Abstract
Background
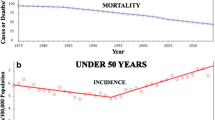
The incidence of colorectal cancer (CRC) in persons under the age of 50 years (EOCRC) is increasing even as the incidence of CRC in persons over age 50 is decreasing. This has led to recommendations to lower the age of CRC screening to age 45. It is not clear whether EOCRC is identical to CRCs in older patients or whether there are distinctive features between the two groups.
Aims and methods
We reviewed the literature on the clinical and genetic aspects of EOCRC.
Results
We found that there is an increased likelihood of a strong genetic basis for EOCRC, but that at least 80% of cases do not come from the known high-penetrance cancer syndromes. Early-onset CRCs tend to occur in the distal colon or rectum, are more likely to be detected due to cancer-related symptoms, appear to be increasing in whites more than non-whites on a population-wide analysis, and are more likely to present in an advanced stage of disease. There are some unique genetic features of EOCRC, including an increased proportion of tumors with LINE-1 hypomethylation, and combined chromosomal and microsatellite stability.
Conclusions
EOCRC deserves additional attention because of the high number of life years at risk with EOCRC, and the implications for earlier CRC screening. Additional focus is needed on determining whether some cases of EOCRC have a unique mechanistic basis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proportion of colorectal cancer (CRC) in persons under the age of 50 years, known as early-onset CRC (EOCRC), has steadily increased from 6 to 11% of the total over the past 25 years in the USA, while the incidence of CRC has fallen in persons ≥ 50 years or age, late–onset CRC (LOCRC) [1,2,3]. The rising incidence in young adults has generated a recent recommendation from the American Cancer Society to screen average-risk adults for CRC beginning at age 45 years [4]. It is not known whether EOCRC is caused by the same factors that cause LOCRC or whether there are unique causes that alter the clinical features [5,6,7,8,9]. Although many distinct features of EOCRC are appreciated, a comprehensive approach to early diagnosis has been elusive. This review was designed to analyze the salient clinical and genetic characteristics of EOCRC and to seek clues to assist in risk management for EOCRC and explanations for the differences from LOCRC.
Clinical Distinctions Between EOCRC and LOCRC (Table 1)
Since screening is not routinely performed in people < 50 years old, 86–98% of these tumors are found because of alarm symptoms such as bleeding and abdominal pain. Additional important differences between EOCRC and LOCRC include that EOCRC is more likely to be located in the distal colon (Fig. 1) and to present more frequently at an advanced stage of disease, the latter of which is associated with a paradoxically shorter interval from the onset of symptoms to diagnosis [5,6,7,8,9,10]. Although persons with EOCRC respond with equal or better outcomes to stage-specific cancer treatment compared to that in LOCRC, the overall survival is worse, a feature attributed to the increased presentation at a later stage of disease [5, 9, 11].

Adapted from: Strum WB and Boland CR (2019, in press) [9]. Data not previously presented
Locations of cancers in EOCRC. The prevalence of colorectal cancer location by specific colon segments among persons with early onset is illustrated in the diagram and demonstrates the predominance of distal colon origins.
Family History
A family history of CRC in persons with EOCRC is vital information, but has limitations in identifying persons at risk, a shortcoming also noted with LOCRC. Meta-analysis of family history data indicates that for all ages, a positive family history conveys an increased risk of up to fourfold depending upon the age of onset for the CRC and the number of relatives affected [12]. The most reliable results come from: (a) persons with a history of more than one first-degree relative (FDR) with CRC or (b) the onset of CRC in the FDR being < 60 years [13]. In the context of this meta-analysis and other reports, persons with EOCRC have at least one FDR with CRC between 7 and 26% of cases and at least one second-degree relative in 12–22% [6,7,8,9]. Using family history data, an estimate of the EOCRC population that would be appropriate for early screening at or before the age of 40 years is around 7% [12, 14]. Consequently, a family history of CRC in the EOCRC population, as in the LOCRC population, identifies a minority of persons with CRC [12, 14,15,16].
