Abstract
Background
Unexplained bloating, gas, and pain are common symptoms. If routine tests are negative, such patients are often labeled as irritable bowel syndrome.
Aims
To determine the diagnostic utility of breath tests that assess for small intestinal bacterial overgrowth (SIBO), fructose or lactose intolerance, and the predictive value of symptoms.
Methods
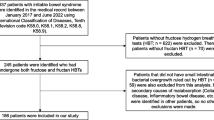
Patients with gas, bloating, diarrhea, abdominal pain (≥ 6 months), and negative endoscopy and radiology tests were assessed with symptom questionnaires, glucose (75 g), fructose (25 g), or lactose (25 g) breath tests. Breath tests were categorized as positive when H2 (≥ 20 ppm) or CH4 (≥ 15 ppm) increased above baseline values or as hypersensitive when symptoms changed significantly without rise in H2/CH4 or as negative.
Results
1230 patients (females = 878) underwent 2236 breath tests. The prevalence of SIBO was 33% (294/883), fructose intolerance was 34% (262/763), and lactose intolerance was 44% (260/590). Hypersensitivity was found in 16% and 9%, respectively, during fructose and lactose breath tests. Although gas (89%), abdominal pain (82%), and bloating (82%) were highly prevalent, pretest symptoms or their severity did not predict an abnormal breath test, but symptoms during the breath test facilitated diagnosis of SIBO, fructose, and lactose intolerance and hypersensitivity.
Conclusions
Approximately 45% of patients with unexplained gas and bloating had SIBO, fructose, or lactose intolerance; another 9–16% had visceral hypersensitivity. Pretest symptoms were poor predictors, but symptoms during the breath tests were useful. Breath tests are safe, provide significant diagnostic yield, and could be useful in routine gastroenterology practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal bloating, gas, distension, and diarrhea are reported by 1/3rd of patients attending gastroenterology clinics [1,2,3]. When routine endoscopic and radiological tests are negative, in community practice most are labeled as irritable bowel syndrome (IBS) [4, 5]. However, these patients continue to doctor shop or seek alternative remedies [6, 7] and have poor quality of life [5,6,7].
One possible explanation for their symptoms is carbohydrate intolerance [3]. The Western diet has changed significantly, and today large amounts of fructose are being consumed [3], often as a sweetener in beverages and candies [3, 8,9,10,11]. Although naturally present in fruits and honey [9, 10], fructose consumption has alarmingly increased [12]. In small amounts, fructose is completely absorbed through the Glut 5 transporters or through facilitated transport using Glut 2 transporter [13,14,15]. However, if a person consumes large amounts of fructose or has limited absorptive capacity, the unabsorbed fructose can serve as an osmotic load that draws fluid and thereafter can be propelled rapidly into the colon. Here, upon exposure to anerobic bacteria, the carbohydrate residue is usually fermented to produce gas, bloating, and diarrhea [3, 11, 16, 17].
Likewise, lactose a disaccharide with a per capita consumption of 1.9 cups/day [18, 19], when malabsorbed, will also cause gas, bloating, and diarrhea [20, 21]. Lactose is normally hydrolyzed in the small intestine by the enzyme lactase into glucose and galactose [20]. Although genetic mutation has led to persistence of lactase in adults [20], about 75% of the world’s population malabsorb lactose after age 30 [20, 22]. Another explanation for refractory gastrointestinal symptoms such as pain, gas, and bloating is small intestinal bacterial overgrowth (SIBO) [23,24,25].
Breath testing has emerged as a simple, noninvasive method of identifying SIBO [23,24,25,26], fructose [11, 16, 17, 26, 27], and lactose intolerance [18, 20, 28, 29], but their clinical utility and diagnostic yield is not known. Our objectives were to investigate a consecutive series of patients with unexplained gastrointestinal symptoms and examine the (1) prevalence of SIBO, fructose, and lactose intolerance as assessed by breath tests; (2) predictive value of pretest symptoms for diagnosis of SIBO or carbohydrate intolerance; and (3) prevalence of and changes in symptom profiles during breath tests.
