Abstract
Purpose
Diopsys® NOVA™ is a novel full-field electroretinography (ffERG) device that can make rapid measurements of retinal electrophysiologic function. Diagnosys® Espion 2™ is a clinical gold-standard ERG device. This study aimed to investigate whether light-adapted Diopsys® NOVA™ fixed-luminance flicker ffERG magnitude and implicit time (converted from phase) measurements correlate with light-adapted Diagnosys® Espion 2™ flicker ffERG amplitude and implicit time measurements, respectively.
Methods
Twelve patients (22 eyes) with various retinal and uveitic diseases underwent light-adapted Diagnosys® Espion 2™ and Diopsys® NOVA™ fixed-luminance flicker testing. Diopsys® magnitude and implicit time (converted from phase) measurements were compared to Diagnosys® amplitude and implicit time measurements, and a Pearson correlation was used to evaluate any existing correlation. Groups were also compared using generalized estimating equations. Bland–Altman plots were utilized to determine agreement between the comparison groups.
Results
Age of patients ranged from 14 to 87 years. 58% (n = 7/12) of patients were female. A significant, positive correlation (r = 0.880, P < 0.001) was observed between magnitude (Diopsys®) and amplitude (Diagnosys®) measurements. Amplitude increases by 6.69 µV for each 1 µV increase in Magnitude (p-value < 0.001). A statistically significant, strong positive correlation was observed between Diopsys® implicit time measurements (converted from phase) and Diagnosys® implicit time measurements (r = 0.814, p-value < 0.001). For each 1 ms increase in Diopsys® implicit time, Diagnosys® implicit time increases by 1.13 ms (p-value < 0.001).
Conclusions
There is a statistically significant positive correlation between light-adapted Diopsys® NOVA™ fixed-luminance flicker amplitude and Diagnosys® flicker magnitude values. Additionally, there is a statistically significant positive correlation between Diopsys® NOVA™ fixed-luminance flicker implicit time (converted from phase) and Diagnosys® flicker implicit time values. These results imply that the Diopsys® NOVA™ module, which utilizes the nonstandard shortened International Society for Clinical Electrophysiology of Vision (ISCEV) ERG protocol, can produce reliable light-adapted flicker ffERG measurements.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The electroretinogram (ERG) is an electrophysiological test measuring the electrical response of various retinal cells to light stimulus. ERG is used to objectively assess retinal function in hereditary retinal diseases such as Leber congenital amaurosis [1], retinitis pigmentosa [2, 3], cone-rod dystrophy [4], achromatopsia [5], as well as acquired retinal and uveitic diseases such as paraneoplastic and autoimmune retinopathies [6], central retinal vein occlusion [7], diabetic retinopathy [8, 9], and drug toxicities [10, 11].
Full-field electroretinography (ffERG) is used to obtain objective quantitative measurements of overall retinal electrophysiologic function [12]. Analysis of ffERG waveforms can be used to distinguish the functions of different retinal cell types, including photoreceptors, bipolar cells, and to a lesser extent, retinal ganglion cells, and amacrine cells [13]. Flicker ffERG, a part of standard ffERG testing, uses 28–33 Hz light frequency to stimulate light-adapted retina, producing waveforms that give insights into cone and bipolar cell function. Rods cannot respond to this frequency; therefore, flicker ffERG response is only generated from the cones and cone-related bipolar cells [14, 15]. Cone On- and Off-bipolar cells are principally responsible for generating flicker ERG waveforms [15]. This signal is additionally dependent on L- and M-cone cells, which are sensitive to long- and medium-wavelength light, respectively [15]. Short-wavelength-sensitive S-cone cells contribute minimally to the light-adapted flicker ERG [15].
Modifications to the International Society for Clinical Electrophysiology of Vision (ISCEV) Standards and Guidelines introduced a nonstandard abbreviated ERG protocol that reduces time of dark adaptation to 10 min, includes fewer dark-adapted ERG recordings, and does not require the use of mydriasis [15]. The Diopsys® NOVA™ device (Diopsys®, Inc., Pine Brook, NJ, USA) adheres to this nonstandard shortened ERG protocol as it does not require pupil dilation and does not include all ERG tests included in the ISCEV standard protocol.
