Abstract
Recently, particulate matter pollution has been worsening, which has been affecting the asthma visits in children. In this study, we assessed the short-term effects of PM10 and PM2.5 on asthma visits in children in Shanghai, China from January 1, 2009 and December 31, 2010, using a generalized additive model. We controlled the confounding factors, such as long-term trends, week day effect, and weather elements. The lag effects of different age subgroups (≤ 2 yr, 3–5 yr, and 6–18 yr subgroups) were performed. The results showed significant effects of PM10 and PM2.5 on asthma visits in children, though the seasonal lags varied for the three age subgroups. In general, the effect of PM2.5 on asthma visits in children was stronger and more acute than that of PM10. PM2.5 showed the highest relative risk of 1.192 at lag 0 day in summer; and PM10 showed the highest relative risk of 1.073 at lag 3 day in autumn. Overall, particulate matter pollution showed a greater effect on relatively younger children. In particular, the ≤ 2 yr subgroup showed the highest seasonal relative risk of PM10. Especially, seasonal relative risk of PM10 in autumn for the ≤ 2 yr subgroup was much higher than that for the other two subgroups. The 3–5 yr and 6–18 yr subgroups showed the highest seasonal relative risk of PM2.5 in summer and winter, respectively. But the pediatric visits data we obtained cannot reflect the true prevalence of asthma and multiple visits. Thus, selection bias may exist in our analysis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Worldwide prevalence of asthma significantly increased from 8.4% (95% CI: 7.8–9.0) in 1996 to 10.9% (95% CI: 10.1–11.7) in 2016 (Maio et al., 2016). According to the National Pediatric Asthma Collaborative Group (2013), asthma is the most prevalent in East China (with a rate of 4.23%) and the least prevalent in Northeast China (with a rate of 2.00%). Generally, asthma is more prevalent in the southern region than in the northern region of China. Based on the city-level prevalence of asthma in children, the highest rate occurs in Shanghai (7.57%), and the lowest rate occurs in Lhasa (0.48%).
Studies have pointed out that particulate matter (PM) pollution is closely correlated with asthma (Liu et al., 2016; Polezer et al., 2018). Around the world, asthma has affected a total of 300 million people (Torgerson et al., 2011). PM pollution significantly affects the epidemic of asthma (Mazenq et al., 2017; Veremchuk et al., 2016). Meta-analysis showed the onset of asthmatic was positively correlated with exposure to PM2.5 and PM10 (Khreis et al., 2017). In Europe, the adverse effect of PM10 on asthma in children was statistically significant, with an odds ratio (OR) of 1.028 (95% CI: 1.006–1.051) (Weinmayr et al., 2010). In addition, excessive exposure to PM10 was found to be associated with increases in asthma-related hospitalization cases, with an odds ratio random effect (ORRE) of 1.017 (95% CI: 1.008–1.025) (Romeo et al., 2006). The risk of asthma in children between 8 and 12 years old was particularly high; the overall OR for time-weighted average exposure to PM10 was 2.0 (95% CI: 1.1–3.5). For non-allergic asthma in children between 8 and 12 years-old, the difference between the 5th and the 95th percentile of the OR for exposure to 7.2 µg/m PM10 was 3.8 (95% CI: 0.9–16.2) (Gruzieva et al., 2013). In Canada, the relative risk (RR) of asthma would increase by 2.24% (95% CI: 0.93%-5.38%) for per 10ug/m3 increase in PM2.5 (Requia et al., 2017). In Hong Kong, China, emergency room (ER) admission rate for asthma would increase by 3.24% (95% CI: 0.93–5.60%) with a 20.6 μg/m3 increase in PM2.5 (Lee et al., 2010). In Shanghai, China, the case of pediatric asthma (between 3 and 14 years-old) would increase by 0.78% (95% CI: 0.16–1.4%) for per 10 ug/m3 increase in PM2.5 (Mo et al., 2014). However, a comprehensive study on the effect of PM pollution on childhood asthma prevalence for different age groups on different timescales in Shanghai has not yet been reported.
In this study, we assumed that PM pollution had hysteresis effect on childhood asthma visits in Shanghai, China. The goal of this study is to quantify the annual and seasonal effects of PM10 and PM2.5 on pediatric asthma visits between 2009 and 2010 in Shanghai, China. We used a generalized additive model (GAM) with lag of 1–6 days to analyze the annual and seasonal effects of PM pollution on the incidence of pediatric asthma visits. Meanwhile, we also conducted a comparative analysis between the effects of PM10 and PM2.5. Our goal is to assist local health and human service authorities to prevent asthma visits in children by identifying links between hospital visits for asthma and pollution.
Data and methods
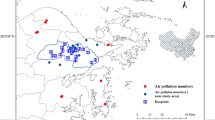
Study area
We chose one of the biggest cities in East China, Shanghai (121°48′E, 31°22′N), as the study area. Shanghai has a subtropical humid maritime monsoon climate, with an annual average air temperature of 17.4 °C, and an annual average relative humidity of 69.4%. Based on demographic statistics, Shanghai’s resident population was about 24.2 million in 2017.
Data
We obtained the concentrations of PM10 and PM2.5 between January 1, 2009 and December 31, 2010, from Shanghai Environmental Protection Bureau. We acquired daily weather data from Shanghai meteorological Bureau, including average air temperature (°C), wind speed (m/s), air pressure (hPa), and relative humidity (%).
We collected the pediatric visits data which summarized and classified into a general group and three subgroups by age (≤ 2 yr, 3–5 yr, and 6–18 yr subgroups) classified according to ICD-10 from the Shanghai Medical Insurance Affairs Management Center, which documents all asthma visits that involve social medical insurance, including date of the visit, age, and sex, as well as diagnosis code. These daily medical records covered all patients with social medical insurance. The law requires that every resident must purchase social medical insurance, whether it is primary or secondary medical insurance. We divided the pediatric visits data by season to study. Four seasons are defined as spring (March–May), summer (June–August), autumn (September–November), and winter (December to the next February). The basic information and summary of daily PM pollutants, meteorological elements, and pediatric visits are shown in Table 1.
