Abstract
Background
Treatment of hepatitis C virus (HCV) has been dramatically improved with the introduction of direct-acting antiviral agents (DAAs). Universal access to pangenotypic DAAs was provided in France from 2017, expanding the type of patients treated. Real-world studies are important to confirm effectiveness and safety in clinical practice, particularly in vulnerable populations.
Aims
To assess real-world effectiveness and safety of sofosbuvir-based therapy in adults with chronic HCV infection before and after universal access to DAAs in France.
Methods
This multicenter, non-interventional, prospective study assessed the effectiveness, safety, patient-reported outcomes and adherence with sofosbuvir-based regimens from October 2015 to July 2016 (Period 1: sofosbuvir-based therapy excluding sofosbuvir/velpatasvir) and from October 2017 to July 2018 (Period 2: pangenotypic sofosbuvir/velpatasvir-based therapy).
Results
Baseline data were documented for 1029 patients. Overall, 797 (77%) had sustained virologic response data available ≥ 9 weeks after treatment completion. Per protocol response was high (97%) irrespective of age, alcohol consumption, recreational drug use, or HIV/HCV coinfection. Adverse events occurred in approximately 25% of patients with the majority experiencing Grade 1 or 2 events. Sofosbuvir-based regimens improved health-related quality of life from baseline to end of treatment in patients with data at all timepoints. Overall, 99% of patients reported total or almost total adherence to therapy.
Conclusions
Sofosbuvir-based therapy, including pangenotypic sofosbuvir/velpatasvir, is effective for the treatment of HCV in real-world clinical practice. This is an important step towards HCV elimination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) is a major health issue: 71 million individuals are chronically infected with HCV [1] and 700,000 HCV-related deaths occur annually worldwide [2]. HCV is a systemic disease associated with both hepatic and extrahepatic manifestations and represents a substantial burden to both the patient and society [3]. Patients chronically infected with HCV report poor health-related quality of life (HRQoL), fatigue and reduced work productivity [4,5,6].
Treatment of patients chronically infected with HCV substantially improved with the introduction of direct-acting antiviral agents (DAAs) [7, 8] in 2013. Sofosbuvir (SOF) has become the backbone of multiple interferon (IFN)-free HCV treatment regimens [9]. Data from clinical trials have demonstrated that SOF, either with ribavirin (RBV) alone or as a fixed-dose combination with other DAAs, such as ledipasvir (LDV) [10,11,12] or velpatasvir (VEL) [13, 14], achieves a sustained virologic response (SVR) and is able to cure HCV in at least 90% of patients, including those historically considered difficult to treat, such as patients with decompensated cirrhosis [15], those coinfected with human immunodeficiency virus (HIV) [16, 17] and people who inject drugs [18, 19]. With high efficacy and a favorable tolerability profile, DAAs have revolutionized the management of HCV and are recommended by the World Health Organization (WHO) to enable elimination of HCV [20]. Introduction of the WHO targets along with the rapid evolution of DAAs, including availability of pangenotypic regimens such as SOF/VEL, has allowed the development of simplified HCV management strategies in a diverse range of populations with chronic HCV infection [21,22,23].
In France, DAA therapy was initially only available to patients with severe liver disease before gradual changes to national policy allowed the treatment of all patients regardless of fibrosis or genotype, meaning that the patient profile receiving HCV treatment has changed considerably since 2013. In 2017, pangenotypic regimens including SOF/VEL, which is the most frequently prescribed therapy in France, became widely available and allowed simplified management and treatment of HCV.
Real-world studies are important for confirming effectiveness and tolerability in patient populations in routine clinical practice, as well as providing information on patient management and the long-term effects of therapy [24]. Results from several real-world studies conducted in the USA and Europe support the effectiveness of SOF-based regimens observed in clinical trials [25,26,27,28,29,30,31,32,33,34,35,36,37]. Knowledge of the long-term efficacy and safety profiles of DAAs, and their impact on adherence and patient-reported outcomes (PROs) in daily practice, is still evolving, especially in specific high-risk patients such as those using recreational drugs, receiving opioid substitution therapy (OST) or consuming excessive alcohol (≥ 3 units/day).
The aim of the HEpatitis C real-LIfe study for patients On Sofosbuvir (HELIOS) was to assess real-world effectiveness, safety, adherence and PROs with SOF-based therapy in France. The objective was to assess changes in patient characteristics during the two assessment periods and investigate the outcomes of evolving therapeutic strategies, including the introduction of pangenotypic regimens, as recommended by guidelines throughout the DAA era.
Methods
Design
HELIOS was a multicenter, non-interventional, prospective study to assess the effectiveness and safety profile of SOF-based regimens in patients (≥ 18 years of age) with chronic HCV managed in routine clinical settings in France. The study was conducted in accordance with good pharmacoepidemiology guidelines, pharmacovigilance practice guidelines, and the 1964 Helsinki Declaration; initially authorized by the Advisory Committee on the Treatment of Research Information (CCTIRS) and the Data Protection Committee (CNIL), the second recruitment period was authorized by a central ethics committee, in accordance with new French Regulations on research Involving Human Beings.
Setting and Patients
Recruitment took place over two periods in 46 centers across France October 2015–July 2016 (Period 1) and October 2017–July 2018 (Period 2). Participating physicians enrolled eligible patients in whom they planned to initiate SOF-based therapy for 8–24 weeks according to local recommendations (Period 1: LDV/SOF ± RBV, SOF ± RBV, SOF + DCV ± RBV, or SOF + SMV ± RBV; Period 2: SOF/VEL ± RBV). Treatment was prescribed at the physician’s discretion. Study drugs were not provided by the sponsor.
