Abstract
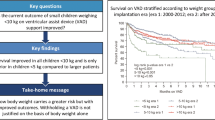
Heart failure is a significant cause of mortality in children with cardiovascular diseases. Treatment of heart failure depends on patients’ symptoms, age, and severity of their condition, with heart transplantation required when other treatments are unsuccessful. However, due to lack of fitting donor organs, many patients are left untreated, or their transplant is delayed. In these patients, ventricular assist devices (VADs) are used to bridge to heart transplant. However, VAD support presents various complications in patients. The aim of this study was to compile, review, and analyse the studies reporting risk factors and aetiologies of complications of VAD support in children. Random effect risk ratios (RR) with 95% confidence intervals were calculated to analyse relative risk of thrombosis (RR = 3.53 [1.04, 12.06] I2 = 0% P = 0.04), neurological problems (RR = 0.95 [0.29, 3.15] I2 = 53% P = 0.93), infection (RR = 0.31 [0.05, 2.03] I2 = 86% P = 0.22), bleeding (RR = 2.57 [0.76, 8.66] I2 = 0% P = 0.13), and mortality (RR = 2.20 [1.36, 3.55] I2 = 0% P = 0.001) under pulsatile-flow and continuous-flow VAD support, relative risk of mortality (RR = 0.45 [0.15, 1.37] I2 = 36% P = 0.16) under left VAD and biVAD support, relative risk of thrombosis (RR = 1.72 [0.46, 6.44] I2 = 0% P = 0.42), infection (RR = 1.77 [0.10, 32.24] I2 = 46% P = 0.70) and mortality (RR = 0.92 [0.14, 6.28] I2 = 45% P = 0.93) in children with body surface area < 1.2 m2 and > 1.2 m2 under VAD support, relative risk of mortality in children supported with VAD and diagnosed with cardiomyopathy and congenital heart diseases (RR = 1.31 [0.10, 16.61] I2 = 73% P = 0.84), and cardiomyopathy and myocarditis (RR = 0.91 [0.13, 6.24] I2 = 58% P = 0.92). Meta-analyses results show that further research is necessary to reduce complications under VAD support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paediatric heart failure is a significant cause of morbidity and mortality in children [1]. In the USA alone, heart failure affects approximately 12,000 to 35,000 patients under the age of 19 years annually [2]. In cases with underlying diseases, including cardiomyopathy and congenital heart disease, early deaths are generally the result of severe heart failure, whilst late deaths are caused by arrhythmias in children where cardiac function does not improve with treatment. Heart failure is linked to cardiomyopathy in approximately 27% of heart failure paediatric patients [2], and congenital heart disease takes place in an estimated 20% of all patients [3].
Treatment of heart failure in paediatric patients depends on symptoms, age, overall health, and the severity of the condition. Numerous pharmacological therapies are used to improve heart failure, including Digoxin, a cardiac glycoside that decreases heart rate and increases ventricular filling, and Beta-blockers which inhibit the release of adrenaline and noradrenaline reducing heart rate. Other pharmacological therapies include diuretics which decrease systemic and pulmonary congestion and angiotensin-converting enzyme (ACE) inhibitors that target ACE activity which is responsible for hormones that narrow blood vessels in order to aid blood pressure control. Therefore, by inhibiting ACE activity, blood vessels relax and widen leading to a reduction in blood pressure and an improved blood flow [3].
Treatment of heart failure can be unsuccessful in severe cases. One of the main reasons for this is that when selecting a medical therapy for paediatric heart failure, the decision usually depends on results recorded in adult heart failure trials, as there is more literature in the adult population, and only a few paediatric guidelines [1]. Therefore, treatment is negatively affected as there are substantial difficulties in employing adult data to paediatric patients due to numerous reasons including, developmental factors, age difference from birth to adolescence, and contrasting gene expression profiling between paediatric and adolescent tissue specimens [4].
Even though medical treatment has been observed to improve survival rate, along with quality of life of paediatric patients suffering from heart failure, there is a substantial percentage of paediatric patients who still have unfortunate outcomes and thus require advanced heart failure treatment, including mechanical support, for instance, VADs, and heart transplantation [5]. However, the present state of donor organ supply with lack of fitting donor organs means that many patients are either left untreated, or their transplant is delayed. In those patients who do not receive a timely heart transplant, VADs are used to bridge the time between the decision to transplant and the actual transplantation itself. The aim of VADs is to either replace the failing ventricle function until heart transplantation or to allow the patients’ heart to recover, by offering additional pumping support. VAD implantation has progressively become a widespread treatment for end-stage heart failure in paediatric patients [6].
The most popular VAD used in the paediatric population is the first-generation Berlin Heart EXCOR pulsatile-flow device (Berlin Heart GmbH, Berlin, Germany), as it can be implanted in patients with a body surface area (BSA) of 0.6 m2 or less. It is placed in a para-corporeal location and offers a range of volume chambers between 10 and 80 mL [7]. The HeartMate II device (Thoratec, Pleasanton, CA) is believed to be a suitable option for paediatric patients with a BSA over 1.3 m2 [8], with over 90% of patients successfully bridged to transplant [9]. Another type of HeartMate device is the HeartMate III (Thoratec, Pleasanton, CA) which is a centrifugal pump [10]. The HeartWare continuous-flow device (HeartWare, HeartWare Systems, Framingham, MA) was designed for patients with BSA under 1.0 m2, and it is a small device that is placed in the pericardial space and does not need a VAD pocket. This centrifugal device offers up to 10 L/min blood flow [11].
