Abstract
Purpose
To evaluate the influence of ranibizumab on the multifocal electroretinogram (Mf-ERG), full-field electroretinogram (Ff-ERG) and optical coherence tomography (OCT) in diabetic eyes (n = 20) with macular oedema.
Methods
In 20 eyes (20 diabetic subjects) with no or background diabetic retinopathy and macular oedema (age 65.7 ± 9.8 years, duration 16.5 ± 10.0 years), the change in ETDRS letters, Mf-ERG, Ff-ERG and OCT was analysed, at baseline, 4 weeks after the first injection, (just before the second injection), and 4 weeks after the last injection with ranibizumab.
Results
From baseline, mean BCVA improved from 64.0 ± 10.0 ETDRS letters to 75.0 ± 7.3 ETDRS letters (p = 0.005) 1 month after the last injection. Mean OCT thickness reduced after the first injection from 418 ± 117 to 311 ± 126 µm; (p = 0.001) and to 302 ± 74 µm after the third injection. Mf-ERG demonstrated in the innermost three rings a shorter implicit time after the first injection with p values of 0.002, 0.005 and 0.017, respectively. After the third injection, implicit time was prolonged to almost the original levels. Cone implicit time with 30-Hz flicker improved significantly between baseline (35.5 ± 3.6 ms) and final follow-up (34.6 ± 3.1 ms) (p = 0.04).
Discussion
Though the central retinal thickness was reduced after three injections of ranibizumab and the subjects gained a mean of 11 ETDRS letters, there was no significant change in amplitude or implicit time in Mf-ERG. The shortened 30-Hz flicker implicit time might imply that ranibizumab has no negative impact on the entire peripheral cone function, but can improve it instead.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy (DR), especially diabetic macular oedema, is the leading cause of visual loss in the adult population in the Western world [1].
Photocoagulation was originally the only recommended treatment for clinically significant macular oedema. This therapy reduced moderate vision loss by approximately 50 % [2]. This contrasts with the new anti-VEGF treatment, where visual improvement can be achieved [3]. Recently, as more and more data have accumulated, it has become clearer that anti-VEGF therapy will play an increasing role in the treatment of diabetic macular oedema [2–4].
Growth factors also appear to play a general role in diabetic retinopathy, contributing to retinal ischaemia, microangiopathy and endothelial cell proliferation [5–7]. Ip et al. [8] were able to demonstrate a significant reduction in progression of DR, and a better chance of regression, in eyes treated with ranibizumab as compared to sham-treated eyes. However, the direct influence of anti-VEGF on retinal function, in the macular area as well as at the periphery, is not fully understood. In addition, the reported correlations between increasing macular thickness and visual acuity have been inconsistent; some authors have described a direct negative influence on visual acuity with increasing oedema, while others have not [9–11].
Full-field electroretinography (Ff-ERG) is an objective method for registration of the overall retinal function. In addition, the development of multifocal electroretinography (Mf-ERG) has made it possible to study the macular region more accurately, allowing evaluation of the extent of macular dysfunction in an objective way [12, 13].
The purpose of the present study was to evaluate repeated intravitreal injections with ranibizumab, taking into account medical parameters that might influence the electroretinography responses, both in different macular areas [with a combination of Mf-ERG and optical coherence tomography (OCT)] and in the entire retina (using Ff-ERG).
Materials and methods
Patients
Twenty eyes in 20 consecutive patients with diabetes type II, who regularly attended the outpatient clinic at the Department of Ophthalmology, Lund University, were included in this prospective study. One eye per patient—the one with the worst visual acuity—was chosen and had to fulfil the inclusion criteria: visual acuity <0.7 (Snellen chart), central macular oedema ≥300 µm, measured with OCT, and no previous treatment with argon laser, anti-VEGF therapy or other intravitreal injections. All the examinations were performed between 8:00 and 11:00 a.m.
All 20 patients gave their written consent to participate in the study. The research procedures were performed in accordance with institutional guidelines and the Declaration of Helsinki. Approval for the study was obtained from a local ethics committee and from the Swedish medical products agency.
Medical parameters
At the time of the first examination, we recorded duration of diabetes, blood pressure, whether or not the patients used antihypertensive drugs, type of diabetes treatment and type of diabetes, and we also measured glycosylated haemoglobin (HbA1c). Fasting blood glucose was measured at all three examinations.