Initially, the number of patients enrolled per center was limited to 10 to prevent any site bias in the study; however, to ensure all patients were recruited within the planned period, the number of patients per site was increased in Period 2. A limited number of sites involved in Period 1 decided not to participate in Period 2.
Participating sites primarily specialized in hepato-gastroenterology, infectious diseases or internal medicine to provide a representative cross section of current practice in France.
Study Assessments and Data Collection
Informed consent was obtained from all individual participants included in the study; permission was given for the collection of anonymized medical data from their medical files. Prospective data were recorded at baseline, end of treatment (EOT) and post-treatment Week 12. To reflect the reality of clinical practice, the HELIOS Scientific Committee agreed to accept SVR values if they were available from ≥ 9 weeks after completion of treatment. Data were collected from medical records using electronic case report forms and questionnaires completed by patients. Patient demographics, medical history, presence of extrahepatic manifestations, liver-related parameters and routine laboratory parameters were collected, as well as treatment-specific variables (genotype, treatment history, prescribed treatment and treatment duration). The cutoff values for fibrosis assessments are described in Supplementary Table 1. PROs were collected using standard instruments: HRQoL was assessed with the EuroQOL five dimensions (EQ-5D) questionnaire, and impairment in functioning was assessed using the work productivity and activity impairment (WPAI) questionnaire. During the post-treatment follow-up period, any patient who initiated a new HCV treatment was no longer followed up within this study (except for safety events occurring within 30 days of study HCV regimen discontinuation).
Endpoints
The primary endpoint of the analysis was to assess effectiveness of SOF-based therapies through the proportion of subjects achieving SVR, defined as HCV ribonucleic acid (RNA) < 25 IU/mL (lower limit of quantification). Plasma HCV RNA was quantified using locally available assays. HCV RNA values were collected at the closest time point to the anticipated date 12 weeks from the end of treatment for each patient. All patients who received at least one dose of SOF-based therapy and had a post-baseline effectiveness or safety assessment were included in the overall population. The per protocol (PP) population excluded patients lost to follow-up, patients who initiated a new HCV treatment, and patients who completed the study but had missing HCV RNA assessment for SVR at ≥ 9 weeks after completion of treatment.
Secondary endpoints included assessment of tolerability, safety, adherence and impact on HRQoL. Patient adherence to HCV treatment was assessed using a self-reported questionnaire. Adherence was scored from 0 (not followed treatment at all) to 10 (no drug dose missed). HRQoL was assessed using the self-reported EQ-5D questionnaire at baseline, EOT and post-treatment Week 12. Only patients with values at all visits were included in these analyses. Both the EQ-5D descriptive and visual analog scale (VAS) were administered. In the EQ-5D descriptive system, patients indicated their health state in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Patients were asked to indicate which statements best described their health state on the day of the assessment in each of the five dimensions with scores ranging from 1 to 5 (worst to best health state, respectively). The EQ-5D index was calculated from this score, with a higher index indicating a better health state. The EQ-5D score corresponds to the result of the EQ-5D VAS ranging from 0 to 100 (worst to best health state). Impairment in functioning was assessed using the self-reported WPAI questionnaire at baseline, EOT and post-treatment Week 12; this instrument quantifies impairment in the patient’s work productivity and daily activities that the patient considers to be a consequence of a specific health problem (i.e., HCV infection). The WPAI has two dimensions. The work productivity impairment dimension is a sum of impairment in work productivity due to missed work hours (absenteeism) and decreased productivity while working (presenteeism); this dimension is only assessed in employed patients. The second dimension relates to activity impairment (i.e., daily activities other than work) and is assessed regardless of employment. Both dimensions of the WPAI are inversely related to health status with a greater impairment indicating worse health. The safety analysis included all treated patients, and safety endpoints included adverse events leading to permanent discontinuation of treatment.
Statistical Analysis
Mean, 95% confidence intervals (CIs), standard deviation (SD), median, first and third quartile (Q1, Q3) range, minimum and maximum were calculated for continuous variables. For categorical variables, the number and percentage of patients were reported. Comparative analyses were performed using the chi-square test and/or Fisher’s exact tests for qualitative variables; t tests for analyses of variance were performed for quantitative variables. Non-parametric tests were used in the case of a non-normal distribution. Univariate and multivariate regression analyses were employed to identify predictors of SVR adjusting for covariates (value at inclusion) as appropriate.
Mixed model analysis was used to identify predictors of the EQ-5D index at selected study visits adjusting for covariates as appropriate, and to compare EQ-5D scores between visits. Covariates included patient age, sex, race, body mass index, presence of extrahepatic manifestations, current addiction, prior HCV treatment, treatment regimen, hepatocellular carcinoma (HCC), presence of comorbidities, employment status, previous liver transplant and RBV use (at baseline, EOT and post-treatment Week 12). A step-by-step backward selection of predictors was used to remove non-specific covariates. However, visit, age, sex and ethnicity were forced into the model based on the literature. Sensitivity analyses were performed with missing values imputed using a multivariate imputation by chained equations (MICE) algorithm. Statistical analysis was performed using the SAS v9.2 statistical software package. See the Supplementary Appendix for additional details on the statistical analyses performed.
Results
Baseline Characteristics
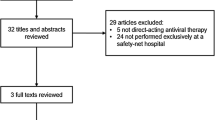
Overall, 1041 patients were prospectively screened and enrolled; of these, 1029 patients had a baseline visit documented and were included in analysis of the overall population (Table 1). Patients received SOF-based treatment for 8–24 weeks; most were treated for 12 weeks without RBV. Among the patients included in the overall population analysis, 1000/1029 (97%) completed treatment and 725/1029 completed the study (Fig. 1).
