Summary
Neuroblastoma, a paediatric malignancy of the sympathetic nervous system, accounts for 15 % of childhood cancer deaths. Despite advances in understanding the biology, it remains one of the most difficult paediatric cancers to treat partly due to the development of multidrug resistance. There is thus a compelling demand for new treatment strategies that can bypass resistance mechanisms. The pyrrolo-1,5-benzoxazepine (PBOX) compounds are a series of novel microtubule-targeting agents that potently induce apoptosis in various tumour models. We have previously reported that PBOX compounds induce apoptosis in drug sensitive and multidrug resistant neuroblastoma cells and synergistically enhance apoptosis induced by chemotherapeutics such as carboplatin. In this study we present further data concerning the molecular basis of PBOX-induced apoptosis in neuroblastoma. We demonstrate that PBOX-6 induced AMP-activated protein kinase (AMPK) activation and downstream acetyl-CoA carboxylase phosphorylation. Increased reactive oxygen species (ROS) appeared to serve as the upstream signal for AMPK activation as pretreatment of cells with the antioxidant N-acetylcysteine inhibited both AMPK activation and PBOX-induced apoptosis. Furthermore, activation of AMPK by PBOX-6 was found to inhibit mTOR complex 1 (mTORC1) signalling. Finally, we demonstrate the efficacy of PBOX-6 in an in vivo xenograft model of neuroblastoma. This study provides new insights into understanding the molecular and cellular mechanisms involved in PBOX-induced cell death in neuroblastoma and further supports their future use as novel anti-cancer agents for the treatment of neuroblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma, a malignancy of neuroectodermal origin, accounts for 15 % of childhood cancer deaths [1]. Despite both advances in understanding the biology of the cancer, and aggressive treatment strategies, it is one of the most difficult paediatric cancers to treat successfully. At diagnosis, more than 60 % of patients present with adverse features, while less than 40 % of these achieve disease free long term survival [2]. A major obstacle in the effective treatment of neuroblastoma is the development of multidrug resistance (MDR) to a broad range of cytotoxic drugs, including vinca alkaloids, alkylating agents, platinum compounds and anthracyclines [3], indicating that there is a compelling demand for new treatment strategies for this cancer.
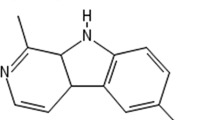
The pyrrolo-1,5-benzoxazepine (PBOX) compounds are a series of novel microtubule-targeting agents which possess the ability to potently induce cell cycle arrest and apoptosis in a number of cancer cell lines, derived from both solid tumours and haematological malignancies [4–10]. We previously demonstrated that one member of this family of compounds, PBOX-15, induces apoptosis both in ex vivo B-cell lymphocytic leukaemia cells harbouring poor prognostic indicators and fludarabine resistance-associated p53 deletions [11], and in primary CML patient samples including those resistant to Imatinib, the current frontline treatment for CML [12]. Additionally, these novel microtubule targeting agents have been shown to induce apoptosis in a numerous in vivo murine cancer models including chronic myeloid leukaemia (CML) [12] and breast cancer [5]. Unlike many chemotherapeutic agents currently used to treat cancers including neuroblastoma, the PBOX compounds are not substrates for many MDR drug efflux pumps [7,8] indicating that they may possess advantages over standard chemotherapy which is currently in clinical use.
We have recently reported that two representative PBOX compounds, PBOX-6 and −15, reduce the viability of a panel of drug sensitive and MDR neuroblastoma cell lines with similar potency [13]. Importantly, we showed that the PBOX compounds synergise with standard chemotherapy, such as carboplatin, in both drug sensitive and MDR cells. PBOX-induced apoptosis in neuroblastoma cells was mediated by a decrease and inactivation of anti-apoptotic Bcl-2 family members Mcl-1 and Bcl-2, an increase in pro-apoptotic Bak and activation of caspases-3, −8 and −9. Furthermore gene silencing of Mcl-1 was shown to sensitise both drug sensitive and multidrug resistant cells to carboplatin induced apoptosis, demonstrating the importance of Mcl-1 downregulation in the apoptotic pathway mediated by the PBOXs in neuroblastoma. In this article, we extend our study of the PBOX compounds in neuroblastoma cells and sought to identify the molecular events associated with PBOX-induced Mcl-1 downregulation.
It has recently been reported in several human cancer cell lines, that a decrease in Mcl-1 expression may be mediated by activation of 5’ adenosine monophosphate-activated protein kinase (AMPK) [14]. AMPK is a sensor of cellular homeostasis which is activated in response to a falling level of cellular ATP, to maintain energy balance within the cell. AMPK is phosphorylated when the ratio of AMP:ATP decreases, leading to inhibition of ATP consuming pathways and activation of ATP producing pathways. Interestingly, recent reports have demonstrated that AMPK is involved in induction of apoptosis by a variety of chemotherapeutics [15–17]. Furthermore, a recent study demonstrated that activation of AMPK is involved in apoptosis induced by the microtubule targeting agents, vincristine and taxol, in B16 melanoma cells [15].
Studies have suggested anti-cancer agents which activate AMPK may mediate their apoptotic effects through the production of oxidative stress, such as the generation of ROS [18, 19], leading us to postulate that the PBOXs may induce production of ROS in neuroblastoma cells, which in turn results in activation of AMPK. Therefore in this study, we investigated the role of ROS production and AMPK activation in PBOX-6 mediated apoptosis. Production of reactive oxygen species (ROS) may be inhibited by the antioxidant N-acetylcysteine (NAC). NAC, a precursor of glutathione, is a scavenger of free radicals and has been extensively used as a means to investigate the role of ROS production in various cellular pathways such as apoptosis, in addition to its role in various pathologies including cancer, inflammation, arthritis and cardiovascular disease [20]. There have been reports that pretreatment with NAC can impair or inhibit the apoptosis inducing ability of anti-cancer agents. Consequently in this study, we utilised NAC to determine any cytoprotective effects upon PBOX-6 treatment.
AMPK phosphorylation triggers a phosphorylation cascade that regulates the activity of various downstream targets such as the mammalian target of rapamycin (mTOR) signalling pathway. Indeed AMPK activation has previously been shown to lead to inhibition of the mTOR signalling pathway, resulting in a block in Mcl-1 translation [14]. mTOR is a highly conserved serine/threonine kinase which regulates a broad range of cellular events including transcription, translation, proliferation and division, therefore control of this pathway is of the upmost importance for maintaining normal cell division. Many studies point to mTOR playing a critical role in the progression of many cancers, including prostate [21], breast [22], haematological malignancies [23] and hepatocellular carcinoma [24]. Oncogenic activation of this pathway induces several processes necessary for tumour growth and proliferation. Indeed, it is interesting to note that proteins in this signalling pathway have been shown to be constitutively activated in neuroblastoma cell lines and patient samples [25]. Inhibition of mTOR by rapamycin and other rapalogues have been shown to effectively induce cell death in neuroblastoma cells, indicating that inhibitors of this pathway may represent a promising new approach for the treatment of neuroblastoma. In this present study, the effects of PBOX-6 on the mTOR signalling pathway, namely mTOR and its downstream targets p70 S6 kinase, S6 ribosomal protein and eEF2K was undertaken.
In this study, we demonstrate for the first time, PBOX-6 induced AMPK activation and downstream ACC phosphorylation in neuroblastoma cells. ROS production appears to be involved in AMPK activation by PBOX-6. Furthermore, evidence is provided to support the suggestion that activation of AMPK plays a role in mediating apoptosis in PBOX-6 treated neuroblastoma cells, through inhibition of the mTOR pathway.