Methods
We used the time series and correlation coefficient to determine whether there was a relationship between particulate matter and pediatric asthma visits (Fig. 1 and Table 2). If the correlation coefficient is greater than 0, it means that there is a positive correlation between the two variables in the study; otherwise, there is a negative correlation. The absolute value of the correlation coefficient closer to 1 represents the stronger the correlation between variables. The specific calculation formula (Eq. (1) is as follows:
We used a GAM [Eq. (2)] model based on time series analysis to evaluate the short-term effect of PM pollution on pediatric asthma visits in Shanghai, China. We presented the results in relative risk (RR) (with 95% CI) of hospital visits for asthma visits in children for each interquartile range (IQR) increase in PM concentrations. As the ratio of morbidity or mortality in the exposed and non-exposed groups, RR is an indicator of the extent to which the exposed research object is susceptible to a certain disease (asthma visits in this study).
where Yi is the number of children asthma visits on day i, E(Yi) is the expected children asthma visits on day i; α is the intercept; β is the coefficient of exposure response; Xi is the pollutant that produces a linear effect on day i; DOW (day of week) and holiday (all statutory holidays) control the confounding factors of week and holiday, respectively; s is a nonparametric smoothing function; df is degree of freedom; time is the calendar date variable with the range from 1 to 730, with a df of 3; T is daily average air temperature, with a df of 4; P is daily average air pressure, with a df of 3; H is daily relative humidity, with a df of 4; and W is daily average wind speed, with a df of 5.
In order to select df for all the involved variables, we set an empirical value (df = 3) for all non-time variables at first, and adjusted df for time according to the lowest Akaike information criterion (AIC) (i.e., when m is the smallest) (Akaike, 1975). Then, we adjusted each of the remaining variables until reaching the minimum of m (2.878 for PM2.5 and 2.845 for PM10 in this study).
Through the GAM model, the effects of smoothing functions of hospital visits for pediatric asthma visits were drawn (Fig. 2).
The effects of smoothing functions in the generalized additive model of hospital visits for pediatric asthma visits (for the entire study group as well as the three age subgroups) and concentrations of PM2.5 (lag 2 day) and PM10 (lag 3 day) from 2009 to 2010 in Shanghai, China. (logRR means the logarithm of RR value)
In the optimal model, we derived the exposure response coefficient to compute RR values (as well as the 95% CI) for per IQR increase in PM (35.63 μg/m3) using Eqs. (3) and (4).
where RR indicates the effect of per IQR change in PM concentrations on the number of children asthma visits. Greater than 1 RR means a positive effect, and less than 1 RR means a negative effect. In addition, we considered the lag effects in the analysis by using the concentrations of PM2.5 and PM10 on the current day (lag 0) and previous one to six days (lag 1–6 days) in the model. We chose the lag day with the highest RR on the number of hospital visits for pediatric asthma visits to build a core model.
In this study, evaluated the short-term effects of annual and seasonal effects of PM2.5 and PM10 on asthma visits. We used the mgcv package in R3.5.0 to adjust the GAM models. The statistical significance level of RR is at p < 0.05.
Results
Variation characteristics of PM concentrations and pediatric asthma visits
From 2009 to 2010, annual average concentrations of PM10 (76.7 µg/m3) were higher than that of PM2.5 (44.0 µg/m3) in Shanghai, China. Within the year, seasonal average concentrations of PM10 and PM2.5 were the highest in winter, with the values of 89.2 and 57.4 µg/m3, respectively, followed by spring and autumn, and the lowest in summer (Table S1).
The numbers of pediatric asthma hospital visits for all study group and three age subgroups of ≤ 2 yr, 3–5 yr, and 6–18 yr are 169, 79, 61, and 29, respectively. ≤ 2 yr subgroup has the highest prevalence, followed by 3–5 yr, and 6–18 yr. Within the year, except for ≤ 2 yr subgroup who have the highest prevalence in the winter (116), the visits of all study group, 3–5 yr, and 6–18 yr subgroups reach the peak in autumn, with the values of 221, 95 and 42, respectively (Table S2).
The average temperature in Shanghai is 17.4 °C, showing a trend of high in summer (27.7 °C) and low in winter (6.6 °C) within a year. The average relative humidity is 69.4%, showing a trend of high in summer (73.1%) and low in spring (66.6 °C) within a year. The average wind speed is 2.9 m/s, showing a trend of high in spring (3.2 m/s) and low in autumn (2.7 m/s) within a year. The average air pressure is 1015.5 hPa, showing a trend of high in winter (1023.1 hPa) and low in summer (1005.7 hPa) within a year. The changes of these meteorological elements are consistent with the characteristics of the subtropical monsoon climate in Shanghai.
For the entire study group, the number of hospital visits for pediatric asthma visits was positively correlated with annual concentrations of PM10 (particularly in autumn and winter) and PM2.5 (particularly in summer and autumn). Among the three subgroups, the ≤ 2 yr subgroup showed the highest positive correlation coefficients between the number of hospital visits for pediatric asthma visits and annual concentrations of PM10 and PM2.5 (Table 2).
For the entire study group, the number of hospital visits for pediatric asthma visits showed negative correlations with annual average wind speed, relative humidity, and air temperature, but positive correlation with annual average air pressure from 2009 to 2010 in Shanghai, China. Annual average wind speed affected the relatively older children more than the relatively younger children. Within the year, relative humidity in autumn and winter showed statistically significant correlations with the number of hospital visits for pediatric asthma visits for the entire study group. In autumn and winter, relative humidity mostly affected the 6–18 yr and ≤ 2 yr subgroups, respectively. Air pressure in autumn showed a statistically significant correlation with the number of hospital visits for pediatric asthma visits, especially in the ≤ 2 yr subgroup. The entire study group showed statistically significant correlations with average air temperature in spring, summer, and autumn. Among the three seasons, autumn average air temperature showed the closest correlation with the number of hospital visits for pediatric asthma visits, especially in the ≤ 2 yr subgroup (Table 2).
