Abstract
Parkinson’s disease (PD) is a neurodegenerative disorder that affects over 10 million aging people worldwide. This condition is characterized by the degeneration of dopaminergic neurons in the pars compacta region of the substantia nigra (SNpc) and by aggregation of proteins, commonly α-synuclein (SNCA). The formation of Lewy bodies that encapsulate aggregated proteins in lipid vesicles is a hallmark of PD. Glycosylation of proteins and neuroinflammation are involved in the pathogenesis. SNCA has many posttranslational modifications and interacts with components of membranes that affect aggregation. The large membrane lipid dolichol accumulates in the brain upon age and has a significant effect on membrane structure. The replacement of dopamine and dopaminergic neurons are at the forefront of therapeutic development. This review examines the role of membrane lipids, glycolipids, glycoproteins and dopamine in the aggregation of SNCA and development of PD. We discuss the SNCA-dopamine-neuromelanin-dolichol axis and the role of membranes in neuronal stem cells that could be a regenerative therapy for PD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a neurodegenerative disorder that develops in about 1% of the aging population and is characterized by the degeneration and cell death of dopaminergic neurons in the midbrain, initially in the substantia nigra pars compacta (SNpc). This degeneration leads to a reduced concentration of circulating dopamine (DA) neurotransmitter. Ten million people worldwide live with PD and experience symptoms such as motor dysfunctions, rigidity, tremor and more. There are many potential and mostly unknown causes of PD where about 10% are genetically based. The major problem appears to be synucleinopathy, i.e. increased aggregation of α-synuclein (SNCA) that accumulates in cytoplasmic inclusions (Lewy bodies) consisting mainly of misfolded and aggregated SNCA together with ubiquitin and membrane components [1,2,3]. High concentrations of both SNCA and gangliosides are present in presynaptic membranes. SNCA interacts with membranes in which specific lipids and gangliosides influence its folding and oligomerization. PD is also associated with neuronal inflammation, oxidative stress, as well as lysosomal and mitochondrial dysfunction [4]. The mechanism of cell death in PD is complex and not well understood.
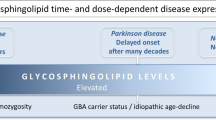
Mutations in the SNCA gene were shown to be associated with a high degree of SNCA aggregation [5,6,7]. Other genetic links include mutations in the genes encoding PARK1, PARK12 and others [8]. Most of the PD cases appear to be sporadic and of unknown causes. In about 10% of PD patients a glucocerebrosidase mutation was found, similar to Gaucher’s disease, and this association indicates a significant risk factor for PD [9]. The decreased activity of mutant glucocerebrosidase causes increases in the concentrations of glucocerebroside (GlcCer) in membranes throughout the brain [10]. However, the activity of this enzyme appears to be low in PD patients even in the absence of mutations. NMR studies suggest that glucocerebrosidase associates with acidic residues and possibly Tyr residues at the C-terminus of SNCA [11].
Aging is a key factor for developing PD and among many age-related alterations, specific membrane lipids and glycosphingolipids (GSL) change upon aging [12, 13]. Despite of a large amount of scientific data, mainly on animal and cell models, it is still unknown which features of aging contribute to PD. Humans accumulate dolichol (Dol) up to 21-fold in the aging brain [14]. Dol is known to disrupt membrane structure and functions [15, 16] and binds to melanin, the dark pigment of SNpc which also accumulates with age [17, 18].
Although SNCA functions normally as a presynaptic protein for many decades, at about age 60 it starts in vulnerable PD patients to form toxic oligomers and fibrous aggregates that cause neuronal cell death, formation of Lewy bodies, synaptic dysfunction and the symptoms of PD. The question is why dopaminergic neurons are preferentially affected in PD patients and why SNCA is the aggregating protein while in other age-related neurodegenerative diseases different proteins aggregate.
SNCA is a small 14 kDa unstructured protein that associates with the membrane due to its amphipathic properties. Under certain conditions SNCA can change conformation that predisposes it to oligomerization and fibrillar aggregation to form cytotoxic species [19, 20]. This process can be caused by overexpression of SNCA [21, 22], SNCA mutations, changes in posttranslational modifications (Table 1) or alterations in membrane composition. The different oligomeric types exist in a dynamic equilibrium and toxic oligomers slowly form fibrils that cannot be degraded [23, 24].
The microenvironments of lipids in membranes, vesicles and lipid rafts determine the functional properties of membranes, and SNCA oligomerization and aggregation is controlled by interactions with membrane lipids and glycolipids [20, 25,26,27,28,29,30,31]. However, the exact mechanisms underlying SNCA misfolding and aggregation remain unknown.
The loss of DA in PD is partially restored with Levodopa (L-DOPA) medications that cross the blood brain barrier (BBB) [32] and are converted to DA in neurons. However, long-term effective neuroprotective or restorative therapies remain to be developed. Research on pluripotent stem cells that differentiate into dopaminergic neurons has brought hope for the restoration of dopaminergic neurons [33, 34].
Several cell and animal models are available that can answer specific questions on pathological mechanisms such as dopaminergic cell death and SNCA aggregation mechanisms, mutations and membrane changes and can be used to assess the effectiveness and toxicity of new pharmacological agents. However, there is no model that has all the features of PD, especially since the causes of sporadic PD are still unknown and the disease is multi-faceted. Cellular models are also useful to study specific aspects of the loss of non-dopaminergic cells [35]. Lund human mesencephalic (LUHMES) cells are immortalized human neuronal cells that can differentiate to dopaminergic cells [36]. The human neuroblastoma cell line SH-SY5Y and rat pheochromocytoma cell line PC12 have been extensively used since they produce catecholamines and can develop neuron-like properties such as the formation of neurites.
Glycosphingolipid changes have been observed in PD and levels of GM1 are low in the SNpc of PD patients [27], but the mechanisms of these changes need to be determined. The effect of ganglioside accumulation and deprivation and the role of SNCA mutations have been examined in mouse models of PD. One of the enzymes that synthesizes GM1 is β1,4-GalNAc-transferase B4GALNT1. B4GALNT1 gene knockout mice lack the major brain gangliosides such as GM2, GD2 and GM1 [37]. These mice show PD symptoms, including motor impairment upon aging, loss of dopaminergic neurons and aggregation of SNCA, as well as non-motor symptoms that can be reversed by GM1 analog treatment.
There is no specific biochemical or cellular test for PD, and the diagnosis is based on the presence of clinical features such as motor deficits and the response to L-DOPA. The search for biomarkers continues, and may well include membrane components that are commonly found in neurodegenerative disease such as PD, Alzheimer’s or Huntington’s disease.
Alterations in the composition of special membrane areas named lipid rafts may be observed before PD symptoms appear [38, 39]. Metabolites related to lipid oxidation and oxidative stress could support an inflammatory environment in the brain [40]. The neuroinflammation in PD patients has also been attributed in part to advanced glycation end products (AGE) that increase with age and cause inflammation by binding to the AGE receptor RAGE [41]. Metabolites of glycated proteins form AGE that are considered pro-inflammatory mediators involved in neurodegeneration [42]. The N-glycosylation patterns of Immunoglobulin G (IgG) have been suggested to be novel biomarkers of PD [43]. Several of the N-glycan structures of IgG from PD patients were different from normal and the IgG glycome may be a marker for PD. These specific glycoforms of IgG may be related to a state of low-grade inflammation. However, differences in N-glycosylation of IgG have previously been observed in several other inflammatory diseases and cancer [43].
In this review we discuss the lipid and glycoconjugate components of neuronal membranes including Dol and focus on their relationship with SNCA and DA. We will summarize the therapies available for PD treatment and evaluate the potential of neural stem cells for restoration of dopaminergic neurons in PD.
Pathophysiology of Parkinson’s disease
Many possible factors are thought to cause the pathogenesis of PD that includes progressive slowing of physical movement and loss of coordination among many other symptoms. Aging is the greatest risk factor for PD but the specific changes responsible need to be determined. Sporadic occurrence of PD contributes to at least 80% of cases and SNCA is the most common protein to aggregate. Hundreds of distinct DNA variants in five disease genes are associated with familial PD. The mutated genes include SNCA, Parkin (PARK2), PTEN-induced putative kinase 1 (PINK1, PARK6), DJ-1 (PARK7), VPS35 (PARK17) and Leucine-rich repeat kinase 2 (LRRK2, PARK8) [8, 44]. The SNCA mutations found in PD patients are A30P, E46K, H50Q, G51D, A53T, A53E within the N-terminal domain. The familial mutations A30P and A53T are associated with a higher ability to form fibrils in the presence of heparin [5]. Overexpression by gene duplication or triplication increases SNCA and symptoms of PD [21]. High amounts of SNCA in the cell therefore enhance its aggregation. The multiple interactions of SNCA with membranes seem to be critical for its function and its pathogenicity [45]. Transgenic mice that express human SNCA or A53T mutant SNCA exhibit the formation of toxic filamentous SNCA in neuronal inclusions with neurodegeneration [46]. The pathophysiology of PD can be studied in mice injected with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, which is toxic to dopaminergic neurons in the SN [47].
Potential risk factors for PD include exposure to environmental toxins, pesticides, metals and drugs. Signaling pathways and receptors, transporters and enzymes involved in DA metabolism are critically involved. Impaired protein clearance via the ubiquitin–proteasome and autophagy-lysosomal systems associated with oxidative stress and dysfunction of mitochondria contribute to accumulation of misfolded proteins and pathogenesis [48].
PD patients also experience non-motor symptoms. The gastrointestinal tract and the enteric nervous system (ENS) are clearly associated with PD and ENS also contains dopaminergic neurons and SNCA. The gut microbiota composition is altered in PD and could be in part due to decreased gut motility [49]. Mucus and electrolyte secretion is regulated by the ENS via acetylcholine and vasoactive intestinal peptide transmitters. Lewy bodies have also been found in the colon. In a mouse model of PD, it was suggested that α-synucleinopathy spread from the ENS to the CNS. Gut colonization in germ-free mice was required to induce SNCA aggregation, neuroinflammation and PD symptoms such as motor deficits [50]. It is possible that short chain fatty acids are involved. However, the detailed pathogenesis of synucleinopathy in the gut needs to be explored [50, 51]. Bacteria adhere to mucins and cleave mucin glycans that serve as a source of energy. The glycosylation of mucins therefore determines the spectrum of adhering bacteria. Neurological dysfunctions in PD lead to decreased gut motility but in addition, the intestinal microbiome plays a role in establishing the mucin expression, glycosylation and barrier function, as well as the ENS function via their outer polysaccharides [51]. There are significant changes in the population of bacteria in the intestine of PD patients [52] but the molecular details of how the altered microbiome affects pathogenicity of PD remain to be established.
One prominent feature of PD is the presence of intracellular neuronal inclusions that are rich in membrane components, neurofilaments, ubiquitin and various forms of oligomeric and insoluble SNCA aggregates and may contain other aggregated proteins. These inclusions develop to Lewy bodies with different morphologies that can be visualized by electron microscopy inside the neuronal cell body and in neurites [1]. Toxic SNCA species disrupt and disorganize membranes [53].
In the intermediate stage of Lewy body formation, the SNpc and other areas of the midbrain are affected and show pathology. Dying dopaminergic neurons release their contents, and Lewy bodies spread further throughout the nervous system [54]. SNCA may pass between cells and has the potential to propagate misfolded and aggregated SNCA in neighbouring cells. Neuroinflammation with activated microglial cells and astrocytes, increased proinflammatory cytokines and altered immune cells are also implicated in the pathogenesis [55, 56]. SNCA is found in secretory vesicles that are externalized via exocytosis, and taken up by other cells via diffusion through the membrane or endocytosis. Thus, Lewy body pathology with SNCA aggregation and spreading of its toxic forms may include a prion-like mechanism [57]. Heparan sulfate appears to be involved in the vesicle trafficking and cell to cell transmission of pathology [58, 59]. The heparan sulfate agrin colocalizes with SNCA in the SNpc and accelerates SNCA fibrillization [60]. The insoluble aggregates of SNCA and Lewy bodies are not specific for PD but are also present in a number of neurological conditions including dementia with Lewy bodies.
The search for the vulnerability of PD patients has suggested that extensive arborization of axons, mitochondrial dysfunction, defects in protein degradation, altered metabolism of DA and increased abundance and mutations of SNCA contribute to the degeneration of dopaminergic neurons in SNpc and to PD pathology [61, 62].
Several cell surface glycoproteins are involved in the interaction with SNCA or its toxic forms and in further transmission of pathology [63]. Toll-like receptors TLR2 and TLR4 are N-glycosylated plasma membrane receptors that are activated by microbial fragments and induce inflammation but also bind SNCA. TLR2 is expressed in microglial cells and appears to be more specific for binding to aggregated SNCA. The N-glycans of TLR2 contribute to its efficient cell surface expression [64]. TLR4 is highly expressed in SN and was shown to contribute to the formation of reactive oxygen species (ROS) and neuronal cell death [65]. Activation of TLR4 is controlled by α2,3-linked sialic acid linkages [66].
The progressive loss of dopaminergic neurons leads to decreased capacity to synthesize DA and loss of the black pigment neuromelanin (MN) in the SN. Other areas of the brain are also affected by the lack of DA, and this contributes to multisystem degeneration. Neuronal cell death is counteracted by survival signals induced by neurotrophic factors. These growth factors bind to their membrane-bound glycoprotein receptors, stimulating survival cascades, neurite outgrowth or synapse formation [67]. Upregulation of the growth factors and their receptors could partially restore dopaminergic cell survival and differentiation and improve DA function.
Biosynthesis and transport of dopamine
The neurotransmitter DA is the major catecholamine in the brain and controls motor activity, mood, autonomic and many other functions. DA is synthesized in the cytosol of dopaminergic neurons in the brain, in the central nervous system (CNS) as well as in the adrenal gland and other organs. The highest concentration of dopaminergic innervations is in the striatum. The precursor substrates for DA synthesis are Phe and Tyr. The major pathway is through the rate-limiting step, hydroxylation of Tyr by cytoplasmic tyrosine 3-monooxygenase (tyrosine hydroxylase, TH) to form L-DOPA (Fig. 1). TH is a major marker for dopaminergic neurons. SNCA can bind to TH and inhibits its activity by preventing its phosphorylation at Ser40 [68,69,70]. L-DOPA is decarboxylated by L-amino acid decarboxylase (AADC) to form DA. In a minor pathway, Tyr is decarboxylated to form tyramine by AADC, followed by CYP2D oxidation to form DA. Oxidation reactions of DA and its metabolites can result in highly reactive compounds and precursors of NM polymers. While the charged DA and its metabolites cannot cross the BBB, L-DOPA can reach the brain if taken orally. It is converted to DA by AADC inside functional dopaminergic neurons and thus partially replaces the DA loss due to decreased numbers of dopaminergic cells in PD.