Genetic Distinctions Between EOCRC and LOCRC
A critical question is whether EOCRC is part of the continuum of CRC just occurring in younger people, or whether it includes groups of cancers that are biologically different from LOCRC. It has been repeatedly shown that no more than 15–20% of EOCRC tumors have microsatellite instability (MSI), reflecting Lynch syndrome and Lynch-like syndrome [17,18,19,20,21,22,23], which is not far from the 10–15% reported in studies of unselected cases of CRC [24,25,26], with minimal variation among various ethnic groups [27]. The older group of CRCs with MSI include a large proportion (~ 75%) that represent the non-familial sporadic methylation-induced silencing of the DNA mismatch repair (MMR) gene, MLH1 [26], whereas the younger population has relatively few of those, and more hereditary cancer accounting for the MSI. This difference is not great but tumors with MSI would predictably skew the outcome in EOCRC in a less aggressive direction and likely lead to tumors that are more proximal in location [28], neither of which is the case in EOCRC.
Germline Mutations in EOCRC
Several large retrospective studies of germline testing using multigene panels have demonstrated the genetic factors involved in CRC in persons under the age of 50 years [21,22,23]. A review of 193 persons under the age of 36 years, selected by having undergone genetic counseling at MD Anderson Cancer Center in Houston and tested for the known high-penetrance CRC genes, reported that 35% had a hereditary cancer syndrome, including 23 with Lynch syndrome, 22 with germline mutation-negative CRCs with defective DNA MMR activity (dMMR), 16 with familial adenomatous polyposis, two with constitutional MMR deficiency, two with biallelic MutYH mutations, and one with Li-Fraumeni syndrome. As expected, those with a hereditary syndrome were more likely to present at an earlier stage and to have a family history of CRC, although 19% of 67 patients with a documented germline mutation in a hereditary cancer gene did not have a family history of cancer [20].
A study from Ohio was published of 450 persons with EOCRC from 2013 to 2016 first screened for dDNA MMR activity, followed by germline testing using a 25-gene cancer panel. Forty-eight (10.7%) had dMMR activity, of whom 37 (8.2% of all persons evaluated and 77% of those with dMMR activity) had mutations in Lynch syndrome-associated genes. Analyses of the remaining 402 patients with MMR-proficient tumors uncovered 32 (8%) with one or more mutations in 9 high-penetrance CRC-associated genes, 13 high-moderate penetrance genes not traditionally associated with CRC, and 10 low-penetrance CRC-associated genes [21].
Four hundred and thirty persons with EOCRC from the clinical genetics service of a tertiary cancer center at the University of Michigan were studied using a variety of commercially available multigene cancer panels (containing up to 124 genes) or a custom-designed next-generation sequencing panel of 67 genes. The participants were selected after having undergone genetic counseling between 1998 and 2015; 111 (26%) had a FDR with CRC. Fewer than half of the tumors were screened for dMMR activity, and 41 of the tumors (10% of the entire cohort) had MSI [22]. Germline sequencing was performed in 315 persons and 79 (25%) had a germline mutation associated with hereditary cancer. An additional 21 persons had DNA variants of unknown significance. Fifty-six persons (17.8%) were identified as Lynch syndrome, 10 persons (3.2%) as FAP, and 13 persons (4.1%) had other cancer-associated genetic mutations. Of these 79 persons, about half had a FDR with CRC. Among 117 patients with uninformative clinical evaluations, next-generation sequence analysis using a multigene panel detected actionable germline variants in six patients (5%), increasing the total to 85 persons (19.8%) with a germline mutation associated with a hereditary cancer [22].
