Abstract
Background and Aim
The efficacy of nucleoside analogs (NAs) for hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) after curative treatment remains unclear. The present study aimed to evaluate the efficacy of these agents by conducting a comprehensive meta-analysis of available studies.
Methods
We searched several databases including Pubmed, Embase, Cochrane Library, Clinical Trials, and Web of Science, according to PRISMA guidelines. We considered all randomized controlled trials and cohort studies that met the inclusion criteria. Statistical analyses were conducted using Review Manager 5.3 and Stata 14.0.
Results
Twenty-one studies with 8752 participants were included in the final analysis. The pooled data showed that patients treated with NAs had significantly lower 1- and 3-year HCC recurrence rates (relative risk [RR] 0.76, 95% confidence interval [CI] 0.65–0.90; P = 0.001 and RR 0.79, 95% CI 0.71–0.88; P < 0.001, respectively), but there was no difference in 5-year recurrence rates (RR 0.87, 95% CI 0.74–1.03; P = 0.10). Regarding overall survival (OS), patients treated with NAs had significantly higher 1-, 3-, and 5-year OS rates (RR 1.05, 95% CI 1.02–1.08; P = 0.003; RR 1.25, 95% CI 1.16–1.34; P < 0.001; and RR 1.28, 95% CI 1.18–1.39; P < 0.001, respectively).
Conclusion
NA therapy has the potential to reduce the risk of early recurrence and improve OS in patients with HBV-related HCC after curative treatment, compared with placebo or no treatment. Further research including more homogeneous studies with large sample sizes is required to improve the reliability of these conclusions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is a common malignant tumor and the second-leading cause of cancer-related deaths worldwide [1]. In addition to liver transplantation, there are currently two treatment options for patients eligible for curative treatment: Partial hepatectomy represents a potentially curative therapy in patients with a solitary tumor of any size with no evidence of gross vascular invasion [2], while ablation, including radiofrequency ablation (RFA), microwave ablation, percutaneous ethanol injection, and acetic acid ablation, can be used in patients with Child–Pugh class A early-stage HCC (either a single tumor ≤ 5 cm or multiple tumors (up to 3 tumors) each ≤ 3 cm) [3,4,5,6,7,8,9,10]. These curative therapies have improved the overall survival (OS) rate, with some studies reporting a 5-year survival rate of > 50% [11,12,13] in patients undergoing liver resection and 70% for RFA [9]. However, the recurrence rate in patients after curative treatment remains poor, and some studies suggested that 5-year recurrence rates in patients after resection and RFA were all > 70% [12, 14, 15]. Adjuvant treatments that can reduce recurrence and further prolong survival are thus of major significance.
About 54.4% of HCC cases can be attributed to hepatitis B virus (HBV) infection [16]. Moreover, some studies of patients with chronic HBV-related HCC undergoing curative treatment reported that tumor recurrence increased in line with levels of HBV DNA. Several studies have investigated the association between the administration of nucleoside analogs (NA) and prognosis, including prolonged survival and decreased recurrence rates [17,18,19,20]. However, conclusions based on studies with small sample sizes are not convincing, and it is therefore necessary to carry out a meta-analysis to summarize and analyze the accumulated evidence to reach a more credible conclusion. In the present study, we retrieved and analyzed 21 studies including 8752 participants, which enabled us to conduct subgroup analyses according to study signs, type of curative treatment, and sample size. More comprehensive data and further research could help to identify the short- and long-term effects of NAs in patients with HBV-related HCC, in addition to providing credible evidence for clinicians.