Dopamine metabolism The nerve transmitter dopamine (DA) is synthesized in dopaminergic neurons. Tyr is converted to levodopa (L-DOPA) by tyrosine hydroxylase (TH). Tyrosinase can also introduce the hydroxyl group into the phenyl ring to synthesize L-DOPA. L-Amino acid decarboxylase (AADC) synthesizes the catecholamine dopamine. A minor reaction is the conversion of tyramine to dopamine by cytochrome oxidase CYP2D. Dopamine metabolites include norepinephrine, synthesized by dopamine beta-hydroxylase (DBH), and 3-methoxytyramine synthesized by catecholamine O-methyltransferase (COMT). A number of oxidation products have various biological effects and are intermediates in the polymerization to form the dark pigment neuromelanin. Tyrosinase is involved in these oxidation reactions and synthesizes the quinones from L-DOPA and dopamine. Dopamine quinone can be cyclized to dopaminochrome and further converted to 5,6-dihydroxyindole, a common precursor for neuromelanin polymer synthesis. Dopamine binds to membrane receptors VMAT2 and DA receptors, to dopamine transporter (DAT), neuromelanin (NM) and alpha-synuclein (SNCA)
The conversion of DA to sulfated and glucuronylated forms enhances its secretion [71]. DA can also be metabolized by monoamine oxidase (MAO) localized to mitochondrial outer membranes and by catechol O-methyl-transferase (COMT) that is found as a soluble enzyme in the cytoplasm and in the membrane-bound form and forms 3-methoxytyramine. Dopamine β-hydroxylase (DBH) is a secreted glycoprotein that converts DA to norepinephrine (Fig. 1). Inhibition of these enzymes has the potential to increase DA levels and this is exploited in PD treatment. The potential of DA to be metabolized can be dangerous for the cell and can lead to high ROS levels and oxidative stress, making the dopaminergic cells susceptible to degeneration [72]. It is therefore advantageous for DA to be sequestered into vesicles. Synaptic vesicular amine transporter VMAT2 that localizes to synaptic vesicular membranes translocates soluble DA into synaptic vesicles and transports DA to the exterior by exocytosis. VMAT2 has 12 transmembrane domains and 2 N-glycosylation sites near the N-terminus and interacts with SNCA. The function of VMAT2 is crucial in maintaining a low concentration of DA in the cytosol, preventing accumulation of toxic metabolites of DA [73]. SNCA maintains vesicle trafficking, tethers synaptic vesicles to the inner leaflet of the cell membrane and affects proteins that regulate DA availability [74]. The complex role of SNCA in DA trafficking was shown by knockdown of SNCA expression in cultured dopaminergic neuronal cells that reduced the cell surface expression of DA reuptake receptor (DAT) but increased the density of VMAT2 transporters per vesicle [69, 75]. A rare mutation of VMAT2 was found in an infant with PD symptoms showing the essential function of VMAT2 in DA homeostasis. The condition was partially corrected with DA agonists but not with L-DOPA [76].
In the exterior of the cell, DA can bind to DAT for re-uptake into the presynaptic terminus. Alternatively, DA binds to DA receptors D1, D2 or D3 on the plasma membrane of the postsynaptic termini. DAT and DA receptors are N-glycosylated glycoproteins. DAT is a Cys-palmitoylated, Thr-phosphorylated plasma membrane protein with 12 transmembrane domains and 3 N-glycosylation sites in the extracellular domain, having both N- and C termini in the cytoplasm. The N-glycosylation of DAT plays a role in the vulnerability of dopaminergic cells in PD. DAT transporter expression and function are regulated by N-glycosylation [77]. DAT is highly expressed in the SN, and translocating excess DA regulates the levels and effects of DA. DAT function is modulated by SNCA and most DAT-SNCA protein complexes are found at the plasma membrane of dopaminergic neurons where SNCA can increase DA efflux [69, 70]. The soluble N-ethylmaleimide-sensitive factor attachment protein receptor (SNARE) complex functions in the release of neurotransmitters, and SNCA has a chaperone-like activity in the maintenance of the complex [78]. These studies indicate that SNCA functions by multiple mechanism to affect DA levels.
Of the five human DA receptors activated by DA, only D1, D2 and D3 have a significant function in the synapses [79,80,81,82]. D2 and D3 receptors are widely distributed in the striatum [83]. These G-coupled receptors activate adenylyl cyclase and are localized at the plasma membrane having 7 transmembrane domains, several N-glycosylation sites, and Cys-palmitoyl modification. While DA binding to D1 and D2 receptors is not changed in PD, there is a significant decrease in D1 and D2 function in Huntington’s disease [82]. An additional minor DA receptor is TAAR1 that is a high affinity plasma membrane receptor for DA with 7 transmembrane domains and 2 N-glycosylation sites.
Both D2 and D3 receptors were shown to carry complex type N-glycans. Studies of D2 receptor expression in CHO cells showed that N-glycans must be fully processed for efficient cell surface expression [84]. Similarly, D2 and D3 expression in HEK293 cells showed that N-glycans are required for the cell surface expression of DA receptors [85]. Tunicamycin treatment of HEK293 cells decreased the cell surface localization of D2 and D3 receptors but decreased the internalization of D3. Mutations of multiple but not individual N-glycosylation sites led to decreased cell surface expression of D3. In contrast, tunicamycin treatment of HEK293 cells increased D2 receptor internalization which reduces its function on the cell surface. This shows that the role of N-glycans varies with the specific receptor protein.
Structures of alpha-synuclein
SNCA is a small amphipathic protein that is mainly found in the nerve terminals of presynaptic neurons in the SNpc of the midbrain. Many functions have been proposed for SNCA, including vesicle trafficking, synaptic activity, regulation of DA activity, metal and lipid binding and interaction with several proteins and membrane lipids [48, 70, 86]. In PD, it is mostly SNCA proteins that form toxic forms such as oligomers, protofibrils and fibrils that cause degeneration and dysfunction of dopaminergic cells and initiation of inflammation in the SNpc. Specific oligomeric forms are thought to be the most cytotoxic species.
SNCA can be purified to a stable monomer of about 18 kDa by various methods including heat treatment and anion exchange chromatography. The N-terminal domain of SNCA is mainly responsible for its α-helix formation upon membrane binding and contains 7 series of KTKEGV repeat sequences that are also found in the α-helical domains of apolipoproteins. The charged Lys residues can interact with phospholipids and mediate membrane association. Polyunsaturated fatty acids (PUFAs) bind to the N-terminus [87]. The central, non-amyloid component (NAC) domain [83] has many hydrophobic residues, flanked by Lys residues and binds phospholipids. The NAC domain is required for aggregation and fibril formation through β-structure formation. Mutagenesis of SNCA showed that a short stretch of 12 amino acids (V71TGVTAVAQKTV82) in the NAC domain is necessary for fibrillization. This peptide alone can also form β-structure and straight filaments [88]. Many Glu and Asp residues render the C-terminal domain highly negatively charged, giving a net negative charge to the molecule. The C-terminal domain is flexible and forms random coils due to its low hydrophobicity and plays a role in regulating SNCA aggregation. Neutralizing the negative charge of the C-terminal domain by mutations increases its aggregation potential [89]. The mutations of SNCA in PD have diverse effects on the structure and function of SNCA [90, 91]. For example, the A53T mutant is more likely to cause fibrillation while the A30P mutation prefers oligomerization.
Interconversion of SNCA structures
After association with the cellular membrane, the unfolded SNCA monomer changes to an extended α-helical conformation [29, 45]. Tetramers of SNCA have been found [92] that are resistant to conversion to toxic forms [93]. The KTKEGV repeat sequences are critical for SNCA tetramerization. Mutations in these repeat sequences caused excess monomers and neurotoxicity [7].
The initiating factors of SNCA aggregation are not well defined. Randomly structured SNCA monomers can form anti-parallel β-sheets and progress to oligomers. The oligomers are thought to be the main toxic species of SNCA that cause neurodegeneration. Toxic oligomers can be removed from neurons via exocytosis. Subsequent aggregation and formation of insoluble fibrils develop slowly. At later stages, loosely associated disordered aggregates are present, and finally protofibrils and amyloid-like mature about 10 nm wide fibrils appear [19].
The aggregated forms of SNCA accumulate in Lewy bodies. In PD models such as cultured dopaminergic SH-SY5Y cells aggregating SNCA can be measured by Thioflavin-T fluorescence, electron microscopy or circular dichroism. Protofibrillar or fibrillar SNCA caused a much more rapid destruction of the membrane than soluble monomeric SNCA [94, 95].
Posttranslational modifications of SNCA
SNCA can undergo a number of posttranslational modifications (PTM) that affect its function and aggregation (Table 1) [20]. Phosphorylation, nitration, and ubiquitination are associated with toxic or aggregated SNCA [91]. A major proportion of SNCA in both Lewy bodies and glial cell cytoplasmic inclusions is phosphorylated at Ser129 [69, 96]. Phosphorylation of Tyr125 and Ser129 promotes aggregation while inhibiting degradation and intracellular trafficking of SNCA. Phosphorylation of Ser87 increases the conformational flexibility of SNCA and blocks its aggregation [97]. Thus, phosphorylation has site-specific functions.
The N-terminal Met residue can be acetylated and this may decrease the rate of fibril formation [98, 99]. The N-acetyl group contributes to the formation of the α conformation of SNCA which is resistant to aggregation and binds to GM1 [100]. N-terminal acetylation was shown to be crucial for the cellular localization of SNCA.
Diabetes appears to pose an increased risk for future PD development [101], and the diagnosis of diabetes prior to PD may be associated with more severe PD disease. Anti-diabetic drugs appear to reduce the incidence of PD and are neuroprotective in animal models of PD. However, the relationship of diabetes, high blood sugar and PD needs to be re-examined in further studies. The 15 Lys residues of SNCA are potential targets for non-enzymatic glycation and the formation of AGE in the presence of prolonged high Glc concentration in the blood. The N-terminal Lys residues are likely to be candidates for glycation [102, 103] which has been shown to induce the nucleation of protein aggregates and oxidative stress, potentially leading to neurodegeneration. AGE levels are increased in PD brains and around Lewy bodies and activate RAGE which stimulates inflammation and the generation of reactive oxygen species and can initiate apoptosis [72, 104].
Lys residues of misfolded SNCA can also be ubiquitinylated which serves to degrade SNCA. Ubiquitin can be attached to Lys residues and target the protein to the proteasome for degradation. However, ubiquitinylated SNCA is resistant to proteases and accumulates in vesicles and Lewy bodies. In addition, Lys residues can be acetylated, and the clearance of acetylated SNCA is increased compared to non-acetylated SNCA. Sirtuin 2 is a deacetylase that can induce aggregation of SNCA and neurodegeneration. This suggests that Lys-acetylation has a protective function in cortical neurons [105].
Nitration of Tyr residues of SNCA can occur in the presence of increased ROS. This nitration is a marker of oxidative stress and promotes oligomerization and Lewy body formation. Nitration of Tyr 39 at the N-terminus interferes with membrane interactions of SNCA [106]. Mutation of Tyr133 to Ala led to SNCA that was mainly in the \(\alpha\)-helical conformation and did not form fibrils [6].
Many cytosolic and nuclear proteins in the brain, and especially in nerve terminals, carry O-GlcNAc [107]. Neurons are an abundant source of the GlcNAc-transferase (OGT) that adds O-GlcNAc to Ser/Thr, as well as the enzyme that hydrolyzes O-GlcNAc (OGA) [108]. O-GlcNAc was found on Thr72 and Ser87 residues of SNCA but can also be attached to additional Ser/Thr residues [109, 110]. Especially the GlcNAc-O-Thr72 form of SNCA showed decreased conversion to toxic species [86, 109,110,111]. GlcNAc-O-Thr72 also affects phosphorylation, and this has potential to diminish aggregation in synucleinopathies [86, 112].
Role of neuronal membranes
The lipids in neuronal membranes are diverse and include phosphatidylcholine (PC), phosphatidylethanolamine (PE), phosphatidylserine (PS), cholesterol, fatty acids, triacylglycerol and glycosphingolipids (GSL). Neurons are particularly rich in di- and tri-sialylated GSL, gangliosides and sulfatide. Neurites contain mainly trisialylated gangliosides GT1b and disialylated GD1b. Docosahexaenoic acid (DHA) and arachidonic acid (AA) are abundant essential fatty acids in brain membranes. In the SN of PD patients, multiple changes of ganglioside levels were found. For example, there is less GD1a and GT1b [113]. The SN of PD patients was also found to have decreased levels of GM1 and increased levels of biosynthetic precursor GSLs such as GM3 and glucosylceramide [114, 115].
The fluidity and lateral mobility of membranes depend largely on the length and degree of unsaturation of acyl chains. Phospholipids, cholesterol and gangliosides contribute to the curvature of the membrane and the fusion of vesicles. There is a dynamic interaction between lipids, proteins and rafts that are specialized areas of the membrane. Specific lipids can disorder the bilayer structure. For example, PUFAs and Dol can disrupt the regular bilayer [31, 116].
Lipid rafts in neuronal membranes are PC-rich and contain protein complexes of diverse biological functions including cell signaling that is supported by the lipid composition. Lipid rafts have a relatively high content of GM1 and GM2 and other GSL. The lipid composition changes upon aging and neurodegeneration [117]. Cholesterol, PUFAs, Dol and gangliosides are particularly prone to changes during aging and this affects the properties of the membranes and lipid rafts [12, 13, 117]. Lipid oxidation also appears to increase with age and this may be a critical factor in neurodegeneration [118].