Materials and methods
Cell culture
SHSY5Y were purchased from the European Collection of Cell Cultures (ECACC). SHSY5Y cells were cultured in DMEM/F12 + GlutaMAX medium supplemented with 10 % (v/v) foetal bovine serum (FBS) and 1 % (v/v) penicillin/streptomycin. Cells were incubated in a humidified environment at 95 % O2 and 5 % CO2 and passaged twice a week depending on levels of confluency. Medium was decanted and the flask was washed in 2–3 mls sterile phosphate buffered saline (PBS). PBS was discarded and cells were trypsinised in 1 ml of trypLE Express at 37 °C for 3 min. Cells were rinsed in 9 mls of medium, transferred to a 30 ml universal tube and centrifuged at 300×g for 5 min in a Sorvall Legend T centrifuge. The supernatant was discarded, the pellet was resusupended in 10 mls medium and the cells were counted using a haemocytometer.
Reagents
The pyrrolo-1,5-benzoxazepine compound, 7-[(N,N-dimethylcarbamoyl)oxy]-6-(naphth-1-yl)pyrrolo[2,1-d][1,5]benzoxazepine (PBOX-6) and was synthesised as described previously [26] and dissolved in ethanol. Anti-AMPK, phospho-AMPK, ACC, phospho-ACC, mTOR, phospho-mTOR, p70 S6 kinase, S6 ribosomal protein, phospho-eEF2k antibodies were purchased from Cell Signalling Technologies. GAPDH antibody was obtained from Millipore. All media and FBS were obtained from Invitrogen. The enhanced chemiluminescence reagents were supplied by Amersham Biosciences. The BCA reagents were from Pierce, the polyvinylidene difluoride membranes from Millipore, while the protease inhibitors were obtained from Roche. Unless otherwise stated, all chemicals were obtained from Sigma-Aldrich. Cell culture materials were sourced from Greiner Bio-One GmbH.
Flow cytometry
Cell cycle analysis
Following the required treatment, floating and adherent cells were harvested and fixed in 70 % ethanol/PBS. Fixed samples were stored at −20 °C until required. Ethanol was removed by centrifugation and pellets were incubated in 400 μl FACS flow sheath fluid supplemented with 10 μg/ml RNase A (Sigma Aldrich, St Louis, MO, USA) and 100 μg/ml propidium iodide (Sigma Aldrich, St Louis, MO, USA). Cells were incubated in the dark at 37 °C for 30 min. Analysis was performed on a FACScalibur Fluorescence Associated Cell Sorter (FACS) (Becton–Dickinson, San Jose, CA, USA) using Cell Quest and Quanti-Quest software. Samples were first gated using a vehicle control to eliminate debris and cell aggregates from analysis. 10,000 cells from each sample were counted and results were visualised on histograms.
Measurement of ROS production
ROS production was determined using the ROS-Glo H202 assay, a luminescent assay that measures the level of the reactive oxygen species, hydrogen peroxide (H202). A H202 substrate is employed that reacts directly with H202 to generate a luciferin precursor. Upon addition of the detection reagent which contains Ultra-Glo recombinant luciferase and D-Cysteine, the precursor is converted to luciferin by the D-Cysteine, and the luciferin reacts with Ultra-Glo recombinant luciferase to generate a luminescent signal which is proportional to the concentration of H202. Cells were seeded at a density of 6.0 × 104 cells/ml in 80 μl of medium in a 96-well plate and allowed to adhere overnight. The substrate dilution buffer was thawed and placed on ice. H202 was added to the substrate dilution buffer as described in Table 2.1 and 20 μl of H202 substrate solution was added to the cells in addition to the required test compound. The 96 well plate was placed in the incubator for the desired time. After such time, 100 μl of the ROS-Glo detection reagent was added to each well. The plate was left to incubate for 20 min at room temp after which time luminescence was read on the spectraMAX Gemini plate reader.
Western blot
Cells were harvested in AMPK lysis buffer (50 mM Tris/HCl, pH 7.4 at 4 °C, 50 mM NaF, 5 mM sodium pyrophosphate, 1 mM EDTA, 1 mM EGTA, 250 mM mannitol, 1 % (v/v), Triton X-100, 1 mM DTT and the protease inhibitors) or mTOR lysis buffer (10 mM Tris pH7.5, 50 mM NaCl, 30 mM sodium pyrophosphate, 50 mM sodium fluoride, 5 μM zinc chloride, 10 % glycerol, 0.5 % triton-X-100, 1 μM DTT and protease inhibitors). DTT (to a final concentration of 50 mM) and bromophenol blue were added to each sample followed by boiling for 3 min at 1000C. Equal quantities of protein (as determined by a BCA assay) were separated on polyacrylamide gels followed by transfer to PVDF membranes. Membranes were blocked in 5 % marvel in PBS-tween for 1 h. Membranes were incubated in the relevant primary antibodies overnight, washed and incubated in horseradish peroxidase conjugated secondary antibody for 1 h and washed again. Enhanced chemiluminescence was used for detection of protein expression. Western blot analysis was performed using antibodies directed against AMPK, phospho-AMK, ACC, phospho-ACC, mTOR, phospho-mTOR, p70 S6 Kinase, S6 ribosomal protein, phospho-eEF2K. Western blots were normalised to the relevant controls (e.g. phospho-mTOR was normalised to mTOR) and densitometric analysis of bands was carried out using imageJ software.
In vivo tumour model of neuroblastoma
Mice
Specific pathogen-free 4- to 6-week-old adult female BALB/c-nu/nu mice were purchased from Harlan Laboratories (Cambridgeshire, UK). Mice were housed in sterile individually ventilated cages; food and water were provided ad libitum, in accordance with the standard operating procedures set down in the EC Directive 86/609. Mice were acclimatised for 1 week before the initiation of any in vivo experiments. Animals were killed by CO2 followed by cervical dislocation if the tumour exceeded 15 mm in diameter or the volume exceeded 10 % of mouse bodyweight or if found to be in distress (hunching, failure to groom etc.). Ethical approval was obtained by the BioResources Committee, Trinity College, Dublin and the Irish Medicines Board.
In vivo tumour study
The in vivo antitumour efficacy of PBOX-6, carboplatin and a combination of the two was examined using an SHSY5Y xenograft in a BALB/c mouse model. Female BALB/c-nu/nu mice were inoculated subcutaneously (s.c.) into the right flank with 2 × 106 SHSY5Y cells in the log phase of growth. After 35 days, when tumours of approximately 3 mm in diameter were observed, mice were randomly divided into two groups (5 mice per group). A stock solution of PBOX-6 was prepared at a concentration of 15 mg ml−1 in 1: 1 ethanol/cremophor EL. When required, this was then diluted 1 in 5 in sterile PBS to give a final concentration of 7.5 mg kg−1 or 0.15 mg per mouse. The PBOX-6 treatment group (n = 5) received an intratumoural (i.t.) injection [27, 28] of PBOX-6 once every 2 days for the duration of the experiment starting on day 35. Control mice (n = 5) received an i.t injection of 50 μl of the vehicle also starting on day 35. Tumour growth was measured every second day with a sterile vernier calliper. The long (L) and short (S) axes were recorded, and tumour volume (V) was calculated using the following equation as described previously [29].
Mice were weighed every 2 days. Mice were killed by CO2 asphyxiation followed by cervical dislocation at the experimental end point or if found to be under any duress.
Statistics
The statistical analysis of experimental data was performed using the computer program Prism GraphPad 4. Results were presented as mean ± S.E.M. For comparison of two groups, values were determined using a Student’s paired t test. For comparison of more than two groups, one way Anova followed by Tukey’s multiple comparison test was employed. A value of P < 0.05 was deemed to be significant.