These studies of EOCRC indicate that about 10–20% of the tumors have dMMR activity. About half these are linked to germline mutations in DNA MMR genes (Lynch syndrome), and the other half have double somatic mutations but no known germline mutation in MMR genes [29, 30], often referred to as Lynch-like syndrome [31]. Another 2–3% are linked to FAP and its variants, and about 2–3% with other hereditary cancer genes not historically associated with CRC [16,17,18,19]. As mentioned, the presence of Lynch syndrome would neither tend to make the clinical outcomes worse or the tumors more distal, suggesting the problem is more complex than just the involvement of Lynch Syndrome.
Somatic Genetic Alterations in EOCRC
Genetic causes for the young age of onset in the remaining 80% of cases of EOCRC are not known. Explanations include the possibility that additional genetic and epigenetic alterations are involved in EOCRC but have not been identified. There is no evidence of global hypermethylation in EOCRC (such as would be seen in the CpG island methylator phenotype, or CIMP), but a subset of these tumors have LINE-1 hypomethylation that occurs in the promotors of LINE-1 sequences, which make up about 17% of the human genome. Expression of these sequences is normally suppressed by promoter methylation. The presence of LINE-1 hypomethylation is highly associated with EOCRC and associated with an appreciably worse clinical outcome [32]. In addition, there are intronic oncogenes (including MET, RAB3IP, CHRM3), located in some of the LINE-1 sequences, and these undergo simultaneous hypomethylation along with the LINE-1 promoters, resulting in re-expression of the oncogene mRNA and protein [33]. One report indicates that NOMO1 is deleted (somatically) in EOCRC [34]. A variety of changes in gene expression are reported in EOCRC, including a subset that are both diploid and microsatellite stable, but none explains the unique clinical features or provides a clue regarding a specific etiology of this variant of CRC [35,36,37,38]. The development of the CpG island methylator phenotype in sessile serrated adenomas is considered a sign of dysplastic progression, predominates in older populations, and might possibly be relevant for persons in the 40–49 year range since its appearance begins to accelerate at age 40 years [39].
Recommendations Regarding Genetic Testing in EOCRC
Although genetic screening of all persons with CRC is not yet advised on a routine basis, it is becoming more applicable for affected persons under the age of 50 years, and is certainly appropriate for persons with multiple FDRs with CRC or an FDR with CRC under the age of 60 years [20,21,22, 40]. A current debate involves whether gene testing should be done with a large comprehensive multiple cancer gene panel or a smaller CRC-specific panel, since the former may uncover 1–3% of individuals with mutations in a gene not linked to familial CRC, thus provoking interpretational challenges in clinical application [41]. The proportion of cases with difficult interpretations would not appear to be sufficient to offset the benefits of genetic screening for these populations. With time, genetic screening will likely become routine for most persons with CRC, as the costs of such testing have fallen substantially in recent years, making it cost-effective.
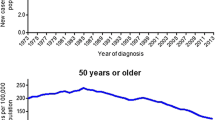
Possible Contributors to EOCRC
Aside from the obvious risk of CRC in persons with familial syndromes associated with CRC, additional factors and combination of factors contribute to risk including race, obesity, physical inactivity, diabetes, tobacco exposure, excess alcohol ingestion, and socioeconomic status [42] (also, Colorectal cancer facts & figures 2017–2019. Atlanta: American Cancer Society, 2018 [http://www.cancer.org/acs/ groups/content/documents/document/acspc-042280]). One study from a single center suggested a significant impact of EOCRC on non-Caucasians over Caucasians [9]. However, a recent large study drawn from the Surveillance, Epidemiology and End Results (SEER) program reported that, between the 1992–1996 and 2010–2014 time periods, CRC in people 20–49 years old rose with a more complex pattern. In that timeframe, the CRC incidence rose from 7.5 to 11.0/100,000 in whites, while it rose from 11.7 to 12.7/100,000 in blacks. The increase in incidence occurred disproportionately in the rectum in the white population [10]. Genetic disparities in CRC have a disproportionate impact on African-Americans where the younger age of onset is coupled with adverse tumor characteristics including a higher proportion of KRAS mutations, a lower prevalence of MSI, a higher prevalence of elevated microsatellite alterations at selected tetranucleotide repeats (EMAST), and decreased anti-tumor cytotoxic immunity, resulting in a poorer prognosis. The negative impact carries over further with insurance coverage being less or nonexistent for African-Americans [43, 44].
