Abstract
Background
Irritable bowel syndrome (IBS) is a common chronic disorder of the gastrointestinal tract. Several treatments have been developed, including rifaximin for the treatment of IBS without constipation (non-IBS-C), but no studies have evaluated the effect of these therapies on patient referral rates to tertiary care gastroenterology clinics.
Aim
To assess referral patterns for IBS patients at a tertiary motility clinic over a 10-year period.
Methods
Data from consecutive patients referred to the clinic during 2006–2016 were analyzed. Trends in the proportion of referrals and prior rifaximin use in IBS-C versus non-IBS-C groups were compared.
Results
A total of 814 adult patients were referred to a single physician panel for IBS-related symptoms. Of these, 776 were included in the study [528 females (68%), average age 45.7 ± 15.9 years), comprising 431 IBS-C (55.5%) and 345 non-IBS-C (44.5%) patients. The proportion of non-IBS-C referrals declined significantly from 53.0% in 2006 to 27.3% in 2016 (Chi-square, p < 0.0001, Cochran–Armitage trend test p = 0.0001), and the proportion of IBS-C referrals increased significantly from 46.9% in 2006 to 72.7% in 2016 (Chi-square, p < 0.0001, Cochran–Armitage trend test p = 0.0004). Non-IBS-C referrals with prior rifaximin use significantly increased from 22.7% in 2006 to 66.7% in 2016 (Cochran–Armitage trend test, p = 0.008).
Conclusions
The results indicate a significantly declining tertiary care referral rate for non-IBS-C over the past decade. While not directly linked, there has been an increase in rifaximin use in the same population during the same time interval.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
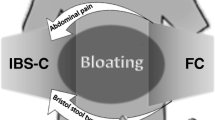
Irritable bowel syndrome (IBS) is one of the most common chronic disorders of the gastrointestinal tract [1]. Currently, the condition is diagnosed by the Rome IV criteria, which mandates that individuals must have abdominal pain for at least 1 day per week that is associated with defecation, changes in stool frequency, or changes in stool appearance for at least a 3-month period [2]. Furthermore, IBS is classified into three principle subtypes based on the predominant bowel disorder: IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), and IBS with mixed symptoms (IBS-M) [2]. The pooled prevalence of IBS has been estimated to be 11.2% globally (95% CI 9.8–12.8%) and 11.8% in the USA (95% CI 7.4–17.2%) [3]. In a meta-analysis of 14 studies of patients with IBS, IBS-D was the most prevalent with 40.0% of the patient population (95% CI 31.0–48.0%), followed by IBS-C at 35.0% (95% CI 29.0–41.0%), then IBS-M at 23.0% (95% CI 15.0–31.0%) [3]. The high frequency of IBS-D constitutes a significant economic burden to the US healthcare system, with IBS-D patients incurring more than $2000 in additional costs per year when compared to matched controls ($9436 for IBS-D patients vs. $7169 for matched controls; p < 0.001) [4].
Despite IBS-D being a well-characterized and highly prevalent condition, it has traditionally been difficult to diagnose and equally difficult to manage medically, leading providers to refer individuals to tertiary care centers for further testing and treatment [1]. Although data for IBS patients in referral versus primary care setting is sparse, there are a few studies that indicate the challenges that physicians face when treating this population of patients. A study comparing IBS patients at a primary care clinic versus a referral center found that female IBS patients had significantly lower quality of life compared to the same cohort in the primary care setting [5]. Another study conducted in two different tertiary clinics in Germany found that the rate of physician visits for IBS is significantly more than those with inflammatory bowel disease (IBD) in the same time course. Further, these patients were dissatisfied with the physicians’ care and more given to having psychophysiological complaints [6]. Management has been highly focused on multimodal means of controlling symptoms, which include initial pharmacologic treatments with antispasmodics, tricyclic antidepressants, and antidiarrheals in conjunction with non-pharmacologic management such as diet, exercise, and stress relief [7].
Treatment failure is common for many patients, and primary care providers often refer patients to a gastroenterologist for further treatment with drugs such as alosetron, eluxadoline, or rifaximin [1, 8]. Some of these medications can have considerable side effects [9, 10]; however, rifaximin has been shown to be an effective and safe therapy for IBS-D and IBS-M, collectively categorized as IBS without constipation (non-IBS-C) [11, 12]. This was demonstrated in the TARGET 1 and 2 randomized controlled trials, where the studies showed that patients with non-IBS-C who received rifaximin had significantly more adequate relief of global IBS symptoms and bloating during the first 4 weeks after a 2-week course of treatment compared to those who received a placebo [11, 12]. Furthermore, rifaximin has been shown to provide significant sustained relief of IBS-D- and IBS-M-related symptoms for the entire 3 months of the TARGET 1 and 2 trials, in addition to repeat treatments for IBS-D in TARGET 3 [11,12,13]. Meta-analyses of rifaximin have reported adverse events in only 1.6% of patients [13, 14].