Methods
Patients 18 years or older, referred to a tertiary care center with unexplained gas (flatulence), bloating, diarrhea, fullness, and pain for at least 6 months, and normal hematological and biochemistry profile(s), normal endoscopy/colonoscopy with biopsies, normal CAT scan, and stool tests were included. Patients with celiac disease, previous abdominal surgery (except cholecystectomy, hysterectomy, and appendectomy), congestive heart failure, chronic renal failure, respiratory failure or cancer or history of recent antibiotic use (6 weeks) were excluded. All patients answered a validated symptom questionnaire [17]. Patients with diabetes were excluded from glucose breath testing.
Study Protocol
All patients discontinued laxatives and drugs that affected motility, such as magnesium compounds, secretagogues (lubiprostone, linaclotide), fiber supplements, prokinetics (tegaserod, prucalopride), and polyethylene glycol, for 1 week and enemas or suppositories for 3 days. One day before the test, patients were asked to refrain from consuming lactose or fructose products, and to eat a low-residue carbohydrate diet, and fast from midnight. Patients were asked to brush their teeth, 2 h prior to the test, and to refrain from smoking or chewing gum or mints during the test. All patients first underwent a glucose breath test, and if negative, they underwent a fructose breath test, and 1 week later a lactose breath test. If the glucose breath test was positive, other breath tests were canceled. This order of testing was used to obviate the possibility of a false positive fructose or lactose breath test, because of SIBO.
Breath Test Protocols
The following protocols were used for performing the breath tests, and patients were asked to refrain from any exercise or smoking.
Glucose Breath Test (GBT)
The patient received 75 g of glucose dissolved in 250 ml of water [23, 26]. End expiratory breath samples were obtained at baseline and at 15-min intervals after ingestion of glucose solution for a 2-h period [23, 26].
Fructose Breath Test (FBT)
The patient received 25 g of fructose dissolved in 250 ml of water [11, 17, 26]. Breath samples were obtained at baseline and at 30-min intervals thereafter for a 3-h period.
Lactose Breath Test (LBT)
The patient received 25 g of lactose dissolved in 250 ml of water [18, 20, 26, 28]. Breath samples were obtained at baseline and at 30-min intervals thereafter for a 5-h period [26, 28].
Breath samples were collected in a bag (QuinTron Instrument Company Inc., Milwaukee, WI.), and alveolar gas samples were analyzed for H2 and CH4 [30] using gas chromatography (QuinTronMicro Analyzer®, QuinTron Instruments, Wisconsin).
Assessment of Gastrointestinal Symptoms
All patients filled out a validated questionnaire before the administration of breath tests that assessed 10 symptoms [17, 23], abdominal pain, belching, bloating, fullness, indigestion, dyspepsia (upper abdominal discomfort), nausea, diarrhea, vomiting, and gas (flatulence) as part of baseline assessment. If present, they scored its frequency, intensity, and duration on a 0–3 point Likert scale. Intensity: 0 = no symptom, 1 = mild, 2 = moderate, 3 = severe symptom. Frequency: 0 = none, 1 = < 1 episode/week, 2 = 1 episode/week, 3 = > 1 episode/week. Duration: 0 = none, 1 = < 10 min, 2 = 10–30 min, 3 = > 30 min. The total score ranged from 0 to 9 for each symptom. A mean score was calculated for each symptom, and an overall mean score for all ten symptoms. Additionally, all patients were asked to rate the intensity (0–3) score for the aforementioned symptoms, just before and throughout the breath tests (15 min intervals for GBT and 30 min intervals for FBT and LBT). The onset of new or worsening symptom(s) during the test was used to identify intolerance and/or hypersensitivity.
Data Analysis
The breath test was categorized as positive (abnormal) or negative. A positive test was defined as ≥ 20 ppm increase in H2 values above baseline or ≥ 15 ppm [11, 16, 17, 23, 26] increase in values above baseline CH4 or an increase in combined values of H2 and CH4 of ≥ 20 ppm above baseline. Additionally, a positive fructose or lactose breath test was further categorized into malabsorption and/or intolerance (Fig. 1). Malabsorption was defined as a significant rise in H2 and/or CH4 levels (as defined above) without any change in symptoms during the test (11). Intolerance was defined as both the presence of malabsorption and new onset of symptoms or an increase in the severity (≥ 2 score) of two or more baseline symptoms. Also, patients who experienced new onset of diarrhea (≥ 2 score) during the breath test, but their breath test values did not meet the threshold values for an increase in H2 or CH4, were also categorized as having a positive breath test.
