Abstract
Objective
We aimed to determine the effects of ambient air pollutants on emergency department (ED) visits for asthma in children.
Methods
We obtained routinely collected ED visit data for asthma (ICD9 493) and air pollution (PM10, PM2.5, O3, NO2, CO and SO2) and meteorological data for metropolitan Sydney for 1997–2001. We used the time stratified case-crossover design and conditional logistic regression to model the association between air pollutants and ED visits for four age-groups (1–4, 5–9, 10–14 and 1–14 years). Estimated relative risks for asthma ED visits were calculated for an exposure corresponding to the inter-quartile range in pollutant level. We included same day average temperature, same day relative humidity, daily temperature range, school holidays and public holidays in all models.
Results
Associations between ambient air pollutants and ED visits for asthma in children were most consistent for all six air pollutants in the 1–4 years age-group, for particulates and CO in the 5–9 years age-group and for CO in the 10–14 years age-group. The greatest effects were most consistently observed for lag 0 and effects were greater in the warm months for particulates, O3 and NO2. In two pollutant models, effect sizes were generally smaller compared to those derived from single pollutant models.
Conclusion
We observed the effects of ambient air pollutants on ED attendances for asthma in a city where the ambient concentrations of air pollutants are relatively low.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute effects of ambient air pollution on mortality and hospital admissions have been well documented (Pope et al. 2002; Samet et al. 2000; Schwartz 1999; Spix et al. 1998). Fewer studies have investigated associations between ambient air pollutants and emergency department (ED) visits and many of these have reported the associations between air pollution and ED visits for asthma (Castellsague et al. 1995; Fauroux et al. 2000; Schwartz et al. 1993; Stieb et al. 1996; Tenias et al. 1998).
Australia has a high prevalence of asthma in children, which increased throughout the 1980s and 1990s (Peat et al. 1994; Robertson et al. 1991). Although, in Australia, the relationship between ambient air pollution and hospital admissions and mortality have been previously investigated (Barnett et al. 2005; Morgan et al. 1998a, b; Simpson et al. 2005a, b), there are few reported studies on the effects of ambient air pollution on ED visits (Jalaludin et al. 2005; Rennick and Jarman 1992).
As it can be difficult to model time series of respiratory disease in children, possibly due to the effects of respiratory disease epidemics and school holidays (Ponce de Leon et al. 1996), we aimed to determine the associations between ambient air pollutants [particulate matter < 2.5 μm in aerodynamic diameter (PM2.5) and particulate matter < 10 μm in aerodynamic diameter (PM10), nitrogen dioxide (NO2), ozone (O3), carbon monoxide (CO) and sulphur dioxide (SO2)] and ED visits for asthma in children using the case-crossover design.
Materials and methods
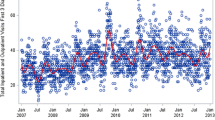
The study period was the 5-year period between 1 January 1997 and 31 December 2001. We used routinely collected data for both the exposures and outcomes. We constructed daily time series of hospital ED visits for asthma in children, air pollution and meteorological factors for the Sydney metropolitan region (population 3.8 million).
ED visit data
We obtained routinely collected ED visit data for metropolitan Sydney from the New South Wales (NSW) Health Department. We obtained daily numbers of ED visits for asthma (ICD9 493) for four age-groups 1–4, 5–9 and 10–14 years, and also for all children aged 1–14 years. We excluded children <12 months of age as the diagnosis of asthma in this age-group is unreliable in the ED setting.
Air pollution and meteorological data
We obtained air pollution and meteorological data from the NSW Department of Environment and Conservation and Bureau of Meteorology, respectively. Data from 14 air-monitoring stations were averaged to represent exposures for metropolitan Sydney. These 14 air-monitoring stations were located to measure background levels of ambient air pollution. Data from a coastal and an inland meteorology station were averaged to represent meteorological conditions.