To our knowledge, no previous study has provided the correlation of the Diopsys® NOVA™ device data with that of a standard ERG system. The index study aimed to investigate whether Diopsys® NOVA™ fixed-luminance flicker ffERG magnitude and phase measurements correlate with amplitude and implicit time measurements made by the Diagnosys® 30 Hz flicker ffERG test.
Methods
Setting of study and subjects
The index study was a retrospective analysis of patients with various retinal and uveitic pathologies who underwent both Diopsys® NOVA™ fixed-luminance flicker ffERG and Diagnosys® Espion 2™ 30 Hz flicker ffERG over a period of seven months at a tertiary care center (Byers Eye Institute at Stanford University). Diopsys® NOVA™ and Diagnosys® Espion 2™ ERG testing were performed in accordance with ISCEV standards [15]. Patients with an interim period of three or more months between the two tests were excluded. In addition, patients with any surgical intervention or change in disease activity between testing sessions were excluded, including those with changes in visual acuity or disease activity markers such as cell count or macular edema.
Data collection and outcomes
We collected baseline patient characteristics, including age, sex, and underlying diseases. For the Diagnosys® flicker ERG, we collected amplitude and implicit time values. As for Diopsys® fixed-luminance flicker ERG, we collected magnitude and phase values.
Before undergoing Diagnosys® testing, patients were kept in a light-adapting room for at least 10 min. All Diagnosys® testing utilized a single Diagnosys® Espion 2™ device (Diagnosys® LLC, Lowell, MA, USA) and took place in the same clinical room under ambient light conditions. Patients were maximally dilated prior to Diagnosys® ERG testing. A patient’s forehead and outer and inner canthi of both eyes were cleansed. The patient’s eyes were then anesthetized with 0.5% proparacaine hydrochloride ophthalmic solution. Then, Dawson–Trick–Litzkow (DTL) electrodes were placed so that they touched the conjunctiva inferior to the limbus of each eye. A ground electrode was then applied to the center of the forehead. The patient’s head was then placed in the Diagnosys® ColorDome™. Flicker testing utilized standard protocol testing with light fixed at a luminance of 3.0 cd s/m2 flashed at 30 Hz (± 1%).
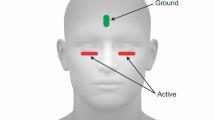
Prior to Diopsys® testing, patients were maximally dilated and kept in a light-adapting room for at least 10 min. To undergo Diopsys® NOVA™ fixed-luminance flicker ffERG, a patients forehead was cleansed with a lid scrub pad, followed by cleansing of the bottom eyelids close to the lash line. ERG lid electrodes were placed under each eyelid, close to the lash line, with lead wire attachments pointed outwards. A ground electrode was then applied to the forehead. Then, corresponding lead wires were attached to the different electrodes. The patient was then instructed to place the mini-ganzfeld stimulator gently covering their right eye first before light stimulation and measurement recordings by the machine. Light fixed at a luminance of 3 cd.s/m2 (600 cd/m2 as 5 ms flashes) at 32 Hz on a white background with a luminance of 30 cd/m2. Magnitude and phase values were then measured. This flash pattern was repeated for 20 s in each eye. If a recording had artifacts > 40%, the flicker test was repeated in accordance with Diopsys® guidelines.
Statistical analysis
Pearson correlation coefficient was used for correlation analysis of values measured by the Diopsys® NOVA™ fixed-luminance flicker ffERG and the Diagnosys® Espion 2™ 30 Hz flicker ffERG. To account for within-subject correlation between eyes, generalized estimating equations with robust standard errors were used. Bland–Altman plots were constructed to determine agreement between measurements made by the two electrophysiologic tests. Statistical analysis was performed using R (programming language). A p-value of less than 0.05 was considered statistically significant.
Results
Demographics
Twelve patients (22 eyes), all with various diseases affecting retinal function, were included in this study. These patients underwent Diopsys® fixed-luminance flicker ffERG and Diagnosys® Espion 2™ 30 Hz flicker ffERG testing. All patients had both tests performed within three months of each other. The mean difference between testing dates was 31.9 days (range, 0–81 days). The age of patients ranged from 14 to 87 years, and 58% were female (Table 1). Best-corrected visual acuity ranged from 20/20 to hand motion. The mean visual acuity was 0.71 logMAR.