Despite rifaximin being increasingly used in outpatient treatment since the original TARGET trials in 2011, there have been no studies to determine whether this therapy has affected patient flow to referral centers. Our hypothesis was that since the emergence of rifaximin as a treatment for non-IBS-C, a significant decline in the rates of referrals for patients with non-IBS-C compared to patients with IBS-C would be identifiable within 5 years (2011–2016). We tested this hypothesis by examining the rate of IBS patient referrals to a tertiary care motility program over a decade (2006–2016) and assessed any effect of new treatments on this.
Methods
Study Design
This study was a retrospective chart review of patients referred to a single gastroenterology physician panel in the GI Motility Clinic at Cedars-Sinai Medical Center, a tertiary care center located in Los Angeles. Data from consecutive new consults were collected between July 2006 and April 2016.
Study Population
The study population included patients referred for IBS symptoms including abdominal pain or discomfort, bloating, diarrhea, constipation, and bacterial overgrowth. Among subjects with a referring diagnosis of IBS, the relative proportion of subjects whose presenting complaints included some component of diarrhea, constipation, or both, as well as prior rifaximin usage, was determined and compared across time. All data used in this study were de-identified and accessed using protocols compliant with the Institutional Review Board at Cedars-Sinai Medical Center.
Inclusion Criteria
Inclusion criteria for the study were adult patients referred for IBS as documented by the clinician at the time of visit. The subtypes of IBS were recorded by study personnel according to Rome II criteria for consistency and standardization with patients diagnosed as early as 2006. Patients who had previously received rifaximin, antidiarrheal agents, narcotics, and/or antidepressants for the treatment of IBS-D prior to the referral were also included, as this represents the general IBS population.
Exclusion Criteria
Patients with a history of IBD, celiac disease, uncontrolled HIV, and any other disease that may mask IBS, such as infectious colitis or malignancies, were excluded.
Data Collection and Management
From the de-identified charts, patients’ sex, age, ethnicity, referring symptoms, diagnosis, comorbidities, prior rifaximin usage, concluding diagnosis, and number and types of physicians seen prior to the referral were recorded. The subtypes of IBS (IBS-C, IBS-D, IBS-M) were recorded by study personnel reviewing the charts according to the earlier Rome II criteria. This was done to standardize diagnostic criteria, as this retrospective chart review spanned 10 years, during which time physicians for the most part were using Rome II criteria. The primary data point was to compare the rates of referral for IBS-C versus non-IBS-C (IBS-D and IBS-M) diagnosis over this time period. IBS-D and IBS-M diagnoses were grouped together versus the IBS-C population as this often reflects the dichotomization of the groups for the pharmacologic treatment strategies. Secondary data points included rates of previous rifaximin use.
Data Analysis
Approximately 60% of subjects referred to the center are referred for IBS. Based on a review conducted prior to this study, it was estimated that in 2006 nearly 50% of IBS subjects referred to this clinic were from the IBS-D subgroup, as compared to the most recent patient population which estimated that approximately 20% of IBS subjects had IBS-D. Based on a comparison of year 1 and year 10 rates, sufficient charts were reviewed to identify 57 IBS subjects per year, allowing for the rejection of the null hypothesis with a probability (power) of 0.9. The type I error probability associated with the test of this null hypothesis is 0.05.
Data were processed using SPSS (IBM Corporation, Armonk, NY, USA) and Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) software. A descriptive statistical analysis of the IBS population examined at our center across 10 years was performed. The trend in the prevalence of IBS-C and non-IBS-C groups over time, the proportion of previous rifaximin use, and the association between the two were analyzed using the Cochran–Armitage trend test and Chi-squared test [15]. The alpha level of significance was set at p < 0.05.