Despite their various advantages, VAD support is also observed to cause a wide range of serious adverse events, with bleeding and thromboembolic complications being the most common and most severe [12]. Other adverse events, including infections, sepsis, multi-organ failure, device malfunction, acquired von Willebrand Disease, or neurological injury, have also been recorded. The complications seen with VAD implantation are associated with several factors, but exact causes and mechanisms remain unclear.
The aim of this project is to compile, review, and analyse the studies reporting risk factors and aetiologies of complications under VAD support in paediatric patients.
Methods
The systematic review and the meta-analyses were carried out following PRISMA guidelines. PRISMA is an evidence-based minimum set of items for reporting in systematic reviews and meta-analyses [13, 14].
Research papers describing experiences and outcomes of VAD implantation in the paediatric population indexed in PubMed between 2010 and 2020 were analysed. Publications reporting experiences with VADs and their complications worldwide were included only if their work was published in English along with their native languages. The process of selecting publications and collecting data was completed on 9 July 2020.
The full search strategy adopted during this review was searching various keywords along with VADs and paediatrics. The screening process of eligible publications involved searching keywords for paediatric patients, VAD, LVAD, BiVAD, mortality rates, complications, outcomes, Heartware, Heartmate III, Berlin EXCOR, patient selection process, anti-coagulation used, and duration of VADs. Eligibility for the meta-analysis included more specific variables, including research that compared the two types of devices (pulsatile-flow and continuous-flow), and studies which clearly stated different complication data, as well as BSA and other characteristics.
Eighty papers were identified through the database searching. During the screening process, 9 publications were removed from total 80 publications of as they did not possess all the relevant keywords and data recorded for this analysis. The eligibility process for both qualitative and quantitative analysis excluded further 34 papers out of 71 publications, leaving 37 papers (Fig. 1). Twelve papers were used in the meta-analyses since all 37 papers did not specifically compare devices or complications and only stated overall results. However, these papers were used to report results and complications that arose from VAD experiences. The full flow diagram of the systematic review is given in Fig. 1.
The list of variables sought within the included publications was the patient selection process, including BSA and previous diagnosis causing end-stage heart failure, for instance, cardiomyopathy, congenital heart disease, and myocarditis. The other variables included anticoagulation therapy, VAD type and duration of implant, and outcome of the specific device used, including complications such as neurological events, thrombosis and infections, and survival rates.
The differences between mortality rates and complications of pulsatile-flow and continuous-flow devices, comparing death rates of left (LVAD) and biventricular VAD devices, were included together with correlations between patient BSA with both mortality rate and complications. Also, the differences between the mortality rates of the three most prevalent diseases that cause end-stage heart failure within paediatric patients, cardiomyopathy, congenital heart disease, and myocarditis were analysed. Results were combined and presented in forest plots along with their risk ratios, 95% confidence intervals (CI), and p-values using Review Manager 5.4 (The Cochrane Collaboration, London, UK).
The risk of bias of the individual studies was assessed through Review Manager 5.4; each study was analysed to determine whether they were at low or high risk of the following possible biases: random sequence generation, blinded investigators and patients, blinding of outcome assessor, incomplete outcome data, and selective reporting. The risk of bias tables is given as supplementary materials.1
Results
Thrombosis
The pulsatile-flow Berlin EXCOR VAD has a higher rate of thrombosis compared with the continuous-flow devices, HeartWare and Heartmate, as reported by several studies reviewing rates of thrombosis: for instance, Jordan et al. [15] reported 86 thrombotic events in 204 patients with Berlin EXCOR. In severe cases of thrombosis, pump changes are required, as shown in Polito et al. [16] where 9 out of 25 patients implanted with a Berlin EXCOR, underwent pump changes as a result of thrombosis. Additionally, Hetzer et al. [17] reported 35 pump exchanges due to thrombosis were required out of 122 Berlin EXCOR implanted patients. Another paper using Berlin EXCOR stated that 3 out of their 4 patients developed thrombosis and needed pump exchanges [18]. Also, when comparing the use of Berlin EXCOR in single ventricle and double ventricle patients, researchers discovered that in their 26 single ventricle patients, 7 developed thrombosis and required pump changes [19]. In their 255 double ventricle patients, 103 patients experienced thrombotic events and received pump changes. Furthermore, in another study, they reported that 5 of their 9 Berlin EXCOR patients developed thrombosis [20].
In contrast, when investigating HeartMate II, Cabrera et al. [9] reported only 1 of their 28 patients had thrombosis. Granegger et al. [21] reported that only 2 of their 14 patients developed thrombosis under HeartWare support. Moreover, research investigating both continuous-flow devices in 51 patients reported 4 incidences of thrombosis [22]. Further supporting the belief that continuous-flow devices develop less thrombosis than pulsatile-flow devices, thrombosis was not reported in the case reports investigating HeartMate devices [23,24,25,26].
Neurological complications
When reviewing and analysing the literature, high neurological injury rate was recorded with Berlin EXCOR compared with the continuous-flow devices. For instance, Su et al. [27] reported that 50% of their 10 deaths were due to neurological injury of patients on pulsatile-flow device support. Similarly, another study stated that they had 3 deaths in 9 patients implanted with Berlin EXCOR, and 100% were a result of neurological injury [20]. Additionally, Jordan et al. [15] discovered that 59 out of their 204 Berlin EXCOR patients experienced neurological events. Finally, in another study using Berlin EXCOR, 9 patients out of 25 suffered from neurological injuries whilst on support [16].