Methods
Search Strategy and Selection Criteria
We conducted a systematic literature search of electronic databases including Pubmed, Embase, Cochrane Library, Clinical Trials, and Web of Science, in accordance with PRISMA guidelines [21], on April 15, 2018. The search terms included “hepatocellular carcinoma,” “liver cancer,” “liver neoplasms,” “HCC,” “hepatitis B,” “hepatitis B virus,” “HBV,” “curative treatment,” “resection,” “hepatectomy,” “ablation,” “percutaneous ethanol injection,” “radiofrequency ablation,” “microwave ablation,” “acetic acid ablation,” “antiviral,” “nucleotide,” “nucleoside,” “lamivudine,” “adefovir,” “entecavir,” “telbivudine,” and “tenofovir.” The search had no limitation on publication dates, but was restricted to articles published in English. We additionally manually searched primary references included in the earlier meta-analyses and continued to monitor the scientific literature after completing the formal search.
We considered all randomized controlled trials (RCTs) and cohort studies if they met the following inclusion criteria: (1) study population definitely diagnosed with HBV-related HCC; (2) treated for HCC by resection or ablation; (3) adjuvant postoperative treatment included NAs for treatment group and placebo or no treatment for control group; and (4) available results for HCC recurrence rate or OS rate. Studies were excluded if the patients suffered from coinfection with hepatitis C virus, hepatitis D virus, or human immunodeficiency virus. Two independent investigators screened the titles, abstracts, and full texts of the retrieved articles. Differences in opinion were resolved by discussion or arbitration by the third author.
Data Extraction
Two reviewers extracted relevant data independently using a standardized data extraction form. The extracted data included information on study design, mean age, sample size, tumor size, proportion of cirrhosis, α-fetoprotein, HBV DNA level, tumor stage, Child–Pugh class, curative treatment, NA type, treatment duration, follow-up duration, and specific data associated with HCC recurrence rate and OS rate.
Quality Assessment
The quality and risk of bias of the RCTs were evaluated using the Cochrane Collaboration tool [22]. The quality of cohort studies was assessed using the modified Newcastle Ottawa Scale (NOS), which evaluated the studies in terms of sample selection, comparability, and outcomes [23]. The NOS gives a maximum score of 9 points, and studies with a score > 5 were considered as high quality.
Data Analysis
Statistical analyses were conducted using Review Manager 5.3 and Stata 14.0. Pooled relative risks (RRs) and 95% confidence intervals (CIs) were used to evaluate the association between NAs and clinical benefit in patients with HBV-related HCC after curative treatment. In terms of incorporating summary time-to-event data into the meta-analysis, reported hazard ratios (HRs) were directly considered as RRs, and if HRs were not reported, published data from the original papers were used to calculate the HR using a spreadsheet developed by Tierney et al. [24]. We tested heterogeneity using Cochran’s Q statistic and Higgins I2 statistic. A value of P > 0.05 was considered to indicate no significant heterogeneity, I2 ≤ 25% indicated little heterogeneity, I2 > 25% and ≤ 50% moderate heterogeneity, I2 > 50% and ≤ 75% substantial heterogeneity, and I2 > 75% considerable heterogeneity [25]. A fixed-effects model was used if the heterogeneity was categorized as low or moderate and a random-effects model if it was considered to be substantial or considerable. We further investigated the possible reasons for any heterogeneity by subgroup analyses based on study design, sample size, and the type of curative treatment. Funnel plots and Egger’s test were used to assess publication bias. Two-tailed P values < 0.05 were considered statistically significant.
Results
Study Description
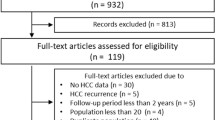
Our search identified 690 citations after the removal of duplicate references. A total of 114 abstracts and 34 full texts were further reviewed after review of the titles. Among the 34 potentially relevant studies, the following publications were excluded: one case report [26], five reviews [27,28,29,30,31], two studies [32, 33] referring to non-curative treatment with transarterial chemoembolization, and five studies [34,35,36,37,38] without relevant data to conduct a meta-analysis. Finally, 21 studies, including three studies [39,40,41] identified by manual search of previous meta-analyses, were confirmed. The 22 trials (one study [42] consisted of two trials) included 20 cohort studies [17,18,19,20, 39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54] and two RCTs [42, 55]. All the studies adjusted for important factors between the treatment and control groups, making the two groups comparable. The studies included 8752 participants, including 2288 patients exposed to NA in the treatment groups and 6464 exposed to placebo or without treatment in the control groups. The study screening process is shown in Fig. 1.
