also known as canonical EF hand).
When S100A12 is stimulated by inflammatory mediators, the target protein binding sites will be exposed. S100A12 will exert its function by combining the corresponding ligands. Therefore, blocking the combination of S100A12 and its corresponding ligands, such as using S100A12 recombinant antibodies to inhibit the function of S100A12, may represent a novel therapeutic strategy for severe acute pancreatitis.
MATERIALS AND METHODS
Experimental Animals
One hundred sixty specific pathogen-free (SPF) imprinting control region (ICR) female mice (weight 21.258 ± 0.933 g) were provided by the animal experiment center of Zhejiang Chinese Medical University. The mice were fed regularly for a week under the appropriate temperature, humidity, and lighting in the animal experiment center. Twelve hours before the experiment, we stopped feeding.
Main Reagent
Caerulein (Cn) and lipopolysaccharide (LPS) were bought from Sigma-Aldrich Co., Ltd.; Mice S100A12 recombinant antibodies were bought from Sino Biological Inc.; Mice S100A12 enzyme-linked immunosorbent assay (ELISA) kit was bought from Elabscience Biotechnology Co., Ltd.; Mice AMY ELISA kit was bought from Cusabio Biotech Co., Ltd.; CRP, IL-1β, IL-6, TNF-α ELISA kits were bought from Shanghai Westang Biological Technology Co., Ltd..
Main Instrument
Dehydrator (STP120, MICROM Co.), embedding machine (AP280-2, MICROM Co.), slicing machine (HM335E, MICROM Co.), microscope (Nikon eclipse 80i, Nikon Co.), charge-coupled device (DS-Fi1, 5 million pixels, Nikon Co.), image analysis software (Carl Zeiss Imaging Systems, Carl Zeiss Co.), and low speed autobalancing centrifuge (LDZ5-2, Beijing Medical Centrifuge Factory) were provided by the animal experiment center of Zhejiang Chinese Medical University; incubator (Saifu Experimental Instrument Factory of Haishu, Ningbo), microplate reader (WellscanMK-3, Labsystems Dragon Co.), etc. were provided by the Life Sciences College of Zhejiang Chinese Medical University.
Building Models
One hundred sixty SPF female ICR mice were completely randomly divided into the control group (group A, weight 21.168 ± 1.022 g, the same hereinafter), the mild group (group B, 21.283 ± 0.915 g), the severe group (group C, 21.215 ± 0.908 g), and the intervention group (group D, 21.365 ± 0.907 g). Each group had 40 mice. Caerulein and lipopolysaccharide were temporarily prepared before the experiment. Mice in group A were intraperitoneally injected with 25 mg/kg normal saline for seven times; every interval time was an hour. Mice in group B were intraperitoneally injected with 50 μg/kg caerulein for seven times; every interval time was an hour. Mice in group C were intraperitoneally injected with 50 μg/kg caerulein for seven times; every interval time was an hour. Five hours after the first injection of caerulein in this group (group C), the mice were intraperitoneally injected with 10 mg/kg lipopolysaccharide. Thirty minutes before the first injection of caerulein in group D, mice were injected with 50 μg/kg S100A12 recombinant antibodies, and the remaining steps are the same as group C.
Blood Tests
We collected the blood at 8, 12, and 24 h after the beginning of the experiment, respectively. We used the eye socket blood-collecting method to take proper amount in 2-ml EP tube, without anticoagulant added. Then, we put the blood into the centrifuge when it was coagulated, centrifuged it at 3000 r/min for 5 min, collected the upper serum, and saved it in the −20 °C refrigerator.
Materials Observing
We used high concentrations of sodium pentobarbital to kill the mice. We then opened the abdomen, removing pancreas and lungs from each mouse, fixed them in 10 % formaldehyde solution, and then, routine paraffin-embedded, sectioned, hematoxylin-eosin (HE) stained, and observed them by optical microscope. Pancreatic pathological alteration was scored by the double-blind method according to Schmidt’s standard [26, 27]. Score standard is shown in Table 1.