Despite most papers reported neurological events in paediatric patients supported with pulsatile-flow devices, neurological events also occur with the support of continuous-flow devices. As shown in a study by Cabrera et al. [9], they reported neurological problems in paediatric patients on HeartMate II.
Infections
Infections are common in patients implanted with VADs and can lead to severe consequences, including sepsis and death. In a pulsatile-flow device study by Schweiger et al. [18] with 4 patients, 1 of their patients developed sepsis. Additionally, Polito et al. [16] reported high cases of infections as 12 of their 25 patients had minor infections and 3 of these later developed sepsis. Chen et al. [28] reported that 50% of the patients suffered from infections under VAD support. Infections are also seen in continuous-flow devices as a study reported that 5 of their 18 HeartWare patients developed infections, compared with 1 patient in their 98 pulsatile-flow patients [29]. Cabrera et al. [9] reported infection in 16 of 28 patients under HeartMate II support.
Bleeding and acquired von Willebrand factor
Bleeding is a significant issue present in paediatric patients on VAD support with all devices. Gossai et al. [30] experienced minor bleeding in 15 out of their 19 patients on pulsatile-flow devices. In another study investigating the use of pulsatile-flow devices, it was reported that in 27 patients, 34 bleeding events occurred [31]. Additionally, Byrnes et al. [32] found that 47% of their 43 pulsatile-flow device implanted patients experienced bleeding events. Steiner et al. [33] also reported major bleeding events in 43% of 68 patients on VAD.
Cabrera et al. [9] reported bleeding in 6 of 28 patients under HeartMate II continuous flow device support. In a study investigating the use of HeartWare in paediatric patients, 42.9% of 14 patients experienced major bleeds, and 28.6% had major bleeding events after eight weeks of implantation [21]. Additionally, another paper reported that major bleeding events were a common cause of death in 205 HeartWare patients [34]. McMillan et al. [35] also stated that 4 out of their 11 paediatric patients had minor bleeds whilst on HeartWare.
Acquired von Willebrand disorder (vWD) results from the activation of vWF through shear stress, caused by the implantation of a VAD, and leads to bleeds. For instance, Gossai et al. [30] found that all of their 10 patients that were diagnosed with acquired vWD had bleeds. Additionally, it was reported by Kubicki et al. [36] that 75% of their acquired vWD patients under VAD support had bleeds. In another study, one patient developed acquired vWD and died as a result of bleeding complications [37].
Mortality under VAD support for the diseases
Overall, congenital heart disease has a higher death rate than other diseases. Hetzer et al. [17] reported the highest mortality rate (53.3%) in patients with congenital heart disease, whereas for cardiomyopathy, it was 26.8% and for myocarditis 17.6%.
Amongst congenital heart disease, single ventricle is believed to have the highest mortality rate in paediatric patients implanted with VADs. Weinstein et al. [19] compared single ventricle with double ventricle patients on Berlin EXCOR and discovered that the single-ventricle patients had a 42.3% death rate, whereas double-ventricle patients had 23.1%. Furthermore, another study reported a 100% mortality rate of their single ventricle patients on Berlin EXCOR support [38]. Additionally, during a study by Chen et al. [28] investigating single-ventricle paediatric patients, they found that 100% of their 3 single ventricle patients died on Berlin EXCOR, whereas 2 out of 6 died on Heartware (33.3%). However, when reviewing six case reports including one patient in each ranging from 18 to 21 years old, there were no deaths reported for both pulsatile-flow and continuous-flow devices [39,40,41,42,43,44]. This contradicts most data stating that the majority of single ventricle patients die whilst on VAD support, especially on the Berlin EXCOR device.
Cardiomyopathy is a prevalent disease amongst patients requiring VAD implants. This is the result of cardiomyopathy patients having high survival rates overall compared with other conditions. Many studies have reported low mortality rates with cardiomyopathy. Vanderpluym et al. [45] reporting that 1 out of 9 cardiomyopathy patients died. Also, McMillan et al. [35] which had 8 cardiomyopathy patients, Owens et al. [23] with 3 patients. and both Hetzer et al. [40] and Pfister et al. [25] with 1 patient all reported no deaths in their cardiomyopathy patients.
For myocarditis, in a number of case reports, including one to two patients, a 100% survival rate was reported in all cases [23, 45]. However, in McMillan et al. [35], the only death of the cohort was the myocarditis patient under VAD support. Hetzer et al. [17] reported that 9 patients out of 17 successfully weaned off VAD support.
Meta-analyses
Meta-analysis results, comparing neurological complications, bleeding, infection, thrombosis, and mortality rates for different type of VADs, supported ventricles; BSA and diseases are shown in Figs. 2, 3, 4 and 5.
Risk ratios for complications and mortality of pulsatile-flow and continuous-flow VAD support are reported in Fig. 2.