The neuronal cell membrane has several enzymes that can form complexes with cell membrane receptors and have the potential to restructure cell surface glycoproteins and glycolipids, including sialyltransferase and neuraminidase [119]. Neuronal membranes are essential for neurotransmitter release and responses, and for receptors of neurotrophins that regulate cell survival and cell death, proliferation, differentiation and neurite outgrowth. Polysialic acids (PSA) are primarily linked to neural cell adhesion molecules (NCAM) [120, 121] and are critical for development as well as maintenance and plasticity of the nervous system. These Sialylα2-8 linked polymers are synthesized by polysialyltransferases and control cell–cell interactions during the development of the nervous system via their anti-adhesive properties. PSA are common on neural stem cells (NSC). During differentiation to dopaminergic neurons the synthesis of PSA increases sharply. However, studies in mice showed that mature dopaminergic neurons no longer require PSA for their functions [122].
Growth factors that affect neuronal proliferation include neurotrophic factors NGF3, NGF4, glial cell derived neurotrophic factor (GDNF), cerebral DA neurotrophic factor (CDNF) and mesencephalic astrocyte-derived neurotrophic factor (MANF). The cell surface-bound receptors involved in neuronal cell survival include NGFR p75 and Tyrosine kinases TrkA, TrkB and TrkC that are heavily N-glycosylated. The p75 receptor is related to TNFα receptors and can also induce apoptosis. O-glycans of p75 direct receptor localization [123]. The N-glycans of TrkA are required for localization of the receptors at the cell surface in a complex with GM1 and neuraminidase Neu3 [124]. Changes in the membrane composition and GM1 content can alter the response to neurotrophic factors such as GDNF [125] and affect neuronal cell survival.
Neurexin and neuroligin are N-glycosylated glycoproteins that cooperate in cell–cell interactions and work together to localize synaptic vesicles and maintain the synapse structure [126, 127]. In SH-SY5Y neuronal cells, complex N-glycans were shown to be essential for neurexin and neuroligin function in binding to N-terminally acetylated SNCA [127] which inhibits aggregation [100]. Neuroligin-1 also has O-glycans in its stem region near the transmembrane domain. The N-acetylated form of SNCA as well as SNCA fibrils bind to neurexin-1α.
Alpha-synuclein interacts with membranes and lipids and changes conformation
The neuronal cell membrane plays a critical role in protein aggregation and controls SNCA conformational transition [128, 129] (Fig. 2). Soluble SNCA exists as a random coil structure that increases its α-helical conformation after interacting with membrane phospholipids. The N-terminal of SNCA is critical for interaction with membranes [38, 130]. N-acetylated SNCA localizes to highly curved, ordered membranes inside a cell. Upon knockdown of the N-acetyltransferase NatB [131] SNCA was observed to redistribute from the plasma membrane to the cytosol.
Proposed pathogenesis of Parkinson’s disease: role of membrane lipids. Alpha-synuclein (SNCA) is central to the pathogenesis of Parkinson’s disease. SNCA interacts with many lipids, proteins, and curved cell membranes and vesicular membranes in the presynaptic termini of dopaminergic neurons. SNCA is normally unfolded but can form tetramers with α-helix structures (α-tetramer) that support neuroprotection. Ganglioside GM1 binds to SNCA, supports formation of SNCA α-tetramers and interacts with growth factor receptors that promote neuronal survival. Under still unknown stimuli involving specific membrane lipids SNCA can misfold to form toxic oligomers with β-sheet structures that develop to toxic fibrils and accumulate in Lewy bodies. Polyunsaturated fatty acids (PUFAs), docosahexaenoic acid (DHA), and phosphatidic acid (PA) have been shown to be involved in the pathways to neurodegeneration. Dolichol (Dol) and neuromelanin (NM) interact with SNCA but the consequence of this interaction is still unclear. Dol disrupts membrane structures and may support SNCA misfolding. Dopamine binds to SNCA, and dopamine metabolites participate in the synthesis of NM. Knowledge of the complex interactions between SNCA and membrane components is critical for understanding the pathogenesis of Parkinson’s disease
The binding of SNCA to membrane lipids facilitates the transport between soluble and membranous compartments of cells and increases pore formation and membrane lysis. SNCA and especially its N-acetylated form prefers to interact with curved membranes which are common in synaptic vesicles [98, 99, 132]. In rat neuroblastoma cells especially the A53T mutant localized near the neuronal membrane compared to A30P mutant and wild type SNCA. Conformational studies confirmed that the A53T mutant as well as the E57K mutant could interact with membranes [90].
Multiple studies have shown that an increase in acidic asymmetric lipids such as phosphatidic acid (PA) and DHA increases SNCA accumulation and aggregation. SNCA binds preferably to phospholipids that are negatively charged such as PA, PS and phosphatidyl inositol (PI) [98, 99, 133, 134]. PUFAs such as α-linolenic, DHA and eicosapentaenoic acid interact with SNCA [20, 135] and can induce aggregation [118, 134, 136,137,138]. The phospholipid 1,2-dimyristoyl-sn-glycero-3-phospho-L-serine co-assembles with SNCA to form thinner and curlier fibrils (proto-fibrils) and thus perturbs the kinetics of SNCA aggregation [24]. The binding to lipids converts most of the SNCA molecules to an α-helical conformation [139] that is not likely to form fibrils [95]. However, specific lipids such as dioleoyl-PA selectively bind to SNCA and strongly induce its aggregation [134]. The composition and ratio of various lipids as well as the ratio of protein to lipids are critical in their effects on SNCA conformation and oligomerization [98]. De Franceschi [137] found that a ratio of 1:10 protein/DHA induces fibril formation while at a ratio of 1:50 protein/DHA oligomerization occurred. The His50 residue of SNCA appears to be responsible for binding to DHA.
In vitro, SNCA preferably binds to small unilamellar vesicles (SUV) that contain ganglioside GM1 [140]. GM1 has been shown to bind to SNCA, supporting the α-helix formation and reducing its propensity to aggregate and form fibrils [27]. Especially the acetylated form of SNCA associates with GM1. In contrast, GM2 or GM3, asialo-GM1 or other GSL showed much less binding or effect on fibril formation. The glycan structure of GSL is therefore critical for SNCA binding. It is likely that the sialic acid moiety interacts with Lys residues in the α-helical conformation of SNCA. Sulfatide does not bind to SNCA which means that it is not simply the charge that is responsible for binding.
GM1 is synthesized from lactosylceramide by the action of sialyltransferase ST3GALV, Gal-transferase B3GALT4 and GalNAc-transferase B4GALNT1. In analyses of postmortem PD brain samples, the enzymes B3GALT4 and ST3GAL2 were found to be reduced in the NM-containing cells of the SN which also showed low levels of gangliosides that carry the GalNAcβ1-4 residue [141]. However, B4GALNT1 expression was not determined. The synthesis of GM1 was deficient in B4GALNT1 knockout mice which also had PD symptoms and aggregated SNCA in the nigral area of the brain [27, 37, 142]. It remains to be determined if the levels of these glycosyltransferases are abnormal in PD and predispose these cells to develop toxic SNCA forms. This may be a cell-specific and age-related defect and the enzyme expression and activity in the degenerated dopaminergic cells may be decreased due to the pathology in these cells. This remains to be determined. The balance of biosynthetic enzyme activities determines the relative amounts of gangliosides. For example, ST8SIA I knockout mice lack gangliosides having multiple sialic acid residues but have increased GM1 and GD1a. These mice were less susceptible to symptoms of PD. Thus, PD therapy may include GM1 or its less hydrophobic, membrane-permeable analog (LIGA-20) [142]. Galβ1–3GalNAcβ1–4(Neu5Acα2-3)Galβ1–4Glc is the oligosaccharide moiety of GM1 and in itself has shown neuritogenic and protective effects in murine neuroblastoma cells, similar to the effect of GM1 [143]. GM1 as well as the GM1 oligosaccharide bound to neurotrophin receptor TrkA and increased its phosphorylation and activation.
The membrane composition of vesicles and membranes regulates the conformational changes of SNCA that could lead to aggregation [144]. The membrane surfaces and their curvature are of critical importance in the normal function of SNCA and in the change to toxic forms but the age-related changes in PD membranes need to be determined. Specific lipids and aggregated proteins can cause pore formation and overall architecture of the membrane [20]. For example, Dol is a large lipid that distorts the bilayer membrane [116]. The concentrations of these lipids relative to protein determine the effect on SNCA aggregation (Fig. 2).
Dolichol
The bilayer structure and permeability of the membrane depend on the temperature, the lipid composition and degree of saturation [145, 146]. The large membrane-bound polyisoprenol Dol (Fig. 3) is found in eukaryotic organisms and archaea and serves several essential functions. Dol, Dol-P and its glycosylated versions are distributed within cellular membranes with a high concentration in the ER. The glycosylated Dol-phosphate (Dol-P)-based metabolites are donor substrates and intermediates for glycosylation reactions in the ER [147]. The biosynthesis of N-glycans, glycosylphosphatidylinositol anchors, O-Man-Ser/Thr and C-Man-Trp linkages all depend on Dol-P as the intermediate. Dol is a mixture of molecules having different numbers of isoprene units and different cis–trans configurations. The number of isoprene units in human Dol varies between 13 to 23. Relevant to PD are the observations that Dol has a significant effect on the structure and permeability of membranes, its accumulation in the aging brain and its association with NM in the SNpc. Analyses of human brain samples from 2 to 90 year-old patients showed that the amount of Dol in the human brain increases up to 21-fold upon aging [3, 14, 148, 149]. The reason for this may be the lack of catabolic pathways for Dol. In mouse liver tissues, Dol-P is a minor component of total Dol and it is mainly the free Dol that increases upon age [150]. An excess of Dol in neuronal membranes could contribute to the imbalance of SNCA oligomeric species. This is supported by our preliminary studies that showed an acceleration of SNCA aggregation by Dol and polyisoprenols.
Synthesis of dolichol. Dolichol (Dol) is a large polyisoprenyl lipid that has significant influence on membrane structure and permeability and binds to neuromelanin and many proteins. Dol concentration in the brain increases with aging. Acetyl-CoA is the precursor for the biosynthesis of Dol and cholesterol. HMG-CoA reductase is the rate-limiting enzyme in the pathways and is inhibited by statins. At the stage of farnesyl-diphosphate (Farnesyl-PP) the pathways branch. In the Dol synthesis pathway, farnesyl-diphosphate is elongated by cis-prenyltransferase, and the diphosphate is removed by polyprenyl diphosphate phosphatase. The α-isoprene unit is reduced by polyprenol reductase to form human Dol that has about 13 to 23 isoprene units. The last two ω isoprene units are throught to be in the trans-configuration while other units are in the cis-configuration. Neuromelanin contains Dol and a small amount of dolichoic acid which carries a carboxyl group replacing the hydroxyl of Dol. A relatively minor proportion of total Dol is converted by Dolichol kinase to Dolichol-phosphate (Dol-P) which serves as an essential intermediate to synthesize donor substrates for glycosylation reactions. This includes Dol-P-Man synthase that synthesizes Dol-P-βMan, Dol-P-Glc-transferase that synthesizes Dol-P-βGlc. GlcNAc-1-P-transferase synthesizes Dol-PP-αGlcNAc upon which the glycan chains of N-glycosylated glycoproteins are built. There are no pathways known that catabolize Dol in mammalian cells, and Dol species accumulate in the brain
In rat liver, most of the cellular Dol-P is present in the microsomal membrane fraction while unmodified Dol is present in lysosomal and mitochondrial membranes [147]. In human brain, between 4 and 9.5% of total lipids are Dol, depending on the region [151]. Human Dol is an alcohol having a saturated α-isoprenoid group which is essential for its function in glycosylation. In contrast, bacteria use undecaprenyl glycosylation intermediates that have an unsaturated α-isoprene group.
Dol may act as a free-radical scavenger in cell membranes. Therefore, it could protect PUFAs from peroxidation [152]. Dol plays a critical structural role in membranes. Because of its large hydrophobic property, Dol significantly disrupts the membrane structures and fluidity [16]. This large lipid has the potential to distort microdomains and influence the interactions between membranes and SNCA. NMR spectroscopy of phospholipid mixtures in the presence and absence of Dol demonstrated that Dol does have a significant effect on bilayer structure. The destabilizing effect on membranes is increased at higher Dol concentrations [153]. Dol promotes the leakage of membranes in liposomes composed of PE and PC but much less in liposomes composed only of PC. Using electron spin resonance experiments and a cationic spin probe, the percentage of membrane leakage induced by Dol was proportional to the concentration of Dol [15]. Measured by calcein fluorescence release, vesicles from PC alone, or with PC and Dol were far less permeable than vesicles containing PE. Thus, Dol significantly enhances the permeability of phospholipid bilayers containing PE [116, 146].
Dolichol biosynthesis
The biosynthetic pathway to Dol is well known (Fig. 3) [147, 154]. Dol and cholesterol are synthesized in the mevalonate pathway from acetyl-CoA. Dol synthesis follows the same pathway as cholesterol synthesis to the conversion of mevalonate to isopentenyl-diphosphate and farnesyl-pyrophosphate (FPP), with HMG-CoA reductase catalyzing the rate limiting step. Statins that inhibit HMG-CoA reductase thus can block both cholesterol and Dol synthesis (Fig. 3) and may have neuroprotective properties [135]. Treatment of SNCA-expressing neuroblastoma cells with statins decreased the amount of SNCA insoluble aggregates [155].
Treatment of SH-SY5Y cells with the HMG CoA reductase inhibitor simvastatin showed a reduction of both cholesterol and Dol levels [156]. The synthesis of the polyprenol Dol occurs in the cytosol through the FPP over several steps. Cis-prenyltransferase extends the isoprenyl chain and is present in a long-chain heteromeric cis-prenyltransferase complex [157, 158]. Polyprenyl diphosphate phosphatase then removes the diphosphate group. The final step is catalyzed by polyprenol reductase that reduces the β and ɣ carbon linkage of the polyprenol chain to form Dol. This enzyme is not present in bacteria that utilize the undecaprenyl intermediate without reduction of the terminal isoprene unit. In humans, a deficiency of polyprenol reductase is associated with cerebellar ataxia and congenital eye malformations, named SRD5A3-congenital disorder of glycosylation [159].
The main metabolite of Dol is synthesized by Dol kinase to produce Dol-P that is used in protein glycosylation pathways. This is an essential enzyme and a deficiency in Dol kinase (DOLK-CDG) is the cause of a severe hypoglycosylation phenotype in humans with death within the first year of life [160]. Several other Dol-related defects are known with patients experiencing severe symptoms, indicating the importance of a proper balance of Dol metabolites [154].