The effects of smoothing functions
The effects of smoothing functions in the generalized additive model showed that as the concentrations of PM10 and PM2.5 increased, RR of pediatric asthma visits for the entire study group increased first then stayed stable. PM2.5 showed a lower critical point than PM10, with a greater logRR value. In addition, when the concentrations of PM were below the critical points, the response curve for PM2.5 was steeper than that for PM10. These indicated that PM2.5 had a stronger short-term effect on the incidence of pediatric asthma visits than PM10 in the study area. The ≤ 2 yr subgroup showed similar response curves to PM2.5 and PM10 with the entire study group. For the 3–5 yr subgroup, as the concentrations of PM2.5 and PM10 increased, RR of the incidence of pediatric asthma visits increased first then decreased. PM2.5 showed a stronger short-term effect on the incidence of pediatric asthma visits than PM10 in the 3–5 yr subgroup, with a lower critical point and a steeper response curve. Nevertheless, only half of the response curve showed greater than 1 RR values, which indicated that PM2.5 and PM10 had relatively weak effects on the 3–5 yr subgroup. For the 6–18 yr subgroup, as the concentrations of PM2.5 increased, RR of the incidence of pediatric asthma visits increased first and then decreased. However, the response curve barely showed greater than 1 RR values, indicating that PM2.5 had a limited short-term effect on the 6–18 yr subgroup when it comes to the incidence of pediatric asthma visits. As the concentrations of PM10 increased, RR of the incidence of pediatric asthma visits in the 6–18 yr subgroup increased first, then decreased, and then back to increasing. The response curve showed a relatively long part with RR value greater than 1, indicating that PM10 had a stronger short-term effect than PM2.5 on the incidence of pediatric asthma visits in the 6–18 yr subgroup.
Relative risks of particulate matter on pediatric asthma visits
For the entire study group, the highest RR of pediatric asthma visits for PM10 (1.064) and PM2.5 (1.060) occurred at a lag of 4 day. Among the three subgroups, the highest RR occurred at a lag of 5 day for the ≤ 2 yr subgroup (1.073 for PM10 and 1.061 for PM2.5), a lag of 4 day for the 3–5 yr subgroup (1.065 for PM10 and 1.071 for PM2.5), and a lag of 2 day for the 6–18 yr subgroup (1.049 for PM10 and 1.052 for PM2.5). In general, PM10 affected the ≤ 2 yr subgroup the most, while PM2.5 affected the 3–5 yr subgroup the most (Table 3).
In spring, the highest RR of PM10 on pediatric asthma visits occurred at a lag of 2 day for the entire study group (1.022). Among the three subgroups, the highest RR of PM10 in spring occurred at a lag of 5 day for the ≤ 2 yr subgroup (1.067) and a lag of 1 day for the 3–5 yr (1.012) and 6–18 yr (0.988) subgroups. From lag 0 to 6 days, only the ≤ 2 yr subgroup showed a consistently greater than 1 average RR, indicating that PM10 had a relatively strong effect on pediatric asthma visits in spring for this subgroup. The highest RR of PM2.5 on pediatric asthma visits occurred at a lag of 0 for the entire study group (1.041) as well as the three different age subgroups (1.045 for ≤ 2 yr subgroup, 1.039 for 3–5 yr subgroup, and 1.025 for 6–18 yr subgroup). From lag 0 to 2 days, average RR for PM2.5 was greater than 1 for the entire study group as well as the three age subgroups. After lag 2 day, only the entire study group and the ≤ 2 yr subgroup showed average RR values that were above 1. Overall, PM2.5 affected spring incidence of pediatric asthma visits in the ≤ 2 yr subgroup more than the 3–5 yr and 6–18 yr subgroups. For the entire study group and the two 3–5 yr and 6–18 yr subgroups, PM2.5 showed a more instant effect on spring incidence of pediatric asthma visits, while PM10 showed a longer-lasting effect. As to the ≤ 2 yr subgroup, spring incidence of pediatric asthma visits was affected more by PM10 than by PM2.5 (Fig. 3a).
In summer, the highest RR of PM10 on pediatric asthma visits occurred at a lag of 4 day for the entire study group (1.034). Among the three subgroups, the highest RR of PM10 occurred at a lag of 4 day for both the ≤ 2 yr (1.029) and 3–5 yr (1.042) subgroups, and a lag of 6 day for the 6–18 yr subgroup (1.073). RR of PM10 on pediatric asthma visits in summer was less than 1 until lag 3 days, indicating a delayed effect on the study group. Meanwhile, the highest RR of PM2.5 on pediatric asthma visits occurred at lag 0 for the entire study group (1.192) as well as the ≤ 2 yr (1.216) and 3–5 yr (1.267) subgroups. As to the 6–18 yr subgroup, the highest RR of PM2.5 on pediatric asthma visits in summer occurred at a lag of 4 day (1.054). Overall, PM10 showed the strongest effect on pediatric asthma visits in summer for the 6–18 yr subgroup; while PM2.5 affected the 3–5 yr subgroup the most. The delayed effect of PM10 and PM2.5 on summer incidence of pediatric asthma visits was stronger for the relatively older children than the younger children (Fig. 3b).
In autumn, the highest RR of PM10 on pediatric asthma visits occurred at a lag of 2 day for the entire study group (1.069). Among the three subgroups, the highest RR of PM10 on seasonal incidence of pediatric asthma visits occurred at a lag of 3 day for the ≤ 2 yr subgroup (1.083), and a lag of 2 day for both the 3–5 yr (1.068) and 6–18 yr (1.063) subgroups. At the same time, the highest RR of PM2.5 occurred at a lag of 3 day for the entire study group (1.073) as well as the ≤ 2 yr subgroup (1.112), and a lag of 0 for the 3–5 yr (1.064) and 6–18 yr (1.081) subgroups. In general, PM10 and PM2.5 both showed the strongest effect on autumn incidence of pediatric asthma visits for the ≤ 2 yr subgroup. PM10 and PM2.5 showed a longer effect on the relatively younger children than on the relatively older children in autumn (Fig. 3c).
In winter, the highest RR of PM10 on pediatric asthma visits occurred at a lag of 4 day for the entire study group (1.052) as well as the 3–5 yr subgroup (1.048), a lag of 5 days for the ≤ 2 yr subgroup (1.074), and a lag of 3 days for the 6–18 yrs subgroup (1.035). Meanwhile, the highest RR of PM2.5 occurred at a lag of 4 days for the entire study group (1.087) as well as the 6–18 yrs subgroup (1.089), a lag of 0 for the ≤ 2 yr subgroup (1.089), and a lag of 5 days for the 3–5 yrs subgroup (1.132). Both PM10 and PM2.5 showed the strongest effect on winter incidence of pediatric asthma visits in the 3–5 yrs subgroup. Overall, PM2.5 showed a stronger effect on winter incidence of pediatric asthma visits for the study group than PM10 (Fig. 3d).