Results
PBOX-6 activates AMPK in SHSY5Y cells
Numerous studies have demonstrated that AMPK plays a vital role in apoptosis induction in multiple cancers [30, 31]. Furthermore, previous studies have indicated that MTAs such as vincristine, which induce apoptosis mediated by the production of ROS, also activate AMPK [15]. We hypothesised that PBOX-6 may induce the production of ROS in neuroblastoma cells which in turn activates AMPK. To test this hypothesis, SHSY5Y cells were treated with PBOX-6 and the activation of AMPK and phosphorylation of the downstream protein acetyl-CoA carboxylase (ACC) was monitored. To assess activation of AMPK, a phospho-specific antibody was utilised. When activated, AMPK is phosphorylated on Thr172 by an upstream MAPK kinase, LKB1. Activation of AMPK up to 6 h post treatment with PBOX-6 was monitored and was shown to increase in a time dependent manner (Fig. 1a). A total AMPK antibody to confirm equal protein loading was utilised. Upon observing activation of AMPK, the effect of PBOX-6 on the downstream target of AMPK, ACC was examined. ACC catalyses the carboxylation of acetyl CoA to malonyl CoA. Malonyl CoA is a key substrate for the synthesis of fatty acids, an anabolic process which consumes ATP. When AMPK is activated by phosphorylation it can phosphorylate ACC causing it to be inactivated, thus switching off an ATP consuming pathway [32]. Following treatment of cells with PBOX-6, a time dependent phosphorylation of ACC in SHSY5Y cells (Fig. 1a) was observed. This correlated with the phosphorylation and activation of AMPK. No change in expression of total ACC was observed demonstrating equal protein loading. Densitometric analysis of the bands followed by statistical analysis demonstrated a significant increase in phosphorylated AMPK and phosphorylated ACC within 2 h of PBOX-6 treatment (Fig. 1b and c).
PBOX-6 activates AMPK and inactivates ACC in SHSY5Y cells in a time dependent manner. SHSY5Y cells were seeded at a density of 3.0 × 105 cells in T25cm2 flasks and left to adhere overnight. The following day, cells were treated with 2.5 μM PBOX-6 for up to 6 h. After the required incubation time, cells were harvested and lysates were prepared for western blot analysis. 30 μg of protein was separated on a 6 % or 10 % resolving gel with 5 % stacking gel, transferred to a PVDF membrane and probed with an anti-phospho-AMPK or anti-phospho-ACC antibody a Membranes were also probed for AMPK or ACC as a loading control. Results are representative of three separate experiments. b Western blots were normalised to total AMPK or ACC as a control and densitometric analysis of bands was carried out with the imageJ software. Statistical analysis was performed using one way ANOVA with Tukey’s multiple comparison test. *** p < 0.001, *p < 0.05
PBOX-6 induces production of reactive oxygen species
Having observed activation of AMPK and inactivation of ACC in response to PBOX-6, examination of both the upstream and downstream events associated with AMPK activation in SHSY5Y cells was undertaken. Previous reports indicated that activation of the upstream kinase, LKB1, mediated the activation of AMPK in response to vincristine while knockdown of LKB1 by siRNA largely inhibited vincristine induced activation of AMPK [15]. Furthermore, LKB1 activation was shown to be dependent on the production of ROS. Therefore an investigation into the production of ROS by PBOX-6 using the ROS-Glo assay (Promega) was undertaken. Menadione was employed as a positive control for the production of ROS. A 15 min treatment with 50 μM menadione was found to induce ROS production when compared to control cells (Fig. 2a). Treatment with 2.5 μM PBOX-6 for up to 6 h was shown to induce ROS production in SHSY5Y cells (Fig. 2a).
PBOX-6 induces production of reactive oxygen species. ROS was detected using the ROS-Glo H202 assay. SHSY5Y cells were seeded in the log phase of growth at 2.5 × 104 cells/well and left to adhere overnight. The following day, the H202 substrate solution was added each will prior to treatment with 2.5 μM PBOX-6 for up to 6 h. Cells were also pretreated with NAC for 1 h and treated with 2.5 μM PBOX-6 for 1 h. After the required incubation time, the ROS-Glo detection reagent was added to the cells and the plate was incubated for 20 min at room temperature. Luminecense was read on the spectraMAX Gemini plate reader. Values represent the mean ± S.E.M of three independent experiments. Statistical analysis was performed using a paired student’s t-test
Having observed an increase in ROS production in response to PBOX-6, work was next undertaken to assess the effect of pretreatment with NAC on PBOX-6 induced ROS production. ROS production was largely diminished by NAC pretreatment. Levels of ROS production were comparable to the vehicle control (Fig. 2b). These results indicate ROS production may be an early event (up to 6 h post treatment) which precedes PBOX-6 induced G2/M arrest and apoptosis in neuroblastoma cells.
Pretreatment with the antioxidant, N-acetylcysteine, inhibits the PBOX-6 mediated activation of AMPK and ACC
Having identified ROS as a possible upstream activator of AMPK in response to PBOX-6 and having observed the inhibitory effects of NAC on ROS production, it was next decided to establish the effect of this antioxidant on phosphorylation of AMPK and the downstream target ACC in SHSY5Y cells. Cells were pretreated with 5 mM NAC for 1 h followed by 2.5 μM PBOX-6 for up to 6 h. Pretreatment with NAC prevented PBOX-6 induced phosphorylation of AMPK, while expression of total AMPK was unaffected (Fig. 3). Similar results were observed with ACC. These findings would support the role of ROS as an activator of AMPK in response to PBOX-6. It was next of interest to investigate the effects of this antioxidant on the anti-proliferative and pro-apoptotic effects of PBOX-6.
Pretreatment with NAC inhibits PBOX-6 mediated phosphorylation of AMPK and ACC in SHSY5Y cells. SHSY5Y cells were seeded at a density of 3.0 × 105 cells in T25cm2 flasks and left to adhere overnight. The following day, cells were treated with either 2.5 μM PBOX-6 or pretreated with 5 mM NAC followed by 2.5 μM PBOX-6 for the indicated times. After the required incubation time, cells were harvested and lysates were prepared for western blot analysis. 30 μg of protein was separated on a 6 % or 10 % resolving gel with 5 % stacking gel, transferred to a PVDF membrane and probed with an anti-phospho-AMPK or anti-phospho-ACC antibody. Membranes were also probed for AMPK or ACC as a loading control. Results are representative of three separate experiments
The antioxidant N-acetylcysteine protects against the pro-apoptotic effects of PBOX-6
As we have previously reported, a PBOX-mediated decrease in neuroblastoma cell viability was attributable to G2/M arrest and induction of apoptosis in SHSY5Y cells [13], we next sought to establish the possible protective effects of NAC pretreatment on PBOX-induced apoptosis in these cells. Pretreatment with NAC was found to significantly protect against induction of apoptosis by both PBOX-6 up to 48 h post treatment. For example, after 24 h 2.5 μM PBOX-6 induced 21.16 % ± 3.3 which decreased to 7.13 % ± 3.3 after treatment with NAC (Fig. 4a). After 48 h the percentage of apoptosis induced by PBOX-6 alone increased to up to a maximum of 48.12 % ± 3.32 which decreased to between 24.6 % ± 4.4 and 6.06 % ± 1.7 upon pretreatment with NAC (Fig. 4b). These results indicated that NAC was protecting against PBOX-induced apoptosis possibly by inhibiting induction of ROS. As apoptosis was only partially inhibited this could be one of a number of pathways through which PBOX-6 mediates its anti-cancer effects.