There are no known pathways for Dol degradation in humans. However, Dol can be oxidized to the acid form, dolichoic acid, that has been found in the SNpc in the brain [161]. The Dol oxidase that synthesizes dolichoate in the presence of NAD+ has been identified in a bovine thyroid mitochondrial fraction. The NM pigment from human brain SN contained a high proportion of dolichoic acids having 14 to 20 isoprene units [17]. It remains to be determined if an imbalance of Dol species in the brain of PD patients affects membrane functions.
Neuromelanin interactions
The dark pigment melanin occurs in several forms in skin, hair and brain. The black appearance of SN is from neuromelanin, a dark pigment in large, double membrane-encased granules in dopaminergic cells [162,163,164,165]. Brain NM is related to skin melanin and is present in lysosomal-like organelles that digest proteins and lipids. NM pigment is mostly insoluble and accumulates with aging, but the physiological function of NM is still not clear. NM can chelate metals, bind toxic chemicals and may protect neurons from oxidative stress [165]. It is possible that the high vulnerability of dopaminergic neurons in PD is due to the age-related production of insoluble NM.
NM reversibly binds to DA and is thought to be involved in DA storage and release through close association with VMAT2. The mixture of NM polymers contains aggregated proteins and Dol that form the insoluble core [18]. Brain NM appears to be specific for primates and is especially high in humans.
Dol as well as cholesterol bind to NM polymers in the SNpc, and Dol is the main lipid component of the pigment [18, 151, 163]. NM contains 14% of its weight in total Dol that includes 3.1% dolichoic acid [17, 18, 151, 163]. In addition, SNCA is entrapped within the pigment, and Lewy bodies are also closely associated with NM in the cytoplasm.
A wealth of Tyr, tyramine, L-DOPA and DA metabolites are formed through oxidation reactions in the cytoplasm that are precursors for NM formation. Tyrosinase is a membrane-bound, heavily N-glycosylated oxidase involved in melanin formation in skin melanosomes and in the human brain. Tyrosinase catalyzes oxidation reactions of catecholamines, including hydroxylation of Tyr to L-DOPA, conversion of L-DOPA or DA to quinones and other precursors for NM formation [165,166,167]. The DOPA quinone and DA quinone can be converted to DOPAchrome, dopaminochrome and 5,6-dihydroxyindoles with various modifications that include incorporation of Cys (Fig. 1). These reactive compounds have cytotoxic, inhibitory and antimicrobial properties. In addition, quinones can react with SNCA and stabilize toxic fibrillization intermediates [166,167,168,169]. The human tyrosinase gene in an adenovirus vector was injected into rat brain SN that lacked NM. The tyrosinase expression caused accumulation of NM in dopaminergic, TH positive neurons and an age-dependent PD phenotype with Lewy body formation and degeneration of dopaminergic neurons [166]. These studies implicate interactions between DA, SNCA, Dol and NM in the pathogenesis of PD. Membranes are intricately involved but the role of membranes in the interactions of NM and its binding partners remains to be shown.
Treatment options for PD
A wealth of compounds is available to relieve Parkinson’s symptoms. However, research should confirm their mechanism of action, transport across BBB, and clinical trials are required to confirm their effectiveness and safety. Other treatment options are being investigated and address neuroprotection or replacement of dead cells.
If specific membrane lipids are partially responsible for SNCA aggregation, then these could be removed, for example by introducing catabolic enzymes or by using specific biosynthetic inhibitors. Alternatively, the concentrations of lipids that inhibit aggregation may be increased by delivering analog compounds that cross the BBB or by overexpressing their biosynthetic enzymes.
Several small molecules were found to inhibit aggregation and even destabilize existing fibrils, for example polyphenols, nicotine and curcumin. Vitamin K counteracts the SNCA fibril nucleation [170] leading to shorter fibrils. Phenolic compounds such as ferulic, caffeic and rosmarinic acid have some structural similarity to L-DOPA; they counteract aggregated SNCA and destabilize fibrils by associating with the β-sheet conformation of proteins [171]. Benzoic acid derivatives such as protocatechuic acid and gallic acid can also block the SNCA aggregation process. These compounds can cross the BBB and may be neuroprotective. The antibiotic Rifampicin can be used [172] to decompose existing fibrils. DA as well as dopaminochrome also inhibit fibril formation [173]. The effect of dopaminochrome (Fig. 1) is based on its interaction with a YEMPS sequence at the C-terminus of SNCA that changes its conformation. Some flavonoid polyphenols have antioxidant properties and can reduce the toxicity of SNCA aggregates.
A high concentration of SNCA supports fibril formation [22]. SNCA expression and thus aggregation could be reduced by viral-based knockdown or by inhibitory RNA. Gene knockdown of SNCA in animal models has proven to be partially successful in preventing PD symptoms [174].
Since DA cannot cross the BBB due to its charge at physiological pH, its biosynthetic precursor L-DOPA which has less charge is given (Fig. 1). Inhibitors of DA degradation enhance its effectiveness, such as AADC inhibitor Carbidopa and COMT inhibitor Entacapone. These compounds do not cross the BBB but increase the availability of L-DOPA in the brain. Other potential compounds that support DA concentrations are MAO and DBH inhibitors, as well as DA agonists, e.g. Rotigotine [175]. Studies in PD models suggested that nicotine and agonists of nicotinic receptors are neuroprotective [176].
Low activity of glucocerebrosidase is a genetic risk factor for about 10% of PD patients [10] and appears to contribute to the accumulation of undegraded GSL in lysosomes. Aggregated SNCA may also reduce normal lysosomal function. The treatment options for PD may resemble those for Gaucher’s disease to reduce the amount of GlcCer. Substrate reduction therapy involves the inhibition of the biosynthesis of GlcCer by ceramide β-Glc-transferase. Enzyme replacement is a difficult procedure and has had moderate therapeutic success. Gene therapy that introduces the glucocerebrosidase gene in an adenovirus vector into the brain has been successful in animal models of Gaucher’s disease and may be an option for patients with advanced PD in the future.
Clinical trials in PD patients showed improvements in PD symptoms upon treatment with GM1 and give hope for a treatment that restores neuronal functions [177, 178]. Ganglioside GM1 has consistently shown to be beneficial in preventing SNCA aggregation and also enhances the survival functions of neurotrophin receptors. The question is if any of these methods and agents are still effective at advanced stages of PD. It is thus critical to develop technology to replace non-functional or dead neurons. Transplantation of dopaminergic neurons developed from stem cells may offer a future remedy for neurodegenerative diseases [179].
Potential of neural stem cells
Stem cells are rich in cell surface receptor glycoproteins and GSL and are of great interest in the field of medical research because of their potential to restore diseased tissues. Therapeutic strategies for PD treatment should aim at preserving the structure and function of dopaminergic neurons. Several stem cell types, procedures and reagents to differentiate them towards dopaminergic neurons are available. Stem cells generally grow well in culture and can be induced to form brain-like organoids. This is a potential problem when introducing stem cells into the brain due to a possibility of tumor development. Stem cells may also be subject to potential transmission of the disease process into the healthy cells [61, 171]. Another potential hurdle is the targeting of stem cells or stem cell-derived cells to a specific area of the brain. The SNpc is buried inside the midbrain, making the delivery difficult. It could be achieved by invasive surgery. There are also reports that suggest homing mechanisms of cells from the CNS bypass the BBB [180] although this approach appears to be inefficient [181].
Human embryonic stem cells (hESC) are derived from blastocysts and can be differentiated with growth factors, small molecules and cytokines under specific conditions into pure populations of the desired cell type. Human induced pluripotent stem cells (iPSC) are very similar to hESC in that they respond to the same differentiation stimulus and generate functional mature cells. iPSC can be reprogrammed somatic cells, commonly fibroblasts or blood cells derived from the patient’s own cells. They have the advantage that they are autologous and do not induce immune responses. Pluripotent stem cells can also be induced to form organoids which may be transplanted into the human brain to replace dopaminergic neurons. Alternatively, neural stem cells (NSC) can be isolated from brain tissue, grown in culture and differentiated into dopaminergic neurons. Undifferentiated NSC proliferate well without changing their multipotency [182]. Self-renewing multipotent NSC are important to maintain the structures and functional plasticity in the adult nervous system. They are abundant during embryonal development but are rare and mostly quiescent in the adult brain. Isolated NSC displayed heterogeneous glycan structures [182,183,184,185,186] and these glycans change during differentiation. Lewisx structures (Galβ1-4 (Fucα1-3) GlcNAc-) and HNK-1 epitopes (HSO3-3GlcAβ1-3Galβ1-4GlcNAc-) are characteristic of undifferentiated NSC. The Lewisx structures are related to the ability of these NSC to undergo apoptosis [182].
Technical difficulties exist in isolating and identifying stem cells. Therefore, biomarkers are critical, and specific glycans have been used as biomarkers. However, there is a great variety of glycans between stem cells from different sources and at different stages of differentiation. As expected, the glycosylation patterns are subject to regulation during growth and differentiation and are cell–type and individual-specific [187,188,189,190]. Human NSC that express specific markers of DA neurons, release DA and exhibit functional properties have been successfully transplanted into animals [191]. Clinical trials in PD patients involving hESC and iPSC-derived neurons as well as fetal ventral mesencephalic cells have been partially successful [33, 179, 192]. Transplantation of iPSC also appeared to be very successful in a patient with advanced PD [193]. Stem cell cultures offer the possibility of gene therapy to change growth factor or SNCA expression. They could also be engineered to decrease the risk of tumor formation [194].
The glycolipids SSEA-3 and SSEA-4 are among the biomarkers to identify ESC [195, 196]. The earliest pluripotent hESC display SSEA-1 (Lewisx) as a marker [197]. Structurally distinct glycans carrying Lewisx determinants exist on subpopulations of NSC [198]. Human ESC were found to be rich in high mannose-type and fewer complex-type N-glycan structures [199]. The glycolipids expressed in NSC include GD2, GD3 and SSEA-1 [200]. Other glycans of stem cells include fucosylated and sialylated structures that are subject to regulation upon cell differentiation and in turn control cell proliferation [201]. Highly charged PSA chains attached to NCAM are common during brain development in humans and play a role in synapse formation and plasticity [121]. ESC also express PSA during their development. PSA promote cell migration and neurite outgrowth [120, 183, 202] and support neuronal survival after transplanting ESC-derived mouse motor neurons into the sciatic nerve of mice [203]. Depending on the cell culture conditions, non-human, potentially antigenic glycans, e.g. Neu5Gc, can be found among cellular glycans [195].
During differentiation of hESC towards neuronal progenitor cells, the cell surface glycans demonstrate a rapid decrease in the expression of SSEA-3 and SSEA-4, globo-series and lacto-series GSL. Simultaneously, the expression of several gangliosides including GM1, GM3, GD3, GT3 and 9-O-acetyl-GD3 was increased. This may reflect altered expression of specific glycosyltransferases [204, 205].
Human iPSC can be differentiated by basic fibroblast growth factor and epidermal growth factor [206] and can be further differentiated to neural progenitor cells (NPC) and to dopaminergic or cortical neurons or to radial glial cells by brain-derived neurotrophic factor and GDNF. Human iPSC can also generate large organoid-like structures that contain distinct layers of neurons having characteristic markers of the midbrain. Among these cells were mature dopaminergic neurons that produced NM-like granules such as those found in the SN [207]. The cells in organoids expressed markers of midbrain dopaminergic neurons that release DA and were functional after transplantation into the adult rat striatum of PD rodent models [191, 208, 209]. Human iPSC can also be modified by multiple passaging to mimic aging [210]. Dopaminergic neurons derived from iPSC that exhibited SNCA triplication expressed nuclear aging markers and more SNCA aggregates compared to the non-aging cells.
A number of clinical trials has been initiated using stem cells transplantation into PD patients [34, 177,178,179]. However, further improvement on the detailed methodology and research on the therapeutic potential of stem cells should be ongoing and should include studies of the biological role of glycosylated proteins and lipids in membranes.
Conclusions
The etiology and pathogenesis of Parkinson’s disease centers around the neuronal plasma membrane, and the lipid composition of membranes regulates their functions. Membranes are instrumental in controlling the effect of DA and the function of SNCA and its conversion to toxic species. While individual lipids have been shown to affect SNCA conversion in PD model systems, membranes are in a dynamic equilibrium and the age-related changes and particular properties of dopaminergic neuronal membranes of PD patients are not well known. The glycoconjugates on neuronal membranes regulate cell survival and apoptosis but their functions during cell differentiation are not well understood. It is essential to stop further SNCA aggregation and restore functional DA levels and synapse function. DA metabolites have a multitude of functions including NM synthesis and effects on SNCA toxicity. A new aspect of PD pathology is the link between SNCA, DA, NM and Dol that remains to be further explored. Clearly, multiple events lead to the unfortunate development of PD. Future knowledge of these events will allow the design of prevention and treatment of PD. Stem cells have enormous potential in replacing degenerated neurons, and methods to improve their delivery and restore DA and synapse function are being developed.