Comparison of the highest RR values
For the entire study group, the highest RR of PM2.5 (PM10) on pediatric asthma visits among lag 0–6 days was in the high-low order of summer, winter, autumn, and spring (autumn, winter, summer, and spring). In four seasons, the highest RR of PM2.5 was greater than that of PM10. This indicates that PM2.5 had a worse effect on the entire study group than PM10. For the ≤ 2 yr subgroup, the highest RR of PM2.5 (PM10) on pediatric asthma visits among lag 0–6 days was in the high-low order of summer, autumn, winter, and spring (autumn, spring, winter, and summer). In summer, autumn, and winter, the highest RR of PM2.5 was greater than that of PM10. For the 3–5 yr subgroup, the highest RR of PM2.5 (PM10) on pediatric asthma visits was in the high-low order of summer, winter, autumn, and spring (winter, autumn, summer, and spring). In spring, summer, and winter, the highest RR of PM2.5 was greater than that of PM10. For the 6–18 yr subgroup, the highest RR of PM2.5 (PM10) on seasonal incidence of pediatric asthma visits was in the high-low order of winter, autumn, summer, and spring (summer, autumn, winter, and spring). In spring, autumn, and winter, the highest RR of PM2.5 on seasonal incidence of pediatric asthma visits was greater than that of PM10 (Fig. 4).
Discussion
As an international metropolis, childhood asthma in Shanghai has become more and more serious in recent years, which has greatly aroused the attention of scholars from various countries (Hong et al., 2018). Zhang et al. (2013) pointed out Shanghai had the highest prevalence of all illnesses for rhinitis and atopic eczema. Therefore, the study of children's asthma in Shanghai is very necessary and urgent.
In this study, we found that the effect of PM2.5 on asthma visits in children was stronger and more acute than that of PM10. PM2.5 (PM10) showed a greater effect on relatively younger children displayed the highest RR of 1.192 (1.073) in summer (autumn). This article focused on the seasonal effects of PM10 and PM2.5 on childhood asthma visits, which had a valuable indicator for the prevention of childhood asthma visits.
Positive correlations were found between the incidence of pediatric asthma visits and the concentrations of PM10 and PM2.5 from 2009 to 2010 in Shanghai, China. This is consistent with David et al. (2000) and Kuo et al. (2018). However, another domestic study that was conducted in Shijiazhuang, Hebei suggested that there were no linear correlations between the hospitalization rate of pediatric respiratory diseases and the concentrations of PM10 and PM2.5 (Zhang et al., 2017). This may be related to the local pollutant content. Hebei is a heavily polluted city, and the daily variation of pollutants is not obvious, so the relationship between pollutants and asthma is not obvious. Our results showed that cool and dry weather is adverse for children due to the potentially high incidence of pediatric asthma visits (Stefaniak, 2007).
We found significant effects of PM10 and PM2.5 on pediatric asthma visits between 2009 and 2010 in the study area. For per IQR (10 µg/m3) increase in PM10 and PM2.5, RR of pediatric asthma visits for the entire study group would increase by 6.4% (1.80%) and 6.0% (1.60%), respectively. In Ji’nan, China, the incidence rate of pediatric asthma would increase by 0.65% and 0.54% for per 10 µg/m3 increase in PM10 and PM2.5 concentrations, respectively (Zhao et al., 2017). This result is much smaller than that in this article. But the increase percentage of PM10 in our study is smaller than that in a previous study performed in Athens, Greece, which showed a 4.3% increase in the number of hospitalization cases due to asthma with per 10 µg/m3 increase in PM10 concentrations, which is higher than the results in this study (Nastos et al., 2010). This difference may be related to PM pollution in various regions (Tzivian, 2011 and Nili et al., 2016), environmental factors (Liu, 2014), population movement (Zanhouo et al., 2019), and children's physique (Pianosi et al., 2004).
Our study confirmed the negative effects of PM10 and PM2.5 on pediatric asthma visits. In addition, we found that the youngest children (≤ 2 yr subgroup) accounted for the largest share of the incidence of pediatric asthma visits in Shanghai, China, which could be explained by the fact that infants/toddlers do not have fully developed defense systems in their lungs and are more susceptible to PM pollution (Qiao et al., 2016), which was also reported by Winter (2012), Chen, Feng, et al. (2016), and Guo (2018). Due to the physical and chemical characteristics of PM2.5 and PM10 in atmospheric pollutants, inhalation of PM could affect the respiratory system in human bodies by reducing the respiratory defense ability and increasing the inflammatory injury of the respiratory tract and lung (Wei, 2013). Children’s immune systems are not fully developed until they reach a certain height, weight, and age. When the immune system is not fully developed, pollutants are more likely to enter children's bodies, and young children are less able to resist the effects of pollutants on the respiratory system, so they are more likely to suffer from asthma and therefore need to visit health clinics. Children’s lung function indicators are negatively correlated with airborne particulate pollution, which implies that PM pollution in the air is one of the main causes for airway ventilatory dysfunction in children (Wei et al., 2001).
We found that PM10 and PM2.5 showed prominent lagging effects between 1 and 6 days in Shanghai, China. The greatest lag effects of both PM10 and PM2.5 were found at lag 4 day for the entire study group. The lag effect of PM pollution on pediatric asthma visits was more delayed in relatively young children than in relatively old children. This result is consistent with that from a similar study in Athens, Greece (Nastos et al., 2010). Other domestic studies showed that the lag effects of PM pollution on pediatric asthma occurred at lag 2 day in Taiwan (Chien et al., 2018) and lag 6 days in Shandong province (Zhao et al., 2017). In Hong Kong, China, for per 10 µg/m3 increase in the concentrations of PM10 and PM2.5, RR of hospitalization rate due to asthma would increase by 1.019 (within lag 0–4 days) and 1.021 (within lag 0–5 days), respectively (Ko et al., 2007). In general, the lagging effect of PM on pediatric asthma exists all over world, and it is concentrated before lag6 days. But there are differences between different regions, which related to the environment and the physique of children between different regions (Liu et al., 2014 and Pianosi et al., 2004). The lag effects could partially be explained by the inflammation of the alveolar in the region of the lung caused by the smaller particles in the pollutant mixture (Peters et al., 1997). Effective deposition of ultrafine particles can penetrate deeply into humans’ lungs, especially those of asthma patients (Anderson et al., 1990). For different individuals, the lag effects could be affected by their behavioral patterns. It usually takes several days for the deterioration to become severe enough to lead to clinical visits. This may explain the fact that the increase in asthma outpatient visits has been delayed (Chien et al., 2018).