Pretreatment with the antioxidant NAC significantly inhibits induction of apoptosis by PBOX-6 in SHSY5Y cells. SHSY5Y cells were treated with either varying concentrations of PBOX-6 (2.5, 5, 10 μM) or pretreated with NAC for 1 h followed by PBOX-6 (2.5, 5, 10 μM) for the indicated times. After the required incubation time, cells were harvested, fixed in 2 mls ethanol and stained with propidium iodide. Cells were analyzed by flow cytometry for the percentage of cells undergoing apoptosis and determined by quantification of the sub G1/G0 peak. Values represent the mean ± S.E.M of three independent experiments. Statistical analysis was performed using one way ANOVA with Tukey’s multiple comparison test. **p < 0.01, *p < 0.05
PBOX-6 inhibits the mTOR signalling pathway in SHSY5Y cells
Many studies have identified mTOR as a downstream target of AMPK. Reports have indicated that activated AMPK phosphorylates TSC2 and RAPTOR to inhibit mTOR signalling [33]. As PBOX-6 was shown to increase phosphorylation of AMPK indicating activation, we hypothesised that this MTA may inhibit the mTOR signalling pathway. Therefore, assessment of the effects of PBOX-6 on mTOR and its downstream targets p70 S6 kinase, S6 ribosomal protein and eEF2K in SHSYSY cells was carried out. Activation/inactivation of these proteins by western blotting up to 6 h post treatment with PBOX-6 was monitored. PBOX-6 was found to decrease phosphorylation of mTOR 60 min after treatment with PBOX-6 (Fig. 5). This decrease was maintained up to 6 h after drug exposure indicating inhibition of this pathway and potential inhibition of protein translation and synthesis (Fig. 5). Analysis of phosphorylation of p70 S6 kinase was next undertaken; a phospho-specific antibody which recognises phosphorylation at Thr389, a site which has previously been shown to be essential for activation, was utilised. A time dependent decrease in phosphorylation of this site in response to PBOX-6 was observed. Comparable to phosphorylated mTOR this decrease in phosphorylation was first observed approximately 60 min post treatment. This inhibition was seen to be transient with expression of phosphorylated p70 S6 kinase increasing between 1 and 2 h, while it should be noted, phosphorylation did not return to the level of the vehicle (Fig. 5). Previous studies have reported transient effects on p70 S6 kinase activation and inactivation [34, 35].
PBOX-6 inhibits the mTOR signalling pathway in SHSY5Y cells in a time dependent manner. SHSY5Y cells were seeded at a density of 3.0 × 105 cells in T25cm2 flasks and left to adhere overnight. The following day, cells were treated with 2.5 μM PBOX-6 for the indicated time. After the required incubation time cells were harvested and lysates were prepared for western blot analysis. 30 μg of protein was separated on a 12 % resolving gel with 5 % stacking gel, transferred to a PVDF membrane and probed with an b anti-mTOR, c anti-phospho-mTOR, d anti-p70 S6 Kinase, e, f anti-phospho-S6 ribosomal protein or g anti-phospho-eEF2K antibody. Membranes were also probed for GAPDH as a loading control. Results are representative of three separate experiments. Western blots were normalised to total GAPDH as a control and densitometric analysis of bands was carried out with the imageJ software programme. Statistical analysis was performed using one way ANOVA with Tukey’s multiple comparison test. *** p < 0.001, **p < 0.01, *p < 0.05
To further examine the effects of the PBOXs on the mTOR signalling pathway, activation of the downstream target S6 ribosomal protein was investigated. When activated this protein is phosphorylated on multiple residues within the small carboxyl-terminal region, therefore the use of several phosphor specific antibodies which recognise multiple sites including Ser235, Ser236, Ser240 and Ser244 were employed. The effect of PBOX-6 on phosphorylation of S6 ribosomal protein was comparable to those observed on p70 S6 kinase (Fig. 5). A time dependent decrease in phosphorylation of these sites in response to PBOX-6 was observed. A decrease in expression was first noted approximately 60 min post treatment.. This inhibition was seen to be transient with expression of phosphorylated S6 ribosomal protein increasing between 1 and 2 h, while it should be noted, phosphorylation did not return to the level of the vehicle (Fig. 5).
In addition to p70 S6 Kinase, the mTOR signalling pathway also regulates the translation elongation process through the phosphorylation of eukaryotic elongation factor 2 (eEF2). As inhibition of upstream members of the mTOR signalling pathway had been observed, work was next undertaken to investigate the possible inhibitory effects of PBOX-6 on translation elongation process. Using a phosphor specific eEF2K antibody a decrease in phosphorylation was observed, beginning 60 min post treatment with significant inhibition evident from 2 h post treatment. An almost complete inhibition in expression was observed after 6 h (Fig 5). Taken together these results indicate that PBOX-6 inhibits multiple members of the mTOR signalling pathway in SHSY5Y which may potentially inhibit protein translation in this cell line.
Pretreatment with the antioxidant N-acetylcysteine inhibits the PBOX-6 mediated decrease in Mcl-1 expression
Primary neuroblastoma tumours have been shown to heterogeneously express Mcl-1, with high expression correlating to high-risk phenotype [36] while downregulation of Mcl-1 expression has been shown to sensitise neuroblastoma cells to chemotherapy [36]. Previously PBOX-6 was shown to induce a time and dose dependent decrease in Mcl-1 expression in SHSY5Y cells while siRNA mediated knockdown of Mcl-1 sensitised neuroblastoma cells to carboplatin pointing to the importance of Mcl-1 in mediating apoptosis [13]. Having observed AMPK activation and consequent inhibition of the mTOR signalling pathway, a regulator of protein synthesis controlling multiple components involved in the initiation and elongation stages of translation, we hypothesised that PBOX-6 induced decrease in Mcl-1 expression may be mediated by activation of AMPK leading to mTOR inhibition, a decrease in phosphorylation of p70 S6 kinase, S6 ribosomal kinase and eEF2K. Altogether this may lead to an inhibition of translation of Mcl-1 and a decrease in expression. As NAC was found to inhibit both AMPK activation and the pro-apoptotic effects of PBOX-6, the effect of this antioxidant on Mcl-1 expression was determined. SHSY5Y cells were pretreated with NAC for 1 h followed by treatment with varying concentrations of PBOX-6. Pretreatment of cells with NAC prevented PBOX-6 mediated decrease in Mcl-1 expression (Fig. 6). These findings may suggest that PBOX-6 induced inhibition of Mcl-1 expression is mediated through the AMPK/mTOR signalling pathway in neuroblastoma cells.
Pretreatment with the antioxidant NAC inhibits PBOX-6 mediated decrease in Mcl-1 expression. a SHSY5Y cells were seeded at a density of 3.0 × 105 cells in T25cm2 flasks and left to adhere overnight. The following day, cells were treated with varying concentrations of PBOX-6 (2.5 μM, 5 μM or 10 μM) or pretreated with 5 mM NAC for 1 h followed by PBOX-6 2.5 μM, 5 μM or 10 μM). After 24 h cells were harvested and lysates were prepared for western blot analysis. 30 μg of protein was separated on a 12 % resolving gel with 5 % stacking gel, transferred to a PVDF membrane and probed with an anti-Mcl-1 antibody. Membranes were also probed for GAPDH as a loading control. Results are representative of three separate experiments. b Western blots were normalised to GAPDH and densitometric analysis of bands was carried out with the imageJ software. Statistical analysis was performed using one way ANOVA with Tukey’s multiple comparison test. ***p < 0.001
PBOX-6 significantly reduces tumour volume in an in vivo model of neuroblastoma
Four-six week-old female BALB/c-nude mice received a subcutaneous injection of 2 × 106 SHSY5Y cells in the log phase of growth into the right flank. Tumours started to appear by day 30 and were measurable by day 35. Mice were randomly divided into two groups (n = 5). The PBOX-6 treatment group (n = 5) received an intratumoural (i.t.) injection of 7.5 mg kg−1 PBOX-6 once every 2 days for the duration of the experiment starting on day 35. Control mice (n = 5) received an i.t. injection of 50 μl of the equivalent vehicle (10 % (v/v) ethanol: cremophor EL in PBS). Welfare was monitored every 2 days to ensure that no mouse suffered any form of distress such as failing to groom or hunching.