Ocular diseases of patients
Ocular pathologies included retinal vasculitis (n = 7/22 eyes, 32%), melanoma associated retinopathy (MAR) (n = 2/22 eyes, 9%), idiopathic panuveitis (n = 2/22 eyes, 9%), autoimmune retinopathy (n = 2/22 eyes, 9%), autoimmune optic neuropathy (n = 2/22 eyes, 9%), non-proliferative diabetic retinopathy (n = 2/22 eyes, 9%), age-related macular degeneration (n = 2/22 eyes, 9%), tuberculous choroiditis (n = 2/22 eyes, 9%), and retinal vein occlusion (n = 1/22 eyes, 5%) (Table 1). Four patients (33%) had known systemic associations including metastatic cutaneous melanoma, tuberculosis, breast cancer, multiple sclerosis, and autoimmune hepatitis (Table 1).
Correlation between flicker ERG measurements
Mean (SD) Diopsys® magnitude and Diagnosys® amplitude measurements were 11.76 ± 3.54 µV and 66.18 ± 25.66 µV, respectively. A statistically significant, strong positive correlation was observed between both measurements (r = 0.880, p-value < 0.001) (Fig. 1). For each 1 µV increase in magnitude, amplitude increases by 6.69 µV (p-value < 0.001). All data points lay within ± 1.96 SD of the mean difference, and there is a negative bias of − 54.42 µV for the Diopsys® NOVA™ fixed-luminance ffERG flicker magnitude measurements (Fig. 2). As magnitude and amplitude increased, the difference between these values also increased. Mean (SD) Diopsys® phase and Diagnosys® implicit time measurements were 301.76 ± 38.02° and 30.63 ± 4.28 ms, respectively. Mean (SD) Diopsys® implicit time measurements (converted from phase) was 5.06 ± 3.30 ms. A statistically significant, strong positive correlation was observed between Diopsys® implicit time measurements and Diagnosys® implicit time measurements (r = 0.814, p-value < 0.001) (Fig. 3). For each 1 ms increase in Diopsys® implicit time, Diagnosys® implicit time increases by 1.13 ms (p-value < 0.001). All but one Bland–Altman data point lay within ± 1.96 SD of the mean difference, and there is a positive bias of 25.58 ms for the Diagnosys® fixed-luminance flicker implicit time measurements (Fig. 4). Figures 5 and 6 show representative reported results for Diopsys® NOVA™ fixed-luminance flicker and Diagnosys® Espion 2™ flicker, respectively.
Representative Diopsys® NOVA™ fixed-luminance flicker ERG results. A. Indicator of signal quality showing the strength of the connection between the electrodes and a patient’s head. B. Graph displaying flicker magnitude (µV) versus time (ms). C. Polar plot depiction of flicker measurements, where magnitude values are shown by radial line length and phase values are represented by the angle at which the radial line falls. Green signifies a ‘within reference range’ response, yellow signifies a ‘borderline reference range’ response, and red signifies an ‘outside reference range’ response. These reference ranges were established using a normative database compiled by the manufacture. D. Tabulated flicker data displaying mean magnitude (µV), mean phase (°), asymmetry in those measurements between eyes, magnitude variance ratio, phase variance ratio, and % of recorded artifacts
Representative Diagnosys® Espion 2™ light-adapted 30 Hz flicker ERG results showing and tabulating amplitude and phase data and flicker waveforms. A. Tabulated flicker data displaying amplitude of troughs and peaks, as well as implicit time, of two recorded flicker waves. B. Graph displaying flicker amplitude (µV) versus time (ms) of two recorded flicker waves. The two waves are translated along the y-axis so that they do not overlap and can be interpreted independently
Discussion
Our findings indicate that Diopsys® NOVA™ fixed-luminance flicker ERG magnitude measurements strongly correlate with Diagnosys® Espion 2™ flicker ERG amplitude measurements. Additionally, these two systems of measurement agree with one another. Our results also show that Diopsys® NOVA™ fixed-luminance flicker ERG phase values converted to implicit time values are strongly correlated with Diagnosys® Espion 2™ flicker ERG implicit time values, implying that Diopsys® NOVA™ fixed-luminance flicker ERG phase is consistent with Diagnosys® Espion 2™ flicker ERG implicit time. However, these two systems of measurement show biased (different) but correlated values. These results suggest that the Diopsys® NOVA fixed-luminance flicker ERG test provides reliable information about the timing and strength of light-adapted flicker responses.