References
Gai, W.P., Yuan, H.X., Li, X.Q., Power, J.T., Blumbergs, P.C., Jensen, P.H.: In situ and in vitro study of colocalization and segregation of alpha-synuclein, ubiquitin, and lipids in Lewy bodies. Exp Neurol. 166(2), 324–333 (2000)
Stefanis, L.: α-Synuclein in Parkinson's disease. Cold Spring Harb Perspect Med. 2(2), a009399 (2012)
Dehay, B., Bourdenx, M., Gorry, P., Przedborski, S., Vila, M., Hunot, S., et al.: Targeting α-synuclein for treatment of Parkinson’s disease: mechanistic and therapeutic considerations. Lancet Neurol. 14(8), 855–866 (2015)
Videira, P.A.Q., Castro-Caldas, M.: Linking Glycation and Glycosylation With Inflammation and Mitochondrial Dysfunction in Parkinson’s Disease. Front Neurosci. 12, 381 (2018). https://doi.org/10.3389/fnins.2018.00381
Li, J., Uversky, V.N., Fink, A.L.: Conformational behavior of human alpha-synuclein is modulated by familial Parkinson’s disease point mutations A30P and A53T. Neurotoxicology 23(4–5), 553–567 (2002)
Ulrih, N.P., Barry, C.H., Fink, A.L.: Impact of Tyr to Ala mutations on alpha-synuclein fibrillation and structural properties. Biochim Biophys Acta. 1782, 581–585 (2008)
Dettmer, U., Newman, A.J., von Saucken, V.E., Bartels, T., Selkoe, D.: J. KTKEGV repeat motifs are key mediators of normal α-synuclein tetramerization: their mutation causes excess monomers and neurotoxicity. Proc Natl Acad Sci USA. 112, 9596–9601 (2015). https://doi.org/10.1073/pnas.1505953112
Nuytemans, K., Theuns, J., Cruts, M.V., Broeckhoven, C.: Genetic etiology of Parkinson disease associated with mutations in the SNCA, PARK2, PINK1, PARK7, and LRRK2 genes: A mutation update. Hum Mutat. 31, 763–780 (2010)
Alcalay, R.N., Levy, O.A., Waters, C.C., Fahn, S., Ford, B., Kuo, S.H., et al.: Glucocerebrosidase activity in Parkinson’s disease with and without GBA mutations. Brain 138(Pt 9), 2648–2658 (2015). https://doi.org/10.1093/brain/awv179
Do, J., McKinney, C., Sharma, P., Sidransky, E.: Glucocerebrosidase and its relevance to Parkinson disease. Mol Neurodegener. 14(1), 36 (2019)
Yap, T.L., Gruschus, J.M., Velayati, A., Westbroek, W., Goldin, E., Moaven, N., et al.: Alpha-synuclein interacts with Glucocerebrosidase providing a molecular link between Parkinson and Gaucher diseases. J Biol Chem. 286(32), 28080–28088 (2011). https://doi.org/10.1074/jbc.M111.237859
López, G.H., Ilincheta de Boschero, M.G., Castagnet, P.I., Giusto, N.M.: Age-associated changes in the content and fatty acid composition of brain glycerophospholipids. Comp Biochem Physiol Part B Biochem. 112, 331–343 (1995). https://doi.org/10.1016/0305-0491(95)00079-8
Ledesma, M.D., Martin, M.G., Dotti, C.G.: Lipid changes in the aged brain: effect on synaptic function and neuronal survival. Prog Lipid Res. 51, 23–35 (2012). https://doi.org/10.1016/j.plipres.2011.11.004
Andersson, M., Appelkvist, E.L., Kristensson, K., Dallner, G.: Distribution of Dolichol and Dolichyl Phosphate in Human Brain. J Neurochem. 49, 685–691 (1987)
Lai, C.S., Schutzbach, J.S.: Localization of Dolichols in Phospholipid Membranes. An ESR Spin Label Study. FEBS Lett 203, 153–156 (1986)
Schutzbach, J.S., Jensen, J.W., Lai, C.S., Monti, J.A.: Membrane Structure and Mannosyltransferase Activities: The Effect of Dolichols on Membranes. Chem. Scr. 27, 109–118 (1987)
Ward, W.C., Guan, Z., Zucca, F.A., et al.: Identification and quantification of dolichol and dolichoic acid in neuromelanin from substantia nigra of the human brain. J Lipid Res. 48(7), 1457–1462 (2007)
Engelen, M., Vanna, R., Bellei, C., et al.: Neuromelanins of human brain have soluble and insoluble components with dolichols attached to the melanic structure. PLoS One. 7(11), e48490 (2012)
Ono, K.: The Oligomer Hypothesis in α-Synucleinopathy. Neurochem Res. 42(12), 3362–3371 (2017)
Ugalde, C.L., Lawson, V.A., Finkelstein, D.I., Hill, A.F.: The role of lipids in α-synuclein misfolding and neurotoxicity. J Biol Chem. 294(23), 9016–9028 (2019)
Singleton, A.B., Farrer, M., Johnson, J., Singleton, A., Hague, S., Kachergus, J., et al.: α-synuclein locus triplication causes Parkinson’s disease. Science 302, 841 (2003). https://doi.org/10.1126/science.1090278
Oliveira, L.M., Falomir-Lockhart, L.J., Botelho, M.G., Lin, K.H., Wales, P., Koch, J.C., et al.: Elevated α-synuclein caused by SNCA gene triplication impairs neuronal differentiation and maturation in Parkinson’s patient-derived induced pluripotent stem cells. Cell Death Dis. 6(11), e1994 (2015). https://doi.org/10.1038/cddis.2015.318
Sandal, M., Valle, F., Tessari, I., Mammi, S., Bergantino, E., Musiani, F., et al.: Conformational equilibria in monomeric alpha-synuclein at the single-molecule level. PLoS Biol. 6(1), e6 (2008). https://doi.org/10.1371/journal.pbio.0060006
Galvagnion, C., Topgaard, D., Makasewicz, K., Buell, A.K., Linse, S., Sparr, E., Dobson, C.M.: Lipid Dynamics and Phase Transition within α-Synuclein Amyloid Fibrils. J Phys Chem Lett. 10(24), 7872–7877 (2019). https://doi.org/10.1021/acs.jpclett.9b03005
α-Synuclein membrane interactions and lipid specificity: Jo, E., McLaurin, J. A., Yip, C. M., St. George-Hyslop, P. Fraser, P. E. J Biol Chem. 275, 34328–34334 (2000)
Lee, H.J., Choi, C., Lee, S.J.: Membrane-bound alpha-synuclein has a high aggregation propensity and The ability to seed the aggregation of the cytosolic form. J Biol Chem. 277(1), 671–678 (2002)
Wu, G., Lu, Z.H., Kulkarni, N., Ledeen, R.W.: Deficiency of ganglioside GM1 correlates with Parkinson’s disease in mice and humans. J Neurosci Res. 90(10), 1997–2008 (2012)
Kubo, S.I.: Membrane lipids as therapeutic targets for Parkinson’s disease: a possible link between Lewy pathology and membrane lipids. Expert Opin Ther Targets. 20(11), 1301–1310 (2016)
Galvagnion, C.: The Role of Lipids Interacting with α-Synuclein in the Pathogenesis of Parkinson’s Disease. J Parkinsons Dis. 7(3), 433–450 (2017)
Hartl, F.U.: Protein Misfolding Diseases. Annu Rev Biochem. 86, 21–26 (2017). https://doi.org/10.1146/annurev-biochem-061516-044518
Brummel, B.E., Braun, A.R., Sachs, J.N.: Polyunsaturated chains in asymmetric lipids disorder raft mixtures and preferentially associate with α-Synuclein. Biochim Biophys Acta Biomembr. 1859(4), 529–536 (2017)
Banks, W.A.: Characteristics of compounds that cross the blood-brain barrier. BMC Neurol. 9 Suppl 1(Suppl 1), S3 (2009). https://doi.org/10.1186/1471-2377-9-S1-S3
Parmar, M.: Towards stem cell based therapies for Parkinson's disease. Development. 145(1), dev156117 (2018).
Reddy, A.P., Ravichandran, J., Carkaci-Salli, N.: Neural regeneration therapies for Alzheimer’s and Parkinson’s disease-related disorders. Biochim Biophys Acta Mol Basis Dis. 1866(4), 165506 (2020). https://doi.org/10.1016/j.bbadis.2019.06.020
Falkenburger, B.H., Saridaki, T., Dinter, E.: Cellular models for Parkinson's disease. J Neurochem. 139 Suppl 1, 121–130 (2016) https://doi.org/10.1111/jnc.13618
Lotharius, J., Falsig, J., van Beek, J., Payne, S., Dringen, R., Brundin, P., Leist, M.: Progressive degeneration of human mesencephalic neuron-derived cells triggered by dopamine-dependent oxidative stress is dependent on the mixed-lineage kinase pathway. J Neurosci. 25(27), 6329–6342 (2005). https://doi.org/10.1523/JNEUROSCI.1746-05.2005
Wu, G., Lu, Z.H., Seo, J.H., Alselehdar, S.K., DeFrees, S., Ledeen, R.W.: Mice deficient in GM1 manifest both motor and non-motor symptoms of Parkinson’s disease; successful treatment with synthetic GM1 ganglioside. Exp Neurol. 329, 113284 (2020). https://doi.org/10.1016/j.expneurol.2020.113284
Mesa-Herrera, F., Taoro-González, L., Valdés-Baizabal, C., Diaz, M., Marín, R.: Lipid and Lipid Raft Alteration in Aging and Neurodegenerative Diseases: A Window for the Development of New Biomarkers. Int J Mol Sci. 20(15), 3810 (2019). https://doi.org/10.3390/ijms20153810
Fabelo, N., Martín, V., Santpere, G., Marín, R., Torrent, L., Ferrer, I., Díaz, M.: Severe alterations in lipid composition of frontal cortex lipid rafts from Parkinson’s disease and incidental Parkinson’s disease. Mol Med. 17(9–10), 1107–1118 (2011). https://doi.org/10.2119/molmed.2011.00119
Powers, R., Lei, S., Anandhan, A., Marshall, D.D., Worley, B., Cerny, R.L., et al.: Metabolic Investigations of the Molecular Mechanisms Associated with Parkinson’s Disease. Metabolites 7(2), 22 (2017). https://doi.org/10.3390/metabo7020022
Viana, S.D., Valero, J., Rodrigues-Santos, P., Couceiro, P., Silva, A.M., Carvalho, F., et al.: Regulation of striatal astrocytic receptor for advanced glycation end-products variants in an early stage of experimental Parkinson’s disease. J Neurochem. 138(4), 598–609 (2016). https://doi.org/10.1111/jnc.13682
Padmaraju, V., Bhaskar, J.J., Prasada Rao, U.J., Salimath, P.V., Rao, K.S.: Role of advanced glycation on aggregation and DNA binding properties of alpha-synuclein. J Alzheimers Dis. 24(Suppl 2), 211–221 (2011). https://doi.org/10.3233/JAD-2011-101965
Russell, A.C., Šimurina, M., Garcia, M.T., Novokmet, M., Wang, Y., Rudan, I., et al.: The N-glycosylation of immunoglobulin G as a novel biomarker of Parkinson’s disease. Glycobiology 27(5), 501–510 (2017). https://doi.org/10.1093/glycob/cwx022
Le Grand, J.N., Gonzalez-Cano, L., Pavlou, M.A., Schwamborn, J.C.: Neural stem cells in Parkinson’s disease: a role for neurogenesis defects in onset and progression. Cell Mol Life Sci. 72(4), 773–797 (2015). https://doi.org/10.1007/s00018-014-1774-1
Alza, N.P., Iglesias González, P.A., Conde, M.A., Uranga, R.M., Salvador, G.A.: Lipids at the Crossroad of α-Synuclein Function and Dysfunction: Biological and Pathological Implications. Front Cell Neurosci. 13, 175 (2019). https://doi.org/10.3389/fncel.2019.00175
Giasson, B.I., Duda, J.E., Quinn, S.M., Zhang, B., Trojanowski, J.Q., Lee, V.M.: Neuronal alpha-synucleinopathy with severe movement disorder in mice expressing A53T human alpha-synuclein. Neuron 34(4), 521–533 (2002). https://doi.org/10.1016/s0896-6273(02)00682-7
Jankovic, J., Tan, E.K.: Parkinson’s disease: etiopathogenesis and treatment. J Neurol Neurosurg Psychiatry. 91(8), 795–808 (2020). https://doi.org/10.1136/jnnp-2019-322338
Bendor, J., Logan, T., Edward, R.H.: The Function of α-Synuclein. Neuro 79(6), 1044–1066 (2013)
Caputi, V., Giron, M.C.: Microbiome-Gut-Brain Axis and Toll-Like Receptors in Parkinson’s Disease. Int J Mol Sci. 19(6), 1689 (2018). https://doi.org/10.3390/ijms19061689
Liddle, R.A.: Parkinson’s disease from the gut. Brain Res. 1693(Pt B), 201–206 (2018). https://doi.org/10.1016/j.brainres.2018.01.010
Elfil, M., Kamel, S., Kandil, M., Koo, B.B., Schaefer, S.M.: Implications of the Gut Microbiome in Parkinson's Disease Mov Disord. 35(6), 921–933 (2020). https://doi.org/10.1002/mds.28004
Herath, M., Hosie, S., Bornstein, J.C., Franks, A.E., Hill-Yardin, E.L.: The Role of the Gastrointestinal Mucus System in Intestinal Homeostasis: Implications for Neurological Disorders. Front Cell Infect Microbiol. 10, 248 (2020). https://doi.org/10.3389/fcimb.2020.00248
Fusco, G., Sanz-Hernandez, M., De Simone, A.: Order and disorder in the physiological membrane binding of α-synuclein. Curr Opin Struct Biol. 48, 49–57 (2018). https://doi.org/10.1016/j.sbi.2017.09.004
Badawy, M.M.S., Okada, T., Kajimoto, T., Hirase, M., Matovelo, S., Nakamura, S., et al.: Extracellular α-Synuclein Drives Sphingosine 1-Phosphate Receptor Subtype 1 out of Lipid Rafts, Leading to Impaired Inhibitory G-Protein Signaling. J Biol Chem. 293, 8208–8216 (2018)
Rasheed, M., Liang, J., Wang, C., Deng, Y., Chen, Z.: Epigenetic Regulation of Neuroinflammation in Parkinson’s Disease. Int J Mol Sci. 22(9), 4956 (2021). https://doi.org/10.3390/ijms22094956
MacMahon Copas, A.N., McComish, S.F., Fletcher, J.M., Caldwell, M.A.: The Pathogenesis of Parkinson’s Disease: A Complex Interplay Between Astrocytes, Microglia, and T Lymphocytes? Front Neurol. 12, 666737 (2021). https://doi.org/10.3389/fneur.2021.666737