Patients included in the HELIOS study. Flow diagram describing the number of people with HCV screened, enrolled, completed treatment and completed the full study protocol including follow-up. *Nine cases of lack of effect, five cases of reinfection, one patient ceased study treatment and initiated an alternative HCV therapy. †Two cases of lack of effect, one case of reinfection. SVR sustained virologic response
Patients enrolled into the HELIOS study were predominantly male, Caucasian and non-cirrhotic, with a median age (range) of 56 (20–91) years in Period 1 and 53 (24–83) years in Period 2. Over both periods, 28% of patients had at least one comorbidity (Table 1). The mean (range) number of concomitant medications was 2.1 (0–32) in Period 1 and 3.0 (1–32) in Period 2; 7% of patients in both Period 1 and Period 2 used proton pump inhibitor (PPI) medication (Table 1).
Notable numerical differences between patients in Period 2 versus Period 1 were: a higher proportion of genotype 3 patients; a lower proportion of genotype 1 patients; less severe fibrosis stage (F); a higher proportion of treatment-naïve patients; fewer extrahepatic manifestations; fewer patients with HIV/HCV coinfection; and a greater proportion of patients reporting excessive alcohol consumption and/or recreational drug use or receiving OST (Table 1).
Effectiveness Endpoints
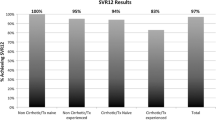
Of the 1029 patients enrolled in the study, 797 (77%) had SVR assessment ≥ 9 weeks after completion of treatment and were included in the PP analysis. SVR results were available for 567/624 (91%) in Period 1 and 230/405 (57%) in Period 2. Baseline characteristics such as fibrosis stage, current drug abuse, excessive alcohol consumption, HIV/HCV coinfection, ≥ 3 comedications and treatment with PPIs were not predictive of availability of SVR results in Period 1. However, current drug use (P < 0.001) and excessive alcohol consumption (P = 0.031) were predictive for no HCV RNA assessment during Period 2.
Overall, 97.0% (773/797) of patients in the PP population achieved an SVR, including 97.8% (490/501) for LDV/SOF ± RBV; 99.6% (226/227) for SOF/VEL ± RBV; and 100% (226/226) for SOF/VEL without RBV. SVR rates of 97.3% (330/339) and 97.4% (222/228) were achieved in Period 1 and 99.4% (175/176) and 100% (54/54) in Period 2 in treatment-naïve and treatment-experienced patients, respectively. High response rates were achieved irrespective of treatment regimen, treatment duration and genotype (Table 2).
According to univariate analysis, SVR rates were high irrespective of age, alcohol consumption, recreational drug use or HIV/HCV coinfection during both periods of the study (Supplementary Table 2).
Safety Endpoints
Overall, 27% of patients in Period 1 and 16% of patients in Period 2 experienced treatment-emergent adverse events (TEAEs). The most common TEAEs are listed in Table 3 and were in accordance with expected adverse events described in the summary of product characteristics of SOF-containing regimens. Early treatment discontinuation due to TEAEs in Period 1 was reported in two patients (asthenia and pruritus) and 19 patients changed dose or interrupted treatment due to TEAEs (12 anemia, two asthenia, two irritability, one insomnia, one affective disorder, one sleep disorder, one hepato-renal syndrome, one hemoglobin decreased, one headache, one pain in extremity). Two patients developed serious TEAEs (one black stool and one hepato-renal syndrome). There were seven deaths in Period 1: one treatment-emergent case of hepato-renal syndrome in the LDV/SOF group and six (HCC, heart failure, cardiac arrest, traffic accident, infectious bilateral pneumonitis and septic shock) not related to antiviral treatment.
In Period 2, early treatment discontinuation due to TEAEs was reported in one patient (experiencing drug interaction, buprenorphine overexposure and alteration of the general condition). No patients changed dose or interrupted treatment due to TEAEs or developed serious TEAEs; there were three deaths (pulmonary adenocarcinoma, alteration of the state of health and acute liver failure) not related to antiviral treatment.
Patient-Reported Outcomes
A total of 459 patients in Period 1 and 223 patients in Period 2 had data available at baseline, EOT and post-treatment Week 12. Overall, PROs improved from baseline to EOT and further to post-treatment Week 12, including EQ-5D score (Fig. 2) calculated from the EQ-5D VAS. Overall, fewer patients reported moderate or severe problems in each of the EQ-5D dimensions at post-treatment Week 12 compared with baseline (Fig. 3). Results were largely comparable in those patients with data available at all three visits compared with those with at least one missing visit (Supplementary Tables 3 and 4). Findings from multivariate regression analyses of predictive factors for HRQoL are reported in Tables 4 and 5. In Period 1, lack of employment at baseline and extrahepatic manifestations at baseline were adversely associated with HRQoL across all five dimensions of the EQ-5D (P < 0.01 for all dimensions). Addiction at baseline also negatively affected HRQoL across all dimensions of the EQ-5D except “self-care.” Ethnicity negatively affected HRQoL across all dimensions of the EQ-5D except “anxiety/depression” (P = 0.5027). BMI, therapeutic strategy and RBV use had no effect in any dimension of EQ-5D. In Period 2, lack of employment at baseline adversely associated with HRQoL across all dimensions of the EQ-5D. Extrahepatic manifestations at baseline negatively affected HRQoL across all dimensions of the EQ-5D except “self-care.” Addiction, prior HCV treatment, HCC, comorbidity, previous liver transplant and RBV use had no effect in any dimension of EQ-5D. Overall, work productivity and regular daily activity improved over both periods with more patients reporting lower impairment scores (i.e., better health status) at EOT and post-treatment Week 12 compared with baseline (Fig. 4).