Obesity has a strong link to CRC. The relationship is stronger in men than women and for colon cancer over rectal cancer [45]. Data relating obesity and physical inactivity to CRC support a consistent demonstration that physical activity is associated with a preventive effect on colon, but not rectal, cancer [46]. The molecular mechanisms relating obesity to cancer are complex and thought to include chronic inflammation in visceral fat and insulin resistance which activate oxidative stress, adipocytokines (adiponectin and leptin), sex steroids, the microbiome, and other genetic mutations and environmental factors [45, 47].
Meta-analyses of diabetes, independent of obesity, physical activity and smoking, show a significant increase in risk of colon cancer for men (RR 1.43) and women (RR 1.35) and for rectal cancer in men (RR 1.22) [48]. Diabetes in the USA is estimated to be present in 1.2% of adults between 18 and 44 years as of 2015. San Diego County is considered to be affected at lower than average rates of obesity (National Diabetes Statistics Report 2017. Centers for Disease Control and Prevention [https:/www.cdc.gov/diabetes/statistics/ Accessed March 12, 2018]). A study of 109 persons with EOCRC in the San Diego area found a 6.3% prevalence of diabetes which supports a relationship between diabetes and CRC [9], but when the persons with EOCRC were compared to 66 persons with asymptomatic LOCRC discovered by screening, no significant differences in prevalence of obesity (30% vs 36%) [9] or diabetes (6.3% vs 11%) were observed (unpublished data) (Fig. 2).

Adapted from: Strum WB and Boland CR (2019, in press) [9]. Data not previously presented
Locations of EOCRC and screen-detected LOCRC. A comparison of proximal and distal locations of early-onset versus late-onset, screen-detected and late-onset, symptom-detected colorectal cancer demonstrates the anatomic differences which are highly significant.
Tobacco-related carcinogens can reach the colorectal mucosa through either the alimentary tract or the circulatory system and could exert a carcinogenic effect by DNA damage or altered expression of important cancer-related genes. Studies of associations between cigarette smoking and incident CRC have demonstrated MSI-high, CIMP-positive, and BRAF-mutated CRC subtypes, suggesting that epigenetic modifications might be involved in smoking-related CRCs [49]. Although no definite links of these factors have been specific to EOCRC, a better understanding of the connection of these factors to CRC, individually and collectively, could lead to targets permitting prevention as well as early detection of CRC in the young, as well as older persons.
There are large-scale targeted deep sequencing studies of EOCRC tumors looking for mutational signatures (other than MSI, CIMP, and LINE-1 hypomethylation) that might provide clues to defects (constitutional or acquired) in DNA repair systems [34, 35, 37, 50]. One possible avenue to be explored is whether there is an interaction between the microbiome and the response of colorectal epithelium to the effects of oxidative stress or other DNA-damaging processes. Such interactions could simultaneously account for changing risks for CRC over time, if linked significantly to changes in the microbiome, possibly modified by temporal changes in diet, obesity, physical activity, or other environmental influences.
New Screening Protocol
On May 30, 2018, the American Cancer Society initiated a qualified recommendation for average-risk adults to begin screening at age 45 years [4], 5 years earlier than most prior recommendations [51,52,53,54] which was endorsed by the American College of Gastroenterology, the American Gastroenterological Association, and the American Society for Gastrointestinal Endoscopy, while recognizing that the supporting evidence is limited. If fully implemented, this expansion of the screening age might be expected to capture up to fifty percent of the EOCRC population at an earlier stage, since about half of this population presents with CRC in their mid- to late 1940s and will have CRC by the time of examination. The impact of colonoscopy on removing colorectal adenomas may be limited as colorectal adenomas tend not to accelerate in growth until the sixth decade [53, 55, 56] and the number of patients needed to screen to prevent one CRC death may be unacceptably high. Additional concerns for a favorable outcome are raised by studies of screening for CRC in asymptomatic persons over the age of 50 years that have not routinely showed improved results over the past decade [57,58,59,60,61,62].