Results
Patient and Clinical Characteristics
Between 2006 and 2016, a total of 814 contiguous adult patients were directly referred to a single physician panel in the GI Motility Clinic at Cedars-Sinai Medical Center for IBS-related symptoms. After application of the inclusion and exclusion criteria, 776 were included in the study with a diagnosis of either IBS-C or non-IBS-C (i.e. IBS-D or IBS-M). The most common causes of exclusion included IBD and history of multiple gastrointestinal surgeries requiring further surgical and anatomical evaluation. Of those 776 patients, 248 patients were male and 528 patients were female, 31.9% and 68%, respectively. The mean age was 45.7 ± 15.9 years old, ranging from 18 to 91 years old. A total of 431 patients were diagnosed with IBS-C, and 345 patients diagnosed with non-IBS-C, 55.5 and 44.5%, respectively (Table 1). Patient characteristics, when segregated into IBS-C and non-IBS-C groups, had similar average ages at 45.2 years and 44.7 years, respectively. However, the sex distribution was predominantly female in the IBS-C group at 80.8%, as compared to 61.8% in the non-IBS-C group.
Overall and Temporal Trends in the Rates of Referral for IBS-C and Non-IBS-C
In 2006, 47% of referrals were for IBS-C and 53% were for non-IBS-C. Five years later, in 2011, there was a marked change in the referral trend, with IBS-C increasing to 73.6% of referrals and non-IBS-C decreasing to 21.4% (Table 2). The overall proportion of non-IBS-C patients in the decade between 2006 and 2016 showed a significant trend towards a decrease in the rate of referral for non-IBS-C (from 53.0% in 2006 to 27.3% in 2016, R2 = −0.48), with Chi-square, p < 0.0001 and Cochran–Armitage trend test p = 0.0001. Consistent with this, there was an increasing trend in the proportion of IBS-C patients referred (from 46.9% in 2006 to 72.7% in 2016, R2 = 0.4808), with Cochran–Armitage trend test p = 0.0004, Chi-square, p < 0.0001 for IBS-C (Fig. 1). Excluding the year 2016, which had a much smaller sample size, the referral trend remained significant, with the decrease in the non-IBS-C group showing a Cochran–Armitage trend test p = 0.0002. In addition, the age and gender of referrals did not change over the study period.
Use of Rifaximin among Non-IBS-C Referrals
Between 2006 and 2016, the proportion of non-IBS-C referrals with previous rifaximin use increased significantly, from 22.7% in 2006 to 66.7% in 2016 (Cochran–Armitage trend test, p = 0.008) (Fig. 2). In particular, in the year 2011–2012, the use of rifaximin among the non-IBS-C referrals was the lowest (21.43%) and subsequently rose to its peak in 2016 at 66.7% (R2 = 0.3221). Of the referral population with non-IBS-C, there was a significant decline in rifaximin non-users between 2006 and 2016; in 2006, 77.3% of non-IBS-C referrals had no prior use of rifaximin, whereas in 2016, 33.3% of non-IBS-C referrals had no prior use. Excluding 2016 data, there was still a significant decline in rifaximin non-users with Cochran–Armitage trend test p = 0.013. This represents a significant overall trend towards increased use of rifaximin in the non-IBS-C referral population (Chi-square, p = 0.019).
Discussion
The population under study consisted of patients referred to a single physician panel for further treatment of IBS-related symptoms by either primary care providers or specialists. Trends over the study period are, however, clear. We found an overall decrease in the rate of referral for non-IBS-C (from 53% in 2006 to 27.3% in 2016) and an increase in the rate of referral for IBS-C (from 47% in 2006 to 72.7% in 2016), as seen in Fig. 1. Additionally, there appeared to be an inflection point after the year 2011–2012 where the use of rifaximin among the non-IBS-C referrals was the lowest (21.43%) and subsequently rose to its peak in 2016 at 66.7% (R2 = 0.3221). This coincides with the publication of the findings of the TARGET 1 and 2 studies for non-IBS-C [11]. These findings may suggest that rifaximin use in the community may be effectively treating patients with non-IBS-C symptoms and thereby lowering referral rates.
Another trend we identified was an increase in prior use of rifaximin in the non-IBS-C referral group. In 2006, only 22.7% of the non-IBS-C referrals had prior use of rifaximin, whereas in 2016, two-thirds of non-IBS-C referrals had previously been treated with the antibiotic. Based on this, one could hypothesize that rifaximin has become a common therapy for non-IBS-C, and may be a possible reason for the decrease in referrals for this condition. One could further hypothesize that the rifaximin-using population now being referred are patients who experienced symptom relapse and who are undergoing retreatment, as seen in the TARGET 3 study population [12]. The TARGET 3 trial demonstrated that 35.6% of patients did not experience IBS-D symptom relapse for up to 18 weeks following treatment with rifaximin, which approximately correlates to the 26% decline in the non-IBS-C population over the years.