Nassar et al. [46] and Sandica et al. [37] reported less thrombus formation under continuous-flow VAD support. Nassar et al. [46] and Redondo et al. [29] reported more favourable VAD support outcome for neurological problems under continuous-flow VAD support, whereas Sandica et al. [37] was in favour of pulsatile-flow VAD support. Nassar et al. [46] reported less infection under continuous-flow VAD support, whilst Redondo et al. [29] and Sandica et al. [37] reported more favourable pump support for pulsatile-flow VADs for infection. Bleeding rates in the patients in Redondo et al. [29] and Sandica et al. [37] were in favour of continuous-flow VAD support. Blume et al. [47] and Redondo et al. [29] reported a better outcome for mortality under continuous-flow VAD support. In contrast, Nassar et al. [46] and Sandica et al. [37] reported higher survival rates under pulsatile-flow VAD support. Forest plot for the mortality under LVAD and BiVAD support is given Fig. 3.
Moreno et al. [48] and Peng et al. [49] reported higher survival rates under BiVAD support, whereas survival rates under LVAD support were higher in Sandica et al. [37], Steiner et al. [33], and Su et al. [27]. Risk ratios for thrombus formation, infection, and mortality for body surface area under VAD support are given in Fig. 4.
Pac et al. [50] reported relatively low thrombus formation for the BSA > 1.2 m2, whereas Schweiger et al. [22] reported similar thrombus formation rates for the BSA > 1.2 m2 and BSA < 1.2 m2. There was less infection in the patients with BSA < 1.2 m2 in Pac et al. [50], whilst Schweiger et al. [22] reported higher infection rates in the patients with BSA < 1.2 m2. All patients with BSA < 1.2 m2 survived under VAD support in Pac et al. [50], whereas Schweiger et al. [22] reported relatively low survival rates in the patients with BSA < 1.2 m2 under VAD support. Risk ratios for deaths in cardiomyopathy, congenital heart disease and myocarditis with VAD support are given in Fig. 5.
Hetzer et al. [17] reported a lower risk of death for the patients with cardiomyopathy than the patients with congenital heart disease under VAD support. However, Su et al. [27] reported a higher risk for patients with cardiomyopathy under VAD support. Hetzer et al. [17] and Pac et al. [50] reported higher survival rates for patients with myocarditis than patients with cardiomyopathy. On the other hand, Mcmillan et al. [35] were in favour of VAD support for cardiomyopathy cases.
Discussion
In this review, it was shown that although VAD support can help bridge paediatric patients to transplant and help the heart recover its function in some cases, the devices initiate numerous complications, including infections, neurological injury, bleeding, and thromboembolic events [12].
Currently, there are various factors believed to cause thrombosis, including device material, infection, and inadequate anticoagulation, with rate of thrombosis increasing with the duration of implantation [51]. As highlighted by the results, pulsatile-flow devices have a higher thrombotic rate than continuous-flow devices. This could be due to the device design as pulsatile-flow devices are prone to stagnating flow. The chamber of these devices fills with blood which is then ejected by a membrane. At every cycle, as the refilling of the chamber takes time, there is increased particle residence with red blood cells accumulating, resulting in thrombosis arising in the stagnation regions [52]. The main issue with Berlin EXCOR is a 20–30% risk for neurologic complications when supporting the systemic ventricle. This high stroke rate is caused mainly by thrombus formation on the valves of the device [53]. Continuous-flow devices have lower rates of thrombosis as they are not only smaller devices, but also have programmed pump speeds to avoid thrombosis [54]. However, various studies still report high rates of thrombosis in continuous-flow devices. It is believed that continuous-flow devices develop thrombosis due to the rotors in the continuous-flow pump which can cause elevated shear stresses, primary cause of pump thrombosis [51].
Additionally, thrombus formation frequently found on the rotor has been linked to the heat generated by the pump, regardless of design changes to reduce rotation-generated heat [55]. These issues were targeted when inventing HeartWare as it contains a magnetically levitated rotor and can achieve the same amount of flow as axial devices, but at significantly lower rotational speed due to their large rotor diameter [4], explaining why third-generation devices have less thrombosis than pulsatile-flow devices.
Another device-related factor believed to create pump thrombosis is the increase in lactate dehydrogenase levels at high VAD power, stated by Peng et al. [49] when investigating HeartWare thrombosis in two patients. This is supported by another study that reported high dehydrogenase levels and high blood pressure in patients with thrombosis [21].
Both continuous and pulsatile-flow devices experience neurological complications; however, the Berlin EXCOR device is seen to have a much higher rate. Despite this pulsatile-flow device having excellent survival rates as approximately 84% of patients on this device is bridged to transplant [29], its main issue is the approximate 25–31% risk for neurologic injury [53]. This was demonstrated in a study where 30.61% experiences neurological injury [29]. This high neurological injury rate has been linked to thrombus formation on the polyurethane tri-leaflet valves of the device as a result of backflow [53]. It has been suggested by various researchers that with a strict anticoagulation procedure and experienced medical staff, the rate of neurological complications related to thrombosis could be reduced [37]. The high occurrence of neurological complications in pulsatile-flow VADs could be also linked to the duration of the implant, with researchers reporting no neurological events in 80.7% of patients with VADs for < 90 days [16]. Neurological complications have been reported in continuous-flow devices at a much lower rate than pulsatile-flow devices [56].
Bleeding is the most common issue faced post-implantation of VADs as it leads to re-operation up to 60% of patients [57]. It is more common in paediatric patients on either BiVAD support, those needing anticoagulation before VAD implantation and those with severe diagnosis [58]. Bleeding events can occur due to the high shear stresses caused by the VAD system, resulting in erythrocytes haemolysis and the development of acquired vWD [57, 59].