EQ-5D score in patients with values at baseline, end of treatment and post-treatment Week 12. The EQ-5D score corresponds to the result of the EQ-5D questionnaire VAS ranging from 0 (worst health state) to 100 (best health state). SD is shown in brackets. EOT end of treatment, EQ-5D EuroQOL five dimensions, VAS visual analog scale
Proportion of patients with values at baseline, end of treatment and post-treatment Week 12 reporting moderate or severe problems in each of the EQ-5D dimensions (pain/discomfort, anxiety/depression, usual activities, mobility, self-care) at baseline, end of treatment and post-treatment Week 12 in (a) Period 1 (N = 624) and in (b) Period 2 (N = 405). Fewer patients reporting problems in the EQ-5D dimensions from baseline to post-treatment Week 12 indicate improvement in health-related quality of life. EOT end of treatment, EQ-5D EuroQOL five dimensions
Work productivity and activity impairment (WPAI) score for a work productivity at baseline (n = 329), end-of-treatment (n = 257) and post-treatment Week 12 (n = 250) in Period 1, b regular daily activity at baseline (n = 610), end of treatment (n = 510) and post-treatment Week 12 (n = 487), in Period 1, c work productivity at baseline (n = 168), end-of-treatment (n = 140) and post-treatment Week 12 (n = 133) in Period 2, and d regular daily activity at baseline (n = 389), end of treatment (n = 283) and post-treatment Week 12 (n = 256) in Period 2. The WPAI score corresponds to the result of the WPAI questionnaire ranging from 0 (the least affected by HCV is the productivity at work in the last 7 days) to 10 (the most affected by HCV is the productivity at work in the last 7 days). Note Results are presented for patients that stated in the WPAI questionnaire that they were employed at each visit (282 patients at baseline, 247 patients at EOT and 221 patients at post-treatment Week 12 in Period 1; 168 patients at baseline, 148 patients at EOT and 140 patients at post-treatment Week 12 in Period 1). Patients with missing data were excluded from the analysis. The WPAI regular activity score corresponds to the result of the WPAI questionnaire ranging from 0 (the least affected by HCV are the regular daily activities in the last 7 days) to 10 (the most affected by HCV are the regular daily activities in the last 7 days). EOT end of treatment, HCV hepatitis C virus
Adherence
Overall, 99% (816/825) of patients reported that they totally or almost totally followed the prescription. At EOT, 96% (784/820) were ≥ 80% adherent. In the univariate analysis of Period 1, male sex (P = 0.0069), Black race (P = 0.0065), addiction (P < 0.001), RBV use (P = 0.0255), current unemployment (P = 0.0064) and cirrhosis (P = 0.0170) were predictive of treatment adherence < 80%. In the subsequent multivariate analysis, male sex (P = 0.0099), addiction (P = 0.0014), Black race (P = 0.0081) and current unemployment (P = 0.0017) remained predictive. No baseline characteristics were predictive of adherence < 80% in the univariate or multivariate analysis of Period 2.
Discussion
HELIOS demonstrated an SVR rate of 97% using SOF-based regimens in a diverse real-world cohort including patients with multiple comorbidities, excessive alcohol consumption and/or recreational drug use. Treatment was generally well tolerated with few discontinuations due to adverse events. The findings were consistent with the virologic cure rates and safety profiles of SOF-based regimens observed in Phase 3 studies and other real-world cohorts [11, 18, 28,29,30, 32,33,34,35,36,37,38]. Genotype, treatment regimen, treatment duration, treatment history, PPI use and OST use had no effect on SVR. Furthermore, response rates were high irrespective of age, alcohol consumption, recreational drug use or HIV/HCV coinfection. The results highlight that vulnerable patient populations can achieve high cure rates despite factors historically associated with poor response to IFN-based treatment. This is in agreement with published studies reporting no differences in SVR in populations such as HIV/HCV or HBV/HCV coinfection, chronic kidney disease or people who inject drugs [39,40,41,42] and supports current recommendations to prescribe pangenotypic regimens to all patients infected with chronic HCV, regardless of liver disease severity or lifestyle [22].
Phase 3 studies have reported improvements in PROs with SOF-based therapies [43,44,45,46,47]; however, real-world data to support clinical findings are scarce. The data from HELIOS indicate that the use of SOF-based regimens leads to significant improvement in HRQoL from baseline to EOT and beyond as measured by the EQ-5D and WPAI, both validated instruments for assessing PROs. Presence of extrahepatic manifestations and employment status, addiction and ethnicity were independent predictors of HRQoL impairment with some SOF-based regimens. Presence of such predictors should also be considered when initiating HCV treatment in these patient groups to help inform caregivers of potential challenges.
HELIOS also provides insight into real-world adherence and treatment outcomes among a heterogeneous population. Overall adherence was high across this diverse group of patients, suggesting that perceptions regarding treating certain patient groups such as recreational drug users, patients on OST or those consuming excessive alcohol might be unfounded. Decisions regarding access to treatment by drug and alcohol users should be made according to clinical and public health requirements rather than coexisting disorders such as addiction [47]. Factors such as addiction, male sex and current unemployment were identified as independent predictors of poor treatment adherence in Period 1, when pangenotypic regimens such as SOF/VEL were not available. Baseline factors such as sex, employment status and substance abuse have previously been identified as predictors of suboptimal adherence in non-pangenotypic regimens [48, 49] and should be considered by healthcare professionals when initiating such HCV treatments in these patient groups. Conversely, no baseline factors included in the analysis were predictive of poor adherence to SOF/VEL ± RBV in Period 2, providing further evidence that the use of pangenotypic regimens may be considered for simplified treatment, regardless of patient population. This is particularly important when prescribing treatment in injecting drug users, a population that has been identified as key if HCV elimination is to be achieved [50]. However, appropriate individual support should be offered to those who may have chaotic lifestyles, including moderate to heavy alcohol use and require additional assistance to ensure appropriate adherence [51].