According to the ISCEV Standard for Full-Field Clinical Electroretinography, reporting ERG results as frequency domain equivalents is accepted [15]. Diopsys® NOVA™ magnitude corresponds to the amplitude or responsivity of a subject's response to light stimulus. Phase relates to implicit time, where a phase closer to 360° corresponds to an implicit time closer to 0 s. Diopsys® NOVA™ utilizes frequency domain analysis to transform time domain units to phase. Throughout Diopsys® NOVA™ light-adapted flicker examination, frames of two responses (to two flashes) are translated from the time domain to the frequency domain, and magnitude and phase of the fundamental frequency are recorded. Once outliers have been eliminated, the means of the magnitude and phase values are reported. To translate the 30-Hz flicker ERG signal into the frequency domain, a rapid Fourier transform is utilized, yielding a complex number. The magnitude of x is calculated as \(\sqrt{({x}_{r}^{2}+{x}_{i}^{2}})\) while the phase is calculated as \(\mathrm{arctan}\left(\frac{{x}_{i}}{{x}_{r}}\right)\), where \({x}_{r}\) and \({x}_{i}\) are the real and imaginary components, respectively [17]. Magnitude and Phase for the Diopsys device are calculated from the first harmonic of the flicker frequency.
Observing Diopsys® NOVA™ fixed-luminance flicker ERG results, a reader can determine the normality of a magnitude or phase response by looking at the color of the result; green signifies a ‘within reference range’ response, yellow signifies a ‘borderline reference range’ response, and red signifies an ‘outside reference range’ response (Fig. 5). ‘Within reference range’ is considered a magnitude greater than 5.06 µV and a phase greater than 267.47°, ‘borderline reference range’ is considered a magnitude between 3.34 µV and 5.06 µV and a phase between 254.74° and 267.47°, and ‘outside reference range’ is considered a magnitude less than 3.34 µV and a phase less than 254.74°. These ranges are derived from a normative database compiled by the maker of the device, Diopsys®, and composed of 50 healthy patients (mean age: 53 years, 56% female) [14]. Additionally, the results are displayed in a polar plot (Fig. 5). From this image, one can determine the strength of a magnitude response by looking at the length of each radial line. One can also determine the phase response by identifying where along the circle the responses fall. As with the tabulated report of the data, green signifies a ‘within reference range’ response, yellow signifies a ‘borderline reference range’ response, and red signifies an ‘outside reference range’ response.
As the Diopsys® NOVA™ module utilizes skin electrodes placed on a patient’s lower eyelids, no topical ophthalmic anesthetic is required. It is important to note, however, that utilization of skin electrodes, as opposed to corneal or conjunctival electrodes, results in reduced amplitude responses. In a study by Tang et al. [18], the authors compared RETeval sensor strip electrodes to Dawson–Trick–Litzkow (DTL) corneal electrodes for photopic negative response recordings using the LKC RETeval device. Similar to our experiment, they reported that the skin electrodes produced an attenuated signal compared to those recorded by DTL electrodes [18]. Additionally, as the Diopsys® NOVA™ fixed-luminance flicker test follows the nonstandard abbreviated ISCEV protocol, the flicker test can be performed in a timelier manner. Utilization of a more patient-friendly electrode and shorter ERG exam might be beneficial for pediatric and disabled patients [19,20,21].
Different from many other ERG systems, the Diopsys® NOVA™ module does not require maximal pupil dilation before ERG testing [15]. The Diopsys® NOVA™ fixed-luminance flicker flash stimulus is constant and does not adjust for changes in pupil size. While patients would benefit from avoiding risks associated with artificial dilation, such as impaired driving and acute closed-angle glaucoma, the intra-patient flicker ERG parameters will change with varying pupil size [22, 23]. This is in contrast to RETeval, another mydriasis-free ERG system, which adjusts retinal illumination according to pupil size [24]. As of 2022, the ISCEV Standards and Guidelines no longer require pupil dilation if stimulus and background light are intense enough to elicit ERG waveforms comparable to those obtained with dilated pupils [15]. Mobasserian et al.[25] showed a statistically significant difference in magnitude of Diopsys® NOVA™ flicker response before and after dilation. Given this finding, we elected to maximally dilate all patients before Diopsys® NOVA™ flicker testing to prevent interpatient ERG variability as a result of differences in pupil size.