A negative breath test was further categorized as either normal or hypersensitivity (Fig. 1). A normal breath test was defined as no significant increase in H2 and CH4 values together with no change in symptom profile(s) during the breath test. A breath test was designated as hypersensitivity during either the FBT or LBT, if there was a significant increase in the symptom severity score (≥ 2) when compared to the baseline pretest symptom score, and with at least two or more symptoms, together with no significant increase in H2 and CH4.
Statistical Analyses
Data are summarized as mean and dispersion ranges for the quantitative variables, and as percentages for the categorical variables. Fisher’s exact test or χ2 test was used for the data analyses whenever appropriate. The individual contingency tables were constructed for the comparisons of each symptom, both before and during the test. GI symptom profiles before and during the test and in subjects with a negative and positive breath test were compared by student t test. The differences in symptom profiles were compared between patients with an abnormal and normal breath test by using linear regression analysis. Differences in symptom profiles between subjects with a positive or negative GBT were analyzed using student t test, and a paired t test was used for comparisons between symptoms before and during the test. Statistical analyses were performed using SPSS v21 (Chicago IL, USA), and a p value < 0.05 was considered significant.
Results
A total of 1230 patients (878 females and 352 males) with chronic symptoms (mean duration > 3 years) were assessed over 4 years. The mean age (± SD) was 47 (± 18) years. A total of 2236 breath tests were performed. Not all patients had all 3 breath tests, because only patients with negative GBT had FBT or LBT. Some patients had GBT outside the study period, but FBT or LBT during the study period. Also, patients treated with antibiotics for a positive GBT, but remained symptomatic, and had a negative GBT subsequently, were evaluated for fructose or lactose intolerance. The lower number for LBT was because some patients had previous diagnosis of lactose intolerance and refused LBT. A total of 411 patients underwent all three breath tests.
Glucose Breath Test
Of the 883 patients (629 females and 254 males) who underwent GBT, 294 (33%) had positive test for SIBO and 589 (67%) had negative test (Fig. 2). The mean (SD) baseline value for H2 was 5.92 ppm (± 10) and for CH4 was 7.85 ppm (± 15). The mean (SD) peak value for H2 was 17.9 (± 32.3) ppm and for CH4 was 10.9 (± 23.9) ppm. The time to reach peak levels for H2 was 48 min and for CH4 was 28 min. Forty-eight patients experienced new onset of significant diarrhea during the test and were designated as abnormal. In this group, 19/48 (38%) showed significant rise in H2 or CH4, but in 29/48 (62%) the rise in H2 and CH4 did not meet our predetermined criteria.
Fructose Breath Test
Of the 763 patients (534 females and 229 males) who underwent FBT, 262 (34%) had a positive test and 501 (66%) had a negative test (Fig. 2). Among patients with a positive test, 139 (18%) had dietary fructose intolerance and 123 (16%) had fructose malabsorption. Among patients with a negative test, 123 (16%) had visceral hypersensitivity and 380 (50%) had a normal test. Seventy-five patients developed diarrhea during the test, of whom 33/75 (44%) patients showed a rise in H2 or CH4 values and 42/75 (56%) patients had no rise in H2 or CH4, but were categorized as positive. The mean (SD) basal levels for H2 and CH4 were 4 and 6 ppm, respectively, the time to reach peak H2 was 84 min and for peak CH4 was 46 min, and the mean peak value for H2 was 24.4 (± 30.8) ppm and for CH4 was 11.9 (± 25.2) ppm, respectively.
Lactose Breath Test
Of the 590 patients (427 females and 163 males) who underwent LBT, 260 (44%) had positive test and 330 (56%) had negative test. In the positive group, 77 (13%) had lactose intolerance and 183 (31%) had lactose malabsorption. In the negative group, 52 (9%) had hypersensitivity and 278 (47%) had normal test. The mean basal levels for H2 and CH4 were 6 and 6 ppm, respectively, and the time to reach peak levels for H2 was 147 min and for CH4 was 78 min. The mean peak values for H2 was 43.9 (± 77.6) and for CH4 was 11.8 (± 23.4) ppm. Thirty-eight patients developed diarrhea, of whom 27/38 (71%) had significant rise in H2 or CH4 and 11/38 (29%) had no rise, but were categorized as positive.