We a priori constructed same day (L0), lagged 1–3 days (L1–L3, respectively) and average of lag 0 and lag 1 (L01) Sydney average pollutant concentrations for particulate matter (PM10, PM2.5; 24-h averages), NO2 (1-h average), O3 (1-h average), CO (8-h average) and SO2 (24-h average).
Statistical analysis
We used case-crossover design to determine the acute effects of daily ambient air pollution levels on ED visits for asthma. The case-crossover design is being increasingly used in epidemiological studies investigating acute effects of ambient air pollution (Jaakkola 2003; Lumley and Levy 2000) and obviates the need for adjusting for long and medium time varying covariates as well as for autocorrelation in the time series. As each case serves as his or her own referent, this design also has the ability to control for short-term time invariant potential confounders (such as smoking, age, sex and socio-economic status) by design rather than by statistical modelling.
Validity of estimators using this design is sensitive to referent selection strategy. To avoid bias, we used the time-stratified approach, which divides time into strata and uses the remainder of the days in each stratum as the referents for a case in that stratum (Levy et al. 2001; Lumley and Levy 2000). We used calendar months as the strata; for example, a case on Monday, 18 April would be compared with all other Mondays in April. In this approach, day of the week was also controlled by design rather than by modelling. We used conditional logistic regression to fit models to the data as it is a valid maximum likelihood and ensures unbiased estimates using the time-stratified approach in case-crossover designs (Janes et al. 2004).
Once we had established the basic model, we then examined the effects of individual air pollutants in single pollutant models. We examined the effects of lagging exposure for 0, 1, 2 and 3 days (L0, L1, L2 and lL3 days, respectively) as well as of a 2-day cumulative lag (L01). We also conducted separate analyses for warm and cool months (warm months: November–April, cool months: May–October). Finally, two pollutant models examined the independent effects of air pollutants. Lags with the absolute greatest single-day effect were included in these two pollutant models. We adjusted for the effects of same-day average temperature, same-day relative humidity, daily temperature range (maximum − minimum temperature), school holidays and public holidays in all models.
Results are presented as percentage change and associated 95% confidence intervals (95% CI) for an inter-quartile range (IQR) increase in concentration for the specific air pollutant.
Results
Summary statistics for daily ED attendances, air pollutants and meteorological variables are presented in Table 1. For children aged 1–14 years, there was a mean of 174 ED visits for asthma/day. Most asthma ED visits were for children aged 1–4 years (60.9%, mean visits/day = 109) (Table 1). Fifty-five percent of ED visits for asthma were in the cool season. The month of January (a summer month) had the lowest proportion of visits (6.1% of all visits) while August (a winter month) had the highest proportion of ED visits for asthma (10.2%).
Mean concentrations for all air pollutants were well below the national standards. Correlations among air pollutants and meteorological variables for both warm and cool periods are presented in Table 2. For the entire year, particulates were highly correlated with each other (r = 0.77–0.93), O3 was moderately correlated with particulates (r = 0.31–0.53) and NO2 was moderately correlated with all other air pollutants (r = 0.39–0.60) except with O3 (r = 0.22). There were weak–moderate correlations between SO2 and the other air pollutants (r = 0.52 with NO2, r = 0.44 with CO, r = 0.27–0.37 with particulates and r = 0.25 with O3).
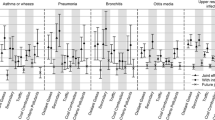
All percent changes and associated 95% CI are presented for an IQR increase in the respective air pollutant. In children aged 1–4 years, in single pollutant models, the largest effects were seen at L0 (except for O3, where the largest effect was seen at L1) (Table 3). All pollutants showed significant associations with ED visits for asthma with the greatest effect seen with NO2 (3.0% increase at L0). The magnitude of effects was similar for PM10 and PM2.5 (about 1.4% increase). Similar effects were seen in children aged 5–9 years although the NO2 effects were reduced. Again, the greatest effects for each of the air pollutants were seen at L0. There were only a few significant associations between air pollutants and ED visits for asthma in children aged 10–14 years (PM2.5 L0, and CO L0 and L01) and the effects were generally smaller (% change towards the null).