Tumour growth was measured every second day, the long (L) and short (S) axes were recorded, and tumour volume (V) calculated using the following equation: V = (S2 × L)/2 [27]. Injections were initiated on day 35 when there was no significant difference in tumour volume between the control and the PBOX-treated groups. By day 7, PBOX-6 had significantly reduced tumour growth when compared to control group (Fig. 7a). Tumour burden was continuously and significantly inhibited up until the experimental end point of the study (Fig. 7a). Statistical analysis was performed using an unpaired Student’s t-test. At the experimental end point, day 13, mice were killed by CO2 asphyxiation followed by cervical dislocation. Mice were weighed every 2 days. Results indicate that neither the vehicle nor PBOX-6 adversely affected body weight. In fact, both groups put on a small amount of weight during the experiment, (Fig. 7b) which would be expected with healthy mice of this age.
Administration of PBOX-6 significantly inhibits tumour growth in an in vivo mouse model of neuroblastoma. Four-six week-old female BALB/c-nude mice received a subcutaneous injection of 2 × 106 SHSY5Y cells in the log phase of growth into the right flank. On day 35 when the tumour diameter was approximately 3 mm, mice were randomly divided into groups (n = 5). a The PBOX-6 treatment group (n = 5) received an intratumoural (i.t.) injection of 7.5 mg kg−1 PBOX-6 once every 2 days for the duration of the study. Control mice (n = 5) received an i.t injection of 50 μl of vehicle (10 % (v/v) ethanol and 10 % (v/v) cremophor EL in PBS). Tumour growth was measured every second day, the long (L) and short (S) axes were recorded, and tumour volume (V) calculated using the equation: V = (S 2 × L)/2. Data shown represents the mean ± SEM of five mice per group. Statistical analysis was performed using the Student’s unpaired t-test. ***p < 0.001, p < 0.01, *p < 0.05. b Following commencement of the vehicle/PBOX-6 injections, animals were weighed once every 2 days for the duration of the study
Discussion
AMPK, a master regulator of homeostasis, is activated in response to stresses such as a decrease in glucose levels, ischaemia or hypoxia [37]. AMPK functions to monitor the ratios of AMP/ATP and ADP/ATP. As ATP is consumed by the cells, levels of AMP and ADP increase. A decrease in ATP leads to AMPK activation; AMP directly binds to the γ subunit of AMPK to prevent dephosphorylation of the critical thr389 residue in the activation loop of the α subunit [38]. Activation results in the inhibition of anabolic pathways which consume ATP, such as protein synthesis, and the switching on of catabolic pathways which produce ATP, such as autophagy, resulting in restoration of cellular energy homeostasis [32]. In order for a tumour to grow, a cell must redirect its bioenergetic resources towards the replication of components such as DNA, proteins and membranes etc., leading to an anabolic shift in cellular metabolism. As AMPK switches off anabolic pathways, activation of this kinase would appear to play a tumour suppressing role. Previous studies have demonstrated that activation of AMPK inhibits the synthesis of the majority of cellular macromolecules, proteins, ribosomal RNA, cholesterol and glycogen [37–40], while also causing cell cycle arrest associated with stabilization of p53 and the cyclin-dependent kinase inhibitors p21WAF1 and p27CIP1 [41, 42]. As multiple chemotherapeutics have been shown to induce AMPK activation, we sought to determine the effects of the PBOXs on AMPK activation in neuroblastoma cells.
Western blotting analysis was employed to elucidate the effects of PBOX-6 on AMPK activation. We determined PBOX-6 induced activation in a time dependent manner. Additionally phosphorylation and inactivation of Acetyl-CoA carboxylase (ACC), a downstream target of AMPK was observed. These findings are in agreement with previous reports detailing AMPK activation in response to MTAs in B16 melanoma cells [15]. Both vincristine and taxol were found to induce AMPK activation in a time and dose dependent manner. siRNA mediated knockdown of LKB1, the upstream activator of AMPK was shown to inhibit vincristine induced AMPK activation. Furthermore Chen et al., [18] highlighted the role of AMPK in mediating the pro-apoptotic effects of reactive oxygen species, H202 induced a time and dose dependent phosphorylation and activation of AMPK in PC12 and primary neurons. Expression of a dominant negative form of AMPK or downregulation of AMPK partially preventing induction of H202 induced cell death.
Having observed PBOX-6 induced activation of AMPK, these findings prompted us to examine both the upstream and downstream events associated with AMPK activation in SHSY5Y cells. Determination of the role of ROS production in PBOX mediated apoptosis was next undertaken. PBOX-6 induced an early increase (from 1 h) in ROS production. This is in agreement with reports detailing the effect of MTAs on ROS production, where both vincristine and taxol were shown to induce apoptosis mediated by ROS production [15]. Various mechanisms have been described to account for the generation of ROS in response to chemotherapeutics, including redox cycling, p53-mediated mitochondrial oxidase activation or electron transport chain disruption [43–45]. The passing of electrons through the electron transport chain creates a proton gradient which is used by ATP synthase to drive the production of ATP. The electrons which pass from complex 3 to complex 4, result in the formation of 02 and H20. About 2 % of these electrons escape and react with molecular oxygen to form superoxide, which is converted to hydrogen peroxide by superoxide dimutase [46]. Chemotherapeutic drugs may induce permeabilisation of the mitochondrial membrane leading to the release of cytochrome c. When this occurs the flow of electrons along the electron transport chain is disrupted; electrons are diverted from the electron transport chain to oxygen by NADPH dehydrogenase and reduced coenzyme Q10 resulting in the formation of superoxide radicals. It is possible that the PBOXs are producing ROS through disruption of the electron transport chain but this would require further investigation.
The NADPH oxidase (NOX) family of proteins have also been implicated in the generation of ROS [47]. The NOX family comprises seven members, NOX 1–5 and the dual oxidases (DUOXs) DUOX 1 and DUOX 2. The NOX complexes were initially thought to be specific to phagocyte cells, but these enzymes are now recognized as being almost universally expressed in virtually every tissue in the body [48]. These transmembrane proteins generate superoxide by transferring electrons from the inside of the cell across the membrane, coupling them to molecular oxygen to produce a superoxide anion which dismutases into hydrogen peroxide. NOX donates an electron from NADPH to molecular oxygen (O2) to produce superoxide (O2-). MTAs have previously been reported to produce ROS mediated by NOX. Paclitaxel was found to increase expression of Rac1, a positive regulator of NOX and activate the membrane associated NOX, leading to extracellular release of superoxide, which is subsequently converted to hydrogen peroxide [49]. It is possible the PBOX-6 is producing ROS through an increase in NOX expression although this would require further investigation. To further support this theory, recent reports have suggested that the activity of NOX is regulated by the MAPK family, in particular JNK, a key mediator in PBOX-induced apoptosis [50]. Inhibition of JNK significantly attenuated NADPH oxidase activation and the upregulation of components, while also reducing production of H202 [51].