Rational Approach to Screening
While we wait for the results of further clinical, microbial, genetic, epidemiologic, and other studies that may provide more precise etiologic explanations for the rise in CRC in young adults, incremental reductions in the rise in incidence of EOCRC could occur with certain tools immediately available. These include obtaining a detailed family history, adhering to the newly recommended age of 45 years to begin CRC screening for all average-risk adults (which could begin with noninvasive screening and advance if the initial tests are positive), continuing to screen at age 40 years or younger for persons with added risk from a positive family history, and consideration of earlier screening for persons with a combinations of risk factors. Additional recommendations include: (1) endoscopy of at least the distal colon in young persons with unexplained rectal bleeding; (2) a complete colonoscopy if a firm explanation for bleeding is not established, a polyp or tumor is found, or unexplained iron-deficiency anemia is present; (3) appropriate imaging tests for persons with unexplained abdominal pain; and (4) continued promotion of a healthy diet, maintenance of ideal body weight, cessation of tobacco exposure and excess alcohol, and a physically active life style.
References
Siegel RL, Miller KD, Jemal A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970–2014. JAMA. 2017;318:572–574.
Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst. 2017;109:djw322.
Siegel RL, Jemal A, Ward EM. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cospons Am Soc Prev Oncol. 2009;18:1695–1698.
Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:31.
Abdelsattar ZM, Wong SL, Regenbogen SE, Jomaa DM, Hardiman KM, Hendren S. Colorectal cancer outcomes and treatment patterns in patients too young for average-risk screening. Cancer. 2016;122:929–934.
Myers EA, Feingold DL, Forde KA, Arnell T, Jang JH, Whelan RL. Colorectal cancer in patients under 50 years of age: a retrospective analysis of two institutions’ experience. World J Gastroenterol. 2013;19:5651–5657.
Ahnen DJ, Wade SW, Jones WF, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc. 2014;89:216–224.
Chen FW, Sundaram V, Chew TA, Ladabaum U. Advanced-stage colorectal cancer in persons younger than 50 years not associated with longer duration of symptoms or time to diagnosis. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2017;15(728–37):e3.
Strum WB, Boland CR. Characterization and identification of colorectal cancer in persons younger than 50 years. Clin Gastroenterol Hepatol. 2018. https://doi.org/10.1016/j.cgh.2018.12.003.
Murphy CC, Wallace K, Sandler RS, Baron JA. Racial disparities in incidence of Young–Onset colorectal cancer and patient survival. Gastroenterology. 2019;156:958–965.
Zbuk K, Sidebotham EL, Bleyer A, La Quaglia MP. Colorectal cancer in young adults. Semin Oncol. 2009;36:439–450.
Lowery JT, Ahnen DJ, Schroy PC 3rd, et al. Understanding the contribution of family history to colorectal cancer risk and its clinical implications: a state-of-the-science review. Cancer. 2016;122:2633–2645.
Fuchs CS, Giovannucci EL, Colditz GA, Hunter DJ, Speizer FE, Willett WC. A prospective study of family history and the risk of colorectal cancer. New Engl J Med. 1994;331:1669–1674.
Ziogas A, Horick NK, Kinney AY, et al. Clinically relevant changes in family history of cancer over time. JAMA. 2011;306:172–178.
Strum WB. Impact of a family history of colorectal cancer on age at diagnosis, anatomic location, and clinical characteristics of colorectal cancer. Int J Gastrointest Cancer. 2005;35:121–126.