Statistical Methods
We used Statistical Product and Service Solutions (SPSS) 17.0 software for statistical processing. Differences between two sample means were analyzed by t test; the data were shown as mean ± standard deviation (\( \overline{x} \) ± SD). Pairwise comparison among multiple experimental groups and one control group were analyzed by LSD test or Dunnett’s test. Pairwise comparison among multiple sample mean were analyzed by S-N-K method. We used the ridit analysis for score class differences. The data were shown as sample numbers (n). Values of p < 0.05 were accepted as significant.
RESULTS
Survival Rate
There was no death in group A, group B, and group D; survival rate was 100 %. Thirty hours after the beginning of the experiment, one mouse in group C was dead; survival rate was 97.5 %.
Serum Tests
In each same period of time compared with group A, amylase (AMY), C-reactive protein (CRP), interleukin (IL-1β, IL-6), tumor necrosis factor (TNF-α), and calcium-binding protein S100A12 levels of group B were increased (p < 0.05), and AMY, CRP, IL-1β, IL-6, TNF-α, and S100A12 levels of group C were significantly increased (p < 0.01). It demonstrated that models were successfully established. In each same period of time compared with group B, S100A12 levels of group D were decreased (p < 0.05). In each same period of time compared with group C, AMY, CRP, IL-1β, IL-6, TNF-α levels of group D were decreased (p < 0.05), and S100A12 levels of group D were significantly decreased (p < 0.01). It suggested that serum S100A12 might serve as a useful marker in severe acute pancreatitis, as shown in Tables 2, 3, 4, 5, 6 and 7.
Macroscopic and Microscopic Observation of Pancreas
Macroscopic observation of pancreas and organs outside the pancreas in group A was generally normal. Pancreas in group B was adhered with surrounding tissues; its glands were swollen, its membranes were tense, its color was pale, but organs outside the pancreas had no obvious abnormal alteration. Pancreas in group C was adhered with surrounding tissues seriously; its glands were swollen, its color was murky gray, several saponified spots and hemorrhagic spots were visible on its surface, and a small amount of saponified spots were appeared on omentum majus, mesentery, etc. The liver was slightly swollen; its color was a little dark. Pancreas in group D had no obvious abnormal appearance; it was slightly adhered with surrounding tissues, and organs outside the pancreas had no obvious abnormal alteration.
Microscopic observation of pancreatic mesenchyme in group A was normal, lobular structures were completed, and there was no hemorrhage or necrosis alteration (Fig. 2: A1, A2). Pancreatic mesenchyme in group B was hyperemia and edema, with inflammatory cells infiltration and a small amount of focal acini necrosis and slight adipocyte necrosis, but hemorrhage was occasionally found (Fig. 2: B1, B2). Pancreatic tissues in group C were serious edema; the distribution of acinar cells were relatively independent (like islands), a large number of glandular cells were necrosis, its structures were fuzzy, necrotic areas were infiltrated by a large number of inflammatory cells (Fig. 2: C1, C2). Pancreatic mesenchyme in group D was slight edema, and there was no vacuolar formation, just some slight adipocyte necrosis and hemorrhage was seldom found (Fig. 2: D1, D2).
Effect of S100A12 recombinant antibodies on pancreatic morphological alterations in severe acute pancreatitis. Sections [A1 (×100), A2 (×400), the same hereinafter] from mice in group A (injected with normal saline). Sections (B1, B2) from mice in group B (injected with caerulein). Sections (C1, C2) from mice in group C (injected with caerulein + lipopolysaccharide). Sections (D1, D2) from mice in group D (injected with S100A12 recombinant antibodies + caerulein + lipopolysaccharide).