The antioxidant NAC, a scavenger of these free radicals, has been extensively used as a tool to elucidate the role of oxidative stress in numerous human pathologies, including cancer, arthritis and cardiovascular disease among others. Pretreatment with the antioxidant NAC was found to inhibit the anti-proliferative effects of PBOX-6 while an induction of apoptosis was diminished upon pretreatment with NAC. Taken together these results would point to a role of ROS in mediating PBOX-6 induced apoptosis in neuroblastoma cells. These findings are supported by previous reports in the literature detailing the effects of both ROS producing drugs and NAC on various cancer cell lines. Numerous ROS producing drugs have been shown to induce mitochondrial damage and cell death. Safingol, a sphingolipid currently in phase 1 clinical trials for the treatment of solid tumours, was found to produce a time and dose dependent increase in ROS in MDA-MB-23 and HT-29 cell lines [52]. In addition to these reports, cisplatin has been shown to induce ROS production in a panel of small cell lung carcinoma cell lines [53]. Cisplatin binds to DNA forming covalent platinum DNA adducts and triggers activation of multiple pathways including DNA repair, transcription inhibition, cell cycle arrest and apoptosis [54]. Generation of ROS lead to activation of the intrinsic pathway as evidenced by the increase in pro-apoptotic Bax, activation of initiator caspase-9 and effector caspase-3 and an increase in PARP cleavage, while the effects of cisplatin were prevented by pretreatment with NAC.
Numerous observations have drawn attention to the role of mTOR signalling in oncogenesis and cancer progression in certain cancers including neuroblastoma. Similar to AMPK, mTOR sits at a central point in a signalling pathway consisting of many components implicated in tumourigenesis, including AKT, PI3K and eIF4E which may behave as oncoproteins, and PTEN, TSC1/TSC2 and LKB1 which may function as tumour suppressors. Therefore regulation of this pathway is paramount to preventing development of cancer and may play a critical anti-cancer role in neuroblastoma, through either downregulation of tumour promoters or upregulation of tumour suppressors. Previous studies have reported increased phosphorylation of mTOR in a panel of neuroblastoma cells lines and tissue samples [25], indicating that the mTOR signalling pathway is overactive in neuroblastoma and drugs which inhibit this pathway may represent a novel therapeutic strategy, particularly for the treatment of advanced stage MYCN amplified tumours.
Therefore, having established the effect of PBOX-6 on ROS production and AMPK activation as well as the chemoprotective effects of NAC, we next sought to examine the effects on the mTOR pathway. A time dependent inhibition of mTOR in response to PBOX-6 was observed while a transient decrease in phosphorylation of the downstream target p70 S6 kinase and S6 ribosomal proteins was observed. Previous studies have reported transient effects on p70 S6 kinase activation and inactivation. AICAR, an activator of AMPK, was found to induce a decrease in phosphorylation (up to 1 h post treatment) followed by a time dependent increase (up to 24 h) which preceded a second decrease in phosphorylation (after 48 h) in CAL62 thyroid carcinoma cell line, although the authors of this paper did not provide an explanation for these findings [54]. Similarly Arsikin et al. [35] observed a transient decrease in phospho-p70 S6kinase, despite continuous inhibition of phospho-mTOR in response to dopaminergic neurotoxin 6-hydroxydopamine (6-OHDA) in SHSY5Y cells.
Although mTOR phosphorylates p70 S6 kinase, other proteins have been implicated in its regulation. p70 S6 kinase has been reported to be phosphorylated by PDK1 [55]. PDK1 is activated downstream of PI 3-kinase. Over activation of the PI 3-kinase/Akt pathway in neuroblastoma has been reported to correlate with poor prognosis [56]. It is hypothesised that over activation of this pathway in SHSY5Y cells may lead to phosphorylation of p70 S6 kinase in spite of mTOR inhibition although this hypothesis would require further investigation.
Expression of eEF2K was also shown to decrease in a time dependent manner in response to PBOX-6. eEF2K activity is regulated by mTOR through p70 S6 Kinase and S6 ribosomal kinase and independently of mTOR by AMPK. Phosphorylation of eEF2K by p70 S6 kinase and S6 ribosomal kinase leads to inactivation of eEF2K, facilitating the dephosphorylation of eEF2 and thus promoting translation. A decrease in expression of both p70 S6 kinase and S6 ribosomal protein, a substrate of S6 ribosomal kinase, was noted in response to PBOX-6 approximately 60 min post treatment, potentially preventing phosphorylation and inactivation of eEF2K. It is possible that even transient inhibition of both p70 S6 kinase and S6 ribosomal protein may be sufficient to inhibit translation of elongation factors such as eEF2. eEF2K expression may also be regulated by AMPK; it has previously been reported that activated AMPK phosphorylates and inactivates eEF2 via direct phosphorylation of eEF2K by AMPK, at a stimulatory eEF2K site that is different from the inhibitory site phosphorylated by S6 ribosomal kinase [57, 58]. The results presented herein demonstrated that activation of this kinase is most evident after 6 h treatment, during which time phosphorylation of p70 S6 Kinase and S6 ribosomal protein has increased. In contrast, phosphorylation of AMPK was found to be maximal after 6 h potentially indicating regulation of eEF2K by AMPK. Therefore, it is possible that both kinases are contributing to eEF2K activation in SHSY5Y cells. Taken together these results indicate that PBOX-6 inhibits multiple members of the mTOR signalling pathway in SHSY5Y which may potentially inhibit protein translation in this cell line.
mTOR inhibitors have been reported to execute their anti-cancer effects through two mechanisms: firstly by inhibiting proliferation by induction of cell cycle arrest and secondly they act as cytotoxic agents which induce apoptosis. The ability of the PBOX compounds to induce both G2/M arrest and apoptosis in neuroblastoma has previously be reported [13], while gene silencing of Mcl-1 has demonstrated the importance of Mcl-1 downregulation in the apoptotic pathway mediated by the PBOXs in neuroblastoma. To further explore the role of mTOR inhibition in PBOX-6 induced cell death, the effects of NAC on Mcl-1 expression post PBOX-6 treatment was determined. As NAC was found to exhibit a protective effect against the action of PBOX-6, it was postulated this may occur by inhibiting the PBOX-6 mediated decrease in Mcl-1 expression. Pretreatment with NAC was found to abrogate the effects of PBOX-6 on Mcl-1 expression. This was in agreement with previous reports of the inhibition of the mTOR pathway by the diuretic, ethacrynic acid, leading to a block in translation of Mcl-1, which could be blocked by pretreatment with NAC in HL-60 cells [59]. It is likely that PBOX-6 induced mTOR inhibition is an early event (up to 6 h) which precedes PBOX-6 induced cell cycle arrest and apoptosis in SHSY5Y cells.
Having previously reported induction of apoptosis by PBOX-6 in vitro, it was next of interest to determine the effects of PBOX-6 in an in vivo neuroblastoma xenograft model. The BALB/C neuroblastoma model has previously been used to study the effects of chemotherapeutics such as cisplatin, on tumour burden. PBOX-6 has previously been shown to restrict tumour growth in an in vivo mouse mammary carcinoma [5] and an in vivo CML model [9, 10]. Results from this study showed that PBOX-6 significantly inhibited neuroblastoma tumour growth when compared to mice receiving vehicle injections. Mice did not experience weight loss or exhibit any signs of distress during PBOX treatment suggesting PBOX-6 does not induce gross toxicity. In fact all mice gained a small amount of weight during the study.
In conclusion, this study has shown for the first time that PBOX-6 induced production of ROS which preceded PBOX-mediated G2/M arrest and apoptosis. As a result AMPK became activated which inactivated the downstream target ACC leading to inhibition of the mTOR signalling pathway. Pretreatment with the antioxidant NAC partially inhibited the apoptotic effects of PBOX-6 and prevented PBOX-6 mediated decrease in Mcl-1 expression, which may suggest that PBOX-6 induced inhibition of Mcl-1 expression is mediated through the AMPK/mTOR signalling pathway in neuroblastoma cells. Additionally we have demonstrated PBOX-6 mediated decrease in tumour burden in an in vivo model of neuroblastoma indicating that the effects of PBOX-6 is not limited to in vitro cell lines. This study provides new insights into understanding the molecular and cellular mechanisms involved in PBOX-6 induced cell death in neuroblastoma.