Ma, J., Gao, J., Wang, J., Xie, A.: Prion-Like Mechanisms in Parkinson’s Disease. Front Neurosci. 13, 552 (2019). https://doi.org/10.3389/fnins.2019.00552
Cohlberg, J.A., Li, J., Uversky, V.N., Fink, A.L.: Heparin and other glycosaminoglycans stimulate the formation of amyloid fibrils from alpha-synuclein in vitro. Biochemistry 41(5), 1502–1511 (2002). https://doi.org/10.1021/bi011711s
Desplats, P., Lee, H.-J., Bae, E.-J., Patrick, C., Rockenstein, E., Crews, L., et al.: Inclusion formation and neuronal cell death through neuron-to-neuron transmission of alpha-synuclein. Proc Natl Acad Sci USA 106, 13010–13015 (2009). https://doi.org/10.1073/pnas.0903691106
Liu, I.H., Uversky, V.N., Munishkina, L.A., Fink, A.L., Halfter, W., Cole, G.J.: Agrin binds alpha-synuclein and modulates alpha-synuclein fibrillation. Glycobiology 15(12), 1320–1331 (2005). https://doi.org/10.1093/glycob/cwj014
Surmeier, D.J.: Determinants of dopaminergic neuron loss in Parkinson’s disease. FEBS J. 285(19), 3657–3668 (2018). https://doi.org/10.1111/febs.14607
Wong, Y.C., Luk, K., Purtell, K., Burke Nanni, S., Stoessl, A.J., Trudeau, L.E., et al.: Neuronal vulnerability in Parkinson disease: Should the focus be on axons and synaptic terminals? Mov Disord. 34(10), 1406–1422 (2019). https://doi.org/10.1002/mds.27823
Karpowicz, R.J., Jr., Trojanowski, J.Q., Lee, V.M.: Transmission of α-synuclein seeds in neurodegenerative disease: recent developments. Lab Invest. 99(7), 971–981 (2019). https://doi.org/10.1038/s41374-019-0195-z
Weber, A.N., Morse, M.A., Gay, N.J.: Four N-linked glycosylation sites in human toll-like receptor 2 cooperate to direct efficient biosynthesis and secretion. J Biol Chem. 279(33), 34589–34594 (2004). https://doi.org/10.1074/jbc.M403830200
Hughes, C.D., Choi, M.L., Ryten, M., Hopkins, L., Drews, A., Botía, J.A., et al.: Picomolar concentrations of oligomeric alpha-synuclein sensitizes TLR4 to play an initiating role in Parkinson’s disease pathogenesis. Acta Neuropathol. 137(1), 103–120 (2019). https://doi.org/10.1007/s00401-018-1907-y
Amith, S.R., Jayanth, P., Franchuk, S., Finlay, T., Seyrantepe, V., Beyaert, R., Pshezhetsky, A.V., Szewczuk, M.R.: Neu1 desialylation of sialyl alpha-2,3-linked beta-galactosyl residues of TOLL-like receptor 4 is essential for receptor activation and cellular signaling. Cell Signal. 22(2), 314–324 (2010). https://doi.org/10.1016/j.cellsig.2009.09.038
Voutilainen, M.H., Arumäe, U., Airavaara, M., Saarma, M.: Therapeutic potential of the endoplasmic reticulum located and secreted CDNF/MANF family of neurotrophic factors in Parkinson's disease. FEBS Lett. 589(24 Pt A), 3739–3748 (2015). https://doi.org/10.1016/j.febslet.2015.09.031
Perez, R.G., Waymire, J.C., Lin, E., Liu, J.J., Guo, F., Zigmond, M.J.: A role for alpha-synuclein in the regulation of dopamine biosynthesis. J Neurosci. 22(8), 3090–3099 (2002). https://doi.org/10.1523/JNEUROSCI.22-08-03090.2002
Venda, L.L., Cragg, S.J., Buchman, V.L., Wade-Martins, R.: α-Synuclein and dopamine at the crossroads of Parkinson’s disease. Trends Neurosci. 33(12), 559–568 (2010). https://doi.org/10.1016/j.tins.2010.09.004
Butler, B., Sambo, D., Khoshbouei, H.: Alpha-synuclein modulates dopamine neurotransmission. J Chem Neuroanat. 83–84, 41–49 (2017)
Itäaho, K., Court, M.H., Uutela, P., Kostiainen, R., Radominska-Pandya, A., Finel, M.: Dopamine is a low-affinity and high-specificity substrate for the human UDP-glucuronosyltransferase 1A10. Drug Metab Dispos. 37(4), 768–775 (2009). https://doi.org/10.1124/dmd.108.025692
Piras, S., Furfaro, A.L., Domenicotti, C., Traverso, N., Marinari, U.M., Pronzato, M.A., Nitti, M.: RAGE Expression and ROS Generation in Neurons: Differentiation versus Damage. Oxid Med Cell Longev. 2016, 9348651 (2016). https://doi.org/10.1155/2016/9348651
Segura-Aguilar, J., Paris, I., Muñoz, P., Ferrari, E., Zecca, L., Zucca, F.A.: Protective and toxic roles of dopamine in Parkinson’s disease. J Neurochem. 129(6), 898–915 (2014). https://doi.org/10.1111/jnc.12686
Man, W.K., Tahirbegi, B., Vrettas, M.D. et al. The docking of synaptic vesicles on the presynaptic membrane induced by α-synuclein is modulated by lipid composition. Nat Commun 12, 927 (2021). https://doi.org/10.1038/s41467-021-21027-4
Fountaine, T.M., Venda, L.L., Warrick, N., Christian, H.C., Brundin, P., Channon, K.M., Wade-Martins, R.: The effect of alpha-synuclein knockdown on MPP+ toxicity in models of human neurons. Eur J Neurosci. 28(12), 2459–2473 (2008). https://doi.org/10.1111/j.1460-9568.2008.06527.x
Rilstone, J.J., Alkhater, R.A., Minassian, B.A.: Brain dopamine-serotonin vesicular transport disease and its treatment. N Engl J Med. 368(6), 543–550 (2013). https://doi.org/10.1056/NEJMoa1207281
Afonso-Oramas, D., Cruz-Muros, I., Alvarez de la Rosa, D., Abreu, P., Giráldez, T., Castro-Hernández, J., et al.: Dopamine transporter glycosylation correlates with the vulnerability of midbrain dopaminergic cells in Parkinson's disease. Neurobiol Dis. 36(3), 494–508 (2009). https://doi.org/10.1016/j.nbd.2009.09.002
Burré, J., Sharma, M., Tsetsenis, T., Buchman, V., Etherton, M.R., Südhof, T.C.: Alpha-synuclein promotes SNARE-complex assembly in vivo and in vitro. Science 329(5999), 1663–1667 (2010). https://doi.org/10.1126/science.1195227
Dearry, A., Gingrich, J.A., Falardeau, P., Fremeau, R.T., Jr., Bates, M.D., Caron, M.G.: Molecular cloning and expression of the gene for a human D1 dopamine receptor. Nature 347(6288), 72–76 (1990). https://doi.org/10.1038/347072a0
Villar, V.A., Jones, J.E., Armando, I., Palmes-Saloma, C., Yu, P., Pascua, A.M., Keever, L., et al.: G protein-coupled receptor kinase 4 (GRK4) regulates the phosphorylation and function of the dopamine D3 receptor. J Biol Chem. 284(32), 21425–21434 (2009). https://doi.org/10.1074/jbc.M109.003665
Albizu, L., Holloway, T., González-Maeso, J., Sealfon, S.C.: Functional crosstalk and heteromerization of serotonin 5-HT2A and dopamine D2 receptors. Neuropharmacology 61(4), 770–777 (2011). https://doi.org/10.1016/j.neuropharm.2011.05.023
Beaulieu, J.M., Gainetdinov, R.R.: The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 63(1), 182–217 (2011). https://doi.org/10.1124/pr.110.002642
Li, A., Mishra, Y., Malik, M., Wang, Q., Li, S., Taylor, M., et al.: Evaluation of N-phenyl homopiperazine analogs as potential dopamine D3 receptor selective ligands. Bioorg Med Chem. 21(11), 2988–2998 (2013). https://doi.org/10.1016/j.bmc.2013.03.074
Fishburn, C.S., Elazar, Z., Fuchs, S.: Differential glycosylation and intracellular trafficking for the long and short isoforms of the D2 dopamine receptor. J Biol Chem. 270(50), 29819–29824 (1995). https://doi.org/10.1074/jbc.270.50.29819
Min, C., Zheng, M., Zhang, X., Guo, S., Kwon, K.J., Shin, C.Y., et al.: N-linked Glycosylation on the N-terminus of the dopamine D2 and D3 receptors determines receptor association with specific microdomains in the plasma membrane. Biochim Biophys Acta. 1853(1), 41–51 (2015). https://doi.org/10.1016/j.bbamcr.2014.09.024
Marotta, N.P., Lin, Y.H., Lewis, Y.E., et al.: O-GlcNAc modification blocks the aggregation and toxicity of the protein α-synuclein associated with Parkinson’s disease. Nat Chem. 7(11), 913–920 (2015)
Karube, H., Sakamoto, M., Arawaka, S., Hara, S., Sato, H., Ren, C.H., et al.: N-terminal region of α-synuclein is essential for the fatty acid-induced oligomerization of the molecules. FEBS Lett. 582, 3693–3700 (2008). https://doi.org/10.1016/j.febslet.2008.10.001
Giasson, B.I., Murray, I.V., Trojanowski, J.Q., Lee, V.M.: A hydrophobic stretch of 12 amino acid residues in the middle of alpha-synuclein is essential for filament assembly. J Biol Chem. 276(4), 2380–2386 (2001). https://doi.org/10.1074/jbc.M008919200
Afitska, K., Fucikova, A., Shvadchak, V.V., Yushchenko, D.A.: Modification of C Terminus Provides New Insights into the Mechanism of α-Synuclein Aggregation. Biophys J. 113(10), 2182–2191 (2017). https://doi.org/10.1016/j.bpj.2017.08.027
Jo, E., Fuller, N., Rand, R.P., St George-Hyslop, P., Fraser, P.E.: Defective membrane interactions of familial Parkinson’s disease mutant A30P alpha-synuclein. J Mol Biol. 315(4), 799–807 (2002)
Ghosh, D., et al.: alpha-synuclein aggregation and its modulation. Int. J. Biol. Macromol. 100, 37–54 (2017)
Wang, W., Perovic, I., Chittuluru, J., Kaganovich, A., Nguyen, L.T., Liao, J., et al.: A soluble α-synuclein construct forms a dynamic tetramer. Proc Natl Acad Sci U S A. 108(43), 17797–17802 (2011). https://doi.org/10.1073/pnas.1113260108
Trexler, A.J., Rhoades, E.: N-Terminal acetylation is critical for forming a-helical oligomer of a-synuclein. Protein Sci. 21, 601–605 (2012)
Zhu, M., Li, J., Fink, A.L.: The association of alpha-synuclein with membranes affects bilayer structure, stability, and fibril formation. J Biol Chem. 278(41), 40186–40197 (2003)
Zhu, M., Fink, A.L.: Lipid binding inhibits alpha-synuclein fibril formation. J Biol Chem. 278(19), 16873–16877 (2003)
Arawaka, S., Sato, H., Sasaki, A., Koyama, S., Kato, T.: Mechanisms underlying extensive Ser129-phosphorylation in α-synuclein aggregates. Acta Neuropathol Commun. 5(1), 48 (2017). https://doi.org/10.1186/s40478-017-0452-6
Paleologou, K.E., Oueslati, A., Shakked, G., Rospigliosi, C.C., Kim, H.-Y., Lamberto, G.R., et al.: Phosphorylation at S87 is enhanced in synucleinopathies, inhibits alpha-synuclein oligomerization, and influences synuclein-membrane interactions. J Neurosci. 30, 3184–3198 (2010). https://doi.org/10.1523/JNEUROSCI.5922-09.2010
O’Leary, E.I., Jiang, Z., Strub, M.P., Lee, J.C.: Effects of phosphatidylcholine membrane fluidity on the conformation and aggregation of N-terminally acetylated α-Synuclein. J Biol Chem. 293, 11195–11205 (2018). https://doi.org/10.1074/jbc.RA118.002780
O’Leary, E.I., Lee, J.C.: Interplay between α-synuclein amyloid formation and membrane structure. Biochim. Biophys. Acta Proteins Proteom. 1867, 483–491 (2018). https://doi.org/10.1016/j.bbapap.2018.09.012
Bartels, T., Kim, N.C., Luth, E.S., Selkoe, D.J.: N-alpha-acetylation of α-synuclein increases its helical folding propensity, GM1 binding specificity and resistance to aggregation. PLoS ONE 9, e103727 (2014). https://doi.org/10.1371/journal.pone.0103727
König, A., Vicente Miranda, H., Outeiro, T.F.: Alpha-Synuclein Glycation and the Action of Anti-Diabetic Agents in Parkinson’s Disease. J Parkinsons Dis. 8(1), 33–43 (2018). https://doi.org/10.3233/JPD-171285
Guerrero, E., Vasudevaraju, P., Hegde, M.L., Britton, G.B., Rao, K.S.: Recent advances in α-synuclein functions, advanced glycation, and toxicity: implications for Parkinson’s disease. Mol Neurobiol. 47(2), 525–536 (2013). https://doi.org/10.1007/s12035-012-8328-z
Vicente Miranda, H., Szego, É.M., Oliveira, L.M.A., Breda, C., Darendelioglu, E., de Oliveira, R.M., et al.: Glycation potentiates α-synuclein-associated neurodegeneration in synucleinopathies. Brain. 140(5), 1399–1419 (2017). https://doi.org/10.1093/brain/awx056
Jin, Q., Chen, H., Luo, A., Ding, F., Liu, Z.: S100A14 stimulates cell proliferation and induces cell apoptosis at different concentrations via receptor for advanced glycation end products (RAGE). PLoS ONE 6(4), e19375 (2011). https://doi.org/10.1371/journal.pone.0019375
De Oliveira, R.M., Vicente Miranda, H., Francelle, L., Pinho, R., Szegö, É.M., Martinho, R., et al.: The mechanism of sirtuin 2-mediated exacerbation of alpha-synuclein toxicity in models of Parkinson disease. PLoS Biol. 15(3), e2000374 (2017). https://doi.org/10.1371/journal.pbio.2000374
He, Y., Yu, Z., Chen, S.: Alpha-Synuclein Nitration and Its Implications in Parkinson’s Disease. ACS Chem Neurosci. 10(2), 777–782 (2019). https://doi.org/10.1021/acschemneuro.8b00288