Pancreatic Histopathology Score of Each Group
The results of histopathology score showed that compared with group A, pancreas in group B appeared to have serious interstitial edema (p < 0.01) and mild-to-moderate inflammatory infiltration (p < 0.05), but didn’t appear to have obvious parenchyma necrosis and hemorrhage (p > 0.05). Pancreas in group C appeared to have serious interstitial edema, inflammatory infiltration, parenchyma necrosis, and different degrees of hemorrhage (p < 0.01). Pancreas in group D appeared to have mild-to-moderate interstitial edema and inflammatory infiltration (p < 0.05), but didn’t appear to have obvious parenchyma necrosis and hemorrhage (p > 0.05). Compared with group B, pancreatic interstitial edema, inflammatory infiltration, parenchyma necrosis, and hemorrhage in group C were much more serious (p < 0.01), but pancreatic inflammatory infiltration in group D would get better (p < 0.05). Compared with group C, the situation of pancreatic interstitial edema, inflammatory infiltration, parenchyma necrosis, and hemorrhage in group D were significantly improved (p < 0.01), as shown in Table 8.
Optical Microscopic Observation of Lungs
Pulmonary alveoli in group A were generally normal (Fig. 3: A, a). The pulmonary capillaries in group B had mild hyperemia, and inflammatory cells infiltration could be found (Fig. 3: B, b). Pulmonary alveoli in group C were collapsed, and the capillaries of alveolar walls were diffuse expanded and hyperemia, there were exudates, inflammatory cells and a few red blood cells in the alveolar space, and pulmonary mesenchyme was obviously infiltrated by a large number of inflammatory cells (Fig. 3: C, c). Pulmonary mesenchyme in group D was slight edema and just infiltrated by a few inflammatory cells (Fig. 3: D, d).
Pulmonary morphological alterations in severe acute pancreatitis. Sections [A (×100), a (×400), the same hereinafter] from mice in group A (injected with normal saline). Sections (B, b) from mice in group B (injected with caerulein). Sections (C, c) from mice in group C (injected with caerulein + lipopolysaccharide). Sections (D, d) from mice in group D (injected with S100A12 recombinant antibodies + caerulein + lipopolysaccharide), a (×400), the same hereinafter] from mice in group A (injected with normal saline). Sections (B, b) from mice in group B (injected with caerulein). Sections (C, c) from mice in group C (injected with caerulein + lipopolysaccharide). Sections (D, d) from mice in group D (injected with S100A12 recombinant antibodies + caerulein + lipopolysaccharide).
The lungs were the mainly organ involved in the early stage of severe acute pancreatitis, because in the early stage of severe acute pancreatitis, pancreatic enzyme and trypsin could further activate phospholipase, collagenase, chymotrypsin, etc. when they were activated. Phospholipase A2 could not only change the lecithin into hemolytic lecithin, thus destroying the cell biofilm, but could also accelerate the decomposition of lecithin, which was the main component of pulmonary surfactant, thus collapsing the pulmonary alveoli. While activated, trypsin could also activate the kallikreins-kinins system, leading to increasing the permeability of pulmonary cells and the abnormal process of intravascular coagulation. Then, acute lung injury (ALI), which was caused by pulmonary microcirculation embolism, appeared.
Serous and Histological findings
Severe acute pancreatitis was induced by administrating caerulein and lipopolysaccharide; serum AMY, CRP, IL-1β, IL-6, and TNF-α levels were significantly increased compared with those in group A (Table 2–6). S100A12, as a marker of inflammatory response, was also significantly increased (Table 7). Treating mice with S100A12 recombinant antibodies before the injection of caerulein and lipopolysaccharide significantly decreased the changes in these inflammatory mediators (Table 2–7). Histological investigation confirmed the development of severe acute pancreatitis induced by caerulein and lipopolysaccharide. Pancreatic damage, including pancreatic interstitial edema, inflammatory infiltration, parenchyma necrosis, and hemorrhage, was markedly enhanced. Treating mice with S100A12 recombinant antibodies reduced the severity of pancreatic interstitial edema, inflammatory infiltration, parenchyma necrosis, and hemorrhage (Fig. 2 and Table 8).