Abbreviations
- ACC:
-
Acetyl Co-A carboxylase
- AMPK:
-
5’ adenosine monophosphate-activated protein kinase
- CML:
-
Chronic myeloid leukaemia
- DTT:
-
Dithiothreitol
- eEF2:
-
Eukaryotic elongation factor 2
- FAC:
-
Fluorescence associated cell sorter
- FBS:
-
Foetal bovine serum
- H202 :
-
Hydrogen peroxide
- Mcl-1:
-
Myeloid cell leukemia 1
- MDR:
-
Multidrug resistance
- MTA:
-
Microtubule targeting agent
- mTOR:
-
Mammalian target of rapamycin
- NAC:
-
N-acetylcysteine
- ROS:
-
Reactive oxygen species
- PARP:
-
Poly (ADP-ribose) polymerase
- PBS:
-
Phosphate buffered saline
- PBOX:
-
pyrrolo-1,5-benzoxazepine
References
Maris JM (2010) Recent advances in neuroblastoma. N Engl J Med 362(23):2202–2211
Cheung NK, Dyer MA (2013) Neuroblastoma: developmental biology, cancer genomics and immunotherapy. Nat Rev Cancer 13(6):397–411
Saraswathy M, Gong S (2013) Different strategies to overcome multidrug resistance in cancer. Biotechnol Adv 31(8):1397–1407
Zisterer DM, Campiani G, Nacci V, Williams DC (2000) Pyrrolobenzoxazepines induce apoptosis in HL-60, Jurkat and Hut-78 cells: a new class of apoptotic agents. J Pharmacol Exp Ther 293(1):48–59
Greene LM, Fleeton M, Mulligan J, Gowda C, Sheahan BJ, Atkins GJ et al (2005) The pyrrolo-1, 5-benzoxazepine, PBOX-6, inhibits the growth of breast cancer cells in vitro independent of estrogen receptor status, and inhibits breast tumour growth in vivo. Oncol Rep 14(5):1357–1363
Mulligan JM, Greene LM, Cloonan S, Mc Gee MM, Onnis V, Campiani G et al (2006) Identification of tubulin as the molecular target of proapoptotic pyrrolo-1,5-benzoxazepines. Mol Pharmacol 70(1):60–70
Nathwani SM, Butler S, Fayne D, McGovern N, Sarkadi B, Meegan MJ et al (2010) Novel microtubule targeting agents, pyrrolo-1,5-benzoxazepines, induce apoptosis in multi-drug resistant (MDR) cancer cells. Cancer Chemother Pharmacol 66(3):585–596
Nathwani SM, Cloonan SM, Stronach M, Campiani G, Lawler M, Williams DC et al (2010) Novel microtubule-targeting agents, pyrrolo-1,5-benzoxazepines, induce cell cycle arrest and apoptosis in prostate cancer cells. Oncol Rep 24(6):1499–1507
Bright SA, McElligott AM, O’Connell JW, O’Connor L, Carroll P, Campiani G et al (2010) Novel pyrrolo-1,5-benzoxazepine compounds display significant activity against resistant chronic myeloid leukaemia cells in vitro, in ex vivo patient samples and in vivo. Br J Cancer 102(10):1474–1482
Bright SA, Campiani G, Deininger MW, Lawler M, Williams DC, Zisterer DM (2010) Sequential treatment with flavopiridol synergistically enhances pyrrolo-1,5-benzoxazepine-induced apoptosis in human chronic myeloid leukaemia cells including those resistant to imatinib treatment. Biochem Pharmacol 80(1):31–38
McElligott AM, Maginn EN, Greene LM, McGuckin S, Hayat A, Browne PV et al (2009) The novel tubulin-targeting agent pyrrolo-1,5-benzoxazepine-15 induces apoptosis in poor prognostic subgroups of chronic lymphocytic leukemia. Cancer Res 69(21):8366–8375
Bright SA, Greene LM, Greene TF, Campiani G, Butini S, Brindisi M, Lawler M, Meegan MJ, Williams DC, Zisterer DM (2009) The novel pyrrolo-1,5-benzoxazepine, PBOX-21, potentiates the apoptotic efficacy of STI571 (imatinib mesylate) in human chronic myeloid leukaemia cells. Biochem Pharmacol 77:310–321
Lennon JC, Bright SA, Carroll E, Butini S, Campiani G, O’Meara A et al (2014) The novel pyrrolo-1,5-benzoxazepine, PBOX-6, synergistically enhances the apoptotic effects of carboplatin in drug sensitive and multidrug resistant neuroblastoma cells. Biochem Pharmacol 87(4):611–624
Pradelli LA, Bénéteau M, Chauvin C, Jacquin MA, Marchetti S, Muñoz-Pinedo C et al (2010) Glycolysis inhibition sensitizes tumor cells to death receptors-induced apoptosis by AMP kinase activation leading to Mcl-1 block in translation. Oncogene 29(11):1641–1652
Chen MB, Shen WX, Yang Y, Wu XY, Gu JH, Lu PH (2011) Activation of AMP-activated protein kinase is involved in vincristine-induced cell apoptosis in B16 melanoma cell. J Cell Physiol 226(7):1915–1925
Chen MB, Zhang Y, Wei MX, Shen W, Wu XY, Yao C et al (2013) Activation of AMP-activated protein kinase (AMPK) mediates plumbagin-induced apoptosis and growth inhibition in cultured human colon cancer cells. Cell Signal 25(10):1993–2002
Wu WD, Hu ZM, Shang MJ, Zhao DJ, Zhang CW, Hong D et al (2014) Cordycepin down-regulates multiple drug resistant (MDR)/HIF-1α through regulating AMPK/mTORC1 signalling in GBC-SD gallbladder cancer cells. Int J Mol Sci 15(7):12778–12790
Chen L, Xu B, Liu L, Luo Y, Yin J, Zhou H et al (2010) Hydrogen peroxide inhibits mTOR signaling by activation of AMPK alpha leading to apoptosis of neuronal cells. Lab Investig 90(5):762–773
Circu ML, Aw TY (2010) Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic Biol Med 48(6):749–762
Kerksick C, Willoughby D (2005) The antioxidant role of glutathione and N-acetyl-cysteine supplements and exercise-induced oxidative stress. J Int Soc Sports Nutr 2:38–44
Bitting RL, Armstrong AJ (2013) Targeting the PI3K/Akt/mTOR pathway in castration-resistant prostate cancer. Endocr Relat Cancer 20(3):R83–R99
Vinayak S, Carlson RW (2013) mTOR inhibitors in the treatment of breast cancer. Oncology (Williston Park) 27(1):38–44
Barrett D, Brown VI, Grupp SA, Teachey DT (2012) Targeting the PI3K/AKT/mTOR signaling axis in children with hematologic malignancies. Paediatr Drugs 14(5):299–316
Matter MS, Decaens T, Andersen JB, Thorgeirsson SS (2014) Targeting the mTOR pathway in hepatocellular carcinoma: current state and future trends. J Hepatol 60(4):855–865
Johnsen JI, Segerström L, Orrego A, Elfman L, Henriksson M, Kågedal B et al (2008) Inhibitors of mammalian target of rapamycin downregulate MYCN protein expression and inhibit neuroblastoma growth in vitro and in vivo. Oncogene 27(20):2910–2922
Campiani G, Nacci V, Fiorini I, De Filippis MP, Garofalo A, Ciani SM et al (1996) Synthesis, biological activity, and SARs of pyrrolobenzoxazepine derivatives, a new class of specific ‘peripheral-type’ benzodiazepine receptor ligands. J Med Chem 39(18):3435–3450
Williams CR, Tabiosa R, Linehana WM, Neckersa L (2007) Intratumor injection of the Hsp90 inhibitor 17AAG decreases tumor growth and induces apoptosis in a prostate cancer xenograft model. J Urol 178:1528–1532
Shah MR, Kriedt CL, Lents NH, Hoyer MK, Jamaluddin N, Klein C et al (2009) Direct intra-tumoral injection of zinc-acetate halts tumor growth in a xenograft model of prostate cancer. J Exp Clin Cancer Res 28:84