Among the included studies, 13 [17, 39,40,41,42, 44,45,46,47, 49,50,51, 54, 55] (n = 7789) adopted resection as a curative therapy, three studies [19, 52, 53] (n = 731) adopted ablation, and the remaining four studies [18, 20, 43, 48] (n = 232) adopted resection and/or ablation without further distinction. Among the trials included in this meta-analysis, lamivudine was the primary antiviral agent, except in one trial [55] that only used entecavir and adefovir. In the 21 trials using lamivudine, patients in 11 [17,18,19,20, 41,42,43,44,45, 47] took lamivudine as antiviral monotherapy and those in the other 10 [39, 40, 46, 48,49,50,51,52,53,54] used it in combination with other antiviral drugs such as entecavir, adefovir, and tenofovir. We assessed the risk of bias of the two RCTs as unclear based on the Cochrane Collaboration tool. The other 20 cohort studies were assessed as high quality by the NOS (Table S). The main characteristics are summarized in Table 1.
NA Therapy and HCC Recurrence Rate
The pooled data showed that patients treated with NAs had significantly lower 1- and 3-year HCC recurrence rates (RR 0.76, 95% CI 0.65–0.90; P = 0.001 and RR 0.79, 95% CI 0.71–0.88; P < 0.001, respectively), but there was no significant difference in 5-year recurrence rates between the treated and control groups (RR 0.87, 95% CI 0.74–1.03; P = 0.10). There was moderate heterogeneity (I2 = 46%, P = 0.03) in terms of 1-year HCC recurrence rate, substantial heterogeneity (I2 = 58%, P = 0.003) in 3-year recurrence rate, and considerable heterogeneity (I2 = 81%, P < 0.001) in 5-year recurrence rate (Fig. 2). We found no evidence of publication bias or small-study effect by Egger’s test (1-year recurrence rate: P = 0.522; 3-year recurrence rate: P = 0.968; 5-year recurrence rate: P = 0.974) or by visualization of funnel plots (Fig. 3).
NA Therapy and OS Rate
Pooled data showed that treatment with NA significantly improved 1-year OS (RR 1.05, 95% CI 1.02–1.08; P = 0.003), 3-year OS (RR 1.25, 95% CI 1.16–1.34; P < 0.001), and 5-year OS (RR 1.28, 95% CI 1.18–1.39; P < 0.001). There was considerable heterogeneity among studies in relation to 1-year OS (I2 =79%, P < 0.001) and 3-year OS (I2 = 79%, P < 0.001), and substantial heterogeneity (I2 = 60%, P = 0.001) among studies in relation to 5-year OS (Fig. 4). We detected some publication bias and a small-study effect by Egger’s test (1-year OS: P = 0.021; 3-year OS: P = 0.018; 5-year OS: P = 0.043) and by visualization of the funnel plot (Fig. 5).
Subgroup Analyses by Study Design, Curative Treatment, and Sample Size
Subgroup Analysis by Study Design
We pooled the data from cohort studies and RCTs. In the NA therapy group of cohort studies, the 1- and 3-year recurrence rates were significantly decreased by 21% and 20%, respectively, and 1-, 3-, and 5-year OS rates were significantly improved by 5, 23, and 27%, respectively. However, there was no significant difference in 5-year recurrence rates between the treated and control groups. There was a slight reduction in heterogeneity in the groups in relation to 1-year recurrence rate and 1-year OS, but not in relation to 3- and 5-year recurrence and OS rates. In the subgroup of RCTs, the meta-analysis demonstrated a significant difference between the groups for 3-year but not 1-year OS, or 1- or 3-year recurrence rates. There was no evidence of heterogeneity between the studies in relation to 3-year recurrence rate, while the heterogeneity in relation to 1-year recurrence rate and 1- and 3-year OS rates was similar to those before subgroup analysis (Table 2).