Cole, R.N., Hart, G.W.: Cytosolic O-glycosylation is abundant in nerve terminals. J Neurochem. 79(5), 1080–1089 (2001)
Gao, Y., Wells, L., Comer, F.I., Parker, G.J., Hart, G.W.: Dynamic O-glycosylation of nuclear and cytosolic proteins: cloning and characterization of a neutral, cytosolic beta-N-acetylglucosaminidase from human brain. J Biol Chem. 276(13), 9838–9845 (2001). https://doi.org/10.1074/jbc.M010420200
Kang, L., Moriarty, G.M., Woods, L.A., Ashcroft, A.E., Radford, S.E., Baum, J.: N-terminal acetylation of α-synuclein induces increased transient helical propensity and decreased aggregation rates in the intrinsically disordered monomer. Protein Sci. 21(7), 911–917 (2012). https://doi.org/10.1002/pro.2088
Levine, P.M., et al.: A-Synuclein O-GlcNAcylation alters aggregation and toxicity, revealing certain residues as potential inhibitors of Parkinson’s disease. Proc Natl Acad Sci U S A. 116(5), 1511–1519 (2019)
Banerjee, P.S., Lagerlöf, O., Hart, G.W.: Roles of O-GlcNAc in chronic diseases of aging. Mol Aspects Med. 51, 1–15 (2016). https://doi.org/10.1016/j.mam.2016.05.005
Wang, A.C., Jensen, E.H., Rexach, J.E., Vinters, H.V., Hsieh-Wilson, L.C.: Loss of O-GlcNAc glycosylation in forebrain excitatory neurons induces neurodegeneration. Proc Natl Acad Sci U S A. 113, 15120–15125 (2016)
Sipione, S., Monyror, J., Galleguillos, D., Steinberg, N., Kadam, V.: Gangliosides in the Brain: Physiology. Pathophysiology and Therapeutic Applications. Front Neurosci. 14, 572965 (2020). https://doi.org/10.3389/fnins.2020.572965
Seyfried, T.N., Choi, H., Chevalier, A., Hogan, D., Akgoc, Z., Schneider, J.S.: Sex-Related Abnormalities in Substantia Nigra Lipids in Parkinson’s Disease. ASN Neuro 10, 1759091418781889 (2018). https://doi.org/10.1177/1759091418781889
Huebecker, M., Moloney, E.B., van der Spoel, A.C., Priestman, D.A., Isacson, O., Hallett, P.J., Platt, F.M.: Reduced sphingolipid hydrolase activities, substrate accumulation and ganglioside decline in Parkinson’s disease. Mol Neurodegener. 14, 40 (2019). https://doi.org/10.1186/s13024-019-0339-z
Lai, C.S., Schutzbach, .JS.: Dolichol Induces Membrane Leakage of Liposomes Composed of Phosphatidylethanolamine and Phosphatidylcholine. FEBS Lett. 169, 279–282 (1984)
Egawa, J., Pearn, M.L., Lemkuil, B.P., Patel, P.M., Head, B.P.: Membrane lipid rafts and neurobiology: age-related changes in membrane lipids and loss of neuronal function. J Physiol. 594(16), 4565–4579 (2016). https://doi.org/10.1113/JP270590
Fecchio, C., Palazzi, L., Polverino de Laureto, P.: α-Synuclein and polyunsaturated fatty acids: molecular basis of the interaction and implication in neurodegeneration. Molecules. 23, E1531 (2018). https://doi.org/10.3390/molecules23071531
Tettamanti, G., Preti, A., Cestaro, B., Venerando, B., Lombardo, A., Ghidoni, R., Sonnino, S.: Gangliosides, neuraminidase and sialyltransferase at the nerve endings. Adv Exp Med Biol. 125, 263–281 (1980). https://doi.org/10.1007/978-1-4684-7844-0_25
Angata, K., Fukuda, M.: Roles of polysialic acid in migration and differentiation of neural stem cells. Methods Enzymol. 479, 25–36 (2010). https://doi.org/10.1016/S0076-6879(10)79002-9
Hildebrandt, H., Dityatev, A.: Polysialic Acid in Brain Development and Synaptic Plasticity. Top Curr Chem. 366, 55–96 (2015). https://doi.org/10.1007/128_2013_446
Schiff, M., Weinhold, B., Grothe, C., Hildebrandt, H.: NCAM and polysialyltransferase profiles match dopaminergic marker gene expression but polysialic acid is dispensable for development of the midbrain dopamine system. J Neurochem. 110(5), 1661–1673 (2009). https://doi.org/10.1111/j.1471-4159.2009.06267.x
Gao, Y., Luan, X., Melamed, J., Brockhausen, I. Role of Glycans on Key Cell Surface Receptors That Regulate Cell Proliferation and Cell Death. Cells. 10(5), 1252 (2021). https://doi.org/10.3390/cells10051252
Woronowicz, A., Amith, S.R., De Vusser, K., Laroy, W., Contreras, R., Basta, S., Szewczuk, M.R.: Dependence of neurotrophic factor activation of Trk tyrosine kinase receptors on cellular sialidase. Glycobiology 17(1), 10–24 (2007). https://doi.org/10.1093/glycob/cwl049
Ledeen, R.W., Wu, G.: Gangliosides, α-Synuclein, and Parkinson’s Disease. Prog Mol Biol Transl Sci. 156, 435–454 (2018). https://doi.org/10.1016/bs.pmbts.2017.12.009
Comoletti, D., Flynn, R., Jennings, L.L., Chubykin, A., Matsumura, T., Hasegawa, H., Südhof, T.C., Taylor, P.: Characterization of the interaction of a recombinant soluble neuroligin-1 with neurexin-1beta. J Biol Chem. 278(50), 50497–50505 (2003). https://doi.org/10.1074/jbc.M306803200
Birol, M., Wojcik, S.P., Miranker, A.D., Rhoades, E.: Identification of N-linked glycans as specific mediators of neuronal uptake of acetylated α-Synuclein. PLoS Bio 17(6), e3000318 (2019). https://doi.org/10.1371/journal.pbio.3000318
Dikiy, I., Eliezer, D.: Folding and misfolding of alpha-synuclein on membranes. Biochim Biophys Acta. 1818, 1013–1018 (2012). https://doi.org/10.1016/j.bbamem.2011.09.008
Terakawa, M.S., Lee, Y.H., Kinoshita, M., Lin, Y., Sugiki, T., Fukui, N., et al.: Membrane-induced initial structure of α-synuclein control its amyloidogenesis on model membranes. Biochim Biophys Acta. 1860, 757–766 (2018). https://doi.org/10.1016/j.bbamem.2017.12.011
Lorenzen, N., Lemminger, L., Pedersen, J.N., Nielsen, S.B., Otzen, D.E.: The N-terminus of α-synuclein is essential for both monomeric and oligomeric interactions with membranes. FEBS Lett. 588(3), 497–502 (2014). https://doi.org/10.1016/j.febslet.2013.12.015
Starheim, K.K., Arnesen, T., Gromyko, D., Ryningen, A., Varhaug, J.E., Lillehaug, J.R.: Identification of the human N(alpha)-acetyltransferase complex B (hNatB): a complex important for cell-cycle progression. Biochem J. 415(2), 325–331 (2008). https://doi.org/10.1042/BJ20080658
Fusco, G., Chen, S.W., Williamson, P.T.F., Cascella, R., Perni, M., Jarvis, J.A., et al.: Structural basis of membrane disruption and cellular toxicity by α-synuclein oligomers. Science 358, 1440–1443 (2017). https://doi.org/10.1126/science.aan6160
Shvadchak, V.V., Yushchenko, D.A., Pievo, R., Jovin, T.M.: The mode of α-synuclein binding to membranes depends on lipid composition and lipid to protein ratio. FEBS Lett. 585(22), 3513–3519 (2011). https://doi.org/10.1016/j.febslet.2011.10.006
Mizuno, S., Sasai, H., Kume, A., et al.: Dioleoyl-phosphatidic acid selectively binds to αsynuclein and strongly induces its aggregation. FEBS Lett. 591(5), 784–791 (2017)
Carroll, C.B., Wyse, R.K.H.: Simvastatin as a Potential Disease-Modifying Therapy for Patients with Parkinson’s Disease: Rationale for Clinical Trial, and Current Progress. J Parkinsons Dis. 7(4), 545–568 (2017). https://doi.org/10.3233/JPD-171203
Perrin, R.J., Woods, W.S., Clayton, D.F., George, J.M.: Exposure to long chain polyunsaturated fatty acids triggers rapid multimerization of synucleins. J Biol Chem. 276(45), 41958–41962 (2001)
De Franceschi, G., Frare, E., Pivato, M., Relini, A., Penco, A., Greggio, E., et al.: Structural and morphological characterization of aggregated species of α-synuclein induced by docosahexaenoic acid. J Biol Chem. 286(25), 22262–22274 (2011). https://doi.org/10.1074/jbc.M110.202937
De Franceschi, G., Fecchio, C., Sharon, R., Schapira, A.H.V., Proukakis, C., Bellotti, V., et al.: α-Synuclein structural features inhibit harmful polyunsaturated fatty acid oxidation, suggesting roles in neuroprotection. J Biol Chem. 292, 6927–6937 (2017). https://doi.org/10.1074/jbc.M116.765149
Davidson, W.S., Jonas, A., Clayton, D.F., George, J.M.: Stabilization of alpha-synuclein secondary structure upon binding to synthetic membranes. J Biol Chem. 273(16), 9443–9449 (1998). https://doi.org/10.1074/jbc.273.16.9443
Martinez, Z., Zhu, M., Han, S., Fink, A.L.: GM1 Specifically Interacts with Alpha-Synuclein and Inhibits Fibrillation. Biochem Pharmacol. 46, 1868–1877 (2007)
Schneider, J.S.: Altered expression of genes involved in ganglioside biosynthesis in substantia nigra neurons in Parkinson’s disease. PLoS ONE 13(6), e0199189 (2018). https://doi.org/10.1371/journal.pone.0199189
Ledeen, R., Wu, G.: New findings on nuclear gangliosides: overview on metabolism and function. J Neurochem. 116(5), 714–720 (2011). https://doi.org/10.1111/j.1471-4159.2010.07115.x
Chiricozzi, E., Di Biase, E., Lunghi, G., Fazzari, M., Loberto, N., Aureli, M., Mauri, L., Sonnino, S.: Turning the spotlight on the oligosaccharide chain of GM1 ganglioside. Glycoconj J. 38(1), 101–117 (2021). https://doi.org/10.1007/s10719-021-09974-y
Galvagnion, C., Buell, A.K., Meisl, G., Michaels, T.C., Vendruscolo, M., Knowles, T.P., Dobson, C.M.: Lipid vesicles trigger α-synuclein aggregation by stimulating primary nucleation. Nat Chem Biol. 11(3), 229–234 (2015). https://doi.org/10.1038/nchembio.1750
Jensen, J.W., Schutzbach, J.S.: Activation of Mannosyltranferase II by Nonbilayer Phospholipids Biochemistry. 23, 1115–1119 (1984)
Monti, J.A., Christian, S.T., Schutzbach, J.S.: Effects of Dolichol on Membrane Properties. Biochim Biophys Acta. 905, 133–142 (1987)
Adair, W.L. Jr., Keller, R.K.: Dolichol metabolism in rat liver. Determination of the subcellular distribution of dolichyl phosphate and its site and rate of de novo biosynthesis. J Biol Chem. 257(15):8990–8996 (1982)
Rip, J.W., Rupar, C.A., Ravi, K., Carroll, K.K.: Distribution, metabolism and function of dolichol and polyprenols. Prog Lipid Res. 24(4), 269–309 (1985)
Edlund, C., Söderberg, M., Kristensson, K.: Isoprenoids in aging and neurodegeneration. Neurochem Int. 25(1), 35–38 (1994). https://doi.org/10.1016/0197-0186(94)90050-7
Daniels, I., Hemming, F.W.: Changes in murine tissue concentrations of dolichol and dolichol derivatives associated with age. Lipids 25(10), 586–593 (1990). https://doi.org/10.1007/BF02536006
Ward, W.C., Zucca, F.A., Bellei, C., Zecca, L., Simon, J.D.: Neuromelanins in various regions of human brain are associated with native and oxidized isoprenoid lipids. Arch Biochem Biophys. 484(1), 94–99 (2009)
Bergamini, E., Bizzarri, R., Cavallini, G., Cerbai, B., Chiellini, E., Donati, A., et al.: Ageing and oxidative stress: a role for dolichol in the antioxidant machinery of cell membranes? J Alzheimers Di 6(2), 129–135 (2004). https://doi.org/10.3233/jad-2004-6204
Schutzbach, J.S., Jensen, J.W.: Bilayer Membrane Destabilization Induced by DolichylPhosphate. Chem Phys Lipids. 51, 213–218 (1989)
Buczkowska, A., Swiezewska, E., Lefeber, D.J.: Genetic defects in dolichol metabolism J Inherit Metab Dis. 38, 157–169 (2015)
Bar-On, P., Crews, L., Koob, A.O., Mizuno, H., Adame, A., Spencer, B., et al.: Statins reduce neuronal α-synuclein aggregation in in vitro models of Parkinson’s disease. J Neurochem. 105, 1656–1667 (2008). https://doi.org/10.1111/j.1471-4159.2008.05254.x
Atil, B., Berger-Sieczkowski, E., Bardy, J., Werner, M., Hohenegger, M.: In vitro and in vivo downregulation of the ATP binding cassette transporter B1 by the HMG-CoA reductase inhibitor simvastatin. Naunyn Schmiedebergs Arch Pharmacol. 389(1), 17–32 (2016). https://doi.org/10.1007/s00210-015-1169-3
Grabinska, K., A., et al.: cis-Prenyltransferase: New Insights into Protein Glycosylation, Rubber Synthesis, and Human Diseases, J Biol Chem. 219(35), 18582–18590 (2016)
Kharel, Y., Takahashi, S., Yamashita, S., Koyama, T.: In vivo interaction between the human dehydrodolichyl diphosphate synthase and the Niemann-Pick C2 protein revealed by a yeast two-hybrid system. Biochem Biophys Res Commun. 318(1), 198–203 (2004). https://doi.org/10.1016/j.bbrc.2004.04.007
Morava, E., Wevers, R.A., Cantagrel, V., Hoefsloot, L.H., Al-Gazali, L., Schoots, J., et al.: A novel cerebello-ocular syndrome with abnormal glycosylation due to abnormalities in dolichol metabolism. Brain 133(11), 3210–3220 (2010). https://doi.org/10.1093/brain/awq261