In this study, ≤ 2-year old's were slower to respond to PM pollution. There may be two possible reasons. First, ≤ 2-year old's have poorer mobility compared to older children, resulting in shorter exposure to pollutants. Older children are often exposed to pollutants and are more directly affected by them, and the probability of asthma visits is higher. Children with asthma are more sensitive to the effects of air pollution than children with non-asthmatic or cough symptoms (Hoek et al., 1994, Pope et al., 1992 and Roemer et al., 1993). Long-term exposure to air pollutants leads to decreased lung function, or acute exposure to other triggers that may worsen the condition, resulting in increased susceptibility to other triggers (such as viral infection). Second, it is true that babies and preschoolers are more likely to cough and wheeze, but these symptoms do not reflect "real" asthma. Because the disease is not chronic, and as the child grows and develops, the symptoms eventually disappear. And the time to discover the illness and go to the hospital after the illness is also varies. But in China, medical insurance is generally reimbursed after treatment. Therefore, unless it is a diagnosis error in the hospital, there is basically no statistical error in Shanghai Medical Insurance Affairs Management Center. Young children were slower to respond to PM pollution. But the threat to them was huge. At least we want to alert parents that they should pay attention to the protection and prevention of young children in order to reduce the children asthma visits.
Seasonally, RR of PM pollution on pediatric asthma visits was the highest in summer. For the entire study group, RR of PM2.5 on annual incidence of pediatric asthma visits was lower than that of PM10; albeit PM2.5 showed higher RR on pediatric asthma visits than PM10 in all four seasons. Among the three subgroups, the ≤ 2 yr subgroup showed the highest RR of PM10, especially in autumn; the 3–5 yr and 6–18 yr subgroups showed the highest RR of PM2.5 in summer and winter, respectively.
In Taipei and Kaohsiung of Taiwan, the effect of PM10 on pediatric asthma was stronger in winter (with an OR of 1.204, 95% CI: 0.950–1.527) than that in summer (with an OR of 1.087, 95% CI: 0.630–1.874) (Kuo et al., 2018). In Adelaide, South Australia, the OR value of PM10 for childhood asthma inpatients was also higher in cold season (1.083, 95% CI: 1.025–1.144) than in warm season (1.011, 95% CI: 0.964–1.060) (Chen, Feng, et al., 2016; Chen, Glonek, et al., 2016). Several studies have indicated that more asthma emergency department ED visits were associated with air pollution during warm season (April–September) (Jalaludin et al., 2008; Strickland et al., 2010). Around the world, for per 10 µg/m3 increase in PM2.5 concentrations, RR of PM2.5 on the number of ER visits due to asthma was higher in warm seasons (3.7%, with 95% CI of 0.5%-6.9%) than in cool seasons (2.6%, with 95% CI of 0.7%-4.6%) (Fan et al., 2015). The same situation that RR in warm season (1.043, 95% CI: 1.016–1.070) higher than in cold season (1.005, 95% CI: 0.978–1.031) is in Atlanta (Matthew et al., 2010). Also in Wenshan District, Taipei, the impact of PM2.5 on the emergency room visit of COPD is concentrated on lag 3, 4, 5 days in summer (RR: 1.704, 95% CI: 1.104–2.632; RR: 1.716, 95% CI: 1.151–2.557; RR: 1.619, 95% CI: 1.111–2.360). But the effect in winter is not obvious (Chang, 2017).
Differences in seasonal effects of PM pollution on pediatric asthma might be explained by the relatively higher pollen (trees, grass, weeds, and so on) level in warm seasons, which is positively associated with the incidence of respiratory diseases (Carracedo et al., 2010). Wang et al. (2000) suggested two pollen peaks in spring–summer and autumn in Shanghai, China. Pollen level can induce bronchial obstruction that leads to increased risk of asthma exacerbation (Barnig & Casset, 2012; Gleason et al., 2014). Exposure to fine particles together with pollen will increase allergen sensitization and the risk of asthma (Barnig et al., 2012; Salvi., 2007). This is because airway mucosal damage and impaired mucociliary clearance caused by air pollution may enable allergens to penetrate immune system cells (DÁmato et al., 2010). Nevertheless, further studies are urged to clearly explain the differences in seasonal effects of PM pollution on pediatric asthma visits.
Generally, fine PM is more closely related to the increase in asthma prevalence and morbidity. However, when fine PM concentrations reached a certain point, increases in the concentrations of coarse PM would lead to higher incidence of asthma: for per 1 µg/m3 increase in the concentrations of coarse PM, RR would be 1.006 (95%CI: 1.001–1.011) for the prevalence of asthma, 1.023 (95%CI: 1.003–1.042) for the number of hospitalization cases due to asthma, and 1.017 (95%CI: 1.001–1.033) for the number of ER visits due to asthma (Keet et al., 2018). PM2.5 showed a stronger effect on the incidence of seizure than PM10. For per 10 µg/m3 increase in the concentrations of PM10 (PM2.5), the number of hospitalization cases for pediatric asthma would increase by 1.75% (3.45%) on average (Ding et al., 2015). The results of above references are consistent with this article.
Our study has found that PMs have significant effects on hospital visits for childhood asthma visits, but Wang et al. (2000) found that there is no obvious correlation between the incidence of asthma and PM10 concentration. This may be related to environmental and cultural differences among regions. We also found that the impact of PM2.5 on asthma is greater than that of PM10, which is similar to some research results all over the world. On the other hands, pollutants may affect asthma by causing other allergens (Villeneuve et al., 2007). And anthropogenic emissions cause approximately 37% and 73% of the total ozone and PM2.5 impact, respectively (Anenberg et al., 2018). These are the possible reasons why PM2.5 has a greater impact in the warm season than in the cold season. But in this article, we do not have the conditions to collect any data about allergens and man-made pollutants, which is also our future research direction. Zhang et al. (2013) also found that the prevalence of allergic diseases (wheezing, rhinitis, and atopic eczema) is not much different from the prevalence of asthma diagnosed by doctors, and the prevalence of the disease is higher under higher climatic conditions. Hu et al. (2019) found that the number of allergic diseases (including asthma) caused by meteorological elements is greater than that of pollutants. In this article, we smoothed the influence of meteorological elements to reduce the impact of meteorological elements as much as possible. In addition, this article focuses on the seasonal effects of PM10 and PM2.5 on childhood asthma (divided into spring, summer, autumn, and winter), which is difficult to be seen in other studies. This is a valuable indicator for the prevention of childhood asthma visits.