Additionally, patients placed on continuous-flow devices may be at higher risk for the development of platelet dysfunction [60] and should be screened for acquired vWD [61]. In a study, they found that most patients on continuous-flow devices developed acquired vWD [62], and in another report, one patient diagnosed with this disorder experienced several bleeding episodes whilst on continuous support eventually resulting in death [37].
Therapies to control acquired vWD are limited. However, in a study by Nubret et al. [63], they managed to control this factor in a child with dilated cardiomyopathy and BiVAD support that experienced persistent bleeding by changing anti-coagulant therapy from heparin to wilfactin. Additionally, treatment of acquired vWD is also being investigated by using VWF-containing concentrate, for instance, Humate-P to control bleeding before restarting anticoagulation [64].
Infections are also a common complication linked to VAD support, recorded in approximately 50–69% of patients [54]. As infections can lead to severe cases of sepsis and death, controlling this complication is paramount. Infections frequently arise as a result of prolonged hospitalisation time and invasive treatment [54], for instance, re-exploration due to pump thrombosis. Moreover, infections are believed to induce pro-coagulant response which can complicate anticoagulation therapy [65].
Cardiomyopathy is the most prevalent disease seen in patients requiring VAD implantation, which is considered a successful treatment option for these patients [54]. This is proven when considering the cardiomyopathy patients on the waiting list for heart transplants, where VAD implantation was not included as a risk factor for fatality [66]. VAD support can be implanted for extended amounts of time, making it an ideal treatment in different circumstances [54].
Moreover, VAD support is a successful bridge to recovery [54] for those paediatric patients with heart failure caused by myocarditis as most successfully wean off support [67]. Additionally, paediatric patients implanted with VAD support straight after heart failure diagnosis were more likely to wean off support [54]. This could be due to early VAD implantation allowing the ventricle not to overwork, therefore halting heart failure progression [54]. Implanting VAD support into congenital heart disease patients is still challenging [68] as they need additional device insertion alterations and anticoagulation therapy [35]. Therefore, it is essential to appropriately evaluate the anatomy of the patient before implantation, taking into consideration any prior cardiac procedures [29]. Compared with cardiomyopathy paediatric patients, congenital heart disease patients have a much lower survival rate with patients over 10 years old being more likely to live compared with infants under a year [68].
Approximately 15% of heart failure patients supported with VAD require Biventricular VAD support [69]. However, BiVAD support has an overall higher death rate than LVAD support as shown in the results section. This could be because the use of BiVAD support is linked to extensive operative and bypass times, as well as an increased rate of postoperative bleeds [58]. Furthermore, BiVAD lower survival rates have led to reduced use [70], which could have influenced by the negative results reported by numerous studies in BiVAD patients [69].
Numerous studies have reported that paediatric patients under 1 year of age do have a lower survival rate than those between the ages of 11–19 [47]. This could explain the higher mortality in pulsatile-flow compared with continuous flow devices, as pulsatile-flow VADs are predominantly utilised in both younger and smaller patients, whereas continuous-flow devices are mainly used in older paediatric patients [47]. Moreover, weight is considered an important factor during patient selection for VAD support, especially in younger paediatric patients [7]: 64% patients under 5 kg died compared with only 25% of patients between 5 and 10 kg in Navaratnam et al. [7]. However, the relation between weight and BSA with VAD mortality has not yet been confirmed, thus making it difficult to determine whether they influence outcomes. In Conway et al. [34], the authors found no statistically significant difference in survival with different BSA groups; however, there was a slight trend toward inferior outcomes in smaller paediatric patients, but the disease complexity in the smaller patients could be a confounding factor [34].
The majority of studies had similar limitations with the commonest being the small sample size. Additionally, some studies did report non-randomised methods, thus making them at high risk of random sequence bias. Also, as the meta-analysis contained contradicting results in some of the analysis, these conclusions could not be confirmed.
In conclusion, paediatric VAD support has led to high survival rates, of approximately 86% [29], in heart failure patients as they are bridged to heart transplants, as well as allowing a small percentage of these to wean off support with a stronger heart. However, VADs are seen to lead to a number of complications, including, thrombosis, neurological injury, infections, and bleeding. Further studies reporting clinical experience, and research into minimising these complications by improving the devices in terms of material and size, are vital for the future of VAD therapy in heart failure.