Rush, E.T., Baker, C.V., Rizzo, W.B.: Dolichol kinase deficiency (DOLK-CDG): Two new cases and expansion of phenotype. Am J Med Genet A. 173(9), 2428–2434 (2017). https://doi.org/10.1002/ajmg.a.38287
Van Dessel, G., Lagrou, A., Hilderson, H.J., Dierick, W.: Characterization of the in vitro conversion of dolichol to dolichoate in bovine thyroid. Biochim Biophys Acta. 1167(3), 307–315 (1993). https://doi.org/10.1016/0005-2760(93)90234-z
Vila, M.: Neuromelanin, aging, and neuronal vulnerability in Parkinson’s disease. Mov. Disord. 34(10), 1440–1451 (2019)
Fedorow, H., Pickford, R., Hook, J.M., et al.: Dolichol is the major lipid component of human substantia nigra neuromelanin. J Neurochem. 92(4), 990–995 (2005)
Conway, K.A., Rochet, J.C., Bieganski, R.M., Lansbury, P.T., Jr.: Kinetic stabilization of the alpha-synuclein protofibril by a dopamine-alpha-synuclein adduct. Science 294(5545), 1346–1349 (2001). https://doi.org/10.1126/science.1063522
Greggio, E., Bergantino, E., Carter, D., Ahmad, R., Costin, G.E., Hearing, V.J., et al.: Tyrosinase exacerbates dopamine toxicity but is not genetically associated with Parkinson’s disease. J Neurochem. 93(1), 246–256 (2005). https://doi.org/10.1111/j.1471-4159.2005.03019.x
Hasegawa, T.: Tyrosinase-expressing neuronal cell line as in vitro model of Parkinson’s disease. Int J Mol Sci. 11(3), 1082–1089 (2010). https://doi.org/10.3390/ijms11031082
Carballo-Carbajal, I., Laguna, A., Romero-Giménez, J., et al.: Brain tyrosinase overexpression implicates age-dependent neuromelanin production in Parkinson’s disease pathogenesis. Nat Commun. 10, 973 (2019)
Haining, R.L., Achat-Mendes, C.: Neuromelanin, one of the most overlooked molecules in modern medicine, is not a spectator. Neural Regen Res. 12(3), 372–375 (2017). https://doi.org/10.4103/1673-5374.202928
Zucca, F.A., Vanna, R., Cupaioli, F.A., Bellei, C., De Palma, A., Di Silvestre, D.: Neuromelanin organelles are specialized autolysosomes that accumulate undegraded proteins and lipids in aging human brain and are likely involved in Parkinson’s disease. NPJ Parkinsons Dis. 4, 17 (2018). https://doi.org/10.1038/s41531-018-0050-8
da Silva, F.L., Coelho Cerqueira, E., de Freitas, M.S., Gonçalves, D.L., Costa, L.T., Follmer, C.: Vitamins K interact with N-terminus α-synuclein and modulate the protein fibrillization in vitro. Exploring the interaction between quinones and α-synuclein. Neurochem Int. 62(1), 103–112 (2013). https://doi.org/10.1016/j.neuint.2012.10.001
Oliveri, V.: Toward the discovery and development of effective modulators of α-synuclein amyloid aggregation. Eur J Med Chem. 167, 10–36 (2019). https://doi.org/10.1016/j.ejmech.2019.01.045
Reglodi, D., Renaud, J., Tamas, A., Tizabi, Y., Socías, S.B., Del-Bel, E., Raisman-Vozari, R.: Novel tactics for neuroprotection in Parkinson’s disease: Role of antibiotics, polyphenols and neuropeptides. Prog Neurobiol. 155, 120–148 (2017). https://doi.org/10.1016/j.pneurobio.2015.10.004
Norris, E.H., Giasson, B.I., Hodara, R., Xu, S., Trojanowski, J.Q., Ischiropoulos, H., Lee, V.M.: Reversible inhibition of alpha-synuclein fibrillization by dopaminochrome-mediated conformational alterations. J Biol Chem. 280(22), 21212–21219 (2005). https://doi.org/10.1074/jbc.M412621200
Tagliafierro, L., Chiba-Falek, O.: Up-regulation of SNCA gene expression: implications to synucleinopathies. Neurogenetics 17(3), 145–157 (2016). https://doi.org/10.1007/s10048-016-0478-0
Bonuccelli, U., Pavese, N.: Role of dopamine agonists in Parkinson’s disease: an update. Expert Rev Neurother. 7(10), 1391–1399 (2007). https://doi.org/10.1586/14737175.7.10.1391
Liu, Y., Hao, S., Yang, B., Fan, Y., Qin, X., Chen, Y., Hu, J.: Wnt/β-catenin signaling plays an essential role in α7 nicotinic receptor-mediated neuroprotection of dopaminergic neurons in a mouse Parkinson’s disease model. Biochem Pharmacol. 140, 115–123 (2017). https://doi.org/10.1016/j.bcp.2017.05.017
Magistretti, P.J., Geisler, F.H., Schneider, J.S., Li, P.A., Fiumelli, H., Sipione, S.: Gangliosides: Treatment Avenues in Neurodegenerative Disease. Front Neurol. 10, 859 (2019). https://doi.org/10.3389/fneur.2019.00859
Sidorova, Y.A., Volcho, K.P., Salakhutdinov, N.F.: Neuroregeneration in Parkinson’s Disease: From Proteins to Small Molecules. Curr Neuropharmacol. 17(3), 268–287 (2019). https://doi.org/10.2174/1570159X16666180905094123
Jang, S.E., Qiu, L., Chan, L.L., Tan, E.K., Zeng, L.: Current Status of Stem Cell-Derived Therapies for Parkinson’s Disease: From Cell Assessment and Imaging Modalities to Clinical Trials. Front Neurosci. 14, 558532 (2020). https://doi.org/10.3389/fnins.2020.558532
Chia, Y.C., Anjum, C.E., Yee, H.R., Kenisi, Y., Chan, M.K.S., Wong, M.B.F., Pan, S.Y.: Stem Cell Therapy for Neurodegenerative Diseases: How Do Stem Cells Bypass the Blood-Brain Barrier and Home to the Brain? Stem Cells International. e8889061 (2020)
Goncharova, V., Das, S., Niles, W., Schraufstatter, I., Wong, A.K., Povaly, T., et al.: Homing of neural stem cells from the venous compartment into a brain infarct does not involve conventional interactions with vascular endothelium. Stem Cells Transl Med. 3(2), 229–240 (2014). https://doi.org/10.5966/sctm.2013-0052
Yagi, H., Kato, K.: Functional roles of glycoconjugates in the maintenance of stemness and differentiation process of neural stem cells. Glycoconj J. 34(6), 757–763 (2017). https://doi.org/10.1007/s10719-016-9707-x
Yu, R.K., Yanagisawa, M.: Glycobiology of neural stem cells. CNS Neurol Disord Drug Targets. 5(4), 415–423 (2006). https://doi.org/10.2174/187152706777950675
Yanagisawa, M., Yu, R.K.: The expression and functions of glycoconjugates in neural stem cells. Glycobiology 17, 57R-74R (2007)
Yuan, S.H., Martin, J., Elia, J., Flippin, J., Paramban, R.I., Hefferan, M.P., et al.: Cell-Surface Marker Signatures for the Isolation of Neural Stem Cells, Glia and Neurons Derived from Human Pluripotent Stem Cells. PLoS One. 6, e17540 (2011)
Yale, A.R., Nourse, J.L., Lee, K.R., Ahmed, S.N., Arulmoli, J., Jiang, A.Y.L., et al.: Cell Surface N-Glycans Influence Electrophysiological Properties and Fate Potential of Neural Stem Cells. Stem Cell Reports. 11, 869–882 (2018)
Murrell, M.P., Yarema, K.J., Levchenko, A.: The systems biology of glycosylation. ChemBioChem 5(10), 1334–1347 (2004). https://doi.org/10.1002/cbic.200400143
Krasnova, L., Wong, C.H.: Exploring human glycosylation for better therapies. Mol Aspects Med. 51, 125–143 (2016). https://doi.org/10.1016/j.mam.2016.05.003
Iqbal, S., Ghanimi Fard, M., Everest-Dass, A., Packer, N.H., Parker, L.M.: Understanding cellular glycan surfaces in the central nervous system. Biochem Soc Trans. 47(1), 89–100 (2019). https://doi.org/10.1042/BST20180330
Cummings, R.D.: Stuck on sugars - how carbohydrates regulate cell adhesion, recognition, and signaling. Glycoconj. J 36(4), 241–257 (2019). https://doi.org/10.1007/s10719-019-09876-0
Kirkeby, A., Grealish, S., Wolf, D.A., Nelander, J., Wood, J., Lundblad, M., et al.: Generation of regionally specified neural progenitors and functional neurons from human embryonic stem cells under defined conditions. Cell Rep. 1(6), 703–714 (2012). https://doi.org/10.1016/j.celrep.2012.04.009
Takahashi, J.: Preparing for first human trial of induced pluripotent stem cell-derived cells for Parkinson’s disease: an interview with Jun Takahashi. Regen Med. 14(2), 93–95 (2019). https://doi.org/10.2217/rme-2018-0158
Schweitzer, J.S., Song, B., Herrington, T.M., Park, T.-Y., Lee, N., Ko, S., et al.: Personalized iPSC-Derived Dopamine Progenitor Cells for Parkinson’s Disease. N. Engl. J. Med. 382(20), 1926–1932 (2020). https://doi.org/10.1056/nejmoa1915872
Venkataramana, N.K., Kumar, S.K., Balaraju, S., Radhakrishnan, R.C., Bansal, A., Dixit, A., et al.: Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease. Transl Res. 155(2), 62–70 (2010). https://doi.org/10.1016/j.trsl.2009.07.006
Lanctot, P.M., Gage, F.H., Varki, A.P.: The Glycans of Stem Cells. Curr Opin Chem Biol. 11, 373–380 (2007)
Breimer, M.E., Säljö, K., Barone, A., Teneberg, S.: Glycosphingolipids of human embryonic stem cells. Glycoconj J. 34(6), 713–723 (2017). https://doi.org/10.1007/s10719-016-9706-y
Terashima, M., Amano, M., Onodera, T., Nishimura, S.-I., Iwasaki, N.: Quantitative glycomics monitoring of induced pluripotent- and embryonic stem cells during neuronal differentiation. Stem Cell Research. 13, 454–464 (2014)
Hennen, E., Czopka, T., Faissner, A.: Structurally Distinct LewisX Glycans Distinguish Subpopulations of Neural Stem/Progenitor Cells. J Biol Chem. 286, 16321–16331 (2011)
An, H.J., Gip, P., Kim, .J, Wu, S., Park, K.W., McVaugh, C.T., et al.: Extensive determination of glycan heterogeneity reveals an unusual abundance of high mannose glycans in enriched plasma membranes of human embryonic stem cells. Mol Cell Proteomics. 11(4), M111.010660 (2012). https://doi.org/10.1074/mcp.M111.010660
Yu, R.K., Suzuki, Y., Yanagisawa, M.: Membrane Glycolipids in Stem Cells. FEBS Lett. 584, 1694–1699 (2010)
Li, Y.L., Wu, G.Z., Zeng, L., Dawe, G.S., Sun, L., Loers, G., et al.: Cell surface sialylation and fucosylation are regulated by the cell recognition molecule L1 via PLCgamma and cooperate to modulate embryonic stem cell survival and proliferation. FEBS Lett. 583(4), 703–710 (2009). https://doi.org/10.1016/j.febslet.2009.01.013
Doherty, P., Cohen, J., Walsh, F.S.: Neurite outgrowth in response to transfected N-CAM changes during development and is modulated by polysialic acid. Neuron 5(2), 209–219 (1990). https://doi.org/10.1016/0896-6273(90)90310-c
El Maarouf, A., Yaw, D.M., Rutishauser, U.: Improved stem cell-derived motoneuron survival, migration, sprouting, and innervation with enhanced expression of polysialic acid. Cell Transplant. 24(5), 797–809 (2015). https://doi.org/10.3727/096368914X679228
He, H., Nilsson, C.L., Emmett, M.R., Marshall, A.G., Kroes, R.A., Moskal, J.R., et al.: Glycomic and transcriptomic response of GSC11 glioblastoma stem cells to STAT3 phosphorylation inhibition and serum-induced differentiation. J Proteome Res. 9(5), 2098–2108 (2010). https://doi.org/10.1021/pr900793a
Itokazu, Y., Tsai, Y.T., Yu, R.K.: Epigenetic regulation of ganglioside expression in neural stem cells and neuronal cells. Glycoconj J. 34(6), 749–756 (2017). https://doi.org/10.1007/s10719-016-9719-6
Brawner, A.T., Xu, R., Liu, D., Jiang, P.: Generating CNS organoids from human induced pluripotent stem cells for modeling neurological disorders. Int J Physiol Pathophysiol Pharmacol. 9(3), 101–111 (2017)
Jo, J., Xiao, Y., Sun, A.X., Cukuroglu, E., Tran, H.D., Göke, J., et al.: Midbrain-like Organoids from Human Pluripotent Stem Cells Contain Functional Dopaminergic and Neuromelanin-Producing Neurons. Cell Stem Cell 19(2), 248–257 (2016). https://doi.org/10.1016/j.stem.2016.07.005
Kriks, S., Shim, J.W., Piao, J., Ganat, Y.M., Wakeman, D.R., Xie, Z., et al.: Dopamine neurons derived from human ES cells efficiently engraft in animal models of Parkinson’s disease. Nature 480(7378), 547–551 (2011). https://doi.org/10.1038/nature10648
Steinbeck, J.A., Studer, L.: Moving stem cells to the clinic: potential and limitations for brain repair. Neuron 86(1), 187–206 (2015). https://doi.org/10.1016/j.neuron.2015.03.002
Tagliafierro, L., Zamora, M.E., Chiba-Falek, O.: Multiplication of the SNCA locus exacerbates neuronal nuclear aging. Hum Mol Genet. 28(3), 407–421 (2019). https://doi.org/10.1093/hmg/ddy355
Acknowledgements
The work was supported by the Natural Sciences and Engineering Research Council of Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brockhausen, I., Schutzbach, J., Wang, J. et al. Glycoconjugate journal special issue on: the glycobiology of Parkinson’s disease. Glycoconj J 39, 55–74 (2022). https://doi.org/10.1007/s10719-021-10024-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10719-021-10024-w