But, we only studied two kinds of particulate matters (PM2.5 and PM10), which is far from enough, because pollutants include not only particulate matters. Pan et al. (2010) found that in six cities (i.e., Anshan, Benxi, Dandong, Liaoyang, Panjin, and Shenyang) and three districts (slight, moderate, heavy) within each city of Northern China, for each interquartile range (IQR) increment of total suspended particulate, SO2 and NO2, the prevalence of persistent cough, persistent phlegm and current asthma increased by 21–28%, 21–30%, and 39–56%, respectively. Cai, (2014) found that when the average concentration of PM10, SO2, NO2, and black carbon in Shanghai increased within the quartile range, asthma hospitalization increased by 1.82%, 6.41%, 8.26%, and 6.62%, respectively. In the research of Hua et al. (2014), the influence of black carbon even exceeded PM2.5. In addition, indoor CO2 concentration also affected the prevalence of asthma, with a negative correlation in spring, summer and autumn, and a positive correlation in winter (Huang et al., 2016).
Inevitably, there are some limitations of the results in this study: (a) the air pollutant concentrations were averaged from different monitoring stations, yet the measurement bias was not eliminated due to its inherent nature (Chen et al., 2012); (b) hospital admissions for asthma were collected from the Shanghai Medical Insurance Affairs Management Center, thus, selection bias may exist in our analysis; (c) it is possible for the same patient to revisit hospitals during a short period of time; however, we did not ID the study group to exclude such hospital visit data in the analysis, which might reduce the accuracy of the results. We suggest further research should combine various pollutants to study their joint impacts on childhood asthma, and try to eliminate the collinearity among pollutants to explore which pollutants will have larger contribution to children asthma under specific environmental conditions.
Conclusions
We concluded that the number of pediatric asthma visits from 2009 to 2010 was significantly affected by particulate matter pollution in Shanghai, China. In general, the relatively younger children were more affected by particulate matter pollution than the relatively older children. Overall, the effect of PM2.5 on pediatric asthma visits was stronger than that of PM10.
References
Akaike, H. (1975). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19(6), 716–723.
Anderson, P. J., Wilson, J. D., & Hiller, F. C. (1990). Respiratory tract deposition of ultrafine particles in subjects with obstructive or restrictive lung disease. Chest, 97, 1115–1120.
Anenberg, S. C., Henze, D. K., Tinney, V., Kinney, P. L., Raich, W., Fann, N., Malley, C. S., Roman, H., Lamsal, L., Duncan, B., Martin, R. V., van Donkelaar, A., Brauer, M., Doherty, R., Jonson, J. E., Davila, Y., Sudo, K., & Kuylenstierna, J. C. I. (2018). Estimates of the global burden of ambient PM2.5, Ozone, and NO2 on asthma incidence and emergency room visits. Environmental Health Perspectives, 126(10), 107004.
Barnig, C., & Casset, A. (2012). Respiratory allergens and asthma exacerbation. Revue des Maladies Respiratoires, 29(6), 810–819.
Cai, J., Zhao, A., Zhao, J., Chen, R., Wang, W., Ha, S., Xu, X., & Kan, H. (2014). Acute effects of air pollution on asthma hospitalization in Shanghai, China. Environmental Pollution, 191, 139–144. https://doi.org/10.1016/j.envpol.2014.04.028
Carracedo, M. E., Sanchez, C., Taracido, M., Saez, M., Jato, V., & Figueiras, A. (2010). Effect of short-term exposure to air pollution and pollen on medical emergency calls: A case-crossover study in Spain. Allergy, 63(3), 347–353.
Chang, J. H., Hsu, S. C., Bai, K. J., Huang, S. K., & Hsu, C. W. (2017). Association of time-serial changes in ambient particulate matters (PMs) with respiratory emergency cases in Taipei’s Wenshan District. PLoS ONE, 12(7), e0181106.
Chen, B., Feng, S., & Yin, X. W. (2016). Clinical characteristics of different ages of children with acute exacerbation of bronchial asthma. Chinese Journal of Contemporary Pediatrics, 18(4), 320–323.
Chen, K., Glonek, G., Hansen, A., Williams, S., Tuke, J., Salter, A., & Bi, P. (2016). The effects of air pollution on asthma hospital admissions in Adelaide, South Australia, 2003–2013: Time-series and case–crossover analyses. Clinical and Experimental Allergy, 46(11), 1416–1430.
Chen, R., Somli, E., Wong, C. M., Huang, W., Wang, Z., Chen, B., & Kan, H. (2012). Associations between short-term exposure to nitrogen dioxide and mortality in 17 Chinese cities: The China air pollution and health effects study (CAPES). Environment International, 45, 32–38.
Chien, L. C., Chen, Y. A., & Yu, H. L. (2018). Lagged influence of fine particulate matter and geographic disparities on clinic visits for children’s asthma in Taiwan. International Journal of Environmental Research and Public Health, 15(4), 829.
D’Amato, G., Cecchi, L., D’Amato, M., & Liccardi, G. (2010). Urban air pollution and climate change as environmental risk factors of respiratory allergy: An update. Journal of Investigational Allergology and Clinical Immunology, 20(2), 95–102.
David, M. S., Robert, C. B., Marc, S. D., et al. (2000). Beyond administrative data: Characterizing cardiorespiratory disease episodes among patients visiting the emergency department. Canadian Journal of Public Health, 91(2), 107–112.
Ding, L., Zhu, D. J., & Peng, D. H. (2015). Meta-analysis of the relationship between particulate matter (PM10 and PM2.5) and asthma hospital admissions in children. Chinese Journal of Pediatrics, 53(2), 129–135.
Fan, J., Li, S., Fan, C., Bai, Z., & Yang, K. (2015). The impact of PM2.5 on asthma emergency department visits: A systematic review and meta-analysis. Environmental Science and Pollution Research, 23(1), 843–850.
Gleason, J. A., Bielory, L., & Fagliano, J. A. (2014). Associations between ozone, PM2.5, and four pollen types on emergency department pediatric asthma events during the warm season in new jersey: A case-crossover study. Environmental Research, 132, 421–429.