Subgroup Analysis According to Curative Treatment
In the subgroup adopting resection as the curative treatment, the pooled results demonstrated that NA therapy decreased both the 1- and 3-year recurrence rates by 24%, and improved the 1-, 3-, and 5-year OS rates by 6, 26, and 29%, respectively. However, there was no significant difference in 5-year recurrence rates. The heterogeneity among studies was slightly reduced in relation to 1-, 3-, and 5-year OS rates, but not 1-, 3-, or 5-year recurrence rates. In the subgroup of studies using RFA, the meta-analysis demonstrated no significant difference between the treatment and control groups for 3-year recurrence rate and 1-, 3-, and 5-year OS rates. There was no evidence of heterogeneity in relation to 1- and 3-year recurrence rates, while heterogeneities in relation to 1-, 3-, and 5-year OS rates were significantly reduced compared with before subgroup analysis (Table 2).
Subgroup Analysis Excluding Trials with Small and Too Large Sample Sizes
We defined a small sample size as < 100 patients in the trial. After excluding trials with small sample sizes [17, 18, 20, 39, 43, 44, 47, 48] and the study by Wu et al. [46], which had an obviously larger sample size (4569) than the other trials, we pooled the remaining studies and found significant differences between the therapy and control groups. Specifically, 1-, 3-, and 5-year recurrence rates were reduced in the therapy group by 23, 22, and 22%, respectively, while 1-, 3-, and 5-year OS rates were improved by 4, 27, and 24%, respectively. Heterogeneity among studies was not significantly reduced in relation to any of the outcomes (Table 2).
Side Effects of NA Therapy
We were unable to conduct a meta-analysis of the adverse effects because of insufficient data. Among the included studies, 24.6–39.4% of cases in six studies [17,18,19, 42, 43, 48] reported lamivudine-resistant tyrosine-methionine-aspartate-aspartate (YMDD) mutants after lamivudine therapy. Furthermore, 31.3–66.7% of YMDD patients in three studies [18, 39, 43] exhibited breakthrough hepatitis, which was controlled by administration of other kinds of NAs. No serious adverse effects were reported in the included studies, except for one patient who suffered from transient anorexia after the administration of lamivudine [42].
Discussion
This systematic review and meta-analysis of pooled data from 22 trials (20 cohort studies and 2 RCTs) demonstrated that NA therapy could reduce the early recurrence rate (by 24% and 21% at 1 and 3 years, respectively) and improve OS (by 5, 25, and 28% at 1, 3, and 5 years, respectively) in patients with HBV-related HCC after curative treatment. These results were consistent with the conclusions derived from cohort studies and studies with curative resection. In the subgroup of cohort studies, NAs reduced the 1- and 3-year recurrence rates by 21% and 20%, respectively, and improved the 1-, 3-, and 5-year OS rates by 5, 23, and 27%, respectively. In the subgroup of studies that adopted curative resection, NAs reduced the 1- and 3-year recurrence rates by 24% and improved the 1-, 3-, and 5-year OS rates by 6, 26, and 29%, respectively. However, NAs failed to reduce late recurrence in the overall and cohort studies, or in the studies using radical resection. To the best of our knowledge, five previous meta-analyses have assessed the association between NA therapy and the prognosis of patients with chronic HBV-related HCC after curative treatment [56,57,58,59,60]. Compared with the present study, the meta-analyses by Wong et al. [56], Sun et al. [57], Zhou et al. [58], and Liu et al. [60] showed that NAs could prolong OS and decrease recurrence, but did not differentiate between the short-term and long-term effects of NA therapy. Although Xia et al. [59] tried to identify short- and long-term effects, it did not exclude the effect of studies with small sample sizes. Moreover, the previous conclusions were based on fewer studies and smaller sample sizes, which may have reduced the credibility of the results.