Table 4 presents the associations between air pollutants (for L0 only) and ED visits for asthma for the four age-groups in warm and cool months. In children aged 1–4 years, increased ED visits were observed in the warm months for PM10, O3 and NO2, and in the cool months for CO. In the 5–9-year age-group, associations were greater in the warm months for particulates, O3 and NO2, and in the cool months for SO2 and CO. For each of the air pollutants, except for CO, there were more significant associations in the warm months compared to the cool months.
Two pollutant models for the four age-groups are presented in Table 5 (reading left–right along the rows, for example, for children aged 1–4 years, the effects of PM10 are presented in the first row of data for a model with only PM10 in a single pollutant model as well the effects of PM10 in two pollutant models). For children aged 1–4 years, the particulate effect was reduced (% change towards the null) when O3, NO2 and CO were added to the model and for children aged 5–9 years, such an effect was seen only with O3 and CO, and in the 10–14-year age-group, this effect was seen only with CO. Particulates marginally reduced the effects of O3 in the two younger age-groups. The NO2 effect remained relatively constant in all two pollutant models for the 1–4 years age-group as was the CO effect in the two older age-groups. In the 1–4-year age-group, all associations, except for two, were statistically significant. In the 5–9-year age-group, significant associations were mainly seen with particulates, O3 and CO, whilst in the 10–14-year age-group, there were few significant associations (mainly with CO).
Discussion
We found significant associations between ED visits for asthma in children and ambient air pollutants in Sydney, Australia. Effects were most consistent for all the six air pollutants in the 1–4 years age-group, for particulates and CO in the 5–9 years age-group and for CO in the 10–14 years age group. The greatest effects were most consistently observed for L0 and effects were greater in the warm months for particulates, O3 and NO2. In two pollutant models (all-year models), the point estimates for particulates were attenuated when CO, NO2 and O3 were added to the single pollutant models.
We analysed our data by three different age-groups chosen a priori. The point estimates for the various air pollutants and for the various lags were similar for all three age-groups. There were no outstanding differences except for the SO2 effect, where the effects were uniformly <0 for the 10–14 years age-group. We have no ready explanation for this. There were more non-significant results for the two older age-groups and this is expected because of smaller daily number of visits in these two age-groups.
In Sydney, we found mainly positive associations (increased ED visits) between air pollutants and ED visits for asthma in all three age-groups. However, the literature is inconsistent. Norris et al. (1999) in Seattle, USA, in children under 18 years of age found effects for PM10 and CO but not for NO2, SO2 and O3, whereas Peel at al. (2005) in Atlanta, USA, in children aged 2–18 years, found increased effects for PM10, NO2 and CO, but the effect was significant only for CO. In a group of children aged 1–15 years, Fauroux et al. (2000) examined L0, L1 and L2 effects for O3, NO2, SO2 and black smoke and found significant effects only for L1 O3. Interestingly, all point estimates showed positive effects (except L2 SO2). Dales et al. (2000) and Stieb et al. (1996) examined the effects of O3 on asthma ED visits in children and neither of them demonstrated effects for O3. In a recent meta-analysis from Australia and New Zealand cities, Barnett et al. (2005) showed only NO2 effects on admissions for asthma, only in the 5–14 years age-group. There were no other effects of air pollution on asthma hospital admissions in this age-group nor of any of the other common pollutants in the 1–4 years age-group.