This prospective, observational study showed differences in the populations receiving DAA therapy for HCV infection in France between October 2015 and July 2018 after it became one of the first European countries to commit to goals to eliminate HCV. On their introduction in 2013, prescription of DAAs was initially restricted to patients with severe disease such as those with F3/F4 liver fibrosis, liver transplant or HCV/HIV coinfected, with management in the specialist setting, reflective of Period 1 of HELIOS. By 2016, DAA prescription was extended to historically difficult-to-treat patients (genotype 3) and those with F2 liver fibrosis. In 2017, DAA reimbursement was extended to all HCV patients, including those with F0/F1 liver fibrosis; in 2019, prescription of DAAs was extended to non-specialists. Availability of simple, pangenotypic regimens has allowed an expanded focus on vulnerable populations infected with HCV, making HCV elimination a realistic goal. As such, the study population in Period 2 had a wider distribution of genotypes, less severe fibrosis stage at baseline, a higher proportion of treatment-naïve patients and fewer patients with extrahepatic manifestations or HIV/HCV coinfection. Additionally in Period 2, there were more reports of current excessive alcohol consumption and/or current recreational drug use and OST use, reflecting improved access to HCV treatment. The proportion of patients completing the study was higher in Period 2 (87%) than in Period 1 (59%), suggesting that simplified management with pangenotypic regimens resulted in fewer patients being retained within care to the end of follow-up. The baseline characteristics of patients enrolled during the two periods can again provide an indication of why fewer patients were retained in care up to the end of the follow-up period in Period 2. The high number of patients with serious liver disease in Period 1 means that these patients would be carefully retained in care to ensure that they achieved a favorable outcome. In contrast, the broader patient population included in Period 2, especially those with a history of alcohol or drug use, is recognized as a factor influencing engagement with care [40]. However, the successful initiation of therapy in this group is encouraging and, given the high response rates with these regimens, many patients will have been cured even if this is not captured during follow-up assessments.
The current study has several limitations. In a non-interventional study, all decisions on patient management are made solely by the treating physician. As such, some data or visits may be missing or visits delayed. In addition, selection bias for patient recruitment cannot be completely ruled out. Physicians at the recruiting sites might have selected one patient in preference to another owing to the small number of patients included per site. However, because of the large number of sites involved, no changes in overall results of the study were expected. To get a good representation of the patients treated with SOF-based regimens in France, sites were selected from all over the French metropolitan territory, including university hospitals, general hospitals and private practice. However, non-inclusion criteria de facto excluded some patients from the study, and patients at risk of not being available for follow-up over the 2-year course of the study were unlikely to be enrolled. In this study, 1029 patients were enrolled and 885 patients were included in the PP analysis at post-treatment Week 12. The remaining 144 patients were excluded due to loss to follow-up or because data relating to HCV RNA were unavailable at the time of analysis for SVR. This reflects everyday clinical practice; however, the proportion of patients with missing data could compromise the effectiveness analysis and the relationship between effectiveness and HRQoL. Although the baseline demographics of patients with and without data relating to HCV RNA at the SVR time point were similar in Period 2, the proportion of patients with experience of addiction was higher in the group without SVR data than the group with SVR data in Period 1. This further highlights the need to ensure appropriate treatment choice and support is given to optimize engagement and adherence among vulnerable populations. With many clinical studies reporting the effectiveness of pangenotypic regimens in up to 99% of patients [13, 14, 52,53,54,55], including a high rate of SVR in those without full adherence to therapy [56], clinical practice is evolving to redefine the parameters of success in HCV treatment. If adequate compliance is attained, which has been reported in diverse populations, it could be assumed that SVR is achieved in the majority of patients and HCV RNA assessment post-treatment may not be needed for some patients. Thus, simplification of HCV care with pangenotypic regimens reduces the burden of healthcare utilization for both the patient and healthcare professionals. With less focus on patient management after HCV diagnosis and linkage to care, more resources can be used to identify people who are unaware of their HCV status and maintain momentum towards achieving HCV elimination.
In conclusion, SOF-based regimens are associated with high response rates, favorable safety profiles, as well as improvements in parameters associated with HRQoL. The effectiveness and safety results with these regimens in clinical practice are similar to the efficacy reported in clinical trials. Data from HELIOS support the findings from clinical studies and demonstrate benefits of achieving an SVR beyond the liver. The study puts the evolution of DAA therapy into perspective, seeing the added benefits of pangenotypic regimens since they became universally available in France in 2017, with SOF/VEL the most frequently prescribed regimen at the time of writing. Continued use of simplified HCV management algorithms, multistakeholder engagement with care and bringing national policy in line with evidence-based recommendations, France is on track for eliminating HCV in line with WHO targets.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AP-HP:
-
Assistance Publique-Hôpitaux de Paris
- BMI:
-
Body mass index
- CCTIRS:
-
Comité consultatif sur le traitement de l’information en matière de recherche
- CI:
-
Confidence interval
- CNIL:
-
Commission nationale de l’informatique et des libertés
- DAA:
-
Direct-acting antiviral agent
- DCV:
-
Daclatasvir
- EOT:
-
End of treatment
- EQ-5D:
-
EuroQOL five dimensions
- F:
-
Fibrosis stage
- GT:
-
Genotype
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HRQoL:
-
Health-related quality of life
- HELIOS:
-
HEpatitis C real-LIfe study for patients On Sofosbuvir
- HIV:
-
Human immunodeficiency virus
- IFN:
-
Interferon
- LDV:
-
Ledipasvir
- LLOQ:
-
Lower limit of quantification
- MICE:
-
Multivariate Imputation by Chained Equations
- NAFLD:
-
Nonalcoholic fatty liver disease
- OST:
-
Opioid substitution therapy
- PEG-IFN:
-
Pegylated interferon
- PP:
-
Per protocol
- PPI:
-
Proton pump inhibitor
- PRO:
-
Patient-reported outcome
- RBV:
-
Ribavirin
- RNA:
-
Ribonucleic acid
- SD:
-
Standard deviation
- SMV:
-
Simeprevir
- SOF:
-
Sofosbuvir
- SVR:
-
Sustained virologic response
- TEAE:
-
Treatment-emergent adverse event
- VAS:
-
Visual analog scale
- VEL:
-
Velpatasvir
- WHO:
-
World Health Organization
- WPAI:
-
Work Productivity and Activity Impairment
References
Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2:161–176.