The results of this study have several important implications. Our study is the first to examine trends in IBS patient referrals to a tertiary care motility program. Current epidemiologic studies report that among patients with IBS, the three subtypes are approximately equally divided, with the IBS-C subtype comprising around 35% [16]. Our study, however, has shown that by 2015 and 2016, IBS-C patients were comprising nearly 60% of the population being referred for treatment. As noted above, we hypothesize that non-IBS-C patients are being treated more adequately in the community setting, a trend which coincided with an increase in treatment with rifaximin. Although rifaximin may not be the sole explanation for the decreasing trend in the referral of non-IBS-C patients, there have been no major changes in management or pharmacotherapy for this population subgroup since the TARGET studies. Our study also had the advantage of following trends within a single physician panel at one patient care center over the study period, minimizing other confounders in the referral pattern.
This changing pattern of referral can also be attributed to the overall changing pattern of clinical care that IBS patients are seeking and receiving. The epidemiology studies that report the prevalence of IBS frequently utilize community surveys, which vary due to individuals reporting symptoms or offering a previous clinical diagnosis of IBS, which inherently assumes that they have sought medical care for their condition. This conflicts with reports that only approximately 25% of patients with IBS seek care with a physician [16]. It was theorized that only a small proportion of patients seek medical care because of the historical stigma associated with the diagnosis of IBS. However, IBS is increasingly being recognized as one of the most common functional disorders [17, 18] with a complex pathophysiology, which may be improving the stigma and encouraging these patients to seek treatment. Additionally, in the primary care setting, IBS has traditionally been a disease that is difficult to diagnose given its heterogeneity and overlap with other functional disorders [19]. With the implementation of formal diagnostic criteria, such as Rome and the NICE guidelines, and studies demonstrating their applicability as useful diagnostic tools in the primary care setting, we hypothesize that primary care providers are increasingly diagnosing and treating IBS, which may explain the increasing trend in the use of rifaximin [20] and decreasing rate of referral.
Finally, the natural history of IBS, and specifically the different subtypes, may be changing from what was previously understood. We have so far associated the increasing use of rifaximin as a validation of the TARGET trials results. However, this also corresponds with the fact that many non-IBS-C patients are refractory to rifaximin therapy. Therefore, this study also underlines the need for the development of additional pharmacotherapy for the management of refractory IBS-D and IBS-M patients. IBS-C, on the other hand, has become increasingly predominant in the GI clinic. Our study indicated an increase in IBS-C relative to the other subtypes, which is reinforced by a similar finding by Sommers et al. who noted the increasing number, frequency, and associated economic burden of constipation-related emergency department visits from 2006 to 2011, illustrating the importance of early diagnosis and management of IBS-C in the outpatient setting [21]. Additionally, despite newer therapies emerging for constipation, one of the reasons for the rising proportion of IBS-C may be related to the increasing use of opioid medications since 2006 for the treatment of pain, which has a well-known side effect of constipation [22]. Although the newest Rome criteria distinguish opioid-induced constipation from IBS-C and chronic idiopathic constipation, the criteria we used in the study did not distinguish between the two identities as this was not employed at the inception of the database in 2006.
Our study has several important limitations. First, although we demonstrated a clear decrease in the rates of referral for non-IBS-C to a large, academic, tertiary care center, the study population was from a single physician panel associated with a single center. We recognize that this is a significant limitation in the study design as there lies an inherent bias associated with the patient population, and it is therefore difficult to generalize our data to the entire IBS population at large. However, this bias is presumably unchanged throughout the years, as this specific study evaluated the trend and change over a decade. Future research should include a larger, multicenter study of tertiary centers encompassing multiple physician–patient panels in order to identify further important trends in IBS. This could be done utilizing a national database of outpatient diagnoses using ICD-10 diagnosis codes of the IBS subtypes. Second, although the study period was a decade in length, it is possible that the non-IBS-C population may have longer term and more predictable relapsing and remitting courses of referral to tertiary care centers, given the retreatment protocols for patients on rifaximin. Third, the population studied is not a cross section of the total population and findings from this study may not be fully representative of the total population of patients with IBS. It should also be noted that this study may be susceptible to measurement bias from the use of medical chart reviews. Nonetheless, this study is, to our knowledge, the first to examine population trends in IBS referrals to a tertiary care center over a period of time when novel medications may have had an impact.