Assessment of Baseline Symptoms and Symptoms During the Test
Table 1 shows the prevalence of pretest symptom scores in patients who tested positive and negative for all 3 breath tests. At baseline, 89% reported flatulence, 82% abdominal pain, 82% bloating, 80% fullness, 74% diarrhea, 73% indigestion, and 70% belching and nausea. Patients with negative breath test also reported similar prevalence of symptoms. We found no significant difference in the prevalence of symptoms between the two groups. Overall, the pretest symptoms were not predictive of a positive or negative GBT, FBT, or LBT (p > 0.05) (Table 1). Furthermore, the prevalence of symptoms during a positive test was not significantly different (p = 0.09, Table 2), when compared to patients with a negative test. There was a significant increase in the prevalence of symptoms during the breath test when compared to baseline symptoms with all three substrates and in those with a positive or negative test (Table 2). When the prevalence of pretest symptoms was compared with those during the test, there was no difference for all three breath tests.
Assessment of Breath H2 and CH4
During the GBT, the mean baseline and peak values for H2 in patients who tested positive was 10.5 ± 20.2 ppm and 73.4 ± 66.6 ppm, respectively, and the mean baseline and peak values for CH4 were 15.3 ± 21.1 and 23.4 ± 29.5 ppm, respectively. For the FBT positive group, the mean baseline and peak values for H2 were 8.3 ± 19.2 and 71.4 ± 63.5 ppm and for CH4 were 14.3 ± 20.1 and 21.4 ± 28.5 ppm, respectively. For the LBT positive group, the mean baseline and peak values for H2 were 8.6 ± 14.9 and 105.8 ± 83.6 ppm and for CH4 17.2 ± 19.8 and 32.2 ± 32.3 ppm, respectively.
Importantly, 280 (31%) patients showed little or no change in H2 values during the GBT but showed a significant rise in CH4 levels, facilitating a diagnosis of SIBO. Similarly, 159 (21.9%) patients with the FBT, and 102 (17.3%), patients with the LBT showed a significant rise in CH4 facilitating a designation of positive test. Overall, the measurement of H2 gas alone provided a diagnosis of SIBO in 69%, and a diagnosis of fructose intolerance in 62%, and lactose intolerance in 68% of patients. The measurement of CH4 gas alone provided an additional diagnostic yield of 15% for SIBO, 14% for fructose, and 18% for lactose intolerance, and combined measurements of H2 and CH4 provided an additional yield of 16% for SIBO, 24% for fructose and 14% for lactose intolerance.
Discussion
Although the use of breath tests for suspected SIBO and/or carbohydrate intolerance has been previously reported [26, 31], their diagnostic utility in clinical practice has not been systematically assessed. In this largest study to date of 1230 patients who underwent 2236 breath tests, we found a prevalence of 33% for SIBO, 34% for fructose intolerance, and 44% for lactose intolerance. Thus, breath tests provided a diagnosis of SIBO or carbohydrate intolerance in a significant proportion of patients with long-standing, unexplained gastrointestinal symptoms.
Our patients presented with common gastrointestinal symptoms, often diagnosed as IBS [32] in community practice; over 2/3rd reported abdominal pain, bloating, distension, gas, diarrhea, belching, nausea, and indigestion. These symptoms were present for over 3 years, emphasizing their chronic nature. Today, such patients may receive an empirical course of antibiotics or low FODMAPs restricted diet [1, 3, 25, 33]. Although reasonable, especially if breath testing is not available, this approach is fraught with problems including the development of antibiotic resistance and C. difficile colitis [34]. Furthermore, long-term use of low FODMAPs diet may lead to intestinal dysbiosis and nutritional deficiency [35,36,37], and a recent meta-analysis showed very low quality evidence for its efficacy in IBS [38]. Hence, objective testing, before embarking on therapeutic strategies, seems more prudent [23,24,25, 36].
Carbohydrate fermentation produces several gases including hydrogen and methane. Methane is not used by human cells and is either excreted as flatus (80%) or through breath (20%) [26, 39]. About 20–30% of population has detectable methane on breath testing [25, 40]. If methane is not measured, a breath test may be wrongly interpreted as normal [23, 26]. We found that 31% of patients with positive GBT and 38% and 32% with positive FBT and LBT were methane producers. Thus, 1/3rd of patients have methane producing microbiota, and breath methane assessment clearly increases the diagnostic yield of breath tests. This finding also explains the lower positive yield for breath tests that only measured hydrogen [23, 26, 40]. Importantly, this new finding of a significant rise in breath methane levels during the GBT suggests that the proximal small bowel was likely colonized by methanogenic microbiota (archae). This condition of small intestinal methanogenic overgrowth merits further validation.