One limitation of our study is the lack of cross-sectional Diagnosys® Espion 2™ or Diopsys® NOVA™ flicker testing. We attempted to mitigate this by excluding patients whose disease activity changed between testing dates. Patients included in this study had no changes in visual acuity or parameters of disease activity, such as cell count or macular edema, between testing sessions. Another limitation of our study was that our sample size was relatively small. Considering a type I error rate of 0.05, our sample size of 22 eyes is adequate to exceed a statistical power of 0.80. Future studies should utilize like-to-like comparisons between flicker parameters, have both experiments occur within a shorter time frame (preferably the same day), and involve a larger number of eyes.
Our study demonstrates that while the Diopsys® NOVA™ module is relatively new and includes several aspects atypical of traditional ERG systems, the fixed-luminance flicker parameters are significantly correlated with those of a standard ERG device commonly used in eye clinics across the globe. Previous studies have demonstrated the precision of the Diopsys® NOVA™ flicker test [14, 26]. There are other additional tests of the Diopsys® NOVA™ that were not evaluated for validity in this study. Other tests that the Diopsys® NOVA™ module can perform include visual evoked potential, multi-focal ERG, and pattern ERG. Future studies should look to evaluate agreement between these Diopsys® NOVA™ tests and those performed by gold-standard clinical ERG devices.
Conclusion
Diopsys® NOVA™ fixed-luminance flicker ERG results are concordant with Diagnosys® Espion 2™ flicker ERG measurements.
References
Robson AG, Nilsson J, Li S, Jalali S, Fulton AB, Tormene AP, Holder GE, Brodie SE (2018) Iscev guide to visual electrodiagnostic procedures. Doc Ophthalmol 136(1):1–26. https://doi.org/10.1007/s10633-017-9621-y
Gundogan FC, Tas A, Sobaci G (2011) Electroretinogram in hereditary retinal disorders. Electroretinograms pp 5–132.
Hassan-Karimi H, Jafarzadehpur E, Blouri B, Hashemi H, Sadeghi AZ, Mirzajani A (2012) Frequency domain electroretinography in retinitis pigmentosa versus normal eyes. J Ophthalmic Vis Res 7(1):34–38
Vincent A, Robson AG, Holder GE (2013) Pathognomonic (diagnostic) ergs A review and update. Retina 33(1):5–12. https://doi.org/10.1097/IAE.0b013e31827e2306
Good PA, Searle AE, Campbell S, Crews SJ (1989) Value of the erg in congenital nystagmus. Br J Ophthalmol 73(7):512–515. https://doi.org/10.1136/bjo.73.7.512
Khanna S, Martins A, Oakey Z, Mititelu M (2019) Non-paraneoplastic autoimmune retinopathy: multimodal testing characteristics of 13 cases. J Ophthalmic Inflamm Infect 9(1):6. https://doi.org/10.1186/s12348-019-0171-1
Johnson MA, Marcus S, Elman MJ, McPhee TJ (1988) Neovascularization in central retinal vein occlusion: electroretinographic findings. Arch Ophthalmol 106(3):348–352. https://doi.org/10.1001/archopht.1988.01060130374025
Bresnick GH, Palta M (1987) Temporal aspects of the electroretinogram in diabetic retinopathy. Arch Ophthalmol 105(5):660–664. https://doi.org/10.1001/archopht.1987.01060050078042
Tahara K, Matsuura T, Otori T (1993) Diagnostic evaluation of diabetic retinopathy by 30-hz flicker electroretinography. Jpn J Ophthalmol 37(2):204–210
Ponjavic V, Andreasson S (2001) Multifocal erg and full-field erg in patients on long-term vigabatrin medication. Doc Ophthalmol 102(1):63–72. https://doi.org/10.1023/a:1017589301855
Zoumalan CI, Zamanian RT, Doyle RL, Marmor MF (2009) Erg evaluation of daily high-dose sildenafil usage. Doc Ophthalmol 118(3):225–231. https://doi.org/10.1007/s10633-008-9148-3
Creel DJ (2019) Electroretinograms. Handb Clin Neurol 160:481–493. https://doi.org/10.1016/B978-0-444-64032-1.00032-1
Wolpert K, Tsang S. Electroretinography. Electroretinograms. IntechOpen; 2011.