In summary, when examining IBS patient referrals to a tertiary care gastroenterology physician panel, the total rate of referral of patients with non-IBS-C compared to IBS-C showed a significant downward trend. This trend correlates with the rise in rifaximin use in patients with non-IBS-C, which is consistent with the efficacy findings for rifaximin in non-IBS-C patients in the TARGET trials. This specifically suggests that rifaximin use may be contributing to the overall decline in referral rates of non-IBS-C patients to tertiary care centers and increasing the incidence of IBS-C.
References
Ford AC, Lacy BE, Talley NJ. Irritable bowel syndrome. N Engl J Med. 2017;376:2566–2578.
Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393-1407.e1395.
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712-721.e714.
Buono JL, Mathur K, Averitt AJ, Andrae DA. Economic burden of inadequate symptom control among US commercially insured patients with irritable bowel syndrome with diarrhea. J Med Econ. 2017;20:353–362.
Simrén M, Abrahamsson H, Svedlund J, Björnsson E. Quality of life in patients with irritable bowel syndrome seen in referral centers versus primary care: the impact of gender and predominant bowel pattern. Scand J Gastroenterol. 2001;36:545–552.
Porsch U, Wanitschke R, Linhart P, et al. A consecutive study of patients with irritable bowel syndrome disease in two tertiary referral centers. Psychother Psych Med. 2001;51:267–275.
Pimentel M. Evidence-based management of irritable bowel syndrome with diarrhea. Am J Managed Care. 2018;24:S35–S46.
Hulisz D. The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Managed Care Pharm. 2004;10:299–309.
Chey WD, Chey WY, Heath AT, et al. Long-term safety and efficacy of alosetron in women with severe diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2004;99:2195.
FDA Drug Safety Communication. FDA warns about increased risk of serious pancreatitis with irritable bowel drug Viberzi (eluxadoline) in patients without a gallbladder. Silver Spring: Food and Drug Administration; 2017.
Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32.
Lembo A, Pimentel M, Rao SS, et al. Repeat treatment with rifaximin is safe and effective in patients with diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2016;151:1113–1121.
Menees SB, Maneerattannaporn M, Kim HM, Chey WD. The efficacy and safety of rifaximin for the irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2011;107:28.
Shah E, Pimentel M. Evaluating the functional net value of pharmacologic agents in treating irritable bowel syndrome. Aliment Pharmacol Therapeut. 2014;39:973–983.
Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11:375–386.
Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80.
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712-721 e714.
Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313:949–958.
Chandar AK. Diagnosis and treatment of irritable bowel syndrome with predominant constipation in the primary-care setting: focus on linaclotide. Int J Gen Med. 2017;10:385–393.
Engsbro AL, Begtrup LM, Kjeldsen J, et al. Patients suspected of irritable bowel syndrome—cross-sectional study exploring the sensitivity of Rome III criteria in primary care. Am J Gastroenterol. 2013;108:972.
Sommers T, Corban C, Sengupta N, et al. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110:572.
Kumar L, Barker C, Emmanuel A. Opioid-induced constipation: pathophysiology, clinical consequences, and management. Gastroenterol Res Pract. 2014;2014:141737.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Cedars-Sinai has licensing agreements with Salix Pharmaceuticals, Naia Pharmaceuticals, Gemelli Biotech, Inc., and Synthetic Biologics Inc. Mark Pimentel is a consultant for Salix Pharmaceuticals, Naia Pharmaceuticals, Synthetic Biologics Inc., Shire, and US Medical, is a board member of Gemelli Biotech and has received research funding from Salix Pharmaceuticals and Synthetic Biologics Inc. Ruchi Mathur is a board member of Gemelli Biotech and has received research funding from Valeant Pharmaceuticals and the American Diabetes Association. Ali Rezaie has received speaker and consultant fees from Commonwealth Laboratories, Actavis, and Salix Pharmaceuticals, and has received research funding from Valeant Pharmaceuticals, the American College of Gastroenterology, and the Kenneth Rainin Foundation. The remaining authors have no conflicts to disclose.
Rights and permissions
About this article
Cite this article
Oh, S.J., Tashjian, V.C., Mirocha, J. et al. Declining Rates of Referral for Irritable Bowel Syndrome Without Constipation at a Tertiary Care Center. Dig Dis Sci 64, 182–188 (2019). https://doi.org/10.1007/s10620-018-5302-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5302-2