Examinations
Three examinations were performed: at baseline, 4 weeks after the first injection (i.e. just before the second injection) and 4 weeks after the last injection.
Visual acuity (Snellen and ETDRS chart), fasting blood glucose, OCT, Mf-ERG and Ff-ERG were measured by an experienced ophthalmologic assistant at all three examinations. In addition, fluorescein angiography was performed at baseline.
The injections
Intravitreal injections of 0.5 mg ranibizumab were given three times, every fourth week, starting within 1 week of the baseline examination.
All patients underwent the same procedure: 0.5 mg ranibizumab was administered at the operating department by an experienced ophthalmologist in a standardized way. This involved thorough rinsing of the eye and cleaning of the area around the eye with saline solution, topical anaesthesia (oxybuprocaine hydrochloride, 0.4 %), topical antibiotic drops (levofloxacin, 5 mg/ml) and finally injection through pars plana into the vitreous cavity. After the procedure, the patients received one more antibiotic drop (levofloxacin, 5 mg/ml).
Classification of retinopathy
A retina specialist who was blinded regarding results diagnosed the level of retinopathy, using fundus photography with a 45° Topcon fluorescein angiography camera [(FA) TRC 501X]. The classification was performed according to the ETDRS [2].
Optical coherence tomography (OCT)
Retinal mapping was performed using the Topcon 3D OCT-1000 standard program for retinal mapping. The OCT software for retinal mapping calculated the mean macular thickness. We examined the central area and the summed response from the middle and outer area (Fig. 1).
Multifocal electroretinography (Mf-ERG)
Multifocal electroretinograms were recorded using a visual evoked response imaging system (VERIS 4; EDI, San Mateo, CA, USA) [13]. The pupils were maximally dilated with 1 % cyclopentolate hydrochloride and phenylephrine hydrochloride. A gold ground electrode was attached to the forehead. Retinal activity was recorded with a gold bipolar contact lens (Hansen Ophthalmic, Iowa City, IA, USA) that was placed on the cornea after anaesthesia with oxybuprocaine. The fixation was controlled using a fundus camera and illumination with infrared light from the recording electrode, with visualization of the hexagonal elements over the retina. The central ring was defined as the summed responses from the first and second rings of the standard Mf-ERG hexagonal pattern. P1 amplitude and implicit time were calculated within the Mf-ERG rings, which corresponded to the three areas measured by the OCT (Ø 6.0 mm) (Figs. 1, 2).
Correlation of macular thickness (by OCT) to Mf-ERG responses
The distance between the foveola and the temporal border of the optic disc is considered to be the length of the radial line used at the OCT examination (3 mm). One millimetre of the radial line corresponds to 4° of the Mf-ERG rings. By superimposing the OCT pattern on the hexagonal pattern from the Mf-ERG registration, hexagons corresponding to the OCT pattern were identified [14] (Fig. 1).
Full-field electroretinography (Ff-ERG)
Full-field ERG was recorded in an Espion Visual Electrophysiology System (Diagnosys LLC, Lowell, MA, USA) according to the standardized protocol for clinical electroretinography by the International Society for Clinical Electrophysiology of Vision (ISCEV), with slight modifications [12]. Responses were obtained with a wide-band filter (−3 dB at 1 and 500 Hz), stimulating with a single full-field flash (30 μs) of blue light (Wratten filters 47, 47A and 47B) and with white light [3.93 (cd × s)/2m]. Cone responses were obtained with 30 Hz flickering white light [0.81 (cd × s)/2m] averaged from 20 sweeps and without any light adaption.
Statistics
Values are given as mean ± standard deviation (SD). Paired t test was used to calculate differences before and after the first injection, and repeated-measures analysis of variance was used to calculate the difference between baseline and after the third injection. Spearman’s rho was used to calculate correlations between parameters. SPSS software version 21 was used for the calculations.