In the current meta-analysis, we found that NA therapy significantly decreased the early recurrence rate at 1 and 3 years after curative treatment. Early recurrence can be attributed to dissemination of the initial HCC [61,62,63]. Furthermore, a high viral concentration has been reported to lead to aggressive behavior of HCC resulting in tumor recurrence via intrahepatic metastasis and growth [39, 64]. NA therapy may thus have decreased the early recurrence rate by inhibiting viral replication and decreasing the viral concentration. However, we failed to find any effect of NA therapy on late recurrence. These results were consistent with the meta-analysis conducted by Xia et al. [59], which reported that NA therapy failed to reduce the late recurrence rate, but decreased the 1- and 3-year recurrence rates by 23% and 19%, respectively. There are two possible reasons for this result. First, although NAs could delay the progression of recurrence, they do not exert any antitumor effect. If any micrometastases that were not detected before partial hepatectomy persisted in the remnant liver, the HCC would still be likely to relapse. Alternatively, the observed results may have been due to small-study effects. When we excluded studies [18, 48] with sample sizes <100, the pooled results showed a significant reduction in late recurrence rate. However, further studies should be conducted to verify the stability of this conclusion.
Our meta-analysis revealed that NA therapy could significantly improve OS rates in patients with HBV-related HCC at 1, 3, and 5 years after liver resection or ablation, in accordance with the conclusions of previous meta-analyses. These improvements may have two possible explanations. First, the reduced and postponed recurrence of HCC may delay disease progression and correspondingly increase survival time. Second, NA administration could effectively improve liver function, as demonstrated by improvements in indicators such as albumin, aspartate aminotransferase, and alanine aminotransferase compared with levels at baseline [43]. An improved liver reserve would thus allow more kinds of salvage therapy to be administered in the event of HCC recurrence, including resection and ablation, while patients with less liver reserve would have fewer treatment options and thus shorter survival.
In the subgroup analysis according to study design, the pooled results from cohort studies were consistent with those of the overall analysis in relation to survival rate and recurrence rate. However, NA therapy failed to display any significant benefits in recurrence or OS rates using pooled data from RCTs [42, 55], possibly due to the small number of trials and small sample sizes. In the subgroup analysis according to type of curative treatment, analysis of pooled data from studies using curative resection produced the same conclusions as analysis of the cohort subgroup study, while the pooled results from RFA studies showed no significant difference between the treatment and control groups in terms of 3-year recurrence rate and 1-, 3-, and 5-year OS rates. However, further studies are needed to validate these conclusions, which were derived from only three studies.
This study was subject to several limitations. First, given that all but two of the included studies were cohort studies, this may have resulted in selection and performance biases that could reduce the credibility of the conclusions. Second, the heterogeneities of the pooled studies for recurrence rate and OS were significant, and subgroup analyses according to study design, curative treatment, and sample size failed to decrease this significance. The most probable reason for the significant heterogeneities among the included studies was differences in HBV DNA levels, which have been shown to be associated with the prognosis of HBV-related HCC after curative treatment. Other reasons, such as tumor size, the percent of cirrhosis, and treatment duration, may also partially explain the source of the heterogeneities. Third, there was evidence of publication bias and a small-study effect in relation to OS, which may derive from the authors’ inclinations to publish positive rather than negative results.
In conclusion, this meta-analysis of 2288 participants exposed to NAs showed that NA therapy could reduce the early recurrence rate and improve OS compared with placebo or no treatment in patients with HBV-related HCC after curative treatment. Overall, NA was well tolerated, with few serious adverse effects. However, in view of the heterogeneity and publication bias identified in this study, further research including more homogeneous studies with larger sample sizes is needed to improve the reliability of the conclusions.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Truty MJ, Vauthey J-N. Surgical resection of high-risk hepatocellular carcinoma: patient selection, preoperative considerations, and operative technique. Ann Surg Oncol. 2010;17:1219–1225.
Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999;210:655–661.
Lencioni RA, Allgaier HP, Cioni D, et al. Small hepatocellular carcinoma in cirrhosis: randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology. 2003;228:235–240.
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma < or =4 cm. Gastroenterology. 2004;127:1714–1723.