DISCUSSIONS
Acute pancreatitis is the most common pancreatic lesion, according to the international clinical data, which showed that the annual incidence is up to 5–80/105 and the trend is rising year by year [1]. Each year in the United States, there are more than 200,000 patients with acute pancreatitis who require hospitalization, and the direct cost of treatment is as much as 2,000,000,000 dollars/year [28]. Mild acute pancreatitis is a self-limited disease; the prognosis is good, but about 25 % of the patients have severe acute pancreatitis. The fatality rate is as high as 10–30 % [2, 3]; the hospitalization is prolonged, and the treatment cost is huge, constituting a great threat to human health and social economy. While, what is used at present to judge the severity and prognosis of acute pancreatitis are Ranson score, Glasgow score, APACHE II score, pancreatic enzyme, trypsinogen activation peptide (TAP), etc. [29], but the sensitivity and specificity of these evaluation methods for early diagnosis of severe acute pancreatitis cannot meet the clinical demand, and also have the limitations of complex detection and high cost.
S100A12 is mainly expressed in neutrophils; besides in the blood, it also can be found in cerebrospinal fluid, saliva, synovial fluid, and even in gastrointestinal mucosal and feces. Recent researches suggest that S100A12 plays a key role in inflammation regulation, which has been confirmed with animal experiments by Rouleau, etc. They found that the marrow granulocyte migrated to peripheral blood after intravenous injecting S100A12 on mice, and then activated granulocyte and made it to the area of inflammation [30]. In addition, S100A12 is also involved in the cell signal transduction [31] and resisting to the invasion of bacterial and virus (related to its cuprum sequence [32]). Neutrophils, activated since the early stage of acute pancreatitis, have an important role in regulating the severity of acute pancreatitis; they can release great quantities of cell factors and inflammatory mediators that induce systemic inflammatory response, which is the central link in severe acute pancreatitis [33, 34].
Through the animal experiments, we found that mice in the mild acute pancreatitis group (group B, the early stage of severe acute pancreatitis), its serum S100A12 had already begun to rise; mice in severe acute pancreatitis group (group C), its serum S100A12 rose obviously. By inhibiting the function of S100A12 with S100A12 recombinant antibodies (group D), the situation of mice pancreatic interstitial edema, inflammatory infiltration, parenchyma necrosis, and hemorrhage were significantly improved when compared with mice in the severe acute pancreatitis group (group C). Even compared with mild acute pancreatitis group (group B), mice pancreatic inflammatory infiltration in intervention group (group D) would also get better.
S100A12 is a sensitive marker for inflammation, but our study does not address whether it is specific for pancreatitis. The most notable finding of our study is that an antibody against S100A12 (when administered prior to caerulein and lipopolysaccharide) does block the inflammatory mediators as well as the histological findings of pancreatitis, suggesting that S100A12 is a mediator not just a marker of the inflammatory response in pancreatitis.
We hold great promise that S100A12 can be used to monitor the development and prognosis of severe acute pancreatitis in mice. By inhibiting the expression of S100A12, the excessive activation of neutrophils will be controlled, which will weaken the inflammatory reaction of severe acute pancreatitis by reducing the release of inflammatory mediators; therefore, the severity of acute pancreatitis is reduced. This may represent a novel therapeutic strategy for severe acute pancreatitis.
References
Sekimoto, M., T. Takada, Y. Kawarada, et al. 2006. JPN guidelines for the management of acute pancreatitis: epidemiology, etiology, natural history, and outcome predictors in acute pancreatitis. J Hepatobiliary Pancreat Surg 13: 10–24.
Granger, J., and D. Remick. 2005. Acute pancreatitis: models, markers, and mediators. Shock 24(Suppl 1): 45–51.