References
Das BB (2018) Current State of Pediatric Heart Failure. Children (Basel) 5:. https://doi.org/10.3390/children5070088
Rossano JW, Kim JJ, Decker JA et al (2012) Prevalence, morbidity, and mortality of heart failure-related hospitalizations in children in the United States: a population-based study. J Cardiac Fail 18:459–470. https://doi.org/10.1016/j.cardfail.2012.03.001
Jayaprasad N (2016) Heart failure in children heart views 17:92–99. https://doi.org/10.4103/1995-705X.192556
Patel MD, Mohan J, Schneider C, et al (2017) Pediatric and adult dilated cardiomyopathy represent distinct pathological entities. JCI Insight 2:. https://doi.org/10.1172/jci.insight.94382
Shin YR, Park Y-H, Park HK (2019) Pediatric ventricular assist device. Korean Circ J 49:678–690. https://doi.org/10.4070/kcj.2019.0163
Huang JY, Monagle P, Massicotte MP, VanderPluym CJ (2018) Antithrombotic therapies in children on durable ventricular assist devices: a literature review. Thromb Res 172:194–203. https://doi.org/10.1016/j.thromres.2018.02.145
Navaratnam M, Maeda K, Hollander SA (2019) Pediatric ventricular assist devices: bridge to a new era of perioperative care. Pediatr Anesth 29:506–518. https://doi.org/10.1111/pan.13609
Adachi I, Burki S, Zafar F, Morales DLS (2015) Pediatric ventricular assist devices. J Thorac Dis 7:2194–2202. https://doi.org/10.3978/j.issn.2072-1439.2015.12.61
Cabrera AG, Sundareswaran KS, Samayoa AX et al (2013) Outcomes of pediatric patients supported by the HeartMate II left ventricular assist device in the United States. J Heart Lung Transplant 32:1107–1113. https://doi.org/10.1016/j.healun.2013.07.012
Mehra MR, Goldstein DJ, Uriel N et al (2018) Two-year outcomes with a magnetically levitated cardiac pump in heart failure. N Engl J Med 378:1386–1395. https://doi.org/10.1056/NEJMoa1800866
Chopski SG, Moskowitz WB, Stevens RM, Throckmorton AL (2017) Mechanical circulatory support devices for pediatric patients with congenital heart disease. Artif Organs 41:E1–E14. https://doi.org/10.1111/aor.12760
Hetzer R, Stiller B (2006) Technology insight: use of ventricular assist devices in children. Nat Clin Pract Cardiovasc Med 3:377–386. https://doi.org/10.1038/ncpcardio0575
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Jordan LC, Ichord RN, Reinhartz O et al (2015) Neurological complications and outcomes in the Berlin Heart EXCOR® pediatric investigational device exemption trial. J Am Heart Assoc 4:e001429. https://doi.org/10.1161/JAHA.114.001429
Polito A, Netto R, Soldati M et al (2013) Neurological complications during pulsatile ventricular assistance with the Berlin Heart EXCOR in children: incidence and risk factors. Artif Organs 37:851–856. https://doi.org/10.1111/aor.12075
Hetzer R, Kaufmann F, Delmo Walter EM (2016) Paediatric mechanical circulatory support with Berlin Heart EXCOR: development and outcome of a 23-year experience. Eur J Cardiothorac Surg 50:203–210. https://doi.org/10.1093/ejcts/ezw011
Schweiger M, Schrempf J, Sereinigg M et al (2013) Complication profile of the Berlin Heart EXCOR biventricular support in children. Artif Organs 37:730–735. https://doi.org/10.1111/aor.12062
Weinstein S, Bello R, Pizarro C, et al (2014) The use of the Berlin Heart EXCOR in patients with functional single ventricle. J Thorac Cardiovasc Surg 147:697–704; discussion 704–705. https://doi.org/10.1016/j.jtcvs.2013.10.030
Iyengar A, Hung ML, Asanad K et al (2017) Association between hematologic and inflammatory markers and 31 thrombotic and hemorrhagic events in Berlin Heart Excor patients. Pediatr Cardiol 38:770–777. https://doi.org/10.1007/s00246-017-1578-9
Granegger M, Thamsen B, Schlöglhofer T et al (2020) Blood trauma potential of the HeartWare Ventricular Assist Device in pediatric patients. J Thorac Cardiovasc Surg 159:1519-1527.e1. https://doi.org/10.1016/j.jtcvs.2019.06.084
Schweiger M, Miera O, de By TMMH et al (2018) Cerebral strokes in children on intracorporeal ventricular assist devices: analysis of the EUROMACS Registry. Eur J Cardiothorac Surg 53:416–421. https://doi.org/10.1093/ejcts/ezx342
Owens WR, Bryant R, Dreyer WJ et al (2010) Initial clinical experience with the HeartMate II ventricular assist system in a pediatric institution. Artif Organs 34:600–603. https://doi.org/10.1111/j.1525-1594.2009.00970.x
Marey G, McHugh KM, Sakhitab-Kerestes AM, et al (2019) HeartMate III as a bridge to transplantation in an adolescent with failed Fontan circulation. JACC: Case Reports 1:512–515. https://doi.org/10.1016/j.jaccas.2019.09.013
Pfister R, Kirsch M, Natterer J et al (2020) Implantation of a HeartMate 3 in a 13-year-old child with dilated cardiomyopathy. Pediatr Cardiol 41:423–424. https://doi.org/10.1007/s00246-019-02229-6
Lowry AW, Adachi I, Gregoric ID et al (2012) The potential to avoid heart transplantation in children: outpatient bridge to recovery with an intracorporeal continuous-flow left ventricular assist device in a 14-year-old. Congenit Heart Dis 7:E91-96. https://doi.org/10.1111/j.1747-0803.2012.00659.x
Su JA, Menteer J (2017) Outcomes of Berlin Heart EXCOR® pediatric ventricular assist device support in patients with restrictive and hypertrophic cardiomyopathy. Pediatr Transplant 21:e13048. https://doi.org/10.1111/petr.13048