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut. 2005;54:1151–1156.
Shiina S, Teratani T, Obi S, et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology. 2005;129:122–130.
Brunello F, Veltri A, Carucci P, et al. Radiofrequency ablation versus ethanol injection for early hepatocellular carcinoma: a randomized controlled trial. Scand J Gastroenterol. 2008;43:727–735.
Giorgio A, Di Sarno A, De Stefano G, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma compared to percutaneous ethanol injection in treatment of cirrhotic patients: an Italian randomized controlled trial. Anticancer Res. 2011;31:2291–2295.
Weis S, Franke A, Mossner J, Jakobsen JC, Schoppmeyer K. Radiofrequency (thermal) ablation versus no intervention or other interventions for hepatocellular carcinoma. Cochrane Database Syst Rev. 2013;12:Cd003046.
Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999;30:1434–1440.
Kianmanesh R, Regimbeau JM, Belghiti J. Selective approach to major hepatic resection for hepatocellular carcinoma in chronic liver disease. Surg Oncol Clin N Am. 2003;12:51–63.
Chok KS, Ng KK, Poon RT, Lo CM, Fan ST. Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg. 2009;96:81–87.
Huang J, Yan L, Cheng Z, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg. 2010;252:903–912.
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236.
Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030–3044.
Kubo S, Tanaka H, Takemura S, et al. Effects of lamivudine on outcome after liver resection for hepatocellular carcinoma in patients with active replication of hepatitis B virus. Hepatol Res. 2007;37:94–100.
Kuzuya T, Katano Y, Kumada T, et al. Efficacy of antiviral therapy with lamivudine after initial treatment for hepatitis B virus-related hepatocellular carcinoma. J Gastroenterol Hepatol. 2007;22:1929–1935.
Yoshida H, Yoshida H, Goto E, et al. Safety and efficacy of lamivudine after radiofrequency ablation in patients with hepatitis B virus-related hepatocellular carcinoma. Hepatol Int. 2008;2:89–94.
Chuma M, Hige S, Kamiyama T, et al. The influence of hepatitis B DNA level and antiviral therapy on recurrence after initial curative treatment in patients with hepatocellular carcinoma. J Gastroenterol. 2009;44:991–999.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6:e1000097.
Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed July 6, 2014.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Wei Q, Xu X, Ling Q, Zheng S. Indefinite antiviral therapy may be required after surgical resection for hepatocellular carcinoma complicating chronic hepatitis. Bos J Res Med Sci. 2013;18:726–730.
Yu Y, Ai J, Zhang W. Current clinical evidence for nucleos(t)ide analogues in patients with HBV-related hepatocellular carcinoma. Expert Rev Gastroenterol Hepatol. 2017;11:925–937.
Yang X, Gao JY, Wang J, Cheng J. The impact of anti-HBV treatment on the occurrence and recurrence of hepatocellular carcinoma: focus on Asian studies. Discov Med. 2015;19:89–99.
Kubo S, Takemura S, Tanaka S, et al. Management of hepatitis B virus infection during treatment for hepatitis B virus-related hepatocellular carcinoma. World J Gastroenterol. 2015;21:8249–8255.
Tan ZM, Sun BC. Effects of antiviral therapy on preventing liver tumorigenesis and hepatocellular carcinoma recurrence. World J Gastroenterol. 2013;19:8895–8901.
Ishikawa T. Anti-viral therapy to reduce recurrence and improve survival in hepatitis B virus-related hepatocellular carcinoma. World J Gastroenterol. 2013;19:8861–8866.
Wong GL, Tse YK, Chan HL, Yip TC, Tsoi KK, Wong VW. Oral nucleos(t)ide analogues reduce recurrence and death in chronic hepatitis B-related hepatocellular carcinoma. Aliment Pharmacol Ther. 2016;43:802–813.
Zhu SL, Zhong JH, Ke Y, et al. Comparative efficacy of postoperative transarterial chemoembolization with or without antiviral therapy for hepatitis B virus-related hepatocellular carcinoma. Tumour Biol J Int Soc Oncodev Biol Med. 2015;36:6277–6284.