World Health Organization. Combating hepatitis B and C to reach elimination by 2030. http://apps.who.int/iris/bitstream/10665/206453/1/WHO_HIV_2016.04_eng.pdf. Accessed May 05, 2018.
Jacobson IM, Cacoub P, Dal Maso L, Harrison SA, Younossi ZM. Manifestations of chronic hepatitis C virus infection beyond the liver. Clin Gastroenterol Hepatol. 2010;8:1017–1029.
Spiegel BMR, Younossi ZM, Hays RD, Revicki D, Robbins S, Kanwal F. Impact of hepatitis C on health-related quality of life: a systematic review and quantitative assessment. Hepatology. 2005;41:790–800.
Kallman J, O’Neil MM, Larive B, Boparai N, Calabrese L, Younossi ZM. Fatigue and health-related quality of life (HRQL) in chronic hepatitis C virus infection. Dig Dis Sci. 2007;52:2531–2539.
Kleinman L, Mannix S, Yuan Y, Kummer S, L’Italien G, Revicki D. Review of patient-reported outcome measures in chronic hepatitis C. Health Qual Life Outcomes. 2012;10:92.
Shah N, Pierce T, Kowdley KV. Review of direct-acting antiviral agents for the treatment of chronic hepatitis C. Expert Opin Investig Drugs. 2013;22:1107–1121.
Asselah T, Boyer N, Saadoun D, Martinot-Peignoux M, Marcellin P. Direct-acting antivirals for the treatment of hepatitis C virus infection: optimizing current IFN-free treatment and future perspectives. Liver Int. 2016;36:47–57.
Bourlière M, Oules V, Ansaldi C, Adhoute X, Castellani P. Sofosbuvir as backbone of interferon free treatments. Dig Liver Dis. 2014;46:S212–S220.
Afdhal N, Reddy KR, Nelson DR, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370:1483–1493.
Afdhal N, Zeuzem S, Kwo P, et al. Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N Engl J Med. 2014;370:1889–1898.
Kowdley KV, Gordon SC, Reddy KR, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014;370:1879–1888.
Feld JJ, Jacobson IM, Hézode C, et al. Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N Engl J Med. 2015;373:2599–2607.
Foster GR, Afdhal N, Roberts SK, et al. Sofosbuvir and velpatasvir for HCV genotype 2 and 3 infection. N Engl J Med. 2015;373:2608–2617.
Curry MP, O’Leary JG, Bzowej N, et al. Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N Engl J Med. 2015;373:2618–2628.
Wyles D, Bräu N, Kottilil S, et al. Sofosbuvir and velpatasvir for the treatment of HCV in patients coinfected with HIV-1: an open-label, Phase 3 study. Clin Infect Dis. 2017;65:6–12.
Naggie S, Cooper C, Saag M, et al. Ledipasvir and sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med. 2015;373:705–713.
Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;. https://doi.org/10.1016/S2468-1253(17)30404-1.
Grebely J, Mauss S, Brown A, et al. Efficacy and safety of ledipasvir/sofosbuvir with and without ribavirin in patients with chronic HCV genotype 1 infection receiving opioid substitution therapy: analysis of Phase 3 ION trials. Clin Infect Dis. 2016;63:1405–1411.
World Health Organization. Global health sector strategy on viral hepatitis 2016–2021. https://www.who.int/hepatitis/strategy2016-2021/ghss-hep/en/. Accessed December, 2019.
Association Française pour l’Étude du Foie. Recommandations AFEF pour l’élimination de l’infection par le virus de l’hépatite C en France. https://afef.asso.fr/wp-content/uploads/2018/06/VF-INTERACTIF-RECO-VHC-AFEF-v2103.pdf. Accessed December, 2019.
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C 2018. J Hepatol. 2018;69:461–511.
Dieterich DT. A simplified algorithm for the management of hepatitis C infection. Gastroenterol Hepatol. 2019;15:1–12.
White TJ. Real world data: moving beyond clinical trials: the WellPoint outcomes-based formulary. https://pharmacy.ucsd.edu/sites/pharmacy.ucsd.edu/files/docs/faculty-residents/T_Jeffrey_White_WellPoint_Outcomes_Based_Formulary.pdf. Accessed May 5, 2018.
Backus LI, Belperio PS, Shahoumian TA, Loomis TP, Mole LA. Effectiveness of sofosbuvir-based regimens in genotype 1 and 2 hepatitis C virus infection in 4026 U.S. Veterans. Aliment Pharmacol Ther. 2015;42:559–573.
Calleja JL, Crespo J, Rincón D, et al. Effectiveness, safety and clinical outcomes of direct-acting antiviral therapy in HCV genotype 1 infection: results from a Spanish real-world cohort. J Hepatol. 2017;66:1138–1148.