Chen S, Rosenthal DN, Murray J et al (2020) Bridge to transplant with ventricular assist device support in pediatric patients with single ventricle heart disease. ASAIO J 66:205–211. https://doi.org/10.1097/MAT.0000000000000983
Redondo A, Davies B, Jones R et al (2019) Durable mechanical circulatory support in paediatric heart failure: the experience at Great Ormond Street Hospital. Cirugía Cardiovascular 26:30–34. https://doi.org/10.1016/j.circv.2018.12.002
Gossai N, Brown NM, Ameduri R et al (2016) Pediatric acquired von Willebrand disease with Berlin Heart Excor Ventricular Assist Device Support. World J Pediatr Congenit Heart Surg 7:614–618. https://doi.org/10.1177/2150135116651836
Rosenthal DN, Lancaster CA, McElhinney DB et al (2017) Impact of a modified anti-thrombotic guideline on stroke in children supported with a pediatric ventricular assist device. J Heart Lung Transplant 36:1250–1257. https://doi.org/10.1016/j.healun.2017.05.020
Byrnes JW, Frazier E, Tang X et al (2014) Hemorrhage requiring surgical intervention among children on pulsatile ventricular assist device support. Pediatr Transplant 18:385–392. https://doi.org/10.1111/petr.12266
Steiner ME, Bomgaars LR, Massicotte MP, Berlin Heart EXCOR, Pediatric VADIDE, study investigators, (2016) Antithrombotic therapy in a prospective trial of a pediatric ventricular assist device. ASAIO J 62:719–727. https://doi.org/10.1097/MAT.0000000000000434
Conway J, Miera O, Adachi I et al (2018) Worldwide experience of a durable centrifugal flow pump in pediatric patients. Semin Thorac Cardiovasc Surg 30:327–335. https://doi.org/10.1053/j.semtcvs.2018.03.003
Nelson McMillan K, Hibino N, Brown EE et al (2019) HeartWare Ventricular Assist Device Implantation for pediatric heart failure—a single center approach. Artif Organs 43:21–29. https://doi.org/10.1111/aor.13344
Kubicki R, Stiller B, Kroll J et al (2019) Acquired von Willebrand syndrome in paediatric patients during mechanical circulatory support. Eur J Cardiothorac Surg 55:1194–1201. https://doi.org/10.1093/ejcts/ezy408
Sandica E, Blanz U, Mime LB et al (2016) Long-term mechanical circulatory support in pediatric patients. Artif Organs 40:225–232. https://doi.org/10.1111/aor.12552
Mackling T, Shah T, Dimas V et al (2012) Management of single-ventricle patients with Berlin Heart EXCOR Ventricular Assist Device: single-center experience. Artif Organs 36:555–559. https://doi.org/10.1111/j.1525-1594.2011.01403.x
Niebler RA, Ghanayem NS, Shah TK et al (2014) Use of a HeartWare ventricular assist device in a patient with failed Fontan circulation. Ann Thorac Surg 97:e115-116. https://doi.org/10.1016/j.athoracsur.2013.11.075
Hetzer R, Miera O, Photiadis J et al (2014) Heart transplantation after longest-term support with ventricular assist devices. Ann Thorac Surg 98:1814–1815. https://doi.org/10.1016/j.athoracsur.2013.12.052
Adachi I, Jeewa A, Burki S et al (2016) Outpatient management of a child with bidirectional Glenn shunts supported with implantable continuous-flow ventricular assist device. J Heart Lung Transplant 35:688–690. https://doi.org/10.1016/j.healun.2016.01.1218
Hoganson DM, Boston US, Gazit AZ et al (2015) Successful bridge through transplantation with Berlin heart ventricular assist device in a child with failing Fontan. Ann Thorac Surg 99:707–709. https://doi.org/10.1016/j.athoracsur.2014.04.064
Morales DLS, Adachi I, Heinle JS, Fraser CD (2011) A new era: use of an intracorporeal systemic ventricular assist device to support a patient with a failing Fontan circulation. J Thorac Cardiovasc Surg 142:e138-140. https://doi.org/10.1016/j.jtcvs.2011.05.018
Halaweish I, Ohye RG, Si MS (2015) Berlin heart ventricular assist device as a long-term bridge to transplantation in a Fontan patient with failing single ventricle. Pediatr Transplant 19:E193-195. https://doi.org/10.1111/petr.12607
VanderPluym JH, Robertson CMT, Joffe AR et al (2017) Neurologic, neurocognitive, and functional outcomes in children under 6 years treated with the Berlin Heart Excor Ventricular Assist Device. ASAIO J 63:207–215. https://doi.org/10.1097/MAT.0000000000000462
Nassar MS, Hasan A, Chila T et al (2017) Comparison of paracorporeal and continuous flow ventricular assist devices in children: preliminary results†. Eur J Cardiothorac Surg 51:709–714. https://doi.org/10.1093/ejcts/ezx006
Blume ED, VanderPluym C, Lorts A et al (2018) Second annual Pediatric Interagency Registry for Mechanical Circulatory Support (Pedimacs) report: Pre-implant characteristics and outcomes. J Heart Lung Transplant 37:38–45. https://doi.org/10.1016/j.healun.2017.06.017
Moreno GE, Charroqui A, Pilán ML et al (2011) Clinical experience with Berlin Heart Excor in pediatric patients in Argentina: 1373 days of cardiac support. Pediatr Cardiol 32:652–658. https://doi.org/10.1007/s00246-011-9949-0
Peng E, Kirk R, Wrightson N et al (2016) An extended role of continuous flow device in pediatric mechanical circulatory support. Ann Thorac Surg 102:620–627. https://doi.org/10.1016/j.athoracsur.2016.02.013