Mayerle, J., V. Hlouschek, and M.M. Lerch. 2005. Current management of acute pancreatitis. Nat Clin Pract Gastroenterol Hepatol 2: 473–483.
Scheiber-Camoretti, R., A. Mehrotra, L. Yan, J. Raman, J.F. Beshai, and M.A. Hofmann Bowman. 2013. Elevated S100A12 and sRAGE are associated with increased length of hospitalization after non-urgent coronary artery bypass grafting surgery. Am J Cardiovasc Dis 3(2): 85–90.
Shiotsu, Y., Y. Mori, M. Nishimura, T. Hatta, N. Imada, N. Maki, K. Iida, N. Iwamoto, E. Matsuoka, K. Tamagaki, and A. Kosaki. 2013. Prognostic utility of plasma S100A12 levels to establish a novel scoring system for predicting mortality in maintenance hemodialysis patients: a two-year prospective observational study in Japan. BMC Nephrol 16: 14–16.
Saito, T., Y. Hojo, Y. Ogoyama, et al. 2012. S100A12 as a marker to predict cardiovascular events in patients with chronic coronary artery disease. Circ J 76(11): 2647–2652.
Shiotsu, Y., Y. Mori, M. Nishimura, et al. 2011. Plasma S100A12 level is associated with cardiovascular disease in hemodialysis patients. Clin J Am Soc Nephrol 6(4): 718–723.
Mori, Y., A. Kosaki, N. Kishimoto, et al. 2009. Increased plasma S100A12 (EN-RAGE) levels in hemodialysis patients with atherosclerosis. Am J Nephroi 29(1): 18–24.
Manolakis, A.C., A.N. Kapsoritakis, P. Georgoulias, et al. 2010. Moderate performance of serum S100A12, in distinguishing inflammatory bowel disease from irritable bowel syndrome. BMC Gastroenterol 10: 118.
Foell, D., T. Kucharzik, M. Kraft, et al. 2003. Neutrophil derived human S100A12 (EN-RAGE) is strongly expressed during chronic active inflammatory bowel disease. Gut 52(6): 847–853.
Leach, S.T., Z. Yang, I. Messina, et al. 2007. Serum and mucosal S100 proteins, calprotectin (S100A8/S100A9) and S100A12, are elevated at diagnosis in children with inflammatory bowel disease. Scand J Gastroenterol 42(11): 1321–1331.
Kaiser, T., J. Langhorst, H. Wittkowski, et al. 2007. Faecal S100A12 as a non-invasive marker distinguishing inflammatory bowel disease from irritable bowel syndrome. Gut 56(12): 1706–1713.
Lorenz, E., M.S. Muhlebach, P.A. Tessier, et al. 2008. Different expression ratio of S100A8/A9 and S100A12 in acute and chronic lung diseases. Respir Med 102(4): 567–573.
Foell, D., S. Seeliger, T. Vogl, H.G. Koch, H. Maschek, E. Harms, C. Sorg, and J. Roth. 2003. Expression of S100A12 (EN-RAGE) in cystic fibrosis. Thorax 58(7): 613–617.
Wittkowski, H., A. Stumock, M.A. van Zoelen, et al. 2007. Neutrophil-derived S100A12 in acute lung injury and respiratory distress syndrome. Crit Care Med 35(5): 1369–1375.
Shepherd, C.E., J. Goyette, V. Utter, et al. 2006. Inflammatory S100A9 and S100A12 proteins in Alzheimer’s disease. Neurobiol Aging 27(11): 1554–1563.
Komatsuda, A., H. Ohtani, H. Wakui, et al. 2006. Increased serum levels of S100A12 in patients with MPO-ANCA-associated glomerulonephritis. Clinical Nephrology 66(5): 315–321.
Kosaki, A., T. Hasegawa, T. Kimura, et al. 2004. Increased plasma S100A12 (EN-RAGE) levels in patients with type 2 diabetes. Journal of Clinical Endocrinology Metabolism 89(11): 5423–5428.