In the all-year analyses, the greatest absolute effects (generally adverse effects) in all three age-groups were seen for same day air pollutant concentrations (except for L1 for O3 for the 5–9 years age-group). The likelihood of presentation for asthma on the same day as ozone exposure may be lower than for other pollutants, as in Sydney, ozone concentrations tend to peak late in the day (NEPC 2005). Other studies have reported inconsistent results for lag periods. Fauroux et al. (2000) and Romieu et al. (1995) have reported O3 effects at L1, whereas Dales et al. (2000) reported O3 effects at L2 and Peel et al. (2005) reported stronger effects at even longer lag periods for asthma ED presentations in children (lag 5–8 days). The differences in lags could be due to the underlying variability in the population’s illness severity or to the time it takes for the exacerbation to progress to a stage where it is necessary to present to ED (Peel et al. 2005). In the 10–14 years age-group, greater effects were more likely with L2 or L3. However, in all three age-groups, the effect differences among the various lag concentrations were small. In a Sydney tertiary paediatric hospital, 54% of children with asthma presented within 2 days of the onset of asthma and 41% were classified as having moderate–severe asthma (Jalaludin et al. 1998). The effects at later lags observed for the older age-group could be explained by the fact that parents are more likely to self-medicate at home for a longer period in an older child compared to younger children.
In order to determine if air pollution effects were dependent on season, we also conducted our analyses in warm and cool months. In single pollutant L0 models, greater adverse effects were demonstrated for PM10, O3 and NO2 in the warm months and for CO and SO2 in the cool months for all children (1–14 years). The warm and cool month effects were more consistently observed across the two younger age-groups compared to the older age-group. In a study on seven cities in Australia and New Zealand, Barnett et al. (Barnett et al. 2005) found greater effects of PM2.5, PM10 and NO2 for respiratory hospital admissions and of O3 for asthma admissions in the warm months. In our study, PM10 and O3 levels were higher in the warm months, whereas NO2 level was higher in the cool months. The greater warm season effect demonstrated here might be due to children not only spending more time outdoors in the warmer months but also engaging in more vigorous physical activity and thereby increasing their minute ventilation and exposure to ambient air pollutants. More puzzling is the cool-month effects seen for CO and SO2, despite extremely low-ambient levels of these two air pollutants. These may reflect chance findings especially for SO2 where the warm and cool month SO2 levels were similar or residual confounding due to winter respiratory virus exacerbation of asthma. In Australia, laboratory notifications for rhinovirus infection peak in late winter and early spring while notifications for respiratory syncytial virus peak in winter (Roche et al. 2002), both in the cool months of our analysis period. Therefore, although the case-crossover design may have to some extent controlled for winter respiratory virus exacerbation of asthma, some residual confounding may be present.
For most pollutants, point estimates from two pollutant models were generally lower, compared to those derived from single pollutant models, and this pattern was observed across all the three age groups. In the 1–4 years age-group, the PM10 effect was reduced with the addition of O3 or NO2, suggesting that the particulate effect could not be completely separated from the effects of O3 and NO2, which appeared to have independent effects on ED visits for asthma. Multi-pollutant models are usually used to address the issue of confounding in single pollutant models by correlated air pollutants. In Sydney, motor vehicle exhaust emissions are the main source of air pollutants in the warm months with wood-smoke making a contribution to levels of air pollution in winter. In our study, air pollutants were generally only moderately correlated except between particulates and NO2 in the cool months where the correlation coefficients were about 0.7. However, interpretation of results may yet be complicated by modelled air pollutants acting as a proxy for some poorly or unmeasured air pollutant (Peel et al. 2005).
The strengths of this study include the long-time series and the use of a case-crossover design that minimises the effects of long-term seasonal and secular trends, and serial autocorrelation in the data. We adjusted for other potential confounders, for example, public and school holidays, and meteorology. However, there are also a number of limitations to our study. We used an administrative database in which about 95% of all ED attendances in Sydney are routinely recorded. This proportion remained constant throughout the study period and there were no changes to the data collection system. Although the recorded diagnosis was the diagnosis made at discharge from ED, there is the possibility that ED diagnoses may have been inaccurate. By excluding children aged <12 months from our analyses, we reduced the diagnosis error. Further, Stieb et al. (1998) reported an absence of ED diagnostic bias for asthma between low and high-pollution days. Therefore, any measurement error is expected to be non-differential. Although we measured the exposure at the aggregate level (using data from ambient air monitoring stations) rather than at the individual level, any measurement error is most likely be non-differential and produces conservative estimates of associations. It may have been possible to reduce exposure misclassification if we could have defined the exposure at the neighbourhood level. However, we did not have access to addresses of subjects and therefore could not model air pollution exposures at the neighbourhood level.