Pac M, Kocabeyoglu SS, Kervan U et al (2018) Third generation ventricular assist device: mid-term outcomes of the HeartWare HVAD in pediatric patients. Artif Organs 42:141–147. https://doi.org/10.1111/aor.12989
Fatullayev J, Samak M, Sabashnikov A, et al (2015) Continuous-flow left ventricular assist device thrombosis: a danger foreseen is a danger avoided. Med Sci Monit Basic Res 21:141–144. https://doi.org/10.12659/MSMBR.894840
Corbett SC, Ajdari A, Coskun AU, Nayeb-Hashemi H (2010) Effect of pulsatile blood flow on thrombosis potential with a step wall transition. ASAIO J 56:290–295. https://doi.org/10.1097/MAT.0b013e3181db2476
Beasley GS, Nelson-McMillan K, Vricella L et al (2019) Direct echocardiographic imaging of Berlin heart valves can aid in early detection of Berlin heart valve dysfunction. ASAIO J 65:e4–e6. https://doi.org/10.1097/MAT.0000000000000756
Miller JR, Lancaster TS, Eghtesady P (2015) Current approaches to device implantation in pediatric and congenital heart disease patients. Expert Rev Cardiovasc Ther 13:417–427. https://doi.org/10.1586/14779072.2015.1021786
Kilic A, Acker MA, Atluri P (2015) Dealing with surgical left ventricular assist device complications. J Thorac Dis 7:2158–2164. https://doi.org/10.3978/j.issn.2072-1439.2015.10.64
Schweiger M, Vanderpluym C, Jeewa A et al (2015) Outpatient management of intra-corporeal left ventricular assist device system in children: a multi-center experience. Am J Transplant 15:453–460. https://doi.org/10.1111/ajt.13003
Goldstein DJ, Beauford RB (2003) Left ventricular assist devices and bleeding: adding insult to injury. Ann Thorac Surg 75:S42-47. https://doi.org/10.1016/s0003-4975(03)00478-8
Hehir DA, Niebler RA, Brabant CC et al (2012) Intensive care of the pediatric ventricular assist device patient. World J Pediatr Congenit Heart Surg 3:58–66. https://doi.org/10.1177/2150135111420888
Uriel N, Pak S-W, Jorde UP et al (2010) Acquired von Willebrand syndrome after continuous-flow mechanical device support contributes to a high prevalence of bleeding during long-term support and at the time of transplantation. J Am Coll Cardiol 56:1207–1213. https://doi.org/10.1016/j.jacc.2010.05.016
Sherwin J, Thompson E, Hill KD et al (2018) Clinical pharmacology considerations for children supported with ventricular assist devices. Cardiol Young 28:1082–1090. https://doi.org/10.1017/S1047951118001075
Miera O, Potapov EV, Redlin M et al (2011) First experiences with the HeartWare ventricular assist system in children. Ann Thorac Surg 91:1256–1260. https://doi.org/10.1016/j.athoracsur.2010.12.013
Meyer AL, Malehsa D, Budde U et al (2014) Acquired von Willebrand syndrome in patients with a centrifugal or axial continuous flow left ventricular assist device. JACC Heart Fail 2:141–145. https://doi.org/10.1016/j.jchf.2013.10.008
Nubret K, Mauriat P, Roubertie F et al (2013) Acquired von Willebrand disease in a child with a ventricular assist device. J Thorac Cardiovasc Surg 146:e30–e32. https://doi.org/10.1016/j.jtcvs.2013.06.023
Gill JC, Ewenstein BM, Thompson AR et al (2003) Successful treatment of urgent bleeding in von Willebrand disease with factor VIII/VWF concentrate (Humate-P): use of the ristocetin cofactor assay (VWF:RCo) to measure potency and to guide therapy. Haemophilia 9:688–695. https://doi.org/10.1046/j.1351-8216.2003.00816.x
Hannan MM, Husain S, Mattner F et al (2011) Working formulation for the standardization of definitions of infections in patients using ventricular assist devices. J Heart Lung Transplant 30:375–384. https://doi.org/10.1016/j.healun.2011.01.717
Kirk R, Naftel D, Hoffman TM et al (2009) Outcome of pediatric patients with dilated cardiomyopathy listed for transplant: a multi-institutional study. J Heart Lung Transplant 28:1322–1328. https://doi.org/10.1016/j.healun.2009.05.027
Pirooz E, Almond Christopher SD, Christine T et al (2013) Post-transplant outcomes of children bridged to transplant with the Berlin Heart EXCOR Pediatric Ventricular Assist Device. Circulation 128:S24–S31. https://doi.org/10.1161/CIRCULATIONAHA.112.000446
Dipchand AI, Richard K, Naftel DC et al (2018) Ventricular assist device support as a bridge to transplantation in pediatric patients. J Am Coll Cardiol 72:402–415. https://doi.org/10.1016/j.jacc.2018.04.072
Shugh SB, Riggs KW, Morales DLS (2019) Mechanical circulatory support in children: past, present and future. Transl Pediatr 8:269–277. https://doi.org/10.21037/tp.2019.07.14
Zafar F, Jefferies JL, Tjossem CJ et al (2015) Biventricular Berlin Heart EXCOR pediatric use across the United States. Ann Thorac Surg 99:1328–1334. https://doi.org/10.1016/j.athoracsur.2014.09.078
Funding
The work has been funded by the Engineering and Physical Sciences Research Council (EP/N02124X/1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Silvia Schievano is consultant for Medtronic. Andrea Nicola George, Tain-Yen Hsia, and Selim Bozkurt report no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
George, A.N., Hsia, TY., Schievano, S. et al. Complications in children with ventricular assist devices: systematic review and meta-analyses. Heart Fail Rev 27, 903–913 (2022). https://doi.org/10.1007/s10741-021-10093-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10093-x