Gong WF, Zhong JH, Lu SD, et al. Effects of antiviral therapy on post-hepatectomy HBV reactivation and liver function in HBV DNA-negative patients with HBV-related hepatocellular carcinoma. Oncotarget. 2017;8:15047–15056.
Zhong JH, Ke Y, Zhu SL, et al. Adefovir dipivoxil is less expensive than lamivudine and associated with similar prognosis in patients with hepatitis B virus-related hepatocellular carcinoma after radical resection. OncoTargets Therapy. 2016;9:6897–6907.
Zhang ZY, Zhou ZQ, Zhou GW. Higher efficacy of antiviral therapy after major hepatectomy in patients with hepatitis B virus-related hepatocellular carcinoma of less than 3 cm. Eur J Gastroenterol Hepatol. 2014;26:1116–1124.
Yeh YC, Liu CJ, Kuo RN, et al. Association of adjuvant antiviral therapy with risk of cancer progression and deaths in patients with hepatitis-B-virus-related hepatocellular carcinoma following curative treatment: a nationwide cohort study. PloS One. 2014;9:e102051.
Jin YJ, Shim JH, Lee HC, et al. Suppressive effects of entecavir on hepatitis B virus and hepatocellular carcinoma. J Gastroenterol Hepatol. 2011;26:1380–1388.
Urata Y, Kubo S, Takemura S, et al. Effects of antiviral therapy on long-term outcome after liver resection for hepatitis B virus-related hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2012;19:685–696.
Yang T, Lu JH, Zhai J, et al. High viral load is associated with poor overall and recurrence-free survival of hepatitis B virus-related hepatocellular carcinoma after curative resection: a prospective cohort study. Eur J Surg Oncol. 2012;38:683–691.
Ke Y, Ma L, You XM, et al. Antiviral therapy for hepatitis B virus-related hepatocellular carcinoma after radical hepatectomy. Cancer Biol Med. 2013;10:158–164.
Yin J, Li N, Han Y, et al. Effect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus-related hepatocellular carcinoma: a two-stage longitudinal clinical study. J Clin Oncol. 2013;31:3647–3655.
Koda M, Nagahara T, Matono T, et al. Nucleotide analogs for patients with HBV-related hepatocellular carcinoma increase the survival rate through improved liver function. Intern Med. 2009;48:11–17.
Li N, Lai EC, Shi J, et al. A comparative study of antiviral therapy after resection of hepatocellular carcinoma in the immune-active phase of hepatitis B virus infection. Ann Surg Oncol. 2010;17:179–185.
Chan AC, Chok KS, Yuen WK, et al. Impact of antiviral therapy on the survival of patients after major hepatectomy for hepatitis B virus-related hepatocellular carcinoma. Arch Surg. 2011;146:675–681.
Wu CY, Chen YJ, Ho HJ, et al. Association between nucleoside analogues and risk of hepatitis B virus-related hepatocellular carcinoma recurrence following liver resection. JAMA. 2012;308:1906–1914.
Yan Q, Ni J, Zhang GL, et al. Efficacy of postoperative antiviral combined transcatheter arterial chemoembolization therapy in prevention of hepatitis B-related hepatocellular carcinoma recurrence. Chin Med J (Engl). 2013;126:855–859.
Nishikawa H, Nishijima N, Arimoto A, et al. Effect of nucleoside analog use in patients with hepatitis B virus-related hepatocellular carcinoma. Hepatol Res. 2014;44:608–620.
Chong CC, Wong GL, Wong VW, et al. Antiviral therapy improves post-hepatectomy survival in patients with hepatitis B virus-related hepatocellular carcinoma: a prospective-retrospective study. Aliment Pharmacol Ther. 2015;41:199–208.