Another new metric was the designation of patients with negative breath test as normal or having visceral hypersensitivity. Hypersensitivity was seen in 16% and 9% of patients undergoing FBT and LBT, respectively. Previously, after lactose, bloating and borborygmi were more frequently observed in IBS patients than controls suggesting hypersensitivity [41]. Thus, breath tests may identify a subgroup of patients with food hypersensitivity but without malabsorption [20, 28] and thereby may serve as a biomarker for visceral hypersensitivity, and this requires further validation. Also, whether this is a nocebo effect cannot be excluded without a placebo controlled study.
Diarrhea was observed during the GBT, FBT, and LBT in 6.5%, 9.8%, and 6.4%, respectively. Between 33 and 50% of this group had no significant rise in H2 or CH4, most likely because of rapid transit of fermented materials or gases or production of H2S [42, 43]. This new finding underscores the importance of documenting symptoms, especially diarrhea and its severity during the breath test and could provide additional diagnostic yield and an explanation for their symptoms.
The pretest symptoms were poor predictors of SIBO, fructose or lactose intolerance, as the symptom profiles were similar between a positive and negative breath group. This finding underscores the need for performing breath tests to diagnose these conditions and extends previous observations [16, 17, 23]. Additionally, the usefulness of symptom(s) assessment during the breath test has not been reported. We found a twofold increase in symptom prevalence during the breath test. This assessment can help to identify patients with carbohydrate intolerance, document reproducibility of symptom(s), identify patients with negative breath tests and visceral hypersensitivity [44, 45], and identify patients with diarrhea as having either SIBO or carbohydrate intolerance.
The exact prevalence of SIBO or carbohydrate intolerance in the population is unknown, because its diagnosis requires breath test or small bowel aspirate/culture [23, 26] or mucosal enzyme assay [45]. Our study provides novel perspectives regarding their prevalence. However, this study has limitations including referral bias to a tertiary care center. The prevalence of these disorders is best assessed by a study in community practice. Another limitation is that our study was not designed to evaluate the outcome of treatment intervention(s). GBT detects proximal SIBO and may have missed distal SIBO [23, 26], underestimating its prevalence. A recent retrospective uncontrolled study suggested that glucose malabsorption may cause rapid transit and false positive GBT in a small number of patients [46]. However, previously we found that the results of GBT correlated well with duodenal aspiration/culture with 84% specificity [23]. Thus, glucose malabsorption is unlikely to occur in the vast majority of subjects. Also, we did not examine the prevalence of abnormal breath tests in the healthy population; although using similar substrates and cutoffs for hydrogen or methane, a prevalence of 0–13.3% has been reported for an abnormal GBT, and about 10% for fructose and lactose malabsorption [25, 26, 47]. We used a higher cutoff value for CH4 positivity (> 15 ppm), as our studies pre-date The North American consensus recommendations [26], and if anything the higher cutoff values would have decreased the sensitivity in our study.
In conclusion, approximately 45% of patients with unexplained gastrointestinal symptoms demonstrated evidence for SIBO or fructose or lactose intolerance. Because pretest symptoms were poor predictors of the underlying diagnosis, breath tests that are noninvasive, standardized, and objective should be considered in the routine evaluation of patients with negative tests. This approach may lead to an early diagnosis of these problems and could have a significant impact on the healthcare burden of these patients.
References
Goebel-Stengel M, Stengel A, Schmidtmann M, et al. Unclear abdominal discomfort: pivotal role of carbohydrate malabsorption. J Neurogastroenterol Motil. 2014;20:228–235.
Ringel Y, Williams RE, Kalilani L, et al. Prevalence, characteristics, and impact of bloating symptoms in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009;7:68–72.
Fedewa A, Rao SS. Dietary fructose intolerance, fructan intolerance and FODMAPs. Curr Gastroenterol Rep. 2014;16:1–13. https://doi.org/10.1007/s11894-013-0370-0.
Fernandez-Banares F, Esteve-Pardo M, de Leon R, et al. Sugar malabsorption in functional bowel disease: clinical implications. Am J Gastroenterol. 1993;88:2044–2050.