Results
Patient characteristics
All twenty patients, 10 of them men, were classified as having type-2 diabetes, i.e. age over 30 years at onset of diabetes and no requirement for insulin treatment within 2 years of diagnosis. The mean values for the medical parameters at baseline were: age 65.7 ± 9.8 years, duration of diabetes 16.5 ± 10.0 years, HbA1c 56.1 ± 16.1 mmol/mol, systolic and diastolic blood pressure 138.6 ± 11.5 and 76.0 ± 12.4 mmHg, respectively. Fasting blood glucose did not change significantly between the three examinations (Table 1).
Retinopathy
All eyes had non-proliferative diabetic retinopathy (NPDR), with a mean central retinal thickness of 418 ± 117 µm at baseline. The mean diameter of the foveal avascular zone measured by fluorescein angiography was 1.12 ± 0.3 mm, and the area of the foveal avascular zone was 0.7 ± 0.3 mm2.
Visual acuity
Mean ETDRS letters increased from 64.0 ± 10.0 to 75.0 ± 7.3 letters at follow-up (p = 0.005). We also found a significant increase already after the first injection, from 64.0 ± 10.0 to 73.1 ± 7.4 (p < 0.001) (Table 2).
OCT
Mean central OCT thickness decreased after the first injection from 418 ± 117 to 311 ± 126 µm (p = 0.001), and to 302 ± 74 µm after the third injection (Table 3). There was no correlation between the reduction in OCT from baseline to follow-up and change in visual acuity (Fig. 3).
Mf-ERG
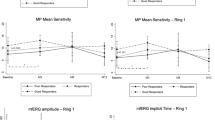
Mf-ERG in all three of the innermost rings showed a shorter implicit time after the first injection, with p values of 0.002, 0.005 and 0.017, respectively (Table 4). After the third injection, implicit time was prolonged almost to the original levels. The amplitude showed the same trend, with a pronounced improvement after the first injection—but with statistical significance only in the central ring (p = 0.04)—and a reduction almost to original levels after the third injection (Table 4; Fig. 4).
No correlation was seen between the decrease in implicit time in the central Mf-ERG ring (0.1 ± 3.2 ms), or the improved amplitude (3.1 ± 6.1 nV/deg2), and the mean reduction in retinal thickness in the central OCT area (116 ± 73 µm) between baseline and after the first injection. There was no correlation between FAZ area and the central ring amplitude or implicit time.
Ff-ERG
Cone implicit time with 30-Hz flicker improved significantly between baseline (35.5 ± 3.6 ms) and follow-up (34.6 ± 3.1 ms) (p = 0.04) (Table 5; Fig. 5).
Rod amplitude also improved between start and after the third injection, but this was not statistically significant (185.6 ± 53.4 and 191.8 ± 44.1 µV, respectively). There was also no significant change in amplitude between baseline and after the first injection (3.7 ± 46.9 µV) (Table 5).
Discussion
Several studies have found improvement in visual acuity and reduction in central retinal thickness after injections of ranibizumab in patients with diabetic macular oedema [3, 4]. The current standard methods for evaluation of the efficacy of a given treatment for diabetic macular oedema are visual acuity and OCT.
Full-field ERG and Mf-ERG are techniques that objectively reflect retinal function. To our knowledge, no one has examined the effect of ranibizumab with Mf-ERG and also with Ff-ERG.
In the present study, we found a significant decrease in 30-Hz flicker implicit time 1 month after the third injection of ranibizumab (Fig. 5). Changes in 30-Hz flicker have been described in other retinal diseases such as central vein occlusion, and after surgery for retinal detachment. In central vein thrombosis, a correlation between retinal ischaemia and delayed 30-Hz flicker implicit time has been shown, whereas after surgical re-attachment of a detached retina, a tendency towards shorter 30-Hz flicker implicit time has been found [15–17].
These studies may indicate that an increased 30-Hz flicker implicit time indicates damaged cone function of the entire retina, either in the form of ischaemia or in the form of a detached retina. Pedersen et al. [18] examined the effect on the electroretinogram after injections of bevacizumab in patients with age-related macular degeneration (AMD). They found significant improvement in the implicit time of the cone flicker response at 6-month follow-up. Others have found no evidence of changes in cone system function over 48 weeks with ranibizumab injections in diabetic patients [19].