Beck MT, Chen NY, Franek KJ, Chen WY (2003) Experimental therapeutics prolactin antagonist-endostatin fusion protein as a targeted dual-functional therapeutic agent for breast cancer. Cancer Res 63:3598–3604
Garcia-Gil M, Pesi R, Perna S (2003) 5’-aminoimidazole-4-carboxamide riboside induces apoptosis in human neuroblastoma cells. Neuroscience 117:811–820
Hadad SM, Appleyard V, Thompson AM (2009) Therapeutic metformin/AMPK activation promotes the angiogenic phenotype in the ERalpha negative MDA-MB-435 breast cancer model. Breast Cancer Res Treat 114:391
Kim HG, Hien TT, Han EH, Hwang YP, Choi JH, Kang KW et al (2011) Metformin inhibits P-glycoprotein expression via the NF-kB pathway and CRE transcriptional activity through AMPK activation. Br J Pharmacol 162(5):1096–1108
Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A, Vasquez DS et al (2008) AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol Cell 30(2):214–226
Choi HJ, Kim TY, Chung N, Yim JH, Kim WG, Kim JA et al (2011) The influence of the BRAF V600E mutation in thyroid cancer cell lines on the anticancer effects of 5-aminoimidazole-4-carboxamide-ribonucleoside. J Endocrinol 211(1):79–85
Arsikin K, Kravic-Stevovic T, Jovanovic M, Ristic B, Tovilovic G, Zogovic N et al (2012) Autophagy-dependent and -independent involvement of AMP-activated protein kinase in 6-hydroxydopamine toxicity to SH-SY5Y neuroblastoma cells. Biochim Biophys Acta 1822(11):1826–1836
Lestini BJ, Goldsmith KC, Fluchel MN, Liu X, Chen NL, Goyal B et al (2009) Mcl-1 downregulation sensitizes neuroblastoma to cytotoxic chemotherapy and small molecule Bcl2-family antagonists. Cancer Biol Ther 8(16):1587–1595
Hardie DG, Ross FA, Hawley SA (2012) AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol 13:251–262
Sanders MJ, Ali ZS, Hegarty BD, Heath R, Snowden MA, Carling D (2007) Defining the mechanism of activation of AMP-activated protein kinase by the small molecule A-769662, a member of the thienopyridone family. J Biol Chem 282:32539–32548
Hardie DG (2011) AMP-activated protein kinase: an energy sensor that regulates all aspects of cell function. Genes Dev 25(18):1895–1908
Hardie DG (2007) AMP-activated/SNF1 protein kinases: conserved guardians of cellular energy. Nat Rev Mol Cell Biol 8:774–785
Jones RG, Plas DR, Kubek S et al (2005) AMP-activated protein kinase induces a p53-dependent metabolic checkpoint. Mol Cell 18:283–293
Liang J, Shao SH, Xu ZX et al (2007) The energy sensing LKB1-AMPK pathway regulates p27(kip1) phosphorylation mediating the decision to enter autophagy or apoptosis. Nat Cell Biol 9:218–224
Hwang PM, Bunz F, Yu J, Rago C et al (2001) Ferredoxin reductase affects p53-dependent, 5-fluorouracil-induced apoptosis in colorectal cancer cells. Nat Med 7:1111–1117
Pelicano H, Carney D, Huang P (2004) ROS stress in cancer cells and therapeutic implications. Drug Resist Updat 7:97–110
Pelicano H, Feng L, Zhou Y, Carew JS, Hileman EO, Plunkett W et al (2003) Inhibition of mitochondrial respiration: a novel strategy to enhance drug-induced apoptosis in human leukemia cells by a reactive oxygen species-mediated mechanism. J Biol Chem 278:37832–37839
Conklin KA (2004) Free radicals: the pros and cons of antioxidants. Cancer chemotherapy and antioxidants. J Nutr 134:3201–3204, ISSN 0022–3166
Bedard K, Krause KH (2007) The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev 87(1):245–313
Paletta-Silva R, Rocco-Machado N, Meyer-Fernandes JR (2013) NADPH oxidase biology and the regulation of tyrosine kinase receptor signaling and cancer drug cytotoxicity. Int J Mol Sci 14(2):3683–3704
Alexandre J, Hu Y, Lu W, Pelicano H, Huang P (2007) Novel action of paclitaxel against cancer cells: bystander effect mediated by reactive oxygen species. Cancer Res 67(8):3512–3517
Mc Gee MM, Campiani G, Ramunno A, Nacci V, Lawler M, Williams DC et al (2002) Activation of the c-Jun NH2 terminal kinase (JNK) signaling pathway is essential during PBOX-6-induced apoptosis in chronic myelogenous leukemia (CML) cells. J Biol Chem 227(21):18383–18389
Han JE, Choi JW (2012) Control of JNK for an activation of NADPH oxidase in LPS-stimulated BV2 microglia. Arch Pharm Res 4:709–715
Ling LU, Tan KB, Lin H, Chiu GN (2011) The role of reactive oxygen species and autophagy in safingol-induced cell death. Cell Death Dis 2:e129
Wu YJ, Muldoon LL, Neuwelt EA (2005) The chemoprotective agent N-acetylcysteine blocks cisplatin-induced apoptosis through caspase signaling pathway. J Pharmacol Exp Ther 312(2):424–431
Siddik ZH (2003) Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene 22:7265–7279
Alessi DR, Kozlowski MT, Weng QP, Morrice N, Avruch J (1998) Phosphoinositide-dependent protein kinase 1 (PDK1) phosphorylates and activates the p70 S6 kinase in vivo and in vitro. Curr Biol 8(2):69–81
Santo EE, Stroeken P, Sluis PV, Koster J, Versteeg R, Westerhout EM (2013) FOXO3a is a major target of inactivation by PI3K/AKT signaling in aggressive neuroblastoma. Cancer Res 73(7):2189–2198
Horman S, Beauloye C, Vertommen D, Vanoverschelde JL, Hue L, Rider MH (2003) Myocardial ischemia and increased heart work modulate the phosphorylation state of eukaryotic elongation factor-2. J Biol Chem 278:41970–41976
Horman S, Browne G, Krause U, Patel J, Vertommen D, Bertrand L et al (2002) Activation of AMP-activated protein kinase leads to the phosphorylation of elongation factor 2 and an inhibition of protein synthesis. Curr Biol 12:1419–1423
Liu G, Wang R, Wang Y, Li P, Zhao G, Zhao L et al (2013) Ethacrynic acid oxadiazole analogs induce apoptosis in malignant hematologic cells through downregulation of Mcl-1 and c-FLIP, which was attenuated by GSTP1-1. Mol Cancer Ther 12(9):1837–1847
Acknowledgments
Stefania Butini would like to thank Istituto Toscano Tumori. This study was funded by the National Children’s Research Centre, Our Lady’s Children’s Hospital, Crumlin, Dublin, Ireland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Grant
The National Children’s Research Centre
Rights and permissions
About this article
Cite this article
Lennon, J.C., Butini, S., Campiani, G. et al. Involvement of AMP-activated protein kinase in mediating pyrrolo-1,5-benzoxazepine–induced apoptosis in neuroblastoma cells. Invest New Drugs 34, 663–676 (2016). https://doi.org/10.1007/s10637-016-0366-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-016-0366-3