Chang L. Review article: epidemiology and quality of life in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004;20:31–39.
Drossman DA, Morris CB, Schneck S, et al. International survey of patients with IBS: symptom features and their severity, health status, treatments, and risk taking to achieve clinical benefit. J Clin Gastroenterol. 2009;43:541–550.
Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders. Gastroenterology. 2006;130:1435–1446.
Riveros MJ, Parada A, Pettinelli P. Fructose consumption and its health implications; fructose malabsorption and nonalcoholic fatty liver disease. Nutr Hosp. 2014;29:491–499.
Vos MB, Kimmons JE, Gillespie C, et al. Dietary fructose consumption among US children and adults: the Third National Health and Nutrition Examination Survey. Medscape J Med. 2008;10:160.
Bray GA. Energy and fructose from beverages sweetened with sugar or high-fructose corn syrup pose a health risk for some people. Adv Nutr. 2013;4:220–225.
Rao SS, Attaluri A, Anderson L, et al. Ability of the normal human small intestine to absorb fructose: evaluation by breath testing. Clin Gastroenterol Hepatol. 2007;5:959–963.
United States Department of Agriculture. Economic Research Service. (2017). Source: USDA, Economic Research Source, Food Availability Data. https://www.ers.usda.gov/data-products/chart_gallery/gallery/chart-detail/?chartld=85059.
Wasserman D, Hoekstra JH, Tolia V, et al. Molecular analysis of the fructose transporter gene (GLUT5) in isolated fructose malabsorption. J Clin Invest. 1996;98:2398–2402.
Corpe CP, Bovelander FJ, Hoekstra JH, et al. The small intestinal fructose transporters: site of dietary perception and evidence for diurnal and fructose sensitive control elements. Biochim Biophys Acta. 1998;1402:229–238.
Biesiekierski JR. Fructose-induced symptoms beyond malabsorption in FGID. United European Gastroenterol J. 2014;2:10–13.
Choi YK, Johlin FC Jr, Summers RW, et al. Fructose intolerance: an under-recognized problem. Am J Gastroenterol. 2003;98:1348–1353.
Choi YK, Kraft N, Zimmerman B, et al. Fructose intolerance in IBS and utility of fructose-restricted diet. J Clin Gastroenterol. 2008;42:233–238.
Di Rienzo T, D’Angelo G, D’Aversa F, et al. Lactose intolerance: from diagnosis to correct management. Eur Rev Med Pharmacol Sci. 2013;17:18–25.
United States Department of Agriculture. Economic Research Service. Dairy products; Per Capita Availability/dymfg.xls.
Deng Y, Misselwitz B, Dai N, et al. Lactose intolerance in adults: biological mechanism and dietary management. Nutrients. 2015;7:8020–8035.
Scrimshaw NS, Murray EB. The acceptability of milk and milk products in populations with a high prevalence of lactose intolerance. Am J Clin Nutr. 1988;48:1079–1159.
Vesa TH, Marteau P, Korpela R. Lactose intolerance. J Am Coll Nutr. 2000;19:165S–175S.
Erdogan A, Rao SS, Gulley D, et al. Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test. Neurogastroenterol Motil. 2015;27:481–489.
Ghoshal UC, Ghoshal U. Small intestinal bacterial overgrowth and other intestinal disorders. Gastroenterol Clin North Am. 2017;46:103–120.
Rezaie A, Pimentel M, Rao SS. How to test and treat small intestinal bacterial overgrowth: an evidence-based approach. Curr Gastroenterol Rep. 2016;18:8.
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American consensus. Am J Gastroenterol. 2017;112:775–784.
Montalto M, Gallo A, Ojetti V, et al. Fructose, trehalose and sorbitol malabsorption. Eur Rev Med Pharmacol Sci. 2013;17:26–29.
Misselwitz B, Pohl D, Fruhauf H, et al. Lactose malabsorption and intolerance: pathogenesis, diagnosis and treatment. United Eur Gastroenterol J. 2013;1:151–159.
Rana SV, Malik A. Hydrogen breath tests in gastrointestinal diseases. Indian J Clin Biochem. 2014;29:398–405.
Christman NT, Hamilton LH. A new chromatographic instrument for measuring trace concentrations of breath-hydrogen. J Chromatogr. 1982;229:259–265.