Some studies have shown less progression of diabetic retinopathy after injections with ranibizumab, and it is possible that the reduced 30-Hz implicit time at follow-up in the present study may indicate that ranibizumab has no negative effect on the entire peripheral cone function, but can improve it instead [20]. However, the results of our study must be viewed with caution because of the small sample size. The combined cone–rod response (white light) and also the rod response (blue light) improved at follow-up—both amplitude and implicit time—but neither of the responses were statistically significant. This may have been due to the small sample size.
In all three Mf-ERG rings, we found the same pattern: an improvement in amplitude and a reduced implicit time after the first injection, corresponding to a reduction in retinal thickness. Interestingly, 1 month after the third injection, despite a continuous decrease in retinal thickness and an improvement in visual acuity, we found a return to levels approaching baseline levels. In contrast, in AMD, Pedersen et al. [18] found a significant improvement in the central retinal amplitude lasting up to 6 months after the first injection [18]. However, the different pathogenesis of diabetic maculopathy and AMD must also to be taken into consideration when evaluating the Mf-ERG. Consideration must also be given to the lack of a control group, and thus we have no knowledge about the natural variations.
In the present study, the improvement in the Mf-ERG amplitudes and the shortening of the Mf-ERG implicit time between baseline and the second examination did not reach statistical significance; nor did the worsening of the amplitude and implicit time between the second examination and follow-up. This could be due to the number of patients being small. But, the trend, with improvement in the Mf-ERG amplitudes and shortened implicit times after the first injections, and a return to almost initial values, was seen in all Mf-ERG rings even though the central retinal thickness continued to decrease even after the third injection. We only analysed the macular oedema quantitatively and not morphologically.
The main reduction in oedema was seen after the first injection, and after the two following injections, we could only see a minor reduction. It has been speculated that it is possible to misinterpret a degeneration of photoreceptors as a remaining macular oedema [21]. According to this, we may have treated a dry macula at the second injection. This could explain the tendency of reduced amplitude and prolonged implicit time.
The fasting blood glucose level may have influenced the Mf-ERG results, as Klemp et al. [22] reported, but we did not find any differences in blood glucose levels between the examinations.
Several authors have reported improvement in visual acuity and reduction in central retinal thickness after injections with ranibizumab. Neither the correlation between visual acuity and Mf-ERG results nor the correlation between central retinal thickness and Mf-ERG results is especially clear [10, 18]. A possible explanation to the return of the Mf-ERG responses almost to baseline at follow-up could be a tendency to develop geographic atrophy, which Grunwald et al. [23] described as an adverse effect of treating AMD with anti-VEGF.
It is therefore of great importance to improve our understanding of diabetic macular oedema so that we can develop more detailed recommendations regarding when to start treatment and when not to start treatment. Electroretinography is an objective way to continue this work. We plan to expand the study by including more patients in future.
References
Moss SE, Klein R, Klein BEK (1988) The incidence of vision loss in a diabetic population. Ophthalmology 95:1340–1348
Early Treatment Diabetic Retinopathy Study Research Group (1985) Photocoagulation for diabetic macular oedema: ETDRS report number 1. Arch Ophthalmol 103:1796–1806
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, Sutter F, Simader C, Burian G, Gerstner O, Weichselberger A, RESTORE study group (2011) The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 118(4):615–625
Massin P, Bandello F, Garweg JG, Hansen LL, Harding SP, Larsen M, Mitchell P, Sharp D, Wolf-Schnurrbusch UE, Gekkieva M, Weichselberger A, Wolf S (2010) Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE study): a 12-month, randomized, controlled, double- masked, multicenter phase II study. Diabetes Care 33(11):2399–2405