Ingiliz P, Christensen S, Kimhofer T, et al. Sofosbuvir and ledipasvir for 8 weeks for the treatment of chronic hepatitis C virus (HCV) infection in HCV-monoinfected and HIV-HCV-coinfected individuals: results from the German hepatitis C cohort (GECCO-01). Clin Infect Dis. 2016;63:1320–1324.
Ioannou GN, Beste LA, Chang MF, et al. Effectiveness of sofosbuvir, ledipasvir/sofosbuvir, or paritaprevir/ritonavir/ombitasvir and dasabuvir regimens for treatment of patients with hepatitis C in the Veterans Affairs national health care system. Gastroenterology. 2016;151:457–471.
Lacombe K, Fontaine H, Dhiver C, et al. Real-world efficacy of daclatasvir and sofosbuvir, with and without ribavirin, in HIV/HCV coinfected patients with advanced liver disease in a French early access cohort. J Acquir Immune Defic Syndr. 2017;75:97–107.
Lai JB, Witt MA, Pauly MP, et al. Eight- or 12-week treatment of hepatitis C with ledipasvir/sofosbuvir: real-world experience in a large integrated health system. Drugs. 2017;77:313–318.
Sulkowski MS, Vargas HE, Di Bisceglie AM, et al. Effectiveness of simeprevir plus sofosbuvir, with or without ribavirin, in real-world patients with HCV genotype 1 infection. Gastroenterology. 2016;150:419–429.
Tapper EB, Bacon BR, Curry MP, et al. Real-world effectiveness for 12 weeks of ledipasvir-sofosbuvir for genotype 1 hepatitis C: the Trio Health study. J Viral Hepatol. 2017;24:22–27.
Welzel TM, Nelson DR, Morelli G, et al. Effectiveness and safety of sofosbuvir plus ribavirin for the treatment of HCV genotype 2 infection: results of the real-world, clinical practice HCV-TARGET study. Gut. 2016;66:1844–1852.
Welzel TM, Petersen J, Herzer K, et al. Daclatasvir plus sofosbuvir, with or without ribavirin, achieved high sustained virological response rates in patients with HCV infection and advanced liver disease in a real-world cohort. Gut. 2016;65:1861–1870.
Buggisch P, Vermehren J, Mauss S, et al. Real-world effectiveness of 8-week treatment with ledipasvir/sofosbuvir in chronic hepatitis C. J Hepatol. 2018;68:663–671.
Buggisch P, Wursthorn K, Stoehr A, et al. Real-world effectiveness and safety of sofosbuvir/velpatasvir and ledipasvir/sofosbuvir hepatitis C treatment in a single centre in Germany. PLoS One. 2019;14:e0214795.
Mangia A, Milligan S, Khalili M, et al. Global real world evidence of sofosbuvir/velpatasvir as a simple, effective regimen for the treatment of chronic hepatitis C patients: integrated analysis of 12 clinical practice cohorts. J Hepatol. 2019;70:e2–e3.
Younossi ZM, Stepanova M, Henry L, Younossi Y, Hunt S. Adherence to treatment of chronic hepatitis C: from interferon containing regimens to interferon and ribavirin free regimens. Medicine. 2016;95:e4151.
Pol S, Parlati L. Treatment of hepatitis C: the use of the new pangenotypic direct-acting antivirals in “special populations”. Liver Int. 2018;38:28–33.
Grebely J, Dalgard O, Conway B, et al. Sofosbuvir and velpatasvir for hepatitis C virus infection in people with recent injection drug use (SIMPLIFY): an open-label, single-arm, phase 4, multicentre trial. Lancet Gastroenterol Hepatol. 2018;3:153–161.
Cunningham EB, Amin J, Feld JJ, et al. Adherence to sofosbuvir and velpatasvir among people with chronic HCV infection and recent injection drug use: the SIMPLIFY study. Int J Drug Policy. 2018;62:14–23.
Foster GR, Dore GJ, Wang S, et al. Glecaprevir/pibrentasvir in patients with chronic HCV and recent drug use: an integrated analysis of 7 phase III studies. Drug Alcohol Depend. 2019;194:487–494.
Younossi ZM, Stepanova M, Afdhal N, et al. Improvement of health-related quality of life and work productivity in chronic hepatitis C patients with early and advanced fibrosis treated with ledipasvir and sofosbuvir. J Hepatol. 2015;63:337–345.
Younossi ZM, Stepanova M, Marcellin P, et al. Treatment with ledipasvir and sofosbuvir improves patient-reported outcomes: results from the ION-1, -2, and -3 clinical trials. Hepatology. 2015;61:1798–1808.
Younossi ZM, Stepanova M, Pol S, Bronowicki J-P, Carrieri MP, Bourlière M. The impact of ledipasvir/sofosbuvir on patient-reported outcomes in cirrhotic patients with chronic hepatitis C: the SIRIUS study. Liver Int. 2016;36:42–48.
Gerber L, Estep M, Stepanova M, Escheik C, Weinstein A, Younossi ZM. Effects of viral eradication with ledipasvir and sofosbuvir, with or without ribavirin, on measures of fatigue in patients with chronic hepatitis C virus infection. Clin Gastroenterol Hepatol. 2016;14:156–164.
Grebely J, Haire B, Taylor LE, et al. Excluding people who use drugs or alcohol from access to hepatitis C treatments—is this fair, given the available data? J Hepatol. 2015;63:779–782.
Yin S, Barker L, White JZ, Jiles RB. Sofosbuvir-based regimens for chronic hepatitis C in a well-insured U.S. population: patient characteristics, treatment adherence, effectiveness, and health care costs, 2013–2015. J Manag Care Spec Pharm. 2019;25:195–210.