Tsai FC, Strum WB. Impact of a family history of colorectal cancer on the prevalence of advanced neoplasia at colonoscopy in 4967 asymptomatic patients. Dig Dis Sci. 2012;57:3234–3239.
Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med. 2000;342:69–77.
Goel A, Nagasaka T, Spiegel J, Meyer R, Lichliter WE, Boland CR. Low frequency of Lynch syndrome among young patients with non-familial colorectal cancer. Clin Gastroenterol Hepatol. 2010;8:966–971.
Giraldez MD, Balaguer F, Bujanda L, et al. MSH6 and MUTYH deficiency is a frequent event in early-onset colorectal cancer. Clin Cancer Res. 2010;16:5402–5413.
Mork ME, You YN, Ying J, et al. High prevalence of hereditary cancer syndromes in adolescents and young adults with colorectal cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33:3544–3549.
Pearlman R, Frankel WL, Swanson B, et al. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncol. 2017;3:464–471.
Stoffel EM, Koeppe E, Everett J, et al. Germline genetic features of young individuals with colorectal cancer. Gastroenterology. 2018;154(897–905):e1.
Yurgelun MB, Kulke MH, Fuchs CS, et al. Cancer susceptibility gene mutations in individuals with colorectal cancer. J Clin Oncol. 2017;35:1086–1095.
Boland CR, Thibodeau SN, Hamilton SR, et al. A National Cancer Institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58:5248–5257.
Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96:261–268.
Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. 2010;138(2073–87):e3.
Berera S, Koru-Sengul T, Miao F, et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14:1163–1171.
de la Chapelle A, Hampel H. Clinical relevance of microsatellite instability in colorectal cancer. J Clin Oncol. 2010;28:3380–3387.
Haraldsdottir S, Hampel H, Tomsic J, et al. Colon and endometrial cancers with mismatch repair deficiency can arise from somatic, rather than germline, mutations. Gastroenterology. 2014;147(1308–16):e1.
Sinicrope FA. Lynch syndrome-associated colorectal cancer. New Engl J Med. 2018;379:764–773.
Rodriguez-Soler M, Perez-Carbonell L, Guarinos C, et al. Risk of cancer in cases of suspected lynch syndrome without germline mutation. Gastroenterol. 2013;144:926–932.
Antelo M, Balaguer F, Shia J, et al. A high degree of LINE-1 hypomethylation is a unique feature of early-onset colorectal cancer. PLoS ONE. 2012;7:e45357.
Hur K, Cejas P, Feliu J, et al. Hypomethylation of long interspersed nuclear element-1 (LINE-1) leads to activation of proto-oncogenes in human colorectal cancer metastasis. Gut. 2014;63:635–646.
Perea J, Garcia JL, Perez J, et al. NOMO-1 gene is deleted in early-onset colorectal cancer. Oncotarget. 2017;8:24429–24436.
Brandariz L, Arriba M, Garcia JL, et al. Differential clinicopathological and molecular features within late-onset colorectal cancer according to tumor location. Oncotarget. 2018;9:15302–15311.
Silla IO, Rueda D, Rodriguez Y, Garcia JL, de la Cruz Vigo F, Perea J. Early-onset colorectal cancer: a separate subset of colorectal cancer. World J Gastroenterol. 2014;20:17288–17296.
Arriba M, Garcia JL, Rueda D, et al. Unsupervised analysis of array comparative genomic hybridization data from early-onset colorectal cancer reveals equivalence with molecular classification and phenotypes. Neoplasia. 2017;19:28–34.
Boardman LA, Johnson RA, Petersen GM, et al. Higher frequency of diploidy in young-onset microsatellite-stable colorectal cancer. Clin Cancer Res. 2007;13:2323–2328.
Liu C, Bettington ML, Walker NI, et al. CpG island methylation in sessile serrated adenomas increases with age, indicating lower risk of malignancy in young patients. Gastroenterology. 2018;155(1362–5):e2.
Ballester V, Cruz-Correa M. How and when to consider genetic testing for colon cancer? Gastroenterology. 2018;155:955–959.