Sakamoto K, Beppu T, Hayashi H, et al. Antiviral therapy and long-term outcome for hepatitis B virus-related hepatocellular carcinoma after curative liver resection in a Japanese cohort. Anticancer Res. 2015;35:1647–1655.
Chen JL, Lin XJ, Zhou Q, Shi M, Li SP, Lao XM. Association of HBV DNA replication with antiviral treatment outcomes in the patients with early-stage HBV-related hepatocellular carcinoma undergoing curative resection. Chin J Cancer. 2016;35:28.
Lee TY, Lin JT, Zeng YS, Chen YJ, Wu MS, Wu CY. Association between nucleos(t)ide analog and tumor recurrence in hepatitis B virus-related hepatocellular carcinoma after radiofrequency ablation. Hepatology. 2016;63:1517–1527.
Sohn W, Kang TW, Choi SK, et al. Effect of oral antiviral treatment on long-term outcomes of radiofrequency ablation therapy for hepatitis B virus-related hepatocellular carcinoma. Oncotarget. 2016;7:47794–47807.
Wei Q, Tian H, Luo HX, et al. Better prognosis of hepatic resection combined with antiviral therapy for HBV-related hepatocellular carcinoma with BCLC Stage B/C. Asian J Surg. 2017;40:453–462.
Huang G, Lau WY, Wang ZG, et al. Antiviral therapy improves postoperative survival in patients with hepatocellular carcinoma: a randomized controlled trial. Ann Surg. 2015;261:56–66.
Wong JS, Wong GL, Tsoi KK, et al. Meta-analysis: the efficacy of anti-viral therapy in prevention of recurrence after curative treatment of chronic hepatitis B-related hepatocellular carcinoma. Aliment Pharmacol Ther. 2011;33:1104–1112.
Sun P, Dong X, Cheng X, Hu Q, Zheng Q. Nucleot(s)ide analogues for hepatitis B virus-related hepatocellular carcinoma after curative treatment: a systematic review and meta-analysis. PLoS One. 2014;9:e102761.
Zhou Y, Zhang Z, Zhao Y, Wu L, Li B. Antiviral therapy decreases recurrence of hepatitis B virus-related hepatocellular carcinoma after curative resection: a meta-analysis. World J Surg. 2014;38:2395–2402.
Xia BW, Zhang YC, Wang J, Ding FH, He XD. Efficacy of antiviral therapy with nucleotide/nucleoside analogs after curative treatment for patients with hepatitis B virus-related hepatocellular carcinoma: a systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2015;39:458–468.
Liu GM, Huang XY, Shen SL, Hu WJ, Peng BG. Adjuvant antiviral therapy for hepatitis B virus-related hepatocellular carcinoma after curative treatment: a systematic review and meta-analysis. Hepatol Res. 2016;46:100–110.
Hung IF, Poon RT, Lai CL, Fung J, Fan ST, Yuen MF. Recurrence of hepatitis B-related hepatocellular carcinoma is associated with high viral load at the time of resection. Am J Gastroenterol. 2008;103:1663–1673.
Wu JC, Huang YH, Chau GY, et al. Risk factors for early and late recurrence in hepatitis B-related hepatocellular carcinoma. J Hepatol. 2009;51:890–897.
Chen L, Zhang Q, Chang W, Du Y, Zhang H, Cao G. Viral and host inflammation-related factors that can predict the prognosis of hepatocellular carcinoma. Eur J Cancer. 2012;48:1977–1987.
Kubo S, Hirohashi K, Tanaka H, et al. Effect of viral status on recurrence after liver resection for patients with hepatitis B virus-related hepatocellular carcinoma. Cancer. 2000;88:1016–1024.
Funding
This study was funded by the National Natural Science Foundation of China (No. 81760497).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, G., Yu, X., Liu, P. et al. Efficacy of Nucleoside Analogs for Chronic Hepatitis B Virus-Related Hepatocellular Carcinoma After Curative Treatment: A Meta-Analysis. Dig Dis Sci 63, 3207–3219 (2018). https://doi.org/10.1007/s10620-018-5252-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5252-8