Liao, H., J. Wu, E. Kuhn, et al. 2004. Use of mass spectrometry to identify protein biomarkers of disease severity in the synovial fluid and serum of patients with rheumatoid arthritis. Arthritis Rheumatism 50(12): 3792–3803.
Foell, D., D. Kane, B. Bresnihan, et al. 2003. Expression of the pro-inflammatory protein S100A12 (EN-RAGE) in rheumatoid and psoriatic arthritis. Rheumatology (Oxford) 42(11): 1383–1389.
Foell, D., H. Wittkowski, I. Hammerschmidt, et al. 2004. Monitoring neutrophil activation in juvenile rheumatoid arthritis by S100A12 serum concentrations. Arthritis Rheumatism 50(4): 1286–1295.
Ye, F., D. Foell, K. Hirono, et al. 2004. Neutrophil-derived S100A12 is profoundly upregulated in the early stage of acute Kawasaki disease. American Journal of Cardiology 94(6): 840–844.
Foell, D., F. Ichida, T. Vogl, et al. 2003. S100A12 (EN-RAGE) in monitoring Kawasaki disease. Lancet 361(9365): 1270–1272.
Guignard, F., J. Mauel, and M. Markert. 1995. Identification and characterization of a novel human neutrophil protein related to the S100 family. Biochem Journal 309(Pt 2): 395–401.
Pietzsch, J., and S. Hoppmann. 2009. Human S100A12: a novel key player in inflammation? Amino Acids 36(3): 381–389.
Schmidt, J., D.W. Rattner, K. Lewandrowski, C.C. Compton, U. Mandavilli, W.T. Knoefel, and A.L. Warshaw. 1992. A better model of acute pancreatitis for evaluating therapy. Annalytical Surgery 215(1): 44–56.
Schmidt, J., K. Lewandrowski, C. Fernandez-del Castillo, U. Mandavilli, C.C. Compton, A.L. Warshaw, and D.W. Rattner. 1992. Histopathologic correlates of serum amylase activity in acute experimental pancreatitis. Dig Dis Sci 37(9): 1426–1433.
Sandler, R.S., J.E. Everhart, M. Donowitz, et al. 2002. The burden of selected digestive diseases in the United States. Gastroenterology 122: 1500–1511.
Christophe, R., C. Laurence, K. Scott, et al. 2002. Identification of hepatocarcinoma-intestine-pancreas/pancreatitis-associated protein I as a biomarker for pancreatic ductal adenocarcinoma by protein biochip technology. Cancer Research 62: 1868–1875.
Rouleau, P., K. Vandal, C. Rvckman, et al. 2003. The calcium-binding protein S100A12 induces neutrophil adhesion, migration, and release from bone marrow in mouse at concentrations similar to those found in human inflammatory arthritis. Clinical Immunology 107(1): 46–54.
Mikkelsen, S.E., V. Novitskaya, M. Kriajevska, et al. 2001. S100A12 protein is a strong inducer of neurite outgrowth from primary hippocampal neurons. J Neuro 79(4): 767–776.
Gottsch, J.D., S.W. Eisinger, and S.H. Liu. 1999. Calgranulin C has filariacidal and filariastatic activity. Infect Immun 67(12): 6631–6636.
Steer, M. 2002. Pancreatitis severity: who calls the shots? Gastroenterology 122: 1168–1172.
Sandoval, D., A. Gukovskaya, P. Reavey, et al. 1996. The role of neutrophils and platelet-activating factor in mediating experimental pancreatitis. Gastroenterology 111: 1081–1091.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yinchu, Z., Feng, Z., Yinsheng, S. et al. Potential Effects of Calcium Binding Protein S100A12 on Severity Evaluation and Curative Effect of Severe Acute Pancreatitis. Inflammation 38, 290–297 (2015). https://doi.org/10.1007/s10753-014-0032-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-014-0032-x