Gruzieva, O., Bergström, A., Hulchiy, O., et al. (2013). Exposure to air pollution from traffic and childhood asthma until 12 years of age. Epidemiology, 24(1), 54–61.
Guo, X. J., Li, Z. Y., Ling, W. J., Long, J., Su, C., Li, J., Liang, S., & Su, L. (2018). Epidemiology of childhood asthma in mainland China (1988–2014): A meta-analysis. Allergy and Asthma Proceedings, 39(3), 15–29.
Hoek, G., & Brunekreef, B. (1994). Effects of low-level winter air pollution concentrations on respiratory health of Dutch children. Environmental Research, 64(2), 136–150.
Hong, J. G., Bao, Y. X., Chen, A. H., et al. (2018). Chinese guidelines for childhood asthma 2016: Major updates, recommendations and key regional data. Journal of Asthma, 55(10), 1138–1146. https://doi.org/10.1080/02770903.2017.1396474
Hu, Y., Xu, Z., Jiang, F., et al. (2019). Relative impact of meteorological factors and air pollutants on childhood allergic diseases in Shanghai, China. Science of the Total Environment, 706, 135975.
Hua, J., Yin, Y., Peng, L., Du, L., Geng, F., & Zhu, L. (2014). Acute effects of black carbon and PM2.5 on children asthma admissions: A time-series study in a Chinese city. Science of the Total Environment, 481, 433–438. https://doi.org/10.1016/j.scitotenv.2014.02.070
Huang, C., Wang, X., Liu, W., et al. (2016). Household indoor air quality and its associations with childhood asthma in Shanghai, China: On-site inspected methods and preliminary results. Environmental Research. https://doi.org/10.1016/j.envres.2016.07.036
Jalaludin, B., Khalaj, B., Sheppeard, V., & Morgan, G. (2008). Air pollution and ED visits for asthma in Australian children: A case-crossover analysis. International Archives of Occupational and Environmental Health, 81(8), 967–974.
Keet, C. A., Keller, J. P., & Peng, R. D. (2018). Long-term coarse PM exposure is associated with asthma among children in medicaid. American Journal of Respiratory and Critical Care Medicine, 197(6), 737–746.
Khreis, H., Kelly, C., Tate, J., et al. (2017). Exposure to traffic-related air pollution and risk of development of childhood asthma: A systematic review and meta-analysis. Environment International, 100(2), 1–31.
Ko, F. W. S., Tam, W., Wong, T. W., et al. (2007). Effects of air pollution on asthma hospitalization rates in different age groups in Hong Kong. Clinical and Experimental Allergy, 37(9), 1312–1319.
Kuo, C. Y., Pan, R. H., Chan, C. K., et al. (2018). Application of a time-stratified case-crossover design to explore the effects of air pollution and season on childhood asthma hospitalization in cities of differing urban patterns: Big data analytics of government open data. International Journal of Environmental Research and Public Health, 15(4), 647.
Lee, S. L., Wong, W. H. S., & Lau, Y. L. (2010). Association between air pollution and asthma admission among children in Hong Kong. Clinical and Experimental Allergy Journal of the British Society for Allergy and Clinical Immunology, 36(9), 1138–1146.
Liu, C. J., Liu, C. Y., Mong, N., & Chou, C. (2016). Spatial correlation of satellite-derived PM2.5 with hospital admissions for respiratory diseases. Remote Sensing, 8(11), 914.
Liu, F. (2014). Asthma and asthma related symptoms in 23,326 Chinese children in relation to indoor and outdoor environmental factors: The Seven Northeastern Cities (SNEC) Study. Science of the Total Environment, 497–498(16), 10–17.
Maio, S., Baldacci, S., & Carrozzi, L. (2016). Respiratory symptoms/diseases prevalence is still increasing a 25-yr population study. Respiratory Medicine, 110, 58–65.
Matthew, J. S., Lyndsey, A. D., Mitchel, K., Flanders, W. D., Sarnat, J. A., Waller, L. A., Sarnat, S. E., Mulholland, J. A., & Tolbert, P. E. (2010). Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. American Journal of Respiratory and Critical Care Medicine, 182(3), 307–316.
Mazenq, J., Dubus, J. C., Gaudart, J., Charpin, D., Viudes, G., & Noel, G. (2017). City housing atmospheric pollutant impact on emergency visit for asthma: A classification and regression tree approach. Respiratory Medicine, 132, 1–8.
Mo, Z., Peng, L., Yang, D. D., Jiang, F., Yin, Y., Hua, J., & Geng, F. H. (2014). Impact of weather and pollution on the number of children with asthma in Shanghai. Chinese Health Statistics, 31(5), 827–829.
Nastos, P. T., Paliatsos, A. G., Anthracopoulos, M. B., Roma, E. S., & Priftis, K. N. (2010). Outdoor particulate matter and childhood asthma admissions in Athens, Greece: a time-series study. Environmental Health, 9(1), 45.
Nili, G., Rafae, S. C., Estela, D., Haim, B., Manor, S., Dorit, T., & Boris. A. P. (2016). Different effects of long-term exposures to SO2 and NO2 air pollutants on asthma severity in young adults. Journal of Toxicology and Environmental Health Part A, 79(8), 1–10.
Pan, G., Zhang, S., Feng, Y., Takahashi, K., Kagawa, J., Yu, L., Wang, P., Liu, M., Liu, Q., Hou, S., Pan, B., & Li, J. (2010). Air pollution and children’s respiratory symptoms in six cities of Northern China. Respiratory Medicine, 104(12), 1903–1911. https://doi.org/10.1016/j.rmed.2010.07.018.
Peters, A., Wichmann, H. E., Tuch, T., Heinrich, J., & Heyder, J. (1997). Respiratory effects are associated with the number of ultrafine particles. American Journal of Respiratory and Critical Care Medicine, 155, 1376–1383.
Pianosi, P. T., & Davis, H. S. (2004). Determinants of physical fitness in children with asthma. Pediatrics, 113(3), 225–229.
Polezer, G., Tadano, Y. S., Siqueira, H. V., Godoi, A., Yamamoto, C. I., De, P. A., Pauliquevis, T., de Fatima Andrade, M., Oliveira, A., Saldiva, P. H. N., Taylor, P. E., & Godoi, R. H. M. (2018). Assessing the impact of PM2.5 on respiratory disease using artificial neural networks. Environmental Pollution, 235, 394–403.