Williams N, Bossert N, Chen Y, et al. Influence of social determinants of health and substance use characteristics on persons who use drugs pursuit of care for hepatitis C virus infection. J Subst Abuse Treat. 2019;102:33–39.
Day E, Hellard M, Treloar C, et al. Hepatitis C elimination among people who inject drugs: challenges and recommendations for action within a health systems framework. Liver Int. 2019;39:20–30.
Mason K, Dodd Z, Guyton M, et al. Understanding real-world adherence in the directly acting antiviral era: a prospective evaluation of adherence among people with a history of drug use at a community-based program in Toronto, Canada. Int J Drug Policy. 2017;47:202–208.
Zeuzem S, Foster GR, Wang S, et al. Glecaprevir-pibrentasvir for 8 or 12 weeks in HCV genotype 1 or 3 Infection. N Engl J Med. 2018;378:354–369.
Puoti M, Foster GR, Wang S, et al. High SVR12 with 8-week and 12-week glecaprevir/pibrentasvir therapy: an integrated analysis of HCV genotype 1–6 patients without cirrhosis. J Hepatol. 2018;69:293–300.
Bourlière M, Gordon SC, Flamm SL, et al. Sofosbuvir, velpatasvir, and voxilaprevir for previously treated HCV infection. N Engl J Med. 2017;376:2134–2146.
Bourliere M, Gordon SC, Schiff ER, et al. Deferred treatment with sofosbuvir-velpatasvir-voxilaprevir for patients with chronic hepatitis C virus who were previously treated with an NS5A inhibitor: an open-label substudy of POLARIS-1. Lancet Gastroenterol Hepatol. 2018;3:559–565.
Read P, Gilliver R, Kearley J, et al. Treatment adherence and support for people who inject drugs taking direct-acting antiviral therapy for hepatitis C infection. J Viral Hepatol. 2019;26:1301–1310.
Acknowledgments
The study was designed and conducted according to the protocol by the sponsor (Gilead Sciences, Inc.) in collaboration with the principal investigators. The sponsor collected the data, monitored the study conduct and performed the statistical analyses. All authors were involved in data acquisition and analysis, interpretation of the data and contributed to drafting the manuscript and critical revision of the manuscript with regard to important intellectual content. All authors approved the final version of the manuscript prior to submission. Authors would like to thank the HELIOS study group for their contribution towards data acquisition (HELIOS group: Dr Ajana, Dr Bellaiche, Dr Bourlière, Dr Bronowicki, Dr Cadranel, Dr Canva-Delcambre, Dr Causse, Dr Cotte, Dr Dao, Dr de Lédinghen, Dr Desmorat, Dr Di Martino, Dr Donnadieu-Rigole, Dr Fontanges, Dr Gournay, Dr Grange, Dr Habersetzer, Dr Hanslik, Dr Jezequel, Dr Leroy, Dr Loustaud-Ratti, Dr Molina, Dr Neau, Dr N’Guyen Khac, Dr Njike-Naksu, Dr Portal, Dr Renou, Dr Ribard, and Dr Rosenthal). The Scientific Committee included Dr T Asselah, Dr F Bailly, Dr D Guyader, Dr Ouzan, Dr Pol and Dr Rosa. Medical writing support was provided by Dr Rima Patel and Dr Holly Hopkins, Elements Communications Ltd, Westerham, Kent, funded by Gilead Sciences, Inc.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Denis Ouzan has served as a speaker for AbbVie and Gilead Sciences, reports research funding from Gilead Sciences, and reports financial support for attending symposia and sponsorship for educational meetings from AbbVie, Gilead Sciences and Merck Sharp & Dohme. Dominique Larrey has served as a speaker/advisor for AbbVie, Gilead Sciences and Merck Sharp & Dohme. Dominique Guyader has served as a speaker for and reports financial support for attending symposia from AbbVie, Gilead Sciences, Merck Sharp & Dohme, and Janssen, and also reports research funding from Janssen. André-Jean Remy has served as a speaker/consultant/advisor for Gilead Sciences. Ghassan Riachi has served as a speaker and advisor for Gilead Sciences. Fréderic Heluwaert, Jean-Marc Combis, Isabelle Rosa, Dominique Roulot, Bruno Roche and Jérôme Dumortier have no conflicts of interest to declare. Régine Truchi has served as a speaker and clinical investigator for Gilead Sciences. François Bailly has served as a speaker/advisor for AbbVie, Bristol-Myers Squibb, Gilead Sciences and Merck Sharp & Dohme, and reports financial support for attending symposia from AbbVie, Gilead Sciences and Merck Sharp & Dohme. Christophe Hézode, Denise Glorian-Petaud, Olivier Libert and Heribert Ramroth is an employee of Gilead Sciences. Tarik Asselah has served as a clinical investigator and speaker for AbbVie, Gilead Sciences, Janssen and Merck Sharp & Dohme. Gérard Thiefin has served as a speaker for and reports financial support for attending symposia from Gilead Sciences. Vincent Leroy has served as a speaker/advisor and clinical investigator for Gilead Sciences. Dominique Thabut reports financial support for attending symposia from AbbVie and Gilead Sciences. Stanislas Pol has served as a speaker/consultant for AbbVie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck Sharp & Dohme, and Roche, and reports research funding from Bristol-Myers Squibb, Gilead Sciences, Merck Sharp & Dohme, and Roche.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ouzan, D., Larrey, D., Guyader, D. et al. Evolution of Hepatitis C Virus Treatment During the Era of Sofosbuvir-Based Therapies: A Real-World Experience in France. Dig Dis Sci 66, 881–898 (2021). https://doi.org/10.1007/s10620-020-06234-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06234-1