Resende AF, Sanvicente CT, Eshraghi H, Garcia A, Pickel K, Zhang Q, Waisbourd M, Jay Katz L (2019) Test-retest repeatability of the pattern electroretinogram and flicker electroretinogram. Doc Ophthalmol 139(3):185–195. https://doi.org/10.1007/s10633-019-09707-5
Robson AG, Frishman LJ, Grigg J, Hamilton R, Jeffrey BG, Kondo M, Li S, McCulloch DL (2022) Iscev standard for full-field clinical electroretinography (2022 update). Doc Ophthalmol 144(3):165–177. https://doi.org/10.1007/s10633-022-09872-0
Maleki A, Ueberroth JA, Manhapra A, Walsh M, Asgari S, Chang PY, Anesi SD, Foster CS (2022) Fixed-luminance and multi-luminance flicker electroretinography parameters in patients with early active birdshot chorioretinopathy. Ocul Immunol Inflamm 30(1):129–135. https://doi.org/10.1080/09273948.2020.1797113
Proakis J, Manolakis D (1996) Digital signal processing. Principles, algorithms, and applications, 4th edn. Prentice Hall.
Tang J, Hui F, Hadoux X, Sarossy M, van Wijngaarden P, Coote M, Crowston JG (2018) A comparison of the reteval sensor strip and dtl electrode for recording the photopic negative response. Transl Vis Sci Technol 7(6):27. https://doi.org/10.1167/tvst.7.6.27
Brodie SE (2014) Tips and tricks for successful electroretinography in children. Curr Opin Ophthalmol 25(5):366–373. https://doi.org/10.1097/ICU.0000000000000093
Hobby AE, Kozareva D, Yonova-Doing E, Hossain IT, Katta M, Huntjens B, Hammond CJ, Binns AM, Mahroo OA (2018) Effect of varying skin surface electrode position on electroretinogram responses recorded using a handheld stimulating and recording system. Doc Ophthalmol 137(2):79–86. https://doi.org/10.1007/s10633-018-9652-z
Lapkovska A, Palmowski-Wolfe AM, Todorova MG (2016) Comparing dtl microfiber and neuroline skin electrode in the mini ganzfeld erg. BMC Ophthalmol 16:137. https://doi.org/10.1186/s12886-016-0311-4
Liew G, Mitchell P, Wang JJ, Wong TY (2006) Fundoscopy: To dilate or not to dilate? BMJ 332(7532):3. https://doi.org/10.1136/bmj.332.7532.3
Wood JM, Garth D, Grounds G, McKay P, Mulvahil A (2003) Pupil dilatation does affect some aspects of daytime driving performance. Br J Ophthalmol 87(11):1387–1390. https://doi.org/10.1136/bjo.87.11.1387
Kato K, Kondo M, Sugimoto M, Ikesugi K, Matsubara H (2015) Effect of pupil size on flicker ergs recorded with reteval system: new mydriasis-free full-field erg system. Invest Ophthalmol Vis Sci 56(6):3684–3690. https://doi.org/10.1167/iovs.14-16349
Mobasserian A, Zaidi M, Halim S, Hwang JJ, Regenold J, Akhavanrezayat A, Karaca I, KhojastehJafari H, Yavari N, Matsumiya W, Yasar C, Than NTT, Uludag G, Do D, Ghoraba H, Nguyen QD (2022) Effect of pupil size on fixed-luminance flicker full-field electroretinogram magnitude. Clin Ophthalmol 16:3733–3740. https://doi.org/10.2147/opth.S382207
Wroblewski JJ, McChancy C, Pickel K, Buterbaugh H, Wieland T, Gonzalez A (2020) Reproducibility of fixed-luminance and multi-luminance flicker electroretinography in patients with diabetic retinopathy using an office-based testing paradigm. J Diabetes Sci Technol 14(6):1095–1103
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stanford University has received research support through the availability of the Diopsys® NOVA™ device for research purposes. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Stanford University School of Medicine and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Human rights and statement
This article does not include any studies involving animals conducted by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Regenold, J., Doan, H.L., Ghoraba, H. et al. Evaluation of correlation between Diopsys® NOVA™ fixed-luminance flicker ERG and Diagnosys® Espion 2™ flicker ERG parameters. Doc Ophthalmol 146, 257–266 (2023). https://doi.org/10.1007/s10633-023-09934-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-023-09934-x