Grant MB, Afzal A, Spoerri P, Pan H, Shaw LC, Mames RN (2004) The role of growth factors in the pathogenesis of diabetic retinopathy. Expert Opin Investig Drugs 13(10):1275–1293
Ferrara N (2004) Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev 25(4):581–611
Tolentino MJ, Miller JW, Gragoudas ES, Jakobiec FA, Flynn E, Chatzistefanou K, Ferrara N, Adamis AP (1996) Intravitreous injections of vascular endothelial growth factor produce retinal ischemia and microangiopathy in an adult primate. Ophthalmology 103(11):1820–1828
Ip MS, Domalpally A, Hopkins JJ, Wong P, Ehrlich JS (2012) Long-term effects of ranibizumab on diabetic retinopathy severity and progression. Arch Ophthalmol 130(9):1145–1152
Nunes S, Pereira I, Santos A, Bernardes R, Cunha-Vaz J (2010) Central retinal thickness measured with HD-OCT shows a weak correlation with visual acuity in eyes with CSME. Br J Ophthalmol 94(9):1201–1204
Holm K, Larsson J, Lövestam-Adrian M (2007) In diabetic retinopathy, foveal thickness of 300 µm seems to correlate with functionally significant loss of vision. Doc Ophthalmol 114(117–124):14
Alasil T, Keane PA, Updike JF, Dustin L, Ouyang Y, Walsh AC, Sadda SR (2010) Relationship between optical coherence tomography retinal parameters and visual acuity in diabetic macular edema. Ophthalmology 117(12):2379–2386
Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M (2009) Standard for clinical electroretinography (2008 update). Doc Ophthalmol 118:69–77
Hood DC, Bach M, Brigell M, Keating D, Kondo M, Lyons JS, Marmor MF, McCulloch DL, Palmowski-Wolfe AM (2012) ISCEV standard for clinical multifocal electroretinography (2011 edition). Doc Ophthalmol 124:1–13
Holm K, Ponjavic V, Lövestam-Adrian M (2010) Using multifocal electroretinography hard exudates affect macular function in eyes with diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 248:1241–1247
Kjeka O, Bredrup C, Krohn J (2007) Photopic 30 Hz flicker electroretinography predicts ocular neovascularization in central retinal vein occlusion. Acta Ophthalmol Scand 85(6):640–643
Larsson J, Bauer B, Andréasson S (2008) The 30-Hz flicker cone ERG for monitoring the early course of central retinal vein occlusion. Doc Ophthalmol 117(2):103–109
Gong Y, Wu X, Sun X, Zhang X, Zhu P (2008) Electroretinogram changes after scleral buckling surgery of retinal detachment. Doc Ophthalmol 117(2):103–109
Pedersen KB, Möller F, Sjölie AK, Andréasson S (2010) Electrophysiological assessment of retinal function during 6 months of bevacizumab treatment in neovascular age-related macular degeneration. Retina 30:1025–1033
Comyn O, Sivaprasad S, Peto T, Neveu MM, Holder GE, Xing W, Bunce CV, Patel PJ, Egan CA, Bainbridge JW, Hykin PG (2014) A randomized trial to assess functional and structural effects of ranibizumab versus laser in diabetic macular edema (the LUCIDATE study). Am J Ophthalmol 157:960–970
Schmidt-Erfurth U, Lang GE, Holz FG, Schlingemann RO, Lanzetta P, Massin P, Gerstner O, Bouazza AS, Shen H, Osborne A, Mitchell P; RESTORE Extension Study Group (2014) Three-year outcomes of individualized ranibizumab treatment in patients with diabetic macular edema: the RESTORE extension study. Ophthalmology 121(5):1045–1053
Lee JY, Folgar FA, Maguire MG, Ying GS, Toth CA, Martin DF, Jaffe GJ, CATT Research Group (2014) Outer retinal tubulation in the comparison of age-related macular degeneration treatments trials (CATT). Ophthalmology 121(12):2423–2431
Klemp K, Larsen M, Sander B, Vaag A, Brockhoff PB, Lund-Andersen H (2004) Effect of short-term hyperglycemia, on multifocal electroretinogram in diabetic patients without retinopathy. Invest Ophthalmol Vis Sci 45(10):3812–3819
Grunwald JE, Daniel E, Huang J, Ying GS, Maquire MG, Ca Toth, Jaffe GJ, Fine SL, Blodi B, Klein ML, Martin AA, Hagstrom SA, Martin DF, CATT Research Group (2014) Risk of geographic atrophy in the comparison of age-related macular degeneration treatments trials. Ophthalmology 121(1):150–161
Acknowledgments
This study was supported by Novartis Sweden AB.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holm, K., Schroeder, M. & Lövestam Adrian, M. Peripheral retinal function assessed with 30-Hz flicker seems to improve after treatment with Lucentis in patients with diabetic macular oedema. Doc Ophthalmol 131, 43–51 (2015). https://doi.org/10.1007/s10633-015-9495-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-015-9495-9