Pope, C. A., & Dockery, D. W. (1992). Acute health effects of PM10 pollution on symptomatic and asymptomatic children. The American Review of Respiratory Disease, 145(5), 1123–1128.
Qiao, S., He, P., Zhang, A. H., et al. (2016). Effect of chemical composition of fine particulate matter on children’s respiratory system health. World Latest Medicine Information, 16(54), 10–11.
Requia, W. J., Adams, M. D., & Koutrakis, P. (2017). Association of PM2.5 with diabetes, asthma, and high blood pressure incidence in Canada: A spatiotemporal analysis of the impacts of the energy generation and fuel sales. Science of the Total Environment, 98(2), 1077.
Roemer, W., Hoek, G., & Brunekreef, B. (1993). Effect of ambient winter air pollution on respiratory health of children with chronic respiratory symptoms. American Review of Respiratory Disease, 147(1), 118.
Romeo, E., Sario, M. D., Forastiere, F., Compagnucci, P., Stafoggia, M., Bergamaschi, A., & Perucci, C. A. (2006). PM10 exposure and asthma exacerbations in pediatric age: A meta-analysis of panel and time-series studies. Epidemiologia and Prevenzione, 30(30), 245-254791259-.
Salvi, S. (2007). Health effects of ambient air pollution in children. Paediatric Respiratory Reviews, 8(4), 275–280.
Stefaniak, J. (2007). Seasonal variation of hospital morbidity from asthma in Poland. Przegleąd Epidemiologiczny, 61(3), 567.
Strickland, M. J., Darrow, L. A., Klein, M., Flanders, W. D., Sarnat, J. A., Waller, L. A., Sarnat, S. E., Mulholland, J. A., & Tolbert, P. E. (2010). Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. American Journal of Respiratory and Critical Care Medicine, 182(3), 307.
The National Cooperative Group on Childhood Asthma Institute of Environmental Health and Related Prod. (2013). Third nationwide survey of childhood asthma in urban areas of China. Chinese Journal of Pediatrics, 51(10), 729–735.
Torgerson, D. G., Ampleford, E. J., Chiu, G. Y., Gauderman, W. J., Gignoux, C. R., Graves, P. E., Himes, B. E., Levin, A. M., Mathias, R. A., Hancock, D. B., & Baurley, J. W. (2011). Meta-analysis of genome-wide association studies of asthma in ethnically diverse north American populations. Nature Genetics, 43(9), 887–892.
Tzivian, L. (2011). Outdoor air pollution and asthma in children. Journal of Asthma Official Journal of the Association for the Care of Asthma, 48(5), 470–481.
Veremchuk, L. V., Yankova, V. I., Vitkina, T. I., Nazarenko, A. V., & Golokhvast, K. S. (2016). Urban air pollution, climate and its impact on asthma morbidity. Asian Pacific Journal of Tropical Biomedicine, 6(1), 76–79.
Villeneuve, P. J., Chen, L., Rowe, B. H., & Coates, F. (2007). Outdoor air pollution and emergency department visits for asthma among children and adults: A case-crossover study in northern Alberta, Canada. Environmental Health, 6, 40. https://doi.org/10.1186/1476-069X-6-40
Wang, B., Gao, P., Liu, J., Zhao, S. K., He, L. M., Zhang, Y. L., Xia, H. L., Mo, B. F., Cao, W., & Wang, L. Y. (2000). Airborne pollen in Southern–west area of Shanghai. Chinese Journal of Allergy and Clinical Immunology, 4(3), 168–175.
Wei, F. S., Hu, W., Wu, G. P., Teng, E. J., Jim, Z., & Chapman, R. S. (2001). Analysis of relation between air pollution and children’s lung function indexes. China Environmental Science, 21(5), 385–389.
Wei, N. (2013). Research progress in pertinence of atmospheric pollution features and common pediatric respiratory disease. Medical Recapitulate, 19(22), 4109–4111.
Weinmayr, G., Romeo, E., De, S. M., Weiland, S. K., & Forastiere, F. (2010). Short-term effects of PM10 and NO2 on respiratory health among children with asthma or asthma-like symptoms: a systematic review and meta-analysis. Environmental Health Perspectives, 118(4), 449–457.
Winer, R. A., Qin, X., Harrington, T., Moorman, J., & Zahran, H. (2012). Asthma incidence among children and adults: Findings from the behavioral risk factor surveillance system asthma call-back survey—United States, 2006–2008. Journal of Asthma, 49(1), 16–22.
Zanhouo, A. K., & Aymar, N. (2019). Modeling climate change impact on health and population migration: A systematic review. Economics Literature, 1(1), 51–65.
Zhang, L., Ma, L., An, H. B., Zhang, J. W., Liu, Z. Y., Ge, S. W., Liu, L., & Wang, L. Y. (2017). Studies about the correlation of air pollutants and hospitalization rate of children respiratory disease in Shijiazhuang city. International Journal of Respiration, 37(20), 1532–1534.
Zhang, Y., Li, B., Huang, C., Yang, X., Qian, H., Deng, Q., Zhao, Z., Li, A., Zhao, J., Zhang, X., & Qu, F. (2013). Ten cities cross-sectional questionnaire survey of children asthma and other allergies in China. Chinese Science Bulletin, 58, 4182–4189. https://doi.org/10.1007/s11434-013-5914-z
Zhao, M. J., Geng, X. Y., Cui, L. L., Zhou, J. W., & Zhang, J. (2017). Association between ambient PM10/PM2.5 concentration and outpatient department visits due to respiratory disease in a hospital in Jinan, 2013–2015: A time series analysis. Chinese Journal of Epidemiology, 38(3), 374–377.
Acknowledgements
We thank the Professional Services for Meteorology, Environment, and Public Health of the National Scientific Data Sharing Platform for Population and Health for providing research data. This research is supported by the National Natural Science Foundation of China (Grant Nos: 41975141 and 41961028).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yu, Z., Ma, Y., Zhang, Y. et al. A study on the short-term effect of particulate matter pollution on hospital visits for asthma in children in Shanghai, China. Environ Geochem Health 43, 4123–4138 (2021). https://doi.org/10.1007/s10653-021-00888-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10653-021-00888-0