Boland PM, Yurgelun MB, Boland CR. Recent progress in Lynch syndrome and other familial colorectal cancer syndromes. CA Cancer J Clin. 2018;68:217–231.
Carr PR, Weigl K, Jansen L, et al. Healthy lifestyle factors associated with lower risk of colorectal cancer irrespective of genetic risk. Gastroenterology. 2018;155(1805–15):e5.
Carethers JM. The increasing incidence of colorectal cancers diagnosed in subjects under age 50 among races: cracking the conundrum. Dig Dis Sci. 2016;61:2767–2769.
Sineshaw HM, Ng K, Flanders WD, Brawley OW, Jemal A. Factors that contribute to differences in survival of black vs white patients with colorectal cancer. Gastroenterology. 2018;154(906–15):e7.
Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–947.
Pan SY, DesMeules M. Energy intake, physical activity, energy balance, and cancer: epidemiologic evidence. Methods Mol Biol. 2009;472:191–215.
Ungefroren H, Gieseler F, Fliedner S, Lehnert H. Obesity and cancer. Horm Mol Biol Clin Investig. 2015;21:5–15.
Yuhara H, Steinmaus C, Cohen SE, Corley DA, Tei Y, Buffler PA. Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer? Am J Gastroenterol. 2011;106:1911–1921.
Limsui D, Vierkant RA, Tillmans LS, et al. Cigarette smoking and colorectal cancer risk by molecularly defined subtypes. J Natl Cancer Inst. 2010;102:1012–1022.
Arriba M, Garcia JL, Inglada-Perez L, et al. DNA copy number profiling reveals different patterns of chromosomal instability within colorectal cancer according to the age of onset. Mol Carcinog. 2016;55:705–716.
Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: recommendations for physicians and patients from the US multi-society task force on colorectal cancer. Gastroenterology. 2017;153:307–323.
Inadomi JM. Screening for colorectal neoplasia. New Engl J Med. 2017;376:149–156.
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for colorectal cancer: US preventive services task force recommendation statement. JAMA. 2016;315:2564–2575.
Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US preventive services task force. JAMA. 2016;315:2576–2594.
Pendergrass CJ, Edelstein DL, Hylind LM, et al. Occurrence of colorectal adenomas in younger adults: an epidemiologic necropsy study. Clin Gastroenterol Hepatol. 2008;6:1011–1015.
Tsai FC, Strum WB. Prevalence of advanced adenomas in small and diminutive colon polyps using direct measurement of size. Dig Dis Sci. 2011;56:2384–2388.
Strum WB. Unrequited returns in asymptomatic colorectal cancer detection. Clin Surg. 2018;3:1–5.
Strum WB. Colorectal adenomas. New Engl J Med. 2016;374:1065–1075.
Welch HG, Robertson DJ. Colorectal cancer on the decline-why screening can’t explain it all. New Engl J Med. 2016;374:1605–1607.
Liang PS, Allison J, Ladabaum U, et al. Potential intended and unintended consequences of recommending initiation of colorectal cancer screening at age 45 years. Gastroenterology. 2018;155:950–954.
Imperiale TF, Kahi CJ, Rex DK. Lowering the starting age for colorectal cancer screening to 45 years: who will come…and should they? Clin Gastroenterol Hepatol. 2018;16:1541–1544.
Corley DA, Peek RM Jr. When should guidelines change? A clarion call for evidence regarding the benefits and risks of screening for colorectal cancer at earlier ages. Gastroenterology. 2018;155:947–949.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Williamson Strum has none to declare; Dr C. Richard Boland is a Consultant with Ambry Genetics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Strum, W.B., Boland, C.R. Clinical and Genetic Characteristics of Colorectal Cancer in Persons under 50 Years of Age: A Review. Dig Dis Sci 64, 3059–3065 (2019). https://doi.org/10.1007/s10620-019-05644-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05644-0