Gasbarrini A, Corazza GR, Gasbarrini G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther. 2009;29:1–49.
Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393–1407.
Gibson PR. History of the low FODMAP diet. J Gastroenterol Hepatol. 2017;32:5–7.
Srigley JA, Brooks A, Sung M, et al. Inappropriate use of antibiotics and Clostridium difficile infection. Am J Infect Control. 2013;41:1116–1118.
Sloan TJ, Jalanka J, Major GAD, et al. A low FODMAP diet is associated with changes in the microbiota and reduction in breath hydrogen but not colonic volume in healthy subjects. PLoS ONE. 2018;13:e0201410.
Rao SS, Yu S, Fedewa A. Systematic review: dietary fibre and FODMAP-restricted diet in the management of constipation and irritable bowel syndrome. Aliment Pharmacol Ther. 2015;41:1256–1270.
Eswaran S. Low FODMAP in 2017: lessons learned from clinical trials and mechanistic studies. Neurogastroenterol Motil. 2017;29:e13055. https://doi.org/10.1111/nmo.13055.
Dionne J, Ford AC, Yuan Y, et al. A systematic review and meta-analysis evaluating the efficacy of a gluten-free diet and alow FODMAPs diet in treating symptoms of irritable bowel syndrome. Am J Gastroenterol. 2018;113:1290–1300.
Pimentel M, Gunsalus RP, Rao SS, et al. Methanogens in human health and disease. Am J Gastroenterol. 2012;1:28–33.
Saad RJ, Chey WD. Breath testing for small intestinal bacterial overgrowth: maximizing test accuracy. Clin Gastroenterol Hepatol. 2014;12:1964–1972.
Lin ESK, Pichetshote N, et al. Measurement of hydrogen sulfide during breath testing correlates to patient symptoms. Gastroenterol. 2017;152:S205–S206.
Singer-Englar T, Rezaie A, Gupta K, et al. Competitive hydrogen gas utilization by methane- and hydrogen sulfide-producing microorganisms and associated symptoms: results of a novel 4-gas breath test machine. Gastroenterology. 2018;154:S-47.
Zhu Y, Zheng X, Cong Y, et al. Bloating and distention in irritable bowel syndrome: the role of gas production and visceral sensation after lactose ingestion in a population with lactase deficiency. Am J Gastroenterol. 2013;108:1516–1525.
Dainese R, Casellas F, Marine-Barjoan E, et al. Perception of lactose intolerance in irritable bowel syndrome patients. Eur J Gastroenterol Hepatol. 2014;26:1167–1175.
Simren M, Tornblom H, Palsson OS, et al. Management of the multiple symptoms of irritable bowel syndrome. Lancet Gastroenterol Hepatol. 2017;2:112–122.
Lin EC, Massey BT. Scintigraphy demonstrates high rate of false-positive results from glucose breath tests for small bowel bacterial overgrowth. Clin Gastroenterol Hepatol. 2016;14:203–208.
Kee WJ, Seo M, Cho YH, et al. Prevalence of fructose malabsorption in patients with irritable bowel syndrome after excluding small intestinal bacterial overgrowth. J Neurogastroenterol Motil. 2018;24:307–316.
Acknowledgments
We thank Mrs. Helen Smith for the excellent secretarial assistance, and Mrs. Collier Badger, Mrs. Arie Mack and Mrs. Michelle Jackson for assistance with the breath tests. Dr. Rao was supported by NIH 5R21 DK104127-02 and U-34, DK109191-02.
Author information
Authors and Affiliations
Contributions
SSCR was involved in study concept, patient recruitment, analysis of breath test, overall supervision, manuscript writing, IRB submission. MA-B helped in data analysis, data interpretation, manuscript writing. EC-A contributed to data analysis, data interpretation, IRB, statistical analysis. NR helped in data entry. BMD contributed to data entry.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest with this article.
Ethical approval
The study was approved by the Augusta University Institutional Review Board No. 1114725 and registered at Clinical Trials Gov: NCTO 03261856.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amieva-Balmori, M., Coss-Adame, E., Rao, N.S. et al. Diagnostic Utility of Carbohydrate Breath Tests for SIBO, Fructose, and Lactose Intolerance. Dig Dis Sci 65, 1405–1413 (2020). https://doi.org/10.1007/s10620-019-05889-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05889-9