Our results have important population health implications as we observed associations between a number of air pollutants and ED attendances for asthma in a city where the ambient concentrations of air pollutants are relatively low. For example in the 5-year study period in Sydney, there were only 7 days where 24-h PM10 levels exceeded 50 μg/m3 and 17 days when 24-h PM2.5 exceeded 25 μg/m3. For PM10, six of the seven exceedences occurred during a severe bushfire episode. There were no exceedences for SO2, NO2 and CO, and there were only 6 days when the 1-h O3 exceeded 100 ppb.
The results from this study provide supporting evidence that the ambient air pollution has acute effects on asthma ED visits in children. It is important to note that morbidity due to ED visits comprises only one aspect of the overall impact of air pollution on human health. However, it should also be noted that there are many other important risk factors for asthma such as viral infections and allergens that may have a greater impact on asthma exacerbation than ambient air pollutants.
References
Barnett AG, Williams GM, Schwartz J, Neller AH, Best TL et al (2005) Air pollution and child respiratory health. A case-crossover study in Australia and New Zealand. Am J Respir Crit Care Med 171:1272–1278
Castellsague J, Sunyer J, Saez M, Anto JM (1995) Short-term association between air pollution and emergency room visits for asthma in Barcelona. Thorax 50:1051–1056
Dales RE, Cakmak S, Burnett RT, Judek S, Coates F, Brook JR (2000) Influence of ambient fungal spores on emergency visits for asthma to a regional children’s hospital. Am J Respir Crit Care Med 162:2087–2090
Fauroux B, Sampil M, Quenel P, Lemoullec Y (2000) Ozone: a trigger for hospital pediatric asthma emergency room visits. Pediatr Pulmonol 30:41–46
Jaakkola JJK (2003) Case-crossover design in air pollution epidemiology. Eur Respir J 21:81s–85s
Jalaludin B, Chey T, Holmwood M, Chipps J, Hanson R et al (1998) Admission rates as an indicator of the prevalence of severe asthma in the community. Aust NZ J Public Health 22:214–219
Jalaludin B, Morgan G, Lincoln D, Sheppeard V, Simpson R, Corbett S (2005) Associations between ambient air pollution and daily emergency department attendances for cardiovascular disease in the elderly (65+ years), Sydney, Australia. J Expo Anal Environ Epidemiol 16:225–237
Janes H, Sheppard L, Lumley T (2004) Assessing the health effects of air pollution using the case-crossover design. UW biostatistics working paper series. vol. 214
Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H (2001) Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology 12:186–192
Lumley T, Levy D (2000) Bias in the case-crossover design: implications for studies of air pollution. Environmetrics 11:689–704
Morgan G, Corbett S, Wlodarczyk J (1998a) Air pollution and hospital admissions in Sydney, Australia, 1990 to 1994. Am J Public Health 88:1761–1766
Morgan G, Corbett S, Wlodarczyk J, Lewis P (1998b) Air pollution and daily mortality in Sydney, Australia, 1989 through 1993. Am J Public Health 88:759–764
NEPC (2005) Preliminary work on ozone for the review of the ambient air quality NEPM. Issues paper. NEPC Service Corporation, Adelaide
Norris G, Young Pong SN, Koenig JQ, Larson TV, Sheppard L, Stout JW (1999) An association between fine particles and asthma emergency department visits for children in Seattle. Environ Health Perspectives 107:489–493
Peat JK, van den Berg RH, Green WF, Mellis CM, Leeder SR, Woolcock AJ (1994) Changing prevalence of asthma in Australian children (see comments). BMJ 308:1591–1596
Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD et al (2005) Ambient air pollution and respiratory emergency department visits. Epidemiology 16:164–174
Ponce de Leon A, Anderson HR, Bland JM, Strachan DP, Bower J (1996) Effects of air pollution on daily hospital admissions for respiratory disease in London between 1987–88 and 1991–92. J Epidemiol Community Health 50(Suppl 1):s63–s70
Pope CA III, Burnett RT, Thun MJ, Calle EE, Krewski D et al (2002) Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287:1132–1141
Rennick GJ, Jarman FC (1992) Are children with asthma affected by smog? Med J Aust 156:837–841
Robertson CF, Heycock E, Bishop J, Nolan T, Olinsky A, Phelan PD (1991) Prevalence of asthma in Melbourne schoolchildren: changes over 26 years [see comments]. BMJ 302:1116–1118
Roche P, Halliday L, O’Brien E, Spencer J (2002) The laboratory virology and serology reporting scheme, 1991 to 2000 communicable diseases intelligence 26:323–374
Romieu I, Meneses F, Sienra-Monge JJ, Huerta J, Ruiz VS et al (1995) Effects of urban air pollutants on emergency visits for childhood asthma in Mexico City. Am J Epidemiol 141:546–553
Samet JM, Dominici F, Curriero FC, Coursac I, Zeger SL (2000) Fine particulate air pollution and mortality in 20 US cities, 1987–1994 [see comments]. N Eng J Med 343:1742–1749
Schwartz J (1999) Air pollution and hospital admissions for heart disease in eight US counties [see comments]. Epidemiology 10:17–22
Schwartz J, Slater D, Larson TV, Pierson WE, Koenig JQ (1993) Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am Rev Respir Dis 147:826–831
Simpson R, Williams G, Petroeschevsky A, Best T, Morgan G et al (2005a) The short-term effects of air pollution on daily mortality in four Australian cities. Aust NZ J Public Health 29:205–212
Simpson R, Williams G, Petroeschevsky A, Best T, Morgan G et al (2005b) The short-term effects of air pollution on hospital admissions in four Australian cities Australian and New Zealand. J Public Health 29:213–221
Spix C, Anderson HR, Schwartz J, Vigotti MA, LeTertre A et al (1998) Short-term effects of air pollution on hospital admissions of respiratory diseases in Europe: a quantitative summary of APHEA study results. Air pollution and health: a European approach. Arch Environ Health 53:54–64
Stieb DM, Burnett RT, Beveridge RC, Brook JR (1996) Association between ozone and asthma emergency department visits in Saint John, New Brunswick, Canada. Environ Health Perspectives 104:1354–1360
Stieb DM, Beveridge RC, Rowe BH, Walter SD, Judek S (1998) Assessing diagnostic classification in an emergency department: implications for daily time series studies of air pollution. Am J Epidemiol 148:666–670
Tenias JM, Ballester F, Rivera ML (1998) Association between hospital emergency visits for asthma and air pollution in Valencia, Spain. Occup Environ Med 55:541–7
Acknowledgments
We acknowledge the Australian Bureau of Meteorology for the meteorological data, and the NSW Department of Environment and Conservation for the air pollution data. We received funding from the Health Research Foundation Sydney South West, Sydney South West Area Health Service, and from the Environmental Health Branch, NSW Health Department. The use of de-identified, routinely collected data in this study did not require approval from an institutional human research ethics committee.
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jalaludin, B., Khalaj, B., Sheppeard, V. et al. Air pollution and ED visits for asthma in Australian children: a case-crossover analysis. Int Arch Occup Environ Health 81, 967–974 (2008). https://doi.org/10.1007/s00420-007-0290-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-007-0290-0